Health Care > QUESTIONS & ANSWERS > NSG 6020 WEEK 1 QUIZ BUILDING A COMPREHENSIVE HEALTH HISTORY (All)
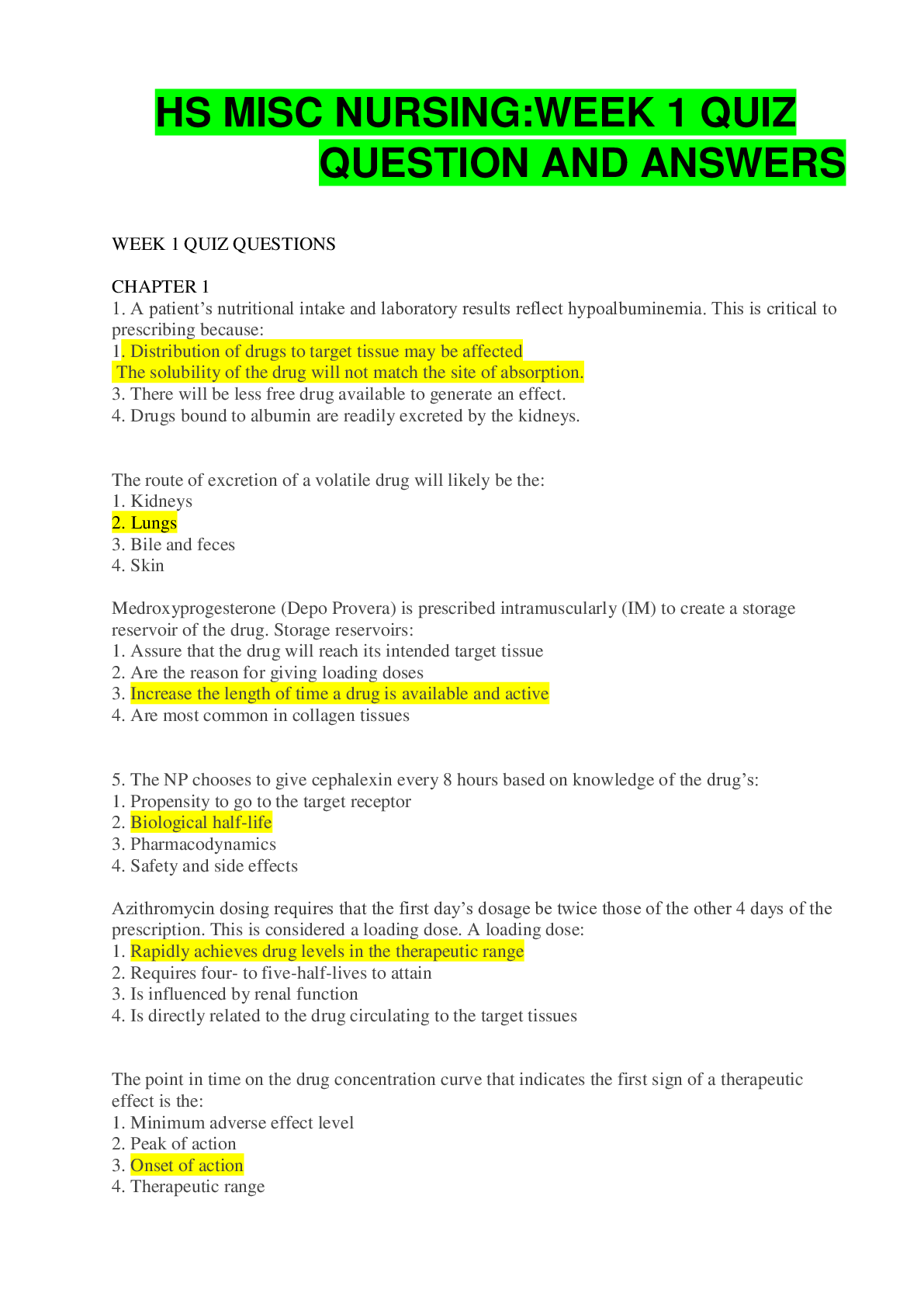
NSG 6020 WEEK 1 QUIZ BUILDING A COMPREHENSIVE HEALTH HISTORY
Document Content and Description Below
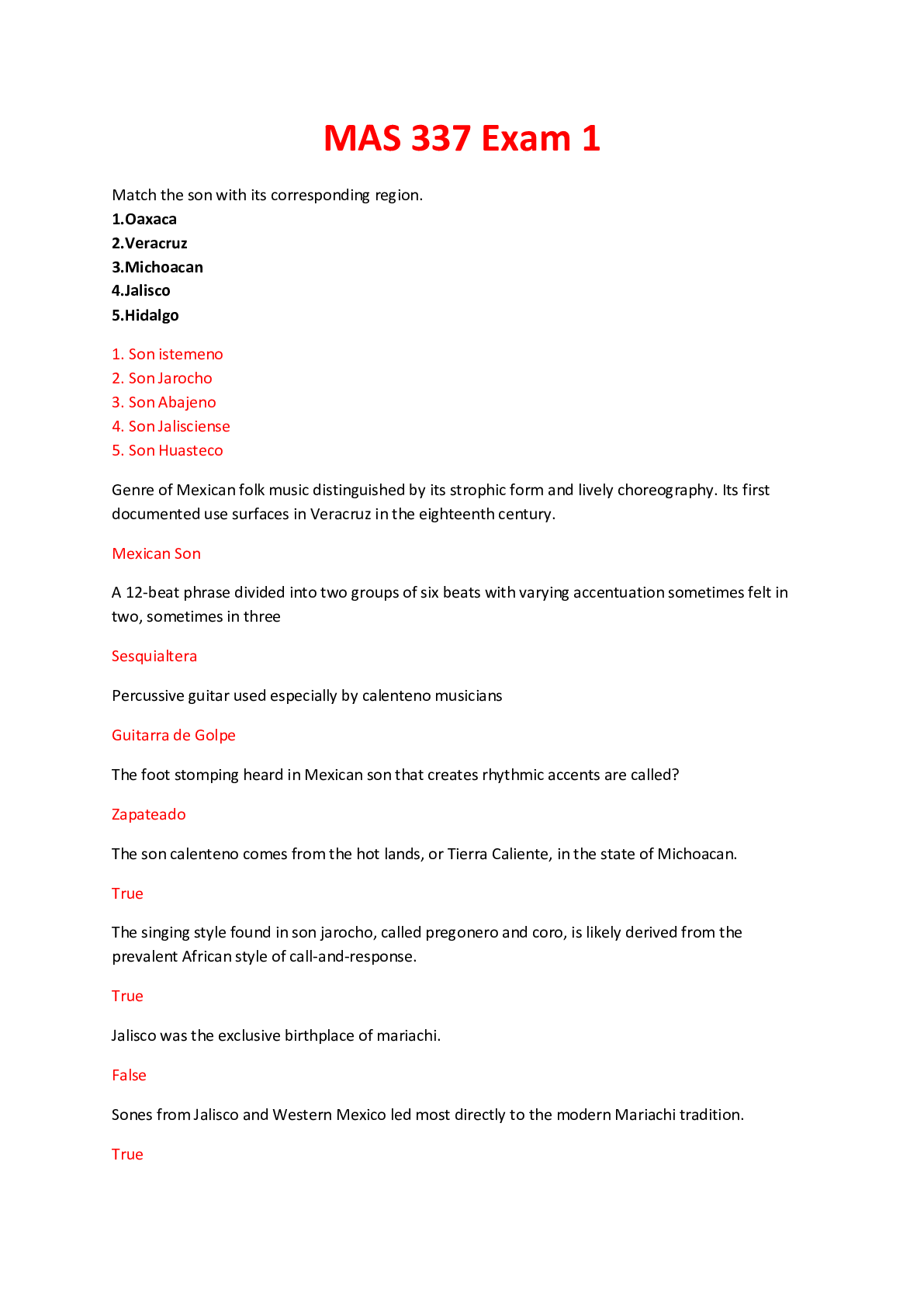
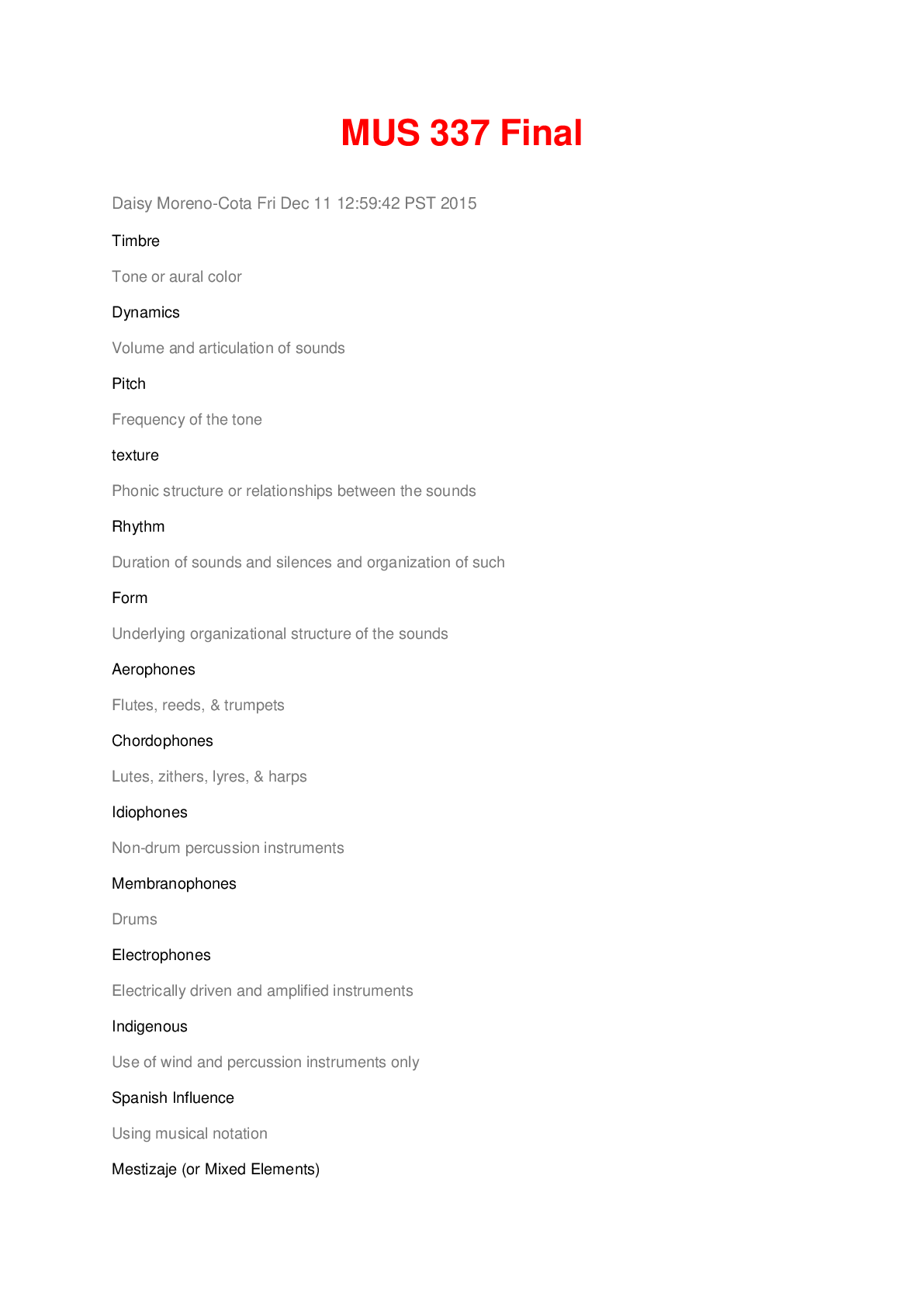
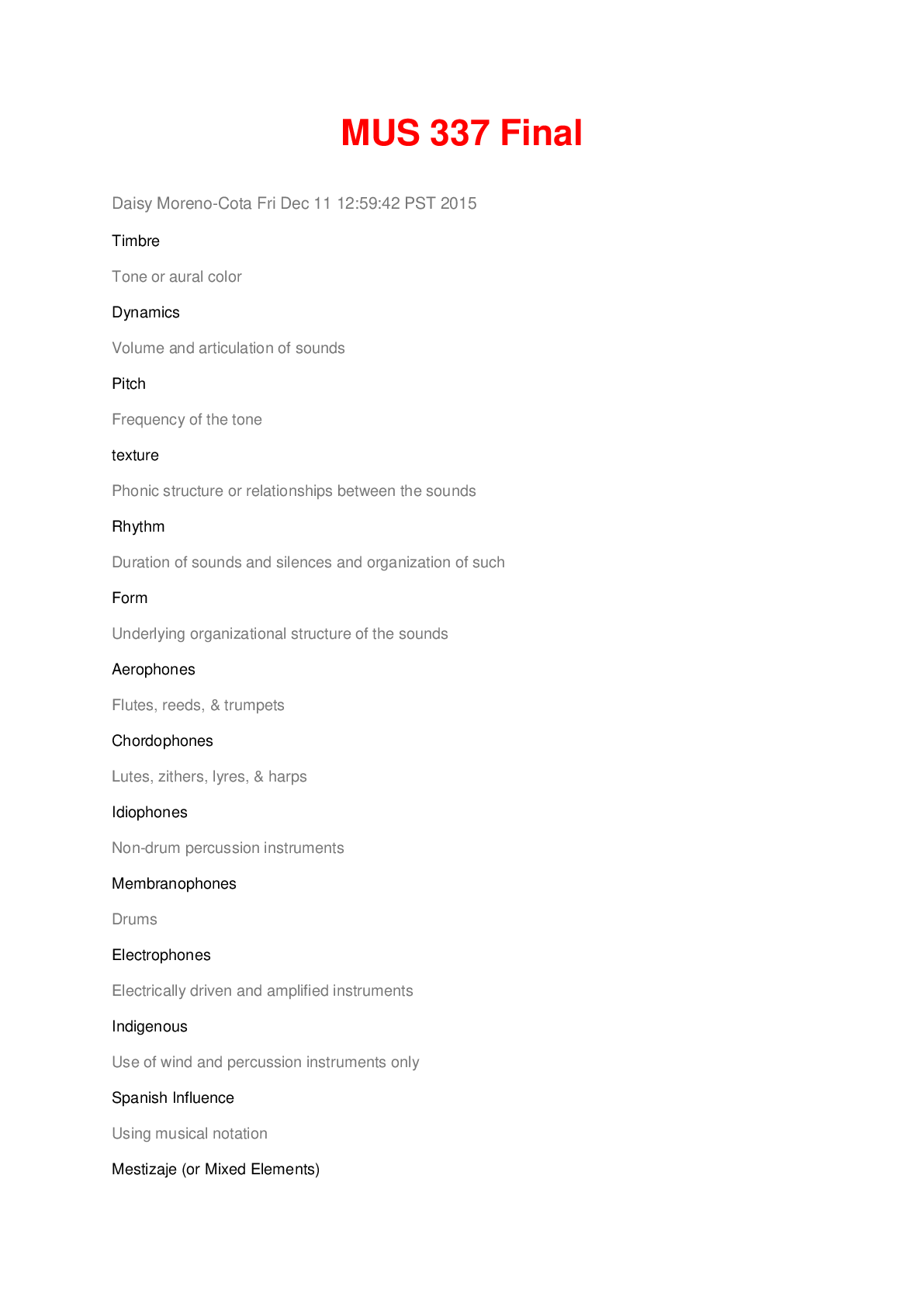
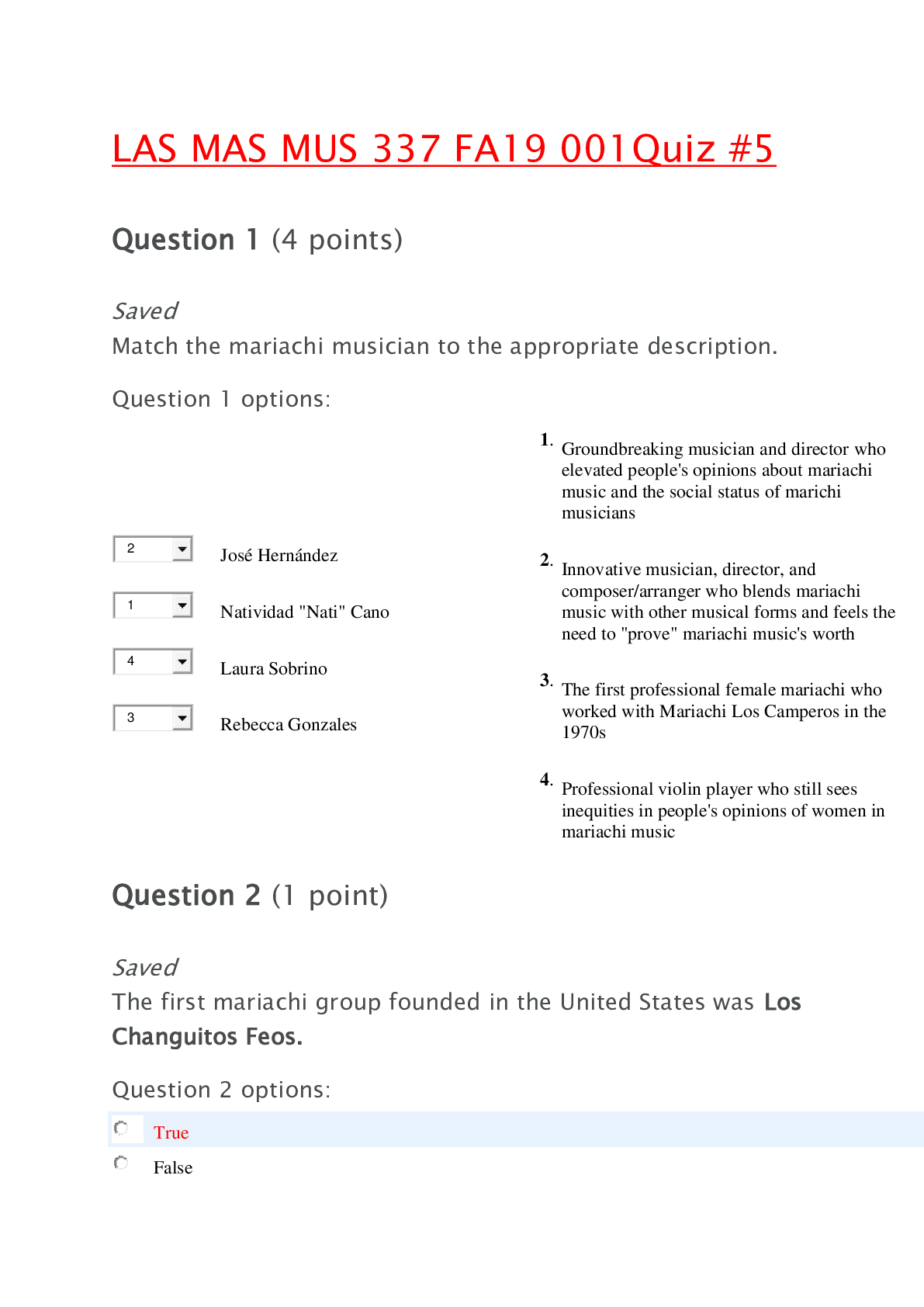
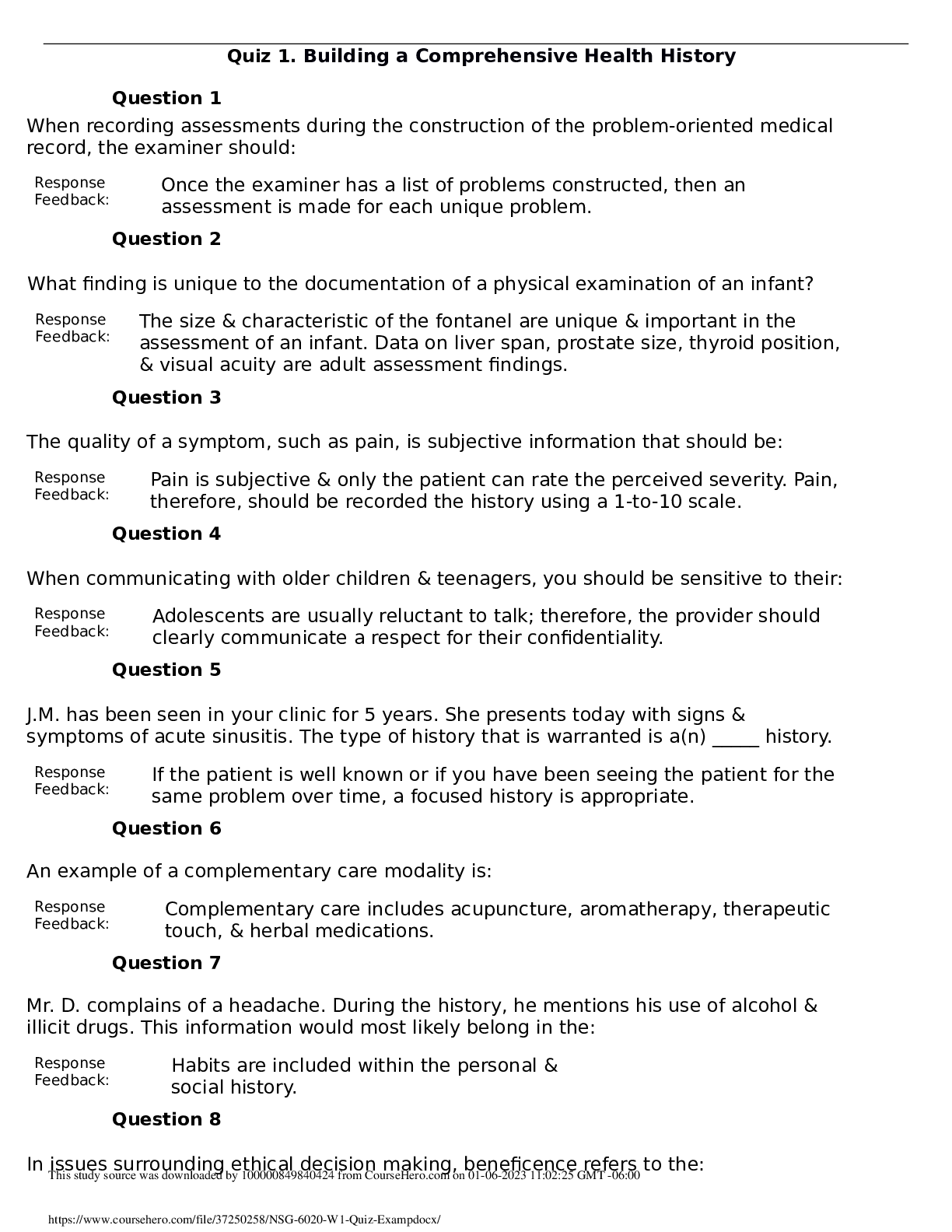
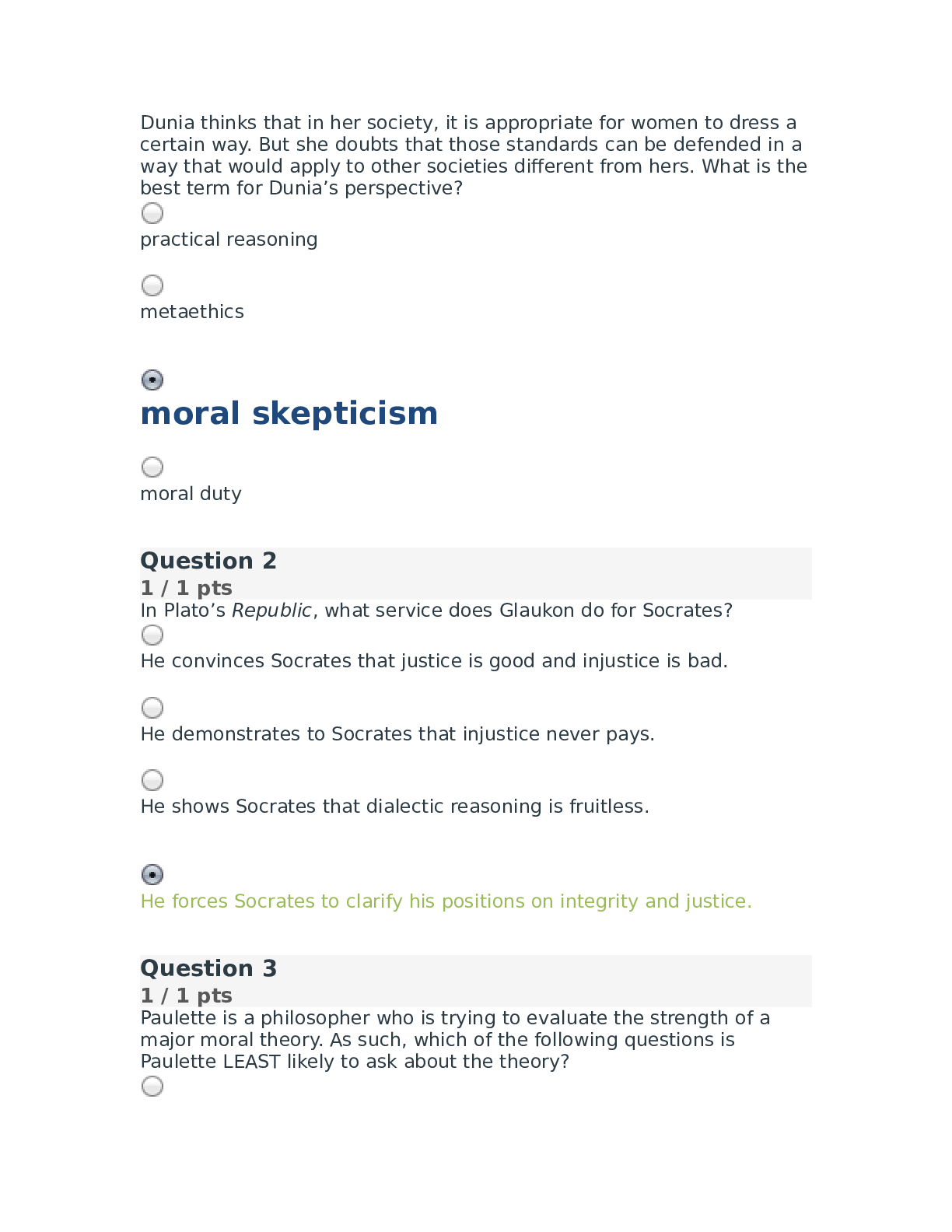
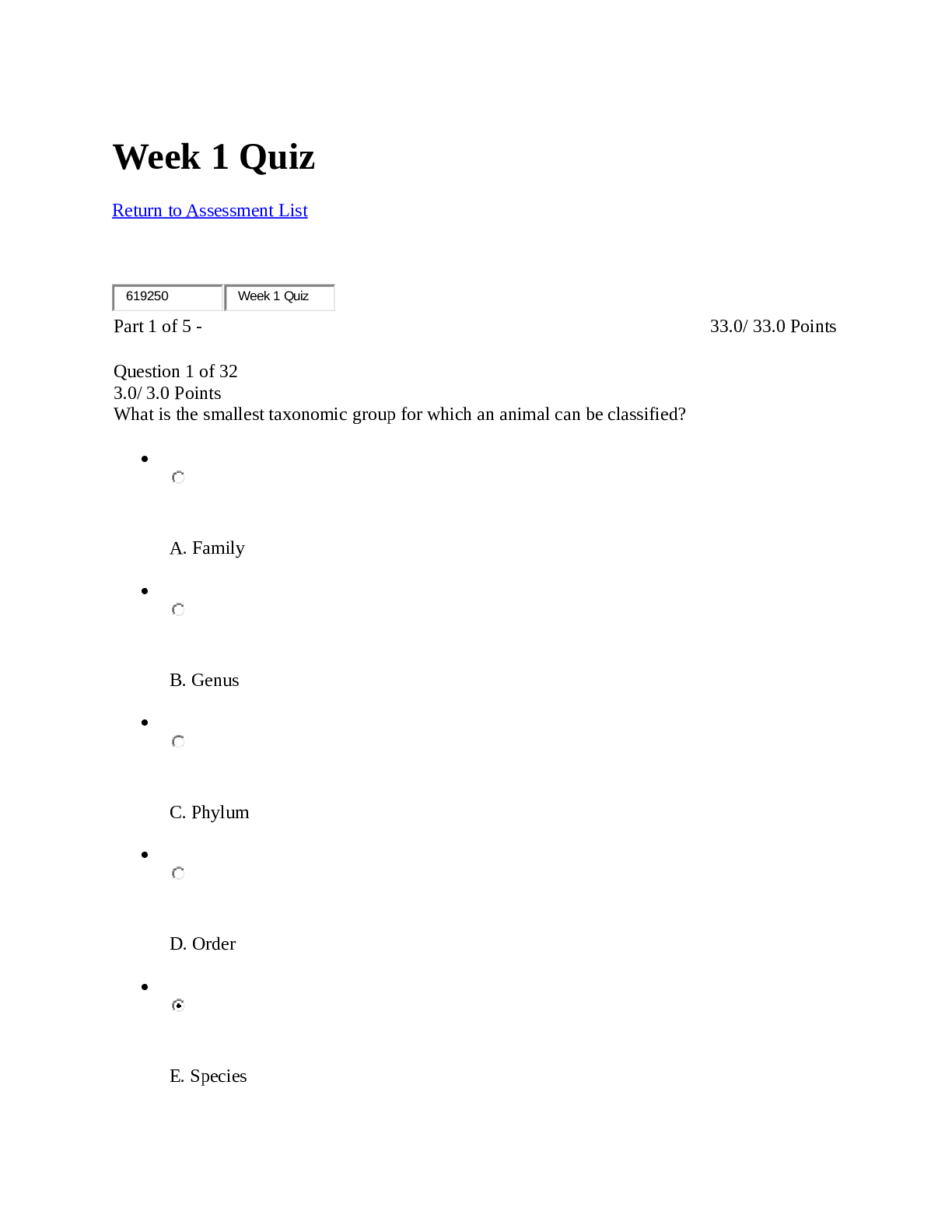
NSG 6020 WEEK 1 QUIZ – BUILDING A COMPREHENSIVE HEALTH HISTORY Physical Examination The History and Interviewing Process 1. In issues surrounding ethical decision making, beneficence ref... ers to: 1. the need to do good for the patient. 2. the care provider acting as a father or mother figure. 3. the care provider knowing what is best for the patient. 4. the need to avoid harming the patient. 2. The term denoting the caregiver’s need to do no harm to the patient is: 1. autonomy. 2. beneficence. 3. nonmaleficence. 4. utilitarianism. 3. The duties of care providers established by tradition, and within the context of culture, are known as: 1. beneficence. 2. deontologic imperatives. 3. paternalistic imperatives. 4. folk imperatives. 4. Which of the following is initially appropriate in the management of a patient’s diagnosed problem? 1. Inform the patient of the treatment plan. 2. Give the patient detailed written instructions regarding the treatment plan. 3. Inform the patient that the plan has been tailored to his needs. 4. Inform the patient of treatment options and possible results. 5. Which question would be considered a “leading question”? 1. “What do you think is causing your headaches?” 2. “You don’t get headaches often do you?” 3. “On a scale of 1 to 10, how would you rate the severity of your headaches?” 4. “At what time of the day are your headaches the most severe?” 