*NURSING > QUESTIONS & ANSWERS > Nursing: This is VCE 2 Exam in 110 Pages. Contains; Lesson 23 - Diabetes Mellitus, Part 2, Lesson 09 (All)
Nursing: This is VCE 2 Exam in 110 Pages. Contains; Lesson 23 - Diabetes Mellitus, Part 2, Lesson 09 - Cancer, Lesson 11 - Care and Treatment of the Patient with Complications of Cancer, Lesson 06 - Acid-Base Imbalance, Lesson 22 - Diabetes Mellitus, Part 1, Lesson 04 - Postoperative Assessment, and Lesson 09 - Care of the Patient Experiencing Exacerbation of an Asthmatic Condition QnA
Document Content and Description Below
Lesson 23 - Diabetes Mellitus, Part 2 • Due No due date • Points 31 • Questions 31 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 452 minutes 5.63 out of 31 * * Some que... stions not yet graded Score for this quiz: 5.63 out of 31 * Submitted Sep 24 at 3:31pm This attempt took 452 minutes. Question 1 1 / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 30 minutes to complete. Exercise 1 - Question 1 Match each insulin to its appropriate classification. (Note: Classifications may be used more than once.) (A) Rapid-acting (B) Short-acting (C) Intermediate-acting (D) Long-acting Correct! Isophane insulin NPH injection (Humulin N, Novolin N) Correct! Human lispro injection (Humalog) Correct! nsulin glargine injection (Lantus) Correct! Regular human insulin injection (Humulin R, Novolin R) Correct! Insulin aspart (Novolog) Question 2 1 / 1 pts Exercise 1 - Question 2 Which insulins has the quickest onset of action? Humulin N C A D B A Humulin R Levimir Correct! Novolog Question 3 1 / 1 pts Exercise 1 - Question 3 Which insulin has no identifiable peak effect? Humulog Correct! Lantus Novolin N Toujeo Question 4 1 / 1 pts Exercise 1 - Question 4 Which insulin has the longest duration of action? Humulin 70/30 Relion N Correct! Tresiba U-100 Humulin R U-500 Question 5 0.63 / 1 pts Exercise 1 - Question 5 Match each classification of oral agents to its appropriate mechanism of action. (A) Trigger release of insulin from the beta cells (B) Act like natural gut hormones to decrease glucagon and glucose secretion and delay gastric emptying (C) Delay digestion of starches and the absorption of glucose from the small intestine (D) Decrease liver glucose production and improve sensitivity of insulin receptors (E) Prevent an enzyme from breaking down natural gut hormones, allowing for decreased glucagon secretion and glucose production (F) Inhibit glucose production by the liver, inhibit intestinal absorption of glucose, and increase insulin Correct! Alpha glucosidase inhibitors You Answered Amylin analogs Correct Answer C B G Correct! Biguanides Correct! DPP-4 inhibitors You Answered Incretin mimetics (GLP-1 agonists) Correct Answer B Correct! Insulin sensitizers Correct! Insulin stimulators (secretagogues) You Answered Sodium glucose transport inhibitors Correct Answer H Question 6 1 / 1 pts F E A D A F Exercise 1 - Question 6 Match each medication with its appropriate classification. (Note: Classifications may be used more than once.) (A) Alpha glucosidase inhibitors (B) Amylin analogs (C) Biguanides (D) DPP-4 inhibitors (E) Incretin mimetic (F) Insulin sensitizers (G) Insulin stimulators (H) Sodium glucose transport inhibitors Correct! Arcabose Correct! Canagliflozin Correct! Glipizide Correct! Glymeperide Correct! Liraglutide Correct! Metformin A H G G E Correct! Pioglitzone Correct! Pramlintide Correct! Repaglinide Correct! Sitagliptin Question 7 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 40 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • From the Patient List, select Harry George (Room 401). • Click on Go to Nurses’ Station. • Click on Chart and then on 401. • Click on Emergency Department. Exercise 2 - Question 1 What two medications were ordered to control Harry George’s diabetes? Include the dose and route for each. Your Answer: Regular insulin 10 units IV and Glyburide 1.25 mg PO C F B G D Regular insulin 10 units IV, followed by 10 units subcutaneously Question 8 Not yet graded / 1 pts Exercise 2 - Question 2 How would you give the IV insulin? (Hint: You can access the Drug Guide by clicking on the Drugicon in the lower left corner of the screen in the Nurses’ Station.) Your Answer: Mix 250 units of regular human insulin in 250 mL of normal saline (1 U/mL). Flush approximately 30 mL through the line prior to administration. Do not use a filter or filtered set with insulin. Piggyback the insulin drip into intravenous fluid using an intravenous infusion pump with a capability of 0.1 mL/hr. Undiluted, IV push Question 9 Not yet graded / 1 pts Exercise 2 - Question 3 Find the Emergency Department physician's progress notes for Monday at 1345. What does the physician plan to order for the sliding scale insulin coverage? Your Answer: sliding scale coverage as follows: 0-150 mg/dL, give 0 units 151-200 mg/dL, give 3 units 201-250 mg/dL, give 7 units 251-300 mg/dL, give 10 units; greater than 300 mg/dL, call physician for orders. 0 to 150 mg/dL, give 0 units regular insulin 151 to 200 mg/dL, give 3 units regular insulin 201 to 250 mg/dL, give 7 units regular insulin 251 to 300 mg/dL, give 10 units regular insulin Above 300 mg/dL, call physician Blood glucose testing to be done before meals and at bedtime. Question 10 Not yet graded / 1 pts • Click on Physician’s Orders. Exercise 2 - Question 4 Look at the orders for Monday at 1345. What was the actual sliding scale insulin order? Your Answer: 1-150 mg/dL give 0 Units 151-200 mg/dL give 3 Units 201-250 give 7 Units 251-300 give 10 Units >300 mg/dL call MD 0 to 150 mg/dL, 0 units regular insulin 151 to 200 mg/dL, 3 units regular insulin 201 to 250 mg/dL, 7 units regular insulin 251 to 300 mg/dL, 10 units regular insulin Above 300 mg/dL, call physician Check blood glucose before meals Question 11 Not yet graded / 1 pts • Click on Return to Nurses' Station. • Click on Kardex and then on 401 to access the correct record. Exercise 2 - Question 5 According to the Kardex, how often should the capillary blood glucose be tested? Your Answer: Capillary blood glucose 4 times/day-before meals and at bedtime 4 times a day; before meals and at bedtime Question 12 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on MAR and then on 401 for Harry George’s records. Exercise 2 - Question 6 According to the MAR, when should the insulin sliding scale be administered? What was the time of this order? Your Answer: PRN ordered on monday at 1830 Sliding scale to be administered before meals. Order dated Monday at 1830. Question 13 Not yet graded / 1 pts Exercise 2 - Question 7 What would you do regarding the inconsistencies identified above? Your Answer: the inconsistencies are intentional because not everytime will you use the sliding scale The nurse can always call the physician to verify an order. However, in this case, if the nurse would go back into the chart and look at the physician’s orders dated Monday 1830, it would be noted that the physician did update the insulin sliding scale orders to be done before meals and at bedtime. Therefore, the nurse simply needs to correct the transcription error on the MAR. According to hospital policy, the nurse might also have to complete a reporting form documenting an error or potential medication error. Question 14 Not yet graded / 1 pts Exercise 2 - Question 8 What problems might occur if Harry George does not receive insulin at bedtime? Your Answer: his blood sugar will rise to drastic levels Elevated fasting blood glucose. If high enough, could result in fluid and electrolyte imbalances as well. Clinical manifestations might include polydipsia and polyurea. Elevation would also cause HbA1c to rise. Question 15 Not yet graded / 1 pts • Click on Return to Nurses' Station. • Click on 401 at the bottom of the screen. • Click on Clinical Alerts. Exercise 2 - Question 9 What is the clinical alert for 0730? Your Answer: Fasting morning glucose of 206. Fasting morning glucose of 206 Question 16 Not yet graded / 1 pts Prepare and administer the sliding scale insulin for this glucose level by following these steps: • Click on Medication Room on the bottom of the screen. • Click on MAR or on Review MAR at any time to verify how much insulin to administer based on sliding scale. (Hint: You must click on the correct room number within the MAR. Remember to look at the patient name on the MAR to make sure you have the correct patient's records.) Click on Return to Medication Room after reviewing the correct MAR. • Click on Unit Dosage and then on drawer 401 for Harry George’s medications. • Select Insulin Regular, put medication on tray, and then close the drawer. • Click on View Medication Room. • Click on Preparation and choose the correct medication to administer. Click on Prepare. • Click on Next, choose the correct patient to administer this medication to, and click on Finish. • You can click on Review Your Medications and then on Return to Medication Room when ready. Once you are back in the Medication Room, you may go directly to Harry George’s room by clicking on 401 at the bottom of the screen. • Click on Patient Care. • Click on Medication Administration and follow the steps in the Administration Wizard to complete the insulin administration. Exercise 2 - Question 10 How much insulin should be administered? Your Answer: 7 units 7 units, or 0.07 mL Question 17 Not yet graded / 1 pts Exercise 2 - Question 11 What is the preferred site of administration for fastest absorption? Your Answer: Abdomin Abdomen Question 18 Not yet graded / 1 pts Exercise 2 - Question 12 List the expected onset, peak, and duration for the insulin you just administered. What actual times would you expect the onset, peak, and duration for Harry George, based on giving the insulin at 0730? Expected length of time: • Onset • Peak • Duration Actual Time After 0730 Dose: • Onset • Peak • Duration Your Answer: Expected length of time: • Onset; 30 min- 1 hour • Peak: 2-4 hours • Duration: 6-8 hours Actual Time After 0730 Dose: • Onset: 0800-0830 • Peak: 0930-1130 • Duration: 1330-1530 Expected Length of Time: • Onset—0.5 to 1 hour • Peak—2 to 4 hours • Duration—5 to 7 hours Actual Time After 0730 Dose: • Onset—0800 to 0830 • Peak—0930 to 1130 • Duration—1230 to 1430 Question 19 Not yet graded / 1 pts Exercise 2 - Question 13 At what time would Harry George be at most risk for hypoglycemia? Describe the signs and symptoms that would indicate this acute complication. Your Answer: 0930-1130 Feeling shaky, Being nervous or anxious, Sweating, chills and clamminess, Irritability or impatience, Confusion, Fast heartbeat, Feeling lightheaded or dizzy, Hunger. Just before eating breakfast, when the insulin’s action is beginning before the patient has eaten any food. He would also be at risk for hypoglycemia midmorning to late morning if he does not eat his breakfast as ordered. Signs and symptoms of hypoglycemia include shakiness, tremor, sweating, nervousness, anxiety, irritability, impatience, tachycardia, palpitations, chills, clamminess, lightheadedness, pallor, hunger, nausea, headache, tiredness, drowsiness, weakness, warmth, dizziness, faintness, blurred vision, nightmares, crying out in sleep, paresthesias, difficulty concentrating, difficulty speaking, incoordination, behavior change, confusion, coma, and seizures. Question 20 Not yet graded / 1 pts Exercise 2 - Question 14 While you are preparing to administer Harry George’s insulin, he asks you why he is taking this because he did not use insulin at home. How would you answer this? Your Answer: I would tell him his blood sugar is high and insulin helps regulate it. I would explain that if his blood sugar doesnt lower he could develop other medical issues The stress of his current illness and hospitalization increases his blood glucose more than at home. Therefore it is common to check the patient's blood glucose four times a day and cover the elevations with Regular insulin. It does not mean that he will have to take insulin once he is recovered. Question 21 Not yet graded / 1 pts Exercise 2 - Question 15 For what side effects should you monitor Harry George related to his insulin regimen? Your Answer: Low blood sugar, Weight gain when you first start using it, Lumps or scars where you've had too many insulin injections, Rash at the site of injection or, rarely, over your entire body. Hypoglycemic reactions, dawn phenomenon, and Somogyi phenomenon. Question 22 Not yet graded / 1 pts Exercise 3 - Virtual Hospital Activity • This exercise will take approximately 35 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 4. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • Click on Chart and then on 401 for Harry George's chart. (Remember: You are not able to visit patients or administer medications during Period of Care 4. You are able to review patient records only.) • Click on Nurses' Notes. Exercise 3 - Question 1 Read the notes for Wednesday at 1730. What does the patient say regarding glyburide? Your Answer: Refused Glyburide. States he just got insulin, so he doesn't need the insulin pill. He doesn't understand why he has to get them both. He did all right before he came to the hospital without insulin or the insulin pill. Harry George refused the glyburide. He states that because he just got insulin, he doesn’t need the insulin pill. Question 23 Not yet graded / 1 pts Exercise 3 - Question 2 How would you respond to the patient's demands? Your Answer: I would listen to his concerns and explain why it is important to take both insulin and glyburide. If he continues to refuse i would document this in his file as a refusal and monitor his blood sugar The nurse needs to explain the medications to the patient. He should be told that the insulin is active for only a short period of time and is given to cover his high blood glucose in conjunction with the use of glyburide. Glyburide is still needed to maintain a more constant, normal level of blood glucose. The goal of medication therapy is to achieve blood glucose levels at near normal with just the use of glyburide so that the patient will not need to use insulin at home. The action of glyburide can be explained more fully once the patient is more cooperative. Question 24 Not yet graded / 1 pts Exercise 3 - Question 3 How often did Harry George take the glyburide at home? Your Answer: rarely ever Once daily Question 25 Not yet graded / 1 pts Exercise 3 - Question 4 Why do you think this was increased in the hospital? What concerns might you have regarding this increase? (Hint: This patient is also receiving insulin.) Your Answer: His blood glucose is out of control so they are trying to get it under control. I would watch him for hypoglycemia Harry George’s blood glucose levels may not have been controlled on the once-daily dose. When he was admitted, his glucose level was 380 mg/dL, necessitating an increase in his oral regimen. However, the patient states that he was unable to take his medication for a week because he did not have it. Therefore the nurse needs to be watchful for signs and symptoms of hypoglycemia, the most common side effect of oral hypoglycemic agents. Question 26 Not yet graded / 1 pts Exercise 3 - Question 5 What classification of oral hypoglycemic does glyburide belong to? (Hint: For help, click on the Drug Guide located on the counter in the Nurses' Station.) Your Answer: Sulfonylurea Second-generation sulfonylureas Question 27 Not yet graded / 1 pts Exercise 3 - Question 6 For what side effects of glyburide should you assess Harry George? Your Answer: diarrhea, dizziness, headache, heartburn, nausea, gas, weight gain. Altered taste sensation, dizziness, drowsiness, weight gain, constipation, diarrhea, heartburn, nausea/vomiting, stomach fullness, headache, photosensitivity, peeling skin, rash, itching Question 28 Not yet graded / 1 pts Exercise 3 - Question 7 What specific patient teaching points should you give this patient regarding glyburide? Your Answer: Instruct patient to take medication at same time each day. Take missed doses as soon as remembered unless almost time for next dose. Do not take if unable to eat. Explain to patient that this medication controls hyperglycemia but does not cure diabetes. Do not skip or delay meals. Watch for signs/symptoms of hypoglycemia and