*NURSING > STUDY GUIDE > Chamberlain University College : NR 565 SG Week 2 - Ch1.4.13.25.52_ LATEST UPDATED 2021,100% CORRECT (All)
Chamberlain University College : NR 565 SG Week 2 - Ch1.4.13.25.52_ LATEST UPDATED 2021,100% CORRECT
Document Content and Description Below
Chamberlain University College : NR 565 SG Week 2 - Ch1.4.13.25.52_ LATEST UPDATED 2021 Chapter 1: The Role of the Nurse Practitioner as Prescriber Roles and Responsibilities of APRN Prescribe... rs APRN prescriber is responsible for the final decision on which drug to use and how to use it. Degree of autonomy in this role and the breadth of drugs that can be prescribed vary from state to state based on the nurse practice act of that state. Nurse practitioner prescriptive authority is regulated by the State Board of Nursing for each state. • Advanced Knowledge o Additional knowledge, critical thinking, and assumption of a higher level of legal responsibility are required to assume the prescriber role o Knowledge of medicine, pharmacology, and nursing intertwine in the NP role o As a prescriber, it becomes the role and responsibility of the NP to determine the diagnosis for which the drug will be ordered, prescribe the appropriate drug, monitor the expected outcome of the drug, and incorporate a holistic assessment of the impact of disease and therapy on patient lives • Benefits of an APRN as Prescriber o Alternative treatment options are also part of the armamentarium that can be used to treat a given disorder and may interact with the pharmacotherapeutic intervention o APRN look at the big picture and consider alternative treatment options and lifestyle changes o Patients are looked at in a holistic approach and include the patient in decision making regarding their care. o NP practice may thrive under healthcare reform because of the demonstrated ability of nurse practitioners to control costs and improve patient outcomes Clinical Judgment in Prescribing • Prescribing drug results from: o Clinical judgment based on a thorough assessment of the patient and the patient's environment o Determination of medical and nursing diagnoses o A review of potential alternative therapies, and specific knowledge about the drug chosen and the disease process it is designed to treat o NPs factoring in the cost to the patient of the medication prescribed • Is there a clear indication for drug therapy? o In the age of health-care reform and increased awareness of the limitations of drugs, whether a medication is the best option for treatment has become an important question. • What drugs are effective in treating this disorder? o Several drugs may be effective in treating a condition, so which one is best for a particular patient? Even if only the most effective class of drug is considered, few classes of drugs include only one drug o How does one determine “best”; what are the criteria? Are there nationally recognized guidelines that can be used? The Agency for Health Care Quality (AHCQ), the National Institutes of Health (NIH), and many specialty organizations publish disease-specific treatment guidelines that include both pharmacological and nonpharmacological therapies Consult nationally recognized guidelines for disease management • What is the goal of therapy with this drug? o What is the best drug to achieve treatment goals? Various goals are possible in the choosing of therapy • Under what conditions is it determined that a drug is not meeting the goal and a different therapy or drug should be tried? o At the onset of therapy, the provider and patient should have a clear understanding of what outcome or goal is expected of the medication prescribed o Follow-up and monitoring times are established to see how well treatment with the drug is meeting the goal • Are there unnecessary duplications with other drugs that the patient is already taking? o The patient’s medication history should be reviewed at each encounter to detect duplications or medications that may be discontinued • Would an OTC drug can be just as useful as a prescription drug? o Increasing numbers of drugs are being moved from prescription to over-the-counter (OTC) status • What about cost? o Who will pay for this drug? Can the patient afford it? Will the cost of the medication affect adherence to the treatment regimen? Cost is an issue for several reasons • Many insurance policies do not cover the cost of drugs or only provide partial coverage, so the patient must pay “out of pocket” • The newer the drug, the more likely the cost is too high based on the drug manufacturer’s need to reclaim research and development costs while the corporation still holds the patent on that drug • Newest is not always best, and condition of cost is a major factor in choosing between newer drugs and ones that have been around long enough to be available in generic form • Many insurance plans have larger copays for name-brand drugs than for generic medications • Multiple national retail pharmacies have developed $4 prescription formularies • Awareness of what is on the local discount formulary may save the patient hundreds of dollars in prescription costs and may increase compliance • Factors likely to lead to poor adherence include a drug that is expensive in relation to a patient's finances, a drug that must be taken daily as part of a complex regimen, and a drug that is not covered by insurance. • Where is the information to answer these questions? o Wide array of professional literature that ranges from the well-reputed journals to literature from specialty and professional organizations, the multitude of computerized drug databases Collaboration with Other Providers Collaborate with physicians, pharmacists, podiatrists, mental health specialists, therapists, and other providers, including APRNs who are not NPs, physician assistants (PAs), and other nurses. • Physicians o Early in the development of the NP role, physicians were the teachers in the NP programs and accepted NPs as physician-extenders • Pharmacists o Profession of pharmacy requires graduate-level preparation for all pharmacists with the granting of a practice doctorate, the Doctor of Pharmacy (PharmD) o A PharmD can assist by offering expertise on the clinical management of patients, including available dosage forms, potential adverse reactions, and drug interactions • Other APRNs o Collaboration with other NPs and APRNs who have prescriptive privileges has two major advantages On a one-to-one basis dealing with individual patient issues, NPs and APRNs can share “clinical pearls” from their knowledge base and collaborate to improve the care of the patient Collaboration on issues related to scope of practice and prescriptive privilege at the state and national level is critical to obtaining and maintaining the autonomy of practice needed to provide optimal patient care • Physician Assistants o The focus of the PA's practice is similar to that of the physician, so both the APRN and the PA can benefit from interaction with each other in much the same way as from their interaction with physicians o Many PAs desire more autonomy in their practice, and the experience of APRNs in developing autonomy may be helpful • Nurses Not in Advanced Practice Roles o APRNs regularly collaborate with other nurse colleagues who are not in advanced practice roles o Some have specialized knowledge, such as Certified Diabetes Educators (CDEs) and Wound and Ostomy Care Specialists (WOCS) o These nurses and their assistants carry out the prescriptive orders of the APRN Autonomy and Prescriptive Authority More states are broadening and expanding the legal, reimbursement, and prescriptive authority to practice for all APRNs, including NPs. • Reimbursement o Reimbursement is evolving, with the Affordable Care Act rollout creating an opportunity for APRNs to address reimbursement parity o The reimbursement by third-party payers continues to be a practice barrier for many nurses in advanced practice • Drug databases o PharmGKB o WAITING FOR CLARIFICATION • Medication adherence o WAITING FOR CLARIFICATION Chapter 4: Legal and Professional Issues in Prescribing New Drug Approval Process Including Clinical Phases I-IV Costs a company approximately $2.6 billion. Takes 8.5 years on average for an experimental drug to travel from laboratory preclinical trials to FDA approval. • State One: Preclinical Research o Process of synthesis and extraction identifies new molecules with the potential to produce a desired change in a biological system o Produced through artificial synthesis or extracted from natural sources Biological screening and pharmacological testing use nonhuman studies pharmacological activity and therapeutic potential of compounds-- animals, isolated cell cultures and tissues, enzymes, and cloned receptor sites, as well as computer models o Pharmaceutical dosage formulation and stability testing make up the process of turning an active compound into a form and strength suitable for human use o Toxicology and safety testing determines the potential risk a compound poses to people and the environment • Stage Two: Clinical Investigation o Investigational new drug (IND) application is filed with the FDA prior to human testing of any new drug entity--description of the clinical research plan -- clinical tests can begin 30 calendar days after submission Phase 1: Establishing the tolerance of healthy human subjects at different doses; defining its pharmacological effects (absorption, distribution, metabolism, and excretion). Phase II: Target disease or disorder to determine a compound's potential --small number of patients. Phase III: Trials are controlled and uncontrolled clinical trials of a drug's safety and efficacy in hospital and outpatient settings--drug's efficacy for specific indications-- broader range of adverse effects --best way of administering and using the drug for the purpose intended.--verify that the acceptable risk/benefit ratio seen in phase II persists under--must report in writing to the FDA within 10 working days any serious and unexpected adverse reactions. • Stage Three: NDA Review o To market a new drug for human use, a manufacturer must have a new drug application (NDA) approved by the FDA o All information about the drug gathered during the drug discovery and development process is assembled in the NDA o During the review period, the FDA may ask the company for additional information about the product or seek clarification of the data contained in the application o The FDA has 60 days to determine whether the NDA will be filed for review o Once filed, a team reviews the drug sponsor’s research on safety and effectiveness of the drug o Usually, the FDA requests additional information, and the manufacturer needs from 1-5 years to complete any additional well-controlled trials necessary to support the claimed indications or prove the drug’s safety • Stage Four: Postmarketing Research o In order to detect rare adverse drug reactions, hundreds of thousands of patients have to have taken the drug. Clinical trials conducted after a drug is marketed are an important source of information for postmarketing evaluation o Regulatory authorities can require companies to conduct phase IV studies as a condition of market approval o An important source of postapproval information is data collected and submitted by practitioners in the field through programs such as MedWatch U.S. FDA Regulatory Jurisdiction • Official Labeling o The legal distinction between a legend drug and an over-the-counter (OTC) drug is not founded on relative safety per se but rather involves a regulatory decision on whether adequate directions for the drug's proper use can be written for the layperson o The FDA is concerned with the marketing and availability of drugs that have demonstrated substantial evidence of an acceptable risk/benefit ratio for labeled indications o The proper and efficacious therapeutic use of these drugs is the responsibility of the prescriber o FDA regulates the official labeling for all prescription and OTC drugs • Off-Label Use of Drugs o Use of an FDA-approved drug in a dose or route for which it was not approved or for a clinical indication other than the FDA-approved use o Nurse practitioners (NPs) are responsible for knowing the FDA indication and approval status of any drug they prescribe o Prescribing is legal if there is scientific evidence for the use • Controlled Substance Laws o The most comprehensive federal drug legislation is the Controlled Substances Act of 1970 o Every person who manufactures, distributes, prescribes, procures, or dispenses any controlled substance must register and obtain a registration number with the U.S. Drug Enforcement Administration (DEA) o NPs wanting authority to prescribe controlled substances must apply for state prescriptive authority prior to application for a federal DEA number o National Provider Identifier number (NPI) The NP should obtain an NPI as soon as it is feasible NPs must know the different classifications and