*NURSING > STUDY GUIDE > Rasmussen College: NUR 2063 Final Exam Study Guide_ LATEST UPDATED,100% CORRECT (All)
Rasmussen College: NUR 2063 Final Exam Study Guide_ LATEST UPDATED,100% CORRECT
Document Content and Description Below
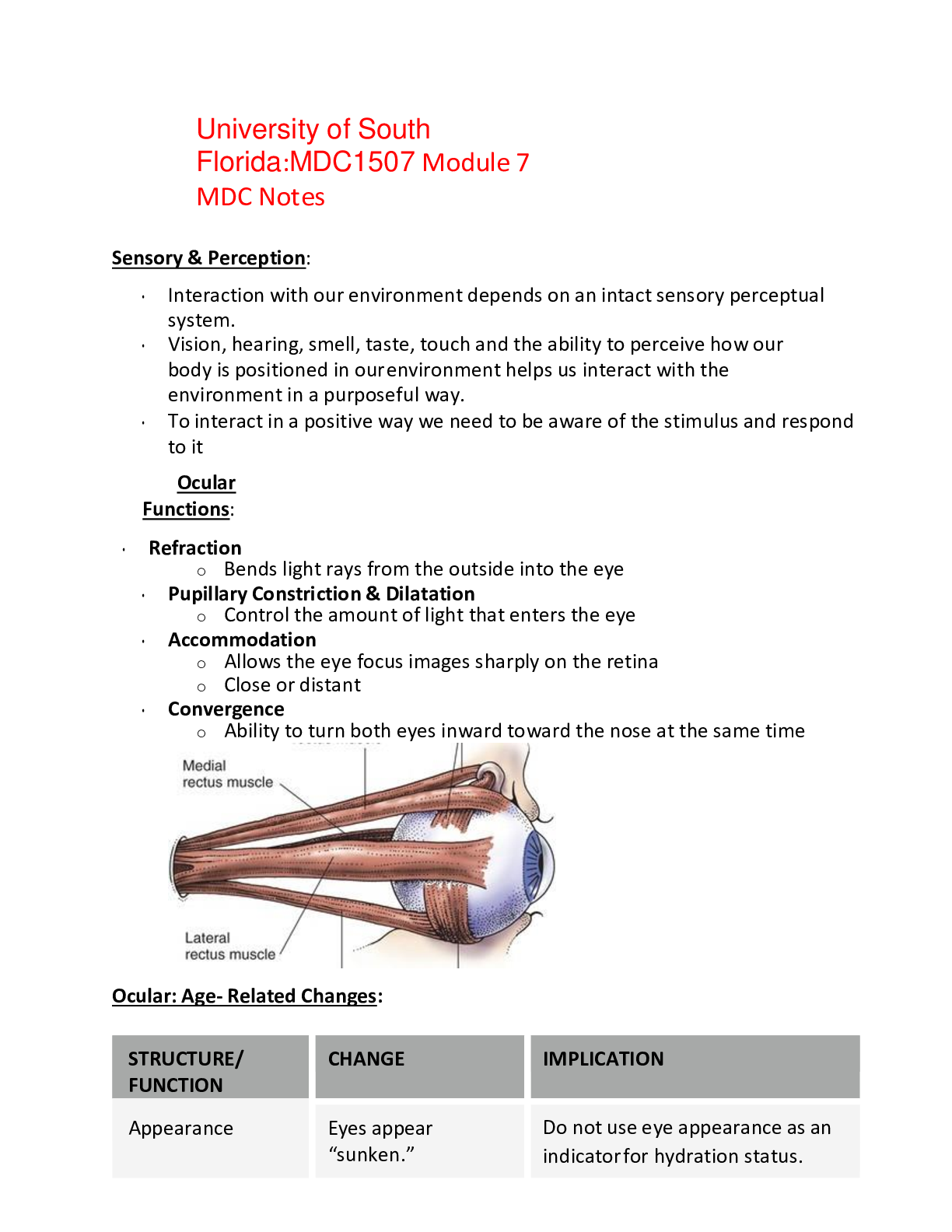
Rasmussen College: NUR 2063 Final Exam Study Guide_ LATEST UPDATED Module 1: STRESS – WHAT IS IT?, PURPOSE OF, WHAT DETERMINES RESPONSE? WHAT IS IT? – physical, chemical or emotional factor tha... t results in tension of body or mind, real or perceived threat to homeostasis, can be positive or negative PURPOSE – WHAT DETERMINES RESPONSE – SELYE GAP SYNDROME STAGES, BODY’S RESPONSES TO STAGES – ALARM, RESISTANCE, EXHAUSTION: ALARM – the stressor upsets homeostasis or cellular balance; releases epi and norepi, and cortisol; Body has decreased resistance to stressors RESISTANCE – Body fights back by adjusting to the stress; body trying to return to homeostasis; Glucose, free fatty acids and amino acids elevated for energy, growth and repair EXHAUSTION – Rest permits enhanced adaptation; No rest = overtraining, injury, lack of adaptation; point where body can no longer reach homeostasis; Allostatic overload – “cost” of body’s organs and tissues for an excessive or ineffectively regulated allostatic response STRESS IN CHILDREN: PHYSIOLOGICAL – Immune system, stunt in growth, high blood pressure MEDIATORS OF STRESS, E.G. NOREPINEPHRINE, EPINEPHRINE, CORTISOL – WHAT DO THEY DO? Norepinephrine (Catecholamines) – released during alarm stage; constricts blood vessels and raises blood pressure; reduces gastric secretions and increases night and far vision Epinephrine (Catecholamines) – released during the alarm stage; enhances myocardial contractibility, increases heart rate, and increases cardiac output; causes bronchodilation; increases the release of glucose from the liver(glycogenolysis) and elevates blood glucose levels Cortisol (Glucocorticoid) – released during alarm stage; primary glucocorticoid; may be synergistic or antagonistic to catecholamines; suppresses the immune system, decreases serotonin, increases blood sugar, increases blood pressure, decreases sensitivity to pain, and heightens memory and attention ALDOSTERONE (mineralocorticoid)– essential for sodium conservation in the kidneys, salivary glands, sweat glands, and colon LONG TERM GLUCOCORTICOID EFFECTS ON BODY: osteoporosis, inability to fight infection (comp host), can weaken muscle/atrophy of skeletal muscle ENDORPHINS AND ENKEPHALINS: ENDORPHINS- are an endogenous opioid peptide derived from cells in the hypothalamus, have analgesic properties ENKEPHALINS – One of two types of pain-suppressing pentapeptides; they are produced in the body and are located in the pituitary gland, brain, and GI tract Module 2 PHAGOCYTOSIS: WHAT IS IT? – When leukocytes attack the bad cells and “eat” them STEPS IN CARCINOGENESIS, INITIATION, PROMOTION, PROGRESSION: INITIATION – Initiating events in chromosomes (such as aberrations) or in DNA; initiators are radiation, chemical carcinogens, UV etc. PROMOTION – low doses of tumor initiators are necessary to convert the initiated cells to cancer cells; EX: TPA, phorbol esters, estrogen and excessive fat PROGRESSION – Increased genetic instability resulting in aggressive growth phenotype GENERAL CHARACTERISTICS OF BENIGN VS MALIGNANT TUMORS: BENIGN – Does not immediately kill host, does not invade or spread to distant sites, causes less damage to host tissue, many are encapsulated, closely resembles original tissue, grows more slowly, little vascularity MALIGNANT – can kill