*NURSING > Class Notes > Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 3Nursing Intervention for Client with Demen (All)
Chamberlain College of Nursing: NR 446 REVIEW NOTES PART 3Nursing Intervention for Client with Dementia,GRADED A
Document Content and Description Below
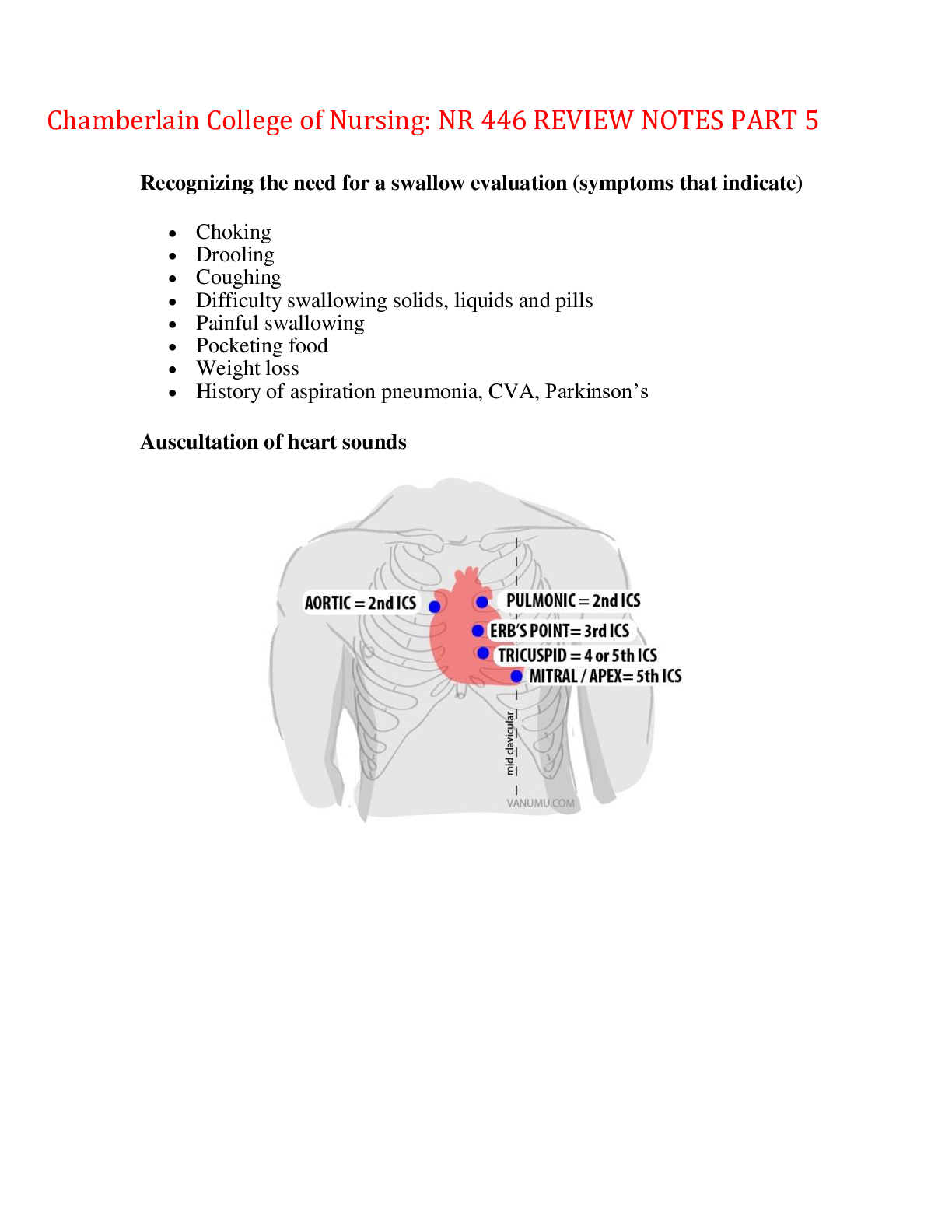
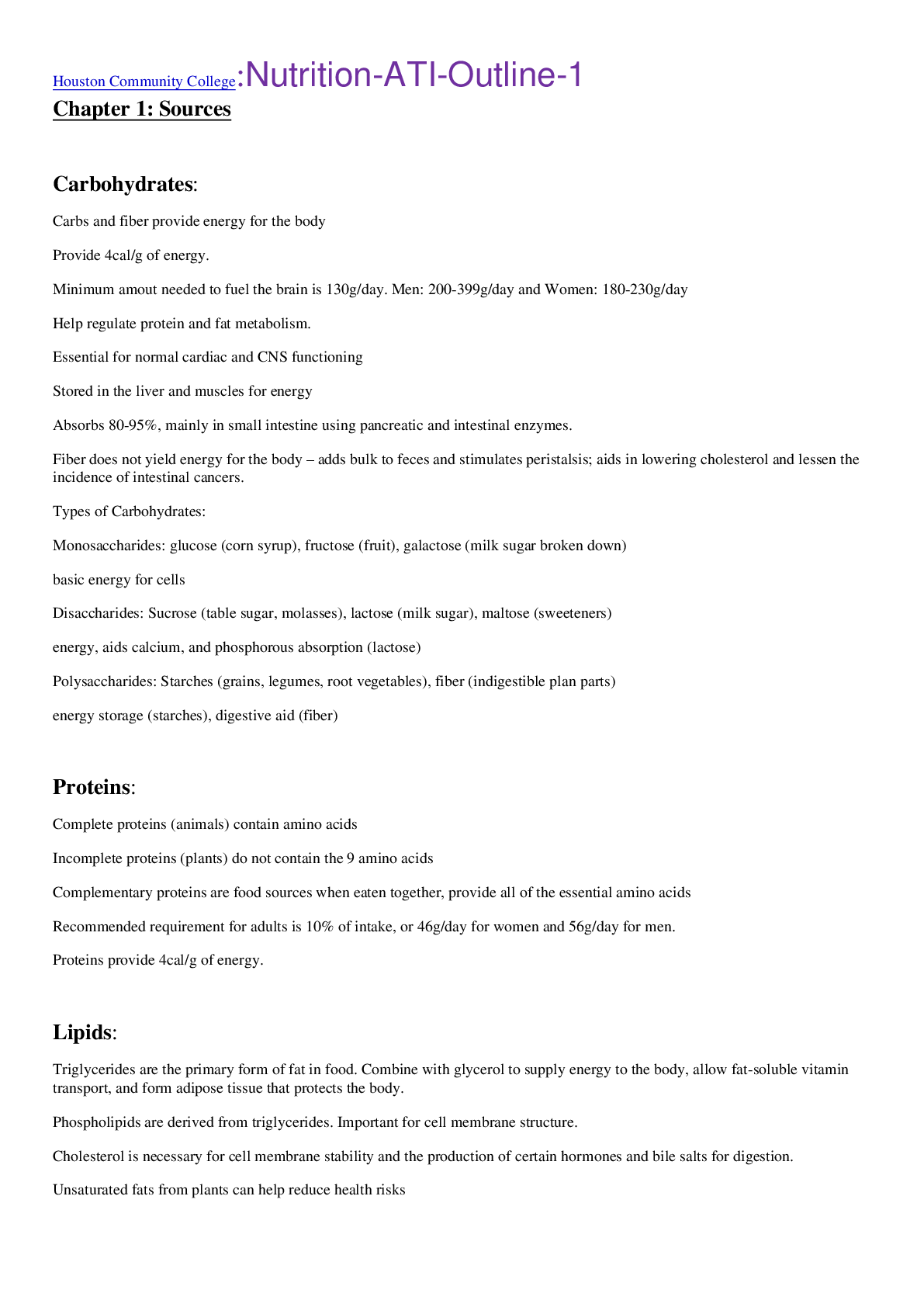
Chamberlain College: NR 446 REVIEW NOTES PART 3Nursing Intervention for Client with Dementia Perform self-assessment regarding possible feeling of frustration, anger, or fear when performing daily ... care for clients with progressive dementia. Nursing interventions are focused on protecting the client from injury as well as promoting client dignity and quality of life. Provide for a safe and therapeutic environment • Assign the client to a room close to the nurse’s station for close observation • Provide a room with the low level of visual and auditory stimuli. • Provide for well lit environment, minimizing contrast and shadows. • Have the client sit in the room with windows to help with time orientation. • Have the client to wear an identification bracelet; use monitors and bed alarm deices as needed. • Use restrains only as an intervention of last resort. • Administer medications PRN for agitation or anxiety. • Ensure safety in the physical environment, such as lowered bed and removal of scattered rugs to prevent falls. • Provide compensatory memory aids, such as clocks, calendars, photographs, memorabilia, seasonal decorations, and familiar objects. Reorient as necessary. • Provide eyeglasses, and assistive hearing device as needed. • Keep consistent caregivers. • Ensure adequate food and fluid intake. • Allow for safe pacing and wandering • Cover or remove mirrors to decrease fear an agitation. Communication • Communicate in calm reassuring tone. • Reinforce reality • Introduce self to client with each new contact. • Establish eye contact and use short, simple sentences when speaking to the client. • Encourage reminiscence about happy time; talk about familiar things. • Break instructions and activities into short timeframe. • Limit the number of choices when dressing or eating. • Minimize the need for decision making and abstract thinking to avoid frustration. • Avoid confrontation. • Encourage family visitation as appropriate. Dietary Rituals Hinduism • Some are vegetarians. Buddhism • Some are vegetarians. • Those practicing Buddhism avoid alcohol and tobacco. • Client may fast during holy day. Islam • Those practicing Islam avoid alcohol and pork. • Client may fast during Ramadan. Judaism • Some may practice Kosher diet. Christianity • Some avoid alcohol tobacco, and caffeine. • Client may fast during Lent. Mormonism • Those practicing Mormonism avoid alcohol, tobacco, and caffeine. Jehovah’s Witnesses • Clients avoid foods having prepared with blood. Communication Do’s and Don’ts: ● Nonverbal Communication ◯Nurses should be aware of how they communicate nonverbally. The nurse should assess the client’s nonverbal communications for the meaning being conveyed, remembering that culture impacts interpretation. Attention to the following behaviors is important, as it is compared to the verbal message being conveyed: ▪ Appearance ▪ Posture ▪ Gait ▪ Facial expressions ▪ Eye contact ▪ Gestures ▪ Sounds ▪ Territoriality ▪ Personal space ▪ Silence ● Essential Components of Therapeutic Communication ◯ Time – Plan for and allow adequate time to communicate. ◯ Attending behaviors or active listening – These are nonverbal means of conveying interest in another. >Eye contact typically conveys interest and respect but varies by situation and culture. >Body language and posture may demonstrate level of comfort and ease. >Vocal quality enhances rapport and emphasizes particular topics or issues. >Verbal tracking provides feedback by restating or summarizing a client’s statements. ◯ Caring attitude – Show concern and facilitate an emotional connection with the client and the client’s family. ◯ Honesty – Be open, direct, truthful, and sincere. ◯ Trust – Demonstrate reliability without doubt or question. ◯ Empathy – Convey an objective awareness and understanding of the feelings, emotions, and behaviors of others, including trying to envision what it must be like to be in the position of the client and the client’s family. ◯ Nonjudgmental attitude – This is a display of acceptance that will encourage open, honest