schedules of controlled drugs as well as the associated prescribing rules and regulations • Controlled Substance Prescribing Precautions o Some states, NP's license number appear on the prescription in addition to that of any supervising/collaborating practitioner o DEA registration number must be designated on all controlled substance prescriptions o DEA registers manufacturers and prescribers of controlled substances o Prescription should be dated on the day it is written, indicating any authorized refills as allowed and clinically appropriate o As of 2009, tamper-proof prescription pads are required for prescriptions written for patients under Medicaid payment plans Controlled Drug DEA Schedules (Table 4-1) Schedule Controls Required Drug Examples I No accepted medical use No legal use permitted For registered research facilities only Heroin, LSD, mescaline, peyote, marijuana* II No refills permitted No telephone orders unless true emergency and followed up by written prescription within 7 days Electronic prescribing permitted as of 2011 with specific software and secure identification processes Narcotics (morphine, codeine, meperidine, opium, hydromorphone, oxycodone, oxymorphone, methadone, fentanyl) Stimulants (cocaine, amphetamine, methylphenidate) Depressants (pentobarbital, secobarbital) III Prescription must be rewritten after 6 mo or 5 refills Telephone or fax prescription okay Narcotics (codeine in combination with non-narcotic ingredients not to exceed 90 mg/tab; hydrocodone not to exceed 15 mg/tab) Stimulants (benzphetamine, chlorpheniramine, diethylpropion) Depressants (butabarbital) Anabolic steroids, testosterone IV Same as Schedule III Penalties for illegal possession are different Pentazocine, phentermine, benzodiazepines, meprobamate V Same as all prescription drugs May be dispensed without a prescription unless regulated by the state Loperamide, diphenoxylate Cough medications with less than 200 mg/100 mL Pregabalin *Marijuana may be classified under individual state law as a Schedule II drug and used for medical purposes. It may not be “prescribed,” however. Controlled Substance Misuse • Prescriber Education o Many opportunities for individuals to obtain excessive quantities of controlled drugs, either intentionally or as a result of duplicate prescribing o Principles for prescribers related to prescription drug misuse assessment include the following: Acquisition and wide use of chemical dependence screening skills/tools Early and firm limit setting regarding indications for controlled drug prescribing o Careful documentation of a confirmed diagnosis and the ruling out of chemical dependence before initiating a controlled prescription or drug subject to misuse o Practice in “just saying no” and feeling comfortable in being firm without escalating the discussion into an argument with the patient o Set limits • Behavioral Red Flags o Almost every practice experiences the chemically dependent patient who uses dishonest mechanisms to obtain increasing supplies of controlled prescriptions o Scams are generally conducted to obtain more medications, more potent or higher-dosage formulations, higher street-value brands of drugs, a controlled drug without a chart or visit note, or to avoid noncontrolled alternatives o Patient-generated pressure to prescribe in the face of clinician hesitancy is one classic sign of a scam o Prescription altering and forging are a frequently encountered scam o Stealing or borrowing another patient’s drugs • Pressure to Prescribe o Another factor that increases the demand for controlled substances is the pressure to prescribe at every visit and the expectation that patients deserve a prescription for something at each visit or for each symptom offered o This process results in two well-known adverse situations Overprescribing of antibiotics and resulting antibiotic resistance Polypharmacy Complaints • Enabling o The powerful instinct in practitioners to do anything medically possible to enable patients with present or potential disability to live at a higher level of function When You Suspect a Patient is Misusing Medications • Communication Barriers o Clinical interview and practitioner–patient relationship-building skills Skill building involves active learning strategies in the areas of verbal and nonverbal communication, empathy, and rapport building Communication Skills • One strategy is to just say no and mean it. By making the statement “I am feeling pressured by you to write a prescription today that is not clinically indicated. Because of this I am really concerned about you, and we need to talk about your use of alcohol or other substances,” the NP can often effectively turn the tables and shift the discomfort to the patient while still refusing to prescribe • Systemic Solutions to Problems of Controlled Substance Prescribing o Careful charting and documentation habits are essential for prescribing controlled drugs Document clearly in a progress note • Physical evaluation of the patient • The diagnosis • The clinical indications for treatment • The written treatment plan • The expected symptom outcomes • Informed consent and agreement for treatment from the patient • Consultation and/or collaboration necessary to meet treatment goals and objectives • These strategies reduce, but do not eliminate, the risk of controlled drug diversion from one's practice • Prescribing Tips o A few tips can help the practitioner reduce environmental facilitation of prescription misuse Collect and document a complete history and examination before prescribing controlled substances • Do not rely on patient-supplied history, xrays, or medical records to confirm your assessment—obtain this information directly from the primary source • Passik and Weinreb (2000) advise use of the four “A’s” to guide initial and ongoing assessment of medication efficacy o Analgesia measurement by use of pain scales or other assessment tools o Activities of daily living (ADLs) as measured by levels of physical and psychological functioning o Adverse effects o Abuse issues Prescribe limited quantities without refills on a first visit, allowing additional time for patient assessment and confirmatory documentation Educate medical and assistive staff in reinforcement of consistent clinic policies and procedures related to scheduling, forms, urine drug screening, records view and release, and refills • It is not uncommon for patients who do misuse substances to quickly identify the “weak link” among the treatment team and focus their energies on this person or process • Standardize expectations regarding after-hours calls, use of multiple providers, and weekend or early refills and post them where they are readily available Patients covered by insurance plans, including Medicaid and Medicare, can be limited to one pharmacy or one prescriber through their payment plan Case managers can often be utilized to help review and manage medication use and advocate for access to additional options for pain management and control Other tips • Prescribing generic, longer-acting formulations of drugs that have less stress value • Writing out the quantity prescribed rather than using only numerals, which can be altered • Use tamper-proof paper for all prescriptions written for controlled drugs • Medication Agreements/”Pain Medication Contracts” o Defining and implementing treatment objectives is the medication agreement This written tool can be incorporated into treatment of chronic pain, particularly if long- term management with opioids is indicated o NPs are advised to familiarize themselves with urine drug and alcohol screens and their availability, cost, sensitivity, and specificity o In-office rapid screenings are now available that can be done quickly and without prior notice in order to confirm adherence to medication agreement criteria o Contract used universally for all prescribing for chronic pain • Prescription Drug Monitoring Programs o As of 2012, all but one state (Missouri) have an active or legislatively enabled Prescription Drug Monitoring Program (PDMP) o A PDMP enables practitioners to query a confidential database of controlled substances statewide to evaluate • State Law o Authority to prescribe is a function of state law o Prescriptive authority varies from state to state o A license is always required for practice as an NP o The state Nurse Practice Act specifies the exact title that must be used for practice and on a prescription o Independent authority permits the prescriber to exert autonomous judgment o Dependent authority exists when the primary prescriber delegates the authority to another through a collaborative or supervisory agreement status of prescribing in each state • Writing and Transmitting the Prescription o Use preprinted prescription pads/electronic templates that contain the name, address, and telephone number and NPI number of the prescriber o This will allow the pharmacist to contact the prescriber if there are any questions about the prescription Designate the complete drug name, strength, dosage, and form Indicate the date of the prescription Use metric units of measure, such as milligrams and milliliters; avoid apothecary units of measure Avoid abbreviations Avoid the use of “as directed” or “as needed.” Include the general indication, such as “for infection.” Indicate “Dispense as Written” if generic substitution is not desired Include the patient weight, especially if pediatric or elderly Indicate if a safety cap is not required, as medications will be dispensed with them by default o Schedule II drugs may not be refilled and require a new prescription for each dispensed quantity o What May Be Prescribed Legend drugs (approved by FDA, prescription medications) Prescriptions are required for the majority of controlled drugs --medical devices, home- health and home-testing equipment, durable medical equipment, needles and syringes, and sometimes for Medicaid or Medicare coverage of OTC medications that are required for patient health FDA approval is required for medical devices, including artificial joints o State-Specific Elements NPs who prescribe in a state with mandated collaboration or supervision may need to indicate the name and information of this person on their prescriptions A state can also designate that a drug is controlled and requires a DEA number o Electronic Prescribing and Secure Prescribing The days of “writing” a prescription may soon be over Electronic prescribing As of June 1, 2010, the DEA's revised “Electronic Prescriptions for Controlled Substances” regulation provides practitioners with the option of writing prescriptions for controlled substances electronically Ethical Aspects of Prescribing • Informed Consent o Provider who performs a specific service is responsible for obtaining consent Referring provider is not responsible for getting consent for a procedure performed by another provider Some exceptions may apply, Informed consent has four critical features • (1) a competent patient (2) who is provided adequate information with which to make a decision (3) and who voluntarily (4) consents to a proposed intervention In general, an adult is presumed to be legally competent unless declared incompetent in formal legal proceedings • Clinical competence is also not an all-or-none phenomenon • Mental health medications have specific consent regulations due to the vulnerability of their target population. --elderly or minor patients • Parental or partner involvement in prescribing determinations related to sexually transmitted infections, family planning, and birth control may be limited under specific state law • Prescribing for Self, Family, or Friends o NO SELF Prescribing o Limited family/friends--may not be ethical • Sale of Pharmaceuticals and Supplements o Can not sell samples provided for free o May stock and sell limited commonly prescribed med o May sell supplements –vitamins Chapter 13: Over-the-Counter Medications OTC Medication Characteristics and Regulation • Characteristics o Must be safe o Has low potential for misuse or abuse o Can be labeled o Patient must be able to self-diagnose the condition for which the drug is being taken o Must be for a condition that the patient can manage without supervision by a licensed health professional • Regulation o FDA Center for Drug Evaluation and Research (CDER) is responsible for ensuring that OTC drugs are properly labeled and that their benefits outweigh their risks o New OTC drug ingredients must undergo the New Drug Application process, just like prescription drugs OTC Medication Sales • The Consumer Healthcare Products Association (CHPA) o $33.1 billion in 2013 in sales of OTC medications o Proposes that every dollar spent on OTC medications by consumers saves the U.S. healthcare system $6-$7, based on cost savings in clinical visits and drugs • Pharmaceutical companies may apply for the drug to change to OTC status in order to continue making large profits from their blockbuster brand-name drug • Cough and