*NURSING > STUDY GUIDE > NURSING MISC AH1 exam 1 Study Guide (All)
NURSING MISC AH1 exam 1 Study Guide
Document Content and Description Below
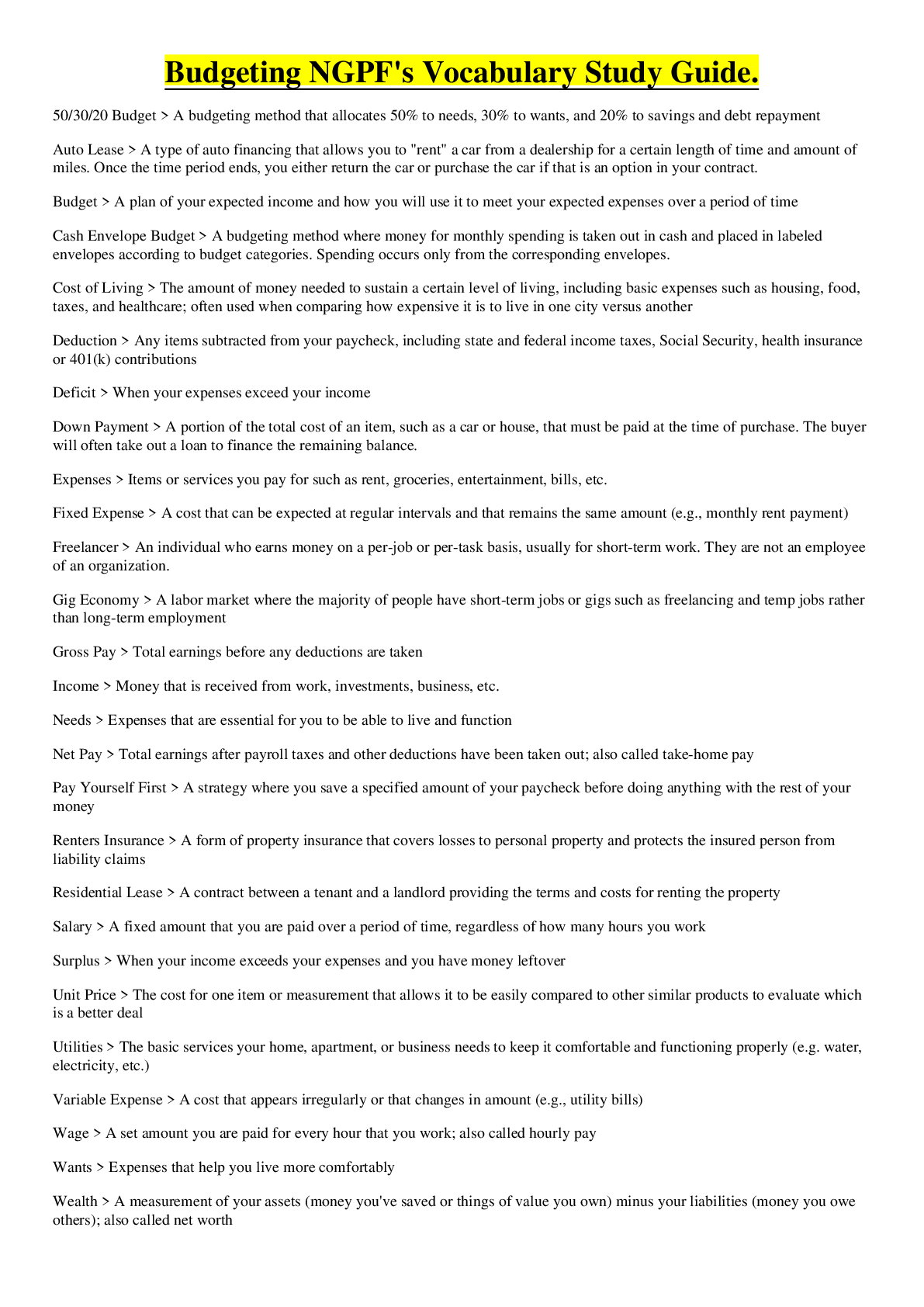
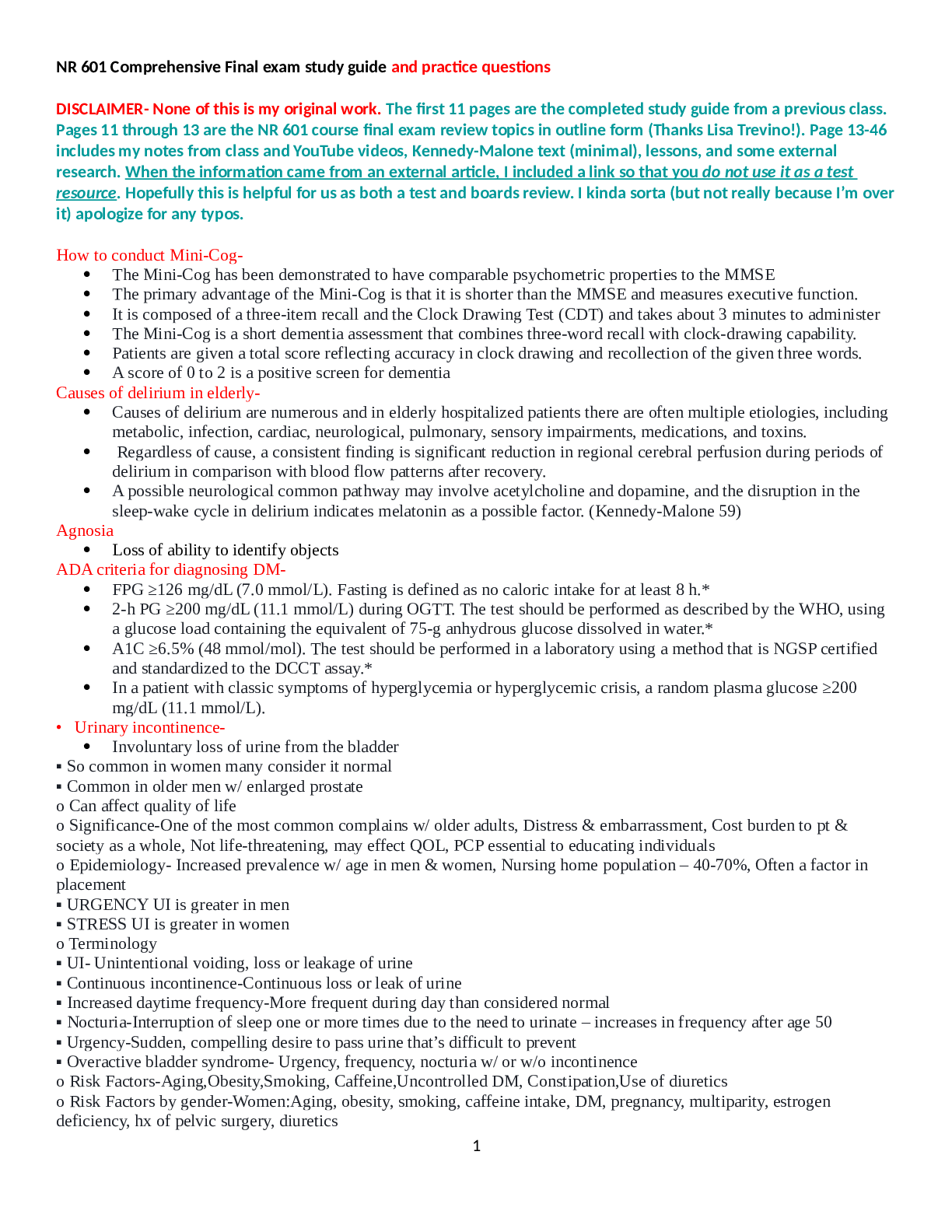
1 AH1 exam 1 Diabetes: o Group of metabolic diseases characterized by increased levels of glucose in the blood = hyperglycemia o Results from defects in: (could be both)* ▪ Insulin secretio... n ▪ Insulin action o Leading cause of death from disease o High rate of cardiovascular disease (MI, stroke, peripheral vascular disease) Classifications ● major classifications of diabetes: o type 1 o type 2 o gestational o latent autoimmune diabetes of adults (LADA) o diabetes associated with other conditions or syndromes Prediabetes: impaired glucose tolerance or impaired fasting glucose o refers to a condition where blood glucose levels fall between normal levels and those considered diagnostic for diabetes Diabetic Screening ● Determine risk factors: obesity, hypertension, sedentary lifestyle, hyperlipidemia, smoking, genetic hx, ethnic group, woman who have ovary syndrome or delivered infants weighing more than 9lbs ● Screen pts whose BMI greater than 25 and age greater than 45 ● Child is overweight and has additional risk factors ● Screening is done with fasting serum glucose levels or glycosylated hemoglobin (A1C) Client education ● Exercise 3x weekly o Pts w/ blood glucose levels of 250mg/dL and who have ketones DO NOT EXERCISE**** ● Good nutrition o Pts who requires insulin should eat a 15g carb snack*** o Carbs: 45% of daily intake o Protein: 15-20% o Unsat/poluunsaturated fats: 30-35% ● Regular diet (eat at same times/same amounts) promotes control of glucose levels2 ● Diet low in saturated fats ● Include Omega-3 fatty acids and fiber o Most important objective from nutrition and dietary management: maintain reasonable weight, control blood glucose levels, and normalize lipids and BP to prevent heart disease*** Risk Factors ● Metabolic syndrome ● Insulin resistance o Pancreatitis and Cushing’s syndrome are secondary causes of diabetes o Vision and hearing deficits o Tissue deterioration (from aging) and affect ADL’s and ability to perform glucose monitoring o Fixed income (can’t afford insulin/meds) ● Age ^^^ Expected Findings ● Hyperglycemia: blood glucose greater than 250mg/dL ● Polyuria: excess urine production & frequency (osmotic diuresis) ● Polydipsia: excessive thirst bc dehydration o Loss of skin turgor, skin is dry and warm o Dry mucous membranes o Weakness and malaise o Rapid weak pulse and hypotension ● Polyphagia: excessive hunger&eating bc the cells do not receive glucose o Weight loss o Ketones accumulate in blood due to breakdown of fatty acids when insulin is not available (causes metabolic acidosis) o Kussmaul respirations: increased RR and depth, trying to excrete CO2 and acid ● Fruity breath ● Headache, nausea, vomiting, abdominal pain, fatigue, weakness, vision changes, slow wound healing, etc Lab Tests: two findings (on separate days) or atleast two of the following ● Manifestations of diabetes + casual blood glucose concentration greater than 200mg/dL ● Fasting blood glucose greater than 126mg/dL ● 2hr glucose greater than 200mg/dL with oral glucose tolerance test ● Glycosylated hemoglobin (A1C) greater than 6.5% ● Urine ketones: high ketones in the urine with hyperglycemia (exceed 300mg/dL) is a medical emergency** Diagnostic Procedures ● Self-monitoring blood glucose:3 o pt pricks their finger and applies a drop of blood to a test strip Complications o Diabetic Macrovascular complications result from changes in the medium to large blood vessels o Diabetic Microvascular disease is characterized by capillary basement membrane thickening Medications Insulin: hormone secreted by beta cells, anabolic ● Actions: o Transports and metabolizes glucose for energy o Stimulates storage of glucose in the liver and muscle (form of glycogen) o Signals liver to stop release of glucose o Enhances storage of dietary fat in adipose tissue o Accelerates transport of amino acids into cells o Inhibits the breakdown of stored glucose, protein and fat ● Glucagon: released when blood glucose levels decrease, stimulates the liver to release stored glucose ● After 8-12 hrs without food, liver forms glucose from the breakdown of noncarbohydrate substances, including amino acids (gluconeogenesis) Rapid acting insulin: Lispro, Aspart, Glulisine o Administer before meals o Onset: 10-30 min o Peak: 1 hr o Duration: 2-4 hrs o Administer with intermediate or long acting o Used for rapid reduction of glucose levels Short acting insulin: regular- Humulin R, Novolin R o Administer 30-60 min before meals o 2 concentrations o U-500 is reserved for pt with insulin resistant-not given IV o U-100 is prescribed for most pts and may be given IV o Onset: 30-60 min o Peak: 2-3 hrs o Duration: 4-6 hrs Intermediate acting insulin: NPH4 o Adminster for glycemic control between meals and at night o Not administered before meals o Contains protamine (a protein), that puts a delay in insulin absorption or onset and extends the duration o Administer SQ only and can only mix with short-acting o Onset: 2-4hrs o Peak: 4-12 hrs o Duration: 16-20 hrs Very-Long acting insulin: Lantus, Glargine o Administered once daily, at the same time each day o Forms microprecipitates that dissolve slowly over 24hrs and maintains a steady blood glucose with no peaks or troughs o Admininster SQ, never IV o Onset: 1-6 hrs o Peak: none o Duration: 24-36 hrs Insulin Regimens ● Vary from 1-4 injections per day ● Usually, a combo of short-acting and longer-acting ● 2 approaches to insulin therapy: o Conventional: simplify the insulin regimen to avoid acute complications of diabetes o Intensive: use a more complex insulin regimen to achieve as much control over blood glucose levels as is safe and practical ● 4 main areas for injection: abdomen, upper arms, thighs and hips Complications of Insulin Therapy ● Local Allergic Reactions o Redness, swelling, tenderness, duration appears around injection site 1-2 hrs after administration ● Systemic Allergic Reaction o Immediate local skin reaction that gradually spreads into generalized urticaria (hives) ● Insulin Lipodystrophy o Localized reaction in the form or either lipoatrophy or lipohypertrophy o Lipoatrophy: loss of subcutaneous fat; appears as a slight dimpling or more serious pitting of subcutaneous fat o Lipohypertrophy: development of fibrofatty masses at injection site, caused by the repeated use of an injection site ● Resistance to injected insulin o Pts may develop insulin resistance and require large