communication. Nursing Process ● Assessment ◯ Assess verbal and nonverbal communication needs. ◯ Consider the client’s developmental level and how communication should be altered during the assessment phase. Children ☐ Use simple, straightforward language. ☐ Be aware of own nonverbal messages, as children are sensitive to nonverbal communication. ☐ Enhance communication by being at the child’s eye level. ☐ Incorporate play in interactions. Older Adult Clients ☐ Recognize that the client may require amplification. ☐ Minimize distractions, and face the client when speaking. ☐ Allow plenty of time for the client to respond. ☐ When impaired communication is assessed, ask for input from caregivers or family to determine the extent of the deficits and how best to communicate. Identify any cultural considerations that may impact communication. ● Planning ◯ Minimize distractions. ◯ Provide for privacy. ◯ Identify mutually agreed-upon client outcomes. ◯ Set priorities according to the client’s needs. ◯ Plan for adequate time for interventions. ● Implementation ◯ Establish a trusting nurse-client relationship. The client feels more at ease during the im plem entation phase w hen a helping relationship has been established. ◯ Provide empathetic responses and explanations to the client by using observations and providing hope, humor, and information. Barriers to effective Communication ● Asking irrelevant personal questions ● Offering personal opinions ● Giving advice ● Giving false reassurance ● Minimizing feelings ● Changing the topic ● Asking “why” questions ● Offering value judgments ● Excessive questioning ● Responding approvingly or disapprovingly Suspicious skin lesions for Cancer: ● Sunlight exposure is the leading cause of skin cancer. The most effective strategy for prevention of skin cancer is avoidance or reduction of skin exposure to sunlight. ● Precancerous skin lesions, called actinic keratoses, are common in people with chronically sun- damaged skin, such as older adults. ● There are three types of skin cancer. ◯ Because of the cumulative effects of sun damage over the lifespan, screening for suspicious lesions is an essential part of the routine physical assessment of older adult clients. ◯ In clients who have dark skin, lesions may appear on the palms or soles of feet. The nurse should assess suspicious lesions or skin patches for change in texture, tautness, or elasticity (color change is not always evident). Fractures: evaluating for assistive actions in assistive personal, What can/cannot be done? • Assess the client’s ability to help with transfers (balance, muscle strength, endurance). • Determine the need for additional personnel or assistive devices (transfer belt, hydraulic lift, sliding board). • Assess and monitor the client’s use of mobility aids (canes, walkers, crutches). • Include assistance or mobility aids needed for safe transfers and ambulation in plan of care. GERD interventions and findings: GERD: is a common condition characterized by gastric content and enzyme leakage into the esophagus. These corrosive fluids irritate the esophageal tissue and limit its ability to clear them from the esophagus. Findings: The main symptom of GERD is frequent and prolonged heartburn(dyspepsia) and regurgitation (acid reflux) in relationship to eating activities or position. Classic symptoms: dyspepsia after eating an offending food or fluid and regurgitation. Other S/S: Throat irritation (chronic cough, laryngitis), hyper-salivation, eructation, flatulence, bitter taste in mouth or atypical chest pain. Interventions: Medications can be taken such as: antacids, Histamine receptor antagonist, Proton Pump inhibitors, Prokinetics Therapeutic Procedures such as Stretta procedure can be done with uses radiofrequency energy, applied by an endoscope to the LES muscle. This causes the tissue to contract and tighten. Educate the client to change their diet by avoiding offending foods, avoid large meals, remain upright after eating and avoiding eating before bed. Nursing Care for a Suicidal Patient (Mental Health, P. 274) Self-assessment • The nurse must determine how she feels personally about suicide. • The nurse must become comfortable asking personal questions about suicidal ideation and following up on client’s answers. • Death of a client by suicide can cause health care professionals to experience a hopelessness, helplessness, ambivalence, anger, anxiety, avoidance, and