host if left untreated, invades local tissue and overruns neighboring cells, can migrate to distant areas (metastasis), does not closely resemble tissue of origin (anaplasia), greater degree of anaplasia indicates aggressive malignancy, grows rapidly, may initiate tumor vessel growth, frequently necrotic, dysfunctional WHAT ARE SIGNS OF INFLAMMATION? Redness, swelling(edema), heat, pain, and loss of function CAUSES OF INFLAMMATION? Infection, build-up of pressure, and injury WHAT CAUSES EDEMA? Staying in one position too long, crushing injury, and fluid that is trapped in the body. WHAT DO TREATMENTS DO TO REDUCE INFLAMMATION, E.G. GLUCOCORTICOIDS, ICE: Ice soothes inflammation by reducing blood in the area and stops spasms causing pain, while glucocorticoids reduce the activity of the immune system and cause the inflammatory cells to not come to the site of inflammation. ACTIVE VS. PASSIVE IMMUNITY: Active: results from the production of antibodies in response to the presence of an antigen. EX. Allergic reaction Passive: Introduction of antibodies from another person or animal. EX. The placenta LYMPH NODE LOCATIONS: Axillary regions, inguinal/groin, and neck. IMMUNOGLOBULIN: WHAT IS IT? - Module 3 MYASTHENIA CRISIS: weakening muscle functioning results in respiratory failure KELOID – Overgrowth of scar tissue HERPES ZOSTER (SHINGLES) – Acute inflammatory disease of a dermatomal segment of the skin; believed to be reactivated by latent varicella zoster virus from previous chicken pox; Unilateral, painful, can result in postherpetic neuralgia Vesicles on erythematous base of single or associated group of dorsal root ganglia; ATOPIC DERMATITIS – complex genetic disease resulting from gene-gene and gene- environment interaction; highest incidence in children most of which are less than 5yrs old; pruritis always present; usually on face, scalp or exterior surfaces of extremities; SIGNS – erythema, papules, lichenification (skin condition that is caused by excessive itching or rubbing which results in thick leathery patches of skin) COMPARTMENT SYNDROME – complication of soft tissue injury; results from swelling and bleeding within a restricted area; can be either acute, chronic or crush; pale and shiny due to lack of blood flow; swelling crushes nerves which causes excruciating pain; Treatment is emergent decompression which is where they cut through tissue to relieve pressure 5 P’s – pain out of proportion, paralysis, paresthesia, pallor, and pulselessness RHEUMATOID ARTHRITIS – systemic, autoimmune, inflammatory; women are 2-3x more likely than men with the peak age being 40-50; it affects the hands, wrists, knees and feet more; if it is in the spine it usually affects the upper cervical area; symptoms are malaise, fatigue, diffuse musculoskeletal pain; bilaterally symmetric HEALING PROCESS – 3 phases – THE FASTEST HEALING OCCURS WHEN EDGES ARE WELL APPROXIMATED INFLAMMATORY PHASE – begins at time of injury and can last up to 4 days; clotting of platelets, constriction of blood vessels, WBCs kills bacteria PROLIFERATION OR GRANULATION PHASE – begins about day 3 and overlaps inflammatory phase; fibroblasts help reduce new collagen, create new blood vessels, and repair epithelial tissue Granulation tissue – highly vascular, very fragile and very susceptible to infection REMODELING PHASE- can continue for 6 months to a year; collagen continues to increase; tissue begins to contract with the help of fibroblasts; adds to the strength of new tissue; scar made up of collagen fibers Module 4: GI PEPTIC ULCER DISEASE: WHAT IS IT? – Disorder