6. To prevent personal appearance from becoming an obstacle in patient care, the health professional should: 1. wear a uniform. 2. avoid wearing white. 3. avoid extremes in dress. 4. avoid wearing any jewelry. 7. Which action would best promote accurate translations as well as confidentiality when the caregiver does not speak the patient’s language? 1. Ask a person unfamiliar with the patient to translate. 2. Have a friend of the patient translate. 3. Involve the family with the translation. 4. Use a neighbor as translator. 8. An example of a complementary care modality is: 1. physical therapy. 2. acupuncture. 3. psychotherapy. 4. chemotherapy. 9. When are open-ended questions generally most useful? 1. During the initial part of the interview 2. After several close-ended questions have been asked 3. While designing the genogram 4. During the review of systems 10. Behaviors that diffuse anxiety during the interview include: 1. avoiding wearing uniforms/laboratory coats. 2. providing forthright answers to questions. 3. providing all necessary information before the patient has to ask for it. 4. completing the interview as quickly as possible. 11. Periods of silence during the interview can serve important purposes, such as: 1. allowing the clinician to catch up on documentation. 2. promoting calmness. 3. providing time for reflection. 4. increasing the length of the visit. 12. Which technique is most likely to result in the patient’s understanding of questions? 1. Use phrases that are commonly used by other patients in the area. 2. Use the patient’s own terms if possible. 3. Use the simplest language possible. 4. Use proper medical and technical terminology. 13. Mr. F. is speaking with you, the health care provider, about his respiratory problem. Mr. F. says, “I’ve had this cough for 3 days, and it’s getting worse.” You reply, “Tell me more about your cough.” Mr. F. states, “I wish I could tell you more. That’s why I’m here. You tell me what’s wrong!” Which caregiver response would be most appropriate for enhancing communication? 