*NURSING > STUDY GUIDE > NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen Colleg (All)
NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen College
Document Content and Description Below
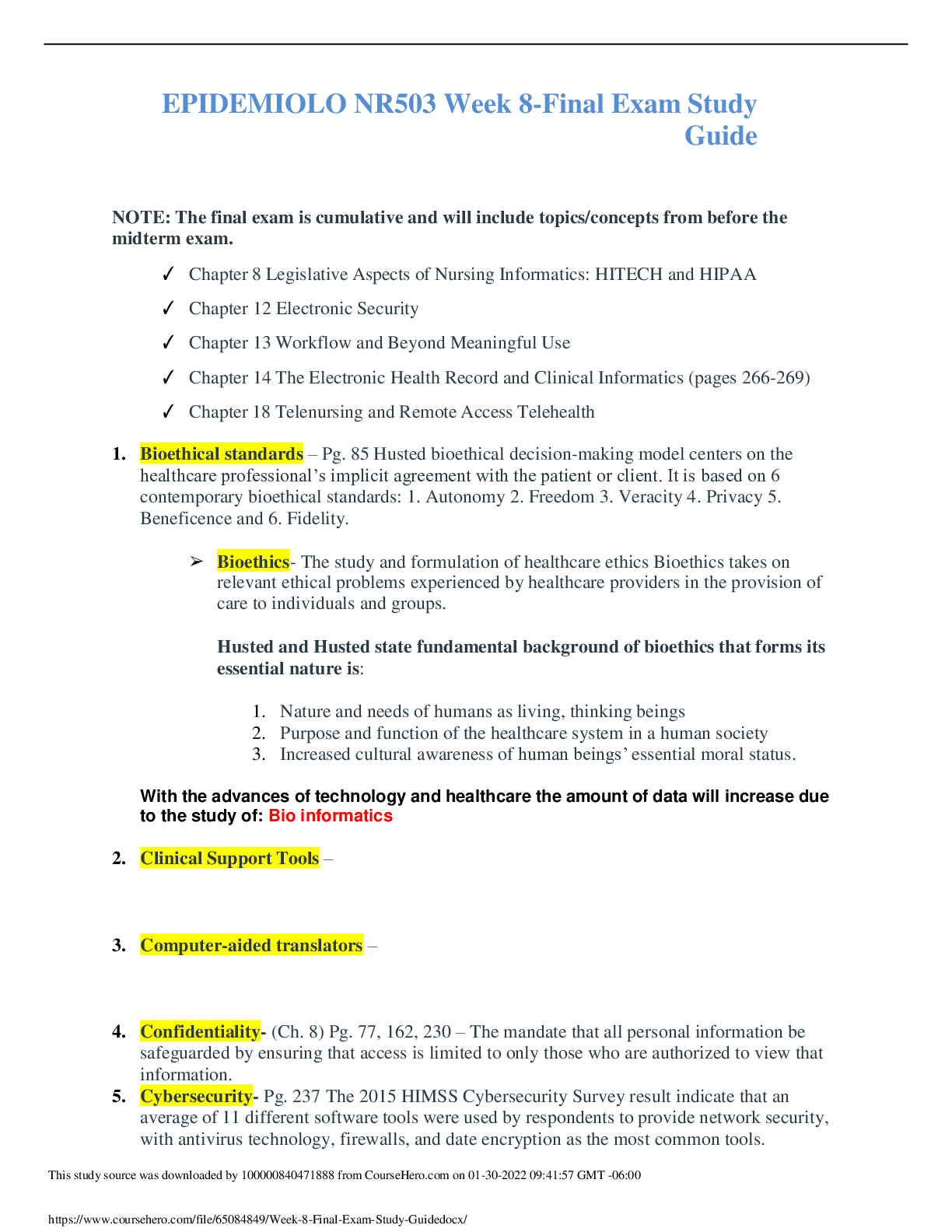
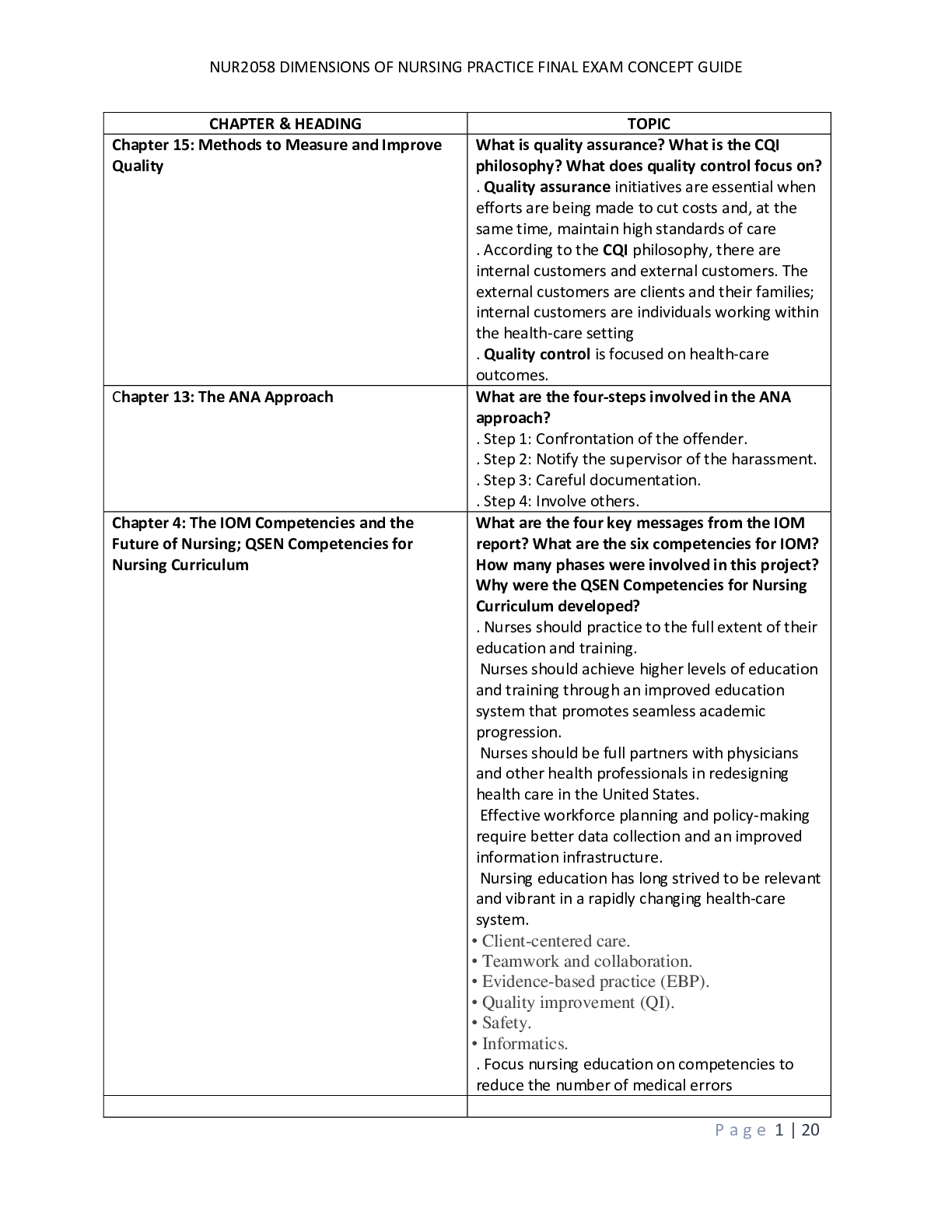
NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen College Nursing is activities that manipulates the environment and helps client achieve the balanced st... ate of health. 1. Definition of terms Values are ideals or concepts that give meaning to an individual’s life. Values are derived most commonly from societal norms, religion, and family orientation and serve as the framework for making decisions and taking action in daily life. Values tend to change as a person grows, and life situations change. Morals are the fundamental standards of right and wrong that an individual learns and internalizes, usually in the early stages of childhood development. Often based on religious beliefs, although societal influence plays an important part in this development. Moral behavior is often manifest as behavior in accordance with group norms, customs, or traditions. Ethics are declarations of what is right and wrong and of what ought to be. Ethics are usually presented as systems of value behaviors and beliefs; they serve the purpose of governing conduct to ensure the protection of an individual’s rights. Can exist in small groups to a society; a system of morals. Laws can generally be defined as rules of social conduct made by humans to protect society, and these laws are based on concerns about fairness and justice. The goals of laws are to preserve the species and promote peaceful and productive interactions between individuals and groups of individuals by preventing the actions of one citizen from infringing on the rights of another. Two important aspects: should be enforceable through police force and applied equally to all persons Ethical dilemma is a situation that requires an individual to make a choice between two equally unfavorable alternatives. The basic, elemental aspects of an ethical dilemma usually involve conflict of one individual’s rights with those of another, conflict of one’s individual obligation with the rights of another, or combined conflict of one group’s obligations and rights with those of another group. A Code of Ethics is generally defined as a written statement or list of the ethical principles that govern a particular profession. They are presented as general statements and thus do not give specific answers to every possible ethical dilemma that might arise. Ethical code: a framework for decision-making, usually for an identified group; should be action oriented and usable on a daily basis. Guides the conduct of a professional. Euthanasia is defined as the act or practice of killing, for reasons of mercy, individuals who have little to no chance of recovery by withholding or discontinuing life support or by administering a lethal agent. Passive Euthanasia usually refers to the practice of