of the upper GI tract by action of hydrochloric acid and pesin CAUSES? – H. Pylori (75% of cases with duodenal ulcers and 60% of those with stomach/gastric ulcers), NSAIDS, excess secretion of acid, stress WHERE IS IT FOUND? – stomach, and duodenum (usually proximal duodenum) MECHANISM – Uncertain HEPATOCELLULAR CARCINOMA: WHAT IS IT? – Most common form of liver cancer; usually occurs in patients with underlying chronic liver disease and cirrhosis SIGNS/SYMPTOMS – Weight loss, upper abdominal pain, jaundice, anorexia TREATMENT- surgery, transplant, freezing or heating the cancer cells, and chemotherapy GASTRITIS: WHAT IS IT? – Inflammation of the stomach lining CAUSES? – Acute is caused by ingestion of toxins like alcohol, aspirin, or other irritating substances • Can also be caused by viral, bacterial, or autoimmune disease SIGNS/SYMPTOMS – Anorexia, nausea, vomiting, and postprandial discomfort • Occasional hematemesis due to mucosal damage HEPATITIS: WHAT IS IT? – Inflammation of the liver 3 MAJOR TYPES: • Hep A – spread by fecal oral route; most adults develop jaundice o SIGNS/SYMPTOMS: malaise, anorexia, nausea, low grade fever, and right upper quadrant pain • Hep B – Spread by parental contact with infected body fluids o SIGNS/SYMPTOMS – can have no symptoms to moderate illness to fulminant hepatitis; major risk factor for hepatocellular cancer • Hep C – spread through blood and blood product; major risk factor for hepatocellular cancer Module 5 GU STI AMENORRHEA: WHAT IS IT? – Absence or suppression of menstruation in females age 16 or older; if female misses or more periods in a row PRIMARY – failure to begin menses by age 16 SECONDARY – cessation of established, regular menstruation for 6 months or longer CAUSES - Usually due to abnormal pattern of hormonal functioning which causes interruption of normal sequence of events of endometrial tissue lining the uterus proliferating and sloughing PROSTATE CANCER SCREENING: BLADDER CANCER RISK FACTORS: CYSTITIS: WHAT IS IT? - inflammation of the bladder lining CAUSES- infection, chemical irritants, stones, and or trauma • Most commonly caused by infection; E-COLI is the most common pathogenic cause and it usually originates in the urethra RISK FACTORS? – being a female, old age, catheterization, diabetes, bladder dysfunction, poor hygiene, and urinary stasis • Children who have a congenital defect called vesicoureteral reflux often have a high risk of cystitis BPH (BENIGN PROSTATIC HYPERTROPHY): WHAT IS IT? – Enlargement of the prostate SIGNS/SYMPTOMS – Hesitancy (difficulty initiating a stream), decreased stream or dribbling, urinary retention, obstruction to flow, interruption of the stream, infection caused by retention HORMONES INVOLVED WITH URINATION: HSV: WHAT IS IT?: Herpes Simplex Virus; causes contagious sores that are often found around the mouth and or genitalia. There is no cure, but it can be treated and prevented by medications. TYPE 1: Oral herpes (cold sores) TYPE 2: Genital warts (sexually transmitted) PYELONEPHRITIS: WHAT IS IT? - inflammation of the kidneys caused by infection; usually caused by E. Coli CAUSES- due to ascending urinary tract infection RISK FACTORS- pregnancy, diabetes mellitus, anatomical abnormalities, and obstructions SIGNS/SYMPTOMS – CVA tenderness, fever, chills, n/v, anorexia, fever induced dehydration TREATMENT- usually 7-10 days of antibiotics Module 6 Diabetes/Endocrine PRIMARY ENDOCRINE DISEASE: WHAT IS IT?: A disease that originates within the gland in question EXAMPLE: Primary hyperthyroidism is a defect in the thyroid. SECONDARY