denial. • Nurses who work with suicidal clients can benefit personally by debriefing, sharing, andcollaborating with other health professionals. Suicide precautions include milieu therapy within the facility. • Initiate one-on-one constant supervision around the clock, always having the client in sight and close. • Document the client’s location, mood, quoted statements, and behavior every 15 min or per facility protocol. • Remove all glass, metal silverware, electrical cords, vases, belts, shoelaces, metal nail files, tweezers, matches, razors, perfume, shampoo, and plastic bags from the client’s room and vicinity. • Allow the client to use only plastic eating utensils. • Check the environment for possible hazards (such as windows that open, overhead pipes that are easily accessible.) • During observation periods, always check the client’s hands, especially if they are hidden from sight. • Do not assign to a private room if possible and keep door open at all times. • Ensure that the client swallows all medications. • Identify whether or not the client’s current medications can be lethal with overdose. If so, collaborate with the provider to have less dangerous medications substituted if possible. • Restrict the visitors from bringing possibly harmful items to the client. Therapeutic communication • When questioning the client about suicide, always use a follow-up question if the first answer is negative. For example: the client says, “I’m feeling completely hopeless.” The nurse says, “Areyou thinking of suicide?” Client: “No, I’m just sad.” Nurse: “I can see you’re very sad. Are you thinking about hurting yourself?” Client: “Well, I’ve thought about it a lot.” • Establish a trusting therapeutic relationship. • Limit the amount of time an at-risk client spends alone. • Involve significant others in the treatment plan. • Carry out treatment plans for the client with comorbid disorders, such as a dual diagnosis of substance use disorder INTERVENTIONS TO PROMOTE SLEEP [FUNDAMENTALS, P. 372] ● Adequate amounts of sleep and rest promote health. Too little sleep leads to an inability to concentrate, poor judgment, moodiness, and an increased risk for accidents. ● Chronic sleep loss can increase the risk of obesity, depression, hypertension, diabetes mellitus, heart attack, and stroke. ● The sleep cycle consists of nonrapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. Typically, after Stage 1 of NREM sleep, people cycle four to six times through the other stages of sleep. With each cycle, the length of time in REM sleep increases. NREM sleep accounts for 75% to 80% of sleep time. ○ Stage 1 NREM ■ Very light sleep ■ Only a few minutes long ■ Vital signs and metabolism beginning to diminish ■ Awakens easily ■ Feels relaxed and drowsy ○ Stage 2 NREM ■ Deeper sleep ■ 10 to 20 min in length ■ Vital signs and metabolism continuing to diminish ■ Requires slightly more stimulation to awaken ■ Increased relaxation ○ Stage 3 NREM ■ Deep sleep ■ 15 to 30 min in length ■ Vital signs continuing to decrease ■ Difficult to awaken ■ Relaxation with little movement ○ Stage 4 NREM ■ Called delta sleep ■ Deepest sleep ■ 15 to 30 min in length ■ Vital signs low ■ Very difficult to awaken ■ Physiologic rest and restoration ■ Enuresis, sleepwalking, sleep talking possible ■ Repair and renewal of tissue ○ REM ■ Vivid dreaming ■ About 90 min after falling asleep ■ Longer with each sleep cycle ■ Average length 20 min ■ Varying vital signs ■ Very difficult to awaken ■ Cognitive restoration ● Sleep Duration 4 ○ Sleep averages vary with the developmental stage, with infants and toddlers averaging 14 to 16 hr/day. This declines gradually throughout childhood, with adolescents averaging 9 to 10 hr/day and adults 7 to 9 hr/day. ● Common Sleep Disorders ○ Insomnia, the most common sleep disorder, is the inability to get an adequate amount of sleep and to feel rested. It might mean difficulty falling asleep, difficulty staying asleep, awakening too early, or not getting refreshing sleep. Acute insomnia lasts a few days and may be due to personal stressors. Chronic insomnia lasts a month or more. Some people have intermittent insomnia, sleeping well for a few days and then having insomnia for a few days. Women and older adults are more prone to insomnia. ○ Sleep apnea is more than five breathing cessations lasting longer than 10 seconds per hour during sleep, resulting in decreased