allowing an individual to die without any extraordinary intervention. Active euthanasia usually describes the practice of hastening an individual’s death through some act or procedure; poison, gun, knife, or pain medication. Ethical Accountability is when each person is responsible for his or her own actions. It is one of the key elements of being a professional, and the individual must be willing to accept the consequences for their own decisions. A responsibility to perform the activities and duties of the profession according to established standards. Accountability is answerability. Nurses are accountable to clients, the public, the profession, facility administration, physicians, and other nurses. Autonomy is the right of self-determination, independence, and freedom. It refers to the client’s right to make health-care decisions for himself or herself, even if the health-care provider does not agree with those decisions. Client has the right to refuse treatment. Under certain circumstances, rights can be imposed on, such as an individual being a threat to society. Beneficence is one of the oldest requirements for health-care providers, views the primary goal of health care as doing good for clients under their care. An ethical principal based on beliefs that the health-care provider should do no harm, prevent harm, remove existing harm, and promote the good and well-being of the client. Good care requires the provider to take a holistic approach to the client, including the client’s beliefs, feelings, and wishes, as well as those of family and significant others. Problem: determining what is best for the client. Nonmaleficence is the requirement that health care providers do no harm to their clients, either intentionally or unintentionally. Requires health-care providers to protect those who cannot protect themselves; evident in groups of children, the mentally incompetent, the unconscious, and the weak. Obligations to report child-abuse. Justice is the obligation to be fair to all people. Individuals have the right to be treated equally, regardless of race, gender, marital status, medical diagnosis, social standing, economic level, or religious belief. Underlines the first statement in the ANA’s code of ethics. Fidelity is the obligation of an individual to be faithful to the commitment made to himself or herself and to others. Fidelity also includes the professional’s faithfulness or loyalty to agreements and responsibilities accepted as part of the practice of the profession. It is the main support for the concept of accountability, although conflicts may arise from obligations owed to different individuals/groups. Veracity is the principle of truthfulness. It requires the health-care provider to tell the truth, and not to intentionally deceive or mislead clients. The primary limitations occur when telling the client, the truth would seriously harm the client’s ability to recover or would produce greater illness. Veracity is the basic foundation for a trusting relationship between