1. “After 3 days, you’re tired of coughing. Have you had a fever?” 2. “I’d like to hear more about your experiences. Where were you born?” 3. “I don’t know what’s wrong. You could have almost any disease.” 4. “I’ll examine you and figure out later what the problem is.” 14. A patient becomes restless during the history and says, “I don’t have time for all of this conversation. I’ve got to get back to work.” Your most appropriate response would be to: 1. acknowledge his anger and proceed with the history and examination. 2. ask another open-ended question and insist on an answer. 3. ask questions about his anger and move closer to him. 4. ignore his displeasure and become more assertive about getting answers. 15. When questioning a patient regarding alcohol intake, she tells you that she is “only a social drinker.” Which initial response is appropriate? 1. “I’m glad that you are a responsible drinker.” 2. “Do the other people in your household consume alcohol?” 3. “What amount and what kind of alcohol do you drink in a week?” 4. “If you only drink socially, you won’t need to worry about always having a designated driver.” 16. Ms. T. is crying and states that her mother couldn’t possibly have a tumor. “No one else in the family,” exclaims the daughter, “has ever had cancer!” The most appropriate response to Ms. T. would be: 1. “Has anyone explained hospice care to your mother?” 2. “I’m so sorry that your mother was diagnosed with cancer.” 3. “That is odd, since cancer usually runs in families.” 4. “Why do you think that your mother’s tumor is cancerous?” 17. A 50-year-old man comes to the primary care clinic. He tells you he is worried because he has had severe chest pains for the past 2 weeks. Which initial history interview question is most appropriate? 1. “Can you describe the pain?” 2. “Are the pains worse after you eat?” 3. “Have you been treated for anxiety before?” 4. “Does your father have heart disease?” 