*NURSING > Class Notes > Chamberlain College of Nursing: NR 446REVIEW NOTES PART 2: Nonpharmacological Pain Management,GRADED (All)
Chamberlain College of Nursing: NR 446REVIEW NOTES PART 2: Nonpharmacological Pain Management,GRADED A
Document Content and Description Below
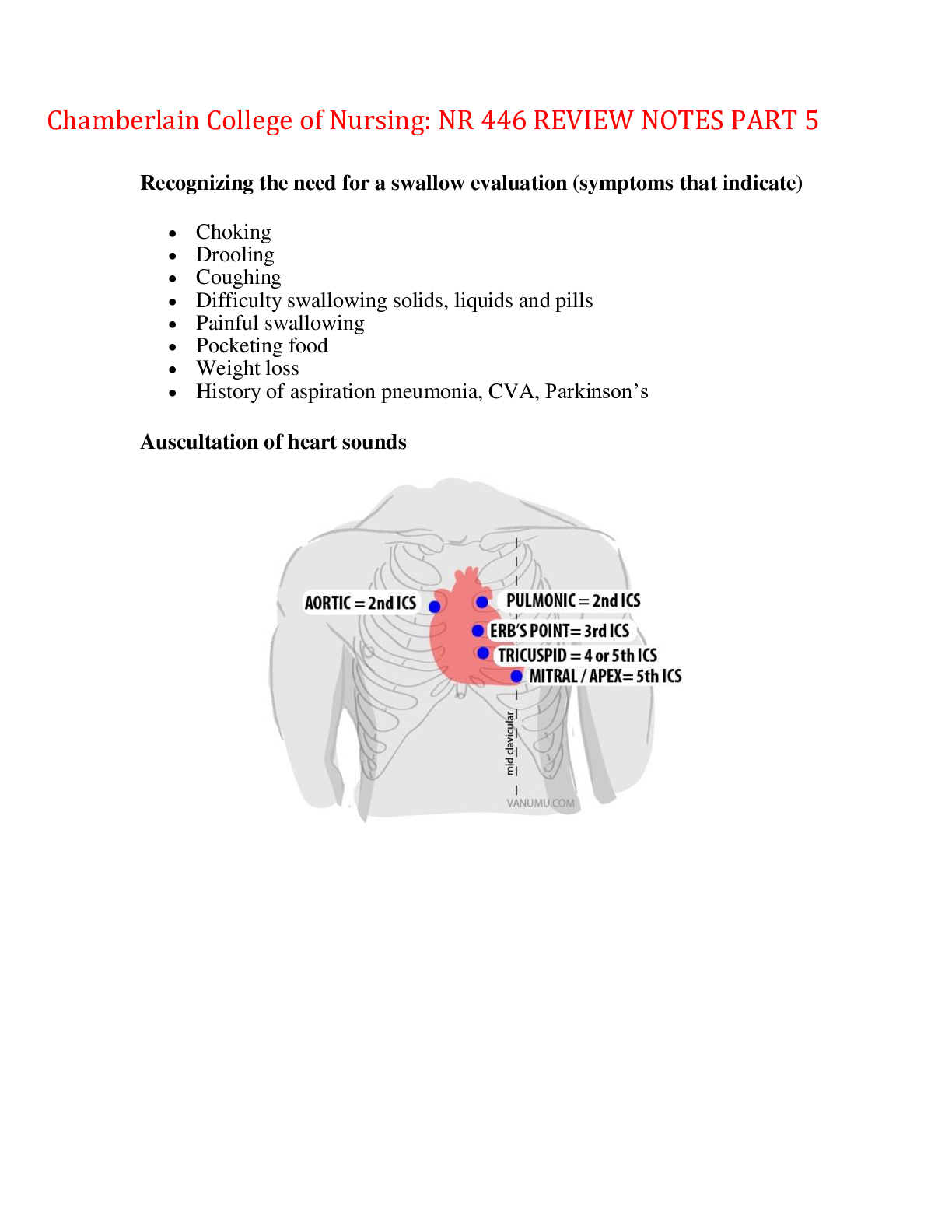
Chamberlain College of Nursing: NR 446REVIEW NOTES PART 2: Nonpharmacological Pain Management 1. Transcutaneous electrical nerve stimulation (TENS), heat, cold. Therapeutic touch and massage. 2. I... nterruption of pain pathway a. Cold for inflammation, b. Heat to increase blood flow and to reduce stiffness. 3. Distraction: includes ambulation, deep breathing, visitors, television and music 4. Relaxation: includes meditation, yoga, and progressive muscle relaxation 5. Imagery: focusing on a pleasant thought to divert focus, requires ability to concentrate 6. Acupuncture: vibration or electrical stimulation via tiny needles inserted into the skin and subcutaneous tissues at the specific points a. Reduction of pain stimuli in the environment b. Elevation of edematous extremities to promote venous return and decrease swelling. Benefits of applying ICE to extremity: 1. Decreases inflammation 2. Prevents swelling 3. Reduces bleeding 4. Reduces fever 5. Diminishes muscle spasms 6. Decreases pain by decreasing the velocity of nerve conduction. Cold application is not approved for clients with cold intolerance, vascular insufficiency and disorders aggravated by cold such as Reynaud’s phenomenon. Make sure to assess the site every 5 to 10 minutes check for: redness pallor pain burning numbness shivering blisters, cyanosis. **Remove application every 15 to 20 minutes PROPER AGENTS TO CLEAN UP BLOOD CONTAMINATION. It is important to prevent exposure hazardous blood spill to other people in the environment or hospital setting. There are two important things to remember when cleaning blood spilled on the floor. 1) You should always assumed that the blood is infection with a dangerous disease. Blood can be infected with diseases like Hepatitis B, Hepatitis C and HIV. 2) The second important thing to know is to always be prepared by having the right clean up equipment and use it properly. Blood can be cleaned safely by following OSHA’s Blood born pathogen clean up kit that requires many equipments. It is important to always protect yourself first. The materials needed to protect your self are: 1) Protective cap 2) Eye protection 3) Protective gown 4) Mask 5) Disposable gloves The materials needed to clean the blood spills are: 1) Absorbent materials 2) Disinfecting towelettes 3) Biohazard bag with zip tie 4) Scoop 5) BLEACH SOLUTION There are steps to cleaning blood spilled on the floor. 1) It is important to prevent any other persons to access the area until the cleanup is completed. 2) Put on disposable gloves, protect yourself 3) Use paper towel or other absorbent materials to wipe the spill from the floor. 4) Use bleach solution, 1 part bleach to 9 parts water to all areas of the floor that contained blood. 5) Let the bleach solution remain on the area for 20 minutes then wipe the bleach solution 6) All non-disposable cleaning materials need to be disinfected by saturating with bleach solution and allowed to air dry. 7) Remove your gloves and place in tie up garbage bags with all other soiled cleaning materials 8) Double bag and discard 9) Then thoroughly wash hands with soap and water. SCHEDULING FOR PEAK AND TROUGH LEVELS PEAK LEVEL: Reflect the highest concentration Average times for drawing peak levels Route of administration Time specimen is drawn after administration Oral Intake 1 to 2 hr Intramuscular 1 hr Intravenous 30 min TROUGH LEVELS: Reflect the lowest concentration or residual level and are usually OBTAINED WITHIN 15 MIN PRIOR TO ADMINISTRATION OF THE NEXT SCHEDULED DOSE. The scheduled dose of medication