hyperglycemia. Carry candy, sugar packets, or other quick source of sugar for immediate response to hypoglycemia. Wear medical alert bracelet with information. Notify provider of any changes that would affect blood glucose levels, such as increased stress, illness, infection, trauma, heavy physical activity. Wear sunscreen and protective eyewear. Demonstrate correct method for blood glucose monitoring. Question 29 Not yet graded / 1 pts • Click on EPR. • Select 401 from the Patient drop-down menu and Vital Signs from the Category drop-down menu. • Click on Exit EPR. • Click on Chart and then on 401. Exercise 3 - Question 8 List the date and time, blood glucose levels, and insulin doses received since Harry George's admission. (Hint: There are eight. You will need to access the chart and review the expired MARs to obtain the sliding scale doses.) Your Answer: mon 2035 10 units Tue 0735 3 units Tue 1135 7 units Tue 1735 7 units Tue 2305 3 units Wed 0720 7 units Wed 1105 7 units Wed 1735 7 units Monday 2035; 253 mg/dL; 10 units Tuesday 0735; 180 mg/dL; 3 units Tuesday 1135; 201 mg/dL; 7 units Tuesday 1735; 220 mg/dL; 7 units Tuesday 2305; 179 mg/dL; None Wednesday 0720; 206 mg/dL; 7 units Wednesday 1120; 226 mg/dL; 7 units Wednesday 1735; 218 mg/dL; 7 units Question 30 Not yet graded / 1 pts Exercise 3 - Question 9 Based on Harry George’s pattern of blood glucose levels, would you evaluate his current therapy as effective? If not, how might the physician further treat his diabetes? Your Answer: No, raise initial dose Somewhat, but his glucose levels are not optimally controlled. The blood glucose levels are remaining consistently above 200 mg/dL The physician may consider the addition of another oral hypoglycemic agent and/or increase the insulin coverage. Question 31 Not yet graded / 1 pts Exercise 3 - Question 10 If you were reviewing the chart orders and the EPR on Wednesday evening and found the information recorded in the table in question 8, what would you be ethically and legally bound to report? Your Answer: that the patients treatment is not effective The medication omission error related to the lack of insulin coverage given on Tuesday at bedtime would need to be reported. With a glucose level of 179, the patient should have received 3 units of regular insulin, but he did not receive it because the order was transcribed inaccurately. Quiz Score: 5.63 out of 31 Previous Next Submission Details: Lesson 09 - Cancer • Due No due date • Points 35 • Questions 35 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 80 minutes 3.4 out of 35 * * Some questions not yet graded Score for this quiz: 3.4 out of 35 * Submitted Sep 23 at 9:23am This attempt took 80 minutes. Question 1 0.6 / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 15 minutes to complete. Exercise 1 - Question 1 Match each term below with its corresponding definition. (A) A substance that promotes or enhances growth of the initiated cancer cell (B) An irreversible event that can lead to cancer development (C) Another name for cancer development (D) Substance that changes the activity of a cell's genes so that the cell becomes a cancer cell (E) The time when bone marrow activity and white blood cell counts (WBCs) are at their lowest levels after chemotherapy Correct! Carcinogenesis Correct! Initiation You Answered Carcinogen Correct Answer D You Answered Promoter Correct Answer A Correct! Nadir Question 2 C B A D E 1 / 1 pts Exercise 1 - Question 2 Match each type of therapy with the most accurate description. (A) Uses high-energy radiation from gamma rays, radionuclides, or ionizing radiation beams to kill cancer cells, provide disease control, or relieve symptoms (B) Often plays a part in the diagnosis and management of cancer. Used for prophylaxis, diagnosis, cure, control, palliation, assessment of treatment effectiveness, or tissue reconstruction (C) Uses antineoplastic drugs to kill cancer cells and disrupt their cellular regulation Correct! Surgery Correct! Radiation therapy Correct! Chemotherapy Question 3 0.8 / 1 pts Exercise 1 - Question 3 What are the common sites of metastasis for lung cancer? Select all that apply. (Hint: See Table 21-1 in your textbook.) Central nervous system Correct! Lymph nodes Correct! B A C Bone Correct Answer Pancreas Correct! Brain Gastrointestinal (GI) tract Correct! Liver Question 4 Not yet graded / 1 pts Exercise 1 - Question 4 List the warning signals associated with lung cancer. (Hint: See Table 30-5 in your textbook.) Your Answer: A new cough that is persistent or worsens, or a change in an existing chronic cough. Cough that produces blood. Pain in the chest, back or shoulders that worsens during coughing, laughing or deep breathing. Shortness of breath that comes on suddenly and occurs during everyday life. • Hoarseness • Change in respiratory pattern • Persistent cough or change in cough • Blood-streaked sputum • Rust-colored or purulent sputum • Frank hemoptysis • Chest pain or chest tightness • Shoulder, arm, or chest wall pain • Recurring episodes of pleural effusion, pneumonia, or bronchitis • Dyspnea • Fever associated with one or two other signs • Wheezing • Weight loss • Clubbing of the fingers Question 5 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 35 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click on Go to Nurses’ Station. • Click on Chart and then on 405 for Pablo Rodriguez’s chart. • Click on History and Physical. Exercise 2 - Question 1 What is Pablo Rodriguez’s main diagnosis? Your Answer: Metastatic lung cancer Advanced metastatic non-small cell lung cancer Question 6 Not yet graded / 1 pts Exercise 2 - Question 2 How long ago was he diagnosed? Your Answer: 1 year ago 1 year ago Question 7 Not yet graded / 1 pts Exercise 2 - Question 3 What risk factor for lung cancer is documented on the History and Physical? Your Answer: Smoking 60 pack-years of smoking Question 8 Not yet graded / 1 pts Exercise 2 - Question 4 What are other risk factors for lung cancer? (Hint: See Chapter 30 in your textbook.) Your Answer: Second hand smoke, exposure to Radon, exposure to asbestos, exposure to other cancer-causing agents, taking certain dietary supplements such as beta carotene, arsenic in drinking water, previous radiation therapy to the lungs Chronic exposure to asbestos, beryllium, chromium, coal distillates, cobalt, iron oxide, mustard gas, petroleum distillates, radiation, tar, nickel, and uranium. Air pollution that contains benzopyrenes and hydrocarbons. Question 9 Not yet graded / 1 pts Exercise 2 - Question 5 What clinical manifestations documented in the physician’s review of systems are related to the disease process of lung cancer? Your Answer: Shortness of breath, muscle weakness, hemoptosis with sputum • Shortness of breath, hemoptysis with sputum • Multiple nodules painful to touch (metastasis) Question 10 Not yet graded / 1 pts Exercise 2 - Question 6 What treatment has Pablo Rodriguez received so far? Your Answer: The patient underwent chemotherapy. After 6 months he underwent radiation therapy for 6 weeks, with a total dose of 63 Gy in 34 fractions, which also included supraclavicular fields in 27 fractions. The patient was then treated with docetaxel and oblimersen sodium. The last dose was 1 month ago. 6 months of chemotherapy followed by 6 weeks of radiation therapy; after radiation therapy he began receiving docetaxel and oblimersen sodium. Question 11 Not yet graded / 1 pts Exercise 2 - Question 7 How long ago did Pablo Rodriguez receive his last chemotherapy? Your Answer: 1 month ago 1 month ago Question 12 Not yet graded / 1 pts • Click on Emergency Department. Scroll down to review the Emergency Department physician's progress notes for Tue at 1800. Exercise 2 - Question 8 The Emergency Department physician notes that Pablo Rodriguez had a chest x-ray and bronchoscopy 1 year ago. Which type of cancer were the findings of the bronchoscopy consistent with? Is this the same type of cancer as was noted by the admitting physician in the History and Physical? Your Answer: adenocarcinoma, no The Emergency Department physician's notes state that findings of Pablo Rodriguez's bronchoscopy were consistent with adenocarcinoma. The admitting physician noted that Pablo Rodriguez has NSCLC. Adenocarcinoma is one of three different types of lung cancer now referred to as NSCLC because of their similar response to treatment. Question 13 Not yet graded / 1 pts Exercise 3 - Virtual Hospital Activity • This exercise will take approximately 30 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click on Get Report. Exercise 3 - Question 1 Which of the problems noted in the shift report were unresolved as of the beginning of Period of Care 1? Your Answer: Pain • Poor sleep • Restlessness • High anxiety Question 14 Not yet graded / 1 pts • Click on Go to Nurses’ Station. • Click on Chart and then on 405. • Click on Nurse's Notes. Exercise 3 - Question 2 Look at the note for Wednesday at 0415. How did the nurse respond to Pablo Rodriguez’s complaints? Were the nurse’s actions appropriate? Your Answer: Reassured patient and told him that the physician will be in for rounds in the early morning. No The nurse reassured Pablo Rodriguez and told him that the physician would be making rounds early in the morning. This is not appropriate in that it does not address the patient's present concerns regarding poor sleep and restlessness. The nurse is just trying to pacify the patient and makes him wait for an intervention. Question 15 Not yet graded / 1 pts Exercise 3 - Question 3 How might you have responded differently? Your Answer: I would ask the patient why he felt restless and if there was anything i could do to help. Suggestions may include calling the physician for a sedative that has a short duration of action and would therefore more suitable to give at this time of night. Comfort care is a priority for Pablo Rodriguez, and he should not have to suffer needlessly for the remainder of the night. Question 16 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on 405 at the bottom of your screen. • Click on Patient Care and then on Nurse-Client Interactions. • Select and view the video titled 0730: Symptom Management. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and on Nurse-Client Interactions to refresh the screen.) Exercise 3 - Question 4 What are Pablo Rodriguez’s two primary concerns at this point? Your Answer: Still sick to stomach and restlessness Nausea and restlessness Question 17 Not yet graded / 1 pts Exercise 3 - Question 5 What assessment should you perform before treating the patient’s complaint of nausea? Your Answer: abdominal exam Gastrointestinal (GI), for bowel sounds Question 18 Not yet graded / 1 pts • Click on MAR; then select tab 405 to access Pablo Rodriguez's record. Exercise 3 - Question 6 What medications are ordered to manage the patient’s nausea? Your Answer: Dexamethasone and Metoclopramide hydrochloride • Metoclopramide 10 mg IV every 6 hours • Metoclopramide 10 mg IV every 2 hours prn nausea Question 19 Not yet graded / 1 pts Exercise 3 - Question 7 What might the nurse question regarding these medication orders? Your Answer: if the patient is on any antidepressants or any other medication that could interact with the medication. The nurse might question the maximum dose of metoclopramide because it is ordered around the clock every 6 hours as well as prn every 2 hours. If the nurse was not cognizant of both orders, the patient could potentially receive too much of the medication if, for example, the patient received a prn dose at 0700 and then the day shift nurse gave the patient the scheduled 0800 dose. Question 20 Not yet graded / 1 pts • Click on Return to Room 405. • Click on Chart and then on 405. • Click on Nursing Admission. Exercise 3 - Question 8 What is the patient’s weight in pounds? What is this in kilograms? Your Answer: 160 lb 73 kg 160 lb (72.73 kg) Question 21 Not yet graded / 1 pts • Click on Return to Room 405. • Click on the Drug icon in the lower left corner of the screen. Exercise 3 - Question 9 Using the information from the Drug Guide and the patient's weight, determine the maximum dose that Pablo Rodriguez can receive of metoclopramide within a 24-hour period for prevention of chemotherapy-induced nausea and vomiting and for postoperative nausea and vomiting. List only the maximum doses for the indications specified below. • Prevention of cancer chemotherapy–induced nausea and vomiting • Postoperative nausea and vomiting Your Answer: • Prevention of cancer chemotherapy–induced nausea and vomiting max dose: 876 mg • Postoperative nausea and vomiting max dose: 20 mg Prevention of cancer chemotherapy–induced nausea and vomiting: 873 mg (patient can receive 2 mg/kg; 72.72 x 2 = 145.5; 145.5 x 6 possible doses = 873 mg total) Postoperative nausea and vomiting: 80 mg (20 mg x 4 possible doses = 80 mg total) Question 22 Not yet graded / 1 pts Exercise 3 - Question 10 Calculate the maximum amount of metoclopramide Pablo Rodriguez could receive per 24 hours as ordered. Is this within the dosage guidelines? Is there any reason to be concerned about Pablo Rodriguez receiving this dosage over long periods of time? Your Answer: 40 mg Maximum dosage is 160 mg/24 hours; this is within the dosage guidelines for preventing chemotherapy-related nausea and vomiting, but not within the guideline for managing postoperative nausea and vomiting. The nurse would be concerned if the patient was to receive this amount over a long period of time, but not if just for 1-2 days because this would be an acceptable post-chemo dose. Question 23 Not yet graded / 1 pts Exercise 3 - Question 11 What are the possible ramifications of giving high doses of this drug? Your Answer: Drowsiness, restlessness, fatigue, lassitude, Dizziness, anxiety, headache, insomnia, breast tenderness, altered menstruation, constipation, rash, dry mouth, galactorrhea, gynecomastia, Hypotension or hypertension, tachycardia Extrapyramidal reactions (akathisia or motor restlessness, involuntary limb movement, and facial grimacing) in children and young adults receiving large doses during cancer chemotherapy. In general, those receiving 2 mg/kg or more or an increase in length of therapy may experience a greater incidence of side effects. Question 24 Not yet graded / 1 pts Exercise 3 - Question 12 What are the ramifications of not administering this drug for Pablo Rodriguez's complaint of nausea? Your Answer: persistent nausea and vomiting Unnecessary suffering for terminally ill patient Question 25 Not yet graded / 1 pts Exercise 3 - Question 13 If the nurse administers the prn dose for this drug at 0730, what should be done with the regularly scheduled 0800 dose? Your Answer: Hold medication The 0800 dose should be held. Question 26 Not yet graded / 1 pts Exercise 4 - Virtual Hospital Activity • This exercise will take approximately 40 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click on Go to Nurses' Station. • Click on Chart and then on 405. • Click on Emergency Department. Exercise 4 - Question 1 What is Pablo Rodriguez’s chief complaint on admission to the Emergency Department? How is this related to his cancer? (Hint: See Chapter 22 in your textbook. Review the Emergency Department physician's note for Tue at 1800.) Your Answer: Nausea and vomiting. related to his chemotherapy treatment. Pablo Rodriguez came in with nausea and vomiting, probably related to hypercalcemia. The hypercalcemia is most likely caused by bone metastasis from the lungs. Question 27 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on MAR and then on 405 to access Pablo Rodriguez's records. Exercise 4 - Question 2 What medications still need to be given to Pablo Rodriguez for the day shift (up to 1500)? Your Answer: Metoclopramide Hydrochloride, Neutra-Phos • Metoclopramide 10 mg IV • Dexamethasone 4 mg IV • Neutra-Phos 1 capsule Question 28 Not yet graded / 1 pts • Click on Return to Nurses' Station. • Click on the Drug icon in the lower left corner of the screen. • Use the Drug Guide to answer the next three questions. Exercise 4 - Question 3 How does ondansetron differ from metoclopramide in regard to antiemetic mechanism of action? Your Answer: Ondansetron: An antiemetic and antinausea agent that is a selective 5-HT3-receptor antagonnist that blocks serotonin, both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone. Therapeutic Effect: Prevents nausea, vomiting. Metoclopramide: A dopamine receptor antagonist that stimulates motility of the upper gastrointestinal (GI) tract. Decreases reflux into esophagus. Raises threshold activity of chemoreceptor trigger zone. Therapeutic Effect: Accelerates intestinal transit and gastric emptying. Produces antiemetic activity. Ondansetron blocks serotonin, both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone. Metoclopramide is a dopamine receptor antagonist that stimulates motility of the upper GI tract. Decreases reflux into esophagus. Raises threshold activity of chemoreceptor trigger zone. Question 29 1 / 1 pts Exercise 4 - Question 4 When administering IV ondansetron, it should be infused over ______ minutes. Correct! Correct Answers 15 Question 30 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on Chart and then on 405 for Pablo Rodriguez's chart. • Click on Patient Education. Exercise 4 - Question 5 Has any teaching been completed? In your opinion, what priority teaching should have been completed upon admission? Your Answer: no, pain management No teaching has been completed, per documentation. Teaching regarding the pain scale should have been completed because pain relief is a priority outcome for this patient and needs to be evaluated appropriately. The other patient teaching can and should wait until the patient’s pain is controlled and the patient is better able to participate. Question 31 Not yet graded / 1 pts 15 • Click on Return to Nurses’ Station. • Click on 405 at the bottom of the screen. • Click on Patient Care and then on Nurse-Client Interactions. • Select and view the video titled 1150: Assessment—Pain. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and then on Nurse-Client Interactions to refresh the screen.) Exercise 4 - Question 6 Why is Pablo Rodriguez not eating? Your Answer: It hurts to chew Sore mouth—probable mucositis Question 32 Not yet graded / 1 pts Exercise 4 - Question 7 Is this a normal side effect of chemotherapy? Your Answer: yes Yes Question 33 Not yet graded / 1 pts Exercise 4 - Question 8 How would you treat this? Your Answer: provide mouth care Frequent mouth assessment and oral hygiene with nontraumatizing products such as soft toothbrush, disposable mouth sponges. New recommendation to include gentle flossing once daily. A variety of alcohol-free compounds for the patient to “swish and spit” are available; these usually contain a local anesthetic and antiinflammatory agents to promote healing. Oral hygiene equipment must be kept clean. Remind patients not to share toothbrushes with anyone. Question 34 Not yet graded / 1 pts • Click on Kardex and select tab 405. Read the outcomes. Exercise 4 - Question 9 What additional outcome(s) might you include for this patient? Your Answer: None. it covered everything i would. Psychosocial and spiritual/cultural outcomes related to end-of-life issues would be important for this patient; however, the psychosocial outcome listed on the Kardex would need to be revised. A suggested outcome might be “Patient/family will express concerns and verbalize a decrease in anxiety.” Question 35 Not yet graded / 1 pts Exercise 4 - Question 10 What is Pablo Rodriguez’s code status? How do you feel about this in relation to his diagnosis and condition? What is the nurse’s professional responsibility related to the patient’s code status? Your Answer: Full. This means that in the event that your heart stops working or you are found to have no pulse, the health care professionals will start chest compressions and/or administer an electrical shock in attempt to resuscitate your heart. The patient is a full code, which would be appropriate for a patient who is being aggressively treated for cancer with hope of recovery or improved quality/duration of life. However, in Pablo Rodriguez’s case, it appears that he is ready to die and is seeking palliative care only. It would be the nurse’s professional responsibility to at least address this issue with the physician or with the patient/family if a rapport has been established and the patient/family is ready to discuss these issues. If a terminal patient still wishes to remain a full code, the nurse must respect the patient’s wishes and not push his or her beliefs on the patient. Quiz Score: 3.4 out of 35 Previous Next Lesson 11 - Care and Treatment of the Patient with Complications of Cancer • Due No due date • Points 32 • Questions 32 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 122 minutes 2.8 out of 32 * * Some questions not yet graded Score for this quiz: 2.8 out of 32 * Submitted Sep 17 at 11:33am This attempt took 122 minutes. Question 1 Not yet graded / 1 pts Exercise 1 - Virtual Hospital Activity • This exercise will take approximately 15 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then Restart the Program to get to the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click Get Report and read the shift report. • Click Go to Nurses' Station. • Click Chart and then 405 to view Pablo Rodriguez's chart. • Click the Emergency Department tab and review the information given. Exercise 1 - Question 1 What are the four priorities identified in the change-of-shift report? Your Answer: 1. Nausea and vomiting most likely secondary to hypercalcemia. 2. Pain secondary to metastatic subcutaneous nodules, which has worsened in the last 2 days as the patient is not tolerating oral medication. 3. Dehydration. 4. Constipation. Continued nausea Pain Anxiety Poor appetite Question 2 Not yet graded / 1 pts Exercise 1 - Question 2 Why was Pablo Rodriguez admitted to the hospital? Your Answer: Patient admitted with nausea and vomiting, and pain unrelieved by home meds. He has been experiencing nausea and vomiting. Question 3 Not yet graded / 1 pts Exercise 1 - Question 3 What has caused this condition? Your Answer: Malignant neoplasm He has metastatic cancer. The progression of the disease has impaired the patient's ability to adequately meet his body's nutritional needs. Pablo Rodriguez has also been unwilling to ask his family members for additional assistance. Question 4 Not yet graded / 1 pts Exercise 1 - Question 4 What findings support this diagnosis? Your Answer: Multiple subcutaneous nodules over left upper chest, back, left hip, and leg. The nodules over lower body warm and tender to touch with some erythema. Upper body lesions dry and intact. Tacky mucous membranes Weak pulse Constipation Decreased urinary output Pallor Question 5 Not yet graded / 1 pts Exercise 1 - Question 5 How was his condition initially managed in the emergency department? Your Answer: Tolerating rehydration therapy without difficulty. IV LR bolus completed and D 5 0.45% NS at 150 mL/hr hung. Decreased nausea. No vomiting. Tolerated PO Neutra-phos well. Nodules continue to be painful. Morphine sulfate 6 mg IV bolus given for pain 7/10. Oxygen 3L flow by nasal cannula with SpO2 90s. VSS. Awaiting transfer to Medical Unit. An IV bolus of lactated Ringer's solution was administered, followed by the administration of D50.45 normal saline at 150 mL/hr. Question 6 Not yet graded / 1 pts Exercise 1 - Question 6 What types of interventions (nursing and medical) may be implemented to manage his care? Your Answer: Comfort care, pain management, wound care IV therapy Antiemetic medications Small, frequent meals Nutritional supplements Quiet environment Rest Question 7 Not yet graded / 1 pts Exercise 1 - Question 7 What should be monitored to determine the degree of dehydration? Your Answer: Urinalysis, sodium, potassium, glucose Mucous membranes Skin turgor Vital signs Intake and output Systems assessments Question 8 Not yet graded / 1 pts Exercise 1 - Question 8 What are the primary goals for this hospitalization? Your Answer: Educational goals: • Understand use of pain scale. • Identify options for end-of-life care. • Use comfort measures. • Keep metastatic lesions clean and dry. Rehydration Pain management Question 9 Not yet graded / 1 pts • Click the History and Physical tab and read the report. Exercise 1 - Question 9 List the impressions identified in the History and Physical. Your Answer: 1. Metastatic lung cancer. 2. Malnutrition related to hypercalcemia and hypophosphatemia. 3. Chronic pain. 4. Constipation. 5. Nausea and vomiting. Metastatic lung cancer Malnutrition related to hypercalcemia and hypophosphatemia Chronic pain Constipation Nausea and vomiting Question 10 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 30 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then Restart the Program to get to the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click Go to Nurses' Station. • Click 405 at the bottom of the screen to enter Pablo Rodriguez's room. • Click Take Vital Signs and then Clinical Alerts and review the information given. • Click Initial Observations and read the notes. • Click Patient Care and complete a head-to-toe assessment. Exercise 2 - Question 1 What current assessment findings support the diagnosis of dehydration? Your Answer: Dry mouth and mucous membranes, Swollen red gums, Skin dry, Capillary refill sluggish at >4 seconds, Last bowel movement on Tuesday of small hard stool reported as passed with difficulty, Voiding freely of clear amber urine in sufficient quantities, Frequency reported. Dry mouth and mucous membranes Generalized weaknesses Fair skin turgor Continued constipation Question 11 Not yet graded / 1 pts • Click Chart and then 405 to view Pablo Rodriguez's chart. • Click the Physician's Orders tab and review the orders since Tuesday at 2300. Exercise 2 - Question 2 Which medications have been ordered to manage Pablo Rodriguez's nausea? Your Answer: 1. Metoclopramide 10 mg IV every 6 hours. 2. Metoclopramide 10 mg IV every 2 hours PRN nausea. Ondansetron hydrochloride and metoclopramide Question 12 Not yet graded / 1 pts • Click Return to Room 405 and then click the Drug icon at the bottom of the screen. • Review the medications you identified in the previous question. Exercise 2 - Question 3 To which drug classification does ondansetron hydrochloride belong? Your Answer: antiemetic It is an antiemetic. Question 13 Not yet graded / 1 pts Exercise 2 - Question 4 What side effects of ondansetron could be problematic, considering Pablo Rodriguez's health concerns? Your Answer: Anxiety, dizziness, drowsiness, headache, fatigue, constipation, diarrhea, hypoxia, urinary retention, Abdominal pain, xerostomia or diminished saliva secretion, fever, feeling of cold, redness and pain at injection site, paresthesia, weakness. This medication may cause fatigue, constipation, and hypoxia. These are symptoms he is already experiencing. This will warrant close observation. Question 14 Not yet graded / 1 pts Exercise 2 - Question 5 What is metoclopramide's mechanism of action? Your Answer: A dopamine receptor antagonist that stimulates motility of the upper gastrointestinal (GI) tract. Decreases reflux into esophagus. Raises threshold activity of chemoreceptor trigger zone. Therapeutic Effect: Accelerates intestinal transit and gastric emptying. Produces antiemetic activity. The medication is used to reduce gastric reflux, thus reducing nausea. Question 15 Not yet graded / 1 pts • Click Return to Room 405. • Once again, click Chart and then 405. • This time, click the Laboratory Reports tab and review the report given. Exercise 2 - Question 6 Review and discuss any significant findings in the CBC results. Your Answer: RBC is low, Hematocrit is very low, Hemoglobin is low, Platelets are elevated. Both the hemoglobin and hematocrit are low. The hemoglobin is especially reduced. Question 16 0 / 1 pts Exercise 2 - Question 7 Consider the clinical presentation of Pablo Rodriguez. Which manifestations may be attributed to his complete blood cell test results? Select all that apply. Nausea You Answered Vomiting Correct Answer Weaknesses Correct! Fatigue You Answered Reduced skin turgor Question 17 Not yet graded / 1 pts Exercise 2 - Question 8 Are there any significant findings in the electrolyte profile? Your Answer: Sodium slightly low, Chloride slightly low, No, these findings are within normal limits. Question 18 Not yet graded / 1 pts Exercise 2 - Question 9 Identify two of the nursing diagnoses that have the highest priority related to Pablo Rodriguez’s admitting diagnosis. Your Answer: Malnutrition, chronic pain, nausea and vomiting, constipation Note: Answers will vary. Potential for fluid imbalance related to nausea Fatigue related to reduced dietary intake Question 19 Not yet graded / 1 pts Exercise 3 - Virtual Hospital Activity • This exercise will take approximately 30 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then Restart the Program to get to the sign-in window.) • From the Patient List, select Pablo Rodriguez (Room 405). • Click Get Report and read the Clinical Report. • Click Go to Nurses' Station and then 405 at the bottom of the screen to enter Pablo Rodriguez's room. • Click Take Vital Signs and review the information given. Exercise 3 - Question 1 How does Pablo Rodriguez rate his pain? Your Answer: 4/10 He rates the pain as a 4 on a 10-point scale. Question 20 Not yet graded / 1 pts • Click MAR and then tab 405 to review the medications ordered for Pablo Rodriguez. Exercise 3 - Question 2 What medications have been ordered to manage Pablo Rodriguez's pain? Your Answer: Morphine sulfate PCA 1 mg/mL 0.5 mg every 10 min/12mg in 4 hr lockout IV continuous Morphine sulfate by PCA pump has been ordered. Question 21 Not yet graded / 1 pts Exercise 3 - Question 3 What is the advantage of this type of dosing? Your Answer: When the patient is in pain he can control when he gets the pain medication and can control his pain himself. Use of the PCA pump provides constant administration of the medication. This promotes consistent blood levels of the analgesic. PCA pumps also allows the patient to participate more actively in his care. It eliminates the need for the patient to wait for the nurse to administer pain medications. Question 22 Not yet graded / 1 pts Exercise 3 - Question 4 List some opioids that may be prescribed to manage the pain associated with advanced cancer. Your Answer: morphine, fentanyl, codeine, oxycodone, hydromorphone, and methadone Hydromorphone Fentanyl Methadone Question 23 0.8 / 1 pts Exercise 3 - Question 5 When administering opioids to manage Pablo Rodriguez's pain, the nurse must understand that which manifestations are common side effects associated with their use? Select all that apply. Diarrhea Correct! Constipation Correct! Bradycardia Correct Answer Rash Correct! Respiratory depression Hyperthermia Correct! Vomiting Question 24 Not yet graded / 1 pts Exercise 3 - Question 6 List several nonopioid medications that can be administered to reduce mild to moderate pain associated with cancer. Your Answer: Acetaminophen (Tylenol), may provide some relief. Nonsteroidal antiinflammatory drugs (NSAIDs), such as aspirin and ibuprofen (Advil), can as well. Acetaminophen Aspirin Ibuprofen Indomethacin Naproxen Question 25 Not yet graded / 1 pts Exercise 3 - Question 7 Discuss medication scheduling techniques that effectively manage pain. Your Answer: You need to take medication at the first sign of any pain. If you wait for the pain to get bad, it takes a while for pain medication to kick in so the patient will be in pain longer. Around-the-clock scheduling is needed to successfully manage the pain. Bolus doses assist with maintaining constant blood levels of pain medicine. Question 26 Not yet graded / 1 pts Exercise 3 - Question 8 As previously stated, Pablo Rodriguez has been experiencing anxiety. Discuss the relationship between pain and anxiety. Your Answer: Researchers recently found that the expression of a neuropeptide called PACAP is increased in animal models of chronic pain, which can lead to anxiety-like behaviors. Pain and anxiety share a cyclic relationship. Pain increases as a result of fear and anxiety. In turn, as the pain increases, fear and anxiousness increase. Question 27 Not yet graded / 1 pts Exercise 3 - Question 9 In addition to medication therapy, what other interventions may be used to manage pain? Your Answer: cognitive behavioral therapy, mindfulness-based stress reduction, acceptance and commitment therapy (ACT), guided imagery and biofeedback. Relaxation therapy Music therapy Massage Positioning to promote comfort Guided imagery Biofeedback Hypnosis Question 28 Not yet graded / 1 pts Exercise 3 - Question 10 What factors may influence a patient's perception of and/or reaction to pain? Your Answer: The perception of, expression of, and reaction to pain are influenced by genetic, developmental, familial, psychological, social and cultural variables. Psychological factors, such as the situational and emotional factors that exist when we experience pain, can profoundly alter the strength of these perceptions. Pain perception is influenced by cultural and religious practices. Question 29 1 / 1 pts • Click Return to Room 405. • Click Patient Care and then Nurse-Client Interactions. • Select and view the video titled 1130: Family Interaction. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and Nurse-Client Interactions to refresh the screen.) Exercise 3 - Question 11 What is the underlying message Pablo Rodriguez is attempting to communicate to his daughter? He is too tired to attend her wedding. The enema has made him feel better. Correct! He is ready to give in to the disease and die. The enema has caused him pain. Question 30 Not yet graded / 1 pts Exercise 3 - Question 12 Does the response by Pablo Rodriguez’s daughter indicate a readiness to accept her father’s condition? Your Answer: She is sad due to her fathers condition but she as well does not want to see her father in pain and agony anymore. Student responses to this question will depend on interpretation. This question can be used to generate a class discussion. It appears that Mr. Rodriguez’s daughter is caught off guard by his admission. As he makes initial attempts to discuss his condition, she continues to address her own activities and concerns. Question 31 1 / 1 pts Exercise 3 - Question 13 Indicate whether the following statement is true or false. Pablo Rodriguez will be allowed to make the decision to forgo further treatment without the approval of his immediate family. Correct! True False Question 32 Not yet graded / 1 pts Exercise 3 - Question 14 Identify referrals that may be beneficial for Pablo Rodriguez and his family at this time. Your Answer: Hospice, Palliative care, psychiatry, Referrals that would be of benefit to the patient and family would include social services and pastoral care. Lesson 06 - Acid-Base Imbalance • Due No due date • Points 30 • Questions 30 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 172 minutes 1.33 out of 30 * * Some questions not yet graded Score for this quiz: 1.33 out of 30 * Submitted Aug 27 at 2:04pm This attempt took 172 minutes. Question 1 0.33 / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 10 minutes to complete. Exercise 1 - Question 1 Match each term with its corresponding definition. (Hint: See Chapter 12 in your textbook.) (A) A measure of the body fluid’s free hydrogen ion level (B) Substance that bindf free hydrogen ions in solution (C) Substance that releases hydrogen ions when dissolved in water You Answered Acid Correct Answer C You Answered Base Correct Answer B Correct! pH Question 2 Not yet graded / 1 pts Exercise 1 - Question 2 Identify and describe three methods of acid-basis homeostasis. Indicate the type of defense and the associated mechanisms of action. • First line of defense • Second line of defense • Third line of defense Your Answer: B C A First line of defense: various chemical buffers which minimize pH changes that would otherwise occur in their absence. Second line of defense: extracellular fluid pH consists in controlling the carbonic acid concentration in the ECF. Third line of defense: renal system, which can add or remove bicarbonate ions to or from the ECF. The bicarbonate is derived from metabolic carbon dioxide which is enzymatically converted to carbonic acid in the renal tubular cells. First line of defense • Type of defense: Chemical/protein buffers • Mechanisms of action: Chemicals (bicarbonate and phosphate) and/or proteins (albumin, globulin, and hemoglobin [Hgb]) rapidly respond to changes in pH by acting as hydrogen ion “sponges.” They can bind hydrogen ions when too many are present or release hydrogen ions when not enough are present. Second line of defense • Type of defense: Respiratory • Mechanisms of action: Works when chemical buffers alone cannot maintain homeostasis. Special receptors in the respiratory areas of the brain respond to changes in amount of carbon dioxide (CO2) in brain tissues. As the amount increases, the brain triggers an increase in the rate and depth of respirations to blow off the CO2. As the amount decreases, central receptors slow the neurons to decrease the rate and depth of respirations, thus increasing CO2 retention. Third line of defense • Type of defense: Renal • Mechanisms of action: Stronger than the first two lines of defense, but takes longer to respond (24-48 hours). When blood pH changes are persistent, renal mechanisms increase excretion and reabsorption rates of acids or bases dependent on direction of the pH changes. Involves three mechanisms: (1) kidney movement of bicarbonate (when blood hydrogen ion levels are high, this bicarbonate is reabsorbed from the kidneys back into circulation, where it can help buffer excess hydrogen ions; when blood hydrogen ion levels are low, the bicarbonate remains in the urine and is excreted); (2) formation of acids (phosphate in urine draws and binds to hydrogen, which is then excreted); and (3) formation of ammonium (ammonia secreted into the urine combines with hydrogen to form ammonium, which is then excreted). Question 3 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 45 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • From the Patient List, select Jacquline Catanazaro (Room 402). • Click on Go to Nurses’ Station. • Click on Chart and then on 402. • Click on History and Physical. Exercise 2 - Question 1 Is there anything in Jacquline Catanazaro’s history that would put her at risk for an acidbase imbalance? Your Answer: Lack of oxygen History of asthma; has not been taking the medication as prescribed Question 4 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on 402 at the bottom of your screen. • Click on Patient Care and then on Nurse-Client Interactions. • Select and view the video titled 0730: Intervention—Airway. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and Nurse-Client Interactions to refresh the screen.) Exercise 2 - Question 2 Based on Jacquline Catanazaro’s history, what would the nurse expect to be causing her respiratory distress? Your Answer: Not taking her medication Asthma exacerbation Question 5 Not yet graded / 1 pts Exercise 2 - Question 3 Why is the nurse waiting until after the arterial blood gases (ABGs) are drawn to give the patient a nebulizer treatment? Your Answer: Depending on what the ABGs say is depending on if a nebulizer treatment is necessary or if a different medication is needed. A nebulizer can change ABGs drastically so you have to be careful. To get a true picture of Jacquline Catanazaro’s acid-base balance while the patient is exhibiting respiratory distress Question 6 Not yet graded / 1 pts • Click on Chart and then on 402. • Click on Laboratory Reports. Exercise 2 - Question 4 Document the results of Jacquline Catanazaro’s ABG on Monday at 1030. • pH • PaO2 • PaCO2 • O2sat • Bicarb Your Answer: • pH: 7.33 • PaO2: 80 • PaCO2: 48 • O2sat: 85 • Bicarb: 23 pH: 7.33 PaO2: 80 PaCO2: 48 O2sat: 85% Bicarb: 23 Question 7 Not yet graded / 1 pts Exercise 2 - Question 5 Document the results of Jacquline Catanazaro’s ABG on Wednesday at 0730. • pH • PaO2 • PaCO2 • O2sat • Bicarb Your Answer: • pH: 7.35 • PaO2: 80 • PaCO2: 50 • O2sat: 85 • Bicarb: 24 pH: 7.35 PaO2: 80 PaCO2: 50 O2sat: 85% Bicarb: 24 Question 8 Not yet graded / 1 pts Exercise 2 - Question 6 How would you interpret the results documented in questions 4 and 5? Is the acid-base imbalance compensated or uncompensated (fully or partially)? Explain your answer. Your Answer: Uncompensated respiratory acidosis Monday: Partially compensated respiratory acidosis. The pH is lower than normal (7.35- 7.45), denoting acidosis. The PaCO2 is slightly above normal (35-45), also denoting acidosis. The bicarb is within normal limits (21-28); it takes 24-48 hours for the renal system to begin to compensate for acidosis. Wednesday: Fully compensated respiratory acidosis. The pH is at the lower limit of normal, but the PaCO2 is increased with the bicarb remaining within normal limits. It is fully compensated because the pH is within normal limits. Question 9 Not yet graded / 1 pts Exercise 2 - Question 7 Based on the acute aspect of Jacquline Catanazaro’s respiratory difficulties, what lines of defense would you expect to be working to compensate for her respiratory acidosis? Your Answer: second Because this is an acute respiratory problem, the chemical/protein buffer system (first line of defense) should be responding to bind to the extra hydrogen ions and increase the serum pH. The third line of defense, the renal system, will take 24-48 hours to respond to and begin compensation for the acidosis. Question 10 Not yet graded / 1 pts Exercise 2 - Question 8 If the patient’s electrolyte results were available, what might you expect her potassium levels to be? Provide a rationale for your answer. (Hint: See Chapter 12 in your textbook.) Your Answer: Elevated. Acidosis causes an extracellular shift of Potassium The potassium may be elevated. In acidosis, the extracellular hydrogen ion content increases, and the hydrogen ions move into the intracellular fluid. To keep the intracellular fluid electrically neutral, an equal number of potassium ions leave the cell, creating a relative hyperkalemia. If the acidosis is chronic, the kidneys have time to compensate for the excess hydrogen and hyperkalemia does not occur. Question 11 Not yet graded / 1 pts Exercise 2 - Question 9 Based on Jacquline Catanazaro’s medical diagnosis, what is the underlying pathophysiologic problem leading to the respiratory acidosis? (Hint: See Chapter 12 in your textbook.) Your Answer: Asthma Airway obstruction—the asthma is causing bronchoconstriction and therefore decreased air movement in and out of the lungs. This decreases gas exchange and causes CO2 retention as well as hypoxia. Question 12 Not yet graded / 1 pts • Click on Return to Room 402. • Click on Patient Care and then Physical Assessment. • Complete a physical assessment for Jacquline Catanazaro by clicking on the body system categories (yellow buttons) and subcategories (green buttons). Exercise 2 - Question 10 Record the findings of your physical assessment below. • Mental status • Musculoskeletal • Cardiovascular • Respiratory • Integumentary Your Answer: • Mental status: Perceptual ability mildly impaired, Agitated and anxious with respiratory distress and expressed concern of safety of therapeutic interventions. • Musculoskeletal: Chest expansion impaired with shallow respirations and complaints of chest tightness, • Cardiovascular: Sinus tachycardia with agitation, • Respiratory: Labored and shallow respiratory effort, Tachypnea, Bilateral breath sounds with crackles in right lower lobes, wheezes present throughout lung fields, Productive cough of white frothy sputum, Substernal retractions and use of neck accessory muscles, Oxygen saturation of 85% in 2 liter flow oxygen via nasal cannula, PEFR of 200. • Integumentary: normal Mental status: Alert and oriented x 3. Perceptual ability slightly impaired. Agitated and anxious. Musculoskeletal: Full range of movement. Moves all extremities equally. Reflexes intact. Cardiovascular: Apical pulse regular. No JVD. S1 and S2 normal. Respiratory: Labored and shallow respiratory effort. Tachypneic. Crackles in right lower lobes, wheezes throughout. Productive cough with white frothy sputum. Substernal retractions and use of neck muscles. Integumentary: Skin warm and moist with flushed color. Question 13 Not yet graded / 1 pts Exercise 2 - Question 11 Are there any clinical manifestations of respiratory acidosis? If so, please describe. If not, how do you explain? Your Answer: respiratory acidosis doesn't typically cause any noticeable symptoms. if it does they are subtle and nonspecific. The reason being is Respiratory acidosis develops over time. the body adapts to the increased acidity. None of the identified key features of acidosis are identified in this patient. The patient is no longer acidotic at the time of this assessment. Question 14 Not yet graded / 1 pts • Click on Take Vital Signs. Exercise 2 - Question 12 What is the patient’s respiratory rate? How does this correlate with her respiratory acidosis? Your Answer: 29, hyperventilation causing increased CO2 due to not breathing in deep enough to gain oxygen and not breathing out long enough to expel the CO2 The exact rate will vary depending on the actual time assessed, but the respiratory rate is elevated in attempt to blow off excess CO2 and normalize pH. Question 15 Not yet graded / 1 pts Exercise 2 - Question 13 If Jacquline Catanazaro’s pH were 7.2, how might her physical assessment differ? Document the expected clinical manifestations of respiratory acidosis below. • Neurologic • Musculoskeletal • Cardiovascular • Respiratory • Integumentary Your Answer: It wouldnt differ too much due to the fact it is still acidosis. If the pH was 7.2 these would be the symptoms: • Neurologic: Confusion, headache, sleepiness, • Musculoskeletal: Chest expansion impaired with shallow respirations and complaints of chest tightness, • Cardiovascular: Tachycardia, • Respiratory: rapid shollow breathing, • Integumentary: Jaundice, Neurologic: Lethargy, confusion, stupor, coma Musculoskeletal: Hyporeflexia, skeletal muscle weakness, flaccid paralysis Cardiovascular: Bradycardia, tall, peaked T waves; widened QRS complexes, prolonged PR interval; heart blocks, hypotension, thready peripheral pulses Respiratory: Variable, ineffective respirations Integumentary: Pale to cyanotic mucous membranes Question 16 Not yet graded / 1 pts • Click on Chart. • Click on 402 for Jacquline Catanazaro’s chart. • Click on Physician’s Orders. Exercise 2 - Question 14 Look at the most recent physician’s orders. What medication is ordered to treat the respiratory acidosis? What is the medication’s underlying mechanism of action to correct the acidosis? (Hint: See Drug Guide.) Your Answer: Beclomethasone inhaler. An adrenocorticosteroid that controls the rate of protein synthesis; depresses migration of polymorphonuclear leukocytes and fibroblasts; prevents or controls inflammation; and reverses capillary permeability. Therapeutic Effect: Inhalation: Inhibits bronchoconstriction, produces smooth muscle relaxation, decreases mucus secretion. Intranasal: Decreases response to seasonal and perennial rhinitis. Albuterol 5 mg via nebulizer x 1 STAT—this is a bronchodilator, which will relieve the airway obstruction caused by the asthma. Dilating the bronchi will increase air movement and gas exchange at the alveolar level, thus increasing CO2 excretion and raising the patient’s pH to normal. Question 17 Not yet graded / 1 pts • Click on Return to Room 402. • Click on Leave the Floor. • Click on Restart the Program. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. • From the Patient List, select Jacquline Catanazaro (Room 402). • Click on Go to Nurses’ Station. • Click on Chart and then on 402. • Click on Laboratory Reports. Scroll down to review the results for Wed 1000. Exercise 2 - Question 15 Look at the ABGs drawn at 1000. Interpret the ABGs. Was the treatment effective? Your Answer: It is compensated now, however she is still in respiratory acidosis. The ABGs are now normal with a pH of 7.40 and a PaCO2 of 40. The medication was effective in increasing air movement and gas exchange. Oxygenation is also improved as demonstrated by an increase in the PaO2 and the oxygen saturation. Question 18 Not yet graded / 1 pts Exercise 3 - Virtual Hospital Activity • This exercise will take approximately 45 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • From the Patient List, select Patricia Newman (Room 406). • Click on Go to Nurses’ Station. • Click on Chart and then on 406. • Click on History and Physical. Exercise 3 - Question 1 Is there anything in Patricia Newman’s history that would put her at risk for an acid-base imbalance? Your Answer: Pneumonia • Emphysema for 12 years • Smoker • Probable pneumonia this admission Question 19 Not yet graded / 1 pts • Click on Laboratory Reports. Exercise 3 - Question 2 Document the results of Patricia Newman's two most recent ABGs (Tuesday at 2300 and Wednesday at 0500) below. Include pH, PaO2, PaCO2, O2 sat, and bicarb. • Tuesday 2300 • Wednesday 0500 Your Answer: Tuesday 2300: pH: 7.35 PaO2: 72 PaCO2: 45 O2 Sat: 93 Bicarb: 25 Wednesday 0500: pH: 7.33 PaO2: 70 PaCO2: 47 O2 Sat: 92 Bicarb: 26 Tuesday 2300 • pH: 7.35 • PaO2: 72 • PaCO2: 45 • O2sat: 93% • Bicarb: 25 Wednesday 0500 • pH: 7.33 • PaO2: 70 • PaCO2: 47 • O2sat: 92% • Bicarb: 26 Question 20 Not yet graded / 1 pts Exercise 3 - Question 3 How would you interpret the results you recorded in the previous table? Is the acid-base imbalance compensated or uncompensated (fully or partially)? Explain your answer. Your Answer: Uncompensated Respiratory Acidosis Tuesday: Normal acid-base balance with hypoxemia. pH is at the lower limit (towards the acidotic side), PaO2 is decreased (normal is 80-100). PaCO2is at the upper limit of normal (towards the acidotic side), as is the bicarbonate level. Wednesday: Partially compensated respiratory acidosis. The pH is decreased (acidotic), and the PaCO2 is elevated (acidotic as well). Although the bicarbonate level is within normal limits (22-28), it is slightly elevated from last evening and demonstrates a partial compensation to maintain pH near normal. Question 21 Not yet graded / 1 pts Exercise 3 - Question 4 Based on the chronic aspect of Patricia Newman’s respiratory difficulties, what lines of defense would you expect to be working to compensate for the respiratory acidosis? Your Answer: Second Because this is a chronic respiratory problem, the first and third lines of defense will be working to maintain the pH in a normal or near normal range. The chemical/protein buffers will respond to acute changes but can only neutralize a finite amount of hydrogen ions. Because Patricia Newman’s emphysema is a chronic condition, the kidneys respond to the elevated PaCO2 levels by excreting more hydrogen ions and resorbing more bicarbonate. In Patricia Newman’s case, although the PaCO2 and bicarbonate levels are within normal limits on Tuesday, the renal system is compensating somewhat for the higher PaCO2 level by keeping the bicarbonate levels equally high. As the pH drops slightly on Wednesday, the kidneys work to retain more bicarbonate. Question 22 Not yet graded / 1 pts Exercise 3 - Question 5 Based on the ABG results, has Patricia Newman’s condition improved or worsened since admission the evening before? Your Answer: Worsened Worsened Question 23 Not yet graded / 1 pts • Click on Nurse's Notes. Exercise 3 - Question 6 Read the notes for Wednesday 0730. Describe the actions taken by the nurse. Are they appropriate or not? Explain your answer. Your Answer: There is no report. so it is not appropriate The nurse reapplied the patient’s nasal cannula after assessing lung sounds and ABG results. These are appropriate actions as long as there was not a significant time delay in applying the oxygen while waiting to review the ABG results. The pulse oximetry itself demonstrated hypoxemia and the need for supplemental O2 for the patient. The ABG results verified the hypoxemia and resultant increase in PaCO2. Question 24 Not yet graded / 1 pts Exercise 3 - Question 7 What additional actions do you think would be appropriate at this time? Your Answer: talk to the doctor about medication for her Pneumonia so her breathing gets better. Patient teaching regarding the need to keep O2 cannula in place. Notify physician of ABG results because the patient is becoming slightly acidotic—the administration of O2 itself may not correct this. Question 25 1 / 1 pts • Click on Laboratory Results. Exercise 3 - Question 8 The patient's serum potassium level is ______ mEq/L. Correct! Correct Answers 3.2 Question 26 Not yet graded / 1 pts • Click on Physician's Orders. Exercise 3 - Question 9 How would you explain the patient’s hypokalemia in relation to respiratory acidosis? (Hint: See the Drug Guide and Chapter 12 in your textbook.) Your Answer: acidosis causes potassium to move from cells to extracellular fluid (plasma) in exchange for hydrogen ions Potassium levels are elevated in patients with acute respiratory acidosis but are normal in patients with chronic respiratory acidosis secondary to renal compensation. With acute acidosis, potassium is exchanged for hydrogen in the blood to decrease pH and maintain electroneutrality. This is not necessary with renal compensation because the 3.2 excess hydrogen ions are excreted. Also, Patricia Newman is on chlorothiazide, a diuretic that causes potassium excretion; this is the reason for the hypokalemia. Question 27 Not yet graded / 1 pts Exercise 3 - Question 10 Based on Patricia Newman’s medical diagnosis, what is the underlying pathophysiologic problem leading to the respiratory acidosis? How does that differ from Jacquline Catanazaro’s problem in the previous exercise of this lesson? (Hint: See Chapter 12 in your textbook.) Your Answer: Pneumonia. it differs because Ms. Catanazaro had asthma while Ms. Newman has Pneumonia Patricia Newman’s problem is twofold: • Reduced alveolar-capillary diffusion: The pathophysiologic changes in the alveoli of a patient with pneumonia impair gas exchange at the alveolar-capillary membranes, causing carbon dioxide retention and acidosis. • Airway obstruction: The pathophysiologic changes of emphysema at the alveolar level prevent adequate air movement, which leads to poor gas exchange as well, particularly causing air-trapping and CO2 retention. Both Jacquline Catanazaro and Patricia Newman have airway obstruction. However, Jacquline Catanazaro’s major problem is getting air movement through constricted bronchials, whereas Patricia Newman’s problem is exhaling air outward. Additionally, the pneumonia is causing reduced diffusion in Patricia Newman, worsening her gas exchange. Question 28 Not yet graded / 1 pts • Click on Return to Nurses' Station. • Click on 406 at the bottom of your screen. • Click on Patient Care and then on Physical Assessment. • Complete a physical assessment for Patricia Newman by clicking on the body categories (yellow buttons) and subcategories (green buttons). • Click on Take Vital Signs. Exercise 3 - Question 11 Record the findings of your physical assessment below. • Mental status • Musculoskeletal • Cardiovascular • Respiratory • Integumentary Your Answer: • Mental status: Mild anxiety level with labored respiratory effort. • Musculoskeletal: Impaired chest expansion with shallow and labored respiratory effort, Strength with mild impairment due to generalized fatigue, Slow and steady gait due to respiratory fatigue. • Cardiovascular: Sinus tachycardia, • Respiratory: Labored and shallow respiratory effort, Bilateral breath sounds with coarse crackles auscultated throughout lung fields, Aeration mildly decreased, Productive cough of thick yellow sputum, Employing some accessory muscles, Exertional dyspnea, Oxygen saturation of 90% in 2 liter flow oxygen via nasal cannula. • Integumentary: Normal Mental status: Awake, alert, and oriented; mild anxiety related to respiratory difficulty Musculoskeletal: Mild weakness due to fatigue, reflexes intact Cardiovascular: Sinus tachycardia; S1 and S2 WNL; no clicks, rubs, or murmurs; +2 peripheral pulses Respiratory: Labored and shallow respirations; rate 31 (answers may vary depending on the actual time assessed); using some accessory muscles; course crackles throughout; expectorating thick yellow sputum Integumentary: Skin warm, dry, and intact Question 29 Not yet graded / 1 pts Exercise 3 - Question 12 Does Patricia Newman demonstrate any clinical manifestations of respiratory acidosis? If so, please describe. If not, explain why not. Your Answer: respiratory acidosis doesn't typically cause any noticeable symptoms. if it does they are subtle and nonspecific. The reason being is Respiratory acidosis develops over time. the body adapts to the increased acidity. No clinical manifestations of respiratory acidosis are evident. Patient is just mildly acidotic at 7.33. At this point, manifestations are at the cellular level. Question 30 Not yet graded / 1 pts Exercise 3 - Question 13 What nursing interventions could you, as a graduate nurse, plan and implement to improve Patricia Newman’s acid-base balance and prevent complications? Your Answer: Keep the patient warm and dry. Encourage the patient to take deep, slow breaths or breathe into a brown paper bag, Monitor vital signs, Monitor ABGs, primarily PaCO2; a value less than 35 mmHg indicates too little CO2. • Monitor ABG levels for decreasing pH level, as appropriate. • Monitor determinants of tissue oxygen delivery (PaO2, SaO2, and Hgb levels) as available. • Monitor for symptoms of respiratory failure (worsening of ABGs, respiratory muscle fatigue). • Monitor work of breathing (use of accessory muscles, respiratory rate, heart rate, diaphoresis). • Provide low-carbohydrate, high-fat diet to reduce CO2 production. • Monitor neurologic status (level of consciousness, confusion). • Maintain O2 delivery as ordered. • Maintain semi-Fowler’s position to increase lung expansion. • Increase fluid intake to liquefy secretions. • Instruct patient in pursed-lip breathing to increase air removal and gas exchange. • Administer medications as ordered (bronchodilators for emphysema, antibiotics for pneumonia). Lesson 22 - Diabetes Mellitus, Part 1 • Due No due date • Points 25 • Questions 25 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 192 minutes 1 out of 25 * * Some questions not yet graded Score for this quiz: 1 out of 25 * Submitted Aug 21 at 11:30am This attempt took 192 minutes. Question 1 Not yet graded / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 20 minutes to complete. Exercise 1 - Question 1 Describe the pathophysiology of diabetes mellitus and the basis for the resulting abnormalities in carbohydrate, protein, and fat metabolism. Your Answer: The basis of the abnormalities in carbohydrate, fat, and protein metabolism in diabetes is deficient action of insulin on target tissues. Deficient insulin action results from inadequate insulin secretion and/or diminished tissue responses to insulin at one or more points in the complex pathways of hormone action. Diabetes mellitus occurs when there is a problem with insulin secretion, insulin action, or both. Insulin is necessary for glucose to enter cells and be used to make energy. The presence of insulin also inhibits the conversion of fats to acids and proteins to glucose. The lack of insulin in diabetes, either from a lack of production or a problem with insulin use at its cell receptor, prevents some cells from using glucose for energy. Without insulin, the body enters a serious state of breaking down body fat and protein. Without insulin, glucose builds up in the blood, causing hyperglycemia. Hyperglycemia leads to fluid and electrolyte imbalances, causing the classic symptoms of diabetes: polyuria, polyphagia, and polydipsia. The dehydration that occurs with hyperglycemia leads to hemoconcentration, hypovolemia, hyperviscosity, hypoperfusion, and hypoxia. The breakdown of fats for energy releases fatty acids, which are converted to ketone bodies, leading to acidosis. The body responds by trying to blow off CO2, resulting in Kussmaul respirations. Hypokalemia or hyperkalemia can occur, depending on the patient’s hydration status, degree of acidosis, and response to treatment. Question 2 Not yet graded / 1 pts Exercise 1 - Question 2 Briefly define and summarize the etiologic differences between type 1 and type 2 diabetes mellitus. Your Answer: People with type 1 diabetes don't produce insulin. You can think of it as not having a key. People with type 2 diabetes don't respond to insulin as well as they should and later in the disease often don't make enough insulin. You can think of this as having a broken key. Type 1 diabetes is an autoimmune disorder in which beta cells are destroyed in a genetically susceptible person. The immune system fails to recognize normal body cells as "self" and takes destructive actions against them. Immune system cells, mediators, and antibodies attack and destroy insulin-secreting cells in the islets. Patients with tissue types HLA-DR or HLA-DQ are at increased risk for type 1 diabetes. Certain viral infections, such as mumps and coxsackievirus infection, appear to trigger autoimmune destruction of the pancreatic beta cells. Type 2 diabetes is a progressive disorder in which the pancreas makes less insulin over time. The specific causes of type 2 DM are not known, although insulin resistance and beta-cell failure have many genetic and nongenetic causes. Obesity and/or the presence of metabolic syndrome increases a patient’s risk of developing type 2 diabetes. Heredity also plays a major role in the development of type 2 diabetes. Question 3 Not yet graded / 1 pts Exercise 1 - Question 3 Provide the distinguishing features of type 1 diabetes mellitus (DM) for each of the features below. • Former names • Age at onset • Symptoms • Antigen patterns • Antibodies • Endogenous insulin and C-peptides • Nutritional status • Inheritance • Insulin • Medical nutrition therapy Your Answer: • Former names: Juvenile diabetes or insulin-dependent diabetes • Age at onset: Although type 1 diabetes can appear at any age, it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old, and the second is in children between 10 and 14 years old. • Symptoms: Increased thirst, frequent urination, unintended weight loss, irritability and other mood changes, blurred vision • Antigen patterns: The list of target antigens in this disease is ever increasing and it is conceivable that additional islet autoantigens, possibly including pivotal β- cell targets, remain to be discovered. • Antibodies: 4 autoantibodies are markers of beta cell autoimmunity in type 1 diabetes: islet cell antibodies: ICA, against cytoplasmic proteins in the beta cell, antibodies to glutamic acid decarboxylase: GAD-65, insulin autoantibodies: IAA, and IA-2A, to protein tyrosine phosphatase. • Endogenous insulin and C-peptides: A C-peptide test is often used to help tell the difference between type 1 and type 2 diabetes. With type 1 diabetes, your pancreas makes little to no insulin, and little or no C-peptide. With type 2 diabetes, the body makes insulin, but doesn't use it well. This can cause C-peptide levels to be higher than normal. • Nutritional status: Most people with diabetes can control their blood sugar by limiting carbohydrate servings to 2-4 per meal and 1-2 per snack. A delicate balance of carbohydrate intake, insulin, and physical activity is necessary for the best blood sugar (glucose) levels. • Inheritance: Diabetes mellitus type 1 itself is not inherited , but a predisposition to developing the condition can run in families. While some people with a family history of DM1 may be at an increased risk, most will not have the condition. • Insulin: People who have type 1 diabetes must take insulin as part of their treatment. Because their bodies can't make insulin anymore, they need to get the right amount to keep their blood sugar levels in a healthy range. The only way to get insulin into the body now is by injection with a needle or with an insulin pump. • Medical nutrition therapy: The nutritional goals for people with type 1 diabetes are to maintain blood glucose concentrations in a physiologically normal range as possible, by coordinating diet and physical activity patterns and insulin therapy, minimizing episodes of hypoglycemia, maintaining optimal blood pressure and lipid levels Former names—Juvenile-onset diabetes; ketosis-prone diabetes; insulin-dependent diabetes mellitus (IDDM) Age at onset—Usually under age 30, occurs at any age Symptoms—Abrupt onset, thirst, hunger, increased urine output, weight loss Antigen