*NURSING > STUDY GUIDE > NR 602 midterm study guide 2021/22 LATEST 100%graded(A) (All)
NR 602 midterm study guide 2021/22 LATEST 100%graded(A)
Document Content and Description Below
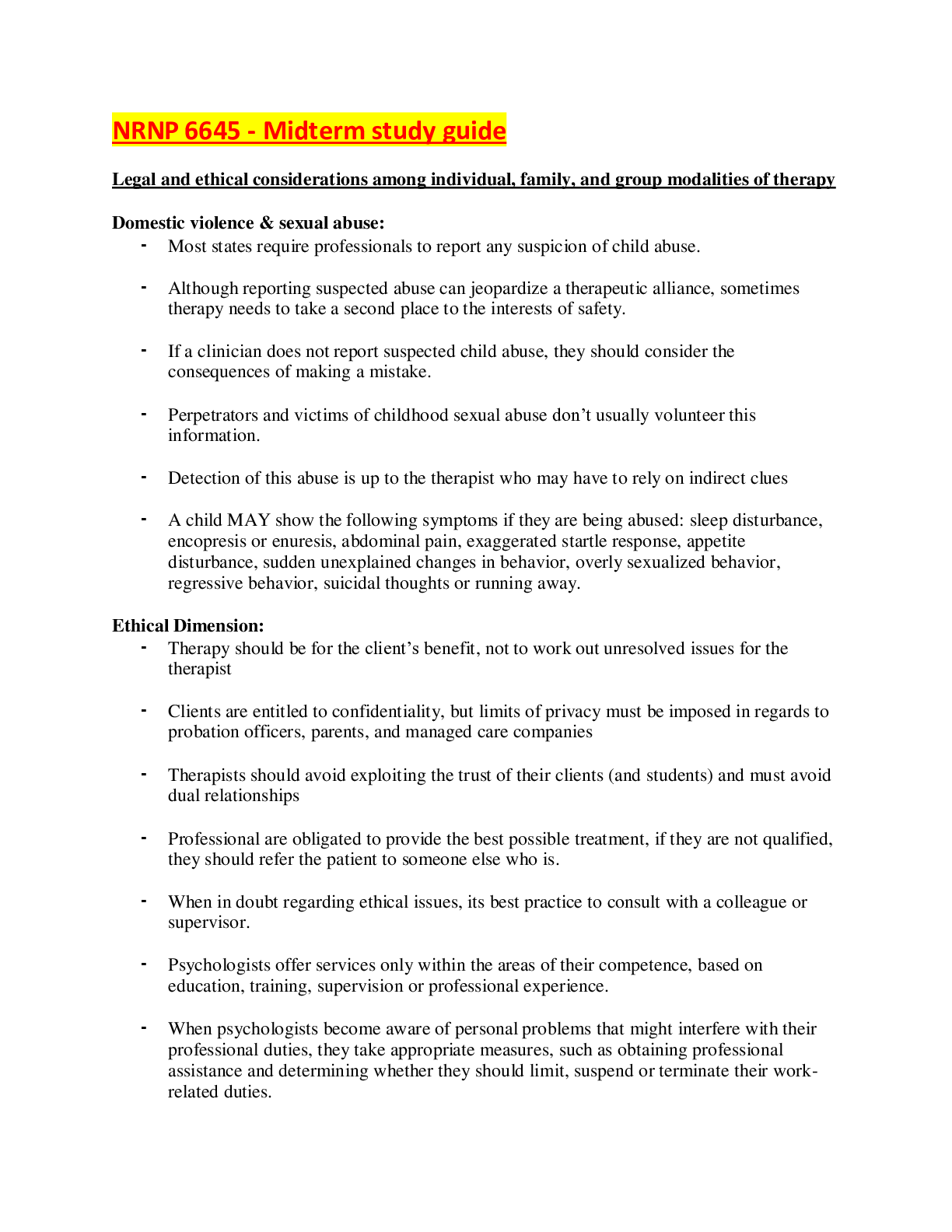
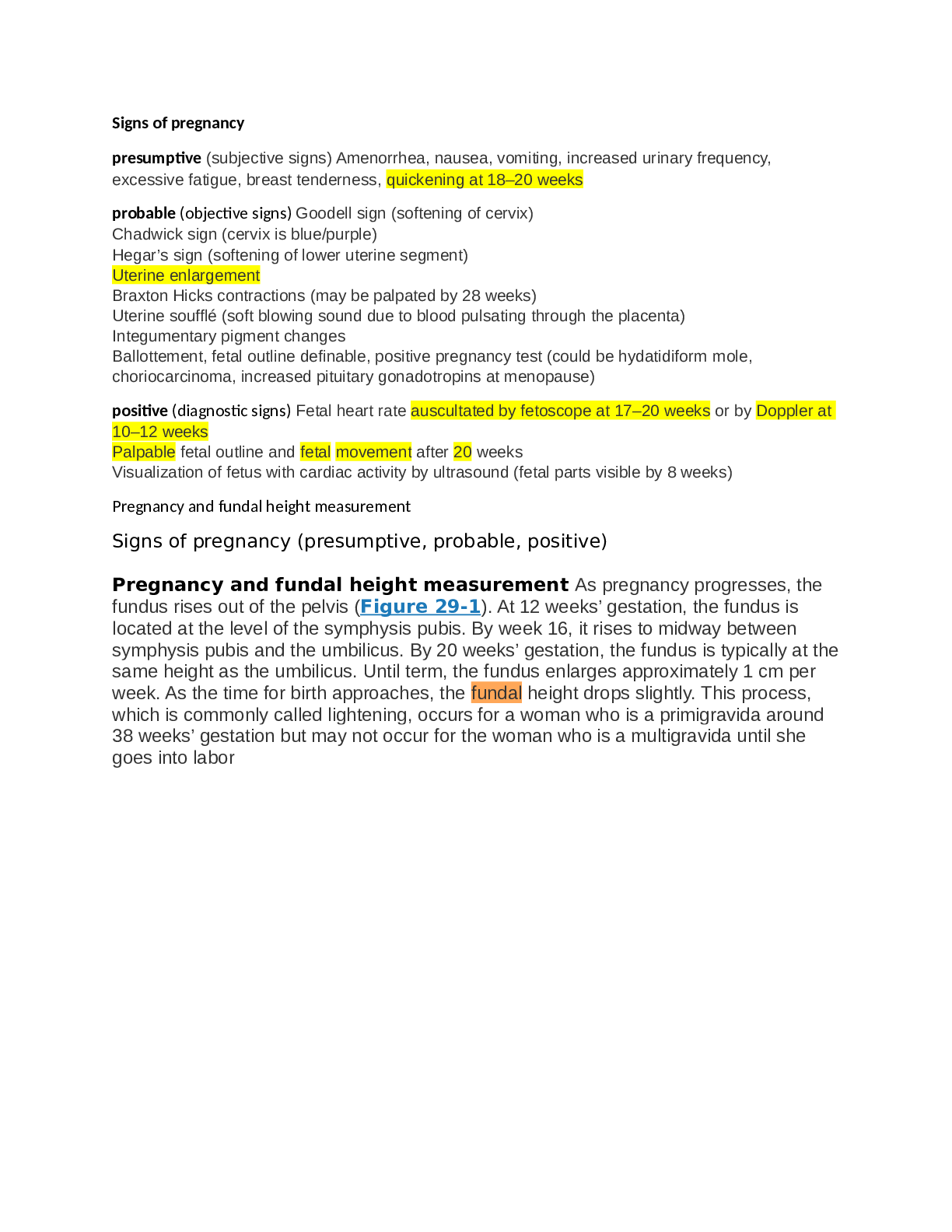
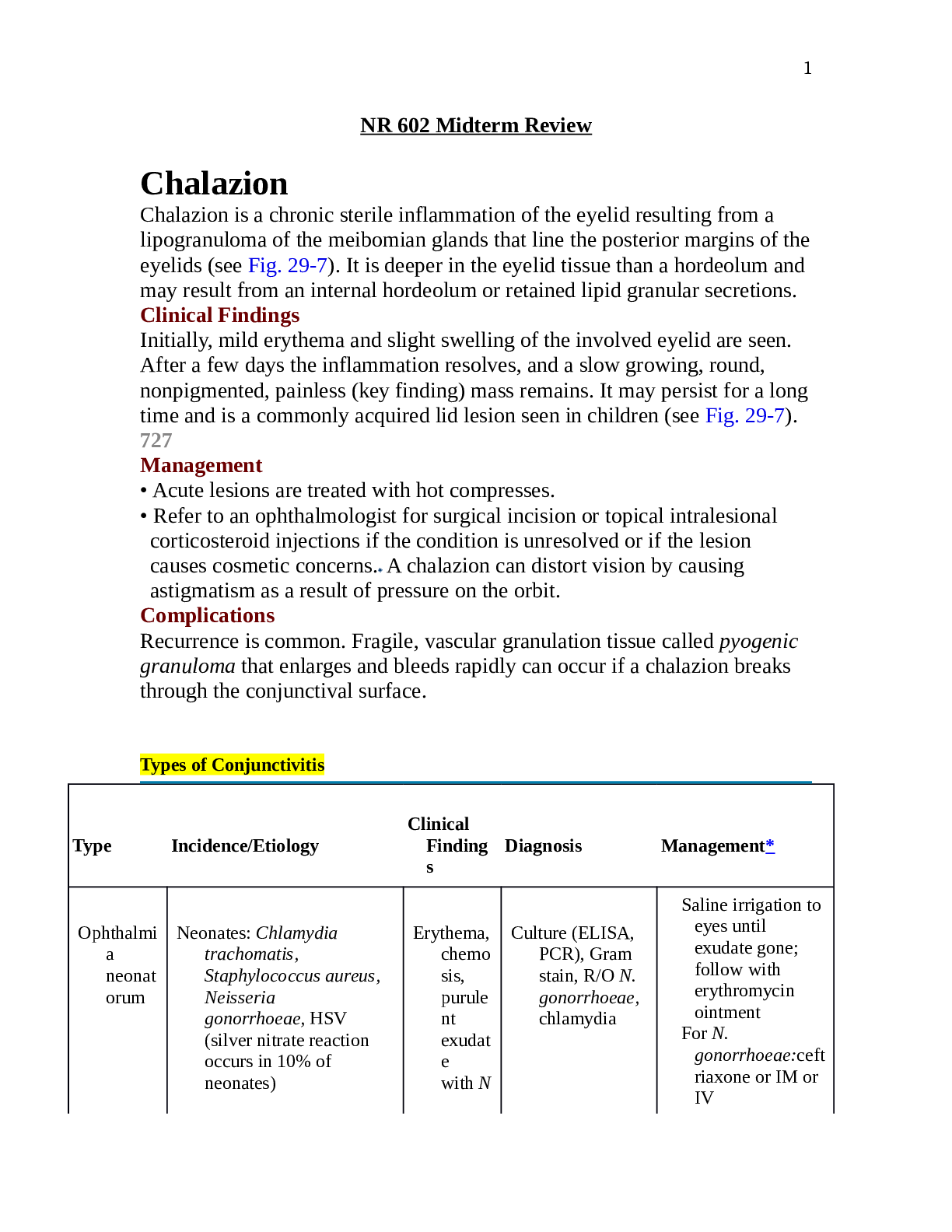
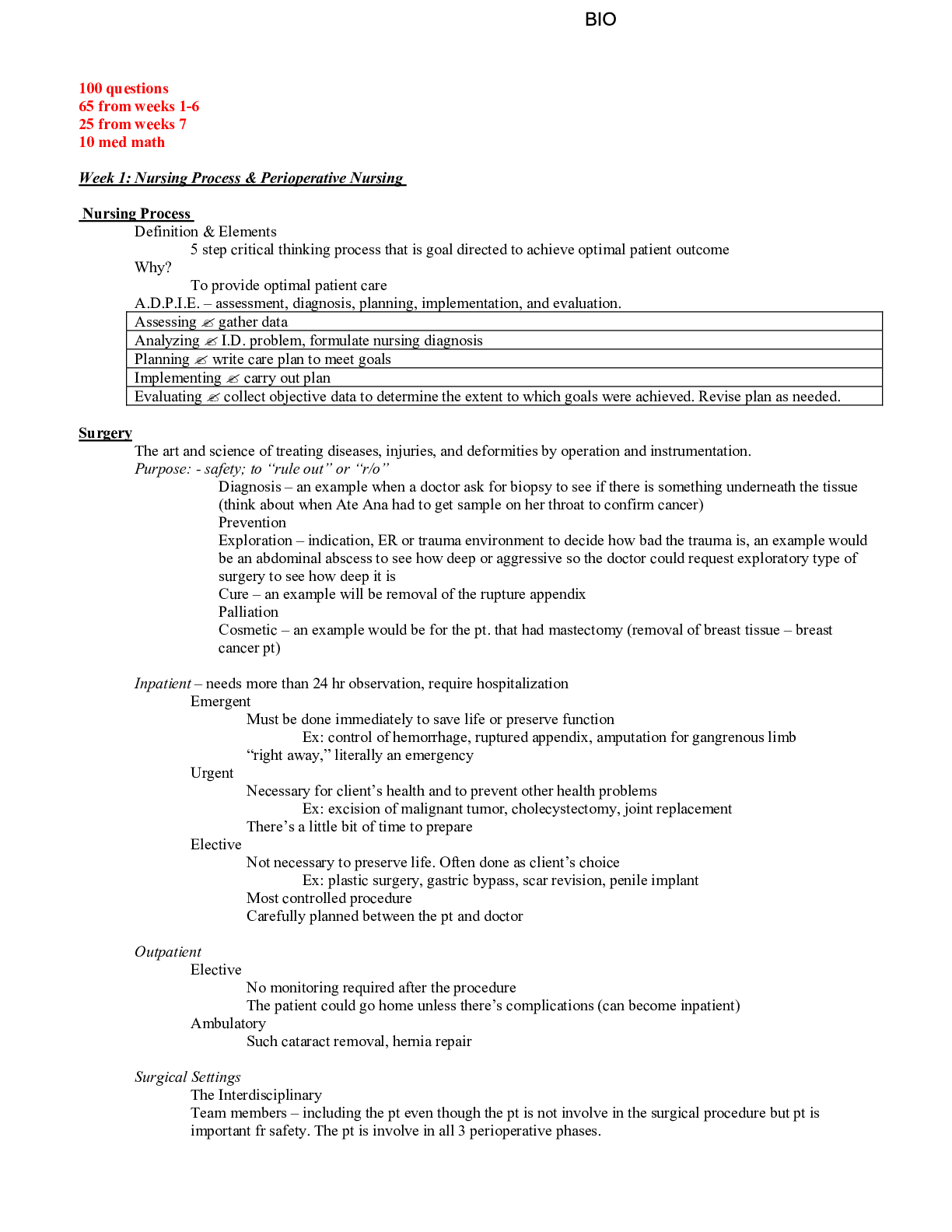
Signs of pregnancy presumptive (subjective signs) Amenorrhea, nausea, vomiting, increased urinary frequency, excessive fatigue, breast tenderness, quickening at 18–20 weeks probable (objective si... gns) Goodell sign (softening of cervix) Chadwick sign (cervix is blue/purple) Hegar’s sign (softening of lower uterine segment) Uterine enlargement Braxton Hicks contractions (may be palpated by 28 weeks) Uterine soufflé (soft blowing sound due to blood pulsating through the placenta) Integumentary pigment changes Ballottement, fetal outline definable, positive pregnancy test (could be hydatidiform mole, choriocarcinoma, increased pituitary gonadotropins at menopause) positive (diagnostic signs) Fetal heart rate auscultated by fetoscope at 17–20 weeks or by Doppler at 10–12 weeks Palpable fetal outline and fetal movement after 20 weeks Visualization of fetus with cardiac activity by ultrasound (fetal parts visible by 8 weeks) Pregnancy and fundal height measurement Signs of pregnancy (presumptive, probable, positive) Pregnancy and fundal height measurement As pregnancy progresses, the fundus rises out of the pelvis (Figure 29-1). At 12 weeks’ gestation, the fundus is located at the level of the symphysis pubis. By week 16, it rises to midway between symphysis pubis and the umbilicus. By 20 weeks’ gestation, the fundus is typically at the same height as the umbilicus. Until term, the fundus enlarges approximately 1 cm per week. As the time for birth approaches, the fundal height drops slightly. This process, which is commonly called lightening, occurs for a woman who is a primigravida around 38 weeks’ gestation but may not occur for the woman who is a multigravida until she goes into labor Naegele’s rule Add seven days to the first day of