*NURSING > STUDY GUIDE > Chamberlain College: NR 566 wk 1 Completed Study Guide LATEST UPDATED,100% CORRECT (All)
Chamberlain College: NR 566 wk 1 Completed Study Guide LATEST UPDATED,100% CORRECT
Document Content and Description Below
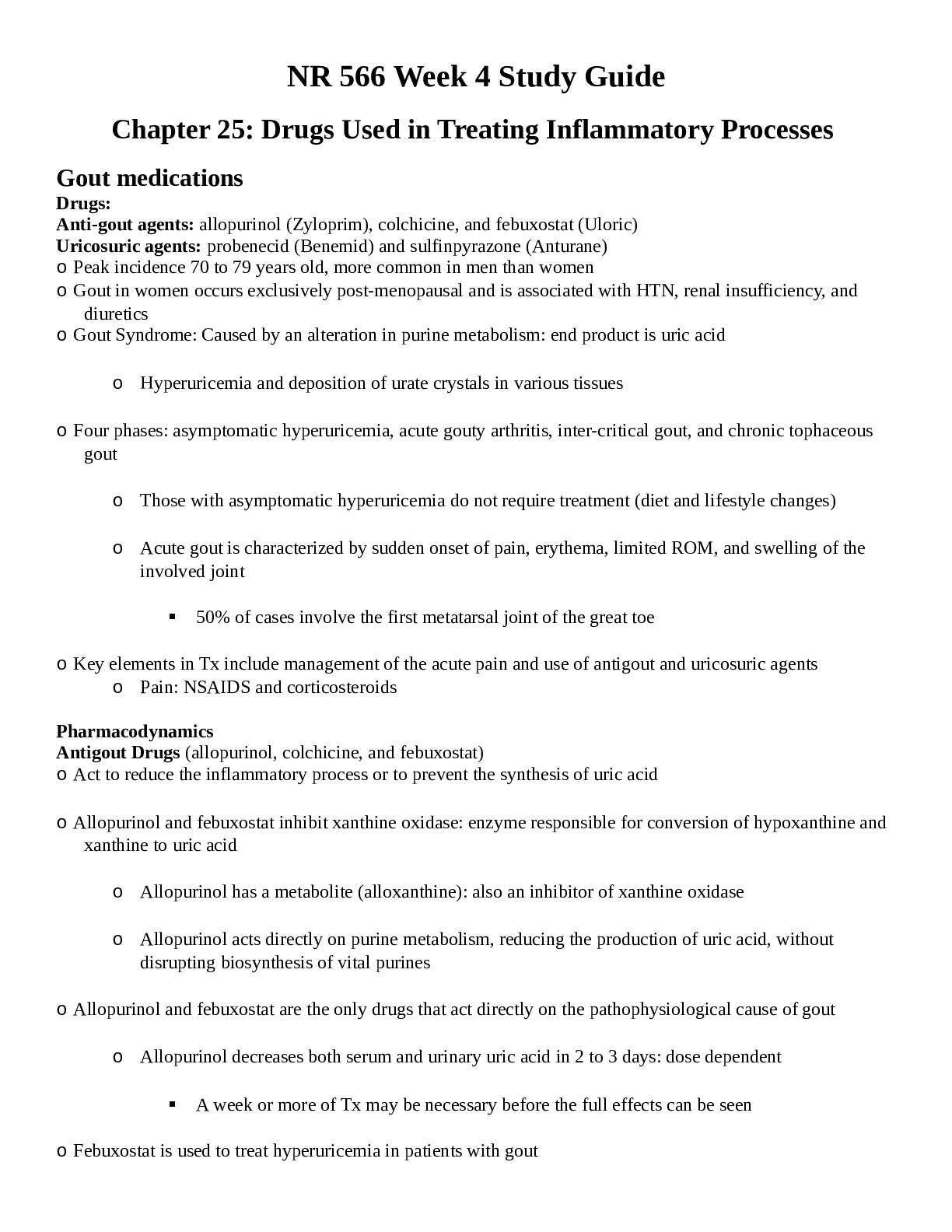