patterns—HLA-DR, HLA-DQ Antibodies—Islet cell antibodies (ICAs) present at diagnosis Endogenous insulin—None Nutritional status—Usually nonobese Inheritance—Complex Insulin—All are dependent on insulin Medical nutrition therapy—Mandatory Question 4 Not yet graded / 1 pts Exercise 1 - Question 4 Provide the distinguishing features of type 2 diabetes mellitus (DM) for each of the features below. • Former names • Age at onset • Symptoms • Antigen patterns • Antibodies • Endogenous insulin and C-peptides • Nutritional status • Inheritance • Insulin • Medical nutrition therapy Your Answer: • Former names: Adult onset diabetes • Age at onset: 45 years • Symptoms: Increased thirst, frequent urination, unintended weight loss, blurred vision, frequent infections • Antigen patterns: The list of target antigens in this disease is ever increasing and it is conceivable that additional islet autoantigens, possibly including pivotal β- cell targets, remain to be discovered. • Antibodies: With type 2 diabetes, the autoantibodies are typically absent. • Endogenous insulin and C-peptides: A C-peptide test is often used to help tell the difference between type 1 and type 2 diabetes. With type 1 diabetes, your pancreas makes little to no insulin, and little or no C-peptide. With type 2 diabetes, the body makes insulin, but doesn't use it well. This can cause C-peptide levels to be higher than normal. • Nutritional status: There it is used for energy. Insulin is produced by the pancreas. In someone who has type 2 diabetes, the pancreas doesn't make enough insulin or the body's cells can't use insulin properly (called insulin resistance). This causes glucose to build up in your blood instead of moving into the cells. • Inheritance: Type 2 is passed down from mothers and fathers to their children. Not everyone who inherits the genes will develop it, but if you have the genes for type 2 diabetes, you've got a greater chance of developing it • Insulin: People with type 2 diabetesmay requireinsulinwhen their meal plan, weight loss, exercise and antidiabetic drugs do not achieve targeted blood glucose (sugar) levels • Medical nutrition therapy: nutrition-based treatmentprovided by a registered dietitian nutritionist. It includes a nutritiondiagnosisas well as therapeutic and counseling services to help manage diabetes. Former names—Adult-onset diabetes Age at onset—May occur at any age in adults Symptoms—Frequently none; thirst, fatigue, blurred vision, vascular or neural complications Antigen patterns—None Antibodies—None Endogenous insulin—Low, normal, or high and C-peptides Nutritional status—60% to 80% obese Inheritance—Autosomal-dominant, multifactorial Insulin—Required for 20% to 30% Medical nutrition therapy—Mandatory Question 5 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 45 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • From the Patient List, select Harry George (Room 401). • Click on Go to Nurses’ Station. • Click on Chart and then on 401. • Click on History and Physical. Exercise 2 - Question 1 What risk factors for diabetes are noted in Harry George’s history? Your Answer: Alcoholism, nicotine dependence. Maternal grandmother has diabetes Hypertension Question 6 Not yet graded / 1 pts Exercise 2 - Question 2 Describe the history of his present illness. Your Answer: Patient has had problems with infection and swelling of left foot off and on since he broke foot approximately 4 years ago in a motorcycle accident. At that time he had fractures of metatarsals and left malleolus. During admission for treatment it was discovered he had type 2 Diabetes Mellitus. Alcohol abuse developed after this accident. He has never been told he had a bone infection. He has smoked 2 packs per day since age 18. Harry George has had problems with infection and swelling of left foot off and on for last 4 years since he broke his foot in a motorcycle accident. Type 2 diabetes was diagnosed at that time. He has a current history of alcohol abuse and smoking. Question 7 Not yet graded / 1 pts Exercise 2 - Question 3 What is the relationship between the infection in Harry George’s foot and his diabetes mellitus? Your Answer: because of his diabetes his body is less capable of fighting off infections so his foot has become infected. Hyperglycemia and vascular changes from diabetes decrease WBC activity, inhibit gas exchange in the tissue, and promote growth of microorganisms. Question 8 1 / 1 pts • Click on Laboratory Reports. Exercise 2 - Question 4 Harry George's blood glucose level on admission was ______ mg/dL. Correct! Correct Answers 380 Question 9 Not yet graded / 1 pts Exercise 2 - Question 5 What abnormalities in his urinalysis results can be attributed to diabetes? Explain the relationship. Your Answer: dark amber color, glucose 4+, moderate ketones 4+ glucose in urine—caused by hyperglycemia, glucose spilling into urine Moderate ketones in urine—related to the breakdown of fatty acids for energy because cells cannot use glucose secondary to diabetes and patient not taking his oral hypoglycemic agent 6 mg protein in urine—may indicate microvascular changes in the kidney Turbid urine with few white blood cells and leukocytes—possible urinary tract infection (UTI); patient is at increased risk for UTI secondary to hyperglycemia Question 10 Not yet graded / 1 pts • Click on Emergency Department. Exercise 2 - Question 6 What factor in Harry George’s recent history most likely contributed to his hyperglycemia? (Hint: Read the emergency department physician’s notes for 1345.) 380 Your Answer: after accident that took him out for a while he lost his job and family which caused him to start drinking and he became homeless Harry George ran out of glyburide about 1 week ago. Question 11 Not yet graded / 1 pts • Click on Nursing Admission. Exercise 2 - Question 7 Listed below are clinical manifestations of diabetes mellitus identified in the textbook. For each manifestation, indicate (Yes or No) whether each manifestation is usually present in type 2 diabetes. Then indicate (with Yes or No) whether it is usually present in type 2 diabetes. • Polyuria • Polydipsia • Polyphagia • Visual blurring • Fatigue • Weight loss • Chronic complications Your Answer: • Polyuria: yes • Polydipsia: yes • Polyphagia: yes • Visual blurring: yes • Fatigue: no • Weight loss: yes • Chronic complications: no Polyuria—Yes Polydipsia—No Polyphagia—No Visual blurring—Yes Fatigue—No Weight loss—No Chronic complications—Yes Question 12 Not yet graded / 1 pts Exercise 2 - Question 8 To what extent does Harry George fit the typical picture of a patient with type 2 diabetes mellitus? Your Answer: i believe he is a little worse off then the "typical" picture due to him being homeless. Harry George is not exhibiting the common symptoms of hyperglycemia such as polyuria and polyphagia. He is not obese either, but that may be more related to his homeless situation and alcohol abuse. He does, however, demonstrate a chronic complication as manifested by his poor wound healing and infection in his leg. Question 13 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on 401 to enter Harry George’s room. • Click on Patient Care and then on Nurse-Client Interactions. • Select and view the video titled 0735: Symptom Management. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and on Nurse-Client Interactions to refresh the screen.) Exercise 2 - Question 9 What does Harry George tell the nurse about his appetite? Your Answer: he needs/wants a drink and a smoke. Did not eat much of breakfast; would like to have a smoke and some alcohol to take away the pain Question 14 Not yet graded / 1 pts Exercise 2 - Question 10 What diet has been ordered for the patient? (Hint: Review his chart.) Your Answer: 1800 calorie ADA diet 1800-calorie ADA diet Question 15 Not yet graded / 1 pts Exercise 2 - Question 11 Describe the principles of this diet. Your Answer: ADA doesn't specify recommended amounts of carbohydrates, protein, or fats. This is because what works for one person may not work for another person. 1800 calories should be consumed daily. Recommended amounts of carbohydrates, fats, and proteins are individualized and based on food preferences. General guidelines include avoiding empty calories, consuming 25 grams of fiber daily, and limiting trans fats, saturated fats, and cholesterol. Question 16 Not yet graded / 1 pts Exercise 2 - Question 12 How might the patient’s alcohol intake affect his blood glucose levels? Your Answer: the blood glucose level increases with the sugar in the alcohol then drops due to the alcohol Blood glucose levels are not affected by moderate use of alcohol. However, alcohol inhibits liver glucose production and is most likely to cause alcohol-related hypoglycemia when ingested without food. Harry George is apparently consuming large amounts of alcohol and small amounts of food. Thus, he is at high risk for alcoholrelated hypoglycemia. Question 17 Not yet graded / 1 pts Exercise 3 - Virtual Hospital Activity • This exercise will take approximately 40 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 2. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then on Restart the Program to get to the sign-in window.) • From the Patient List, select Harry George (Room 401). • Click on Go to Nurses’ Station. • Click on Chart and then on 401. • Click on Physician's Orders. Exercise 3 - Question 1 What test is ordered that can be used to determine Harry George’s control of diabetes mellitus? Describe the purpose of this test. How often should it be done? Your Answer: HgbA1c/ hemoglobin A1c (HbA1c) measures the amount of blood sugar (glucose) attached to hemoglobin. Hemoglobin is the part of your red blood cells that carries oxygen from your lungs to the rest of your body/ every 3-6 months HgbA1c. This test demonstrates the patient’s average serum glucose levels over the past 120 days. HgbA1c testing is recommended at least twice yearly in patients who have stable blood glucose control. Quarterly assessment is recommended for patients whose therapy has changed or who are not meeting the glycemic controls. Question 18 Not yet graded / 1 pts • Click on Laboratory Reports. Exercise 3 - Question 2 What were the results of this test for Harry George? Based on these results, evaluate and explain how well his diabetes is controlled. Your Answer: 9.0/ this shows that his diabetes is not controlled at all. Normal HbA1c is below 5.7. Prediabetes is between 5.7-6.4. diabetes is 6.5 or higher. 9.0%; normal HgbA1c results are 4%-6%; levels above 8% indicate poor diabetic control. Therefore Harry George’s diabetes is not well controlled. Question 19 Not yet graded / 1 pts Exercise 3 - Question 3 What implication does Harry George’s level of glycemic control have for his future? Your Answer: he wont have a future if he doesnt get it under control. His body cant withstand diabetes unchecked Lack of glycemic control increases Harry George’s risk for developing long-term complications such as nephropathy, neuropathy, retinopathy, cardiovascular disease (including myocardial infarction), and cerebrovascular disease. Question 20 Not yet graded / 1 pts • Click on Return to Nurses’ Station. • Click on 401 at the bottom of the screen. • Click on Patient Care and then on Physical Assessment. Exercise 3 - Question 4 Perform a head-to-toe assessment on Harry George, focusing on the areas listed below. Document any abnormal results. • Head & Neck • Chest • Back & Spine • Upper Extremities • Abdomen • Pelvic • Lower Extremities Your Answer: • Head & Neck: gums mildly swollen, large amount of cerumen in ear canal, Intermittent agitation and combativeness with expressed frustration of high pain level and limited mobility. • Chest: Few small nevi over chest surface, • Upper Extremities: Capillary refill sluggish at 4 seconds, Intermittent mild to moderate tremors. • Lower Extremities: Skin of left leg erythematoedematous from toes to mid-calf, Open lesion 2-3 cm in size on left ankle draining serous fluid, Impaired range of motion, sensation, and movement in left leg, Capillary refill sluggish at 4 seconds, Posterior tibialis and dorsalis pedis pulses diminished in left foot, 1+ to Doppler, Sensation and strength in left leg impaired with pain response to touch. Head & Neck • Hair dry and flaky; skin warm and moist with diaphoresis • Chipped front teeth and dental caries • Intermittent agitation and combativeness Chest • Skin warm and moist with diaphoresis • Few small nevi over chest area • Nonproductive cough Back & Spine • Skin warm and moist • Assessment within normal limits Upper Extremities • Nails thick and brittle • Capillary refill sluggish at 4 seconds • Intermittent mild tremors Abdomen • Mild distension Pelvic • Palpable bilateral inguinal lymph nodes • Foley indwelling catheter in place Lower Extremities • Skin on right leg warm, dry, erythematous over anterior tibial surface, and intact without lesions • Skin of left leg erythematous from toes to mid-calf • Open lesion 2-3 cm in size on left ankle draining serous liquid • Left lower extremity: impaired ROM, sensation, and movement; painful to touch; capillary refill sluggish at 4 seconds; left posterior tibial and dorsalis pedis pulses 1+ to Doppler; intermittent mild to moderate tremors of left lower extremity Question 21 Not yet graded / 1 pts • Click on EPR and Login. • Choose 401 from the Patient drop-down menu and Neurologic from the Category drop-down menu. Exercise 3 - Question 5 Below, document any abnormal information obtained from the neurologic assessment completed on Monday at 1835. Your Answer: left foot numbness, Left foot reddened and edematous--entire foot up to midcalf. Open area 2 cm over left malleolus with serous drainage. Wrapped in sterile gauze and elevated on two pillows. Left foot numbness Question 22 Not yet graded / 1 pts • Select Cardiovascular from the Category drop-down menu. Exercise 3 - Question 6 Below, document any abnormal information obtained from the cardiovascular assessment completed on Monday at 1835. Your Answer: left Posterior Tibialis doppler 1 left Dorsalis Pedis doppler 1 cap refill hands sluggish cap refill feet sluggish left foot pitting edema 2+ Capillary refill in hands sluggish, also sluggish in feet bilaterally, 2+ pitting edema in left foot Question 23 Not yet graded / 1 pts Exercise 3 - Question 7 Describe the following potential long-term complications for diabetes mellitus. • Cardiovascular disease • Cerebrovascular disease • Retinopathy (nonproliferative and proliferative) • Peripheral vascular disease • Neuropathy • Nephropathy • Erectile dysfunction Your Answer: • Cardiovascular disease: generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack, chest pain (angina) or stroke • Cerebrovascular disease: refers to a group of conditions, diseases, and disorders that affect the blood vessels and blood supply to the brain. If a blockage, malformation, or hemorrhage prevents the brain cells from getting enough oxygen, brain damage can result. • Retinopathy (nonproliferative and proliferative): disease of the retina which results in impairment or loss of vision • Peripheral vascular disease: a blood circulation disorder that causes the blood vessels outside of your heart and brain to narrow, block, or spasm. • Neuropathy: disease or dysfunction of one or more peripheral nerves, typically causing numbness or weakness. • Nephropathy: disease of the kidneys caused by damage to the small blood vessels or to the units in the kidneys that clean the blood • Erectile dysfunction: inability of a man to maintain an erection sufficient for satisfying sexual activity. Cardiovascular disease Patients with diabetes, those with prediabetes, and those with metabolic syndrome are at increased risk for CVD. This excess risk affects women to a greater degree than men and is influenced by the patient’s ethnic group. Cerebrovascular disease The risk for stroke is 2 to 4 times higher in people with diabetes mellitus compared with those who do not have the disease. Diabetes also increases the likelihood of severe carotid atherosclerosis. Patients with diabetes mellitus are likely to suffer irreversible brain damage with carotid emboli that produce only transient ischemic attacks in people without diabetes mellitus. Elevated