your LMP and then subtract three months. For example, if your LMP was November 1, 2017: Add seven days (November 8, 2017). Subtract three months (August 8, 2017). The EDD is calculated by adding seven days to the first day of the last menstrual period, subtracting three months and adding one year. This formula is known as Naegele's Rule. For example, if the patient's last menstrual period, LMP, was on August 10, 2019, the EDD would be calculated as follows. LMP equals August 10, 2019 plus seven days. August 17, 2019, minus three months. May 17, 2019 plus one year and that equals May 17, 2020. Hematological changes during pregnancy During pregnancy, the heart is displaced upward and to the left within the chest cavity by the gravid uterus’s pressure on the diaphragm. As pregnancy progresses, the risk for inferior vena cava and aortic compression leading to supine hypotension increases when the woman lies in a supine position. To avoid hypotension and potential syncope, the woman should be advised to lie in a left lateral position. Hemodynamic changes and anatomic changes also may alter vital signs in the pregnant woman (Table 29-2). Cardiac output in pregnancy increases by 30% to 50% over that in women who are not pregnant (Blackburn, 2013; Ouziunian & Elkayam, 2012). This increase peaks in the early third trimester and is maintained until birth. Half of the total increase in cardiac output, however, occurs by the eighth week of pregnancy (Blackburn, 2013). Therefore, women with cardiac disease may become symptomatic during the first trimester. Stroke volume is also increased during pregnancy by 20% to 30%. These increases in cardiac output and stroke volume allow for the 30% increase in oxygen consumption observed during pregnancy. TABLE 29-2 Vital Sign Changes in Pregnancy Vital Sign Changes in Pregnancy Measurement Alterations in Pregnancy Heart rate and heart sounds Volume of the first heart sound may be increased with splitting. Third heart sound may be detected. Systolic murmurs may be detected. Increases by 15–20 beats/min by 32 weeks’ gestation. Palpate the maternal