ENDOCRINE DESEASE: WHAT IS IT?: Represents change in one organ as a result of disease in another organ EXAMPLE: Secondary hyperthyroidism may be due to a TSH secreting pituitary adenoma. DIABETES TYPE 1: WHAT IS IT?: A chronic adolescence condition in which the pancreas produces too little or no insulin. SYMPTOMS: Increased thirst, frequent urination, hunger, fatigue, and blurred vision. TREATMENT: Uncurable, but can be treated by monitoring blood sugar levels, insulin therapy, diet, and exercise. DIABETES TYPE 2: WHAT IS IT?: Adult-onset chronic condition that affects the way the body processes sugar; the body does not produce enough insulin or it resists it. SYMPTOMS: Sometimes none occur, increased thirst and urination, hunger, fatigue, and blurred vision. TREATMENT: Diet, exercise, medication, and insulin therapy. MYXEDEMA: WHAT IS IT?: Severe form of hypothyroidism that can occur when left untreated or is not treated sufficiently. SYMPTOMS: Dry and pale skin, swelling of the face, tongue, and legs. TREATMENT: Synthetic hormones, antibiotics, steroids, and oxygen support. GRAVE’S DISEASE (HYPERTHYROIDISM): WHAT IS TI?: AKA: Basedow’s disease; the immune system attacks the thyroid and causes it to produce more thyroid hormone than the body needs. SYMPTOMS: Anxiety, hand tremor, heat sensitivity, weight loss, puffy eyes, and enlarged thyroid. TREATMENT: Medications and sometimes removal of the thyroid SIGNS OF DIABETES: Polydipsia, polyphagia, and polyuria Module 7: Neuro Topics: GLASGOW COMA SCALE: WHAT IS IT? – Standardized tool for assessing LOC in acutely brain injured person Numeric scores given to arousal-directed responses of eye opening, verbal utterances, and motor reactions (less than 8 = coma) INCREASED INTRACRANIAL PRESSURE (ICP): Results in impaired neurological function which causes- 1. Compression of brain 2. Inflammation of brain tissues 3. Inability of cranium to expand in adults 4. Reduced blood flow to the brain due to pressure SIGNS/ SYMPTOMS: Headache, N/V, Confusion MENINGITIS: WHAT IS IT? – Infection of the meningeal tissues; can be bacterial or viral; tissues swell increasing ICP, blood flow to brain is decreased BACTERIAL- Most common cause is streptococcus pneumoniae; usually reaches the CNS via the bloodstream or extension from cranial structures like sinuses or ears TRANSMISSION – Droplets of respiratory or throat secretions, smoking, close or prolonged contact such as kissing, sneezing or coughing on someone SYMPTOMS- Headaches, AMS, phonophobia, fatigue, severe muscle pain, dislike bright lights, high fever, seizures, stiff neck, sleepiness or trouble waking, N/V, paleness, spots or rash DIAGNOSIS- Lumbar Puncture (LP) TREATMENT – IV antibiotics PREVENTION – Vaccinations for HIB and Meningitis HEAD INJURY TYPES: HYPOXIA IMPACT ON BRAIN CELLS: O2 too low so not enough ATP produced HEMORRHAGIC STROKE: WHAT IS IT? – Hemorrhage within or around the brain; usually occurs secondary to severe, chronic hypertension; degree of secondary injury and associated morbidity and mortality much higher than in ischemic stroke WHERE DOES IT MOST OFTEN OCCUR? – in the basal ganglia or thalamus TREATMENT? – Cardiovascular stabilization, brain CT to determine type and location, ICP monitoring and management, Blood pressure management (keep mildly hypertensive at first ISCHEMIC STROKE: WHAT IS IT? – Stroke that results from sudden occlusion of cerebral artery secondary to thrombus formation or emboli THROMBOTIC STROKE – associated with atherosclerosis and coagulopathies EMBOLIC STROKE – associated with cardiac