colds are the ailments that generates the greatest OTC annual drug sales Hazards of OTC Self-Medication • Self-Prescribing o The treatment of common health problems with medicines especially designed and labeled for use without medical supervision and approved as safe and effective for use • Interactions o OTC medications may be harmful if misused or may cause harmful interactions with prescription drugs Ex: A patient may accidentally overdose on acetaminophen by taking two OTC medications that both contain acetaminophen or by taking OTC acetaminophen with prescription drugs that contain acetaminophen such as Vicodin or Percocet Adverse Effects of OTC Self-Medication • Adverse Effects o All medications have predictable and unpredictable adverse effects o May be mild such as GI upset, or severe, such as GI bleeding associated with NSAID or aspirin use • Treatment Duration o Exceeding treatment duration or taking the wrong dose increases the likelihood of adverse reactions • Patient Education o Patients must be educated regarding the adverse effects of OTC medications o Education includes reading the label carefully and asking questions of a pharmacist or the provider o Patients must be educated about disclosing intermittent OTC medication use as part of their drug history Drug Interactions • Antacids o Consist of a metallic cation and basic ion (calcium carbonate, magnesium hydroxide), which neutralize acidity in the stomach by raising the pH o Basic property of these drugs causes them to interact with most medications by either binding with the drug molecule or altering pH and thus the absorption of drugs that need an acidic environment for optimal absorption o Most interactions can be avoided by separating the dosing of antacids by at least 2 hours from the dosing of the other oral medications Ex: tetracycline. Aluminum hydroxide and magnesium hydroxide have a strong affinity for tetracycline and form an insoluble and inactive chelate. This interaction can reduce bioavailability of tetracycline by 90% • Anticholinergics o The primary adverse effects of diphenhydramine and doxylamine are anticholinergic, such as dry mouth, constipation, blurred vision, and tinnitus o Older male patients may have difficulty in urinating o Older patients may develop delirium from modest doses of diphenhydramine • CNS Depressants o OTC medication taken with prescribed medication can cause additive CNS sedating effects o OTC medications that contain alcohol, antihistamines, antitussives, or antidiarrheals may all cause additive sedation when taken with CNS-sedating medications • NSAIDS & ASA o The cyclooxygenase inhibitors (aspirin & NSAIDS) have a well-documented risk of GI bleeding o When combined with antiplatelet or anticoagulant medications, the risk is significantly increased and may be life-threatening o Patients who are taking antiplatelet or anticoagulant medications should be educated to not taking any OTC medication without consulting with a pharmacist or their provider Abuse of OTC Medications • Combat Methamphetamine Epidemic Act o Concern over the use of OTC decongestant medications to manufacture methamphetamine has led to changes in how the drugs are sold in the U.S o The Combat Methamphetamine Epidemic Act (2006 Patriot Act) restricts the sales of all cough and cold products that contain methamphetamine precursor chemicals ephedrine, pseudoephedrine, or phenylpropanolamine o The law includes a daily and 30-day limit on retail store and internet purchases of known methamphetamine precursors o All potential precursors are to be stored behind the counter in retail stores and retailers are required to ask for ID and keep a log of who is purchasing the drugs Patient Education Regarding OTC Medications • Patients should be educated on reading the label and following the label instructions • If the patient does not understand the label, they should ask for assistance from a pharmacist or provider • Educating patients that even though a medication is available OTC, it still has the same concerns for adverse effect, drug interactions, and toxicity as prescription medication Chapter 25: Anti-inflammatories: NSAIDs, Acetaminophen & Aspirin Pharmacodynamics Two cyclo-oxygenase isoenyzmes have been identified: COX-1 and COX 2. • COX-1 o Expressed systemically and synthesized continuously so that it is present all the time in all tissues and cells, especially platelets; endothelial cells; the GI tract; and renal microvasculature, glomeruli, and collecting duct o It has roles in homeostatic maintenance, such as platelet aggregation, the regulation of blood flow to the kidney and stomach, and the regulation of gastric acid secretion and production of protective mucus, especially in the stomach o Inhibition of these activities by NSAIDs accounts for their adverse reactions, especially on the renal and GI tracts • COX-2 o An inducible enzyme that is synthesized mainly in response to pain and inflammation o Nonspecific NSAIDs inhibit both COX-1 and COX-2. Most NSAIDs (aspirin, ketoprofen, flurbiprofen, indomethacin, piroxicam, sulindac) are mainly selective for COX-1 o Some (ibuprofen, naproxen, diclofenac) are slightly selective for COX-1, and others (etodolac, nabumetone, meloxicam) are slightly selective for COX02 • COX-2 Selective Drugs o Three COX-2 selective drugs (celecoxib, rofecoxib, valdecoxib) have been developed that appear not to inhibit COX-1 These drugs were used for patients who had higher risks for GI bleeding In 2004 research indicated that the overall risk for GI bleeding was not sufficient to compensate for the increased risk of cardiovascular events that occurred with these drugs Rofecoxib and valdecoxib are no longer on the market At this time, a Black-Box Warning was placed on all NSAIDs and on celecoxib related to this risk • Label Changes o In 2005, the FDA requested that sponsors of all NSAIDs and celecoxib add to the labeling a boxed warning about cardiovascular risk events and the well-described, serious GI bleeding associated with their use o Medication Guide must now be provided with each prescription • Acetaminophen o Analgesic and antipyretic with limited anti-inflammatory activity o Although its mechanism of action is unknown, it is thought to act by inhibiting central and peripheral prostaglandin synthesis o Central inhibition is almost as potent as that of aspirin, but its peripheral action is minimal o Reduces fever by direct actions on the hypothalamic heat-regulating centers, which increase dissipation of body heat via vasodilation and sweating o Has advantages of minimal GI irritation and of not affecting bleeding times, uric acid levels, or respiration Pharmacokinetics • After oral administration, NSAIDs are rapidly and almost completely absorbed • All NSAIDs are more than 90% protein bound • Widely distributed in tissues, cross the placenta, and enter breast milk in low concentrations • NSAIDs are all metabolized by the liver and excreted by the kidneys, primarily as metabolites • Acetaminophen is extensively metabolized by the liver and excreted by the kidneys, primarily as inactive metabolites • When it is taken regularly or in large doses, the stores of one hepatic conjugate become depleted, and hepatic necrosis may occur Pharmacotherapeutics • Only relative contraindications are for ketorolac, mefenamic acid, flurbiprofen, and nabumetone in the presence of preexisting renal impairment • Because NSAID metabolites are excreted primarily by the kidneys, all others should be used with caution in the presence of renal function impairment • The liver extensively metabolizes NSAIDs • Naproxen may exhibit an increase in unbound fraction and reduced clearance of free drug in cirrhotic patients • A reduced dose may be necessary • Acetaminophen Poisoning o Common cause of poisoning, either intentional or accidental, due to the lay public underestimating the toxicity of the drug o A single dose of 150mg/kg of acetaminophen in children or 7.5 g to 10g in adults may be toxic o Drugs that induce CYP2E1 enzymes (carbamazepine, phenobarbital, phenytoin, isoniazid, and rifampin) or alcohol ingestion may cause hepatotoxicity when combined with acetaminophen o Stages Stage 1: 0.5-24 hours: Nausea, vomiting, diaphoresis, pallor, and anorexia. Some patients may be asymptomatic initially. Stage 2: 25-72 hours: Clinically improved; AST, ALT, bilirubin, and prothrombin levels begin to rise. Stage 3: 72-96 hours: Peak hepatotoxicity; jaundice, confusion, AST of 10,000 not unusual. Stage 4: 4-14 days: Death or recovery. Patients who survive enter a recovery phase. o Treatment Should be referred to a poison control center hospital If this is not possible, the following treatment regimen may be followed • If the acute ingestion is more than 150mg/kg or the dose cannot be determined, obtain a serum acetaminophen assay 4 hours after ingestion • If the level is more than 300mg/mL, hepatic damage has occurred in 90% of patients Minimum hepatic damage results from a level below 120mg/mL Treatment is by gastric lavage in all cases, preferably within 4 hours of ingestion Oral N-acetylcysteine is a specific antidote for acetaminophen toxicity Contact a poison control center for correct dosing of the antidote Drug Interactions • NSAIDs decrease the effectiveness of antihypertensive drugs because of their tendency to cause fluid retention and increased extracellular fluid volume • Coadministraction with anticoagulants may prolong prothrombin time because both drugs affect platelet aggregation (ex. Warfarin) • Drugs that have adverse reactions associated with increased risk for GI bleeding or ulcerations associated with increased risk for GI bleeding or ulceration have an even higher risk if taken with NSAIDs • Drugs that require glucuronidation for metabolism may affect the metabolism of acetaminophen by competing for metabolic sites Rational Drug Selection • There is no clear difference in efficacy between NSAIDs, although there may be individual differences in response • The rationale for choices is provided in the Clinical Use and Dosing section below • Acetaminophen is used for fever and for mild to moderate pain not associated with inflammation! Monitoring • Required for long-term therapy • Because NSAIDs may produce acute renal insufficiency, assess renal function (serum Cr) before initiation of therapy and annually throughout long-term therapy • A CBC prior to initiation of therapy and annually is appropriate because of the risk for GI bleeding Patient Education • Take the dose exactly as prescribed • A missed dose should be taken as soon as the patient remembers unless it is almost time for the next dose • For drugs taken more than once daily, ideally the missed dose should be taken within 1-2 hours of the time it was scheduled • Doses should not be doubled • Taking higher doses than prescribed dose not increase efficacy and may increase adverse reactions • Patients should be informed if there is a prescribed length of time beyond which the drug may not be taken. • Taking the drug with food or a full glass of fluid and remaining in an upright position for 15-30 minutes may reduce GI discomfort and adverse reactions • Remind patients to avoid aspirin, alcohol, or other GI irritants while taking these drugs • Patients should be aware of products that may contain acetaminophen, including cough and cold products and combination opioid products to avoid accidental overdose of acetaminophen Clinical Dosing for RA • Initial drug treatment involves the use of salicylates, NSAIDs, or celecoxib to reduce join pain and swelling and to improve joint function • They have analgesic and anti-inflammatory properties but do not alter the course of the disease or prevent joint destruction, so they should not be used as the sole treatment for RA • Choice is determined by adverse reactions, cost, duration of action, and patient preference. See Table 25-9 page 823. Clinical Dosing for OA • No known cure for OA • Treatment can help to maintain or improve join mobility and limit functional impairment • Drug therapy includes acetaminophen, NSAIDs, and COX-2 inhibitors • Topical agents such as capsaicin (hand OA only) and trolamine salicylate may also be used • Initially, acetaminophen in doses 650mg 4x/day or 1g 3x/day (maximum 3g/24hrs) are given to manage joint pain • If this drug fails to control pain, NSAIDs are prescribed • All NSAIDs except ketorolac and mefenamic acid have an indication for treatment of OA. See Table 25- 9 page 823. Clinical Dosing for Gout • Indomethacin, naproxen, and sulindac list acute gout as an indication. See Table 25-9 page 823. • Low dose colchicine can be prescribed o May cause diarrhea • If patient is taking allopurinol, monitor BUN, creatinine, and creatinine clearance labs • Febuxostat (Uloric) may worsen gout with therapy when starting medication Clinical Dosing for Mild to Moderate Pain • Ibuprofen is the most commonly used because it is inexpensive, available OTC, and short-acting so that acute pain can be managed