pulse when auscultating the fetal heart rate to be able to distinguish between the two. Respiratory rate Increases by 1–2 breaths/min None BP First trimester: same as prepregnancy values Second trimester: systolic BP decreases by 2–8 mm Hg and diastolic BP decreases by 5–15 mm Hg due to peripheral vascular resistance Third trimester: gradually returns to prepregnancy values Use of an automated cuff may improve accuracy of measurement, as some pregnant women do not have a fifth Korotkoff sound. Systolic and diastolic BP may be 16 mm Hg higher when taken while the woman is sitting. BP readings may decrease in the maternal left lateral position. Abbreviation: BP, blood pressure. Data from Jarvis, C. (2016). Physical examination and health assessment (7th ed.). St. Louis, MO: Saunders Elsevier; Ouziunian, J., & Elkayam, U. (2012). Physiologic changes during normal pregnancy and delivery. Cardiology Clinics, 30, 317–329; Tan, E., & Tan, E. (2013). Alterations in physiology and anatomy during pregnancy. Best Practice & Research Clinical Obstetrics & Gynaecology, 27, 791–802. During pregnancy, blood volume increases by 30% to 50%, or 1,100 to 1,600 mL (Ouziunian & Elkayam, 2012), and peaks at 30 to 34 weeks’ gestation. The increase in blood volume improves blood flow to the vital organs and protects against excessive blood loss during birth. Fetal growth during pregnancy and newborn weight are correlated with the degree of blood volume expansion. Of the blood volume expansion occurring during pregnancy, 75% is considered to be plasma (King et al., 2015). There is also a slight increase in red blood cell volume (RBC). The blood volume changes result in hemodilution, which leads to a state of physiologic anemia during pregnancy. As the RBC volume increases, iron demands also increase. Leukocytosis occurs in pregnancy, with white blood cell counts increasing to as much as 14,000 to 17,000 cells per mm3 of blood (Table 29-3). Clotting factors increase as well, creating a risk for clotting events during pregnancy. Systemic vascular resistance is reduced due to the effects of