arterial oxygen saturation levels. Sleep apnea can be a single disorder or a mixture of the following: ■ Central - central nervous system dysfunction that fails to trigger breathing during sleep. ■ Obstructive - structures in the mouth and throat occlude the upper airway. ○ Narcolepsy - sudden attacks of sleep during waking hours. It often happens at inappropriate times and increases the risk for injury. ● Assessment and Data Collection ○ Ask about sleep patterns, history, and any recent changes. ○ Ask about sleep problems (type, symptoms, timing, seriousness, related factors, aftereffects). ○ Use a linear scale or visual with “best sleep” on one end and “worst sleep” on the opposite end and ask for a sleep rating on a 0 to 10 scale. ○ Check for common factors that interfere with sleep: ■ Illness – may require more sleep or disrupt sleep, such as nocturia. ■ Current life events (traveling more, change in work hours). ■ Emotional stress or mental illness (anxiety, fear). ■ Diet (caffeine consumption, heavy meals before bedtime). ■ Exercise – promotes sleep if at least 2 hr before bedtime; otherwise, it can disrupt sleep. ■ Sleep environment too light, the wrong temperature, or too noisy (children, pets, loud noise, snoring partner). ■ Medications – may induce sleep but interfere with restorative sleep; others cause insomnia (bronchodilators, antihypertensives). ● Nursing Interventions ○ Help clients establish and follow a bedtime routine. ○ Limit waking clients during the night. ○ Help with personal hygiene needs or a back rub prior to sleep to increase comfort. ○ Instruct clients to: ■ Exercise regularly at least 2 hr before bedtime. ■ Arrange the sleep environment for comfort. ■ Limit alcohol, caffeine, and nicotine at least 4 hr before bedtime. ■ Limit fluids 2 to 4 hr before bedtime. ■ Engage in muscle relaxation if anxious or stressed. ○ Instruct clients with narcolepsy to: ■ Exercise regularly. ■ Eat small meals that are high in protein. ■ Avoid activities that increase sleepiness (sitting too long, warm environments, drinking alcohol). ■ Avoid activities that would cause injury should the client fall asleep (driving, heights). ■ Take naps when drowsy or when narcoleptic events are likely. ■ Take stimulants the provider prescribes. ○ Consider continuous positive airway pressure (CPAP) devices for clients who have sleep apnea. ○ Consult the provider about trying sleep-promoting, over-the-counter products (melatonin, valerian, chamomile). ○ As a last resort, suggest that the provider prescribe a pharmacological agent. Medications of choice for insomnia are benzodiazepine-like medications, which include the sedativehypnotics zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata). TPN monitoring Infection and sepsis are evidenced by a fever or elevated WBC count. Infection can resultfrom contamination of the catheter during insertion, contaminated solution, or a long-termindwelling catheter. Metabolic complications include hyperglycemia, hypoglycemia, hyperkalemia, hypophosphatemia,hypocalcemia, hypoalbuminemia, dehydration, and fluid overload (as evidenced by weight gaingreater than 1 kg/day and edema). Mechanical complications include catheter misplacement, pneumothorax (evidenced by shortnessof breath, diminished or absent breath sounds), subclavian artery puncture, catheter embolus, airembolus, thrombosis, obstruction, and bolus infusion. Nursing care is focused on preventing complications through consistent monitoring. Specificmonitoring guidelines vary among health care facilities. Ongoing assessment parameters include I&O, daily weights, vital signs, pertinent laboratoryvalues (e.g., serum electrolytes, blood glucose), and ongoing evaluation of the client’s underlyingcondition. This data is used to determine the client’s response to therapy and the formulation ofthe solution to prevent nutrient deficiencies or toxicities. Monitor serum and urine glucose as prescribed and per facility guidelines. Sliding scale insulinmay be prescribed to intervene for hyperglycemia, or regular insulin may be added to thePN solution. Flow rate should be monitored carefully.Failure to provide optimal nutritional intake is the result of solutions administered too slowly. Hyperosmolar diuresis can result from an infusion that is too rapid, and can lead todehydration, hypovolemic shock, seizures, coma, and death. Hyperglycemia, hyperosmolar diuresis, and fluid overload may