*NURSING > STUDY GUIDE > NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rate (All)
NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rated | Latest | Chamberlain College
Document Content and Description Below
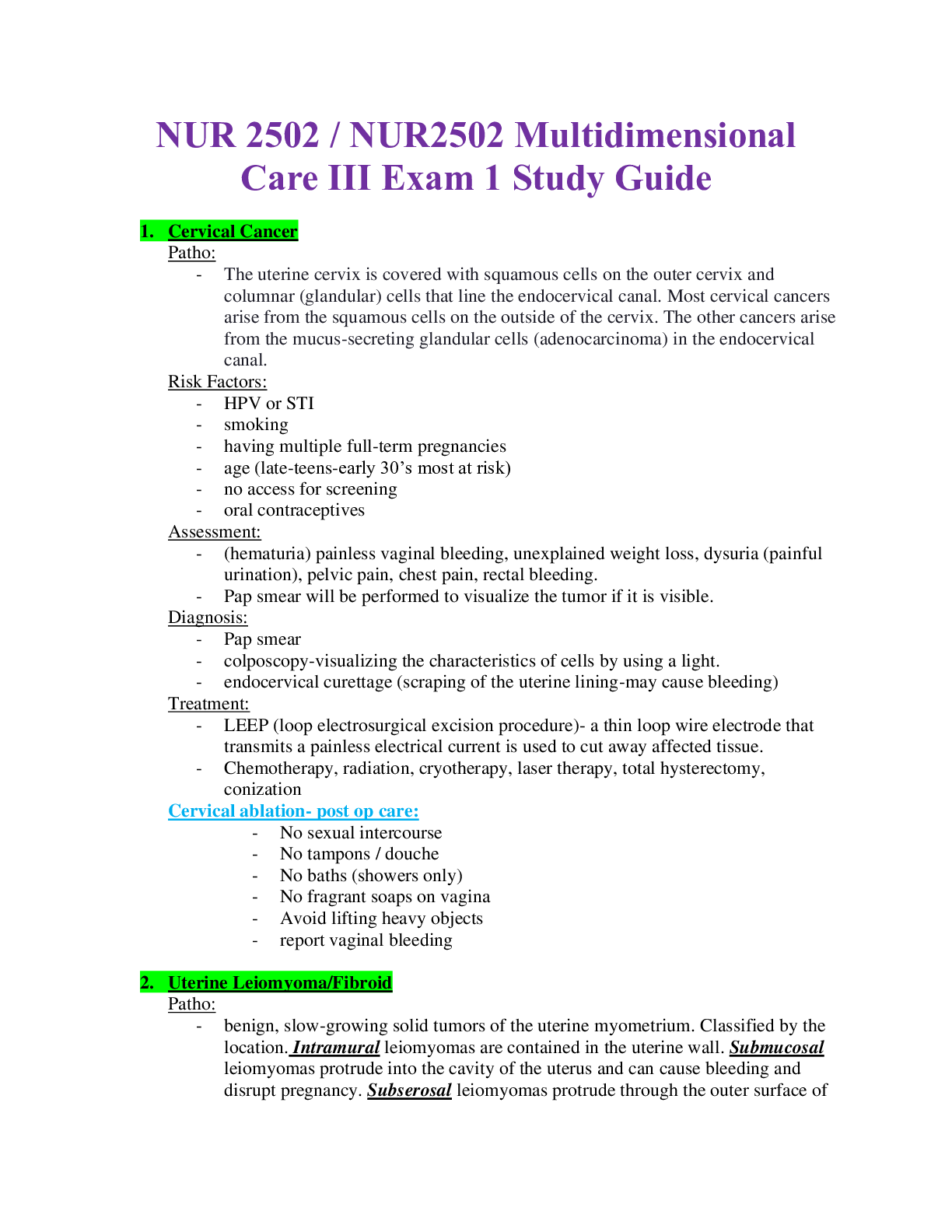
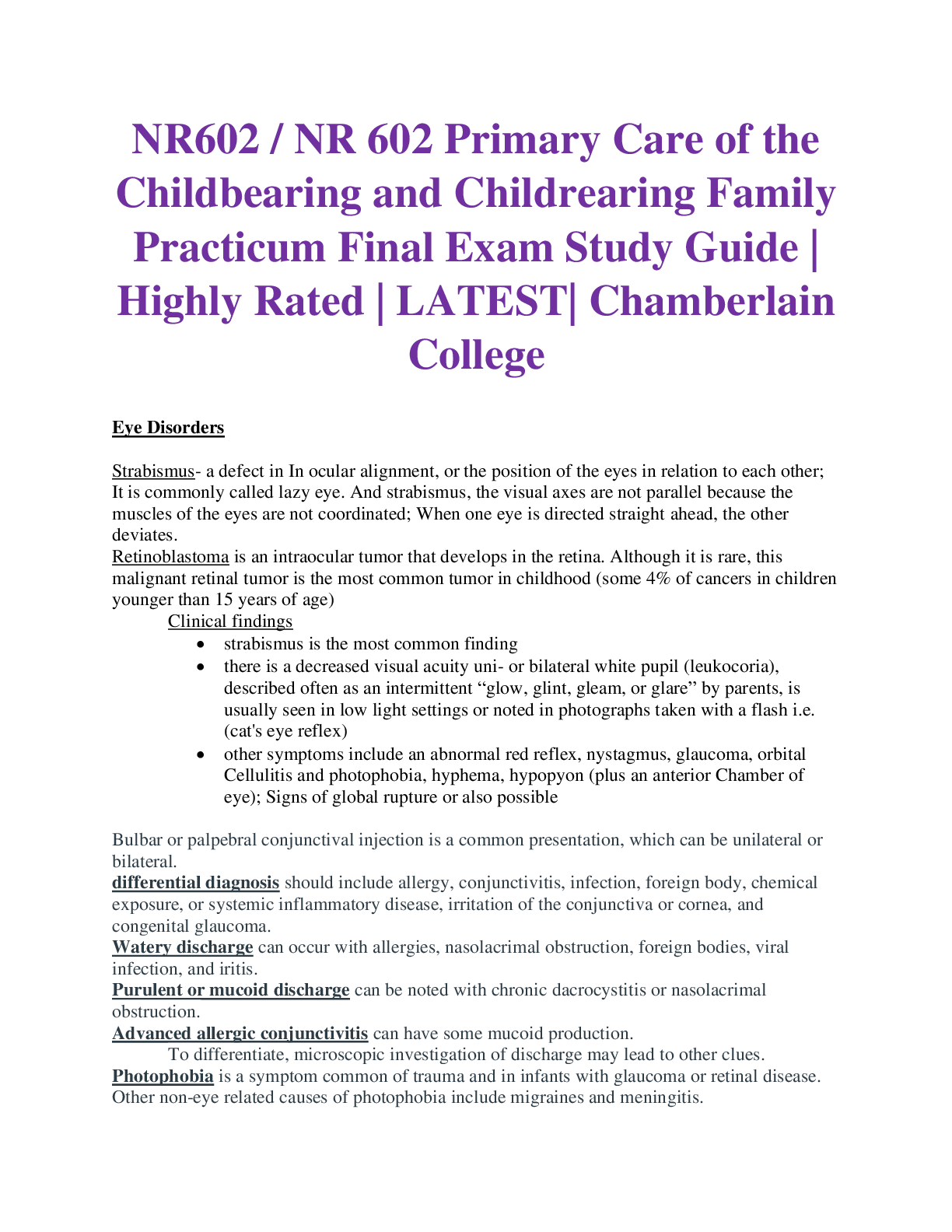
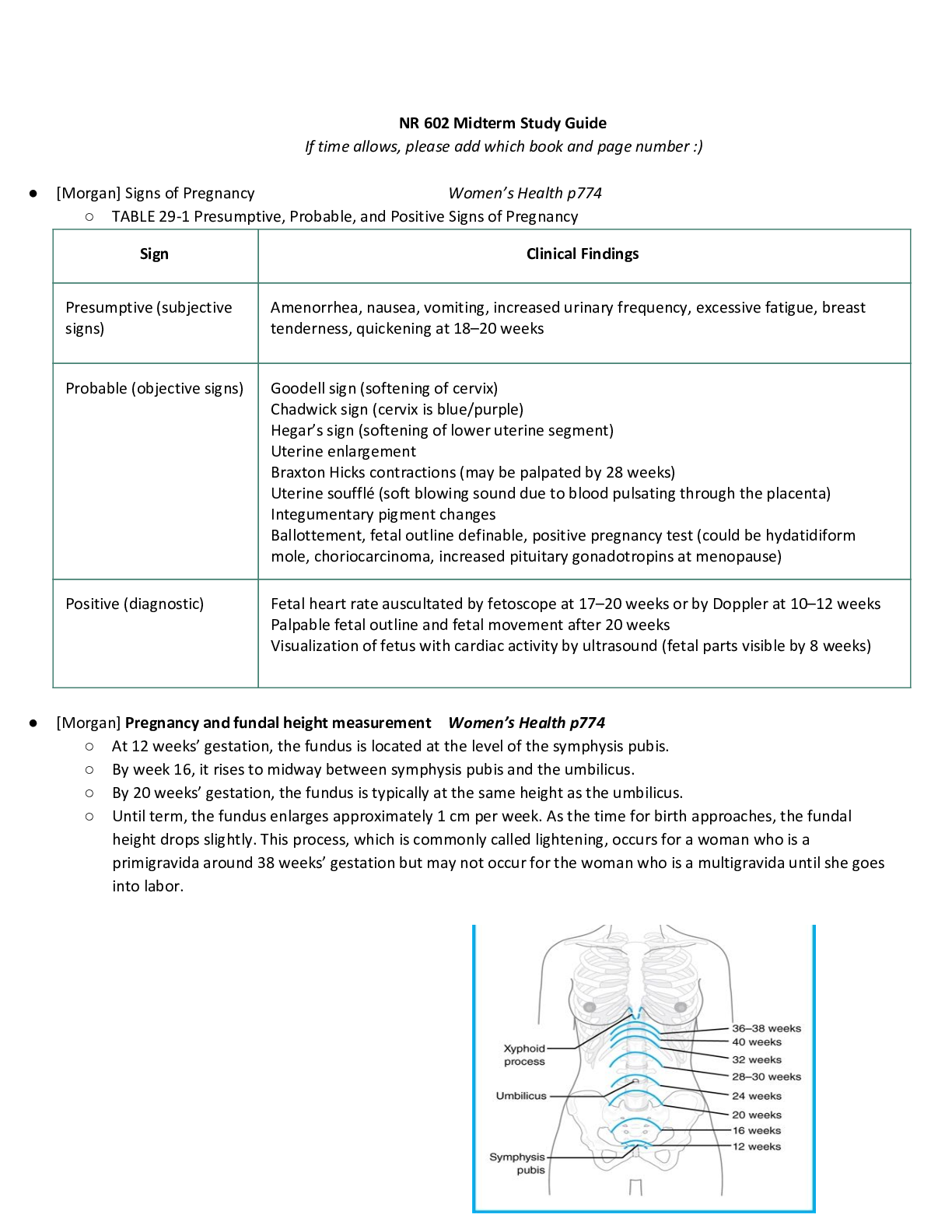
NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rated | Latest | Chamberlain College 1. Signs and symptoms and management of thyroid disorders Hy... perthyroidism: • excessive secretion and synthesis of one or both of the thyroid hormones thyroxine (T4) and triiodothyronine (T3) • Risk factors: Women age 20-40 • Causes: • Graves’ disease is the most common cause of spontaneous hyperthyroidism. It is an autoimmune disorder characterized by autoreactive, agonistic antibodies to the TSH receptor • Graves’ disease accounts for 80% to 90% of hyperthyroid cases • Subacute thyroiditis is the most common cause of thyrotoxicosis, accounting for 15% to 20% of cases. Characterized by glandular inflammation and follicular cell destruction, viral etiology, frequently occurring following an acute viral infection. • Toxic multinodular goiter (Plummer disease) is as common as subacute thyroiditis, more common in other parts of the world where dietary iodine deficiency is prevalent. • A tumor of the pituitary gland causing hypersecretion of TSH (thyrotropin) is a rare cause of hyperthyroidism • S/S: Anxiety, nervousness, diaphoresis, fatigue, heat intolerance, palpitations, weight loss, and insomnia. In situations in which the thyroid tissue has become enlarged, the patient may complain of fullness or