insulin doses to control symptoms ● Hypoglycemia o Low sugar in the blood, occurs when blood glucose falls less than 70mg/dL5 o Mild hypoglycemia s/s: sweating, tremors, tachycardia, palpitation, nervousness, hunger o Moderate hypoglycemia s/s:inability to concentrate, headache, lightheadedness, confusion, memory lapses, numbness of the lips and tongue, slurred speech, impaired coordination, emotional changes, irrational behavior, double vision o Severe hypoglycemia s/s: disoriented behavior, seizures, difficulty waking up from sleep, or loss of consciousness Methods of Insulin Delivery: ● Pens ● Jet Injection ● Pumps *Pt may complain of headache and pain at injection site. Ensure patency of IV line used for injection of 50% dextrose bc it is very irritating to veins* Oral Hypoglycemics Biguanides: Metformin ● Reduces production of glucose by the liver ● Increases tissue sensitivity to insulin ● Slows carb absorption in the intestines Nursing considerations: ● Monitor GI effects ● Monitor for lactic acidosis ● Stop med for 48 hrs before any elective radiographic test and restart 48hrs after Client education: ● Take with food ● Take Vitamin B12 and folic acid supplements ● Contact provider if manifestations of lactic acidosis (sluggishness, hyperventilation) ● May be taken during pregnancy ● Never crush or chew Sulfonylureas: Glipizide, glimepirirde, glyburide ● Stimulates insulin release from the pancreas causing decrease in blood sugar levels ● Increases tissue sensitivity to insulin Nursing considerations: ● Monitor for hypoglycemia ● Beta-blockers can mask tachycardia seen during hypoglycemia6 Client Education: ● Administer 30min before meal ● Monitor for hypoglycemia and report frequent episodes to the provider ● Avoid alcohol Meglitinides: Repaglinide, nateglinide ● Stimulates insulin release from the pancreas ● Administered for post-meal hyperglycemia Nursing Considerations: ● Monitor for hypoglycemia ● Monitor HbA1c every 3 months Client Education ● Administer 15-30 min before meal ● Must eat 30min of administration ● Do not take if skipped a meal Thiazolidinediones: Pioglitazone ● Reduces the production of glucose in the liver (gluconeogenesis) ● Increases tissue sensitivity to insulin Nursing Considerations: ● Monitor for fluid retention, esp pts with hx of heart failure ● Monitor for elevation of ALT, LDH, and triglycerides levels Client Education: ● Report rapid weight gain, shortness of breath, or decreased exercise tolerance ● Have liver function test at baseline and every 3-6 months after Alpha-glucosidase inhibitors: Acarbose, miglitol ● Slow carb absorption ● Reduce post-meal hyperglycemia Nursing Considerations: ● Alert the pt that GI discomfort (cramps, excessive gas, diarrhea) is common ● Monitor liver function every 3 months ● Treat hypoglycemia with dextrose Client Education: ● Instruct pt to have liver function tests every 3 months ● Take med with the first bite of each meal ● Have dextrose paste available for hypoglycemia Dipeptidyl peptidase-4 (DPP-4) inhibitors: Sitagliptin ● Augments naturally occurring intestinal incretin hormones, which promotes release of insulin and decrease secretion of glucagon ● Lowers fasting and postprandial glucose levels Nursing Considerations: ● Few adverse effects but upper respiratory manifestations: nasal and throat inflammation and pancreatitis can occur7 ● Alert the pt of GI discomforts Client Education: ● Report persistent respiratory manifestations ● Report severe abdominal pain, with or without emesis ● Med only works if blood sugar is rising Sodium-glucose cotransporter 2 inhibitors: Canagliflozin, dapagliflozin ● Blocks reabsorption of glucose from the kidneys Nursing Considerations: ● Monitor for development of UTI and yeast infections in women ● Monitor postural hypotension in older adults Client Education: ● Take med before first meal of the day ● Change positions slowly ● Monitor and report genital itching, burning, and increased drainage Non-insulin injectable medications Incretin mimetic: Exentadie, liraglutide ● Mimics the function of intestinal incretin hormone by decreasing glucagon secretion and gastric emptying ● Decrease insulin demand by reducing fasting and postprandial hyperglycemia Nursing Considerations: ● Adminster SQ 60min before morning and evening meal ● Monitor for gastrointestinal distress Client Education: ● Do not administer after a meal ● Oral antibiotic, oral contraceptive, or acetaminophen should never be given within 1 hr of oral exenatide or 2 hr after an injection of exenatide ● Can have decreased appetite and weight loss ● Wait for next scheduled dose if the scheduled med is missed ● Report severe abdominal pain Amylin mimetic: Pramlintide ● A synthetic amylin hormone found in the beta cells of the pancreas, it suppresses glucagon secretion and controls postpradial blood glucose levels Nursing Considerations: ● Administer SQ immediately before each meal ● Do not administer if pt has hypoglycemia unawareness, or noncompliance/poor adherence to treatment regimen and blood glucose monitoring ● Can be administered with insulin therapy and oral hypoglycemic agent ● Pre-meal doses of rapid- or short acting insulin should be reduced by 50% to reduce risk of hypoglycemia Client Education: ● Monitor and report frequent periods of hypoglycemia ● Monitor for injection site reactions8 Patient-Centered Care: Nursing Care o Monitor the following: ▪ Blood glucose levels ▪ I&O and weight ▪ Skin integrity (wound healing) ▪ Sensory alterations: tingling numbness ▪ Visual alterations ▪ Dietary practices ▪ Exercise patterns ▪ SMBG skill ▪ Self-med administration profiency o Teach pt to rotate injection site** Retinopathy: damage to small blood vessels that nourish retina Nephropathy: damage to kidney cells Neuropathy: damage to nerve cells Type 1: insulin-dependent diabetes or juvenile diabetes o 5% of all diabetes *** o destruction of beta cells of the islets of Langerhans in the pancreas o absence of insulin production Characteristics for type 1: ● onset any age, usually <30 years old ● thin at diagnosis; recent weight loss ● etiology: o genetic o immunologic o environmental factors (virus) ● require insulin ● ketosis prone ● acute complications of hyperglycemia: keto acidosis Osmotic diuresis: excess glucose in the urine and excessive loss of fluids and electrolytes Glycogenolysis: break down of stored glucose Gluconeogenesis: production of new glucose from amino acids and other substrates Diabetic Ketoacidosis: common in ppl with type 1** ● deficiency of insulin ● highly acidic ketones are formed o ketone bodies: highly acidic substance formed