occur if the PN solution isincreased when available. Do not attempt to increase the rate of the PN solution to “catch up.” Monitor for “cracking” of TPN solution. This occurs if the calcium or phosphorous content ishigh or if poor-salt albumin is added. A “cracked” TPN solution has an oily appearance or alayer of fat on top of the solution and should not be used. For mild to moderate pain Medication ›› Acetaminophen (Tylenol), Ketorolac (Toradol), Aspirin (acetylsalicylic acid), Ibuprofen (Motrin), Celecoxib (Celebrex) For moderate to severe pain ›› For breakthrough pain Medication ››Morphine sulfate, Meperidine (Demerol), Hydromorphone (Dilaudid), Oxycodone (Oxycontin), Fentanyl (Sublimaze) available for transdermal use May reduce pain by reducing swelling Medication ›› Prednisolone (Prelone), Dexamethasone (Decadron) Treat neuropathic pain Used in conjunction with bupivacaine in epidural or other local infusions. Medication ›› Clonidine (Catapres), Muscle spasms associated with cancer pain Medication ›› Baclofen (Lioresal) May be administered via an infusion pump directly into the area of pain (intrathecal, intra-articular, intrapleural) to provide pain relief Medication ›› Lidocaine (Xylocaine), Bupivacaine (Marcaine), Ropivacaine (Naropin) Treat oral ulcers that may be caused by radiation or chemotherapy and neuropathic pain, such as in postmastectomy axillary pain Medication ›› Lidocaine HCl (Lidoderm patch), Eutectic mixture of local anesthetic (EMLA) cream Regional nerve blocks An anesthetic agent, such as bupivacaine, and/or a corticosteroid is injected directly into a nerve root to provide pain relief. Used to identify or treat an isolated area of pain For example, an intercostal nerve block may be used to treat chest or abdominal wall pain. The procedure may take from 15 min to 1 hr, depending upon the area receiving the block. Epidural or intrathecal catheters A local anesthetic or analgesic is injected into the epidural space (the area outside the dura mater of the spinal cord) or intrathecal space (the subarachnoid area within the spinal cord sheath that contains cerebrospinal fluid). An external catheter is surgically placed under the skin with an external port for long- term use. Used for chronic pain management. May be attached to a continuous infusion or injected as needed. Used for upper abdominal pain, thoracic pain, and pain located below the umbilicus Blood Transfusion (Process and Nursing Interventions) Preprocedure o Explain the reason for blood transfusion o Check blood type compatibility o Assess lab values (H&H) o Verify prescription o Obtain blood samples for compatibility determination and cross match o Initiate large-bore IV access (20-gauge needle) o Assess hx of blood transfusion reactions o Obtain blood product, then inspect for discoloration, excessive bubbles, and cloudiness o Protocol – with another nurse, confirm client’s identity, blood compatibility, and expiration time of the blood product o Prime administration set with 0.9% Sodium Chloride (ONLY) o Ascertain whether a filter should be used o Obtain v/s o Begin blood transfusion and use blood warmer if needed Intraprocedure o Remain with the client for the first 15-30min. Monitor: V/S (qh afterwards) Rate of infusion Respiratory status Sudden increase in anxiety Breath sounds Neck-vein distention o Notify provider if reaction occur o To avoid infection, infuse blood product within 2-4 hrs. Postprocedure o Obtain v/s after transfusion o Dispose administration set to biohazard bags o Monitor blood values (CBC, H&H) o Document the client’s response Chest Tube Insertion (Identifying Complications) Complications Cause and Manifestation Air leaks Cause - Continuous bubbling Accidental disconnections, system breakage, or removal Occurs any time Tension pneumothorax Cause - Sucking chest wounds, prolonged clamping of the tubing, kinks in the tubing, or obstruction Manifestation - Tracheal deviation, absent breath sounds on one side, distended neck veins, respiratory distress, asymmetry of the chest, and cyanosis Contraindication for diabetic patient w/ radiography If patient is taking metformin HCI/gluchpahage → stop medication for 48 hrs before any type of radiographic test with iodinated contrast dye: may cause lactic acidosis Clinical manifestation of smallpox The first symptoms of smallpox usually appear 12 to 14 days after you're infected following the incubation period, a