pressure in the neck. Additional symptoms include weakness, exercise intolerance, tremors, lower extremity edema, weight loss in the presence of an increased appetite, menstrual irregularities, frequent bowel movements or diarrhea, and exertional dyspnea. Eye complaints include blurred vision, proptosis (downward displacement of the eyeball), photophobia, and double vision. Patients may also report that they are unable to concentrate, extremely irritable, and emotionally labile • clinical manifestations of thyrotoxicosis, which include palpitations, diaphoresis, heat intolerance, and anxiety • Testing: sensitive serum TSH assay, measurement of T4 and T3 levels, Graves’ disease, antithyroglobulin and antimicrosomal antibodies are elevated A 24-hour radioactive iodine uptake (RAIU) test can differentiate Graves’ disease from subacute thyroiditis and toxic nodular goiters, thyroid ultrasound • Treatment: beta blocker initially, radioactive iodine therapy, Two antithyroid drugs are used—propylthiouracil (PTU) and methimazole (MMI), ablation or surgery Hypothyroidism: • Primary: 95% of patients with hypothyroidism, dysfunction or atrophy of the thyroid gland • Central: thyroid dysfunction is caused by failure of the pituitary gland, the hypothalamus, or both, • Secondary: failure of the pituitary gland to secrete adequate amounts of TSH • Tertiary hypothyroidism: inadequate secretion of thyrotropin-releasing hormone (TRH) by the hypothalamus or failure of TRH to activate its cognate receptors within the pituitary gland • Causes: atrophy (probably autoimmune), TSH receptor–blocking antibodies, Chronic autoimmune thyroiditis (Hashimoto’s