18. After you ask a patient about her family history, she says, “Tell me about your family now.” Which response is generally most appropriate? 1. Ignore the patient’s comment and continue with the interview. 2. Give a brief, undetailed answer. 3. Ask the patient why she needs to know. 4. Tell the patient that you don’t discuss your family with patients. 19. A 36-year-old woman complains that she has had crushing chest pain for the past 2 days. She seems nervous as she speaks to you. An appropriate response is to: 1. continue to collect information regarding the chief complaint in an unhurried manner. 2. finish the interview as rapidly as possible. 3. ask the patient to take a deep breath and calm down. 4. ask the patient if she wants to wait until another day to talk to you. 20. Ms. A. states, “My life is just too painful. It isn’t worth it.” She appears depressed. Which one of the following statements is the most appropriate caregiver response? 1. “Try to think about the good things in life.” 2. “What in life is causing you such pain?” 3. “You can’t mean what you’re saying.” 4. “If you think about it, nothing is worth getting this upset about.” 21. During an interview, tears appear in the patient’s eyes and his voice becomes shaky. Initially, you should: 1. ask him if he would like some time alone. 2. offer a tissue and let him know it is all right to cry. 3. explain to the patient that you will be able to help him more if he can control his emotions. 4. ask the patient what he is upset about. 22. During an interview, you have the impression that a patient may be considering suicide. Which action is essential? 1. Ask whether the patient has considered self-harm. 2. Avoid directly confronting the patient regarding your impression. 3. Ask whether the patient would like to visit a psychiatrist. 4. Record the impression in the patient’s chart and refer the patient for hospitalization. 