dysfunction or dysrhythmias (A-FIB) CLINICAL MANIFESTATIONS – Contralateral hemiplegia, hemisensory loss, and contralateral visual field blindness TREATMENT- Salvaging the penumbra is the aim of early thrombotic therapy; however, treatment must be started within 3 hours of symptom onset to be maximally effective, thrombolytics, anticoagulant, antiplatelet, stents ALZHEIMER DISEASE: WHAT IS IT? – Characterized by amyloid plaques and neurofibrillary tangles, degeneration of neurons in temporal and frontal lobes, brain atrophy; deficient synthesis of acetylcholine CAUSE- remains unknown, although genetic factors and environmental triggers suspected RISK FACTOR – family history, and age REPERFUSION INJURY: SEIZURE DISORDER: refers to recurrent seizures (epilepsy), classified by clinical symptoms and EEG WHAT IS IT? – Transient neurologic event of paroxysmal abnormal or excessive cortical electrical discharges CLINICAL MANIFESTATIONS – Disturbances of skeletal motor function, sensation, autonomic visceral function, behavior, or consciousness CAUSES – Cerebral injury, lesions, metabolic/nutritional disorders, idiopathic (no known cause) DIAGNOSIS – EEG, Laboratory studies (to identify metabolic/nutritional deficits, infections, and exposure to toxins), LP (for CNS infections), CT and MRI (for structural causes) TREATMENT – DURING (maintain airway, protect from injury, document course of seizure), anticonvulsant medications (continue until no seizures for at least 2 years and then gradually withdraw), avoid triggers, surgery (removal or seizure foci or neurostimulation) GENERALIZED/ GRAND MAL: WHAT IS IT? – seizure involving whole brain surface; involvement of the thalamus and tonic- clonic (grand mal) jerking of many muscles PARTIAL SEIZURES: ABSENCE (petite mal): occurs in children, staring spells that last only seconds ATYPICAL ABSENCE – myoclonic jerks, automatisms with the staring spell MYOCLONIC – Single/several jerks ATONIC – drop attack; fall down STATUS EPILEPTICUS: WHAT IS IT? – Continuing series of seizures without a period of recovery between episodes; can be life-threatening (brain damage may occur if not halted) CRANIAL NERVES BY NUMBER AND WHAT THEY DO: CEREBRAL PLASY: WHAT IS IT? – Diverse group of crippling syndromes that appear during childhood and involve permanent, nonprogressive damage to motor control areas of the brain CAUSES – Prenatal infections or disease of the mother; mechanical trauma to the head before birth or after birth; exposure to nerve damaging poisons or reduced oxygen supply to the brain TREATMENT – varies depending on the nature and extent of brain damage; muscle relaxants, anticonvulsants, orthopedic therapy, casts, braces, and traction; botox for pain and range of motion ALS: AMYOTROPHIC LATERAL SCLEROSIS (Lou Gehrig’s Disease) WHAT IS IT? – Progressive neurodegenerative disease; it affects the nerve cells in the brain and spinal cord; 100% fatal EARLY SIGNS/SYMPTOMS – Muscle twitching, dropping things, slurred speech, muscle cramps, tripping, uncontrollable crying or laughing LATER SIGNS/SYMPTOMS – Progressive muscle weakness beginning typically in hands, feet or limbs spreading throughout; trouble chewing, swallowing, speaking and breathing, generally no pain TREATMENT – Riluzole can extend life 3 to 6 months or Edaravone reduces decline in daily functioning, unknown life extension CAUSE/MECHANISM – No direct cause identified MULTIPLE SCLEROSIS: WHAT IS IT? – Chronic demyelinating disease of the CNS that primarily affects young adults; autoimmune disorder that results in inflammation and scarring