disease) Amiodarone, External radiation Status—post-radioiodine (131I) treatment Status—post-thyroidectomy Infiltrating disorders: malignancy, granulomatous disease, Thyroid dysgenesis • S/S: early symptoms are often subtle and nonspecific, fatigue, dry skin, slight weight gain, cold intolerance, constipation, and heavy menses. Myalgia, muscle cramps, headaches, and weakness, very dry skin, coarse hair, loss of lateral eyebrows, alopecia, hoarseness, continued weight gain, slight impairment in mental ability, depression, decreased libido, decreased GI motilitiy and hypersomnia. patients with autoimmune thyroid disease and atrophic gastritis who also present with pernicious anemia • Testing: measuring serum TSH. TSH and FT4, antithyroid antibody titers—either for antimicrosomal (anti-TPO) antibodies or antithyroglobulin antibodies • Side note: Medications such as metoclopramide (Reglan) increase TSH levels. Dopamine (Intropin), glucocorticoids, NSAIDs, and somatostatin decrease TSH levels. Other medications, such as phenytoin (Dilantin), amiodarone (Cordarone), and lithium carbonate, can also affect thyroid function tests. Smoking (nicotine) also impacts thyroid hormone levels. These medication and chemical exposures act via a number of mechanisms to affect thyroid function. A drug may bind with albumin and displace thyroid hormone off carrier proteins, or it may prevent albumin from binding with T3 or T4, in each case resulting in more active hormone in circulation. Some drugs may cause an upregulation in metabolic processing proteins (i.e., different cytochrome P oxidase isomers), which normally inactivate thyroid