when the liver breaks down free fatty acids in the absence of insulin9 ● results in metabolic acidosis o No insulin is present to break down ketone bodies and ketoacidosis 3 main clinical features of Diabetic Ketoacidosis: o Hyperglycemia o Dehydration and electrolyte loss o Acidosis Treatment: o Fluid replacement o Correction of electrolyte imbalances o Insulin administration Type 2: non-insulin dependent or adult-onset diabetes o affects 95% of ppl with the disease*** o inability of cells to respond to insulin o decreased production of insulin o linked to: obesity, sedentary lifestyle, and heredity o metabolic syndrome often proceeds type 2 o a constellation of symptoms: hypertension, hypercholesterolemia, abdominal obesity, other abnormalities Characteristics of type 2: ● more common in people >30 years old ● obese ● can control blood glucose levels through weight loss if obese ● oral antidiabetics may improve blood glucose levels if dietary changes do not work ● ketosis uncommon except in stress & infection ● acute complications: hyperglycemic hypersmolar syndrome (from uncontrolled type 2; DEADLY) o s/s: hypotension, profound dehyradtion, tachycardia, variable neurological signs (alterations in consciousness, seizures, hemiparesis) o Treatment same as DKA ● intracellular reactions are diminished ● beta cells cannot keep up with increased demand for insulin = type 2 Symptoms: ● fatigue ● irritability ● polyuria ● polydipsia ● poor wound healing ● vaginal infections ● blurred vision (glucose levels are very high)10 *Consequence of Undetected diabetes is that long-term diabetes complications like eye disease, peripheral neuropathy, peripheral vascular disease may develop before the actual diagnosis of diabetes is made, which tells BGL have been high for a while.* Gestational: onset is pregnancy ● high risk ethnic groups: o Hispanic americans o Native americans o Asian americans o African americans o Pacific islanders Latent Autoimmune Diabetes of Adults (LADA): ● Progression of autoimmune beta cells destruction in the pancreas is slower than in types 1 and 2 ● Not insulin dependent in the first 6 months of onset ● Clinical manifestations shares the same as type 1 and type 2 Foot Care o Inspect feet daily o Pat dry, esp between toes and avoid lotions o Use mild foot powder o Do not use at home remedies for foot care o Best time to perform foot care is after bath/shower o Avoid open toe, open-heel shoes o Avoid prolonged sitting, standing and crossing legs o If trimming toe nails: straight acrossed Nutritional Guidelines: o Meal planning to include food intake, weight management, and lipid/glucose management o Plan meals for appropriate timing, activity, onset, and peak of insulin o Count grams of carbs o Restrict calories and increase activity as appropriate for weight loss o Use artificial sweeteners o Read and interpret food labels Illness Teach pt guidelines to follow when sick: ● Monitor blood glucose every 3-4 hrs ● Continue taking insulin or oral hypoglycemic agents ● Consume 4 oz of sugar free, noncaffeinated liquid every 30min ● Meet carb needs thru soft foods (custard, gelatin, graham crackers) ● Test urine for ketones and report to provider if outside expected range ● Rest ● Call provider: o Blood glucose greater than 240mg/dL11 o Fever greater than 101.5, does not respond to acetaminophen, and lasts longer than 24hr o Feeling disoriented or confused o Rapid breathing o Vomiting more than once o Diarrhea more than 5x or longer than 24hr o Inability to tolerate liquids o Illness longer than 2 days Complications: ● Cardiovascular and cerebrovascular disease ● Diabetic retinopathy ● Diabetic neuropathy ● Diabetic nephropathy12 Respiratory- Rhinitis, Sinusitis, Influenza, Pneumonia Rhinitis: ● Inflammation and irritation of the mucous membranes of the nose ● Causes: o Changes in temp or humidity o Odors o Infection o Age o Systemic disease o Use of over the counter and prescribed nasal decongestants o Presence of a foreign body ● Allergic rhinitis: seasonal rhinitis associated with exposure to airborne particles such as: dust, dander, plant pollens o May occur from allergies such as foods (nuts, shellfish, soy), medications (penicillin, aspirin), and particles indoor/outdoor environment o Most common cause of nonallergic rhinitis: common cold Signs/Symptoms: ● Rhinorrhea: runny nose ● Congestion ● Nasal discharge (purulent with bacteria rhinitis) ● Sneezing ● Pruritis of the nose, roof of mouth, throat eyes, and ears ● Headache Viral Rhinitis (Common Cold) ● Most frequent viral infection in the general population ● “common”: caused by a virus ● “cold”: refers to infectious, acute inflammation of the mucous membranes of the nasal cavity ● Term is also used when the virus is influenza Signs/symptoms: ● low-grade fever ● nasal congestion ● runny nose/nasal discharge ● halitosis ● sneezing ● teary watery eyes ● “scratchy” sore throat ● General malaise ● Chills ● Headache/muscle aches13 Medical Management ● warm saltwater gargles ● nonsteroidal anti-inflammatory drugs (NSAIDS) o ex: aspirin, ibuprofen o relieves headaches and pains ● Antihistamines used to relieve sneezing & runny nose ● Petroleum jelly to soothe dryness around the nose Nursing Management ● Most viruses can be spread by: o Direct contact with infected secretions o Inhalation of large particles from others’ coughing or sneezing o Inhalation of small particles (aerosol) that may be in the air for up to an hour Rhinosinusitis “sinusitits” ● Inflammation of the paranasal sinuses and nasal cavity ● Typical pathogens: Streptococcus pneumonia, Haemophilus influenzae, and less commonly Staphylococcus aureus and Moraxella catarrhalis Causes of Rhinosinusitis Category Causes Vasomotor Idiopathic Abuse of nasal decongestants Psychological stimulation (anger, Sexual assault) Irritants Mechanical Tumor Deviated septum Crusting Hypertrophied turbinates Foreign body Cerebrospinal fluid leak Chronic Inflammatory Polyps (in cystic fibrosis) Sarcoidosis Wegener granulomatosis Midline granuloma Infectious Acute viral infection14 Acute or chronic rhinosinusitis Rare nasal infections (syphilis, TB) Hormonal Pregnancy Use of oral contraceptives Hypothyroidism Influenza Seasonal influenza “flu”: occurs as an epidemic, usually in the fall and winter months ● Highly contagious acute viral infection, occurs in children & adults ● Caused by one of several virus families and can vary yearly o Adults: contagious 24 hrs before manifestations develop & up to 5 days after they start Pandemic influenza: viral infection among animals or birds that has mutated and is becoming highly