23. During a history-taking session, Mr. B. appears to be avoiding certain questions. He keeps looking out the window. What should the caregiver do? 1. Ask direct questions and insist on a “Yes” or “No” answer to each question. 2. Continue to ask questions until Mr. B. responds appropriately. 3. Make a note to pursue sensitive issues later in the interview. 4. Stop the interview until the patient is ready to cooperate. 24. You are collecting a history from an 11-year-old girl. Her mother is sitting next to her in the examination room. When collecting history from older children or adolescents, they should be: 1. given the opportunity to be interviewed without the parent at some point during the interview. 2. mailed a questionnaire in advance to avoid the need for her to talk. 3. ignored while you address all questions to the parent. 4. allowed to direct the flow of the interview. 25. Information that is needed during the initial interview of a pregnant woman includes all of the following except: 1. the gender that the woman hopes the baby will be. 2. past medical history. 3. health care practices. 4. the woman’s knowledge about pregnancy. 26. When communicating with older children and teenagers, you should be sensitive to their: 1. desire for adult companionship. 2. natural urge to communicate. 3. need for verbal instructions. 4. typical reluctance to talk. 27. When interviewing older adults, the examiner should: 1. speak extremely loudly, because most older adults have significant hearing impairment. 2. provide a written questionnaire in place of an interview. 3. position himself face-to-face with the patient. 4. dim the lights to decrease anxiety. 28. When you suspect that your 81-year-old patient has short-term memory loss because he cannot remember what he had for breakfast, you should: 1. order a neurology consult. 2. stop all of his medications. 3. validate the concern with his family or caregivers. 4. dismiss the finding as normal age-related change. 