*NURSING > Class Notes > Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 5,GRADED A (All)
Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 5,GRADED A
Document Content and Description Below
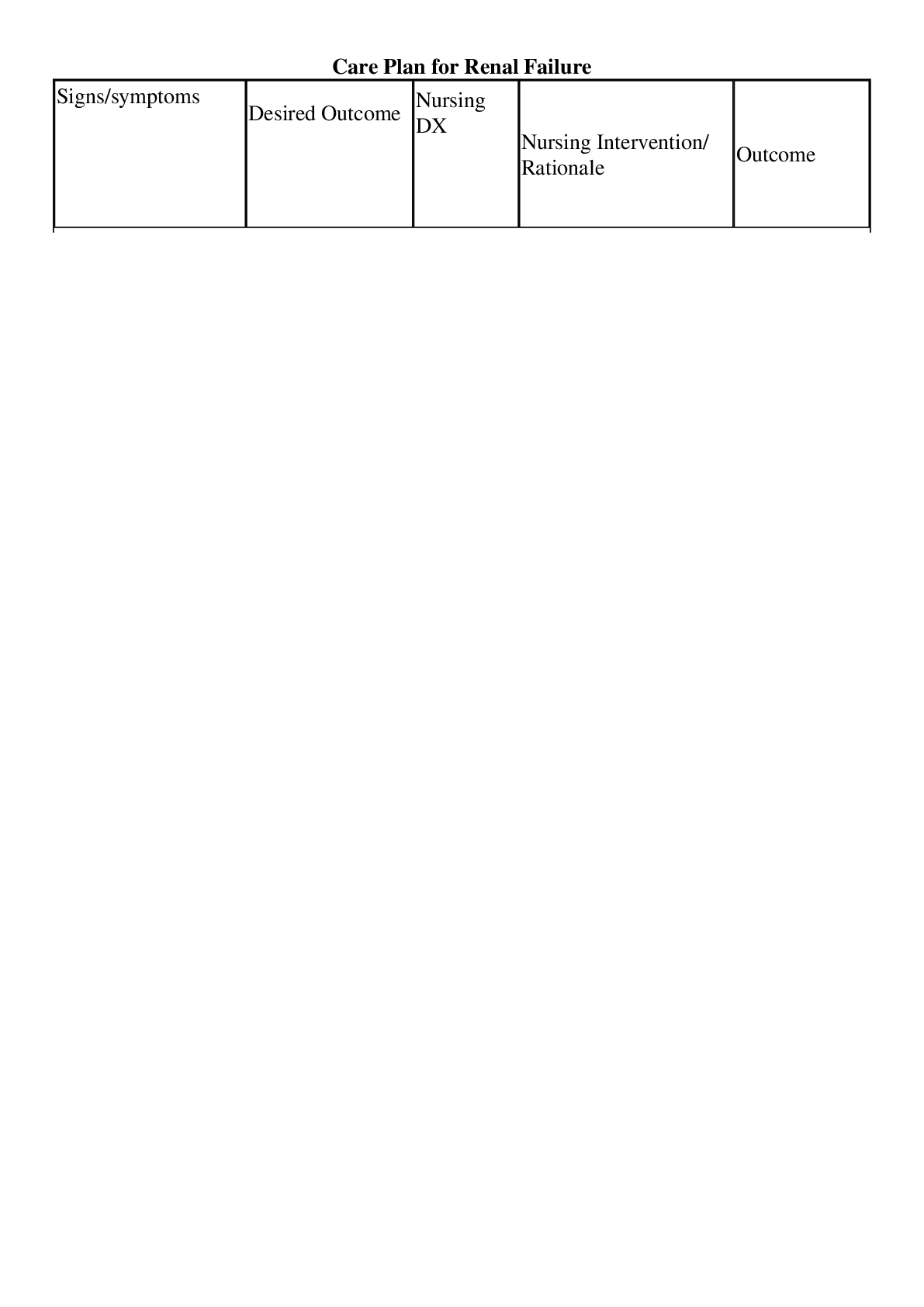
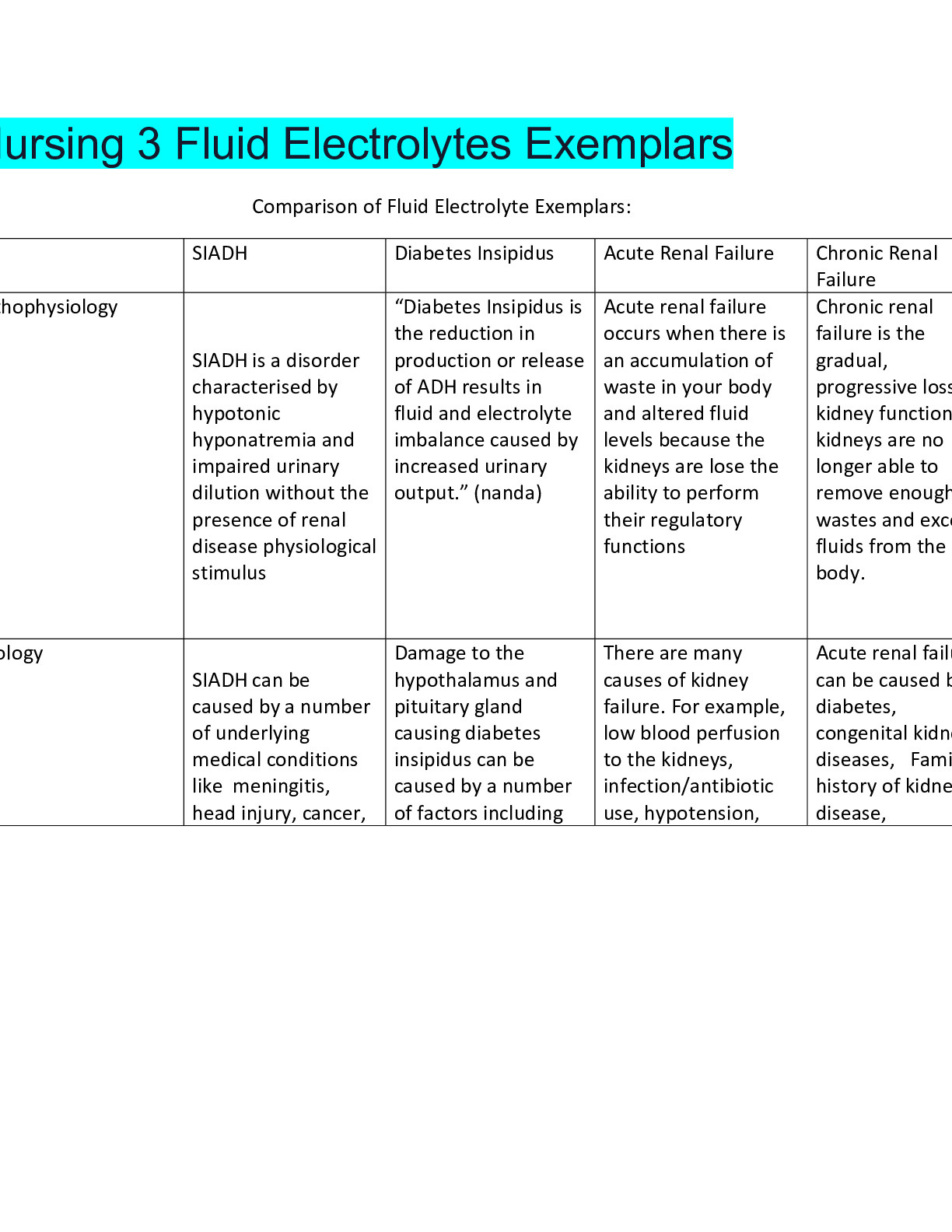
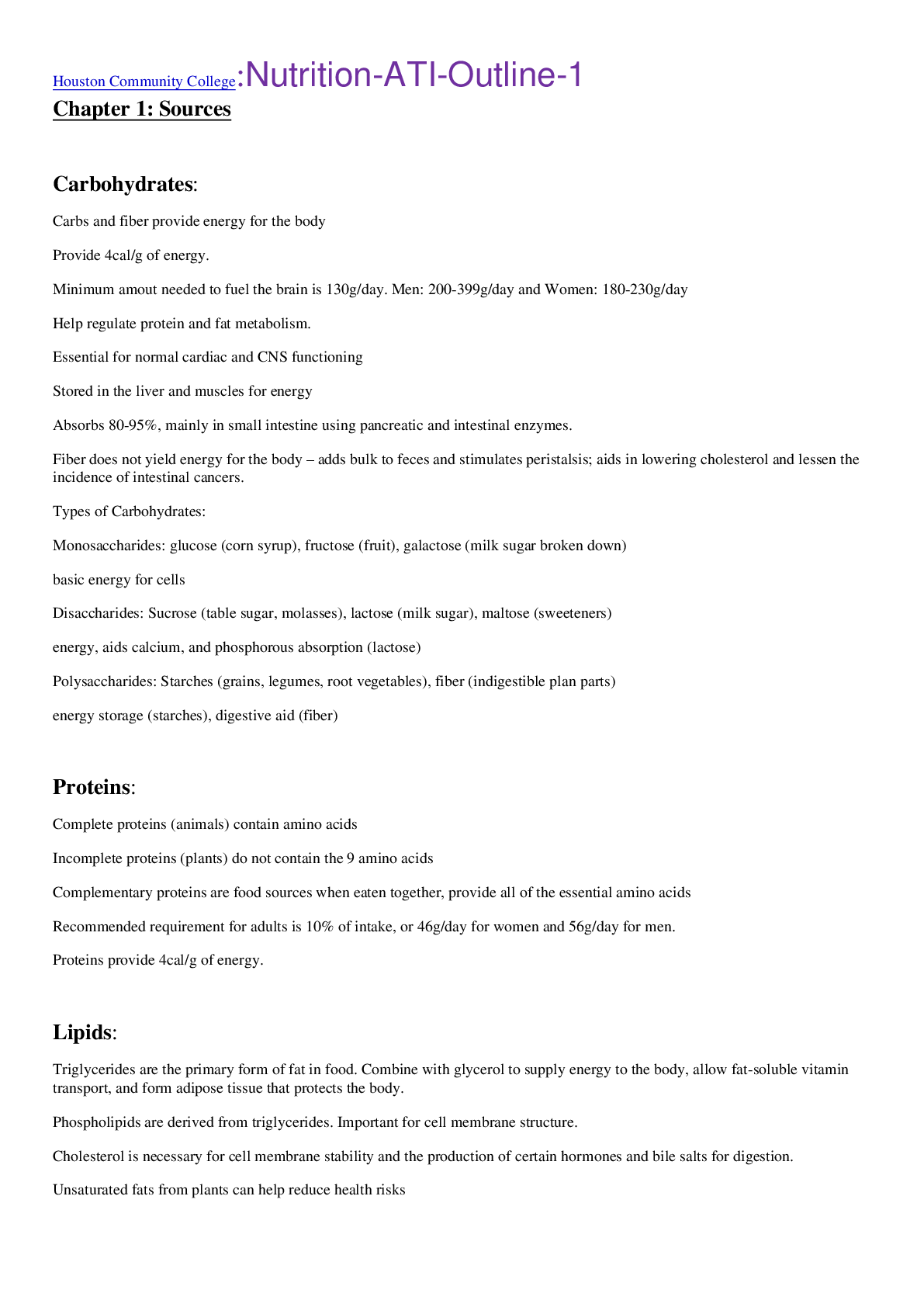
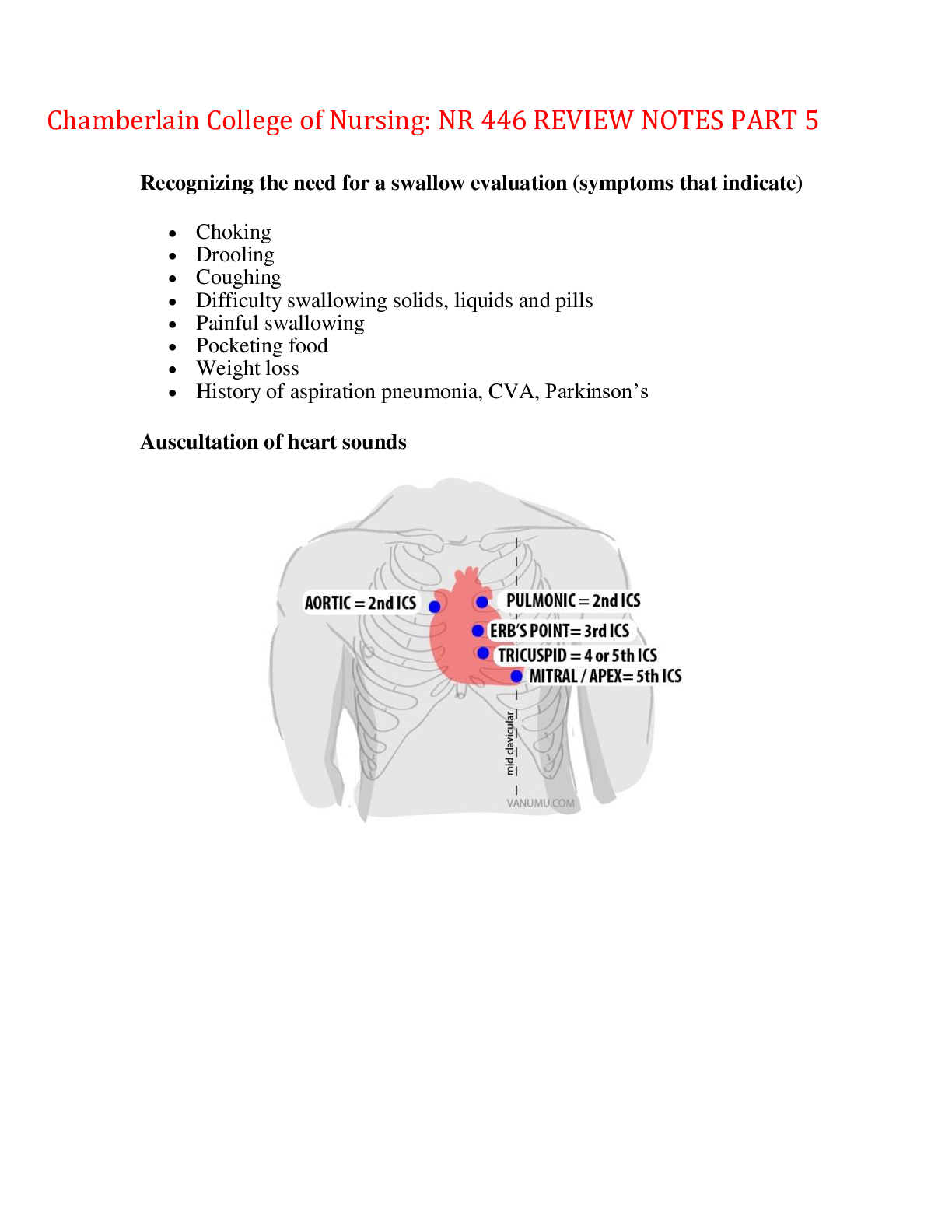
Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 5 Recognizing the need for a swallow evaluation (symptoms that indicate) • Choking • Drooling • Coughing • Difficulty swallowi... ng solids, liquids and pills • Painful swallowing • Pocketing food • Weight loss • History of aspiration pneumonia, CVA, Parkinson’s Auscultation of heart sounds Nursing interventions and management for bacterial meningitis. 1) Health Promotion and Disease Prevention: • Haemophilus influenzae type b (Hib) vaccine – Ensure infants receive vaccine for bacterial meningitis on schedule. • Pneumococcal polysaccharide vaccine (PPSV) – Vaccinate adults who are immunocompromised, who have a chronic disease, who smoke cigarettes, or who live in a long-term care facility. CDC guidelines should be followed for revaccination. Give one dose to adults older than 65 years of age who have not previously been vaccinated nor have history of disease. • Meningococcal vaccine (MCV4) (Neisseria meningitidis) – Ensure that adolescents receive the vaccine on schedule and prior to living in a residential setting in college. Individuals in other communal living conditions (military) also should be immunized. 2) Client Education • Use an insect repellent when risk of being bitten by a mosquito exists. 3) Nursing Care • Isolate the client as soon as meningitis is suspected. Maintain isolation precautions per hospital policy. • This should be droplet precautions, which require a private room. Droplet precautions should continue until antibiotics have been administered for 24 hr and when oral and nasal secretions are no longer infectious. • Standard precautions are implemented for all clients who have meningitis. Clients who have bacterial meningitis should remain on droplet precautions continuously. • Implement fever-reduction measures, such as a cooling blanket, if necessary. • Report meningococcal infections to the public health department. • Decrease environmental stimuli. • Provide a quiet environment. • Minimize exposure to bright light (natural and electric). • Maintain bed rest with the head of the bed elevated to 30°. • Monitor the client for increased intracranial pressure (ICP). Tell the client to avoid coughing and sneezing, which increase ICP. • Maintain client safety, such as seizure precautions. • Replace fluid and electrolytes as indicated by laboratory values. • Older adult clients are at an increased risk for secondary complications, such as pneumonia. 4) Medications • Ceftriaxone (Rocephin) or cefotaxime (Claforan) in combination with vancocin (Vancomycin) • Antibiotics given until culture and sensitivity results are available. Effective for bacterial infections. • Phenytoin (Dilantin) • Anticonvulsants given if ICP increases or client experiences a seizure. • Decadron (dexamethasone) • Corticosteroid, may improve outcome in adults if given before first dose of antibiotic • Acetaminophen (Tylenol), ibuprofen (Motrin) • Analgesics for headache and/or fever – nonopioid to avoid masking changes in the level • of consciousness. • Ciprofloxacin (Cipro), rifampin (Rifadin), or ceftriaxone (Rocephin) • Prophylactic antibiotics given to individuals in close contact with the client. 5) Potential Complications/Observe for these possible complications: • Increased ICP (possibly to the point of brain herniation) • Syndrome of inappropriate antidiuretic hormone (SIADH) • Septic emboli (leading to disseminated intravascular coagulation or cardiovascular accident) Evaluating client understanding of SSRI: • Select Prototype Medication: Paroxetine (Paxil); Other Medications: Sertraline (Zoloft),Escitalopram (Lexapro),Fluoxetine (Prozac),Fluvoxamine (Luvox) 1) Therapeutic Uses: • Paroxetine: GAD<generalized anxiety disorder>, Panic disorder<decreases both the frequency and intensity of panic attacks and also prevents anticipatory anxiety about attacks>, Obsessive-compulsive disorder (OCD) <reduces manifestations by increasing serotonin>, Social anxiety disorder, Trauma- and stressor-related disorders, & Depressive disorders • Sertraline: is indicated for panic disorder, OCD, social anxiety disorder, and PTSD. • Escitalopram: is indicated for GAD and OCD. • Fluoxetine:is used for panic disorder and OCD. • Fluvoxamine: is used for OCD and social anxiety disorder. 2) Nursing Administration: • Advise clients that medications may be taken with food. Taking medication in the morning minimizes sleep disturbances. • Instruct clients to take the medication on a daily basis to establish therapeutic plasma levels. • Assist with medication regimen adherence by informing clients that it may take up to 4 weeks to achieve therapeutic effects from an SSRI. 3) Medication Effectiveness: • Maintaining normal sleep pattern • Verbalizing feeling less anxious and more relaxed • Greater ability to participate in social and occupational interactions 4) Expected Pharmacological Action: • Paroxetine selectively inhibits serotonin reuptake, allowing more serotonin to stay at the junction of the neurons. • It does not block uptake of dopamine or norepinephrine. • Paroxetine produces CNS stimulation, which can cause insomnia. • The medication has a long effective half-life. A time frame of up to 4 weeks is necessary to produce therapeutic medication levels. • Planning care for pt who is going through alcohol withdrawal o Withdrawal Manifestations › Effects usually start within 4 to 12 hr of the last intake of alcohol, peak after 24 to 48 hr, and then suddenly disappear. › Manifestations include abdominal cramping; vomiting; tremors; restlessness and inability to sleep; increased heart rate; transient hallucinations or illusions; anxiety; increased blood pressure, respiratory rate, temperature; and tonic-clonic seizures. › Alcohol withdrawal delirium may occur 2 to 3 days after cessation of alcohol and may last 2 to 3 days. This is considered a medical emergency. Symptoms include severe disorientation, psychotic symptoms (hallucinations), severe hypertension, cardiac dysrhythmias, and delirium. Symptoms may progress to death. o Safety is the primary focus of nursing care during acute intoxication or withdrawal. Maintain a safe environment to prevent falls; implement seizure precautions as necessary. Provide close observation for withdrawal symptoms, possibly one- on-one supervision. Physical restraint should be a last resort. Orient the client to time, place, and