NSG 316 EXAM 1
Document Content and Description Below
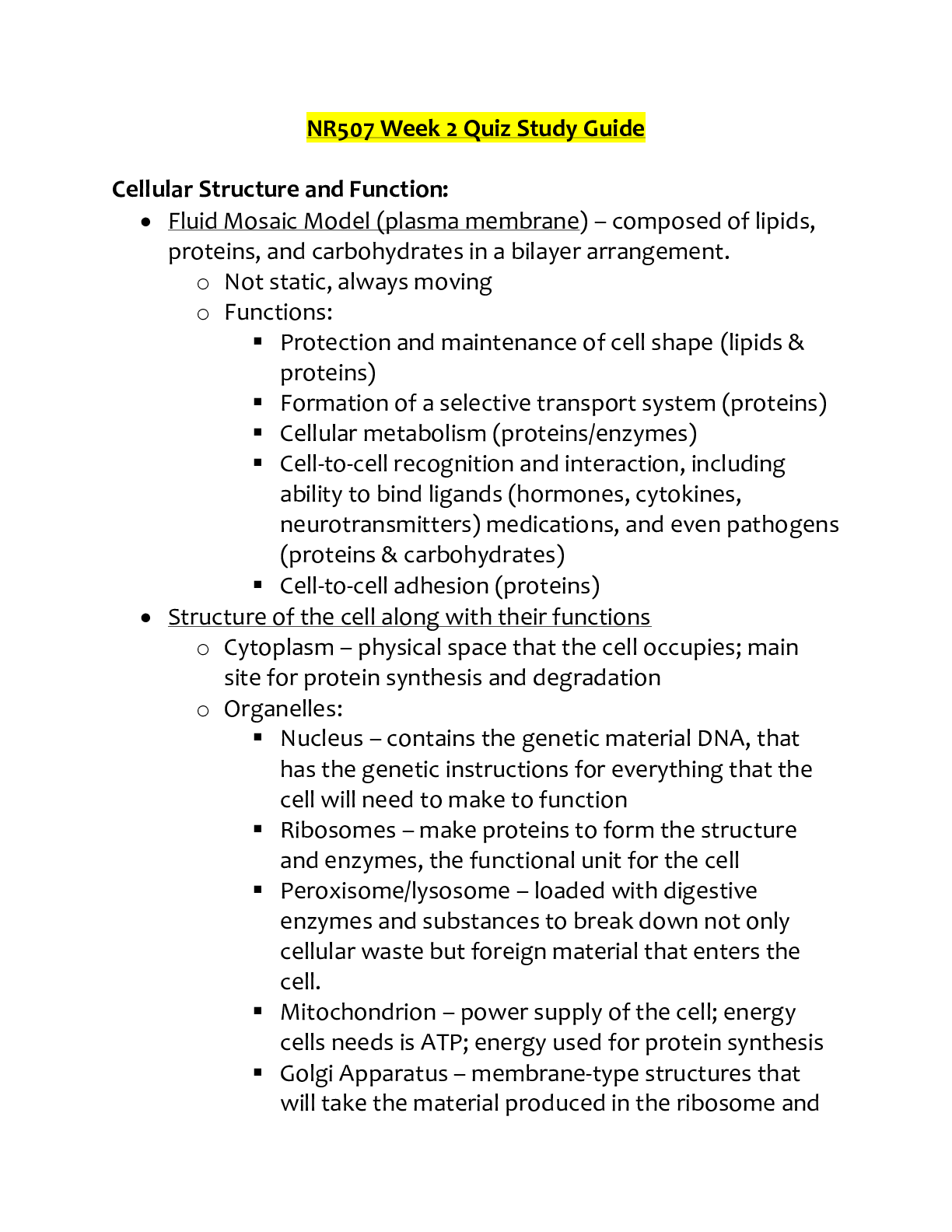
TOPIC 1: 1. Describe the elements of a general survey and health assessment. • Generalsurvey: o The generalsurvey is a study of the whole person o Covers general health state and any obvious phy... sical characteristics o An introduction for physical examination that will follow; o should give an overall impression, a “gestalt,” of person o Objective parameters are used to form generalsurvey o these apply to whole person, not just to one body system o 4 areas: physical appearance, body structure, mobility, and behavior • Health assessment: o Point of entry in an ongoing process 2. Differentiate between a comprehensive assessment and a focused assessment and when each type of assessment would be implemented. • Comprehensive assessment- (or complete/total), includes complete health history and full physical examination, describes current and past state, form baseline against all future changes can be measured, yields first diagnosis o Primary care settings (pediatric or family practice clinic, private practice, college health service, etc.), also when admission to the hospital (physician collects pathology and you collect additional info on the rest) o Well person- this describes person’s health state, perception of health,strengths or assets such as health maintenance behaviors, individual coping patterns, support systems, and current developmental tasks, any risk factors or lifestyle changes. o Ill person- also includes a description of the person’s health problems, perception of illness, and response to problems o Both-screen for pathology and determine the ways people respond to that pathology or to any health problem. • Focused assessment- (or problem centered or episodic), collect mini database, smaller in scope and more targeted than complete assessment, concerns mainly one problem, one cue complex, or one body system o Used in all settings (hospital, primary care, or long-term) 3. Differentiate between subjective and objective data gathered during the health assessment process. • Subjective data- what the person says about them self during history talking • Objective data- what we as the health professional observe by inspecting, percussing, palpating, and auscultating during the physical examination EXAM 1_316 4. Identify client safety and privacy best practices when obtaining a health history and conducting an assessment. • HIPAA- Health Insurance Portability and Accountability Act (1996) • any written, verbal, or electronic communications = medical records, accounting information, patient information, and conversations between or among healthcare professionals about patients are confidential under law and this agreement 5. List major factorsthat affect health promotion and disease prevention throughout the life span. • Interval of assessment o Ill people seek care because of pain or abnormal signs and symptoms o Well persons, Annual or yearly- opinions are changing when o Hospitalized patients require frequently repeated Head to toe, focused, and Focused reassessment in response to treatments • Routine periodic examination might include the following services for preventive health care: o Screening history for dietary intake, physical activity,tobacco/alcohol/drug use, and sexual practices o Counseling forinjury prevention,substance use,sexual behavior, diet and exercise, and dental health o Immunizations o Chemoprophylaxis for multivitamin with folic acid for females capable of or planning pregnancy TOPIC 2: 1. Examine key components of obtaining an accurate and current health history, including variations for culture, age, gender, ethnicity, religion, and spirituality. • Be culturally sensitive: basic knowledge