progesterone, prostaglandins, estrogen, and prolactin. This lowered systemic vascular resistance, in combination with inferior vena cava compression, is partly responsible for the dependent edema that occurs in pregnancy. Epulis of pregnancy, or hypertrophy of the gums accompanied by bleeding, may also occur and is due to decreased vascular resistance and increase in the growth of capillaries during pregnancy (Jarvis, 2016). Indications and contraindications for prescribing combined estrogen vs. progesterone-only birth control Progestin-only contraceptives are used continuously; there is no hormone-free interval, as occurs with combined methods. These contraceptive methods have minimal effects on coagulation factors, blood pressure, or lipid levels and are generally considered safer for women who have contraindications to estrogen, such as cardiovascular risk factors, migraine with aura, or a history of VTE. In spite of this belief, the product labeling for some progestin-only products mimics the labeling for products containing estrogen. The U.S. Medical Eligibility Criteria for Contraceptive Use (CDC, 2010; see Appendix 11-A) can be used to identify appropriate candidates for progestinonly contraception. Progestin-only contraceptives do not provide the same cycle control as methods containing estrogen, and unscheduled bleeding is common with all progestin-only methods. Typically, unscheduled bleeding occurs most frequently during the first 6 months of method use, with a substantial number of users becoming amenorrheic by 12 months of use (Hubacher, Lopez, Steiner, & Dorflinger, 2009). Overall blood loss decreases over time, making progestin-only methods protective against irondeficiency anemia. With appropriate counseling, many women see amenorrhea as a benefit of these methods. All progestin-only methods are likely to improve menstrual symptoms, including dysmenorrhea, menorrhagia, premenstrual syndrome, and anemia (Burke, 2011). The thickening of cervical mucus seen with progestin methods is protective against PID. Progestin-only contraceptives include the progestin-only pill (POP), an injection, an implant, and three progestin-containing intrauterine devices. The implant and devices are covered in the section on long-acting reversible contraception. The U.S. Medical Eligibility Criteria for Contraceptive Use (CDC, 2010) is a comprehensive, evidence-based guide for determining whether women have relative or absolute contraindications to contraceptive methods. The Medical Eligibility Criteria uses the following four classification categories of whether a person can use or should not use a method: Category 1: a condition for which there is no restriction for the use of the contraceptive method Category 2: a condition where the advantages of using the method generally outweigh the theoretical or proven risks Category 3: a condition where the theoretical or proven risks usually outweigh the advantages of using the method Category 4: a condition that represents an unacceptable health risk if the contraceptive method is used Menstrual cycle physiology The initiation of menstruation, called menarche, usually happens between the ages of 12 and 15. Menstrual cycles typically continue to age 45 to 55, when menopause occurs. Many women find themselves reluctant to discuss the existence and normality of menstruation. The word menstruation has been replaced by a variety of euphemisms, such as the curse, my period, my monthly, my friend, the red flag, or on the rag. Most women experience deviations from the average menstrual cycle during their reproductive years. As a result, it is not uncommon for women to display certain preoccupations regarding their menstrual bleeding, not only in relation to the regularity of its occurrence, but also in regard to the characteristics of the flow, such as volume, duration, and associated signs and symptoms. Unfortunately, society has encouraged the notion that a woman’s normalcy is based on her ability to bear children. This misperception has understandably forced women to worry over the most miniscule changes in their menstrual cycles. Indeed, changes in menstruation are one of the most frequent reasons why women visit their