infectious to humans ● Has potential to spread globally like H1N1 (swine flu) Assessment Expected Findings: ● Severe headaches ● Chills ● Fatigue, weakness ● Severe diarrhea & cough (avian flu) ● Fever ● Hypoxia (avian flu) Medications Antivirals ● Amantadine, rimantadine, and ribavirin Influenza Vaccines Client Education ● Encourage flu vaccines ● Reduce risk by washing hands & following cough etiquette ● Avoid close personal contact (handshaking, hugs, kissing) ● If flu manifestations occur: increase fluid intake, rest, and stay home ● Avoid travel to places with pandemic ● Be aware of public health announcements Pneumonia Expected Findings: ● Anxiety ● Fatigue ● Weakness ● Chest discomfort due to coughing ● Confusion from hypoxia (most common in older adults)15 Physical assessment findings: ● Fever ● Chills ● Flushed face ● Diaphoresis (sweating) ● Shortness of breath/difficulty breathing ● Tachypnea ● Sharp chest pain ● Sputum production (yellow-tinged) ● Crackles and wheezes ● Coughing ● Dull chest percussion over areas of consolidation ● Decreased O2 sats (range 95-100%) ● Purulent, blood-tinged or rust-colored sputum Lab Tests ● Sputum Culture and sensitivity o Obtain before starting antibiotic therapy o Obtain by suctioning if pt unable to cough o Difficult to obtain from older pts bc of weak cough reflex ● CBC: elevated WBC count ● ABG’s: hypoxemia (decreased PaO2 less than 80 mmHg) ● Blood culture: to rule out organisms in the blood ● Serum electrolytes: to identify causes of dehydration Diagnostic Procedures ● Chest X-ray ● Pulse ox Nursing Care ● Position pt high-Fowler’s ● Encourage coughing or suction to remove secretions ● Administer breathing treatments & meds ● Administer O2 therapy ● Monitor for skin breakdown around nose & mouth ● Deep breathing with incentive spirometer ● Promote adequate nutrition/fluid intake: o Increase calories o Aids in preventing secondary illnesses o Fluid intake 2-3L/day ● Provide rest periods ● Reassure pt in respiratory distress Medications Antibiotics16 ● Used to destroy infections ● Commonly used: Penicillin, Cephalosporins ● Given IV and then switched to oral form as condition improves ● Obtain sputum culture before giving first dose of antibiotic Nursing Considerations: ● Observe pt taking cephalosporins for frequent stools ● Monitor kidney function Bronchodilators ● Given to reduce bronchospasms and reduce irritation ● Short acting beta agonists like albuterol, rapid relief ● Cholinergic antagonists (anticholinergic meds) like ipratropium, block sympathetic nervous system, allowing increased bronchodilation & decreased pulmonary secretions ● Methylxanthines (theophylline) require close monitoring of serum medication level due to narrow therapeutic range Asthma ● Chronic inflammatory disorder of the airways that result in intermittent and reversible airflow obstruction of the bronchioles o Obstruction occurs either by inflammation or airway hyperresponsiveness Risk Factors: ● Family hx of asthma ● Smoking & secondhand smoke exposure ● Environmental allergies ● Exposure to chemical irritants or dust ● Gastroesophageal reflex disease (GERD) Medications Bronchodilators (inhalers) ● Short acting beta2 agonists (rapid relief): albuterol ● Anticholergenic meds: ipratropium ● Methylxanthines: theophylline ● Long acting beta2 agonists: salmeterol Nursing Considerations: Albuterol: watch for tremors and tachycardia Ipratropium: observe for dry mouth Theophylline: Monitor serum levels for toxicity. Side effects: tachycardia, nausea and diarrhea COPD ● Combination of emphysema and chronic brochitits ● Inflammation of the bronchi and bronchioles due to chronic exposure to irritants Risk Factors:17 ● Advanced age ● Smoking ● Alpha1-antitrypsin (AAT) deficiency ● Exposure to environmental factors (air pollution) Expected Findings: ● Chronic dyspnea Physical Assessment Findings: ● Dyspnea upon exertion ● Productive cough (severe in the morning) ● Hypoxemia ● Crackles and wheezes ● Rapid and shallow respirations ● Use of accessory muscles ● Barrel chest or increased chest diameter ● Hyperresonance on percussion due to “trapped air” (w/ emphysema) ● Irregular breathing pattern ● Thin extremities and large neck muscles ● Dependent edema secondary to right sided heart failure ● Clubbing of fingers and toes ● Pallor and cyanosis of nail beds ● Decreased O2 sat ● Older adults w/ darker skin, lower O2 sats Nursing Care: ● For pursed lip breathing: o Form mouth like going to whistle o Take a breath in thru the nose and out thru lips/mouth o Don’t puff cheeks o Take breaths deep and slow Medications Bronchodilators(inhalers) Anti-inflammatory agents ● Corticosteroids: fluticasone o Monitor for adverse effects: fluid retention, immunosuppression, hyperglycemia, hypokalemia, poor wound healing) ● Leukotriene antagonists ● Mast cell stabilizers ● Monoclonal antibodies Mucolytic agents ● thin secretions ● nebulizer treatment ● guaifenesin ● Combo of guaifenesin and dextromethorphan can be taken orally to loosen secretions18 TB ● Infectious disease in the lungs caused by Myobacterium tuberculosis o Can spread to any organ in the blood Nursing Care ● Administer heated & humidified oxygen therapy ● Prevent infection transmission o Wear a N95 HEPA filter or powdered air purifying respirator o Place pt in a negative-ariflow room and imprement airborne precautions o Use barrier protection o Pt wears surgical mask if transporting out of the room o Pt should sneeze/cough into disposable tissues o Administer meds o Promote adequate nutrition ▪ Encourage fluid-intake and well-balanced diet for adequate caloric intake ▪ Ecourage foods rich in protein, iron & vitamins C and B ▪ Provide emotional support Coronary Arteriosclerosis: most common cause of cardiovascular disease ● Abnormal accumulation of lipid or fatty substances and fibrous tissue in the lining of arterial blood vessel walls ● The presence of inflammation attracts inflammatory cells, such as monocytes (macrophages) o Activated macrophages also release biochemical substances that can further damage the endothelium by contributing to the oxidation of low-density lipoprotein (LDL) o Following the transport of lipids into the arterial wall, smooth muscles cells proliferate and form a fibroud cap over a core filled with lipid and inflammatory infiltrate: ▪ Atheromas: protrude into the lumen of the vessel, narrowing it and obstructing blood flow ● A thrombus may then obstruct blow flow, leading to acute coronary syndrome (ACS), which then can result in an myocardial infarction (MI), a portion of the heart muscle no longer receives blood flow and becomes