of myelin sheaths covering nerves and slowly progresses CAUSE- Unknown MOSTLY AFFECTS – the optic and oculomotor nerves and spinal nerve tracts CLINICAL MANIFESTATIONS – Double/blurred vision, weakness, poor coordination, and sensory deficits; bowel and bladder control may be lost; memory impairment common DIAGNOSIS – MRI Module 8: Respiratory ASTHMA: WHAT IS IT? – Airway inflammation; increased airway responsiveness to a variety of stimuli, two types – extrinsic and intrinsic EXTRINSIC – Allergic, pediatric onset; 1/3 to ½ of asthma cases; IgE is elevated Pharmacologic therapy, allergen specific immunotherapy, and environmental control INTRINSIC – Non-allergic, adult onset; develops in middle age with less favorable prognosis, no history of allergies, respiratory infections or psychological factors appear to be contributory CLINICAL MANIFESTATIONS – Wheezing, feeling of tightness of chest, dyspnea, cough (dry or productive), increased sputum production (thick, tenacious, scant, and viscid), hyperinflated chest, decreased breath sounds Severe attack manifestations – Use of accessory muscles when breathing, intercostal retractions, distant breath sounds with inspiratory wheezing, orthopnea, agitation, tachypnea >30 breaths/min, tachycardia >120 bpm, PERF <80 L/min DIAGNOSIS – Pulmonary function tests, skin testing (young patients with extrinsic asthma), CBC (Elevated WBCs and eosinophils) TREATMENT – Avoid triggers, environmental control (dust control, removal of allergens, air purifiers, air conditioners), preventative therapy (stop smoking, avoid second hand smoke, aerosols, odors, early treatment for respiratory infections), desensitization (allergen specific immunotherapy); MEDICATIONS- O2 therapy, small volume nebulizers, B2 agonists, corticosteroids, leukotriene modifiers, mast cell inhibitors SEVERE CASES – Epinephrine, SQ terbutaline, aminophylline, IV corticosteroids; and oxygen therapy with or without mechanical ventilation ACUTE BRONCHITIS: WHAT IS IT? - Inflammation of the trachea and bronchi CAUSES – Viral or non-viral, heat, smoke inhalation, inhalation of irritant chemicals, allergic reactions PATHOGENESIS – Airways become inflamed and narrowed from capillary dilation, swelling from fluid exudation, infiltration with inflammatory cells, increased mucus production, loss of portions of the ciliated epithelium CLINICAL MANIFESTATIONS – Usually mild and self-limiting, cough (productive or nonproductive), low-grade fever, substernal chest discomfort, sore throat, postnasal drip, fatigue DIAGNOSIS – Clinical presentation, recent onset of cough (hallmark or disease), chest x-ray to distinguish from pneumonia TREATMENT – usually no treatment for viral, antibiotics for bacterial, codeine containing medications for cough, increase fluid intake, avoid smoke, use vaporizer in bedroom CHRONIC BRONCHITIS: WHAT IS IT? – Chronic inflammation and swelling of the bronchial mucosa resulting in scarring CAUSES – Cigarette smoking (90%), repeated airway infections, genetic predisposition, inhalation of physical or chemical irritants CLINICAL MANIFESTATIONS – Patient is typically overweight, commonly associated with emphysema, SOB on exertion, excessive sputum, chronic cough (more severe in mornings), evidence of excess body fluids (edema, hypervolemia), cyanosis (late sign) DIAGNOSIS – Chest X-ray, Pulmonary function test, ABG (Arterial blood gases), ECG, secondary polycythemia (R/t continuous or nocturnal hypoxemia) TREATMENT – Goals (block progression of the disease, return to optimal respiratory function, return to ADLs), Medication (inhaled short acting B2 agonists, inhaled anticholinergic bronchodilators, cough suppressants, antimicrobial agents, inhaled/ oral corticosteroids, theophylline products) EMPHYSEMA: WHAT IS IT? – Abnormal enlargement of the distal air sacs, destructive changes of the alveolar walls without fibrosis; damage is irreversible and is associated with chronic bronchitis CAUSES – Smoking >70 packs/year, air pollution, certain occupations (mining, welding, working with asbestos), a1-antitrypsin deficiency PATHOGENESIS – Reduction in pulmonary capillary bed (exchange of O2 and CO2 between alveolar and capillary blood impaired), Loss of elastic tissue in lung, air becomes trapped in distal alveoli, loss of alveolar wall and air trapping leads to bullae formation CLINICAL MANIFESTATIONS – Progressive, exertional dyspnea, thin, use of accessory muscles, pursed-lip breathing, cough, digital clubbing, barrel chest DIAGNOSIS – Pulmonary function test, Chest x-ray, ECG, ABG, Patient history, common physical findings (Thin, wasted individual hunched forward, using accessory muscles, decreased breath sounds, prolonged expiration, decreased heart rate, hyperresonance, decreased diaphragmatic excursion, chronic morning cough TREATMENT – O2 therapy, smoking cessation, medications (inhaled short acting B2 agonists, inhaled anticholinergic bronchodilators, cough suppressants, antimicrobial agents, inhaled/ oral corticosteroids, theophylline products) PLEURAL EFFUSION: WHAT IS IT? - Fluid or pus in the pleural cavity CAUSES – Pneumonia, heart failure, cirrhosis of the liver, rheumatoid arthritis, lupus, mesothelioma, low protein level in the blood TREATMENT – Thoracentesis (drains fluid) PNEUMOTHORAX: WHAT IS IT? – Accumulation of air in the pleural space PRIMARY – Spontaneous, occurs in tall thin men 20 to 40 years; no underlying disease factors, cigarette smoking increases risk SECONDARY – Results or complications from preexisting pulmonary disease CLINICAL MANIFESTATIONS – Small pneumothoraxes’ (<20%) are usually not detectable on physical examination, tachycardia, decreased or absent breath sounds on affected side, hyperresonance, sudden chest pain on affected side, dyspnea DIAGNOSIS – ABG, ECG, Chest X-ray TREATMENT – Depends on severity; less than 15-25% lung collapse = treat symptomatically and monitor closely; greater than 15-25% = chest tube placement with H2O seal and suction to remove pleural air; Chemical pleurodesis (Promotes adhesion of visceral pleura to parietal pleura to prevent further ruptures); Thoracotomy (permits stapling or laser pleurodesis of ruptured blebs) COPDs – types: Asthma, Chronic bronchitis, Emphysema, Bronchiectasis, Cystic Fibrosis SARCOIDOSIS: WHAT IS IT? – Multisystem granulomatous disease CAUSE – Unknown CLINICAL MANIFESTATIONS – 30-50% without symptoms; malaise, dyspnea of insidious onset, dry cough PULMONARY FIBROSIS: WHAT IS IT? – Scarring of the lungs, no cure; average life expectancy 3-5 years Pons & medulla – respiratory center Stimulation of sympathetic nervous system – bronchodilation Module 9: Cardiac FAMILY OF HTN WHAT INDICATES NEED FOR MORE EDUCATION: Non-modifiable risk factors – family history, age, ethnicity, and gender Modifiable risk factors – Diet, weight, alcohol, smoking, sedentary lifestyle, metabolic syndrome, high blood sugar, elevated total cholesterol 2 ORGANS MOST AFFECTED BY UNCONTROLLED HYPERTENSION: Heart and eyes MODIFIABLE RISKS FOR ARTERIOSCLEROSIS AND ATHEROSCLEROSIS: smoking tobacco, obesity, hypertension WHAT IS MEAN ARTERIAL PRESSURES (MAP): The average pressure in an artery