sudden onset of flu-like signs and symptoms occurs These include → Fever, overall discomfort, headache, severe fatigue, severe back pain, loss of appetite, vomiting, possibly Rash → macules start in trunk and face, spreading to rest of the body, progressing to papules → Vesicles follow, with crusts forming → Scabs appear in approximately 1 week All infections we want CONTACT PRECAUTIONS "MRS WEE" M: MRSA R: RSV S: Skin infections (herpes zoster, cutaneous diphtheria, impetigo, pediculosis, scabies, and staph) W: Wound infections E: Enteric infections (C-Diff) E: Eye infections (conjunctivitis) VRSA - contact and airborne precautions (private room, door closed, negative pressure) Contact Precautions • Prevent transmission of infectious agents that are spread by direct or indirect contact with the client or the client’s environment. These precautions are applied in the presence of wound drainage, fecal incontinence, or other bodily discharges that suggest an increased potential for environmental contamination and risk of contamination. • PPE: gloves, gown; as needed use of mask and goggles. o Order of PPE application: gown, mask, goggles/face shield, gloves o Order of PPE removal: gloves, goggles/face shield, gown, mask • Nursing interventions: (in addition to standard precautions) o Private room preferred; may cohort with client who has infection with same organism. o Gloves and gown worn by caregivers and visitors. o Disposal of infectious dressing material into nonporous bag. o Dedicated equipment for the patient or disinfect after each use. o Client to leave room only for essential clinical reasons. • Protective isolation: o Used to protect clients who have an increased susceptibility to infections, are receiving chemotherapy, or are immunosuppressed or neutropenic. o Nursing interventions: Follow standard precautions. Institute maximum protection, which may include the use of sterile linens, food, and other supplies. Minimize exposure to microorganisms found on the outer layers of fresh flowers, fruits, and vegetables. Wear sterile gloves and gown/mask when in contact with client. Maximum protection will require ventilated/positive pressure room. Medication Classification: Anticoagulants – Parenteral and Glycoprotein Inhibitors Medication: heparin, enoxaparin (Lovenox), dalteparin (Fragmin), tinzaparin (Innohep), fondaparinux (Arixtra) Therapeutic Uses ■ In conditions necessitating prompt anticoagulant activity (evolving stroke, pulmonary embolism, massive deep- vein thrombosis) ■ Prophylaxis against postoperative venous thrombosis (for example, hip/knee or abdominal surgery) ■ For treatment of disseminated intravascular coagulation (DIC) ■ Prevent and treat deep-vein thrombosis (DVT) and pulmonary Complications Nursing Intervention/ Education › Hemorrhage › Monitor vital signs. › Advise clients to observe for bleeding (increased heart rate, decreased blood pressure, bruising, petechiae, hematomas, black tarry stools). › Monitor platelet count. Instruct client to avoid aspirin. › Monitor activated partial thromboplastin time (aPTT). Keep value at 1.5 to 2 times the baseline. › Neurologic damage from hematoma formed during spinal or epidural anesthesia › Assess insertion site for signs of hematoma formation, such as redness or swelling. Monitor sensation and movement of lower extremities. Notify provider of abnormal findings. › Thrombocytopenia, as evidenced by low platelet count › Monitor platelets. Discontinue medication for platelet count less than 100,000/mm3. › Toxicity/overdose › Administer protamine (heparin antagonist) › Protamine should be administered slowly intravenously, no faster than 20 mg/min or 50 mg in 10 min. Contraindications › Anti-platelet agents such as aspirin, NSAIDs, and other anticoagulants may increase risk for bleeding. › Avoid concurrent use when possible. › Monitor carefully for evidence of bleeding. › Take precautionary measures to avoid injury (limit venipunctures and injections). Antiplatelet/glycoprotein inhibitors • Select Prototype Medication: abciximab (ReoPro) • Other Medications: eptifibatide (Integrilin), tirofiban (Aggrastat) Therapeutic Uses • Primary prevention of acute myocardial infarction • Prevention of reinfarction in clients following an acute myocardial infarction • Prevention of ischemic stroke • Acute coronary syndromes Adverse Effects Nursing Interventions/Education › Hypotension and bradycardia › Monitor