person. Maintain adequate nutrition and fluid balance. Create a low-stimulation environment. Administer medications as prescribed to treat the effects of intoxication or to prevent or manage withdrawal. Monitor for covert substance use during the detoxification period. ◯ Nursing Considerations Monitor the client’s vital signs and neurological status. Provide for client safety by implementing seizure precautions. o Pharmacological Therapy Alcohol withdrawal – Diazepam (Valium), lorazepam (Ativan), carbamazepine (Tegretol), clonidine (Catapres), chlordiazepoxide (Librium) Alcohol abstinence – Disulfiram (Antabuse), naltrexone (Revia), acamprosate (Campral) o Client Education Encourage the client to adhere to the treatment plan. Advise client taking disulfiram to avoid all alcohol. Provide emotional support and reassurance to the client and family. ■ Educate the client and family about codependent behaviors. • Begin to educate the client and family about addiction and the initial treatment goal of abstinence. • Educate the client and family regarding removing any prescription medications in the home that are not being used. Encourage the client not to share medication with someone for whom that medication is not prescribed. • Begin to develop motivation and commitment for abstinence and recovery (abstinence plus working a program of personal growth and self-discovery). • Encourage self-responsibility. • Help the client develop an emergency plan – a list of things the client would need to do and people he would need to contact. • Encourage attendance at self-help groups. • Contraindications for Statins o Pregnancy Risk Category X. o Contraindicated in clients who have hepatitis induced by viral infection or alcohol. o Rosuvastatin should be avoided for clients of Asian descent or prescribed in a smaller dose than for other clients. o Use cautiously in older adult clients, clients in debilitated condition, and those who have chronic renal disease. Expected physiological findings in elderly (more than 65 years) -Kidney size and function decrease with aging. -Blood flow adaptability decreases, especially during a hypotensive or hypertensive crisis. -Glomerular filtration rate (GFR) decreases by half the rate of a young adult. -Medical conditions – diabetes, hypertension, and heart failure can affect GFR. -Kidney injury can occur more easily from contrast dyes and medication due to decreased renal size, blood flow, and GFR. -Tubular changes can cause urgency and nocturnal polyuria. -Weak urinary sphincter muscle and shorter urethra in women can cause incontinence and urinary tract infections. -Enlarged prostate in men can cause urinary retention and infection. Intramuscular sites and rationale for selection. Intramuscular sites are appropriate for irritating medications, solutions in oils, and aqueous suspensions. Common sites include ventrogluteal, deltoid, and vastus lateralis (pediatric). Dorsogluteal site is not recommended due to its proximity to sciatic nerve. Use a needle size 18- to 27-gauge (usually 22- to 25-gauge), 1- to 1.5-inch long, and inject at a 90° angle. Volume injected is usually 1 to 3 mL. If a greater amount is required, it should be divided into two syringes and two different sites should be used. In adults give IM immunizations into the deltoid. Cleft Palate Post Operative Care Cleft lip and cleft palate repair - Perform standard postoperative care, including assessment of vital signs and pain management using an age-appropriate tool. - Keep the infant pain-free to decrease crying and stress on repair. - Administer analgesics as prescribed. - Assess the operative sites for signs of crusting and infection. - Avoid sucking on nipple or pacifier. - Avoid hard toys that the infant may bring to their mouth to protect the incision site. - Monitor I&O and weigh daily. - Observe the family’s interaction with the infant. - Assess family coping and support Cleft palate repair - Change the infant’s position frequently to facilitate breathing. The infant may be placed on the abdomen in the immediate postoperative period. - Maintain intravenous fluids until the infant is able to eat and drink. - Monitor packing, which is usually removed in 2 to 3 days. - Avoid placing objects (tongue depressor, pacifier) in the infant’s mouth after cleft palate repair - Elbow restraints may needed to be used to prevent the infant from injuring the repair Client Education - Inform the parents that the infant may require elbow restraints for 4 to 6 weeks. - Instruct the parents in the proper use of the restraints. - Instruct the parents on the postoperative diet and feeding techniques. - Instruct parents in proper care of operative site. Medical Errors/Variance Report Incident Reports (Unusual Occurrences) - Incident/variance reports are an important part of a facility’s quality improvement plan. - An incident is the occurrence of an accident or an unusual event. Examples of incidents are medication errors, falls, and needlesticks. - Nurses must document the facts without judgment or opinion. - Nurses must not refer to an incident report in the client’s medical record. - Incident reports contribute to changes that help improve health care quality. Common medication errors - Wrong medication or IV fluid - Incorrect dose or IV rate - Wrong client, route, or time - Administration of known allergic medication - Omission of dose - Incorrect discontinuation of medication or IV fluid Assessment/Data Collection - Ensure knowledge of medication to be administered and why the client is receiving it. - Obtain information about the client’s medical diagnoses and conditions related to medication administration, such as the ability to swallow, allergies, heart, liver, and/or kidney disorders. - Identify the client’s allergies. - Obtain necessary preadministration data (heart rate, blood pressure) to assess appropriateness of medication and obtain baseline data to evaluate effectiveness of medication. - Omit or delay doses as indicated by the client’s condition. - Determine if the medication prescription is complete – To include the client’s name, date and time, name of medication, dosage, route of administration, time and frequency, and signature of the prescribing provider. - Interpret the medication prescription accurately. Refer to the ISMP lists. - Question the provider if the prescription is unclear or seems inappropriate for the client’s condition. Refuse to administer a medication if it is believed to be unsafe. Notify the charge nurse or supervisor. - Dosage changes are usually made gradually. Question the provider if abrupt and excessive changes in dosages are made. Planning - Identify client outcomes for medication administration. - Set priorities. Implementation - Avoid