clinician. Numerous patterns in the secretion of estrogens and progesterone are possible; in fact, it is difficult to find two cycles that are exactly the same. Studies that include women of different ethnicities, occupations, genetics, nutritional status, and age have demonstrated that the length and duration of the menstrual cycle vary widely (Assadi, 2013; Johnson et al., 2013; Karapanou & Papadimitriou, 2010). Menarche is the most readily evident external event that indicates the end of one developmental stage and the beginning of a new one. It is now believed that body composition is critically important in determining the onset of puberty and menstruation in young women (Ferin & Lobo, 2012). The ratio of total body weight to lean body weight is probably the most relevant factor, and individuals who are moderately obese (i.e., 20–30% above their ideal body weight) tend to have an earlier onset of menarche (Johnson et al., 2013). Widely accepted standards for distinguishing what are regular versus irregular menses, or normal versus abnormal menses, are generally based on what is considered average and not necessarily typical for every woman. According to these standards, the normal menstrual cycle is 21 to 35 days with a menstrual flow lasting 4 to 6 days, although a flow for as few as 2 days or as many as 8 days is still considered normal (Ferin & Lobo, 2012). The amount of menstrual flow varies, with the average being 50 mL; nevertheless, this volume may be as little as 20 mL or as much as 80 mL. Generally, women are not aware that anovulatory cycles and abnormal uterine bleeding (changes in bleeding outside of normal; see Chapter 24) are common after menarche and just prior to menopause (Ferin & Lobo, 2012; Fritz & Speroff, 2011). Menstrual cycles that occur during the first 1 to 1.5 years after menarche are frequently irregular due to the immaturity of the hypothalamic–pituitary–ovarian axis (Fritz & Speroff, 2011). Vaccines during pregnancy Live vaccines are contraindicated during pregnancy (MMR, Oral Polio, Varicella & FluMist) Injectable influenza vaccine is an