heart rate and blood pressure. › Prolonged bleeding time, gastric bleed, thrombocytopenia, bleed from cardiac catheterization site › Monitor bleeding time. › Monitor for gastric bleed (coffee-ground emesis or bloody, tarry stools). › Monitor for bruising, petechiae, and bleeding gums. › Apply pressure to cardiac catheter access site. Contradictions • Pregnancy Risk Category C. • Contraindications include clients who have bleeding disorders, thrombocytopenia, recent stroke, AV malformation, aneurysm, uncontrolled hypertension, and recent major surgery. • Use cautiously in clients who have peptic ulcer disease and severe renal and/or hepatic disorders. Calorie calculation for weight management; able to read nutritional label Carbohydrates – 4cal/g Proteins – 4cal/g Fats – 9cal/g Nutritional Labels: In order to read nutritional labels it is first important to look at the serving size, the number of servings per container, and the grams of total carbohydrates, proteins, and fats per serving. The total carbohydrates, proteins, and fats tell how many grams of each are in one serving. There can be more than one serving size in the package so if you eat more than one serving, you will need to multiply the grams of each accordingly. EXAMPLE: • The serving size listed is 1 cup (or 4 ounces). • The number of servings per container is 3. • The grams of total carbohydrate per serving is 10 grams. • If you eat the entire box, you would be eating 30 grams of total carbohydrate (3 servings x 10 grams total carbohydrate equals 30 grams). • Or if you eat half the box, you would eat 15 grams of total carbohydrate (30 grams of total carbohydrate divided by 2 equals 15 grams of total carbohydrate). Indications of withholding medication propranolol (Inderal) beta-blocker Indications to withholding Propranolol: • Contraindicated in clients who have AV heart block, sinus bradycardia, bronchial asthma, cardiogenic shock, or heart failure • Nonselective beta-adrenergic blockers are contraindicated in clients who have asthma, bronchospasm, and heart failure • In general, use beta-adrenergic blockers cautiously in clients who have myasthenia gravis, diabetes mellitus, depression, and in older adults and those with a history of severe allergies. • Hold medication if HR is less than 60/min • Use cautiously in clients who have Wolff-Parkinson-White syndrome, liver, thyroid, or respiratory dysfunction • Treadmill test • Other contraindications include depression, tobacco smoking, muscle problems, cerebrovascular anomaly associated with PHACE syndrome, complete heart block, sick sinus syndrome, occasional numbness, prickling, or tingling of fingers and toes, chronic bronchitis, emphysema, severe COPD, bronchospasm, hardening of the liver, liver problems, kidney disease, blood circulation failure, GDM, and low blood sugar Domestic Abuse Violence by one person toward another is a social act involving a serious abuse of power. Usually, a relatively stronger person controls or injures another, typically the least powerful person accessible to the abuser. This includes acts of violence committed by spouse against spouse, parent against child, child against parent, or stranger against victim. Risk Factors • The female partner is the victim in the majority of family violence, but the male partner may also be a victim of violence. • Victims are at the greatest risk for violence when they try to leave the relationship. • Pregnancy tends to increase the likelihood of violence toward the domestic partner. The reason for this is unclear, but could be jealousy or feelings of rejection. • Victims of rape include individuals of all ages and can be either male or female Within the family, a cycle of violence can occur between domestic (intimate) partners: • Tension-building phase – The abuser has minor episodes of anger and may be verbally abusive and responsible for some minor physical violence. The victim is tense during this stage and tends to accept the blame for what is happening. • Serious battering phase – The tension increases and a serious incident takes place. The victim may try to cover up the injury or may get help. • Honeymoon phase – The situation is defused for awhile after the violent episode. The abuser becomes loving, promises to change, and is sorry for the behavior. The victim wants to believe this and hopes for a change. Eventually, the cycle begins again. Periods of escalation and de-escalation