without long-term effects and adverse reactions • Acetaminophen is useful in treating mild to moderate pain that is not accompanies by or caused by inflammation • It is not intended for pain management for more than 5 days in children or 10 days in adults because of the increased risk for hepatic adverse reactions • For adults, a dose of 325 to 650mg every 4-6 hours usually suffices • Children’s doses are based on weight: 10-15mg/kg per dose every 4-6 hours • After age 14 adult dose is used. See Table 25-9 page 823. Clinical Dosing for Dysmenorrhea • Ibuprofen, diclofenac potassium, ketoprofen, meclo-fenamate, mefenamic acid, and naproxen are the drugs used for dysmenorrhea • The best response occurs if NSAIDs are starting with the onset of menses symptoms. See Table 25-9 page 823. Clinical Dosing for Tendinitis/Bursitis • Indomethacin SR, naproxen, and sulindac are used • Naproxen and sulindac both are intermediate-acting and provide longer duration of action than indomethacin • Naproxen is less likely to produce GI adverse reactions • These same three drugs are used to manage the pain in gout because it is associated with inflammation. See Table 25-9 page 823. Clinical Dosing for Fever • Ibuprofen is the NSAID of choice for fever in children over age 6 months and adults • Acetaminophen may also be used for this purpose, but for no longer than 3 days • Patients should be well hydrated if using ibuprofen for fever to decrease renal toxicity. See Table 25-9 page 823. Aspirin • Pharmacodynamics o All salicylates have analgesic, anti-inflammatory, antipyretic, and antiplatelet actions o Salicylates lower body temperature through their effect on the hypothalamic thermostat and vasodilation of peripheral vessels, thus enhancing dissipation of heat • Prostaglandin o The anti-inflammatory and analgesic activities are mediated through inhibition of prostaglandin synthesis in the same manner as NSAIDs o However, aspirin more potently inhibits prostaglandin synthesis and has greater anti- inflammatory activity than the NSAIDs o The acetyl group of the aspirin molecule is thought to be responsible for these differences • COX Inhibitor o Aspirin acetylates the cyclo-oxygenase enzyme in the prostaglandin biosynthesis pathway; therefore, it may be theoretically classified as a COX inhibitor • Antiplatelet o Aspirin also irreversibly inhibits platelet aggregation o Single analgesic-level doses prolong bleeding time o Acetylation of platelet cyclo-oxygenase prevents synthesis of thromboxane A, which is a potent vasoconstrictor and inducer of platelet aggregation for the life of the platelet o This drug has shown success as an antiplatelet agent for patients with thromboembolic disease Pharmacokinetics • Salicylates are rapidly and completely absorbed after oral administration • Bioavailability depends on the dosage form, gastric emptying time, gastric pH, presence of antacids or buffering agents, and particle size • Salicylic acid is eliminated by renal excretion of salicylic acid and by oxidation and conjugation of metabolites by the liver • Include H2 blockers if patient complains of heartburn to prevent GIB Pharmacotherapeutics • Taking salicylates, especially aspirin, by children or adolescents with influenza or chickenpox has been associated with the development of Reye Syndrome (vomiting, lethargy, delirium and coma) • The mortality rate is 20-30%, and permanent neurological deficits have been reported in survivors • Long term therapy should have CBC checked annually • Hepatic Impairment o Salicylates should be used cautiously for patients with hepatic impairment o Reversible hepatic encephalopathy has occurred after even therapeutic doses for RA • Renal Impairment o Cautious use is also required for patients with renal insufficiency because salicylates may cause a transient decrease in renal function and aggravate chronic kidney diseases • Uric Acid Accumulation o In low doses (<2g/day), they decrease urate excretion and raise serum uric acid levels o At high doses (3-5g/day), they have a uricosuric effect; however, they are rarely tolerated at this high a dose • Gout o Salicylates should be used with caution in the presence of gout • ADRs o Most common adverse reaction to salicylates is GI irritation and bleeding o The amount of blood lost from GI bleeding secondary to salicylate use is usually clinically insignificant, but with prolonged use it can result in IDA o Hypersensitivity to salicylates or NSAIDs contraindicates aspirin use and requires extremely cautious use of the other salicylates o Aspirin sensitivity is more prevalent in patients with asthma, nasal polyps, or chronic urticaria o Ototoxic at increased blood levels Should be discontinued if dizziness, tinnitus, or impaired hearing develops Temporary hearing loss disappears gradually when the drug is stopped • Toxicity o The acute lethal dose of salicylates in adults is 10-30g, and in children it is 3 g o Chronic salicylate toxicity can occur when more than 100mg/kg is ingested daily for 2 or more days o Signs of salicylate poisoning appear at serum levels of 30-60mg/dL o Early sign of toxicity is tinnitus o Respiratory alkalosis is seen initially o Hyperpnea and tachypnea occur as a results of increased CO2 production and a direct stimulatory effect of the salicylate on the respiratory center in the brain o Other symptoms include nausea, vomiting, hypokalemia, tinnitus, disorientation, irritability, seizures, dehydration, hyperthermia, thrombocytopenia, and other hematological disorders • Treatment o Induction of emesis or gastric lavage to remove any unabsorbed drug from the stomach o Activated charcoal diminishes salicylate absorption if it is given within 2 hours of ingestion o Salicylate levels and acid-blasé, fluid, and electrolyte balances are carefully monitored o Forced alkaline diuresis by administering sodium bicarbonate increases salicylate excretion. Hemodialysis for severe poisoning Clinical Use and Dosing for Fever • Aspirin is the salicylate of choice for reduction of fever in adults • Contraindicated for use with pregnant patients • Acetaminophen or ibuprofen are probably better for fever management in children because there is not the risk of Reye syndrome. See Table 25-12 page 832. Clinical Use and Dosing for Mild to Moderate Pain • Pain associated with inflammation is especially well managed with salicylates or NSAIDs • Aspirin, choline salicylate, choline magnesium salicylate, and diflunisal are all approved for this indication. See Table 25-12 page 832. Clinical Use and Dosing for RA • Salicylates or NSAIDs can be used as adjunctive treatment for RA • Serum levels can be measured to determine adherence and therapeutic efficacy, and it is the least expensive salicylate • Nonacetylated salicylates are less potent anti-inflammatory agents, but have fewer adverse reactions than aspirin • A therapy trial of 3-4g/day for 4-6 days is recommended because 70-80% of patients who will respond will do so within this time frame • Older adults are less tolerant to the adverse GI reactions, and their trial dose should be 2-3g/day • Blood levels should be drawn before changing drugs • If the salicylate level is too low but the patient has been adherent and tolerates the aspirin, the dose should be increased by 325-650mg/day until the desired anti-inflammatory level of the drug is reached. See Table 25-12 page 832. Clinical Use and Dosing for OA • Usually well tolerated in divided doses of 1.2-2.4g/day • NSAIDs tend to have more adverse reactions with no better pain relief when given at anti-inflammatory doses over the course of more than a few days • The nonacetylated salicylates are also effective and have fewer GI adverse reactions than aspirin • Diflunisal has the advantage of twice-daily dosing but may take up to 2 weeks to achieve full anti- inflammatory effects. See Table 25-12 page 832. Clinical Use and Dosing for MI Prophylaxis • Low dose aspirin (75-100mg daily) is recommended in patients age 50 years or older for primary prevention of cardiovascular disease • It is recommended that low dose aspirin (75-100mg/day) or clopidogrel be given in patients with established coronary artery disease, patients with coronary stenosis greater than 50% and those with evidence of cardiac ischemia. See Table 25-12 page 832. Clinical Use and Dosing for TIAs • Aspirin (50-325mg/day) monotherapy or a combination of aspirin and extended release dipyridamole are accepted therapy options for stroke prevention. See Table 25-12 page 832. Monitoring • A random salicylate level should be drawn 7-10 days after initiation of chronic therapy • Periodic salicylate levels should be drawn during long-term management to check maintenance of therapeutic levels and monitor for toxic manifestations • Elimination o Because all of these drugs are eliminated by the kidneys and dosage adjustments may be required based on renal function, serum Cr levels should be assessed before therapy is begun and annually throughout long-term therapy o Urinary pH should also be monitored regularly o Sudden acidification of urine can more than double the plasma salicylate level, resulting in toxicity • CBC o Salicylates interfere with homeostasis o A CBC should be drawn prior to initiating therapy and at least annually throughout long-term therapy o A CBC should also be drawn and fecal occult blood studies should be done as well if there is any indication of GI bleeding • Hepatic Function o Should be monitored prior to anti-rheumatic therapy and if hepatotoxicity symptoms occur o These problems are more likely in patients with rheumatic fever, juvenile RA, or preexisting hepatic diseases, especially children • Ophthalmic Effects o Have been reported in patients taking diflunisal o Ophthalmic studies are appropriate for patients who develop eye complaints during therapy Patient Education • Instruct the patient to take salicylates exactly as prescribed • Taking with food or a full glass of water and remaining in the upright position for 15-30 minutes after administration can reduce GI irritation. Food slows absorption but does not alter the total amount absorbed • Do not crush or chew enteric-coated tablets or take antacids within 1 hour of enteric-coated tablets • Chewable tablets may be chewed, dissolved in liquid, or swallowed whole • Instruct patients not to increase the dose beyond that prescribed • Increased doses increase the risk for salicylate poisoning • Most common adverse reactions are ototoxicity and GI irritation/bleeding • Advise patients to report tinnitus; unusual bleeding from the gums; bruising; black tarry stools; or fever lasting longer than 3 days • Patients taking salicylates should not use alcohol or other substances that increase GI irritation • Parents should be informed of the risk of Reye Syndrome and educated regarding not giving aspirin to a child with a viral illness Prednisone • If patient is taking 10mg daily > 6 mo, monitor for osteoporosis, especially in women • If patient’s total dose will exceed 1 gram, patient will need a second prescription for omeprazole or a PPI to prevent peptic ulcer disease • When discontinuing prednisone, develop a tapering schedule to slowly wean pt off medication • Pt taking chronic low-dose prednisone with RA, will need co-treatment with bisphosphonate to prevent further adverse effects Corticosteroids • Patients starting chronic corticosteroid therapy will need monitoring of serum glucose • Educate patients to report black tarry stools and abdominal pain Chapter 52: Pain Management: Acute and Chronic Pain Overview of Pain Concepts Pain • Most common reason people seek medical attention (CDC and NIH) • Expect relief when seeking treatment • Brennan/Colleagues and Fishman (2007) o Pain management is a basic human right o BUT standard of care for pain management is not an absolute science or free of risk o (2011) Undertreatment for pain widely reported in the literature = Significant problem • Failure to treat pain is • Unethical • Poor clinical practice • Violation of human rights (Appropriate management) IOM- examining pain as a national health problem and transforming the understanding, prevention, assessment and treatment of pain International Association for the Study of Pain (IASP) • Pain is the unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage or both • PAIN IS SUBJECTIVE Suffering • Emotional reaction to pain and can be manifested by feelings of helplessness or hopelessness • Understanding these terms can help APN to assess pain symptoms, consider cause and develop the best pain management plan with specific presentations Acute vs Chronic Pain can be acute or chronic, generally classified by duration of symptoms and presence or absence of sympathetic nervous system activity Acute Associated with tissue injury and resolves when healing occurs. (Subcategorized: Physiological) Chronic Last more than 6 months- well beyond expected time of healing. (Subcategorized: Pathological) IASP Taxonomy (2012) Pain Terms Characteristic Allodynia pain