inactivated virus and is safe to use in pregnancy Ask if the woman has ever known anyone with tuberculosis or traveled to areas where tuberculosis is common. If she is at risk, she should receive a tuberculin skin test when she can return in 48 to 72 hours. Past history of varicella is important, as well as the woman’s vaccine history, to determine if she is at risk for chickenpox. Women can receive vaccines in pregnancy (Table 30-1). The Centers for Disease Control and Prevention (CDC) updates the adult vaccine schedule often, and this information can be easily accessed on its website. The CDC website also includes detailed information about safety of vaccines for travel of local disease outbreaks during pregnancy (CDC, 2014). All women who are pregnant should be offered the influenza vaccine during flu season, though live attenuated influenza vaccine (LAIV [FluMist]) should not be given to pregnant women. All women should be encouraged to receive a tetanus, diphtheria, and acellular pertussis (Tdap) vaccination in the third trimester (CDC, 2016). Other vaccines, such as hepatitis B, can be administered if the woman is at risk (CDC, 2016). During pregnancy, women have a decreased immune response to pathogens, making them more susceptible to infection. If a woman has cats, she should be careful to avoid contracting toxoplasmosis—an infection that is spread through cat feces. Someone else should change the cat litter box daily to prevent contact with the Toxoplasma gondii parasite. Wearing gloves while gardening, and careful hand washing are also essential. More information and patient handouts are available for free at the CDC website. TABLE 30-1 Vaccines in Pregnancy Recommended Each Preg nancy Rationale Timing Influenza (flu)a Women who are pregnant are at increased risk for flu-related complications. Any gestation when the injection is available [Show More]
Last updated: 1 year ago
Preview 1 out of 77 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2022
Number of pages
77
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2022
Downloads
0
Views
39




.png)
.png)