should not be administered until the trough level is confirmed (The timing of for drawing a peak and trough level varies based on the half-life (time required for the body to decrease the medication blood level by 50% for the medication) Additional information : DRUG DRAW TIMES Aminoglycosides: Gentamicin & Tobramycin IV Trough: collect just prior to next dose IV PEAK: Infuse over 30 minutes, wait 30 minutes after infusion is complete to collect IM Therapy: Draw trough just prior to next dose and at one hour after injection Carbamazepine Collect just prior to next dose Digoxin One determination is needed within 6- 24 hours after the previous dose Phenytoin Collect just prior to next dose Phenobarbitol Collect just prior to next dose Quinidine Collect just prior to next dose Theophylline IV Infusion: Wait 30 minutes after loading dose and resample at 4-8 hour intervals IV Bolus: Draw 30 minutes after infusion has completed Vancomycin Trough: Collect just prior to next dose Peak: Draw 1/12 hours after IV infusion has completed LIST OF REPORTABLE INFECTIONS • Anthrax • Arboviral diseases (diseases caused by viruses spread by mosquitoes, sandflies, ticks, etc.) o California serogroup virus disease o Eastern equine encephalitis o Powassan virus disease o St. Louis encephalitis o West Nile virus o Western equine encephalitis • Botulism • Brucellosis • Chancroid • Chickenpox • Chlamydia trachomatis • Cholera • Coccidioidomycosis • Cryptosporidiosis • Cyclosporiasis • Diphtheria • Giardiasis • Gonorrhea • Haemophilus influenza, invasive disease • Hansen disease (leprosy) • Hantavirus pulmonary syndrome • Hemolytic uremic syndrome, post-diarrheal • Hepatitis A • Hepatitis B • Hepatitis C • Influenza-related infant deaths • Legionellosis • Listeriosis • Lyme disease • Malaria • Measles • Meningococcal disease • Mumps • Novel influenza A virus infections • Pertussis • Plague • Poliomyelitis • Poliovirus infection, nonparalytic • Psittacosis • Q-fever • Rabies (human and animal cases) • Rocky Mountain spotted fever • Rubella (including congenital syndrome) • Salmonellosis • Severe acute respiratory syndrome (SARS) • Shiga toxin-producing Escherichia coli (STEC) • Shigellosis • Smallpox • Syphilis, including congenital syphilis • Tetanus • Toxic shock syndrome (other than streptococcal) • Trichinosis • Tuberculosis • Tularemia • Typhoid fever • Vancomycin intermediate Staphylococcus aureus (VRSA) • Vancomycin resistant Staphylococcus aureus (VRSA) • Vibriosis • Yellow fever LEUKOTRINEMODIFIERS: Action: Prevent effects of leukotrine resulting in decreased inflammation, bronchoconstriction, airway edema, and mucus production. Medications include: Montelukast (Singulair), Zileuton (Zyflo), Zafirlukast (Accolate) Therapeutic uses: ---Long---termmanagement of asthma inadultsand children olderthan 15 years. ---Prevention of exercise---induced bronchospasm Precautions/Interactions: ---Do not use for acuteasthma attack ---Zileuton or Zafirlukast: high risk of liver disease, increased warfarin effects, and theophylline toxicity ---Phenobarbitalwill decreasecirculatinglevels of montelukast. ---Chewable tablets contain phenylalanine. Side/adverse effects ---Elevated liver enzymes (zileuton or zafirlukast) ---Warfarin andtheophylline toxicity(zileuton or zafirlukast) Nursing Interventions and Client Education ---Never abruptly substitute for corticosteroid therapy ---Teach client to take daily ---Do not decrease or stop taking other prescribed asthma drugs until instructed ---If using oral granules, pour directly into mouth or mix with cold soft foods (never liquids). ---Use open packets within 15 minutes Signs and symptoms to differentiate right and left sided heart failure ◯ Risk Factors: Left-sided heart (ventricular) failure ▪ Hypertension ▪ Coronary artery disease, angina, MI ▪ Valvular disease (mitral and aortic) ◯ Risk Factors: Right-sided heart (ventricular) failure ▪ Left-sided heart (ventricular) failure ▪ Right ventricular MI ▪ Pulmonary problems (COPD, pulmonary fibrosis) ◯ Systolic blood pressure is elevated in older adults, putting them at risk for coronary artery disease and heart failure. ◯ Certain medications may increase the risk of heart failure or worsen manifestations in the older adult client. ● Subjective and Objective Data ◯ Left-sided failure ▪ Dyspnea, orthopnea (shortness of breath while lying down), nocturnal dyspnea ▪ Fatigue ▪ Displaced apical pulse (hypertrophy) ▪ S3 heart sound (gallop) ▪ Pulmonary congestion (dyspnea, cough, bibasilar crackles) ▪ Frothy sputum (can be blood-tinged) ▪ Altered mental status ▪ Manifestations of organ failure, such as oliguria (decrease in urine output) ◯ Right-sided failure ▪ Jugular vein distention ▪ Ascending dependent edema (legs, ankles, sacrum) ▪ Abdominal distention, ascites ▪ Fatigue, weakness ▪ Nausea and anorexia ▪ Polyuria at rest (nocturnal) ▪ Liver enlargement (hepatomegaly) and tenderness ▪ Weight gain LVN Delegation Monitoring client findings (as input to the RN’s ongoing assessment of the client) › Reinforcement of client teaching from a standard care plan › Tracheostomy care › Suctioning › Checking nasogastric tube patency › Administration of enteral feedings › Insertion of a urinary catheter › Medication administration (excluding intravenous medications in several states) Auscultate/Listen Check(s) Reinforce/remind Administer (PO,SubQ,IM -- NO high alert meds, plasma, blood products-- these and IV are done by RN) Observe Collect (data, specimens) Monitor Set up (basic equipment) Review/Teach-- Usually standard practices (hand washing/hygiene) or med administration (ie. eye drops) – RN mostly teaches/educated and LPNs Reinforce Routine/Standard Wound care/Suction/Urinary Cath/Blood glucose readings ** Don't assign LVN/LPN to do a task an nurse assistant can complete** Delegation of task in a Peds Unit Delegation Factors: Nurses can only delegate tasks appropriate for the skill and education level of the health care provider who is receiving the assignment. Considerations for selection of an appropriate delegatee include: • Education, training, and experience • Knowledge and skill to perform the task • Level of critical thinking required to complete the task • Ability to communicate with others as it pertains to the task • Demonstrated competence • Agency policies and procedures • Licensing legislation (state nurse practice acts) Signs and symptoms of dehydration in elderly and children. Dehydration is a body fluid disturbance when the output exceeds intake. It results from many causes such as fluid losses through the skin, respiratory tract, urinary tract, or GI tract. It is the most common fluid and electrolyte imbalance in older adults, and they are more prone to dehydration due to decreased fluid and protein intake, decrease in total body mass, and use of medications such as diuretics. Subjective Data and Objective Data in Elderly Vital signs – Hyperthermia, tachycardia, thready pulse, hypotension, orthostatic hypotension, decreased central venous pressure, tachypneic (increased respirations), hypoxia Tachycardia occurs in an attempt to maintain a normal blood pressure. Neuromusculoskeletal – Dizziness, syncope, confusion, weakness, fatigue Gastrointestinal – Thirst, dry furrowed tongue, nausea/vomiting, anorexia, acute weight loss Renal – Oliguria (decreased production and concentration of urine) Other signs – Diminished capillary refill, cool clammy skin, diaphoresis, sunken eyeballs, flattened neck veins, poor skin turgor, and tenting. Clinical findings of dehydration in children: listlessness, sunken eyes, sunken fontanels, decreased tears, dry mucous membranes, and decreased urine output. FERROUS SULFATE: Ferrous sulfate is an Oral Iron preparation. parenteral