and understanding • Culturally appropriate: apply knowledge to improve health outcomes • Culturally competent: universal concept of understanding to all aspects of care • Cultural care: provision of health care across cultural boundaries 2. Describe the components of an effective interview to elicit an accurate and realistic history. • First and most important part of data collection, collectssubjective data, individual knows everything about their health • Gather complete and accurate data about person’s health state, including description and chronology of any symptoms of illness • Establish rapport and trust so person feels accepted and free to share all relevant data • Teach person about health state so they may participate in identifying problems • Build rapport to continue therapeutic relationship and to facilitate diagnoses, planning, and treatment • Begin teaching for health promotion and disease • Contract: mutual goal is optimal health for patient • Internal factors: liking others, empathy, ability to listen EXAM 1_316 • External factors: privacy, refuse interruptions, environment, dress, tape and video • Open and close-ended questions • Assisting the narrative:silent attentiveness, reflection, empathy, clarification, confrontation, interpretation, explanation, summary • Nonverbal behaviors: vocal cues, action cues, object cues, personal space, touch • Improve health literacy 3. Determine the importance of cultural, ethnic, and spiritualsensitivity and competence when obtaining a client health history and conducting a health assessment. • Effective care: positive outcomes and satisfaction for patient • Respectful care: considers values, preferences, and expressed needs of patient • Cultural and linguistic competence: congruent behaviors, attitudes, and policiesthat come together in a system among professionals that enables work in cross-cultural situations • Pain: expectations, manifestations, and management of pain are embedded in a cultural context, silent suffering is most valued identified by HCPs 4. Apply principles or conceptsfor therapeutic communication. 5. Identify the components of a functional assessment. • Assessment questions: Functional ability? ADLs affected? o ADLs- activities of daily living (eating, bathing, grooming, toileting) o IADLs- instrumental activities of daily living/necessary for independent living (shopping, meal prep, housekeeping, laundry, finances) o AADLs- advanced activities of daily living/member ofsociety/family member activities (work, mobility, self-care, activities/hobbies, socialization) • Reason forseeking care: older minimize symptoms, may have chronic problems and just have been living with it • Past health history: general health in past 5 years • Medication reconciliation: list of all current meds, consider polypharmacy • Alcohol C.A.G.E. test- cut down drinking (told by someone)? Annoyed by criticism? Guilty about drinking? Eye opener (drink in the morning) • Cognition assessment: attention, memory, orientation, language o Dementia-slow onset, difficulty word finding, naming objects, memory o Delirium- acute changes in cognition and attention • Caregiver assessment- caregiver burden NOTES: -religion: belief in divine powers to be obeyed and worshiped as creator/ruler of universe -spirituality: system of beliefs, practices, and ethical values EXAM 1_316 - Complete health history: past and present health, well person: lifestyle, diet, exercise; ill person: info about health problem - Biographical data: name, age, DOB,sex, maritalstatus, race, ethnicity, address, phone # - Source of history: judge the source of the info for its accuracy - Reason forseeking care:signs(detected) and symptoms(feeling), person’s own words - Present or history: location, character