distractions during medication preparation (poor lighting, phones). Interruptions may increase the risk of error. - Prepare medications for one person at a time. - Check the labels for the medication name and concentration. Read labels carefully. Measure doses accurately, and double-check high-alert medications such as insulin and heparin with a colleague. Check the medication expiration date. - Doses are usually one to two tablets or one single-dose vial. Question multiple tablets or vials for a single dose. - Follow the six rights of medication administration consistently. Take the MAR to the bedside. - Only give medications that have been personally prepared. Evaluation - Evaluate the client’s response to a medication, and document and report appropriately. - Recognize side/adverse effects, and document and report appropriately. - Report all errors, and implement corrective measures immediately. How to maintain confidentiality and information security. The Privacy Rule of HIPAA requires that nurses protect all written and verbal communication about clients. Components of the privacy rule include: Only health care team members directly responsible for the client’s care should be allowed access to the client’s records. Nurses may not share information with other clients or staff not involved in the care of the client. Clients have a right to read and obtain a copy of their medical record, and agency policy should be followed when the client requests to read or have a copy of the record. No part of the client record can be copied except for authorized exchange of documents between health care institutions. For example: Transfer from a hospital to an extended care facility Exchange of documents between a general practitioner and a specialist during a consult Client medical records must be kept in a secure area to prevent inappropriate access to the information. Using public display boards to list client names and diagnoses is restricted. Electronic records should be password-protected, and care must be taken to prevent public viewing of the information. Health care workers should use only their own passwords to access information. Health information systems (HIS) are used to manage administrative functions and clinical functions. The clinical portion of the system is often referred to as the clinical information systems (CIS). The CIS may be used to coordinate essential aspects of client care. In order to comply with HIPAA regulations, each health care facility has specific policies and procedures designed to monitor staff adherence, technical protocols, computer privacy, and data safety. Information security protocols include: Logging off from the computer before leaving the workstation to ensure that others cannot view protected health information (PHI) on the monitor Never sharing a user ID or password with anyone Never leaving a client’s chart or other printed or written PHI where others can access it Shredding any printed or written client information used for reporting or client care after it is no longer needed. 2.) Isolation/treatment of herpes simplex. Identification between 1 and 2. Contact precautions protect visitors and caregivers when they are within 3 ft of the client against direct client and environmental contact infections (respiratory syncytial virus, shigella, enteric diseases caused by micro-organisms, wound infections, herpes simplex, impetigo, scabies, multidrug-resistant organisms). Contact precautions require: A private room or a room with other clients with the same infection. Gloves and gowns worn by the caregivers and visitors. Disposal of infectious dressing material into a single, nonporous bag without touching the outside of the bag. Herpes simplex viruses -- more commonly known as herpes -- are categorized into two types: herpes type 1 (HSV-1, or oral herpes) and herpes type 2 (HSV-2, or genital herpes). Most commonly, herpes type 1 causes sores around the mouth and lips (sometimes called fever blisters or cold sores). HSV-1 can cause genital herpes, but most cases of genital herpes are caused by herpes type 2. In HSV-2, the infected person may have sores around the genitals or rectum. Although HSV-2 sores may occur in other locations, these sores usually are found below the waist. Early Decelerations Early Decelerations: Slowing of fetal heart rate with start of contraction with return of fetal heart rate to baseline at end of contraction Cause: Compression of the fetal head resulting from uterine contraction Management: Identify labor progress, vaginal exam, fundal pressure, no intervention required Evaluating Effectiveness of Allopurinol Indications: Prevention of gouty arthritis and nephropathy; Treatment of secondary hyperuricemia which may occur during treatment of tumors or leukemias. Action: Inhibits the production of uric acid by inhibiting the action of xanthine oxidase. Therapeutic Action: Lowers serum uric acid levels Assessment: • Monitor intake and output ratios. Decreased kidney function can cause drug accumulation and toxic effects. Ensure that patient maintains adequate fluid intake (minimum 2500– 3000 mL/day) to minimize risk of kidney stone formation.. • Assess patient for rash or more severe hypersensitivity reactions. Discontinue allopurinol immediately if rash occurs. Therapy should be discontinued permanently if reaction is severe. Therapy may be reinstated after a mild reaction has subsided, at a lower dose (50 mg/day with very gradual titration). If skin rash recurs, discontinue permanently. • Gout: Monitor for joint pain and swelling. Addition of colchicine or NSAIDs may be necessary for acute attacks. Prophylactic doses of colchicine or an NSAID should be administered concurrently during the first 3–6 mo of therapy because of an increased frequency of acute attacks of gouty arthritis during early therapy. • Lab Test Considerations: Serum and urine uric acid levels usually begin to ↓ 2–3 days after initiation of oral therapy.. • Monitor blood glucose in patients receiving oral hypoglycemic agents. May cause hypoglycemia.. Patient/Family Teaching • Instruct patient to take allopurinol as directed. Take missed doses as soon as remembered. If dosing schedule is once daily, do not take if remembered the next day. If dosing schedule is more than once a day, take up to 300 mg for the next dose. • Instruct patient to continue taking allopurinol along with an NSAID or colchicine during an acute attack of gout. Allopurinol helps prevent, but does not relieve, acute gout attacks. • Alkaline diet may be ordered. Urinary acidification with large doses of vitamin C or other acids may increase kidney stone formation (see Appendix M). Advise patient of need for increased fluid intake. • May occasionally