usually continue with shorter and shorter periods of time between the two. Repeated episodes of violence lead to feelings of powerlessness. Nursing Care All states have mandatory reporting laws that require nurses to report suspected abuse. There are civil and criminal penalties for not reporting suspicions of abuse. Nursing interventions for child or older adult abuse must include the following: • Mandatory reporting of suspected or actual cases of child or older adult abuse • Complete, accurate documentation of subjective and objective data obtained during data collection • Conduct a nursing history. • Provide privacy when conducting interviews about family abuse. • Be direct, honest, and professional. • Use language the client understands. • Be understanding and attentive. • Use therapeutic techniques that demonstrate understanding. • Use open-ended questions to elicit descriptive responses. • Inform the client if a referral must be made to children’s or adult protective services and explain the process. • Provide basic care to treat injuries. • Request appropriate referrals. Contraindications of using Nitrates: Contraindications/Precautions ●● Nitroglycerin is Pregnancy Risk Category C. ●● This medication is contraindicated in clients with hypersensitivity to nitrates. ●● Nitroglycerin is contraindicated in clients with traumatic head injury because the medication can increase intracranial pressure. ●● Use cautiously in clients taking antihypertensive medications and clients who have renal or liver dysfunction. Appropriate use of crutches Standing up with crutches • Ensure the patient can tolerate sitting in an upright position • Place both crutches in the unaffected side • Have the other hand grab onto the side rail, and have the patient push up to a standing position. • Once standing in a stable position, have the patient place a crutch under each arm • At this point have the patient get into the crutch stance by placing the crutches 6 inches to the side of their feet, and 6 inches forward. Sitting down with crutches • Have the patient turn around and place grasp the crutches under one hand, and have the other hand as support themself on the bed rail • Instruct the client to lower themself down slowly 4 point gait • Have the patient move the right crutch forward and then the left foot even with right crutch. • Next have the patient move the left crutch forward and the right foot and even with the left crutch • Repeat the sequence 3 point gait • move both crutches forward with weight on the unaffected leg • move unaffected leg forward, shifting weight to the crutches • and repeat the sequence 2 point gait • Move the left foot and right crutch forward • Move the right foot and left crutch forward • Repeat the sequence Swing-to gait • Move both crutches forward • lift both feet and swing forward next to the crutches • Repeat the sequence Swing through gait • Move both crutches forward • lift both feet and swing the feet in front of the crutches • Repeat the sequence Interventions to prevent delays in wound healing • Provide adequate hydration and meet protein and calorie needs o Encourage an intake of 2000 to 3000 mL of fluid/day from food and beverage sources if not contraindicated (Heart failure or renal failure) o Provide education about good sources of protein (meat, fish, poultry, eggs, dairy products beans, nuts whole grains). o If serum albumin is below 3.5 g/dL, because a lack of protein puts teh client at greater risk for delayed wound healing and infection o Provide nutritional support as indicated (vitamin and mineral supplements, • Perform wound cleansing o Cleanse in a direction from the least contaminated toward the most contaminated o Use gentle friction when cleansing or applying solutions to the skin to avoid bleeding or further injury of the wound o While other mild cleansing agents may be prescribed, isotonic solutions remain the preferred cleansing agents o Never use the same gauze to cleanse across an incision or wound more than once o Irrigation with a solution filled syringe held 2.5 cm (1 in) above the wound may be used • Notes: Factors affecting wound healing o Loss of skin turgor o Skin fragility o decreased peripheral circulation and oxygenation o slower tissue regernation o decreased absorption of nutrients o decreased collagen o impaired function of the immune system [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
48