necrotic Clinical Manifestations ● Produces signs/symptoms according to the location and degree of narrowing of the arterial lumen, thrombus formation, and obstruction of blood flow to the myocardium ● Lack of blood flow is usually progressive, causing an inadequate blood supply that deprives the cardiac muscle cells of oxygen needed for their survival: known as ischemia ● Decrease in blood supply or long enough duration, irreversible damage and death to myocardial cells can occur19 ● Significant myocardial damage may result in persistently low cardiac output & heart failure where the heart cannot supply the body with enough blood ● Decrease in blood supply from CAD may cause the heart to abruptly stop beating: sudden cardiac death ● Most common manifestation of myocardial ischemia is the onset of chest pain ● Some complain of epigastric distress & pain that radiates to the jaw or left arm***** ● Pts with hx of diabetes or heart failure may report shortness of breath ● Women show symptoms: indigestion, nausea, palpitations, and numbness ● Major cardiac event may be the first indication of coronary atherosclerosis** Risk Factors ● Elevated low-density lipoprotein (LDL) cholesterol, known as bad cholesterol ● Pt at highest risk: those with known CAD, diabetes, peripheral arterial disease, abdominal aortic aneurysm, or carotid artery disease ● Metabolic Syndrome Nonmodifiable Risk Factors ● Family hx ● Increasing age (more than 45 yrs for men; more than 55 yrs for women) ● Gender (men develop CAD at an earlier age) ● Race (higher in African Americans than Caucasians) Modifiable Risk Factors ● Hyperlipidemia ● Smoking ● Hypertension ● Diabetes ● Metabolic syndrome ● Obesity ● Physical inactivity Diagnosis of this syndrome includes three of the following conditions: ● Insulin resistence ● Central obesity (waist circumference more than 35 inches in females, more than 40 inches in males) ● Dyslipidemia (triglycerides more than 150 mg/dL, HDL less than 50 mg/dL in females, less than 40 mg/dL in males) ● BP persistently greater than 130-85 mmHg ● Proinflammatory state (high levels of C-reactive protein) ● Prothrombotic state (high fibrinogen level) *many ppl with type 2 diabetes fit this* Pathophysiology20 Controlling Cholesterol Abnormalities ● A fasting lipid profile should demonstrate the following values: o LDL cholesterol less than 100mg/dL (less than 70mg/dL for very high-risk patients) o Total cholesterol less than 200mg/dL o HDL cholesterol greater than 40 mg/dL for males & greater than 50mg/dL o Triglyceride less than 150mg/dL Dietary Measures Total Calories: Balance intake & expenditure to maintain desirable weight Total Fat: 25-35% of total calories Saturated fat: <7% of total calories Polyunsaturated fat: up to 10% of total calories Monosaturated fat: up to 20% of total calories Carbohydrates: 50-60% of total calories Dietary fiber: 20-30 g/day Protein: approximately 15% of total calories Cholesterol: <200mg/day *Eat a treat* Physical Activity ● Atleast 150 minutes per week or vigorous intensity aerobic activity of atleast 75 minutes/week Medications ● Lipid-lowering meds can reduce CAD mortality in pts with elevated lipid levels and in at-risk pt with normal lipid levels o Types lipid lowering agents:21 ▪ 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) (or satins) ▪ Fibric acids (or fibrates) ▪ Bile acid sequestants (or resins) ▪ Cholesterol absorption inhibitors ▪ Omega-3 acid ethyl esters ▪ Proprotein convertase subtilisin-kexin type 9 Medication Therpeutic Effects Considerations HMG-CoA Reductase Inhibitors (Statins) Atovastatin (Lipitor) Simvastatin (Zocor) Total cholesterol LDL ^ HDL TGs -Enhibit enzyme involed in lipid synthesis -Favorable effects pm vascular endothelium, including anti-inflammatory & antithrombotic effects -Freq given as initial therapy for significantly ^ cholesterol & LDL levels -Myalgia & arthralgia: adverse effects -Myopathy & rhabdomyolysis: potential serious effects -Monitor liver function tests -contraindicted in liver disease -Check for drug interactions -Indication for use: ACS & stroke -Administer in evening Fibric Acids (Fibrates) Fenofibrate (TriCor) Gemfibrozil (Lopid) ^ HDL TGs Synthesis of TGs & other lipid -Adverse effects: diarrhea, flatulence, rash, myalgia -Serious: pancreatitis, heptoxicity, & rhabomyolsis -Containdicted in severe renal & liver disease -**Use with caution in pts who are taking satins*** Cholesterol Absorption Inhibitors Ezetimibe (Zeta) LDL Inhibits absorption of cholesterol in small intestine -Better tolerated than bile acid sequestrants -Used in combo w: satins -Side effects: abdominal pain, arthralgia, myalgia -Contraindicted in liver disease Omega-3-Acid Ethyl Easters Fish oil capsules TGs -May be used alone or in combo with other agents22 Inhibit TG production in liver -side effects: GI distress, taste perversion, rash, & back pain TG means: true glucose Angina ● chest pain that is brought about by myocardial ischemia ● associated a significant with a significance obstruction of at least one major coronary artery ● myocardium extracts a large amount of oxygen from the coronary circulation to meet its continuous demands ● when demand ^^^ flow thru the coronary arteries needs to be increased ● when there is a blockage in a coronary artery, flow cannot be increased and ischemia result Several factors associated: ● physical excretion, which precipitates an attack by ^ myocardial oxygen demand ● Exposure to cold, which causes vasoconstriction & elevated BP, with increased oxygen demand ● Eating a heavy meal, increases the blood flow to the mesenteric area for digestion, thereby reducing the blood supply available to the heart muscle o Severely compromised heart shunting of blood for digestion can be sufficient to induce anginal pain ● Stress or any emotion-provoking situation causing the release of catecholamines (increases BP, heart rate, myocardial workload) Stages of Angina: ● Stable angina: predictable & consistent pain that occurs on exertion and relieved by rest and/or nitroglycerin ● Unstable angina: (also called preinfarction angina or crescendo angina); symptoms increase in frequency&severity; may not be relieved w/ rest or nitroglycerin ● Intractable or refractory angina: severe incapitating chest pain ● Variant angina: (also called Prinzmetal’s angina): pain at rest w/ reversible ST-segment elevation; thought to be caused by coronary artery vasospasm ● Silent ischemia: objective evidence of ischemia (such as electrocardiographic changes w/ stress test), but pt reports no pain Medical Management ● Objectives of meds are to decrease the oxygen