cause drowsiness. Caution patient to avoid driving or other activities requiring alertness until response to drug is known. • Instruct patient to report skin rash, blood in urine, or influenza symptoms (chills, fever, muscle aches and pains, nausea, or vomiting) to health care professional immediately; skin rash may indicate hypersensitivity. • Advise patient that large amounts of alcohol increase uric acid concentrations and may decrease the effectiveness of allopurinol. Evaluation/Desired Outcomes • Decreased serum and urinary uric acid levels. May take 2–6 wk to observe clinical improvement in patients treated for gout. • Normal Uric Acid level between 3.5-7.2 mg/dL Chronic Kidney Disease Chronic kidney disease (CKD) is a progressive, irreversible kidney disease. Risk Factors and Causes of Chronic Kidney Disease- • Acute kidney injury • Diabetes mellitus • Chronic glomerulonephritis • Nephrotoxic medications (gentamicin, NSAIDs) or chemicals • Hypertension, especially if African American • Autoimmune disorders (systemic lupus erythematosus) • Polycystic kidney • Pyelonephrosis • Renal artery stenosis • Recurrent severe infections CKD is comprised of five stages: • Stage 1: Minimal kidney damage with normal GFR (greater than 90 mL/min) • Stage 2: Mild kidney damage with mildly decreased GFR (60 to 89 mL/min) • Stage 3: Moderate kidney damage with moderate decrease in GFR (30 to 59 mL/min) • Stage 4: Severe kidney damage with severe decrease in GFR (15 to 29 mL/min) • Stage 5: Kidney failure and end-stage kidney disease with little or no glomerular filtration (less than 15 mL/min) Health Promotion and disease prevention • Encourage clients to drink at least 3 L of water daily. Consult with the provider regarding any restrictions. • Promote smoking cessation. • Encourage diet and activities to control or prevent diabetes and hypertension Subjective and objective Data • Fatigue, lethargy, involuntary movement of legs, depression, intractable hiccups • Neurologic – lethargy, decreased attention span, slurred speech, tremors or jerky movements, ataxia, seizures, coma • Cardiovascular – fluid overload (jugular distention; sacrum, ocular or peripheral edema), hypertension, dysrhythmias, heart failure, orthostatic hypotension • Respiratory – uremic halitosis with deep sighing, yawning, shortness of breath, tachypnea, hyperpnea, Kussmaul respirations, crackles, pleural friction rub, frothy pink sputum • Hematologic – anemia (pallor, weakness, dizziness), ecchymoses, petechiae, melena • Gastrointestinal – ulcers in mouth and throat, foul breath, blood in stools, nausea, vomiting • Musculoskeletal – osteodystrophy (thin fragile bones) • Renal – urine contains protein, blood, particles; change in the amount, color, concentration • Skin – decreased skin turgor, yellow cast to skin, dry, pruritus, urea crystal on skin (uremic frost) • Reproductive – erectile dysfunction Laboratory Tests Urinalysis- Hematuria, proteinuria, and decrease in specific gravity. Serum creatinine- Gradual increase over months to years for CKD exceeding 4 mg/dL. May be as high as 15 to 30 mg/dL. BUN-Gradual increase with elevated serum creatinine over months to years for CKD. May be as high as 180 to 200 mg/dL. Serum electrolytes-Decreased sodium (dilutional) and calcium; increased potassium, phosphorus, and magnesium. CBC-Decreased hemoglobin and hematocrit from anemia secondary to the loss of erythropoietin in CKD. Diagnostic Procedures Ultrasound, Kidneys, ureter, and bladder (KUB), Computerized tomography (CT), Magnetic resonance imaging (MRI) without contrast dye, Aortorenal angiography, Cystoscopy, Retrograde pyelography, Kidney biopsy Complications of CKD Potential complications of kidney failure include electrolyte imbalance, dysrhythmias, fluid overload, hypertension, metabolic acidosis, secondary infection, and uremia. Nursing Care Urinary elimination patterns (amount, color, odor, and consistency), Vital signs (blood pressure may be increased or decreased), Weight – 1 kg (2.2 lb) daily weight increase is approximately 1 L of fluid retained, Assess and monitor vascular access or peritoneal dialysis insertion site, Obtain a detailed medication and herb history to determine the client risk for continued kidney injury, Control protein intake based on the client stage of chronic kidney disease and type of dialysis prescribed, Restrict the client dietary sodium, potassium, phosphorous, and magnesium, Provide the client a diet that is high in carbohydrates and moderate in fat, Restrict the client intake of fluids (based on urinary output), Monitor for weight gain trends, Adhere to meticulous cleaning of areas on skin not intact and access sites to control infections, Balance the client activity and rest, Prepare the client for hemodialysis, peritoneal dialysis, and hemofiltration if indicated, Provide skin care to the client in order to increase comfort and prevent breakdown, Protect the client from injury, Provide emotional support to the client and family, Encourage the client to ask questions and discuss fears, Administer medications as prescribed. Medications Avoid administering antimicrobial medications (e.g., aminoglycosides and amphotericin B), NSAIDs, angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers, and IV contrast dye, which are nephrotoxic. Digoxin (Lanoxin), a cardiac glycoside, increases contractility of the myocardium and promotes cardiac output. Monitor digoxin laboratory levels due to slow excretion of the medication with CKD. Administer digoxin (Lanoxin) after receiving dialysis. Sodium polystyrene (Kayexalate) to increase elimination of life-threatening serum potassium, which may cause dangerous cardiac dysrhythmias and peaked T waves. Restrict sodium intake. Sodium polystyrene contains sodium and can cause fluid retention and hypertension, a complication of CKD. Erythropoietin alfa (Epogen, Procrit) to stimulate production of red blood cells, given for anemia Ferrous sulfate (Feosol), an iron supplement to prevent severe iron deficiency. Aluminum hydroxide gel (Amphojel)- Taken with meals to bind phosphate in food and stop phosphate absorption and take 2 hr before or after digoxin. Furosemide (Lasix), a loop-diuretic administered to excrete excess fluids- Avoid administering to a client who has end-stage kidney disease and clients may also receive thiazide diuretics, potassium-sparing diuretics, and osmotic diuretics. Teamwork and Collaboration • Nephrology services may be consulted to manage dialysis or kidney failure. • Nutritional services may be consulted to manage the nutritional needs of the client. Therapeutic Procedures • Hemodialysis • Care after Discharge • Nephrology services may be indicated if the client is to receive outpatient