from a stimulus that does not normally produce pain Analgesia absence of pain in response to stimulation that would normally be painful Causalgia a syndrome of sustained burning pain after a traumatic nerve lesion Dysesthesia an unpleasant abnormal sensation, whether spontaneous or evoked Hyperalgesia increased pain from a stimulus that normally provokes pain Hyperesthesia increased sensitivity to stimulation Hyperpathia a painful syndrome characterized by an abnormally painful reaction to a stimulus, especially a repetitive stimulus, as well as an increased threshold Hypoalgesia diminished pain response to a normally painful stimulus Hypoesthesia decreased sensitivity to stimulation Neuralgia pain in the distribution of a nerve or nerves Neuritis inflammation of a nerve or nerves Neuropathic pain pain caused by a lesion or disease of the somatosensory nervous system Neuropathy a disturbance of function or pathological change in a nerve: in one nerve, mononeuropathy; in several nerves, mononeuropathy multiplex; if diffuse and bilateral, polyneuropathy Nociception the neural process of encoding noxious stimuli Nociceptive pain pain that arises from actual or threatened damage to nonneural tissue and is due to the activation of nociceptors Nociceptor a high-threshold sensory receptor of the peripheral somatosensory nervous systems that is capable of transducing and encoding noxious stimuli Paresthesia an abnormal sensation, whether spontaneous or evoked Sensitization increased responsiveness of nociceptive neurons to their normal input and/or recruitment of a response to normally subthreshold inputs Table 52-1 (p. 1352) Types of Pain Acute Chronic Etiology Physiological Pathological Onset Sudden Gradual Localization Generally, well identified Less easy to differentiate Duration Self-limiting with healing Last beyond 6 months Character Varies, More overt signs Varies, fewer overt signs Temporal Pattern Varies, Correctable symptoms Varies, Persistent symptoms Associated Symptoms Physical and Psychological (Anxiety/Irritability) Physical and Psychological (Depression, Insomnia, Lethargy) Prognosis Complete relief in most cases Complete relief generally not achieved The Experience of Pain • Stimulation of nociceptive system – physiological mechanisms of pain can occur with disease process without specific injury present • At other times pain may not be related to physical process, indicating the influence of emotional and psychological factors that produce subjective reports of pain • “Whatever the experiencing patient says it is and exists whenever he says it does” -McCaffery (1972) o It is important that the patient statements are believed by the APN o Comprehensive assessment vital BUT also understand nature of the pain (Table 52-1) including pathophysiology, relevant comorbid conditions and the impact on activities and Quality of Life (QOL) • Melzack and Casey (1968): Model for pain levels o Sensory-Discriminative: Location, intensity and quality of pain o Motivation-Affective: Depression/Anxiety associated with pain o Cognitive-Evaluation: Patient’s thought about significance of pain Pain Threshold and Pain Tolerance • Threshold o Lowest point at which a nociceptive stimulus is perceived as pain Varies between patients and within the individual o Perceptual dominance- extreme pain in one location raises threshold in other areas o Pain as a threat to well-being may also influence pain threshold (Ex. Chest pain = MI = Death= Patient seeks treatment) • Tolerance o Amount of intensity or time a patient will endure before taking steps to relieve pain o Past experience with pain is a factor o May decrease over time o Influenced by anger, fear, lack of sleep and other cognitive factors o May increase with medications, recreational drugs, alcohol, distraction, application of heat/cold, herbs or alternative therapies (Acupuncture, hypnosis, cultural beliefs/expectations/religious activities) Special Populations • Pain assessment should include detailed history: characteristics, symptom treatment prior to visit, impact on function/well-being, sleep, medical/psychiatric conditions, and current medications • Complete physical conducted with focus on neurological and musculoskeletal systems – identify sensory and functional deficits • Review medical record – ascertain previous conditions, diagnostic test results which may contribute to current pain complaint • Thorough data collection helps to formulate a working diagnosis for the etiology of the pain and help plan the best treatment for underlying cause and symptoms related to cause • Undertreatment in the very young and the elderly and minority populations has been an issue for decades • Unable to adequately report pain- may be part of APN lack of attention to evaluate further • Multifactorial sources of pain MUST be assessed and understood to provide the best practices • A review of past medical records and diagnostic studies should be included in the pain assessment o It is also important to obtain a history of potential substance abuse, which typically begins by asking about past or current smoking and use of alcohol and progresses to specific questions about recreational and prescription drug use o Other data may include the patient's mood, coping strategies, and pain interference with activities of daily living o The practitioner should develop a working diagnosis for the pain etiology and a plan of care that may include additional diagnostic studies and treatments Pediatric Patients • Nervous system is sufficiently developed prior to birth • Inflammatory response is robust in infants and young children- can produce a greater neural response following noxious stimuli • BUT enzyme systems that metabolize drugs is immature in preterm and neonates • Pain producing events have an impact on young nervous system- can have lasting effect and lower threshold for months • Older children have higher pain thresholds • Response to pain is always INDIVIDUAL Assessment • Pain assessment in infants and children younger than 18 months can be a challenge due to their inability to verbally express their discomfort • Validated pain scales for preterm and term infants can be used to monitor behaviors • The Premature Infant Pain Profile • CRIES Postoperative Pain combine physiological measurements along with facial expressions to determine the degree of pain • The FLACC (Face, Legs, Activity, Cry and Consolability) Scale (is a behavioral scale that can be used in children 2 months to 7 years in age • A pain score is calculated after observing the child for 5 minutes • Children as young as 18 months may be able to indicate their discomfort • Children ages 3 to 4 years and older have acquired words they can use to report the pain location and describe its characteristics o They can generally use self-report pain scales Wong-Baker Faces Scale Oucher Scale Poker Chip Scale o School-age children may be able to use adult scales such as the Numeric Rating Scale or the Visual Analog Scale • Questionnaires have also been developed for children with chronic pain and include the Children's Comprehensive Pain Questionnaire and the Varni-Thompson Pediatric Pain Questionnaire Older Adults • 65yo+ have multiple causes of pain • May not be adequately identified, increasing risk for inadequate pain management • Aging = physiological changes, anatomical changes, and the underlying neurophysiological mechanisms of pain, coupled with comorbid conditions o Can lead to an increase in pain threshold o Arthritis is the most common persistent pain in people over 85 • Reluctant to report pain for many reasons, making assessment challenging especially if there is cognitive decline • APN may need to clarify words used by the elderly to describe discomfort, as they dismiss pain as part of the aging process, disease progression or fear additional costs and tests Assessment • Practitioners should take a thorough pain history and assess for pain as a routine part of the elderly patient's visit • The physical exam should focus on the musculoskeletal and neurological systems • Functional and range of motion testing should be included in the pain assessment • Cognitive ability is also an important part of the assessment process; look for new or worsening symptoms along with evaluation for depression or anxiety, which can accompany persistent pain • Using common visual analog or numeric rating scales are useful but geriatric pain assessment tools may better assist in the overall assessment of pain in the elderly • Patients with cognitive deficits may do better with the Faces Scale or other pictures • Pain has a significant impact on quality of life in the older adult and should not be overlooked Cognitive Impairment • Dementia and cognitive impairment common in the elderly but can occur at any age • Mental capacity may be reduced but that does not mean that physiological response to pain is reduced • Pain assessment is challenging when patient can’t communicate clearly (needs and symptoms) • Poor pain management can manifest as behaviors that mimic psychological disorders- leading to misdiagnosis and inappropriate treatment o Agitation, mood changes, withdrawal from activities, or other behavior disturbances can indicate pain/distress but is not recognized as a pain issue o Mini Mental Status Exam (Folstein, Folstein and McHugh-1975) has been used significantly o Pain assessment tools for dementia patients can be found at www.alz.org (Alzheimer’s) o Checklist for nonverbal pain indications- more recent specifically to measure pain in cognitively impaired patients o Pain Assessment in Advanced Dementia (PAINAD)- measures breathing vocalization, facial expressions, body language and consolability in non-verbal patients o Pictoral pain scales can be used in children and patient that can’t communicate Comorbid Chronic Illnesses • Older adults are more prone to having comorbid conditions (Arthritis, CVD, DM) requiring pharmacological therapies • NSAIDs o Mild to moderate pain from arthritis, has potential to interact with other commonly prescribed medications for this age group: antihypertensives, antidiabetic, etc o The risk of serous GI side effects and renal toxicity also contribute to complications o Aging process alters organ function- Important to absorption, distribution, metabolism and elimination o Patients should be screened carefully for GI disorders, hepatic and renal function, adrenal function and hypothyroidism o Contraindicated with those with a history of GI bleeds • Endocrine deficiencies o Prolonged and exaggerated response to opiates • Kidney dysfunction o Alters elimination – Dosing of analgesics is critical to avoid toxicity Pregnancy • General- pregnant women should avoid medications o Safe use of analgesics in pregnancy has not been well established Most analgesics are Pregnancy Category C or D • Carefully weigh benefits vs. fetal harm o Research has shown the following drugs demonstrate no fetal risk Category B Acetaminophen Naproxen Oxycodone Topical analgesics • Mother addicted to opiates = Newborn is subject to respiratory depression or excessive sedation along with withdrawal symptoms • FDA (2013) o Relabeled ALL extended-release and long-acting opioids – boxed warning that maternal use could cause neonatal opioid withdrawal symptoms Substance Abuse • Overuse of alcohol or prescription drugs in prevalent in society and an issue • APNs who treat both acute and chronic pain are likely to face the dilemma to select appropriate pain treatment for known or suspected substance abuser • Chronic overuse of addictive substances alters the brain's neurochemistry, neurotransmission, and interactions within the reward structures in the frontal cortex that control motivation, memory, impulse, and craving • Problems in the frontal cortex lead to altered judgment, impulsivity, and a dysfunctional need for gratification • Development of these brain structures are still in process into adolescence and young adulthood, an important factor to consider when assessing the history and possible early exposure to addictive substances • Genetics also plays a significant role in the likelihood of addiction • Cultural factors can influence how a patient develops behaviors in a desire to be socially accepted within a group • Addictive behaviors o Characterized as the inability to abstain from the drug of choice, impaired behavioral control, craving for drugs, inability to recognize significant problems with behaviors or relationships, or dysfunctional emotional responses (American Society of Addiction Medicine [ASAM]) • Pseudo-addiction o Described as addiction-like behaviors such as “clock-watching” that occur when pain is under- treated • A distinction can be made between addiction and pseudo-addiction when eliciting history and pain assessment data because patients with pseudo-addiction no longer exhibit these drug-related behaviors when pain is effectively treated (AMA) Prescribing and Substance Abuse • When considering prescribing potentially