29. To what extent should the patient with a physical disability or emotional disorder be involved in providing health history information to the health professional? 1. The patient should be present during information collection but should not be addressed directly. 2. All information should be collected from past records and family members while the patient is in another room. 3. The patient should be involved only when you sense that he or she may feel ignored. 4. The patient should be fully involved to the limit of his or her ability. 30. A brief statement of the reason the patient is seeking health care is called the: 1. medical history. 2. chief complaint. 3. assessment. 4. diagnosis. 31. The iatropic stimulus refers to the: 1. patient’s stimulus to seek care. 2. mode of transportation used to get to the health center. 3. person who accompanied the patient to the health center. 4. most recent health care encounter. 32. When taking a history, you should: 1. ask patients to give you any information they can recall about their health. 2. start the interview with the patient’s family history. 3. use a chronologic and sequential framework. 4. use a holistic and eclectic structure. 33. When questioning the patient regarding his or her sexual history, which question should be asked initially? 1. “Do you have any particular sexual likes or dislikes?” 2. “Do you have any worries or concerns regarding your sexual life?” 3. “How often do you have intercourse and with whom?” 4. “Do you have any reason to think you may have been exposed to a sexually transmitted infection?” 34. A guideline for history taking is for caregivers to: 1. ask direct questions before open-ended questions so that data move from simple to complex. 2. ask for a complete history at once so that data are not forgotten between meetings. 3. make notes sparingly so that patients can be observed during the history taking. 4. write detailed information as stated by patients so that their priorities are reflected. 