dialysis. • Refer the client to a community support group relating to the disease. • Nutritional services may be consulted for the client’s dietary needs. • Refer the client to a smoking-cessation support group and counseling if needed. Client Education • Instruct the client to monitor the daily intake of carbohydrates, proteins, sodium, and potassium, according to the provider. • Instruct the client to monitor fluid intake according to fluid restriction prescribed by the provider. • Encourage the client who has diabetes mellitus to adhere to strict blood glucose control because uncontrolled diabetes is a major risk factor for chronic kidney disease. • Instruct the client to avoid antacids containing magnesium. • Encourage the client to take rest periods from activity. • Educate the client who is receiving hemodialysis or peritoneal dialysis on an outpatient basis. • Educate the client on how to measure blood pressure and weight at home. • Encourage the client to ask questions and discuss fears. • Encourage the client to diet, exercise, and take medication as prescribed. • Advise the client to notify the provider if she observes signs of skin breakdown. Infection mononucleosis Infectious mononucleosis (mono) is often called the kissing disease. The virus that causes mono is transmitted through saliva, so you can get it through kissing, but you can also be exposed through a cough or sneeze, or by sharing a glass or food utensils with someone who has mono. However, mononucleosis isn't as contagious as some infections, such as the common cold Spread- “Contact” The cause of mononucleosis is the Epstein-Barr virus. Mononucleosis usually isn't very serious. Most adults have been exposed to the Epstein-Barr virus and have built up antibodies. They're immune and won't get mononucleosis again. Incubation- 4 t0 6 weeks Communicability- unknown Risk Factors • Immunocompromised status • Crowded living conditions • Poor sanitation • Poor nutrition • Poor oxygenation and impaired circulation • Chronic illness • Recent exposure to a known case of a communicable disease Subjective and objective findings- • Headache, malaise, and fatigue • Loss of appetite • Fever, sore throat • Puffy eyes • Cervical adenopathy • Splenomegaly (tender upper abdomen), which may persist for months • Palatine petechiae • Pharyngitis/tonsillitis exudate • Elevated WBC and atypical lymphocytes detected • Possible liver enzymes elevation (AST, ALT) with possible jaundice Complication- Few complications, but ruptured spleen may result from blow to upper abdomen if splenomegaly is present. Reye syndrome may be associated with the use of aspirin during a viral illness. Nursing Action- Nursing care is provided in the ICU and includes maintaining vital functions, assisting with lumbar puncture, obtaining blood samples, administering IV fluids, performing nasogastric intubation, and inserting an indwelling urinary catheter. Laboratory Tests • CBC • Electrolyte panels • Mono spot blood test for infectious mononucleosis Treatment • Risk of rash with some medications. Amoxicillin and other penicillin derivatives aren't recommended for people with mononucleosis. In fact, some people with mononucleosis who take one of these drugs may develop a rash. The rash, however, doesn't necessarily mean that they're allergic to the antibiotic. If needed, other antibiotics that are less likely to cause a rash are available to treat infections that may accompany mononucleosis. • Corticosteroids. To ease some of your symptoms, such as severe swelling of your throat and tonsils, your doctor may prescribe a corticosteroid medication such as prednisone. Care after discharge • Drink plenty of water • Take over the counter pain reliever • Gargle with salt water Addressing family concerns- when advocating for patients: One of the most vital and basic functions of a RN is the duty to intervene when the safety or well being of a client is obviously at risk. Effective communication requires commitment, effort, focus, and cooperation especially when dealing with complex clinical issues and people who have diverse backgrounds and perspectives. The purpose of communication is to build and maintain helping relationships with clients, families and significant others. Therapeutic communication is client-centered, purposeful, planned and goal directed. Interventions and findings for fracture/cast: Fracture: Physical assessment findings: Crepitus- which is a grating sound created by the rubbing of bone fragments Deformity- may observe internal rotation of extremity, shortened extremity, visible bone with open fracture Muscle spasms- Occur from the pulling forces of bone when not aligned Edema- swelling from trauma Ecchymosis- bleeding into underlying soft tissues from trauma Interventions: Provide emergency care at this time of injury, maintain ABC’s, monitor patients V/S and neurological status, place patient in SUPINE position, stabilize injured area including joints above and below the fracture, avoiding unnecessary movement, elevate limb and apply ice, assess for bleeding and apply pressure if needed. Cast: type of immobilization device that prevents from further injury, promotes healing and corrects deformity. Casts are more effective than splints or immobilizers because cannot be removed by the patient. They are applied once the swelling has subsided to avoid compartment syndrome. Types: Short and long arm and leg casts, Spica cast, which are usually on children with congenital hip dysplasia Interventions: Prior to casting, make sure the area is cleaned and dried. Tubular cotton web roll is placed over the affected area to maintain skin integrity. The casting material is than applied. After cast is put on make sure to position the patient so that warm, dry air circulates around and underneath the cast so it can dry faster and to prevent pressure from changing the shape of it. Elevate cast above the level of the heart during the first 24 hours-48 hours to prevent swelling. Acute Kidney Injury: (Symptoms and interventions/management) Acute renal failure: An abrupt decrease in renal function; may be the result of trauma, allergic reactions, drug overdose, kidney stones, or shock Contributing Factors: • Prerenal: disrupted blood flow to the kidneys; hypovolemic shock, dehydration, HF, burn injury, and anaphylaxis • Renal: renal tissue damage; trauma, hypokalemia, acute glomerulonephritis, hemolytic uremic syndrome (infection causes by E Coli; common in children), substance abuse • Postrenal: urine flow from the kidney is compromised; kidney stones, prostate hyperplasia, tumors, and structures Manifestations: • Onset: begins with the onset of the event and lasts for hours to days • Oliguric (1 to 3 weeks): sudden onset, less than 400 