demand of the myocardium & to ^ oxygen supply Nitroglycerin23 ● Potent vasodilator that improves blood flow to the heart muscle & relieves pain ● Dilates primarily the veins & to a lesser extent, the arteries o Dilation of the veins causes venous pooling of blood throughout the body o As a result less blood returns to the heart & filling pressure (preload) is reduced o Relax the systemic arteriolar bed, lowering BP & decreasing overload ▪ These effects decrease myocardial oxygen requirements Beta-adrenergic Blocking Agents: metoprolol (Lopressor) ● Reduce myocardial oxygen consumption by blocking beta-adrenergic sympathetic stimulation to the heart ● Result: o Reduced HR o Slowed conduction of impulses thru the conduction system o Decreased BP o Reduced myocardial contractility (force of contraction) ● Beta-blockers balance the myocardial oxygen needs (demands) and the amount of oxygen available (supply) o Helps control chest pain & delays the onset of ischemia during work or exercise ● Reduce the incidence of recurrent angina, infarction, and cardiac mortality o Dose can be titrated to achieve a resting heart rate of 50-60 bpm Calcium Channel Blocking Agents: ● Decrease sinoatrial node automatically & atrioventricular node conduction resulting in: o Slower heart rate o Decrease in the strength of myocardial contraction (negative inotropic effect) ● ^ myocardial oxygen supply by dilating the smooth muscle wall of the coronary arterioles o They decrease oxygen demand by reducing systemic arterial pressure & the workload of the left ventricle ● Most commonly used: o Amlodipine (Norvasc) o Diltiazem (Cardizem) o They are commonly prescribed for hypertension Antiplatelet and Anticoagulant Medications: ● given to prevent platelet aggregation & subsequent thrombosis, which impledes blood flow thru the coronary arteries Aspirin ● prevents platelet aggregation & reduces the incidence of MI and death in pts with CAD24 ● Pts should contine taking even if also take other analgesics like acetaminophen (Tylenol) Adenosine Diphosphate Receptor Antagonists (P2Y12) ● Clopidogrel(Plavix) most commonly prescribed in addition to aspirin for pts at high rish for MI ● Prasugrel (Effient) may be prescribed during coronary events and interventions Heparin*** ● Prevents formation of new blood clots ● Dose of heparin is based on the results of the activated partial thromboplastin time(aPTT) ● Heparin therapy is considered therpuetic when the aPTT is 2-2.5 times the normal aPTT value *(TEST)* ● SQ injection of low-molecular-weight-heprin:enoxaparin (Lovenox) or dalteparin (Fargmin) may be used to treat pts with unstable angina or Non-ST-segment elevation myocardial infarction (NSTEMI) ● Heparin & warfarin can be used simultaneously Labs to use for heparin: aPTT Glycoprotein IIb/IIIa Agents ● Prevent platelet aggregation by blocking the GP IIb/IIIa receptors on the platelets, preventing adhesion of fibrinogen & other factors that crosslink platelets to each & form intracoronary vlots ● Examples: abciximab (ReoPro) or eptifibatide (Integrilin) ● IV administration indicated for hospitilazewd pts with unbstable agina & as adjunct therpay for PCI ● Like heparin, bleeding is the major side effect (initiate bleeding precations*** Nursing Interventions Treating Angina ● Pt experiencing agina should stop all activities and sit or rest in bed in a Semi-Fowler’s position ● Assess pt: vital signs & observe for signs of respiratory distress o If pt is in the hospital, a 12-lead ECG is obtained & assessed for ST-segment and T-wave changes ● Nitroglycerin is given sublingualy & pts response is assessed o Relief of chest pain and effet on BP & HR ● Assess BP, HR, and ST segment (if pt is on a monitor with ST-segment monitoring) each time Acute Coronary Syndrome ● Emergency situation characterized by an acute onset of myocardial ischemia that results in myocardial death25 Clinical Manifestations ● Chest pain that occur suddenly & continues despite rest & medications ● Combo of symptoms: chest pain, shortness of breath, indigestion, nausea, anxiety o Cool, pale, moist skin o HR and Respirations faster than normal Assessment and Diagnostic Findings (for Acute Coronary Syndrome & MI) ● Cardovascular o Chest pain/discomfort not relieved by rest or nitroglycerin ▪ Heart sounds: S3 & S4; new onset of murmur o Increased jugular venous distention if MI has caused heart failure o BP elevated bc of sympathetic stimulation or decreased bc of decreased contractibility, cardiogenic shock, or medications o Irregular pulse could indicate atrial fibrillation o ST-segment & T-wave changes, the electrocardiogram may also show tachycardia, bradycardia, or other dysrhythmias ● Respiratory o Shortness of breath, dyspnea, tachypnea, and crackles if MI has caused pulmonary congestion o Pulmonary edema may be present ● Gastrointestinal o Nausea, indigestion, vomiting ● Genitourinary o Decreased urinary output may indicate cardiogenic shock ● Skin o Cool, clammy, diaphoretic, and pale appearance due to sympathetic stimulkation may indicate cardiogenic shock ● Neurologic o Anxiety, restlessness, and lightheadedness may indicate ^ sympathetic stimulation o Or decrease in contractility and cervral oxygenation o Same symptoms could indicate cardiogenic shock ● Psychological o Fear with feeling of impending doom or denial that anything is wrong MI Classification ● Affected area of the heart: anterior, lateral, inferior, or posterior ● ECG changes produced: ST elevated myocardial infarction vs non-ST elevation myocardial infarction ● Time frame within the progression of the infarction: acute, evolving, old Heart Failure26 ● Clinical syndrome resulting from structural or functional cardiac disorders that impair the ability of the ventricles to fill or eject blood ● Referred to as Congestive Heart Failure bc many pts experience pulmonary or peripheral congestion with edema ● “Heart Failure”: indicates myocardial disease with impaired contraction of the heart (systolic dysfunction) or filling of the heart (diastolic dysfunction) may cause pulmonary or systemic congestion Chronic Heart Failure ● Approx.. 6 million ppl in the US have heart failure; 870,000 new cases each year ● Most common reason for hospitalization of ppl older than 65 ● 2nd most common reason for visits to physician’s offices ● Approx.. 