abusable drugs, the American Academy of Pain Medicine and the American Society of Addiction Medicine) recommend using the following definitions to determine the degree of substance abuse disorder o Addiction is a primary, chronic, neurobiological disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations It is characterized by behaviors that include one or more of the following • Impaired control over drug use • Compulsive use • Continued use despite harm • Craving o Physical dependence A state of adaptation that is manifested by a drug class-specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist o Tolerance A state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug's effects over time • Patients with addiction are often extremely anxious about insufficient receipt of pain medications in association with trauma, disease, or surgery, which may influence how they express their pain • Practitioners should assure these patients that acute pain will be adequately treated despite the addiction (AMA) • Those who are opioid-dependent may require higher doses to reduce acute pain due to higher tolerance • Decision making about choice of drug, dosing, and scheduling should be shared to provide the patient with a sense of control and satisfaction that pain relief will be achieved Acute Pain • Due to mechanical or thermal stimulation of nociceptive receptors in somatic or visceral tissues • Symptoms are of sudden onset and generally disappear when healing occurs • Pathophysiology o May be somatic, visceral, referred, neuropathic, or psychogenic in origin o A patient may experience single or multiple types of pain o The following are found in the skin, muscle, connective tissues, joints, and in some visceral tissues Afferent neurons A-delta fibers- myelinated and respond to thermal and mechanical sources; stimuli are fast-traveling and highly localized C-fibers- unmyelinated and are activated by multiple sources; stimuli are poorly localized, and impulses travel more slowly than through A-delta fibers • Types o Somatic Involves skin, joints, bone, muscle, or connective tissue and is generally localized and described as aching, throbbing, stabbing, squeezing, stinging, pinching, or sharp • Examples might be burns, arthritis, or metastatic bone pain Somatic pain responds well to NSAIDs, acetaminophen, corticosteroids, opiates, and topical applications of anesthetics, cold, or heat o Visceral Pain arises from hollow organs and is often described as dull, aching, and burning, gnawing, or cramping sensations Tissue damage to organs such as the heart produces complaints of sharp, stabbing, or throbbing pain and other descriptors similar to somatic pain The use of opiates, NSAIDs, and corticosteroids are useful for this type of pain o Referred Perceived at a more distant site; some patterns are clinically relevant • Examples might be pain referred to the right shoulder from inflammation of the gallbladder or pain in the groin due to ureteral colic o Neuropathic Pain is felt along dermatomes and can originate in central or peripheral nerves It is described as tingling, prickling, burning, or shock-like • Examples of this type of pain might be neuropathy due to herpes zoster or trigeminal neuralgia, or radiculopathy in an extremity from compression on a spinal nerve root More problematic - Pain that has no identifiable physiological etiology o Psychogenic pain Phenomenon - often seen in patients with psychiatric conditions or psychosocial disorders Can be a component of acute pain or caused by an array of reactive psychosocial disturbances Assessment is complex and the practitioner should evaluate both the pain component and the psychiatric problem The neurotransmitters norepinephrine and serotonin play a role in depression but also modulate sensitivity to pain in the efferent pathway For psychologically based pain, traditional analgesics are not indicated (Agency for Healthcare Research and Quality [AHRQ]) • Signs and Symptoms o Typically associated with stimulation of the nociceptors arising from tissue injury o Include both physiological responses in the sympathetic nervous system and behaviors used to express pain o Be alert to physiological responses, which include increased heart rate and blood pressure, increased respiratory rate, dilated pupils, diaphoresis, and pallor as blood flow to the skin decreases o Elevation of blood sugar can occur o Gastric motility and blood flow to the viscera decrease and can produce nausea and vomiting o Behavioral signs can range from stoicism and stillness to demonstrative expressions such as grimacing, moaning, crying, guarding, rocking, or pacing • Pain management is dependent on a detailed pain history and appropriate physical examination • Information about the onset, location, duration, characteristics, aggravating or relieving factors, and self-treatment is essential. Information regarding characteristics and intensity can be obtained through the use of pain scales o Numeric pain scale measures pain intensity on a 0 to 10 scale with 0 being no pain straight line with dichotomous endpoints o The Brief Pain Inventory (BPI) is multidimensional and includes four pain intensity scales and seven scales that measure the pain impact on activity, mood, relationships, sleep, and quality of life (Daut, Cleeland, & Flanery) o The McGill Pain Questionnaire (MPQ) is a tool that assesses three pain dimensions—sensory, affective, and evaluative—in sets of words the patient chooses that describe the pain, which, in turn, may suggest to the practitioner the underlying etiology (Melzack, ’75) Pharmacodynamics • The use of nonopioid and opioid analgesics is the primary intervention to reduce or alleviate pain • Anti-inflammatory drugs and opiates are the two primary classes used to treat acute pain Corticosteroids also have value in reducing inflammation • In addition to analgesics, nonpharmacological strategies may also be used such as physical therapy, massage therapy, complementary and alternative medicine (CAM), and biofeedback or other behavioral or psychological interventions • See Table 53-3 at end of the chapter summary Anti-Inflammatory Drugs • Pain is commonly caused by inflammation at the cellular level • Are often the first-line drugs to manage acute pain symptoms and are generally administered orally • This class of drugs interrupts the chemical mediators released from destruction of cell membranes at the site of injury • COX enzyme discussed earlier is the target of these drugs, which include salicylates, acetaminophen, and nonsteroidal anti-inflammatory (NSAID) agents o Although the exact mechanism of NSAIDs is not known, it is believed they inhibit the action of the COX enzyme and the production and synthesis of prostaglandins, thus reducing inflammation and pain o COX enzyme consists of three currently identified isoenzymes o COX-1 is continuously present (constitutive) in all body cells and tissues with concentration in the endothelium; in platelets to cause aggregation; in the stomach to regulate acid and mucous production; and in the microvasculature, glomerulus, and collecting ducts in the kidney to regulate water excretion o COX-2 is not normally present in tissues but rapidly increases in concentration when inflammation is present (inducible) o COX-3 has been more recently identified and is located only in the CNS within the blood–brain barrier The properties of COX-3, also inducible, are to mediate central analgesia and to provide antipyretic activity o Nonselective NSAIDs inhibit both COX-1 and COX-2 isoenzymes; the ratio varies by drug o COX-1 inhibition decreases the availability of gastroprotective prostaglandins, which is a primary factor in the development of adverse GI effects, particularly erosion and bleeding o Specific COX-2 inhibition is increased with celecoxib (Celebrex), currently the only drug on the market in this class, but which carries a Black-Box Warning of increased risk for cardiovascular events • NSAIDS, as a class, bind to plasma proteins tightly, and interactions with other drugs commonly occur when they compete for binding sites o For example, platelet action is blocked by aspirin and other NSAIDs, which may have an effect on low-dose aspirin use associated with cardiovascular disease o The decision to initiate NSAID therapy must include consideration of the risk/benefit • Opioids act both central and peripheral pain receptors, most notably the μ (mu)and κ (kappa) receptors, to inhibit the transmission and perception of pain impulses o Opioids are further classified according to their binding action at opioid receptor sites o Full agonists are the most widely prescribed and include morphine, codeine, hydrocodone, oxycodone, fentanyl, hydromorphone, methadone, and meperidine o Partial agonists (e.g., buprenorphine) have decreased activity at the μ sites, and mixed agonist- antagonists (e.g., butorphanol, nalbuphine) have action that can either bind or block opiates at receptor sites Most have an analgesic ceiling that relates to opioid-related side effects o Opioids have a high abuse potential and can cause withdrawal symptoms, especially in patients who are physically dependent on agonist opioids o Agonist drugs can be further classified into categories based on duration of action Short-acting opioids (4 to 6 hours) • Like morphine, require more frequent dosing to maintain a therapeutic effect Long-acting opioids (8 hours or more) • Have long half-lives and release the drug more slowly o Examples include extended-release preparations of oxycodone, oxymorphone, morphine, and fentanyl and long-acting agents like methadone; these drugs may be preferred when managing chronic pain o Adverse effects at the μ sites include euphoria, which is an incentive for abuse and contributes to dependence, as well as undesired effects of respiratory depression, constipation, and urinary retention o Tramadol is non-narcotic but acts on μ receptors to produce centrally acting analgesia This drug also inhibits the reuptake of serotonin and norepinephrine, which provides dual-action pain relief. Sedation is produced at the κ sites without the other side effects o Naloxone is an antagonist for both μ and κ receptors and is the agent of choice for reversing the effects of opioids • Goals of Treatment o For acute pain is complete relief. In some cases, this may not be possible, so reduction may be a more realistic outcome o In either case, pain management with the least amount of adverse effects is desirable • Addiction and Dependency o Opiates carry a high risk for tolerance, dependence, and abuse but are still appropriate to use for pain management with monitoring Red flags for addiction or dependency (7 total) Concurrent use of alcohol or illicit drugs used for recreation Frequent need for dose escalations Multiple episodes of prescription loss Seeking prescriptions from multiple providers Prescription forgery Selling prescription drugs or buying from unauthorized sources Resisting change in therapy from pills to other modalities Screening • Screening for substance abuse risk can be done with the use of questionnaires • Two popular tools are the CAGE-AID and the Drug Abuse Screening Test (DAST) o CAGE-AID (Brown & Rounds, 1995) Has the patient ever: • Felt you ought to cut down on your drinking or drug use? • Had people annoyed you by criticizing your drinking or drug use? • Felt bad or guilty about the consequences of your drinking or drug use? • Had a drink or used drugs first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)? Scoring for item responses are “0” for no and 1 for “yes.” While the normal cutoff for this tool is two positive answers, it is recommended that primary care practitioners lower the threshold to one positive answer to identify more patients who may have a substance abuse disorder o The DAST questionnaire (Gavin, Ross, & Skinner, 1989) has been found useful in screening for drugs of abuse other than alcohol. See page 1362. There are 28 questions Pain Contract • When substance abuse is suspected or detected, a pain contract may be appropriate • Opioids have been implicated in accidental death or even suicide due to overdose, particularly in combination with alcohol or other drugs • Setting clear expectations and responsibilities is critical to achieve mutually set treatment goals Rational Drug Selection • Drug selection should be based on overall severity of pain, SE profile, and suspected source of pain • Non-opioids o Provide effective relief for many types of acute pain and inflammation o Salicylates, acetaminophen, and NSAIDs are useful for somatic, dental, arthritic, traumatic, and post-operative pain of mild to moderate intensity o Differ from opioids in that they inhibit prostaglandin formation, have antipyretic properties, and are not associated with dependence or addiction o Regular use of nonopioids carries risks for bleeding and has potential for interaction with other drugs that may be taken on a regular basis See Figure 52-4 Acute Pain