35. Mr. D. complains of a headache. During the history, he mentions his use of alcohol and illicit drugs. This information would most likely belong in the: 1. chief complaint. 2. past medical history. 3. personal and social history. 4. review of systems. 36. Direct questioning about domestic violence in the home should be: 1. a routine component of history taking with female patients. 2. avoided for fear of offending the woman’s partner. 3. conducted only in cases in which there is a history of abuse. 4. used only when the patient is obviously being victimized. 37. Mrs. G. reports an increase in her alcohol intake over the past 5 years. To screen her for problem drinking, you would use the: 1. CAGE questionnaire. 2. PACE assessment. 3. MILLER analogies. 4. GLASGOW scale. 38. A tool used to screen adolescents for alcoholism is the: 1. CAGE. 2. CRAFFT. 3. PACE. 4. HITS. 39. When you enter the examination room of a 3-year-old girl, you find her sitting on her father’s lap. She turns away from you when you greet her. Initially, your best response is to: 1. leave the child sitting in the father’s lap while you talk to the father. 2. ask the child to be seated on the examination table so that you can talk to her father. 3. explain to the child that you will not hurt her and that she will have to trust you. 4. ask the father to persuade the child to cooperate with you. 40. Tom is a 16-year-old diabetic who does not follow his diet. He enjoys his dirt bike and seems unconcerned about any consequences of his activities. Which factor is typical of adolescence and pertinent to Tom’s health? 1. Attachment to parents 2. High self-esteem 3. Low peer support needs 4. Propensity for risk taking 41. In the review of systems, the data obtained: 1. is organized according to the chief complaint. 2. is primarily objective data. 3. is ordered in a chronologic fashion. 4. follows a head-to-toe sequence. 42. Pain is difficult to assess in older adults because: 1. drugs act more rapidly with age. 2. their language skills decline. 