25% of pts discharged after treatment for HF return within 30 days Clinical Manifestations Assessment (signs/symptoms) ● Congestion o Dyspnea o Orthopnea o Paroxysmal nocturnal dyspnea (difficulty breathing @ night) o Cough o Pulmonary crackles that do not clear w/ cough o Weight gain (rapid) o Dependent edema o Abdominal bloating or discomfort o Ascites o Jugular venous distention o Sleep disturbance o Fatigue ● Poor Profusion/Low Cardiac Output o Decreased exercise tolerance o Muscle wasting or weakness o Anorexia or nausea o Unexplained weight loss o Lightheadedness or dizziness o Unexplainable confusion or altered mental status o Resting tachycardia o Daytime oliguria w/ recumbent nocturia o Cool or vasoconstricted extremities o Pallor or cyanosis Left-sided Heart Failure: LUNGS ● Pulmonary congestion occure when the left ventricle cant effectively pump blood out to the aorta and the systemic circulation ● Increased left ventricular end-diastolic blood volume increase the left ventricular end diastolic pressure27 o Decreases blood flow from the left atrium into the left ventricle during diastole ● Blood volume & pressure build up in left atrium which decreases flow thru the pulmonary veins into the left atrium o Pulmonary blood volume and pressure increases in the lungs, forcing the fluid from the pulmonary capillaries into the pulmonary tissues and alveoli o Resulting in pulmonary intersistial edema & impaired gas exchange ● Clinical Manifestations: o Dyspnea, cough, pulmonary crackles, and low O2 sats o Extra heart sound; S3 or “ventricular gallop” could be heard bc of abnormal ventricular filling o orthopnea: difficulty breathing when lying flat o paroxysmal nocturnal dyspnea (PND): sudden attacks of dyspnea at night Right-Sided Heart Failure: SYSTEMS ● Right side cant eject blood effectively & cant accommodate all of the blood that normally returns to it from venous circulation o Causes congestion in the peripheral tissues & the viscera predominates Medical Management ● Treatment options depend on the severity and could be oral & IV meds, lifestyle changes, supplemental O2, and surgical interventions including: implantation of cardiac devices and cardiac transplant Medication Therapeutic Effects Considerations Angiotensin-Convertin Enzyme Inhibitors Lisinopril (Prinivil) Enalapril (Vasotec) BP and afterload Relieves s/s of HF Prevents progression of HF -Observe for symptomatic hypotension, increased serum K+, cough & worsening renal function Angiotensin Receptor Blockers Valsartan (Diovan) Losartan (Cozaar) BP and afterload Relieves s/s of Hf Prevents progression of HF -Observe for symptomatic hypotension, increased serum K+, worsening renal function Hydralazine and Isosorbide Dinitrate (Dilatrate) Dilates blood vessels BP and afterload -Observe for symptomatic hypotension Beta-Adrenergic Blocking Agents (Beta-Blockers) Carvedilol (Coreg) Bisoprolol (Zebeta) Dilates blood vessles s/s of HF and afterload -Observe for decreased heart rate, symptomatic hypotension, dizziness, fatigue28 Metoprolol (Lopresssor, Toprol XL) improves exercise capacity Diuretics Loop diuretic : Furosemide (Lasix) Thiazide diuretic : metolazone (Zaroxolyn) Hydrocholorothiazide (HCTZ) Aldosterone antagonist : Spironolactone (Aldactone) Fluid volume Overload S/S of HF Improves HF sysmptoms in advanced HF -Observe for electrolyte abnormalities, renal dysfunction, diuretic resistance, decreased BP -monitor I&O and daily weight -Observe for hyperkalemia & hyponatremia Digitalis Digoxin (Lanoxin) Improves cardiac contractility S/S of HF -observe for bradycardia and digitalis toxicity Pharmacologic Therapy ● Meds commonly prescribed: ACE inhibitors, beta-blockers, and diuretics o Diuretics improve symptoms but may not affect survival ● Hydralazine & Isosorbide Dinitrate o Combo is recommended for HF and may be more effective for African Americans who do not respond to ACE inhibitors ● Beta-Blockers o Produce side effects: dizziness, hypotension, bradycardia, fatigue, depression ● Digitalis o Key concern w/ digoxin: digitalis toxicity ** Physical Exam ● Assess: Rate and depth of respiration & effort required for breathing ● Auscultate: listen for S3 sounds, which is an early sign that increased blood volume fills the ventricle with each beat ● Assess: peripheral pulses and rate their volume on a scale from 0 (not palpable) to 3+ (bounding) ● Assess: feet and lower legs for edema; if pt is supine in bed assess sacrum and back also ● Assess: abdomen for tenderness and hepatomegaly ● Meaure urinary I&O’s o Oliguria: diminished urine out, less than 0.5 mL/kg/hr o Anuria: urine output less than 50mL/24hr29 o Significant change in weight (2-3lbs increase in a day or 5lbs increase in a week) tell provider and adjust meds Pulmonary Edema ● Abnormal accumulation of fluid in the interstitial spaces & alveoli of the lungs ● Results from left ventricular failure ● Rapid increase in atrial pressure results in an acute increase in pulmonary venous pressure o This produces an increase in hydrostatic pressure that forces fluid out of the pulmonary capillaries and into the interstitial spaces & alveoli ● Fluid within the alveoli mixes with air producing the classic sign of pulmonary edema: o Frothy pink (blood-tinged),sputum ● Large amounts of alveolar fulid creates a diffusion block that impairs gas exchange o Result: hypoxemia Clinical Manifestations ● Restless and anxiety ● Sudden onset of breathlessness; sense of suffocation ● Tachypneic w/ noisy breathing and low O2 sats ● Crackles ● Reduced urine output ● Confusion; stupor ● S3 heart sound: gallop Medical Managemant Rapid-acting diuretics: Furosemide & bumetanide, promote fluid excretion Morphine: decreases sympathetic nervous system response and anxiety and promotes mild vasodilation Vasodilators: (nitroglycerin) decrease preload and afterload Inotropic agent: (digoxin) improve cardiac output Antihypertensives: (ACE inhibitors & beta-blockers) decrease afterload Nursing Care ● pt is positioned upright w/ legs dangling over side of bed ● Monitor vital signs every 15min until stable ● Monitor I&O’s ● Monitor pulmonary wedge pressures; cardiac output ● Check ABG’s, electrolytes (esp potassium if on diuretics), SaO2, chest x-ray findings ● Maintain pt airway, suction if needed ● Administer high-flow oxygen ● Restrict fluid intake30 ● Monitor hrly urine output: watch for intake greater than output or hrly urine less than 30mL/hr Thromboembolism ● Intracardiac thrombi can form in pts with Afib bc the atria do not contract forcefully, resulting in slow turbulent flow ● Clots within the cardiac chambers can be detected by an echocardiogram o Treated with anticoagulant agents: heparin & warfarin ● S/S: o Leg pain and swelling, feels warm: DVT ● These clots can break off and travel thru the inferior vena cava & thru the right side of the heart into the pulmonary artery (causes pulmonary embolus) Pulmonary