Algorithm page 1363 o Long term study of NSAID use long-term (1 year) Findings included a significant increase in major vascular and coronary events, including death, occurring with long-term use of high dose coxibs and diclofenac (Voltaren); ibuprofen significantly increased coronary events but not vascular; and naproxen showed no increased risk for vascular or coronary events The risk of heart failure was nearly doubled with all NSAIDs, and all NSAIDs increased GI complications APN needs to keep this in mind when choosing to prescribe NSAIDs. Coxibs and diclofenac should be avoided in patients with known heart disease and cautiously in patients with high risk for coronary or vascular events • Opioids o Short-term use and should be reserved for moderate to severe acute pain that is not well controlled with nonopioid analgesics o Carries risk for potential tolerance or abuse, and pain management should be monitored as to drug effect and pain reduction o The best choices for moderate pain are codeine, oxycodone, and hydrocodone, usually in combination with acetaminophen or aspirin o Better for severe pain Morphine, oxycodone, hydromorphone, oxymorphone, or fentanyl • Hydromorphone in high doses is more potent than morphine and could be considered in special cases • Meperidine is no longer a favorable drug to use for pain management due to its degradation to neurotoxic metabolites and association with tremors, delirium, and seizures. (Renal Clearance) Neuropathic pain • Effectively treated with anticonvulsants such as gabapentin and pregabalin, which are analgesic adjuncts that bind to calcium channels in CNS tissue and stabilize neuronal membranes, thus interfering with the transmission of pain impulses rather than binding to opioid receptors • No single approach for the use of drugs to manage pain o Treatment requires skillful application of multimodal therapies to include pharmacological and nonpharmacological interventions • Pharmacotherapy is a mainstay in the treatment of acute pain, other strategies such as psychological, rehabilitative, injections and/or blockades, behavioral therapies, or complementary medicine can be used alone or in combination with analgesic • Consider the simplest approaches but recognize that other forms of treatment may also be valuable. o In all cases, consider the patient variables • Monitoring o Self-reporting most effective way of monitoring pain management o Use of pain rating scales or other assessment tools when monitoring trends in pain intensity or patterns o Acute pain - the intensity should diminish as healing occurs If pain intensity is not abating, reevaluation of the drug or dose should occur, and a new plan of care developed • Outcome Evaluation o The acute pain treatment algorithm can be used as a guideline to develop and monitor the pain management plan and responses to treatment o Patients who have relief of symptoms and are pain free, no further treatment is indicated o Patient that remain symptomatic, further changes in the treatment plan can be made based on a reassessment of the patient's needs o A specific drug could be continued, the dose changed, or a different combination of nonopioid and opioid drugs could be used Nonpharmacological therapies could also be tried Questions to consider at this phase of treatment could be: • What pain relief measures are currently being used? • Should additional or different measures be tried? • When is the pain medication being used? • Is it timely? • Is the individual waiting until the pain becomes severe before taking the medication? o Fixed intervals have been shown to be more effective in controlling pain than “as-needed” dosing • Does the individual believe the treatment plan is effective? o There tends to be a placebo effect for pain treatment and if a patient believes a drug will be effective, it likely will be; and if he or she believes a drug will not be effective, the expected outcome will likely not occur o Response to initial or readjusted therapy is not successful, or if complications related to the pain source arise, the individual may need consultation with a specialist o If the complications are related to the pain medication, referral to a pain specialist may be prudent, especially in the case of dependency or addiction, even if pain relief is accomplished • Patient Education (Acute Pain) o APN should provide education about the drug, its side effects, dosing regimen, and the expected length of time the drug should be taken. The patient should also be informed about follow-up visits, particularly if complications occur. SEE ACUTE PAIN PATIENT EDUCATION BOX (p 1364) Chronic Pain • The IOM (2011) stated that nearly 120 MILLION people in the US suffer from chronic pain. Profound effect on ability to function, QOL- Higher utilization of healthcare, loss of productivity and societal costs • Two categories for chronic pain o Nonmalignant and malignant pain o Less well defined in terms of its onset and duration o Usually lasts longer than 3-6 months • Pain can also be classified as chronic if it meets criteria of lasting a month beyond the usual course of an illness or injury, is associated with chronic pathological conditions, or if it is recurrent over weeks or months • Recurrent pain can be a hallmark of certain disorders o Headaches o Inflammatory arthritis o Dysmenorrhea o Inflammatory bowel disease o Musculoskeletal disorders o Sickle cell disease • Recurrent acute pain can also occur in patients with cancer or AIDS related to the disease processes, treatments, or both • Acute episodes occur in the presence of otherwise controlled underlying pain, it is known as breakthrough pain • Pathophysiology o The AMA- key concept when pain is persistent, it should be conceptualized as its own illness o Pain that is present most of the time can be due to a variety of pain syndromes The underlying cause is not always identifiable o Chronic pain is not generally associated with sympathetic activity seen in the presence of acute pain o Body is accustomed to the pain and the nervous system has been desensitized to noxious stimuli o Changes occur over time in nerve terminals, dorsal root ganglion, afferent fibers, and the CNS, thus increasing stimulation of C-fibers and decreasing the production of endorphins o Persistent pain causes physiological adaptation over time so that blood pressure along with heart and respiratory rates remain normal o Responses to chronic pain vary and have fewer overt signs but tend to be more psychological than physical o The origins of persistent, nonmalignant pain are often multifactorial o The etiology of chronic pain is described as nociceptive, neurogenic, or psychogenic o Chronic pain is difficult to assess in that there are often no overt signs of tissue injury, nerve damage, or inflammation Nociceptive • Tissue damage or inflammation to somatic or visceral tissues • In the case of chronic pain, the damage may be ongoing and insidious • Ongoing tissue injury or inflammation leads to neurochemical and neurophysiological changes that affect the nervous system, leading to persistent input along afferent neurons from a specific source as discussed earlier Neurogenic • Underlying cause of neurogenic pain is damage to neural tissues in the central nervous system, the peripheral nervous system, or both • Characteristics are varied but are usually expressed as burning, tingling, or electric shock sensations • Neuropathic pain syndromes can also be accompanied by allodynia, hyperalgesia, hyper-pathia, or referred pain • Neuralgia occurs as a result of injury to a peripheral nerve from infection or disease o Classic examples are postherpetic neuralgia and diabetic neuropathy • Tinel's sign, a pain or tingling response to tapping over a nerve, is often positive o Over time, atypical cross-connections are developed between somatic and efferent nerves and nociceptors, which alter transmission of pain impulses o Nerve sprouts may also occur in the dorsal horn of the spinal cord following a peripheral injury o These changes also occur at sites of demyelination o Reports of pain may or may not be out of proportion to overt signs of injury o If peripheral injury is most likely, interventions such as release of entrapped nerves, anesthetic injection, or resection of a neuroma should be considered o In the case of a CNS injury, as seen with spinal cord trauma, there is little information about the processes that cause central pain syndromes Psychogenic • Generally used when there seems to be no physiological evidence of the source of pain, and the pain becomes predominantly unremitting due to psychological factors • Complex relationship between pain perception and psychological factors • Persistent pain can induce changes in mood, coping abilities, or behavior changes • Some patients develop these in the presence of chronic pain while others have underlying comorbid psychiatric disturbances that become exaggerated when pain is unrelieved • All patients who present with suspected psychogenic pain may be inappropriately labeled and stigmatized, so it is imperative to conduct both physical and psychological assessments before making a judgment • Pharmacodynamics o NSAIDs and opioids are commonly prescribed for patients with chronic pain o The addition of a psychological factor associated with chronic pain, patients who exhibit signs of depression or anxiety may require medications such as SNRIs or TCAs to manage those symptoms o Patients with neurogenic pain may benefit from the use of anticonvulsants o The transmission of pain impulses is inhibited by the presence of norepinephrine in the rostral pons and serotonin in the PAG These neurotransmitters also play a role in mood stabilization Decreased levels of norepinephrine and serotonin are common in depression SNRIs inhibit the reuptake of serotonin and norepinephrine into nerve terminals thus making more of the transmitter available at the synapses Originally developed to treat depression, TCAs are now more commonly used to treat neuropathic pain syndromes and insomnia, which can accompany chronic pain Full analgesic effect may take several weeks or months TCAs also block the reuptake of norepinephrine and serotonin but have a more significant side-effect profile due to their additional blockage of histaminergic, dopaminergic, adrenergic, and muscarinic receptors Of particular note is the risk for dysrhythmias and suicidal thoughts • Goals of Treatment o Ultimate goal is elimination of all pain, however, chronic pain this is less likely to occur, and a more realistic goal might be to reduce the pain to a tolerable level to maximize function and quality of life o Desired meet treatment goals with minimum side effects o A comprehensive approach is needed, and multimodal forms of pain relief should be incorporated into the plan of care o Mutual decision making between the patient and practitioner should be employed when choosing the drug, dosing, pain relief goals, and follow-up o Spiritual and cultural factors should be incorporated into the plan to make pain management patient centered • 2010: Pawar and Garten o Children should have chronic pain managed in the same manner as adults o Treatment is aimed at the underlying cause and associated symptoms o Oral medication is preferred and on a scheduled rather than a prn basis o Consider the neurodevelopmental age of the child as well as to know how to assess pain in different age groups so that the most effective treatment plan can be implemented o A young infant may have a central respiratory problem, so opioid use should be minimized o A toddler or older child may require less medication and use play or other distraction methods to cope with pain o No analgesia should be withheld from a child due to practitioner bias or insufficient assessment • Rational Drug Selection o Treatment is not solely based on the use of drugs o Multimodal interventions are available to attain the treatment goal of reducing chronic pain while maintaining maximum function. See Figure 52-5, pg. 1367. • Lifestyle Modification o Essential for chronic pain o Weight loss can be helpful in those who are overweight o Small, incremental weight losses can be of benefit to reduce stress on muscles and joints o Physical activity can help with weight loss as well as maintenance of mobility, and positive effect on mood and sleep o A progressive plan (not all or nothing) to improve flexibility, strength, balance, and endurance o Walking and resistance training are low-impact exercises that are suitable for patients with chronic pain Increase based on the patient's tolerance and allows the patient to have an active role in the treatment plan. o Rehabilitative methods can improve physical functioning Physical therapy, occupational therapy, ice, heat, massage, and aquatic therapy are useful for many types of pain but particularly for fibromyalgia • Cognitive-Behavioral Interventions o The Institute for Clinical Systems Improvement recommend several strategies for