mL in 24 hours, edema, elevated BUN, creatinine and potassium, increased specific gravity; acidosis; heart failure; dysrhythmias • Diuretic: urine output increases followed by diuresis of up to 4,000 to 5,000 mL/day, indicating recovery of damaged nephrons; decreased specific gravity; hypotension and fluid and electrolyte imbalances are a concern • Recovery: may take up to 1 year until renal function returns to normal (baseline); older adults are at increased risk for residual impairment Nursing interventions: • Eliminate or prevent cause. • Correct metabolic acidosis, hyperkalemia, hyperphosphatemia, and hypocalcemia • Kayexalate (an ion exchange resin given orally or by enema to treat hyperkalemia) • IV glucose and insulin (causes potassium to enter the cell) • Calcium IV or sodium bicarbonate to stabilize cell membrane • Implement diet: • For olgiuric phase, low-protein, high-carbohydrate diet and restricted potassium intake. • For diuresis phase, low-protein, high-calorie diet and restricted fluids as indicated • Encourage bed rest in the oliguirc phase • Monitory daily weights • Monitor I&O • Implement dialysis (as ordered) until renal function returns • Assess for pericarditis (friction rub) Client teaching for Radiation Therapy: • Radiation therapy involves the use of ionizing radiation to target tissues and destroy cells. • Adverse effects include skin changes, hair loss, and debilitating fatigue. • Can be administered internally with an implant(s) (brachytherapy) or externally with a radiation beam. • The client’s body fluids are contaminated with radiation and should be disposed of appropriately, as directed by the facility. • Radiation therapy can be given preoperatively to decrease the size of a tumor. • Radiation exposure to health care personnel and visitors is reduced by limiting indirect contact time, maintaining indicated distances from sources of radiation, and preventing direct contact with the source • Internal Radiation Therapy • Brachytherapy describes internal radiation that is placed close to the target tissue. This is done via placement in a body orifice (vagina) or body cavity (abdomen) or delivered via IV such as with radionuclide iodine, which is absorbed by the thyroid. • Nursing Actions Place the client in a private room away from other clients when possible. Place appropriate sign on the door warning of the radiation source. Wear a dosimeter film badge that records personal amount of radiation exposure. Limit visitors to 30-min visits, and have visitors maintain a distance of 6 ft from the source. Visitors and health care personnel who are pregnant or under the age of 16 should not come into contact with the client or radiation source. Keep a lead container in the client’s room if the delivery method could allow spontaneous loss of radioactive material. Tongs are available for placing radioactive material into this container. Precautions listed above should be carried out at home if the client is discharged during therapy. Client Education Inform client of the need to remain in an indicated position to prevent dislodgement of the radiation im plant. Instruct the client to call the nurse for assistance with elimination. Instruct client and family about radiation precautions needed in the health care and home environments. External Radiation Therapy External radiation or teletherapy is delivered over the course of several weeks and aimed at the body from an externalsource. Nursing Actions ▪ The client’s skin over the targeted area is marked with “tattoos” that guide the positioning of the external radiation source. ▪ Provide a well-balanced diet that does not contain red meat. Radiation can cause dysgeusia, making foods such as red meat unpalatable. ▪ Help the client manage fatigue by scheduling activities with rest periods in between and using energy-saving measures (sitting during showers and ADLs). ▪ Monitor for radiation injury to skin and mucous membranes and implement a skin care regimen. ▪ Skin – blanching, erythema, desquamation, sloughing, hemorrhage ▪ Mouth – mucositis, xerostomia (dry mouth) ▪ Neck – difficulty swallowing ▪ Abdomen – gastroenteritis ▪ Monitor CBC (possible decreased platelets and WBCs). Client Education ▪ Review nutrition considerations related to mucositis (avoid spicy, salty, acidic foods; hot foods m ay notbe tolerated). ▪ Gently wash the skin over the irradiated area with mild soap and water. Dry the area thoroughly using patting motions. ▪ Do not remove or wash off radiation “tattoos” (markings) that are used to guide therapy. Do not apply powders, ointments, lotions, deodorants, or perfumes to the irradiated skin. ▪ Wear soft clothing and avoid tight or constricting clothes. ▪ Do not expose the irradiated skin to sun or a heat source. ▪ Inspect skin for evidence of damage and report to the provider. Time Management • Good Time Management o Facilitates greater productivity o Decreases work related stress o Helps ensure the provision of quality and appropriately prioritized client care • Poor time management o Impairs productivity o Leads to feelings of being overwhelmed and stressed o Increases omission of important tasks o Creates dissatisfaction with care provided • Time management involves organizing care according to client care need and priorities. o What must be don immediately (administration of analgesics or antiemetic, assessment of unstable client)? o What must be done by a specific time to ensure client safety, quality care, and compliance with facility policies and procedures (Medication administration, vial signs, blood glucose monitoring) o What must be done by the end of the shift (ambulation of the client, discharge and/or discharge teaching, dressing change)? o What can be delegated? What can be done only by an RN? What client care responsibilities can be delegated to other health care team members, such as an LVN or a CNA? How can scheduled client care activities most efficiently be shared by these two groups of care providers? • Time management involves using time saving strategies and avoiding time wasters. • Time management is a cyclic process o Time initially spent developing a plan will save time later and help avoid management crisis o Set goals and plan care based on established priorities and thoughtful utilization of resources o Complete one client care task before beginning the next, starting with the highest priority task o Reprioritize remaining tasks based on continual reassessment of client care needs o At the end of the day, perform a time analysis and determine if time was used wisely. Compartment syndrome and assessment Page 344 of new Adult Medical Surgical Nursing ATI Book • Compartment syndrome is pressure from tissue swelling or bleeding within a