iron preparation is Iron Dextran (INFeD) Pharmacological action: Needed for RBC development & oxygen transport. Remember!: during times of inceased growth (growing kids, menarche, pregnancy) the need for ir increases Remember!: Iron is poorly absorbed by the body so large amounts are needed to increase Hgb & Hct Therapeutic uses: Iron- deficiency anemia Side effects: GI: Nausea, constipation, heartburn advise that these effects usually resolve with continued use if they cannot tolerate the S/E take w/food (this reduces the absorption) Teeth staining (liquid form) dilute liquid iron w/water or juice drink w/ straw rinse mouth after swallowing staining of the skin w/IM INJECTIONS Z track technique anaphalaxis monitor patient, have life support equipment Hypotension Monitor VS when giving parenteral Iron toxicity children 2-10g Antidote: Deferoxamine (Desferal) it is an chelating agent used to treat iron toxicity CONTRAINDICATIONS: Hemolytic Anemia [destruction of RBC happens faster thatn what the bone marrow can make] PUD, Liver disease INTERACTIONS/AVOID: antiacids, coffee, tea, dairy producst, TCA'S, whole grain breads [TELL THE PATIENT TO WATI 1 TO 2 HRS] NURSING ADMINISTRATION: instruct to take on emptystomach, 1 hr before meals [stomach acid increases absorption] *Tell the pt if taken w/food the absorption will be decreased [it does increased adherance but decreases absorption] * Tell pt that green/dark stools are expected & harmless * Tell pt to dilute liquid it with water, OJ, drink w/straw, and rinse after taking it *Citrus juices are best to increase absroption * Tell pt to increase fiber and water intake [why? because constipation is a SE] tell them to exercise too. *Tell the pt theray may ned to last 1 to 2 months * Encourage foods high in iron: organ meats, egg yolks, fish, enriched breads & macaroni, green leafy vegetables, whole grain products, dried fruits * DONT MASSAGE INJECTION SITE!!!! HOW DO YOU KNOW ITS WORKING? *increased reticulocyte count [immature RBC]: should happen around 1 week after starting therapy *Increased Hgb of 2g/dL expected 1 month after therapy has started *decrease in fatigue, pallor *increased energy NORMAL LABS (CBC): RBC: [Male 4.7 to 6.1 million/uL] [Female 4.2 to 5.4 million/uL] Hgb: [Male 14 to 18 g/dL] [Female 12 to 16 g/dL] Hct : [Male 42 to 52%] [Female 37 to 47%] Platelets: 150,00 to 400,000 calculating due date Nageles rule: formula to calculate estimated date of confinement [EDC] or estimated date of birth [EDB] keep i mind that this formula presumes the mentrual cycle of the woman is regular and 28 days duration [First day of last menstrual period] - 3 months + 7days + 1 year December 21 (2014) - 3 months = Setember 21 september 21 + 7 days = September 28 2014 September 28 2014 + 1 year = SEPTEMBER 28 2015 Extra OB info: * ovum life time: 24 hr * sperm life time: 72hr * menstruation starts 14 days after ovulation * Fertilization: 7-10days [outer 1/3 of fallopian tube] * zygote: fertilized egg *hCG: detected by 6th day *hight hCG: Trisonomy 21, multifetal,ectopic, hydatidiform mole * Low hCG: misscarriage * Progesterone levels increase [to close the cervix] when delivery is occuring progesterone levels decrease & the cervix dilates. *Umbilical cord : AVA [1vein&2artries], no pain receptors * wharton jelly: around UC relievs pressure [protects] *amniotic fluid: 800-1200 normal, replaced every 3hrs *oligo[not enough AF] amnioinfusion [NS/LR] risk of cord compression *poly[to much AF] reverse trandelenburg risk of cod prolapse *Sex cells: Miosis [1/2 #DNA is haploid] *Body cells: Mitosis [Phases: Prophase, Metaphase, Anaphase, telenophase (PMAT) *OTC remedies for striae wont work *presumptive signs [woman feels]: amenorrhea, fatigue, N/V, quickening [16-20weeks], montgomerry tubules*Probable signs [HCP feels]: Hegars[softening of lower uterus], chadwicks[blu/violetmucosa], goodwells [softening of cervical tip], positive pregnacy test* Potive signs: [due o fetus]: Fetal heart tones, ultrasound of fetus, fetal movement *VEAL: CHOP * Rhogam: 28weeks & 72 hrs post delivery [Mom Rh- & Dad Rh+ then wont affect first baby but will affect 2nd baby so will need Cesarian. Rhogam administration is a blood product so you need another RN to verify before you give it. Key Elements of Incident Reports Incident reports are records made of unexpected or unusual incidents that affected a client, employee, volunteer, or visitor in a health care facility. Examples of circumstances under which an incident report should be filed include the following: Medication errors Procedure/treatment errors Equipment-related injuries/errors Needlestick injuries Client falls/injuries Visitor/volunteer injuries Threat made to client or staff Loss of property (dentures, jewelry, personal wheelchair) In the event of an incident that involves a client, employee, volunteer, or visitor, the nurse’s priority is to assess the individual for injuries and institute any immediate care measures necessary to decrease further injury. If it was a client-related incident, the provider should then be notified, and additional tests or treatment should be carried out as prescribed. Incident Reports Should be completed by the person who identifies that an unexpected event has occurred. (This may or may not be the individual most directly involved in the incident.) Should be completed as soon as possible and within 24 hr of the incident. Are considered confidential and are not shared with the client. (Nor is it acknowledged to the client that one was completed.) Are not placed in the client’s health care record nor mentioned in the client’s health care record. However, a description of the incident itself should be documented factually in the client’s record. Include an objective description of the incident and actions taken to safeguard the client, as well as assessment and treatment of any injuries sustained. Are forwarded to the risk management department or officer (varies from facility to facility), possibly after being reviewed by the nurse manager. Provide data that may be used in performance improvement studies regarding the incidence of client injuries and care-related errors. When completing an incident report, the nurse should include the following: The client’s name and hospital number (or visitor’s name and address if visitor injury), along with the date, time, and location of the incident A factual description of the incident and injuries incurred, avoiding any assumptions as to the cause of the incident Names of any witnesses to the incident and any client or witness comments regarding the incident Corrective actions that were taken, including notification of the provider and any referrals The name and dose of any medication or identification number of any piece of equipment that was involved in the incident Lab Findings for MI Cardiac enzymes are specific markers in diagnosing a myocardial infarction (MI). CBC Rule out anemia caused by decreased oxygen supply and before giving thrombolytic. White blood cells may me elevated due to inflammatory process Platelet count may be low from heparin use causing heparin-induced thrombocytopenia BMP Monitor potassium and magnesium levels Creatinine levels considered before giving ACE inhibitors ESR rises within 3 days and may remain elevated Lactate Dehydrogenase rises above reference range within 24 hours of MI C-Reactive Protein Measures inflammation levels upon presentation of acute coronary syndrome Advanced Directives: Advance Directives is a document is which a patient who is competent is able to express whishes regarding future acceptable health care and/or designate another person to make decisions when the client becomes physically or mentally unable to do so. 2 types of