managing chronic pain. (2011) No specialist needed Specialist needed Relaxation techniques Biofeedback Meditation Hypnosis Imagery Guided imagery Diaphragmatic breathing Counseling Muscle relaxation exercises • Family members and the APN can be powerful reinforcers of wellness behaviors that are beneficial to overall well-being o Regular progress visits rather than when pain is unmanageable/out of control Drug Therapy • 1986 – WHO o Conceptual analgesic ladder to help guide the management of pain. (Originally for cancer pain- now widely used) o Used to achieve best outcomes based on pain severity • Step One: Nonopioids + adjuvants such as antidepressants or antiepileptics that do not have primary indications for pain management • Step Two: Adding an opioid for mild to moderate pain • Step Three: Adding a stronger opioid for moderate to severe pain Anti-Inflammatories • First-line drugs of choice in Step One of the analgesic ladder, but all carry risk of serious adverse effects, especially in the elderly who are more likely to have comorbid conditions • The patient's risk for cardiovascular disease, GI bleeding, and renal dysfunction should be assessed before recommending this class of drugs • All patients should be cautioned to read labels for common OTC remedies also containing acetaminophen to avoid accidental overdosing Drugs Cautions/SE NSAIDs in general Renal Insufficiency (Esp. diabetics) Piroxicam and Indomethacin CNS issues (older adults) GI bleed Drug-induced hepatitis Use Naproxen over Diclofenac when risk of CVD is high Celecoxib BLACK box warning for CVD Ketorolac SHORT TERM ONLY (5 days) Acetaminophen Better for older adults but monitor in long-term use. (Liver Function) Adjuvant Analgesics • Adjuvant drugs are used for treating conditions other than pain • In combination with analgesics, have a synergistic effect to reduce multiple types of pain • Corticosteroids such as prednisone and dexamethasone can be helpful in relieving the discomfort of inflammation but are generally used short-term for this purpose o Chronic use can cause adrenal suppression, GI bleeding, or thromboembolism • Depression or anxiety can be managed with SNRIs or TCAs along with pain modulation o Of the SNRIs, duloxetine (Cymbalta) 30 mg daily (titrated to 60 mg daily) can be useful for diabetic peripheral neuropathy with results in approximately 1 week; venlaxafine (Effexor) has also shown to be effective at doses of 150 to 225 mg daily o TCAs are effective for several types of neuropathic pain but can take up to 6 weeks for full analgesic effect Avoid amitriptyline in older adults due to its anticholinergic effects TCAs are contraindicated in patients with heart disease because sudden death can occur A baseline ECG for patients over the age of 40 should be obtained prior to treatment with any TCA Tramadol (Ultram) is a nonopioid analgesic that binds to the μ receptor and has weak opioid and serotonin-norepinephrine reuptake inhibitor (SNRI) activity • Because of its opioid-like activity, tramadol should not be used in patients recovering from narcotic addiction • Dosing of tramadol is usually 50 to 100 mg every 4 to 6 hours and should not exceed 400 mg/d; the maximum dose in patients older than 75 years is 300 mg/d • Seizures and serotonin syndrome are adverse effects • Safety has not been established in children • Cyclobenzaprine or other skeletal muscle relaxants are useful for fibromyalgia o Muscle relaxants are also helpful in the short-term management of acute exacerbations of muscle spasms associated with chronic low back pain o They are not helpful for long-term use due to their sedating properties • Topical applications of anesthetics or capsaicin can be useful for neuropathic pain at peripheral sites without significant systemic effects • Other drug classes for neuropathic pain o Anticonvulsants; gabapentin (Neurontin) and pregabalin (Lyrica) are recommended for diabetic neuropathy, post-herpetic neuralgia, and fibromyalgia Gabapentin is more efficacious than TCAs in treating postherpetic neuralgia • Initially dosed at 300 mg 3 times a day and titrated to 900 to 1,800 mg 3 times a day; it is a suitable drug for children over the age of 3 at initial doses of 10 to 15 mg/kg 3 times a day and titrated based on age and weight Pregabalin also has anxiolytic effects, which are helpful for mood stabilization in patients with neuropathic pain • The starting dose of pregabalin for the pain of diabetic neuropathy is 50 mg 3 times a day, then titrated over the next 7 days to 100 mg 3 times a day • The dose for fibromyalgia is 75 mg twice a day initially, then may be increased over the next 7 days to 150 mg twice a day • Patients may also wish to use complementary or alternative therapies for chronic pain relief o Herbal preparations are not regulated, nor do they undergo the rigorous testing done on pharmaceuticals; however, they may play a role in treating chronic pain conditions o Internet consumers can find multiple Web sites that list “natural pain killers” such as turmeric (fibromyalgia), feverfew (rheumatoid arthritis), eucommia (connective tissue disorders), kava kava (arthritis and neuropathic pain), capsaicin (neurogenic pain), or Devil's claw (muscle and low back pain), to name a few • Practitioners should educate themselves about herbs and the possible interactions between herbs and pharmaceuticals o For instance, turmeric interacts with anticoagulants, antidiabetic agents, antihypertensives, and hepatotoxic agents, which would increase the risk of bleeding, hypoglycemia, higher blood pressure, and liver damage; feverfew interacts with antiplatelets and antidepressants, which would increase the risk of bleeding and may worsen depression Opioids • Step Two of the analgesic ladder when pain is persistent or not well controlled with nonopioids for mild to moderate pain • Step Three opioids are used for moderate to severe pain • Opioids can be administered by a variety of routes and have a wide range of drug duration • An initial trial should be made and if the drug of first choice is not effective, a trial of a different opioid or route is warranted o Episodic or breakthrough pain episodes, short-acting opioids (4 to 6 hr) are appropriate and can be taken as needed Examples are codeine, hydrocodone, or oxycodone o Persistent and unrelenting pain, long-acting opioids (8 to 12 hr or more) provide a steadier state of analgesia and should be taken on a regular schedule Examples are OxyContin or MS Contin, which can provide relief for up to 12 hours o More recent preparations of morphine (Kadian and Avinza) and hydromorphone (Palladone) can last 12 to 24 hours The fentanyl transdermal patch can provide relief for up to 72 hours • Start with lower doses of opioids and gradually titrate to the desired effect • Convert from a short-acting agent to a long-acting opioid- transition should be done cautiously, especially in opioidnaïve patients and the elderly o Methadone should be used with extreme caution because of its unpredictable pharmacokinetics and accumulation from repeated doses o Treatment is best provided by a pain management expert • Patients should be weaned from opioid therapy for the following reasons o There is little clinical benefit despite multiple dosing adjustments and opioid rotation o The patient has poor tolerance to the opioid at doses required for analgesia o There are ongoing adherence issues (e.g., drug-seeking behaviors or diversion) despite the use of a pain contract or other treatment limits set with the patient o The patient has a comorbid condition that makes opioid therapy more harmful than helpful • Downward tapering of drug doses should be done over time by decreasing the opioid dose by 10% of the original dose each week over several weeks o Abrupt cessation or rapid tapering can precipitate seizures or withdrawal symptoms o Switching from a long-acting opioid to a short-acting one may also be helpful because some patients may do better with lower potency drug • To decrease the possibility of nonadherence to the treatment plan, limit the opioid supply to 7 days at the new dose during tapering o Monitor the patient during the withdrawal period for signs of abstinence syndrome, such as nausea, diarrhea, muscle pain, and myoclonus These symptoms can be managed with clonidine (Catapres) 0.1 to 0.2 mg every 6 hours or a clonidine patch 0.1 mg over 24 hours weekly during the transition period (Washington State Agency Medical Directors’ Group, 2007) Mild withdrawal symptoms may last up to 6 months after opioids have been discontinued; although the symptoms may be unpleasant, they are not serious The patient should be monitored for behavioral changes during the tapering process and appropriate management strategies utilized Schedule II • Controlled substance prescriptions are written for a 30-day supply (subject to state laws and insurance carriers) without refills, which would ordinarily require an office visit for renewal • Drug Enforcement Administration (DEA) revised its regulations to allow multiple prescriptions for Schedule II drugs in some cases, authorizing a total of a 90-day supply under the following conditions: o Practice of writing multiple prescriptions is permissible under applicable state laws o APN indicates on each prescription the earliest date the prescription can be filled o APN concludes there is no risk of aberrant behavior or drug abuse • Schedule III and IV controlled substances may be refilled if authorized on the prescription o These prescriptions may only be refilled up to 5 times within 6 months of the original issue date; after that time a new prescription is required o In 2014 the DEA rescheduled Hydrocodone to a Class II drug related to the misuse. Medication is the most prescribed Monitoring • Periodic assessment should be made of patients treated for chronic pain • Progress toward goal attainment should include documentation of pain intensity, functional ability, and quality of life • APN should observe mood, affect, and coping abilities along with a physical examination • If the patient's status is stable, these assessments can be brief; if worsening conditions or complications are encountered, a more in-depth assessment is necessary • Always assess for changing conditions and the risk of aberrant behavior • Patients with a high risk of peculiar drug use, such as patients who are only interested in obtaining oral pills or who “run out” of medication before the 30-day period, other strategies should be utilized o Urine drug screens or frequent follow-up visits with pill counts could be initiated o Pain contract that clearly identifies goals, expectations, and responsibilities of both patient and practitioner may be useful for patients who have a history of substance abuse or fall in the high- risk category o Co-management with or referral to an addiction specialist could also be arranged Outcome Evaluation • Goals of treatment should be negotiated when therapy begins, and a baseline of acceptable pain level should be established. Quality of life is also a mainstay of therapy • The outcome may not be total pain relief but should aim to restore as much function as possible • Since psychological effects of chronic pain are prevalent, assessing mood and coping skills is also important • It is difficult to use physiological measures but other indicators such as sleep, appetite, amount of physical activity, participation in work or hobbies, and social relationships can give insight into the success or failure of the treatment plan Patient Education • Individual should be educated about the specific choice of drug or combination drug therapy to address chronic pain, dosing regimens, and realistic goals about pain management • Complete relief may be an unrealistic expectation, yet there are not only drugs but also adjunct and alternative therapies that can be helpful in reducing the pain to an acceptable level • Common side effects with long-term use of an opioid should be explained along with adverse effects • Differences between drug dependence, tolerance, and addiction should be reviewed because many patients are fearful that addiction will occur • The practitioner should assure the individual's report of pain is believed and that there are multiple modalities that can address the pain as well as the accompanying symptoms • Establishing a therapeutic partnership for the control of chronic persistent and recurrent pain is key See Chronic Pain Management Patient Education (Page 1370) [Show More]
Last updated: 1 year ago
Preview 1 out of 77 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 12, 2022
Number of pages
77
Written in
Additional information
This document has been written for:
Uploaded
Mar 12, 2022
Downloads
0
Views
44



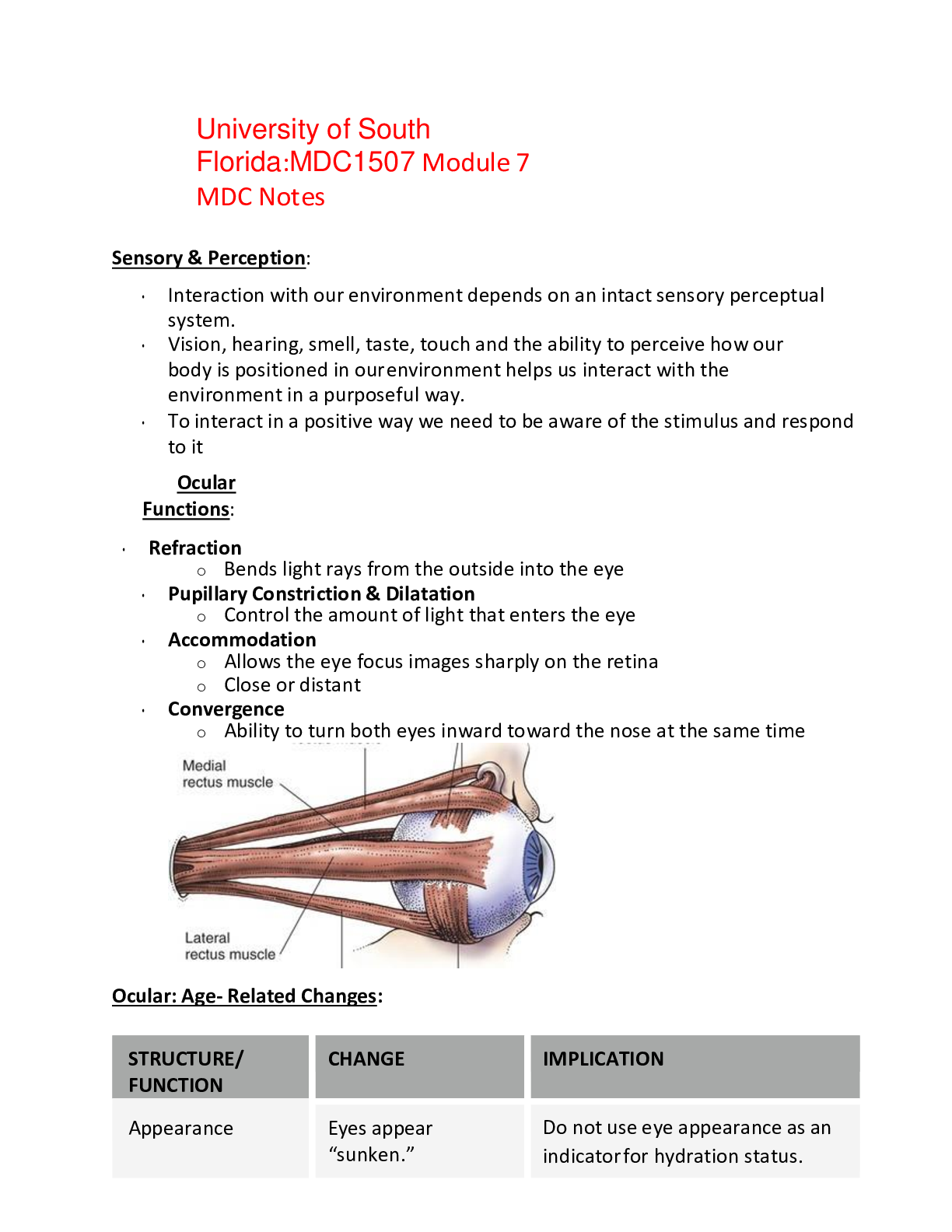
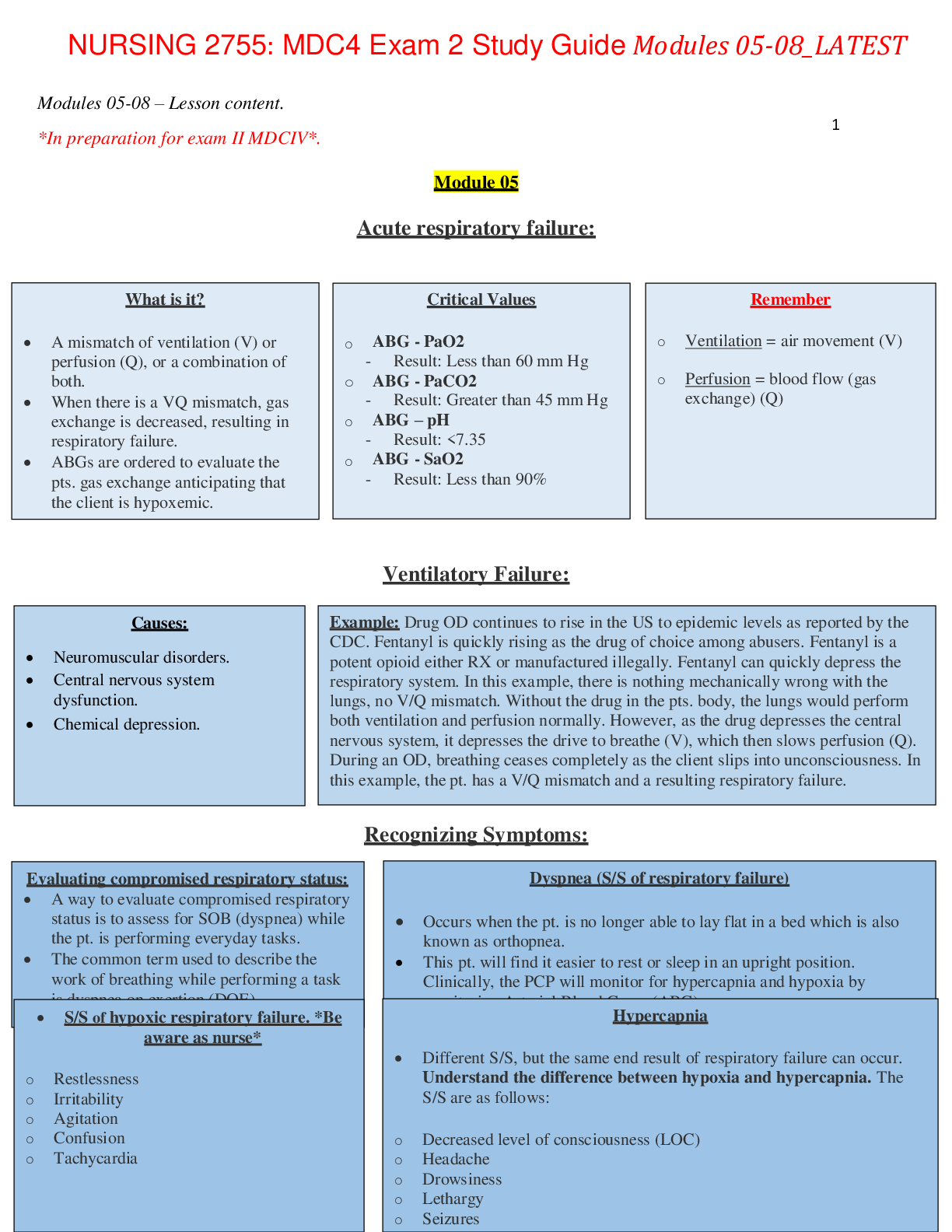


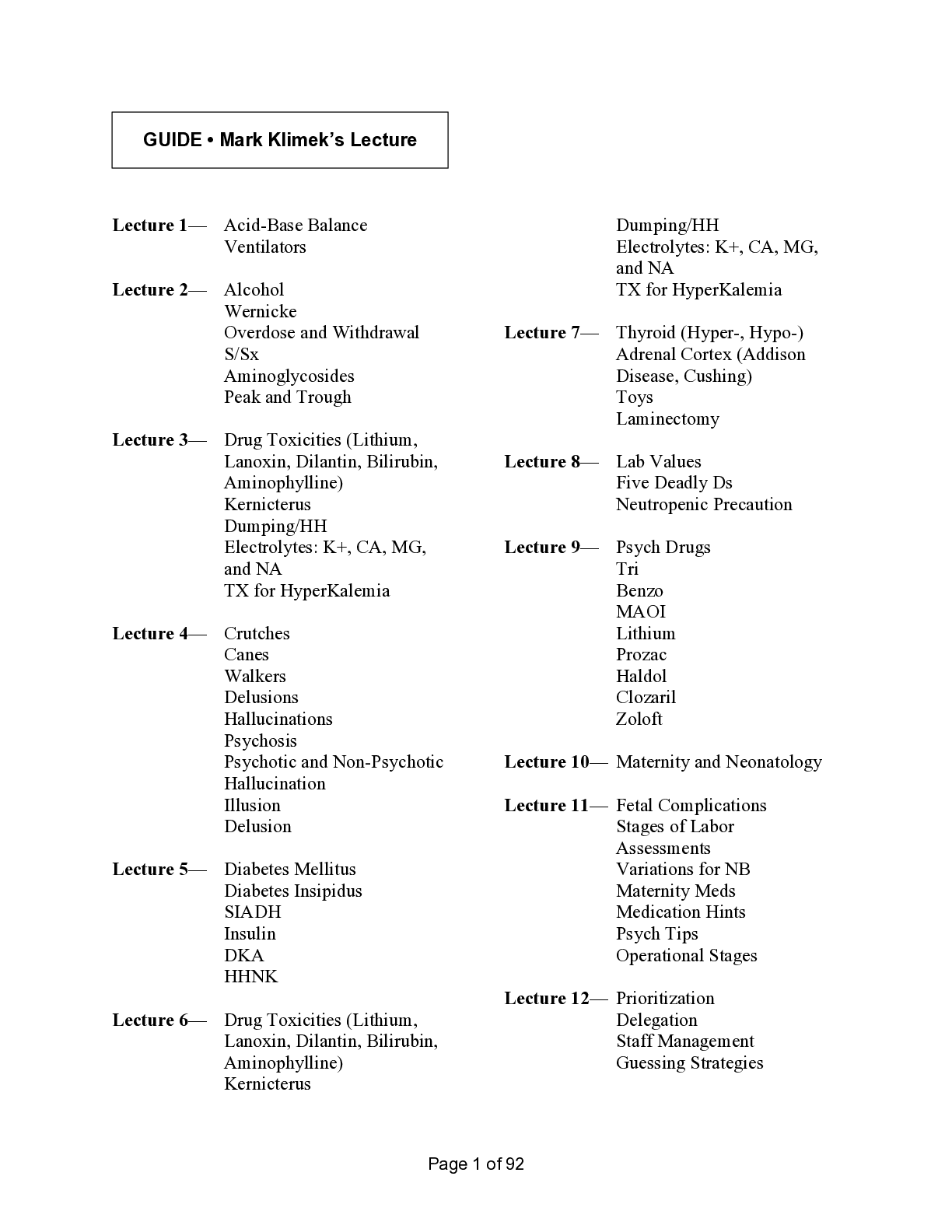
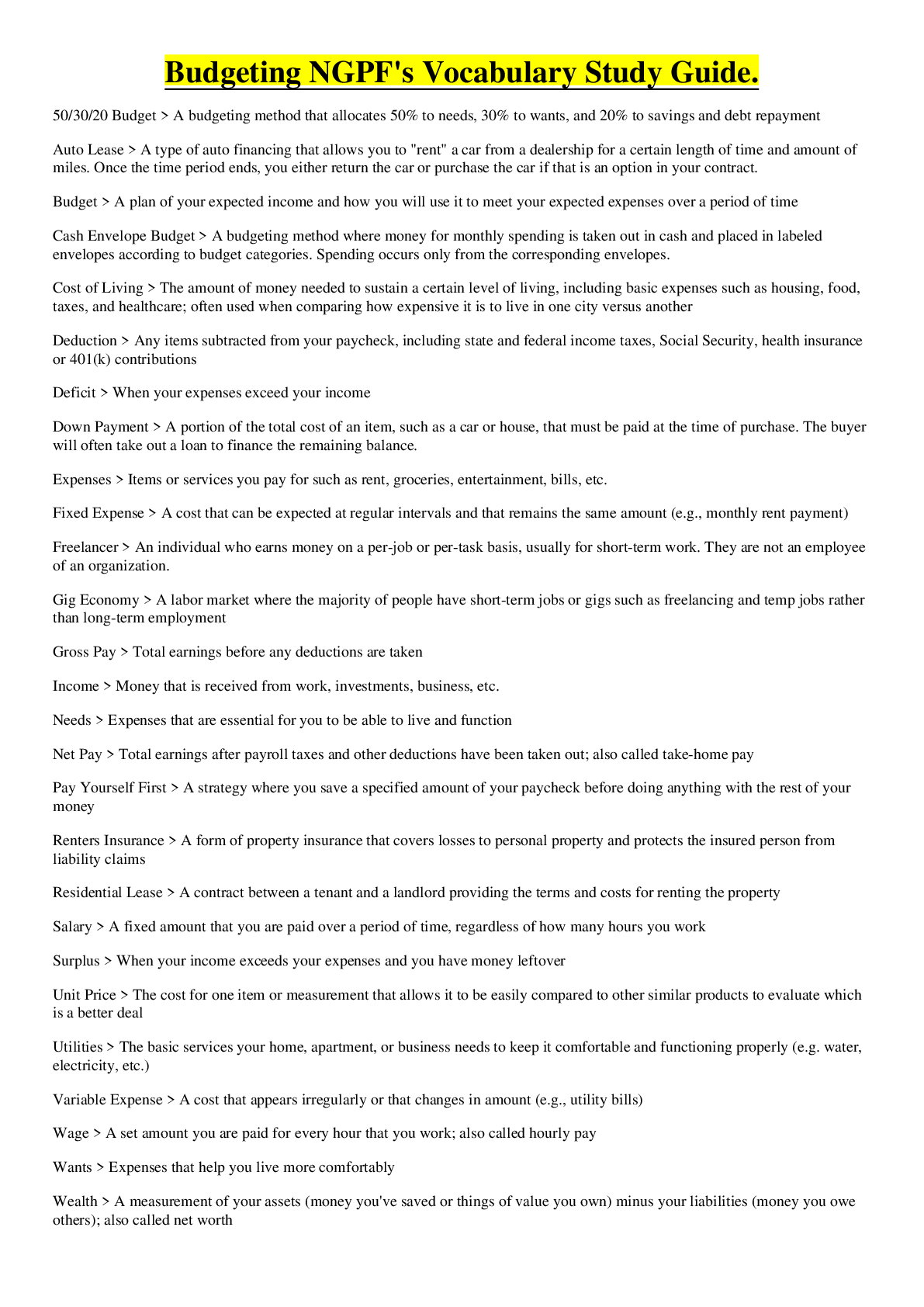

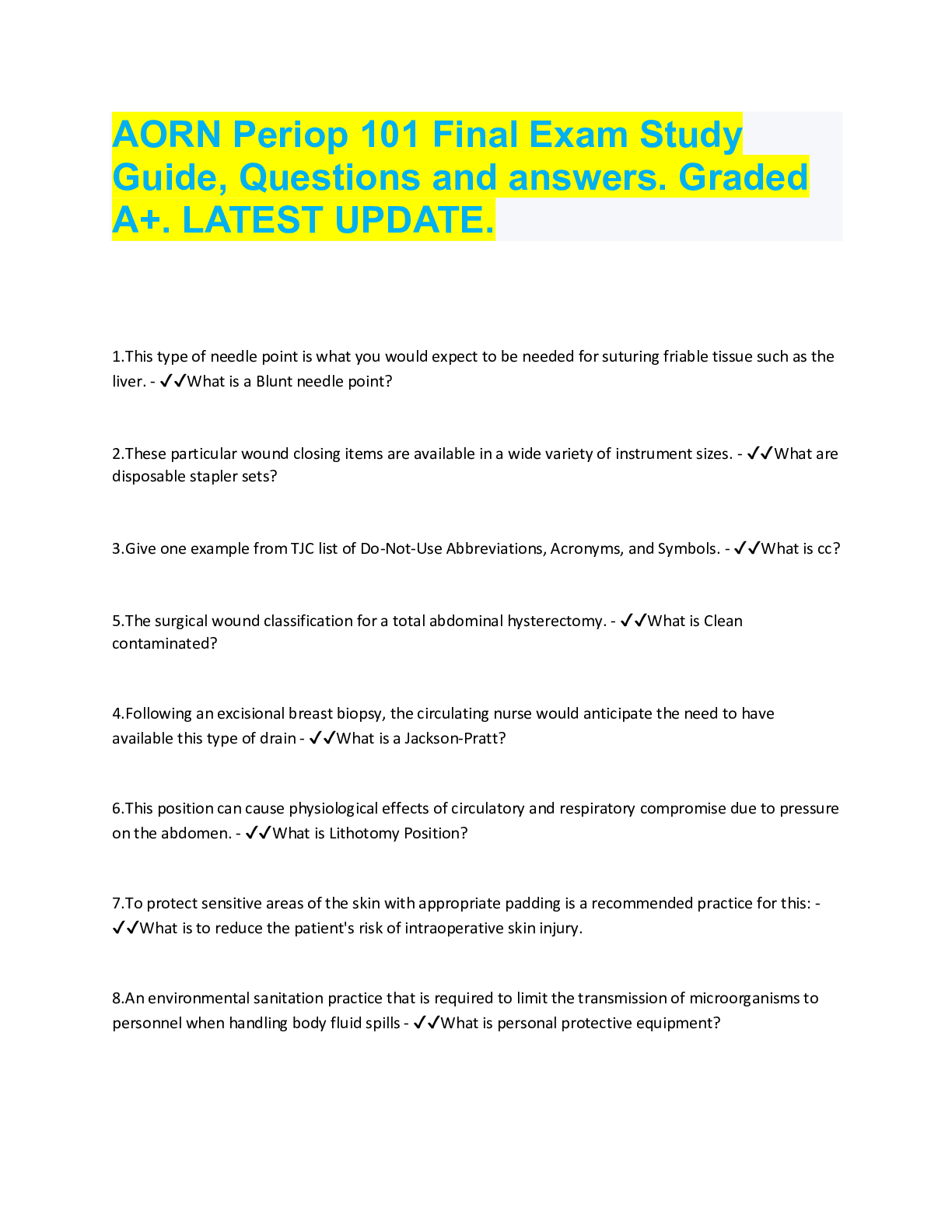
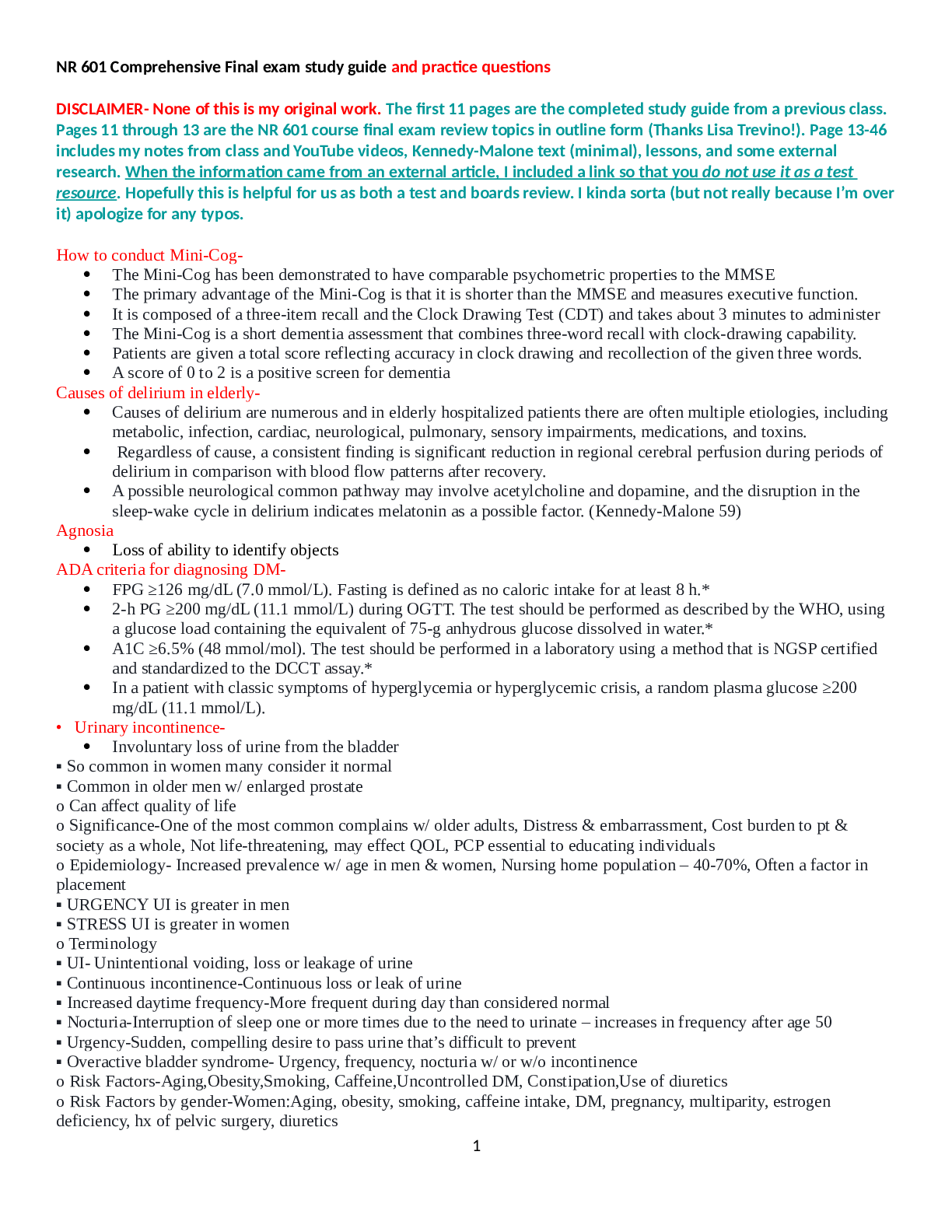



.png)