compartment or a restricted space causes reduced blood flow to the area. Untreated, the affected tissue will become necrotic and die. • Nursing Actions o Assess for worsening pan, swelling, and tense or taunt skin. o Report any unusual findings to the provide immediately o Prepare the client for a fasciotomy to relieve compartmental pressure Page 398 of new Adult Medical Surgical Nursing ATI Book • Compartment syndrome is considered a medical emergency. Tissue pressure within a confined body space can restrict blood flow and the resulting ischemia can lead to irreversible tissue damage. • Nursing Action o Manifestations of compartment syndrome include tingling, numbness, worsening pain, edema, pain on passive movement, and unequal pulses. Immediately report findings to the provider. o Loosen dressing o Prepare to assist with fasciotomy (surgical opening into the tissue); which may be necessary to prevent further injury to save the limb Page 795 of new MedSurg ATI book • Compartment syndrome (ACS) is assessed by using the five P’s (pain, paralysis, paresthesia, pallor, and pulselessness). o Increased pain unrelieved with elevation or by pain medication. o Intense pain when passively moved. o Paresthesia or numbness, burning, and tingling are early signs. o Paralysis, motor weakness, or inability to move the extremity indicate major nerve damage and are late signs. o Color of tissue is pale (pallor), and nail beds are cyanotic. o Pulselessness is a late sign of compartment syndrome. o Palpated muscles are hard and swollen from edema. • Client education o Instruct the client to report pain not relieved by analgesics or pain that continues to increase in intensity. o The client should also be instructed to report numbness, tingling, or a change in color of the extremity. Ileostomy Care Begin teaching in preoperative and continue after surgery Stoma & peristomal skin care -healthy stoma appears pink or read and moist and should protrude about ¾ inches (2cm) from abdominal wall - report if stoma turns dusky, brown. Black or white to provider immediately as these findings indicate compromised circulation -cleansing agent=> mild, pH- balanced soap or no soap @ all just water *DO NOT use alcohol, povidone-idoine (Betadine) or oil-based soap can intervene with adhesion of the skin barrier and could promote skin breakdown -need to measure the stoma w/ each pouch change over the first 8 weeks following surgery to verify that the opening of the pouch is the current size. Notify clinician for: -increased pain in the abdomen or incision; fever, redness, or drainage of the incision; or irritation, redness or breakdown of the peristomal skin -change in bowel habits, such as diarrhea or constipation -skin irritation unrelieved by properly fitted pouch system -Problems obtaining a good seal Follow up care Have follow up appointment 2 weeks after discharge , then 6 weeks, 3 months, 6 months and 1 year after surgery. Patients want to resume normal activity Exercise: -advise against contact sports (soccer, basketball, football) due to possible injury to the stoma from severe blow *INSTEAD: engage in a regular exercise routine that includes activities that promote cardiovascular & musculoskeletal fitness Travel: -acquire adequate supplies, using pre-cut barriers & to minimize the amount of equipment they need and packing supplies -bring statement from provider incase questions arise Sexuality: -Important for patient to expect to feel sensitive about change in body image. -Encourage them to share feelings with their partners and to respond to any concerns -sexual activity will not hurt stoma -Empty pouch first, wear smaller pouch, cover pouch w/ specially designed underwear, lingerie or pouch covers Initial drainage=typically dark green viscid, odorless Gradually thickens and becomes yellow to brown Empty pouch when 1/3 to ½ full bag= may require drainage several times a day Effluent contains enzymes & bile salts can irritate the skin Advise to use skin barriers and prompt attention to any sign of leakage. Teach patient to recognize s/s of food blockage and to contact provider if manifestations: Abdominal cramping, nausea, vomiting, high volume odorous effluent, swelling stoma, no ileostomy output for at least 6 hours Intervention from food blockage: Place moist towels on abdomen, drink hot tea, lie down and assume a knee-chest position to relieve intra abdominal pressure, and/or massage the abdominal are to promote peristalsis and fecal elimination High Volume output at risk of dehydration, electrolyte, imbalance extreme thirst Common manifestations: -extreme thirst -dry skin and oral muscous membranes -decrease urine output -weakness, fatigue -headaches, dizziness -muscle cramps -abdominal cramps, nausea -SOB -orthostatic hypotension Dehydration/hypotension increases with hot weather b/c of perspiration -drink enough fluids to maintain a urine output of at least one quart per day -when active in hot weather consume extra fluid, sodium and high potassium foods such as bananas and oranges To avoid food blockage should avoid high fiber foods difficult to digest foods=> popcorn, nuts, corn, cucumbers, celery, fresh tomatoes, figs, strawberries, black berries, caraway seeds. Hepatic Encephalopathy Clients who have a poorly functioning liver are unable to convert ammonia and other waste products to a less toxic form. These products are carried to the brain and cause neurological symptoms. Clients are treated with medications such as lactulose to reduce the ammonia levels in the body via intestinal excretion. Reductions in dietary protein are indicated as ammonia is formed when protein is broken down by intestinal flora. Nutrition encephalopathy Maintain a high-calorie, low-protein (20 to 40 g/day), low-fat, low sodium diet (maintain protein restriction during stage I and stage II of encephalopathy; no protein allowed during stage III and IV). Limit sodium and fluid intake as prescribed. Schizophrenia Expected Findings Positive symptoms – The manifestation of things that are not normally present. These are the most easily identified symptoms. -Hallucinations -Delusions -Alterations in speech -Bizarre behavior, such as walking backward constantly Negative symptoms – The absence of things that are normally present. These symptoms are more difficult to treat successfully than positive symptoms. -Affect – usually blunted (narrow range of normal expression) or flat (facial expression never changes) -Alogia – poverty of thought or speech; the client may sit with a visitor but may only mumble or respond vaguely to questions. -Anergia – lack of energy -Anhedonia – lack of pleasure or joy; the client is indifferent to things that often make others happy, such as looking at beautiful