or quality, timing,setting, factors - PQRSTU for pain symptoms: o P/P= provocative or palliative o Q/Q= quality or quantity o R/R= region or radiation o S= severity scale: 1 to 10 o T= timing or onset o U= understand patient’s perception of problem - Past medical history: childhood illnesses, accidents or injuries, meds, allergies - Family History: family history of various conditions - Review ofsystems: each body system has present/past state of health, double check important data, eval health promotion, rough head to toe - Functional assessment: ADLs, IADLs, AADLs TOPIC 3: 1. Differentiate among the assessment techniques of inspection, palpation, percussion, and auscultation. • Inspection: concentrated watching, close carefulscrutiny, first as a whole individual then each body system • Palpation: applies yoursense of touch to assessthese factors: texture, temp, moisture, organ location, and size, swelling, vibration/pulsation, rigidity/spasticity, crepitation, lumps or masses, tenderness or pain • Percussion: tapping the person’s skin with short,sharp strokesto assess underlying structures, sound depicts the location, size and density of the underlying organ • Auscultation: listening to sounds produced by the body (heart, lungs, vessels, abdomen) 2. Differentiate among the types, causes, and characteristics of pain. • Nociceptive pain: functioning and intact nerve fibers in periphery and CNS are stimulated. From actual or potential tissue damage, transduction, transmission, perception, and modulation. • Neuropathic pain: pain caused by a lesion or disease of the somatosensory nervous system. Constant irritation = increased sensitivity • Acute pain: short term and self-limiting, often follows a predictable trajectory, and dissipates after an injury heals. (surgery, trauma, kidney stones). Warnsthe individual of actual or threatened tissue damage. • Chronic (persistent) pain: diagnosed when the pain continues for 6 months or longer. Divided into malignant (cancer-related, created by pathology of tumor cells, necrosis & stretching) of an organ and nonmalignant (not cancer related). EXAM 1_316 3. Describe techniques used to assess a client's pain. • Pain is what the patient says it is, and cannot rely on physical exam to “see” it • PQRST, numeric rating scales, verbal descriptorscales, visual analog scales, • Establishing a diagnosis is first priority • Behavioral cues (acute will change vitals, chronic will have bracing, rubbing, sighing) • Different in dementia 4. Identify changes that occur when a client's pain is poorly controlled. • Can change into Neuropathic pain: pain caused disease of the somatosensory nervous system. Constant irritation = increased sensitivity 5. Explain best practices for documenting client health history and health assessment data. NOTES: -Visceral pain: larger interior organs -Deep somatic pain: blood vessels, joints, tendons, muscles, and bone injury -Cutaneous pain:skin surface and subcutaneous tissue -Referred pain: felt at a particular site but originates from another location TOPIC 4: 1. Describe techniques used to assess a client's skin, hair, and nails. • Skin: color: general pigmentation, freckles, moles, birthmarks; widespread color change; temperature: use backs of hands to palpate person, normal-warm, and temperature equal bilaterally; warmth suggests normal circulatory status, hands and feet may be slightly cooler in a cool environment; moisture (diaphoresis & dehydration), texture, thickness, edema, mobility and turgor, vascularity or bruising, edema (1+ mild, slight indentation, no perceptible swelling; 2+ moderate, indentation subsides rapidly; 3+ deep, indentation remains for short time, appears swollen; 4+ very deep, indentation lasts long time, appears very