advance directives: living will and durable power. Living will: is a legal document that expresses the patients wishes regarding medical treatment in the event the patient becomes incapacitated and is facing end of life issues. Durable power of attorney for health care: is a legal document that designates a health care proxy who is an individual authorized to make sure decisions for a patient who is unable too. Nursing interventions: Its important for the RN to identify patients who do not have advance directives, inform them of their rights and ensure that clients who have advance directives have copies places in their medical records. Monitoring lab values in cardiovascular disease Lab tests: Serum electrolytes Erythrocyte sedimentation rate (ESR) C-reaction protein, Blood coagulation tests- PTT, which would be most significant if the patient was on heparin, PT- which would be most significant is the patient is on warafin , INR BUN and creatinine- which reflect renal function and perfusion; levels may increase in MI, CHF and cardiomyopathy total serum cholesterol – LDL, HDL and triglycerides BNP, which is an indicator for diagnosing heart failure Less than 100 no risk 100-300 possible Greater than 300 mild Greater than 600 moderate Greater than 900 severe Enzymes- which is a test that indicates death of myocardial muscles; heart attack Creatinine phosphokinase MB- increases 4-6 hours after an MI and stayed elevated for 24-72 hours Troponin- is considered the “gold standard” in diagnosing an MI. This remains elevated for 2-3 weeks after. Normal levels is less than 0.2ng/dL Nursing Interventions for Sprains: • Refrain from weight-bearing. • Apply ice to decrease inflammation. • Apply a compression dressing to minimize swelling. • Elevate the affected limb. • The acronym RICE – Rest, Ice, Compression, Elevation is helpful for remembering treatment intervention. • After the acute inflammatory stage (24 to 48 hours after injury), heat may be applied intermittently (for 15 to 30 minutes four times a day) to relieve spasm and to promote vasodilation, absorption and repair. Signs and Symtpoms of Electrolyte Imbalances Signs & Symptoms Hypo Hyper Potassium (3.5-5.0) • Disorientation/Confusion • Tiredness • Abdomen Distention • Paralytic Ileus • Nausea/Vomitting • Constipation • Polyuria • Tachypnea • Tachycardia • Dysrythmias • Dysrythmias • EKG changes • Diarrhea • Abdominal Cramping • Irritability Muscle Weakness Urine,oliguria, anuria Respiratory Distress Decreased cardiac contratility EKG changes Reflexes, hyperflexia or flaccid Sodium (136-145) • Headache • Tiredness • Dry mucous membranes • Nausea/Vomitting • Abdominal Cramping • Dry pale Skin • Disoriented • Muscle Cramps and Muscle Weakness • Tachycardia • Seizures • Thirst • Dried Flushed Skin • Sticky Tounge or mucous membranes • Fever • Nausea/Vomitting • Anorexia • Polyuria • Tachycardia • Restlessness, Irritation, Confusion, Seizures F ever, flushed skin R estless I ncreased fluid retention and BP E dema D ecreased urine output Calcium (9.0- 10.5) • Respiratory Distress • Cardiac Dysrythmias • Tetany • Tingling or numbeness • Seizures • Irritability • Osteomalacia • Osteoporosis • Rickets • Anorexia • Nausea/Vomitting • Increase Thirst • Dry Mucous Membranes • constipation • Abdominal Pain • Kidney Stones • Polyuria C onvulsions A rrythmias T etany S pasms and stridor • Impaired Memory • Mood Swings INDICATION OF CARDIOVERSION Synchronized cardioversion is a LOW ENERGY SHOCK that uses a sensor to deliver electricity that is synchronized with the peak of the QRS complex (the highest point of the R- wave). When the “sync” option is engaged on a defibrillator and the shock button pushed, there will be a delay in the shock. During this delay, the machine reads and synchronizes with the patients ECG rhythm. This occurs so that the shock can be delivered with or