Embolism ● Blood clots in the lungs ● Indicators: o Dyspnea o Pleuritic chest pain o Tachypnea ● Diagnostic Tests: o Chest x ray o Ventilation-perfusion lung scan o High-resolution helical computed tomography o Computed tomographic pulmonary angiogram o Blood D-dimer assay is helpful screening test that identifies whether clotting and fibrinolysis are taking place somewhere in the body Peripheral Vascular Diseases ● Inadequate peripheral blood flow occurs when the heart’s pumping action becomes inefficient ● Circulatory insufficiency of the Extremities: o Most types of peripheral vascular disease result in ischemia o Symptoms: pain, skin changes, diminished pulses, possible edems ● Characteristic. Arterial. Venous ral Characteristics s mittent claudication to sharp, unrelenting, constant shed or abset ng, throbbing, cramping nt, but may be difficult to palpate thru edema entation in area of medial and lateral malleolus,31 characteristics ndent rubor—elevation pallor of foot; dry, shiny skin; cool to cold temp, loss of hair over toes and top of foot, nails thick & rigid skin thick and tough, may be reddish blue, frequently with associated dermitits Characteristics on of ulcer e base dema toes, toe webs, heel or other pressure areas if confined to bed paiful often involving joint space ar o black/dry gangreaen al unless extremity kept in dependent position constantly to relieve pain al malleolus, lateral malleolus, anterior tibial area al pain if superficial, could be very painful rficial lar border ulation tissue—beefy red to yellow fibrinous in chronic long term ulcer rate to severe32 Physical Assessment Palpation of pulses ● Determine presence/absence o Absence may indicate that the site is stenosis: narrowing or constricted ● Quality of peripheral pulses Diagnostic Evaluation Doppler Ultrasound Flow Studies ● When pulses cant be palpated, a handled continuous wave (CW) Doppler ultrasound is used to detect blood flow in vessels Venous thromboembolism ● Deep vein thrombosis (DVT) + pulmonary embolism (PE)= VTE ● Superficial veins, such as the greater saphenous, short saphenous (lesser saphenous), cephalic, basilic, and expternal jugular veins, are thick-walled muscular structures that lie under the skin o Deep & superficial veins have valves that permit unidirectional flow back to the heart Clinical Manifestations: ● S/S are non specific o Exception: phlegmasia cerulea dolens (massive iliofemoral venous thrombosis) ▪ The entire extremity is massively swollen, tense, painful, and cool to the touch ● Deep veins o Edema o Swelling ● Superficial veins o Pain or tenderness o Redness o Warmth in involved area Leg Ulcers ● Inadequate exchange of oxygen and other nutrients in the tissue Assessment and Diagnostic Findings ● Hx of condition is important ● Examine pulses in lower extremities: femoral, popliteal, posterior tibial, dorsalis pedis ● Cultures of the ulcer bed to determine whether an infecting agent is the primary cause Arteriosclerosis and Atherosclerosis ● Arteriosclerosis33 o Hardening of the arteries o Muscle fibers and the endothelial of the walls of small arteries and arterioles become thick ● Atherosclerosis o Affecting the intima of large and medium-sized arteries o Accumulation of lipids, calcium, blood compnents, carbs, and fibrous tissue on the intimal layer of the artery o Most common result: narrowing (stenosis) of the lumen, obstruction of thrombosis, aneurysm, ulceration, and rupture o Can develop at any point in the body o 2 types of lesions: ▪ Fatty streaks: yellow and smooth, protrude slightly into the lumen of the artery & composed of lipids and elongated smooth muscle cells ● Found in all age groups; even infants ● Do not cause clincal symptoms ▪ Fibroud plaques: smooth muscle cells, collagen fiber, plasma components, and lipids. ● White to white-yellow ● Protrude into the arterial lumen, sometimes completely obstructing it ● Found in the abdominal aorta and the coronary, popliteal, and internal carotid arteries’ ● Progressive lesions Peripheral Arterial Occulsive Disease ● Main symptom: intermittent claudication described as aching, cramping, or inducing fatigue or weakness that occurs w/ some degree of exercise or activity o Relieved with rest Pharmacologic Therapy: Pentoxifylline (Trental) & cilostazol (Pletal) o For treatment of symptomatic claudication ● Pentoxifylline o Increases erythrocyte flexibility, lowers blood fibrinogen concentrations, and inhibits neutrophil adhesion & activation ● Cilostazol o Phosphodiesterase III inhibitor; a direct vasodilator that inhibits platelet aggregation Antiplatelet agents: aspirin & clopidogrel (Plavix) ● Prevent formation of thromboemboli, which can lead to myocardial infarction and stroke Statins ● Improve endothelial function in pt w/ PAD ● Improve symptoms of intermittent claudication ● Increase walking distance to the onset of claudication34 Hypertension ● Systolic BP of 140 mmHg or higher or diastolic blood pressure of 90 mmHg or higher, based on the average of the two BP Classification Systolic BP Diastolic BP Normal <120 <80 Prehypertension 120-139 80-89 Stage 1 hypertension 140-159 90-99 Stage 2 hypertension Less than or equal 160 Less than equal 100 Medications ● Diuretics ● Calcium-channel blockers ● Angiotension-converting enzyme (ACE) inhibitors o Lisinopril and enalapril ● Angitension II receptor antagonists o Valsartan and losartan ▪ Good for pts taking ACE inhibitors who have a cough or hyperkalemia o Monitor for angioedema (swollen lips & face) and heart failure o Pt should avoid foods high in potassium and monitor serum potassium levels ● Aldosterone-receptor antagonists o Eplerenone; blocks aldosterone action ▪ Promotes the retention of potassium and excretion of sodium and water o Monitor kidney function, triglycerides, sodium & potassium levels o Pt education ▪ Hypertriclyceridemia, hyponatremia, kyperkalemia: risks increase as dose increases ▪ Grapefruit juice & St. John’s wort can increase adverse side effects ▪ No salt substitutes ● Beta-Blockers ● Central-alpha2 agonists o Clonidine o Reduce peripheral vascular resistance & decrease BP by inhibiting the reuptake of norepinephrine o Monitor BP and pulse ● Alpha-adrenergic Antagonists o Prazosin o Reduce BP by causing vasodilation o Start w/ low dose, usually given at night o Monitor BP for 2hr after administration35 [Show More]
Last updated: 1 year ago
Preview 1 out of 35 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 16, 2021
Number of pages
35
Written in
Additional information
This document has been written for:
Uploaded
May 16, 2021
Downloads
0
Views
30



 (4).png)





.png)