nurse and client. Advance directives are decisions made by competent individuals about their future health care. It is essential that the clients wish about health care be followed, and all client communication to the nurse about desires for future care should be documented. This is a form of self-determination. Should designate an individual to act as moral surrogate, if client becomes unable to make their own decisions. Legal Requirement. Living Will is a signed legal document in which an individual makes known their wishes about the care they are to receive if they should become incompetent at a future date; it usually specifies what types of treatments are permitted and what types are to be withheld. Ethical difficulties include moral conflict, lack of clarity, and the lack of client knowledge on disease and conditions. Should be updated, as life situations change. Often poorly written and too general. The Durable Power of Attorney for Health Care (DPOAHC) refers to a person who is legally designated to make health-care decisions for an individual who is no longer able to make those decisions for himself or herself. The Omnibus Budget Reconciliation Act (OBRA) of 1990 made it mandatory for all health-care facilities, such as hospitals, nursing homes, and home health-care agencies, to provide information to clients about the living will and DPOAHC. The DPOHAC, in consultation with medical professionals, should consider the client’s cognitive abilities, the level of pain, loss of dignity and humiliation, life expectancy, treatment options, and risk/benefits to treatment options. Abandonment is leaving a client without the client’s permission; terminating the professional relationship without providing for appropriate continued or follow-up care by another equally qualified professional. The relationship between client and nurse continues till mutual termination. Key phrase: “without adequate notice.” Leaving after your shift is not considered to be abandonment on your part, but by the hospital. Going on strike with an adequate notice is not considered abandonment. Module 1 : Chapter 2,4,5 Nursing Now Chapter 2 • Identify the “father of modern medicine” and key historical persons who advanced the nursing profession Hippocrates was considered to be the father of modern medicine. His beliefs focused on harmony with the natural law instead of on appeasing the gods. He emphasized treating the whole client-mind, body, spirt, and environment -and making diagnoses on the basis of symptoms rather than on an isolated idea of a disease Florence Nightingale is universally regarded as the founder of modern nursing. Dedicated her life to improving health care and nursing standards. Played a huge part in the Crimean War and [Show More]
Last updated: 1 month ago
Preview 1 out of 38 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 05, 2020
Number of pages
38
Written in
Additional information
This document has been written for:
Uploaded
Dec 05, 2020
Downloads
0
Views
48



.png)
 Rasmussen College.png)