just after the peak of the R-wave in the patients QRS complex. Synchronization avoids the delivery of a LOW ENERGY shock during cardiac repolarization (t- wave). If the shock occurs on the t-wave (during repolarization), there is a high likelihood that the shock can precipitate VF (Ventricular Fibrillation) The most common indication for synchronized cardioversion are unstable atrial fibrillation, atrial flutter, atrial tachycardia, and supraventicular tachycardia. If the medication fail in the stable patient with arrhythmias, synchronized cardioversion will most likely be indicated. Unsynchronized cardioversion (defibrillation) is a HIGH ENERGY shock which is delivered as soon as the shock button is pushed on a defibrillator. This means that the shock may fall randomly anywhere within the cardiac cycle (QRS complex). Unsynchronized cardioversion (defibrillation) is used when there is no coordinated intrinsic electrical activity in the heart (pulseless VT/VF) or the defibrillator fails to synchronize in an unstable patient For the cases where electrical shock is needed, if patient is stable and QRS is visible, low energy, synchronized cardioversion. If the patient is pulseless, or if the patient is unstable and the defibrillator will not synchronized use high energy unsynchronized cardioversion or defibrillator. DELAGATING TASK FOR FLOAT NURSE Your patients lives are at stake, so never do something outside your scope of practice, such as perform as procedure you have not be validated to do. If you are assigned a patient you do not feel qualified to take care of, it is your responsibility to notify the charge nurse or supervisor. You are accountable for every action you perform as a float nurse and doing something you are not authorized to do put your patients and your career at risk! Osteoporosis Prevention: Exercise -Weight-bearing -walking -Dancing -Aerobics Diet: -Calcium -low fat dairy products * Nuts and pulses: almonds, Brazil nuts, hazelnuts, sesame seeds. * Green leafy vegetables: broccoli, spinach, watercress, curly kale. * Dried fruits: apricots, dates, figs. * Fish: mackerel, pilchards, salmon, sardines. * Tofu and various calcium-fortified foods. Supplements: -Calcium -VItamin D Hormone Replacement therapy: Hormone replacement therapy replaces oestrogen and so reduces the rate of bone loss. Interventions in Osteoporosis Injury: -Physical Therapy -Pain Management Long term adverse effects of haldol Tardive dyskinesia (TD) is a side effect that develops with prolonged use of antipsychotics. If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your healthcare provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their healthcare provider to monitor for TD. Symptoms of EPS include restlessness, tremor, and stiffness. TD symptoms include slow or jerky movements that one cannot control, often starting in the mouth with tongue rolling or chewing movements. Principles of Prioritization • Priority setting requires that decisions be made regarding the order in which: o Clients are seen. o Assessments are completed. o Interventions are provided. o Steps in a client procedure are completed. o Components of client care are completed. • Establishing priorities in nursing practice requires that these decisions be made based on evidence obtained: o During shift reports and other communications with members of the health care team. o Through careful review of documents. o By continuously and accurately collecting client data. • • Boggy Uterus • Determine whether the fundus is firm or boggy. o If the fundus is boggy (not firm), lightly massage the fundus in a circular motion. o o o Put baby on the breast of the mother if the mother is nursing. o Medications to contract the uterus. Pitocin o Lochia Checks • [Show More]
Last updated: 1 year ago
Preview 1 out of 31 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
44