3. they tend to exaggerate symptoms. 4. sharp pain may be felt as a dull ache. 43. A survey of mobility and activities of daily living (ADLs) is part of a/an: 1. ethnic assessment. 2. functional assessment. 3. genetic examination. 4. social history. 44. Constitutional symptoms in the ROS refer to: 1. height, weight, and body mass index. 2. fever, chills, fatigue, malaise. 3. hearing loss, tinnitus, and diplopia. 4. rashes, skin turgor, and temperature. 45. J.M. has been seen in your clinic for 5 years. She presents today with signs and symptoms of acute sinusitis. The type of history that is warranted is a(n) _____ history. 1. complete 2. inventory 3. problem or focused 4. interim 46. Mary Jane has brought in her 16-year-old son, Kyle. She states that he has been sleeping more, doesn’t hang around his friends, and recently his girlfriend broke up with him. Your most immediate question is to ask Kyle: 1. “Do you want to see a counselor today?” 2. “Is your father out of jail yet?” 3. “Are you taking any illegal drugs?” 4. “Have you made plans to harm yourself?” 47. Which of the following is considered an IADL but not an ADL? 1. Paying bills 2. Toileting 3. Walking around the house 4. Dressing oneself 48. Statistically, the patient at highest risk for suicide is the: 1. married woman. 2. single father. 3. older woman in a nursing home. 4. older man living alone. 49. The mnemonic used to characterize symptoms comprehensively is: 1. CAGE. 2. PQRST. 3. HITS. 4. TACE. 50. A pedigree diagram is drafted for the purpose of obtaining: 1. sexual orientation and history. 2. growth and developmental status. 3. genetic and familial health problems. 4. ethnic and cultural backgrounds. [Show More]
Last updated: 4 months ago
Preview 1 out of 14 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 18, 2020
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Feb 18, 2020
Downloads
5
Views
170

.png)

.png)