scenery. -Avolition – lack of motivation in activities and hygiene; for example, the client completes an assigned task, such as making his bed, but is unable to start the next common chore without prompting. Cognitive symptoms – Problems with thinking make it very difficult for the client to live independently. -Disordered thinking -Inability to make decisions -Poor problem-solving ability -Difficulty concentrating to perform tasks -Memory deficits Intermittent Tube Feedings Intermittent tube feeding – Formula is administered every 4 to 6 hr in equal portions of 200 to 300 mL over a 30- to 60-min time frame, usually by gravity drip. -Often used for noncritical clients, home tube feedings, and clients in rehabilitation. Assessing and interventions for a patient with PTSD. ● Manifestations include: increased arousal, irritability, difficulty with concentration, and sleep disturbance. May show avoidance of stimuli associated with trauma, such as avoiding people or inability to show feelings. ● The client persistently re-experiences the event through: recurrent, intrusive recollection of the event, dreams or images, reliving through flashbacks, illusions, or hallucinations. ● Assess for any comorbidities such as substance or alcohol abuse. Perform suicide risk assessment. ● Interventions: - Provide safe and comfortable environment. - Stay with client during times of distress. - Eye movement desensitization and reprocessing (EMDR) is a therapy for clients who have PTSD. EMDR encourages eye focus on a separate stimuli while thinking of or talking about the traumatic event. Modified diets ● Clear Liquid Diet: consists of foods that are clear and liquid at room temperature. - Primarily consists of water and carbohydrates. This diet requires minimal digestion, leaves minimal residue, and is non-gas forming. It is nutritionally inadequate and should not be used long term. - Indications include acute illness, reduction of colon fecal material prior to certain diagnostic tests and procedures, acute gastrointestinal disorders, and some postoperative recovery. - Acceptable foods are water, tea, coffee, fat-free broth, carbonated beverages, clear juices, ginger ale, and gelatin. - Limit caffeine consumption, which can lead to increased hydrochloric acid and upset stomach. ● Full Liquid Diet: consists of foods that are liquid at room temperature. - Offer more variety and nutritional support than a clear liquid diet and can supply adequate amounts of energy and nutrients. - Acceptable foods include all liquids on a clear liquid diet, all forms of milk, soups, pureed vegetables and fruits, vegetable and fruit juices, eggnog, plain ice cream and sherbet, refined or strained cereals, and puddings. - Evaluate the need for high-protein and high-calorie supplements if this diet is used more than 2 to 3 days. - Indications include a transition from liquid to soft diets, postoperative recovery, acute gastritis, febrile conditions, and intolerance of solid foods. - Provides oral nourishment for clients having difficulty chewing or swallowing solid foods. Use cautiously with clients who have dysphagia (difficulty swallowing) unless liquids are thickened appropriately. - Contraindicated for clients who have lactose intolerance or hypercholesterolemia. Use lactose-reduced milk and dairy products when possible. ● Blenderized Liquid (Pureed) Diet - Consists of liquids and foods that are pureed to liquid form. - The composition and consistency of a pureed diet varies, depending on the client’s needs. - Modify with regard to calories, protein, fat, or other nutrients based on the dietary needs of the client. - Adding broth, milk, gravy, cream, soup, tomato sauce, or fruit juice to foods in place of water provides additional calories and nutritional value. - Each food is pureed separately to preserve individual flavor. - Indications include clients who have chewing or swallowing difficulties, oral or facial surgery, and wired jaws. ● Soft (Bland, Low-Fiber) Diet: contains whole foods that are low in fiber, lightly seasoned, and easily digested. - Food supplements or snacks in between meals add calories. - Food selections vary and can include smooth, creamy, or crisp textures. Fruits, vegetables, coarse breads and cereals, beans, and other potentially gas-forming foods are excluded. - Indications include clients transitioning between full liquid and regular diets, or those who have acute infections, chewing difficulties, or gastrointestinal disorders. ● Mechanical Soft Diet: A regular diet that is modified in texture. The diet composition is altered for specific nutrient needs. - Includes foods that require minimal chewing before swallowing (ground meats, canned fruits, softly cooked vegetables). - Excludes harder foods (dried fruits, most raw fruits and vegetables, foods containing seeds and nuts). - Indications include limited chewing ability; dysphagia, poorly fitting dentures, and clients who are edentulous (without teeth); surgery to the head, neck, or mouth; and strictures of the intestinal tract. Clinical manifestations and interventions of hyperthyroidism Manifestations: - Anxiety and irritability - Insomnia and fatigue - Tachycardia - Tremors - Diaphoresis - Intolerance of heat - Weight loss (despite food intake) - Exophthalmos - Diarrhea - Light or absent menstrual cycle Diagnostic Procedures/Findings: - Elevated T4 and T3 - Decreased TSH Nursing interventions: - Assess vital signs - Promote comfort - Encourage the client to get adequate rest in a cool, quiet environment - Provide a high-caloric diet without extra stimulants - Weigh the client daily - Provide the client emotional support - Provide eye protection for the client who has exophthalmos by giving ophthalmic medicine, taping the client’s eyes at night, and decreasing sodium and water - Elevate head of bed Medications: - Beta-blocker medications to manage tachycardia, anxiety and tremors - Propylthiouracil (Propyl-Thyracil or PTU) - Methimazole (Tapazole) - Iodides (Lugol’s solution/saturated solution of potassium iodide (SSKI)) - Radioactive iodine treatment shrinks the thyroid gland Therapeutic Measures: - Thyroidectomy Evaluating proper functioning of NG tube - The auscultatory method of checking placement is NOT considered reliable. Initial placement of the nasogastric or nasointestinal tube should be checked by x-ray. Subsequent placement should be checked by aspirating stomach or intestinal contents and measuring pH. Gastric pH should be between 1.5 and 4; intestinal aspirate pH is around 6; respiratory aspirate pH is 7 or higher. [Show More]
Last updated: 1 year ago
Preview 1 out of 43 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
43
Written in
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
54