blood glucose levels at the time of the stroke may lead to greater brain injury and higher mortality. In addition, chronic hyperglycemia with microvascular disease may contribute to neuronal damage, brain atrophy, and cognitive impairment. These problems are more frequent and more severe in patients who have longer-duration diabetes mellitus and an increase in the complications of neuropathy and retinopathy. Retinopathy (nonproliferative and proliferative) Legal blindness (a corrected visual acuity of 20/200 or less) is 25 times more common in patients with diabetes. Diabetic retinopathy (DR) is strongly related to the duration of diabetes. Proliferative retinopathy leads to blurry vision, vision loss, early onset of cataracts, and open-angle glaucoma. Nonproliferative retinopathy causes structural problems that lead to poor retinal circulation, edema, hard fatty deposits in eye, and hemorrhages. Proliferative retinopathy causes new growth of fragile blood vessels, which also lead to retinal hemorrhage. Blindness is more likely to occur with proliferative retinopathy than with nonproliferative retinopathy. Peripheral vascular disease A macrovascular complication of diabetes leading to poor tissue circulation and cell death. Diabetes is the leading cause of nontraumatic amputations. Neuropathy A progressive degeneration of nerves that results in loss of nerve function. Damage to sensory nerve fibers results in either pain or loss of sensation. Damage to motor nerve fibers results in muscle weakness. Damage to nerve fibers in the autonomic nervous system can cause dysfunction in every part of the body. Nephropathy A pathologic change in the kidney that reduces kidney function and leads to renal failure. Diabetes mellitus is the leading cause of end-stage kidney disease and kidney failure in the United States. The earliest clinical sign of nephropathy is microalbuminuria. Erectile dysfunction Defined as the inability to achieve or maintain a penile erection sufficient for satisfactory sexual performance. Occurs at a higher rate and an earlier age among men with diabetes mellitus as compared with the general population. Related to poor blood glucose control, obesity, hypertension, heavy cigarette smoking, and the presence of other chronic vascular complications. Question 24 Not yet graded / 1 pts Exercise 3 - Question 8 Does Harry George exhibit signs or symptoms that would alert you to the possibility of any of the long-term complications noted in question 7? If so, explain. Your Answer: neuropathy due to the damage to his leg Harry George is demonstrating the effects of peripheral vascular disease as evidenced by sluggish capillary refill and diminished pulse strength in the left lower extremity. The skin on the right leg is also demonstrating poor circulation in that it is dry and erythematous over the anterior tibial surface, a clinical manifestation of peripheral vascular disease. He is also demonstrating potential diabetic nephropathy as evidenced by proteinuria. The left foot numbness may also be a sign of peripheral neuropathy. Question 25 Not yet graded / 1 pts Exercise 3 - Question 9 What interventions, including patient teaching, would you plan to offer Harry George for prevention of injury secondary to reduced sensation in his left foot? (Hint: See Chart 64- 6 in your textbook.) Your Answer: constantly irrigate wound and teach proper wound care at home and the importance of taking medication on time everyday. Protect feet and other body areas where sensation is reduced (e.g., do not walk around in bare feet or stocking feet; always wear shoes with a protective sole). Be sure shoes are long enough and wide enough to prevent formation of sores or blisters. Provide a long break-in period for new shoes; do not wear new shoes for longer than 2 hours at a time. Avoid pointed-toe shoes and shoes with heels higher than 2 inches. Inspect your feet daily (with a mirror) for open areas or redness. Avoid extremes of temperature; wear warm clothing in the winter, especially over hands, feet, and ears. Test water temperature with a thermometer when washing dishes or bathing. Use warm water rather than hot water (less than 110° F). Quiz Score: 1 out of 25 Previous Next Submission Details: Lesson 04 - Postoperative Assessment • Due No due date • Points 27 • Questions 27 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 64 minutes 4.67 out of 27 * * Some questions not yet graded Score for this quiz: 4.67 out of 27 * Submitted Sep 10 at 2:52pm This attempt took 64 minutes. Question 1 0.5 / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 15 minutes to complete. Exercise 1 - Question 1 and are two other names for degenerative joint disease. Answer 1: Correct!Osteoarthritis Answer 2: You Answeredwear-and-tear arthritis Correct Answer hypertrophic arthritis osteoarthritis w ear-and-tear ar Question 2 0.67 / 1 pts Exercise 1 - Question 2 Which populations are at increased risk for developing degenerative joint disease? Select all that apply. Small-framed patients Correct! Obese patients Correct! Older patients Correct! Patients employed in occupations with activities that place joints in stressful positions You Answered Women of childbearing age Patients with diabetes Question 3 0.5 / 1 pts Exercise 1 - Question 3 The nurse is reviewing the medical record of a patient suspected of having degenerative joint disease. Which findings are considered consistent with degenerative joint disease? Select all that apply. Symmetrical joint discomfort You Answered Family history of degenerative joint disease Correct! Changes in joint function noted in hands and hips Correct! Localized pain and stiffness in affected joints Warmth over affected joints Question 4 Not yet graded / 1 pts Exercise 1 - Question 4 What are some management techniques for degenerative joint disease? Your Answer: Regular exercise is important to keep joints flexible and improve muscle strength, reducing the burden on affected joints. Initial work with a physical therapist can reveal specific exercises that build strength and increase your joints' range of motion. Medication therapy includes oral analgesics and nonsteroidal antiinflammatory drugs. Exercise is also prescribed. Question 5 Not yet graded / 1 pts Exercise 1 - Question 5 What is arthroscopy? Your Answer: the use of an arthroscope to diagnose an injury to or disease of a joint or to perform minor surgery on a joint. Arthroscopy is an endoscopic examination used to visualize the joints. It can also be used in the treatment of musculoskeletal disorders. It allows drainage of fluid from the joint cavity and removal of damaged tissue or foreign bodies from the joint capsule. Question 6 0 / 1 pts Exercise 1 - Question 6 The nurse is reviewing the laboratory results for the patient with suspected degenerative joint disorder. What results support this potential diagnosis? Select all that apply. Correct Answer Erythrocyte sedimentation rate 12 mm/hr You Answered Rheumatoid factor (RF) 65 units/mL You Answered Uric acid 10.1 mg/dL Correct Answer Calcium 10 mg/dL Correct! Alkaline phosphatase 43 units/mL Question 7 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 45 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then Restart the Program to get to the sign-in window.) • From the Patient List, select Clarence Hughes (Room 404). • Click Get Report and read the Clinical Report. • Click Go to Nurses' Station and then 404 to enter Clarence Hughes' room. • Read the Initial Observations. • Click Chart and then 404 to view Clarence Hughes' chart. • Click the History and Physical tab and review the information given. Exercise 2 - Question 1 What signs and symptoms of degenerative joint disease has Clarence Hughes experienced? Your Answer: Clarence Hughes has a several year history of degenerative joint disease and osteoarthritis causing chronic pain in both knees that has become progressively worse over time. The pain in the left knee has reached a point where it is affecting mobility and overall quality of life. He had a prior arthroscopy 6 years ago which showed arthritic changes at that time. His condition has progressed to the point that another arthroscopy is unlikely to help him. The symptoms he is currently experiencing are severe enough to justify a left total knee replacement. Pain and increased immobility Question 8 Not yet graded / 1 pts Exercise 2 - Question 2 What other methods of disease management did Clarence Hughes try before he had surgery? Your Answer: Arthroscopy 6 years ago and taking Celecoxib to help alleviate pain. He underwent arthroscopy 6 years ago. Question 9 1 / 1 pts • Click Return to Room 404. • Click Clinical Alerts and read the information given. • Now click Patient Care and complete a head-to-toe assessment. Exercise 2 - Question 3 Indicate whether the following statement is true or false. Findings from Clarence Hughes' physical assessment warrant physician notification. True Correct! False Question 10 Not yet graded / 1 pts Exercise 2 - Question 4 What are the two most important priorities for care at this time? Your Answer: Pain management and infection control Management of pain and constipation Question 11 Not yet graded / 1 pts Exercise 2 - Question 5 Which are the two priority nursing diagnoses for this patient? Your Answer: Acute pain related to inflammation of the synovium and irritation of the nerve endings. Activity intolerance related to joint pain. Note: Answers will vary. Potential for constipation related to postoperative immobility Alteration in comfort related to surgical procedure Question 12 Not yet graded / 1 pts Exercise 2 - Question 6 Why are these issues most important to the successful management of Clarence Hughes' care? Your Answer: because the pain is causing potential health issues we need to address immediately. Answers will vary, depending on your answer to question 5. However, you should have noted that Clarence Hughes is reporting a pain level of 8 on a 10-point scale. This level of pain impairs his ability to focus on getting better. It is Wednesday, and he has not had a bowel movement since Saturday (over 5 days ago). Furthermore, constipation is a specific concern of his. Question 13 Not yet graded / 1 pts Exercise 2 - Question 7 Are there any abnormal findings in the abdominal assessment? Your Answer: No No, bowel sounds are present in all four quadrants. There no palpable tenderness or masses. Question 14 Not yet graded / 1 pts • Click MAR and then tab 404 to review Clarence Hughes' record. Exercise 2 - Question 8 What medication options are available to manage Clarence Hughes' pain? Your Answer: Celecoxib, OxyCODONE with acetaminophen Oxycodone with acetaminophen, 1-2 tablets PO every 4-6 hours Question 15 Not yet graded / 1 pts • Click Return to Room 404. • Click the Drug icon and review the pain medication(s) prescribed for Clarence Hughes. Exercise 2 - Question 9 Does Clarence Hughes have any contraindications for the pain medication(s) you identified in question 8? Your Answer: OxyCODONE: He has medication for GI obstruction so that is a possible complication No Question 16 Not yet graded / 1 pts Exercise 2 - Question 10 What side effects can be anticipated with administration of the medication(s)? Your Answer: OxyCODONE: Drowsiness, dizziness, hypotension, anorexia, Confusion, diaphoresis, facial flushing, urinary retention, constipation, dry mouth, nausea, vomiting, headache, Tolerance to analgesic effect and physical dependence may occur with repeated use. Celecoxib: Fatigue, anxiety, depression, nervousness, paresthesia, dysuria, tachycardia, CHF, GI bleeding, nephrotoxicity, hematuria, oliguria, azotemia, abdominal pain, angina, dysrhythmias, hypertension, fluid retention, nausea, anorexia, vomiting, constipation, dry mouth, diverticulitis, gastritis, gastroenteritis, hemorrhoids, hiatal hernia, stomatitis, cystitis, UTI, epistaxis, bruising, anemia, purpura, rash, pruritus, sweating, erythema, petechiae, photosensitivity, alopecia, pharyngitis, shortness of breath, pneumonia, coughing. Drowsiness, dry mouth, hypotension, and anorexia Question 17 Not yet graded / 1 pts Exercise 2 - Question 11 Discuss any safety precautions that may need to be instituted with use of the medication(s). Your Answer: Patient teaching for OxyCODONE: Tell the patient that oxycodone may cause drowsiness and dry mouth, Warn the patient to avoid performing tasks that require mental alertness or motor skills, Urge the patient to avoid alcohol while taking oxycodone, Caution the patient that oxycodone may be habit-forming, Instruct the patient not to break, chew, or crush controlled-release tablets. Patient teaching for Celecoxib: Discuss specific use of drug and side effects with patient as it relates to treatment, Patient may experience headache, dyspepsia, pyrosis, nausea, or diarrhea, Have patient report immediately to prescriber edema or pain of hands or feet, angina, strength differences from one side to another, significant weight gain, melena, hematuria, ecchymosis, jaundice, inability to eat, fatigue, or rash, Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Use the side rails on his bed. Ambulate with assistance only. Assess frequently for toileting needs. Keep call light within reach. Question 18 Not yet graded / 1 pts Exercise 2 - Question 12 Discuss any special monitoring that will be needed with the administration of the medication(s). Your Answer: OxyCODONE: Palpate the patient's bladder for urine retention. Monitor the patient's pattern of daily bowel activity and stool consistency, Initiate deep breathing and coughing exercises, particularly in patients with impaired pulmonary function, Monitor the patient's blood pressure (B/P), mental status, respiratory rate, and pain relief. Celecoxib: Evaluate the patient for therapeutic response, decreased stiffness, swelling, and tenderness, improved grip strength, increased joint mobility, and pain relief. Monitor his vital signs. If his respirations are less than 12/minute, hold dose. Question 19 Not yet graded / 1 pts Exercise 2 - Question 13 What regularly scheduled medication has been ordered to reduce the patient's constipation? What is the mechanism of action for this medication? Your Answer: Docusate Sodium: A bulk-producing laxative that decreases surface film tension by mixing liquid and bowel docusate contents. Therapeutic Effect: Increases infiltration of liquid to form a softer stool. Docusate sodium 100 mg daily has been ordered. It is a stool softener. Question 20 Not yet graded / 1 pts Exercise 2 - Question 14 What prn medications have been ordered to reduce constipation? How do these medications work? Your Answer: Magnesium hydroxide:Osmotic effect primarily in small intestine. Draws water into intestinal lumen. Therapeutic Effect: Produces distention; promotes peristalsis, bowel evacuation. Bisacodyl Suppository: A gastrointestinal (GI) stimulant that has a direct effect on colonic smooth muscle by stimulating the intramural nerve plexi. Therapeutic Effect:Promotes fluid and ion accumulation in colon to increase peristalsis, promote a laxative effect. Milk of magnesia and bisacodyl suppositories have been ordered. These are laxatives that promote peristalsis. Question 21 Not yet graded / 1 pts • Click Return to Room 404. • Click Chart and then 404 to view Clarence Hughes' chart. • Click the Physician's Notes tab. Exercise 2 - Question 15 What are the physician's plans concerning Clarence Hughes' discharge? Your Answer: CPM goal of 75 degrees, continue postop recovery and rehabilitation. Plan to discharge tomorrow The physician intends to discharge him tomorrow. Question 22 Not yet graded / 1 pts • Click the Consultations tab. Exercise 2 - Question 16 What consultations have been ordered for Clarence Hughes? What is the purpose of these consultations? Your Answer: PT/OT: to get him up and moving and get back most if not all range of motion and strength back, Occupational therapy and physical therapy consults have been ordered. These consults will prepare him for mobility tasks after discharge. They will also cover appliance use. Question 23 Not yet graded / 1 pts • Click the Patient Education tab. Exercise 2 - Question 17 What are Clarence Hughes' educational needs? Your Answer: • Ambulation, home maintenance • Enoxaparin prophylactic therapy • Incision care Ambulation, home maintenance Medication therapy Incision care Question 24 Not yet graded / 1 pts Exercise 2 - Question 18 List five benefits of early postoperative ambulation. (Hint: See page 51 in your textbook.) Your Answer: Walking promotes blood flow of oxygen throughout the body while maintaining normal breathing functions. Ambulation stimulates circulation which can help stop the development of stroke-causing blood clots. Walking improves blood flow which aids in quicker wound healing. Failure to walk may cause increased constipation and gas pain and weakness, and puts you at a higher risk for infections, blood clots and lung problems such as pneumonia. Increased rate and depth of breathing Increased circulation Increased urinary elimination Increased metabolism Increased peristalsis Question 25 1 / 1 pts • Click on the Physician's Orders tab. Exercise 2 - Question 19 When does the surgeon request that physical therapy begin? Physical therapy will begin the day of surgery. Correct! Physical therapy will begin the day after surgery. Physical therapy will begin on a limited basis 3 to 5 days after surgery. Physical therapy will be prescribed to start at the time of discharge. Question 26 Not yet graded / 1 pts Exercise 2 - Question 20 What are the physician orders and expectations for use of the continuous passive motion (CPM) machine? Your Answer: Continuous passive motion (CPM) machine 6 hours per day to L knee with the following goals: 45 degrees postop day 1 60 degrees postop day 2 75 degrees postop day 3 90 degrees postop day 4 Notify MD if unable to meet goals as specified. Continuous passive motion (CPM) machine 6 hours per day to L knee with the following goals: 45 degrees postop day 1, 60 degrees postop day 2, 75 degrees postop day 3, 90 degrees postop day 4. Notify MD if unable to meet goals as specified. Question 27 1 / 1 pts Exercise 2 - Question 21 Clarence Hughes' physician has ordered use of a CPM machine. Which term best describes the action of this device? (Hint: Review page 134 in your textbook.) Correct! Passive flexion Active flexion Passive extension Active extension Quiz Score: 4.67 out of 27 Previous Next Submission Details: Lesson 09 - Care of the Patient Experiencing Exacerbation of an Asthmatic Condition • Due No due date • Points 27 • Questions 27 • Time Limit None Attempt History Attempt Time Score LATEST Attempt 1 58 minutes 5.08 out of 27 * * Some questions not yet graded Score for this quiz: 5.08 out of 27 * Submitted Sep 11 at 8:33am This attempt took 58 minutes. Question 1 Not yet graded / 1 pts Exercise 1 - Writing Activity • This exercise will take approximately 15 minutes to complete. Exercise 1 - Question 1 What is asthma? Your Answer: a respiratory condition marked by spasms in the bronchi of the lungs, causing difficulty in breathing. It usually results from an allergic reaction or other forms of hypersensitivity. Asthma involves episodes of increased tracheal/bronchial responsiveness to various stimuli. This reaction is also accompanied by narrowing of the airways. Question 2 0 / 1 pts Exercise 1 - Question 2 Which statement concerning the mechanisms of asthma is true? You Answered Air tubes narrow as a result of swollen tissues and excessive mucus production. Correct Answer Edema of the respiratory mucosa and excessive mucus production occur, thus obstructing airways. The walls of the alveoli are torn and cannot be repaired. The bronchioles are scarred and unable to expand. Question 3 Not yet graded / 1 pts Exercise 1 - Question 3 List the clinical manifestations of mild asthma. Your Answer: Shortness of breath, Chest tightness or pain, Wheezing when exhaling, which is a common sign of asthma in children, Trouble sleeping caused by shortness of breath, coughing or weezing, coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu. Dyspnea with exertion Wheezing Question 4 Not yet graded / 1 pts Exercise 1 - Question 4 List the signs and symptoms associated with an acute asthmatic attack. Your Answer: Severe shortness of breath, chest tightness or pain, and coughing or wheezing, Low peak expiratory flow (PEF) readings, if you use a peak flow meter, Symptoms that fail to respond to use of a quick-acting (rescue) inhaler. Tachypnea Tachycardia Diaphoresis Expiratory wheezes Use of accessory muscles Nasal flaring Increased anxiety Question 5 0.67 / 1 pts Exercise 1 - Question 5 Which events can trigger an asthmatic episode? Select all that apply. Hormone levels Correct! Mental and physical fatigue Correct! Emotional factors Correct! Environmental exposures You Answered Electrolyte imbalances Question 6 0 / 1 pts Exercise 1 - Question 6 When an asthmatic condition is suspected, which diagnostic tests will confirm a diagnosis? Select all that apply. You Answered Platelet count You Answered Serum electrolyte levels Correct! Arterial blood gas Correct! Pulmonary function tests Correct Answer Sputum cultures Question 7 0 / 1 pts Exercise 1 - Question 7 A should be obtained to rule out a secondary infection. Answer 1: You AnsweredCT Correct Answer sputum Answer 2: You AnsweredScan Correct Answer culture Question 8 0 / 1 pts Exercise 1 - Question 8 When a patient is experiencing an asthma attack, a complete blood cell count will show an elevation in which blood cell type? Correct Answer Eosinophils You Answered CT Scan Platelets Red blood cells Monocytes Question 9 0 / 1 pts Exercise 1 - Question 9 A patient experiencing a severe, life-threatening exacerbation of asthma will likely have which peak flow meter reading? 100% You Answered 45% Correct Answer 55% 85% Question 10 Not yet graded / 1 pts Exercise 2 - Virtual Hospital Activity • This exercise will take approximately 45 minutes to complete. • Sign in to work at Pacific View Regional Hospital for Period of Care 1. (Note: If you are already in the virtual hospital from a previous exercise, click on Leave the Floor and then Restart the Program to get to the sign-in window.) • From the Patient List, select Jacquline Catanazaro (Room 402). • Click Get Report and read the report. • Click Go to Nurses' Station. • Click Chart and then 402 to view Jacquline Catanazaro's chart. • Click the Emergency Department tab and review the information given. Exercise 2 - Question 1 Review the admitting vital signs. What is the significance of the findings? Your Answer: All vital signs are elevated but the ones that i find the most significant are the respiratory rate is very high as well as her pulse. this is saying to me that when she came into the ER she was having an asthma attack. The vital signs reflect respiratory distress. Her pulse rate and respiratory rate are elevated. She is mildly hypertensive. Question 11 Not yet graded / 1 pts Exercise 2 - Question 2 What is the primary admitting diagnosis? Your Answer: Acute asthma exacerbation Acute asthma exacerbation Question 12 Not yet graded / 1 pts • Click Return to Nurses' Station and then 402 at the bottom of the screen. • Read the Initial Observations. • Click Take Vital Signs and review the results. • Click Clinical Alerts and read the Clinical Report. Exercise 2 - Question 3 Jacquline Catanazaro is demonstrating extreme agitation. What is the impact of this on her health status? Your Answer: Because she is agitated and anxious it is causing her body to breath faster and harder to try and calm her down causing her asthma to worsen. Her vital signs are affected by the agitation. Her oxygen saturation has dropped. She is experiencing respiratory distress. Her respirations are labored, and she is demonstrating the presence of wheezes and substernal retractions. Question 13 0.75 / 1 pts Exercise 2 - Question 4 When preparing to perform a pulse oximeter reading on Jacquline Catanazaro, which sites would be appropriate for this test? Select all that apply. Correct! Ear lobe Correct Answer Bridge of the nose Tip of the nose Correct! Finger Correct! Toe Question 14 1 / 1 pts Exercise 2 - Question 5 Indicate whether the following statement is true or false. When using the pulse oximeter, the probe should be placed over a pulsating vascular bed. Correct! True False Question 15 Not yet graded / 1 pts • Click Patient Care and then Nurse-Client Interactions. • Select and view the video titled 0730: Intervention—Airway. (Note: Check the virtual clock to see whether enough time has elapsed. You can use the fast-forward feature to advance the time by 2-minute intervals if the video is not yet available. Then click again on Patient Care and Nurse-Client Interactions to refresh the screen.) Exercise 2 - Question 6 Jacquline Catanazaro is experiencing an acute asthma attack. What has been planned to manage the onset of this attack? Your Answer: nebulizer treatment The respiratory department has been contacted to draw arterial blood gases. After the blood is drawn, she will be allowed to have a breathing treatment. The pulse oximeter will also be used. Question 16 Not yet graded / 1 pts Exercise 2 - Question 7 What will the arterial blood gases determine? Your Answer: This test may reveal dangerous levels of hypoxemia or hypercarbia secondary to hypoventilation; typically, results are consistent with respiratory alkalosis. These tests will determine the blood's pH and concentration of oxygen, carbon dioxide, and HCO2. Question 17 Not yet graded / 1 pts • Click Physical Assessment and complete a head-to-toe assessment. Exercise 2 - Question 8 What respiratory system findings in Jacquline Catanazaro's assessment are consistent with an exacerbation of asthma? Your Answer: Labored and shallow respiratory effort, Tachypnea, Bilateral breath sounds with crackles in right lower lobes, wheezes present throughout lung fields, Productive cough of white frothy sputum, Substernal retractions and use of neck accessory muscles, Oxygen saturation of 85% in 2 liter flow oxygen via nasal cannula, PEFR of 200. Shallow, labored respirations Tachypnea Wheezes throughout Crackles in lower right lobes Reduced oxygen saturation levels Use of accessory muscles Complaints of chest tightness Question 18 1 / 1 pts Exercise 2 - Question 9 Jacquline Catanazaro's lung assessment reveals the presence of wheezes. Which description is consistent with wheezes? Heard most frequently with inspiration Correct! Caused by air movement through narrowed bronchioles Caused by fluid, mucus, or pus in the small airways and alveoli Dry, creaking, grating, low-pitched sounds heard during inspiration and expiration Question 19 0 / 1 pts Exercise 2 - Question 10 Jacquline Catanazaro's lung assessment reveals the presence of crackles. Which description is consistent with crackles? Correct Answer Bubbling sounds that are similar to the sound produced when strands of hair are rubbed between the fingers You Answered Caused by inflammation of the respiratory tree Loud machine-like sounds heard over the anterior chest wall High-pitched musical sounds heard with inspiration or expiration Question 20 Not yet graded / 1 pts Exercise 2 - Question 11 Are there any other significant system findings? Your Answer: respiratory distress, Chest expansion impaired with shallow respirations and complaints of chest tightness. Peak flow meter reading of 200, No, the other system findings are within normal range. Question 21 0.33 / 1 pts • Click Chart and then 402 to view Jacquline Catanazaro's chart. • Click the Physician's Orders tab and note the admission orders for Monday at 1600. • Click Return to Room 402 and then click the Drug icon at the bottom of the screen. • Review the information for the drugs that have been prescribed for Jacquline Catanazaro. Exercise 2 - Question 12 What are the doses and routes of administration for each of the medications ordered to manage Jacquline Catanazaro's respiratory condition? Beclomethasone: Dose mcg, Route Albuterol: Dose mg, Route Ipratropium bromide: Dose mcg, Route Answer 1: You Answered80 Correct Answer 84 Answer 2: You AnsweredOral Correct Answer puff Answer 3: Correct!5 Answer 4: Correct!oral Answer 5: You Answered17 Correct Answer 18 Answer 6: You AnsweredOral Correct Answer puff Question 22 1 / 1 pts Exercise 2 - Question 13 Below, match each prescribed medication with its correct mode of action. (A) Relief of bronchospasms 80 Oral 5 Oral 17 Oral (B) Reduction of bronchial inflammation (C) Control of secretions Correct! Beclomethasone Correct! Albuterol Correct! Ipratropium bromide Question 23 0.33 / 1 pts Exercise 2 - Question 14 When reinforcing patient instructions concerning the use of beclomethasone, which should be emphasized in the list of potential side effects associated with the medication? Select all that apply. Correct! Throat irritation Correct! Productive cough Increased pulmonary secretions Correct Answer Skin rash You Answered B A C Activity intolerance Question 24 Not yet graded / 1 pts • Click Return to Room 402. • Click Chart and then 402. • Click the Physician's Orders tab and review the orders for Monday at 1600. Exercise 2 - Question 15 What tests and/or assessments will be used to monitor Jacquline Catanazaro's respiratory status? Your Answer: Vital signs including oxygen saturation every 2 hours for first 4 hours, then every 4 hours, PEFR every 4 hours, Activity up as tolerated; encourage ambulation. Vital signs Oxygen saturation rate PEFR Question 25 Not yet graded / 1 pts Exercise 2 - Question 16 What medication has been ordered for Jacquline Catanazaro? Your Answer: 1. Beclomethasone (80 mcg/puff) via MDI, 2 puffs every 6 hours. 2. Albuterol 5 mg via nebulizer every 6 hours. 3. Ipratropium bromide (17 mcg/puff) via MDI, 2 puffs every 6 hours following Albuterol. 4. Amoxicillin 500 mg IV in 100 mL D5W every 6 hours today. Prednisone Question 26 Not yet graded / 1 pts Exercise 2 - Question 17 What are the classification and mode of action for this medication? Your Answer: 1. Beclomethasone: An adrenocorticosteroid that controls the rate of protein synthesis; depresses migration of polymorphonuclear leukocytes and fibroblasts; prevents or controls inflammation; and reverses capillary permeability. Therapeutic Effect: Inhalation: Inhibits bronchoconstriction, produces smooth muscle relaxation, decreases mucus secretion. Intranasal: Decreases response to seasonal and perennial rhinitis. 2. Albuterol: A sympathomimetic (adrenergic agonist) that stimulates beta2- adrenergic receptors in the lungs, resulting in relaxation of bronchial smooth muscle. Therapeutic Effect: Relieves bronchospasm, reduces airway resistance. 3. Ipratropium bromide: An anticholinergic that blocks the action of acetylcholine at parasympathetic sites in bronchial smooth muscle. Therapeutic Effect: Causes bronchodilation, inhibits secretions from the glands lining the nasal mucosa. 4. Amoxicillin:A penicillin that inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins which inhibits bacterial cell wall synthesis. Therapeutic Effect: Bactericidal in susceptible microorganisms. Prednisone is a corticosteroid that will be used to reduce swelling in the airways. Question 27 Not yet graded / 1 pts Exercise 2 - Question 18 List several clinical manifestations that would indicate improvement in Jacquline Catanazaro's condition. Your Answer: lessened shortness of breath, little to no chest tightness, pain, coughing or wheezing. higher peak expiratory flow (PEF) readings, closer to normal. no need for the use of a quick-acting (rescue) inhaler. Reduced respiratory rate Reduced blood pressure Reduced heart rate Improved air exchange throughout lung fields Reduced wheezes, rhonchi, and crackles No further use of accessory muscles with breathing Increased oxygen saturation rate [Show More]
Last updated: 1 year ago
Preview 1 out of 110 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 03, 2021
Number of pages
110
Written in
Additional information
This document has been written for:
Uploaded
Aug 03, 2021
Downloads
0
Views
30


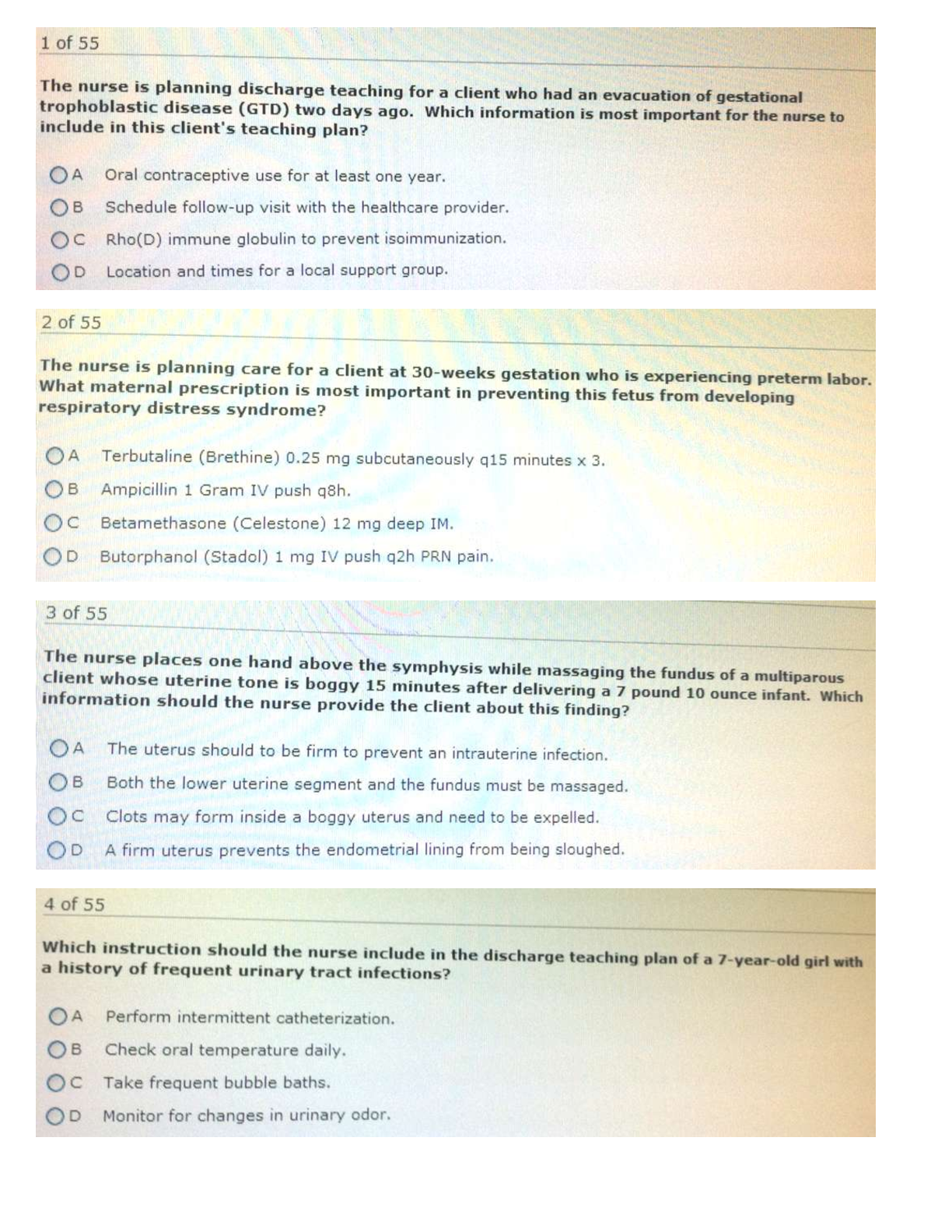
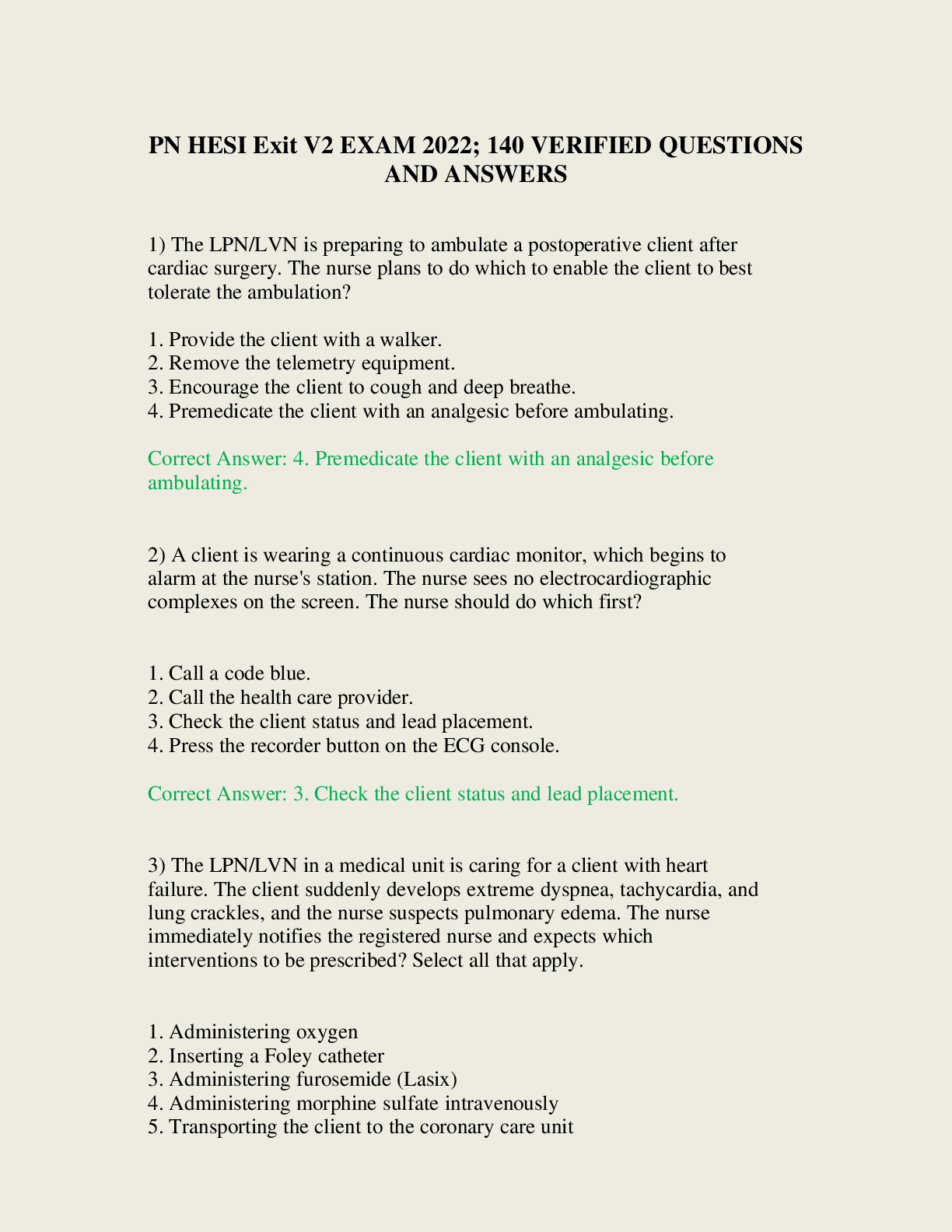
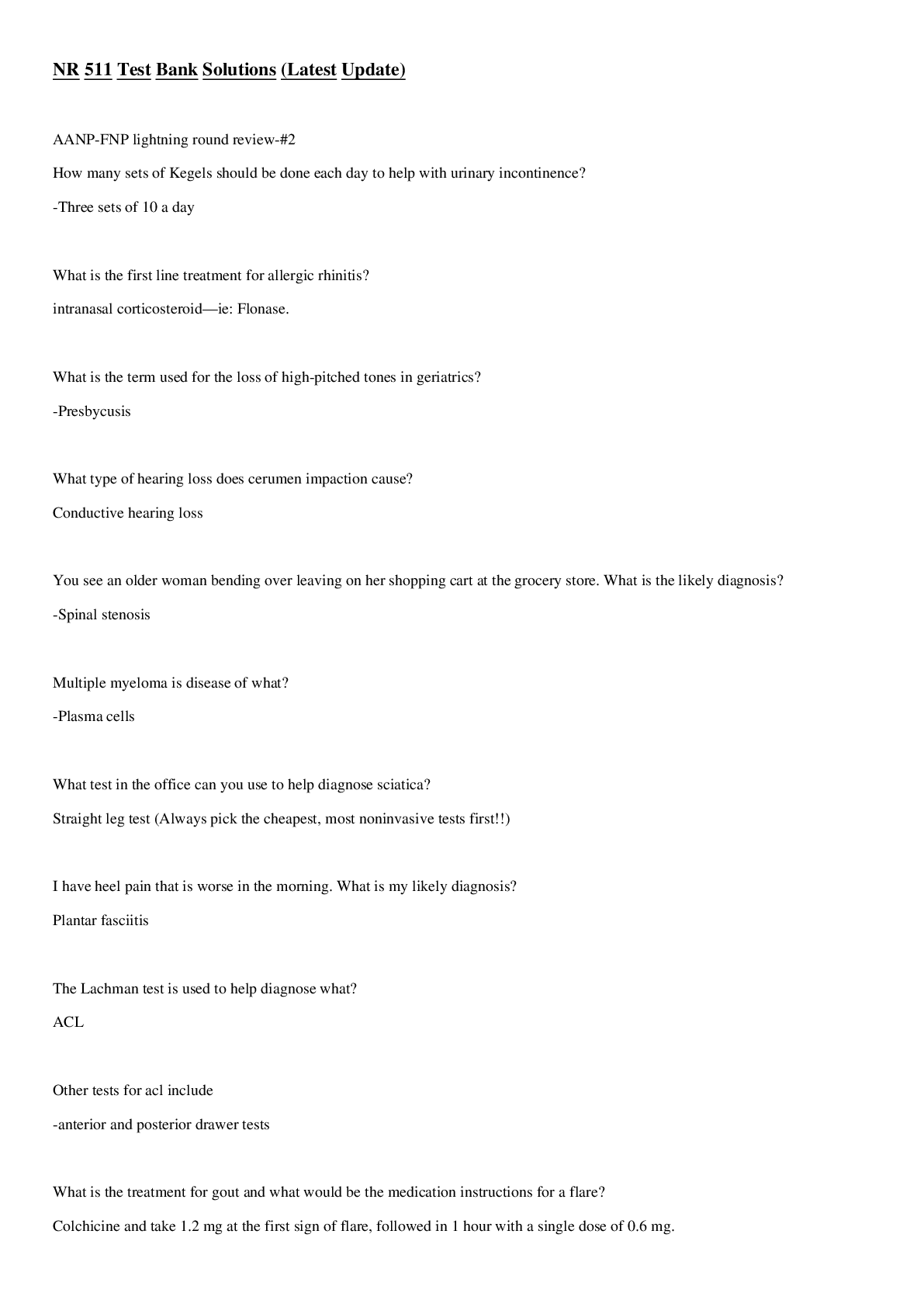
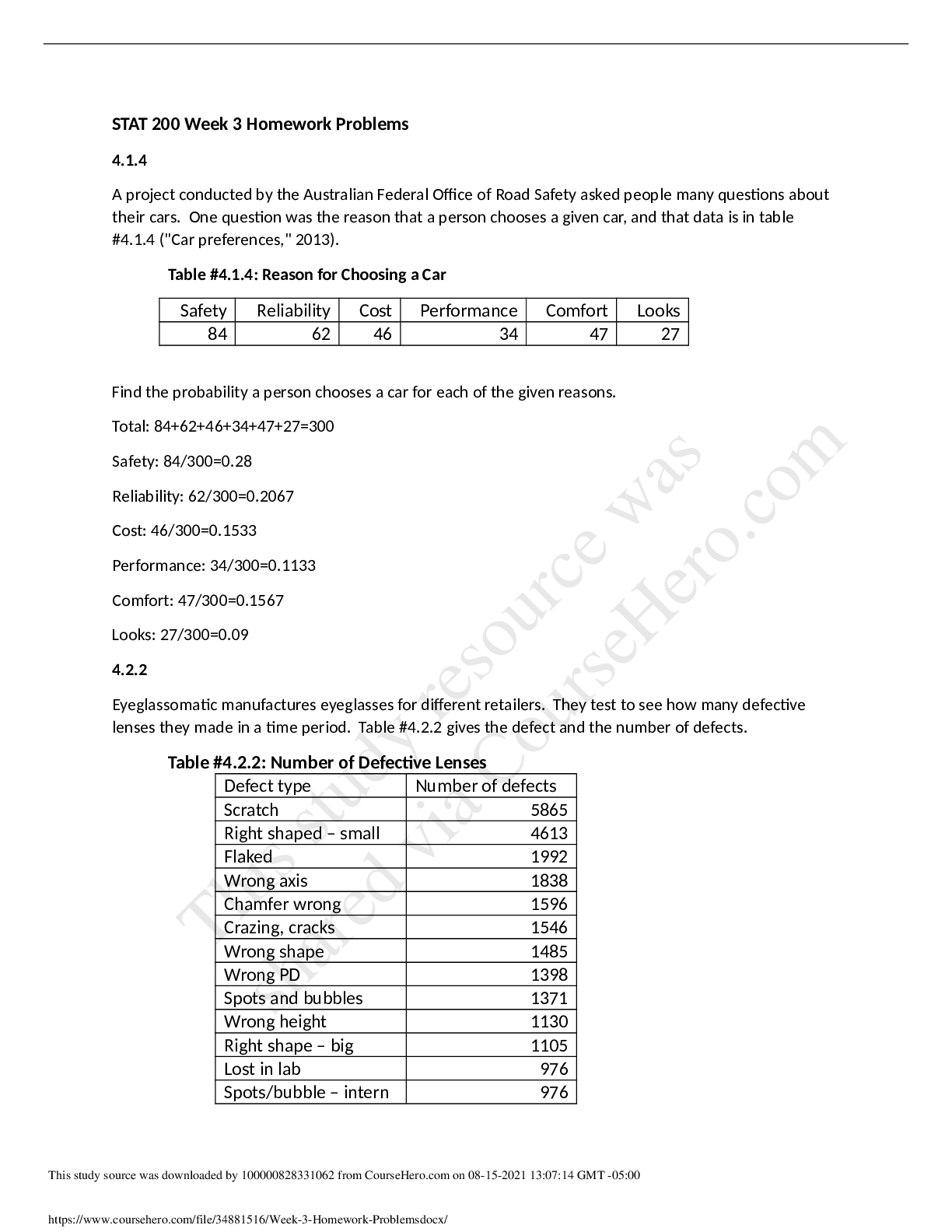
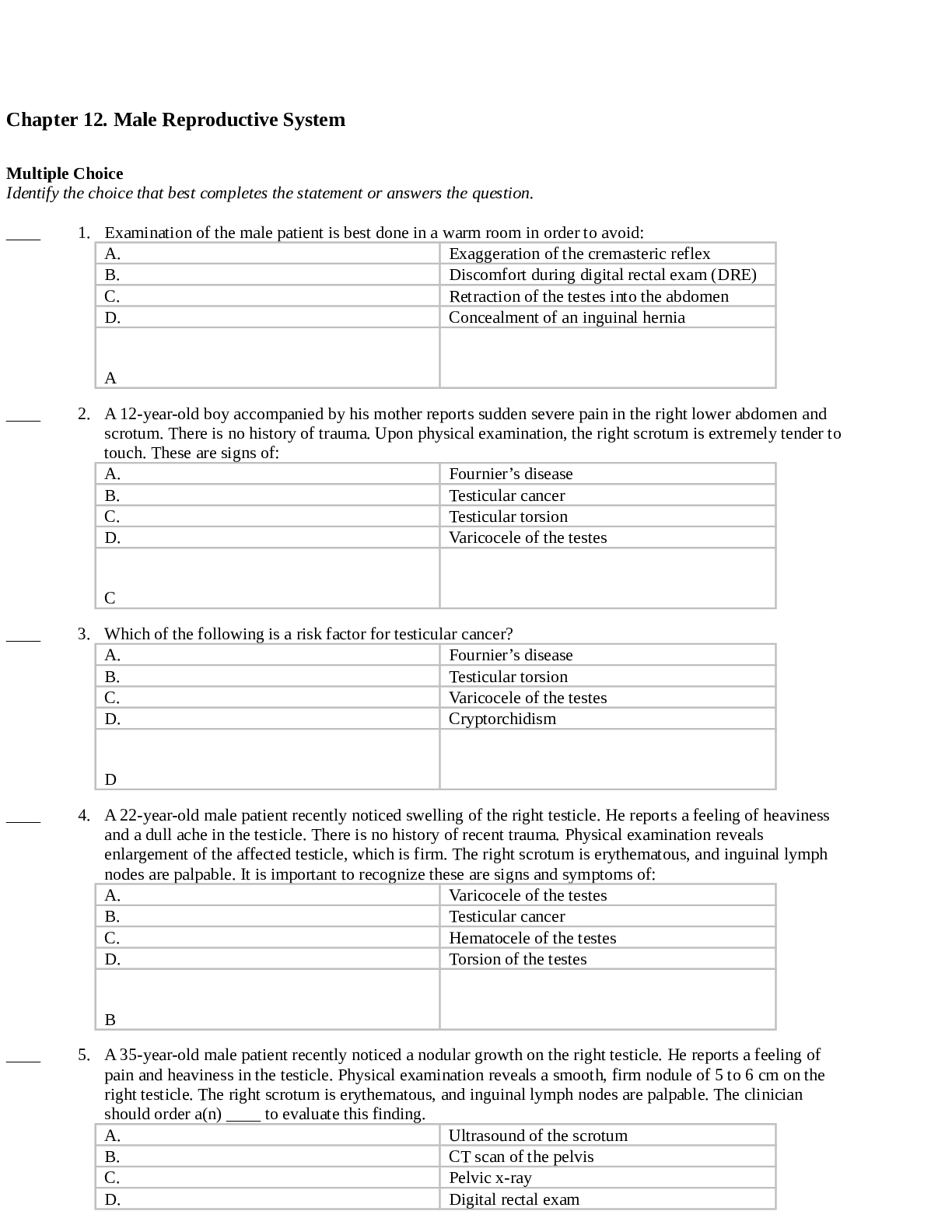
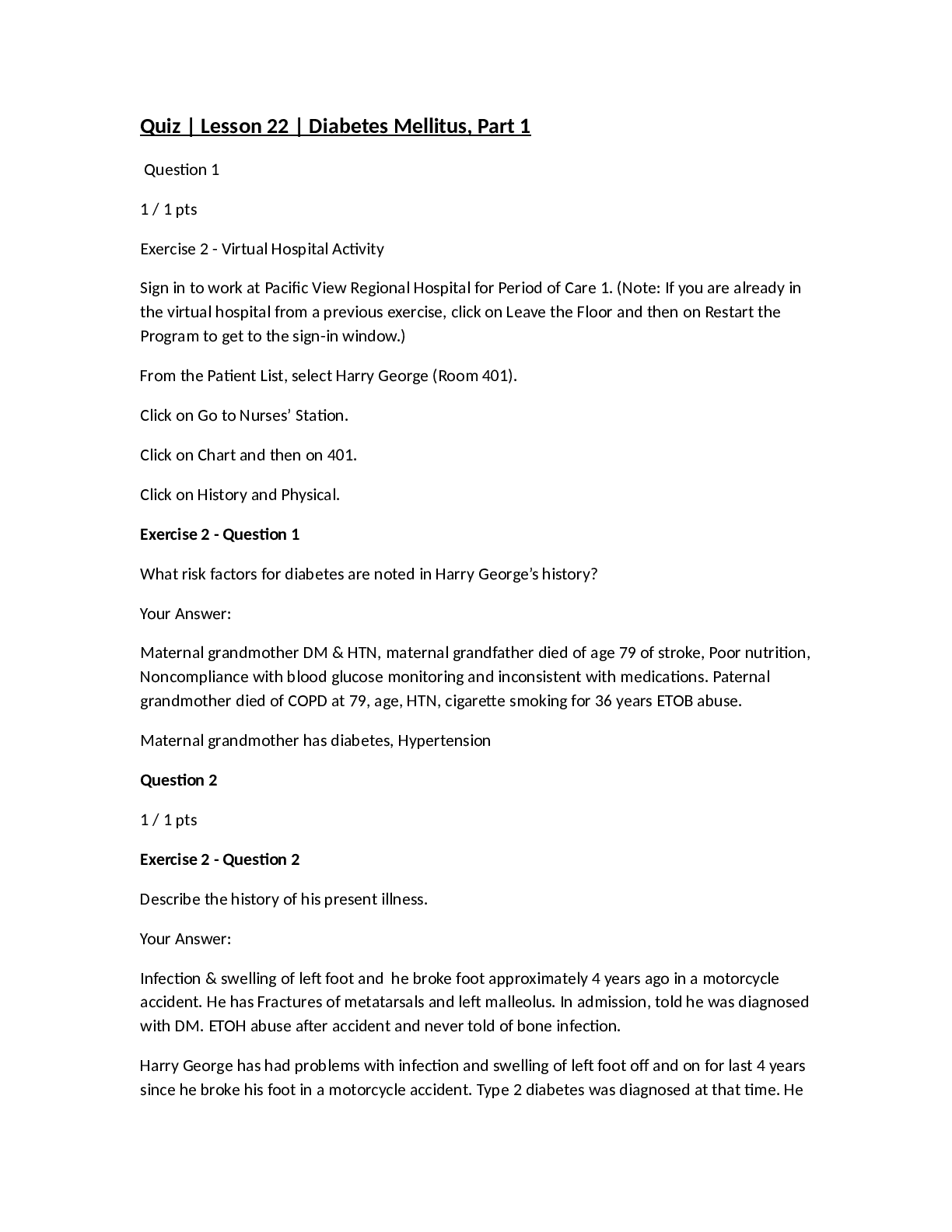
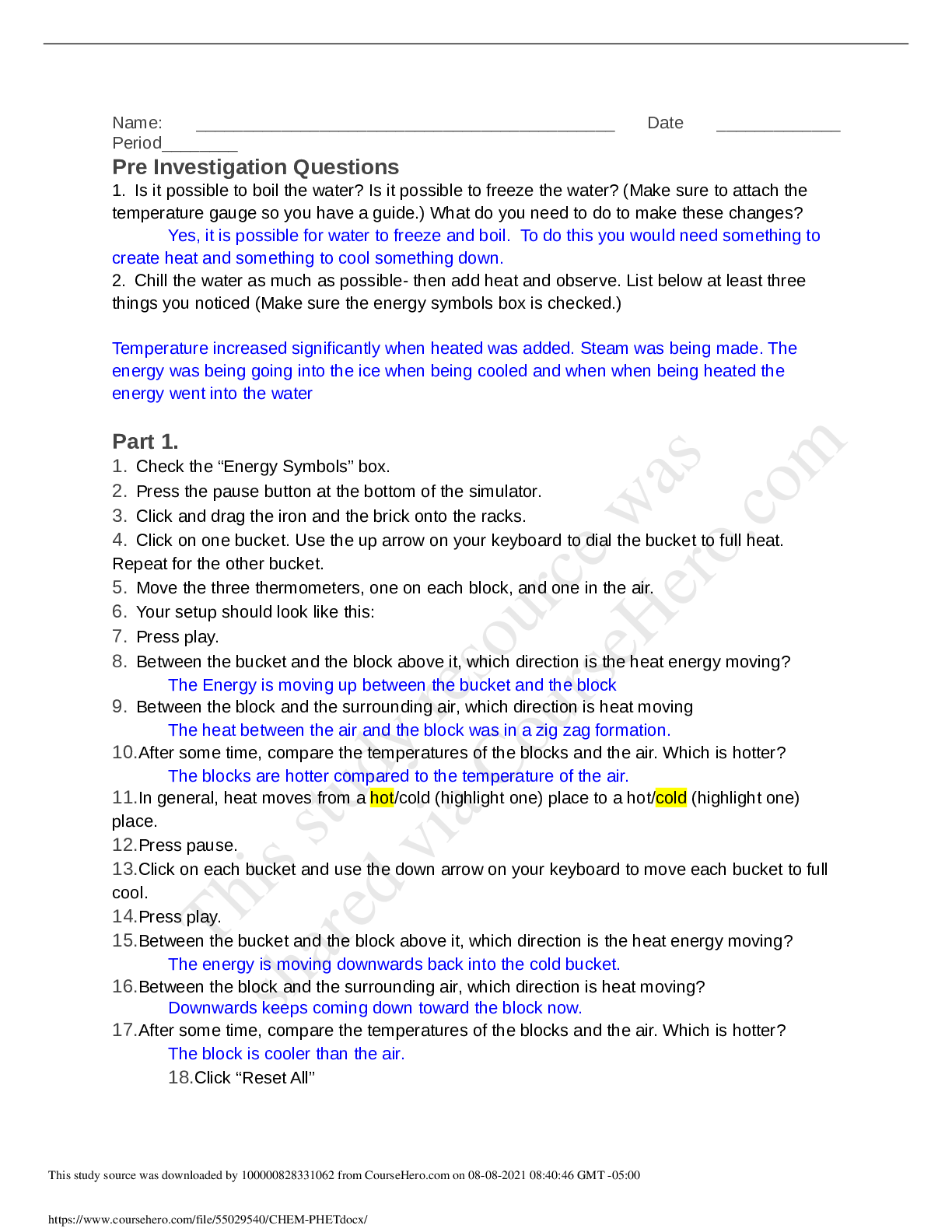
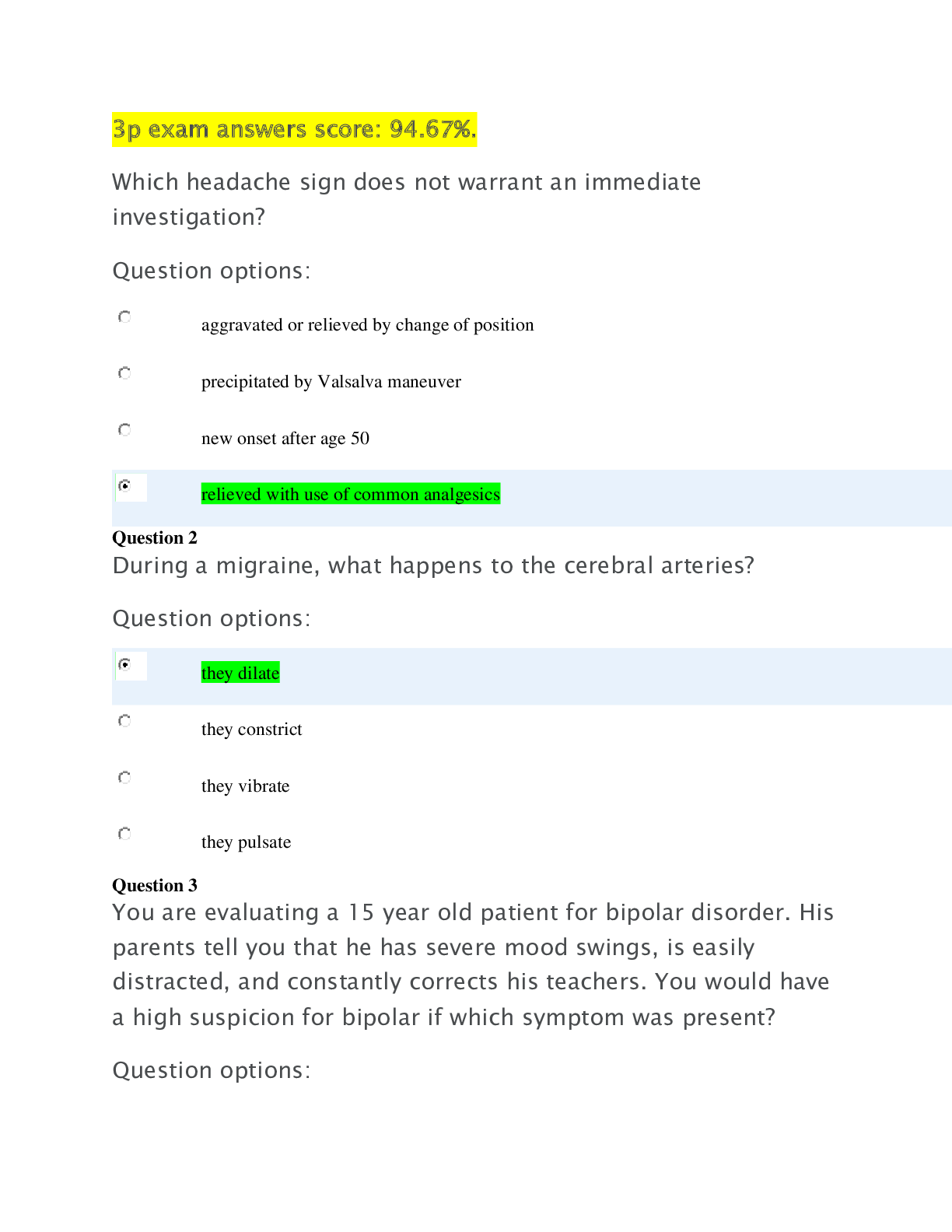





.png)
.png)
.png)
.png)