hormones; thus, their upregulation can lead to more rapid processing of thyroid hormones and, in turn, affect TSH levels. • Treatment: synthroid or levothyroxine 2. Thyroid screening tests, confirmatory tests and monitoring - There are differing opinions on whether to screen for thyroid disorders in asymptomatic adults. Recommendations of 6 Organizations Regarding Screening of Asymptomatic Adults for Thyroid Dysfunction Organization Recommendation American Thyroid Association Women and men > 35 years old should be screened every 5 years. American Association of Clinical Endocrinologists Older patients, especially women, should be screened. Academy of American Family Physicians Patients > 60 years old should be screened. American College of Physicians Women > 50 years with an incidental finding suggestive of symptomatic disease should be evaluated. U.S. Preventative Services Task Force There is insufficient evidence for or against screening. Royal College of Physicians of London Screening of the healthy adult population is unjustified. Although there is no consensus about population screening in healthy individuals, there is evidence to support screening in the following at-risk populations, including those with • autoimmune disorders; • pernicious anemia; • first-degree relative with AI thyroid disease; • history of neck radiation; • history of prior thyroid surgery or dysfunction; • abnormal thyroid examination; and • psychiatric disorders. [Show More]
Last updated: 1 month ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 02, 2021
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Mar 02, 2021
Downloads
0
Views
152



.png)