swollen) • Hair: color, texture, distribution, lesions • Nails:shape and contour-smooth, uniform-curved or flat, view index finger at its profile and note angle of nail base; it should be about 160 degrees, consistency, color, capillary refill (depress nail edge to blanch and then release, noting return of color; indicates status of peripheral circulation, color return is normally instant, sluggish color return takes longer than 1 or 2 seconds) 2. Identify appropriate skin, hair, and nail assessment techniquesfor clients based on age, development, and other psychosocial or environmental variables. • Aging o Senile lentigines- age spots,sun spots o Keratoses- crusty patch EXAM 1_316 o Xerosis- dry skin o Skin tags or acrohordons o Thin parchment-skin tears o Decreased hair growth o Decreased nail growth and brittle nails 3. Differentiate between normal and abnormal findings of the skin, hair, and nailsthat require further evaluation. • Skin: ABCDE rule to detect suspicious lesions o A: asymmetry o B: border o C: color o D: diameter o E: elevation and enlargement • Nails: clubbing, • Hair: 4. Document health history and key components of a skin, hair, and nail assessment in the client record. • Annular (or circular) • Confluent (flow together, annular but together) • Discrete (separated, pus filled things?) • Grouped (together, vesiclestogether) • Gyrate (spiral, worm, S shaped) • Target or iris (has two parts, inner and outer) • Linear (line,straight) • Polycyclic (annular lesions, that grow together) Primary skin lesions EXAM 1_316 • Zosteriform (starts linear but then curves along nerve route) • Macule- freckle, flat, circumscribed, less than 1 cm • Papule- worts and moles, elevated,solid, circumscribed, less than 1 cm • Nodule-solid, elevated, hard orsoft, greater than 1 cm • Wheal- hives, mosquito bite, elevated,superficial, erythema, urticaria • Vesicle/bulla- vesicle = smaller than 1 cm, bulla = larger than 1 cm, both = elevated and contain fluid, chicken pox, burn, blister • Cyst- encapsulated, fluid filled cavity in dermis orsubcutaneous, tensely raisesskin, deeper and more elevated • Pustule- filled w/pus, circumscribed, elevated, acne, impetigo (rash) Secondary skin lesions (follows primary but after scratching/messing with it) • Crust- impetigo, crust on top of original lesion • Scale- eczema, psoriasis, dry,scaly, elevated • Fissure- crack into dermis, athlete’sfoot • Erosion-scooped butshallow depression, top layer • Ulcer- deep depression into dermis, irregular shape, may bleed • Excoriation-scratching,self-inflicted,superficial • Scars- healed area that was replaced w/collagen instead of normal tissue • Atrophic scar-stretch marks, loss of dermis and is depression w/loss of tissue, thin epidermis • Lichenification- tightly packed set of papules, caused by itching • Keloid- excessscartissue, more in black/Hispanic/Asian and younger people Vascular lesions • Petechiae- light red spots, smaller • Purpura- larger red spots, clumped together • Bruiseso Red-blue or purple (immediately after or first 24 hours) o Blue to purple o Blue to green o Yellow o Brown to disappearing Pressure Ulcers • Stage I-intactskin, red, unbroken, localized redness, lighterskin-does not blanch, darker skin remains darker-does not blanch • Stage II-Partial thickness erosion, loss of epidermis,shallow abrasion or open blister looking, red-pink wound bed • Stage III-full thickness extending into SQ, crater like, fat may be visible • Stage IV-full thickness, all layersto supporting structures, muscle, tendon, bone,slough and eschar [Show More]
Last updated: 1 year ago
Preview 1 out of 7 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 14, 2022
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
May 14, 2022
Downloads
0
Views
55