over 1 cardiac cycle ORTHOSTATIC HYPERTENSION: WHAT IS IT? – Drop in systolic pressure greater or equal to 20mm Hg or in diastolic pressure greater or equal to 10 mm Hg when moving into the upright position CAUSES – Dizziness, blurred vision, fainting, and fall injuries LEFT SIDED HEART FAILURE, PRIORITY ASSESSMENT: Lung sounds RIGHT SIDED HEART FAILURE: peripheral edema ANGINA PECTORIS UNSTABLE: NOT RELIEVED BY REST WHAT IS IT? – chest pain associated with intermittent myocardial ischemia CORONARY HEART DISEASE: WHAT IS IT? – Characterized by insufficient delivery of oxygenated blood to the myocardium ETIOLOGY – Atherosclerosis, possible microcirculation abnormalities HOW IS MI DIFFERENT FROM UNSTABLE ANGINA: WHY IS SHOCK LIFE THREATENING? SEPTIC SHOCK: WHAT IS IT? – Results from severe systemic inflammatory response (SIRS) to infection CAUSES – Gram-negative and gram-positive bacteria, fungal infections INITIAL FINDINGS – Fast deep respirations, AMS, and cool clammy skin TREATMENT – Antibiotics, IV fluids, and drugs to improve cardiac and vascular performance OBSTRUCTIVE SHOCK: WHAT IS IT? – Results from mechanical obstructions impending blood flow CAUSES – Pulmonary embolism, cardiac tamponade, and tension pneumothorax CLINICAL MANIFESTATION – Right sided heart failure Module 10 - Blood ERYTHROPOIETIN: Hormone produced primarily by the kidneys that stimulates bone marrow to produce erythrocytes HEMATEMESIS: Blood in vomit CLOT FORMATION: RESULT OF ANEMIA: Tissue hypoxia due to the low oxygen carrying capacity of the blood, orthostatic and nonorthostatic hypotension, vasoconstriction, pallor, tachypnea, dyspnea, tachycardia, transient murmurs, angina pectoris, heart failure, intermittent claudication, night cramps in muscles, lightheadedness, tinnitus, roaring in the ears, and faintness HEMOSTASIS: conceptualized as a state of being in which all systems are in balance around a particular ideal “set-point.” SICKLE CELL CRISIS HOW DOES IT CAUSE PAIN: DISSEMINATED INTRAVASCULAR COAGULATION (DIC): WHAT IS IT? – Immune activation of the clotting cascade results in widespread clot formation which consumes platelets and clotting factors resulting in bleeding in other areas CAUSES- Usually due to septic shock WHY WOULD YOU TEST BLOOD COAGULATION? WHY DOES HEPATIC FAILURE CAUSE BRUISING? CHARACTERISTICS OF HEMATOLOGIC NEOPLASMS: CLINICAL MANIFESTATIONS – fever, weight loss, night sweats, itching, fatigue, bone pain, abdominal fullness, bleeding episodes, bruising, petechiae, frequent infections, headaches, n/v, enlarged spleen, liver, lymph nodes, hyperplasia of gums POLYCYTHEMIA VERA: WHAT IS IT? – Blood cells are present in excess, increasing blood viscosity, which in turn causes clinical manifestations such as hypertension CAUSES – Arises from the transformation of a single stem cell into a cell with selective growth advantage that gradually becomes predominant source of marrow precursors. The exact cause is unknown SIGNS/ SYMPTOMS- Headache, backache, weakness, fatigue on exertion, pruritis, dizziness, sweating, visual disturbances, weight loss, paresthesia, dyspnea, joint complications, and epigastric distress and pressure CLINICAL MANIFESTATIONS – Hypertension, thrombosis, and mucosal hemorrhage attributed to engorgement of retinal and sublingual veins [Show More]
Last updated: 1 year ago
Preview 1 out of 21 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 25, 2022
Number of pages
21
Written in
Additional information
This document has been written for:
Uploaded
Feb 25, 2022
Downloads
0
Views
39






 Rasmussen College.png)