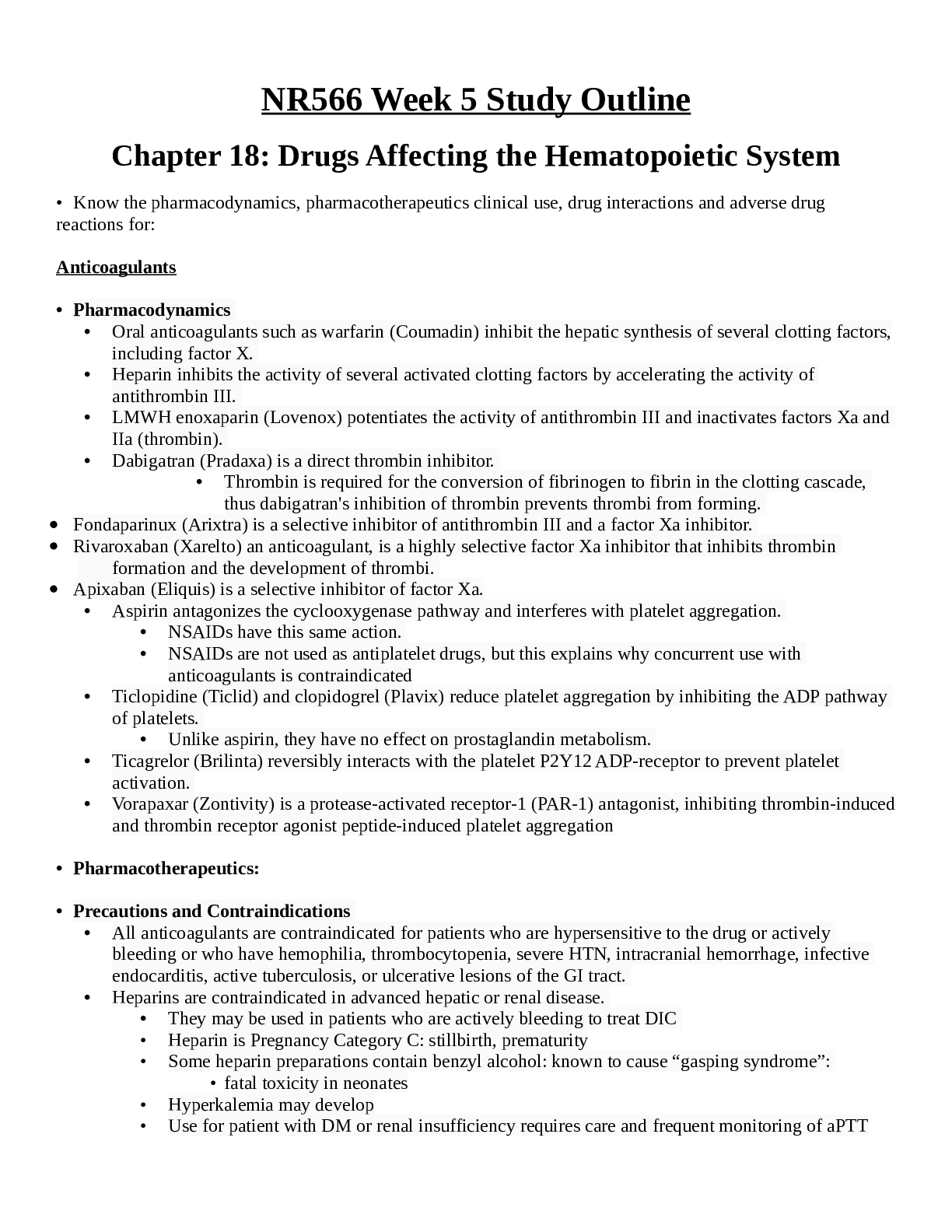
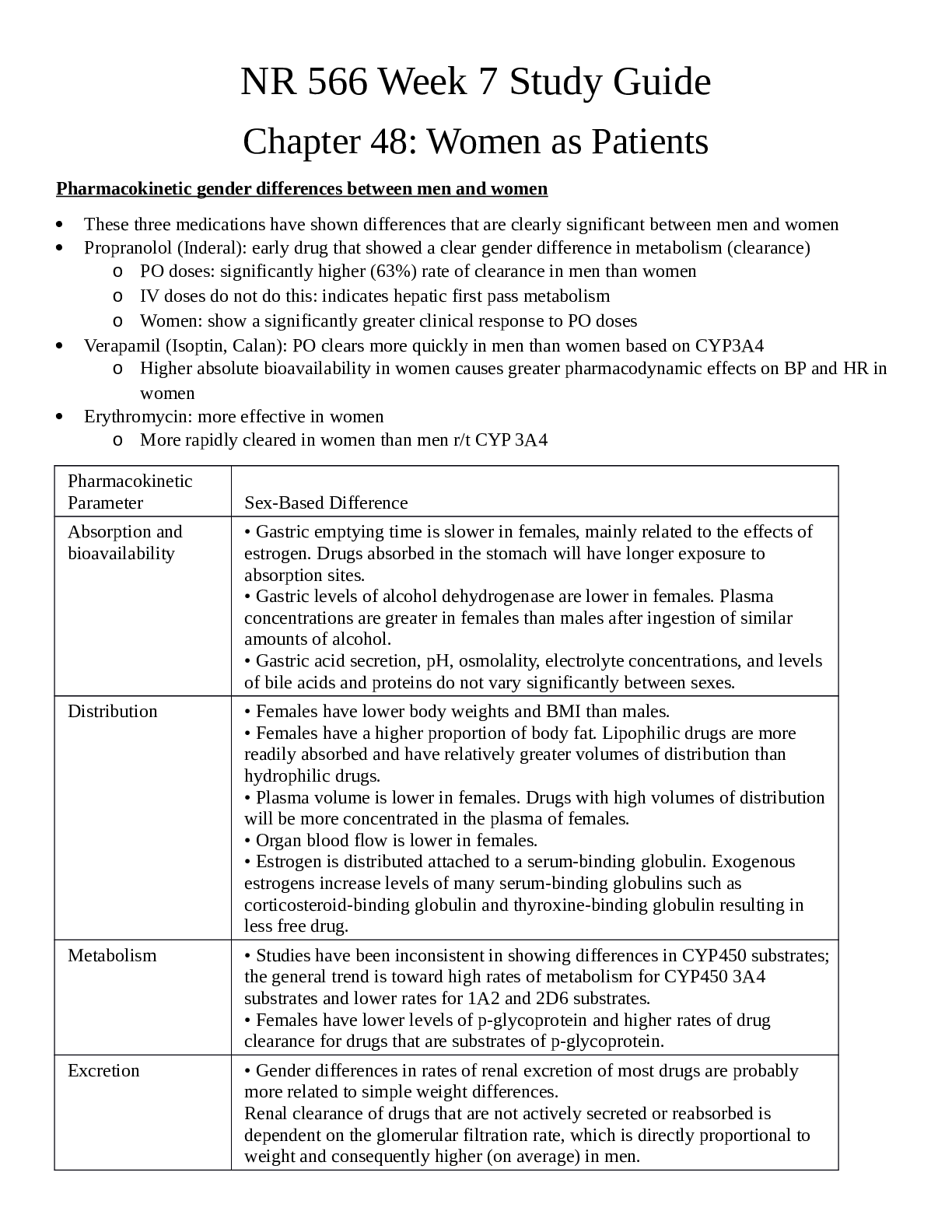
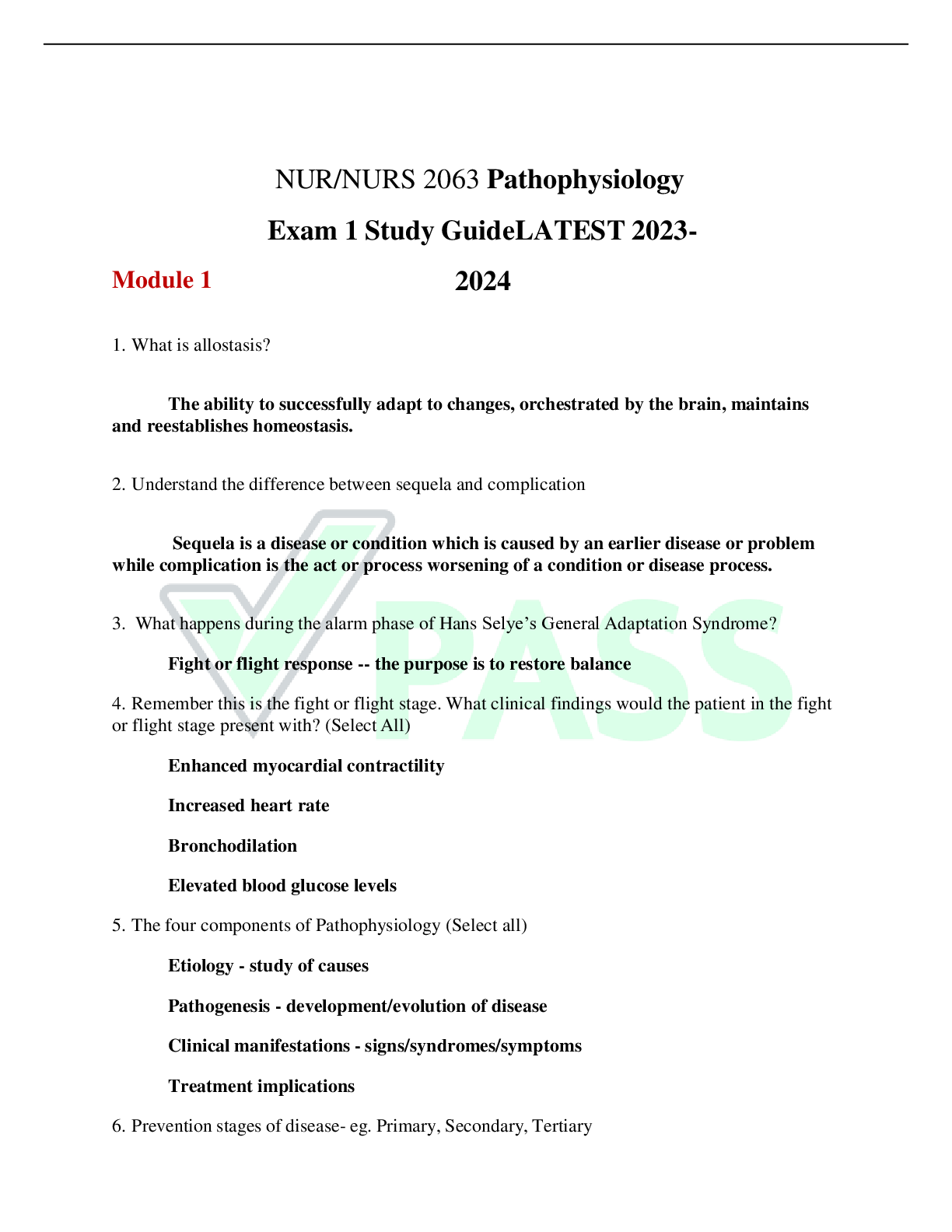
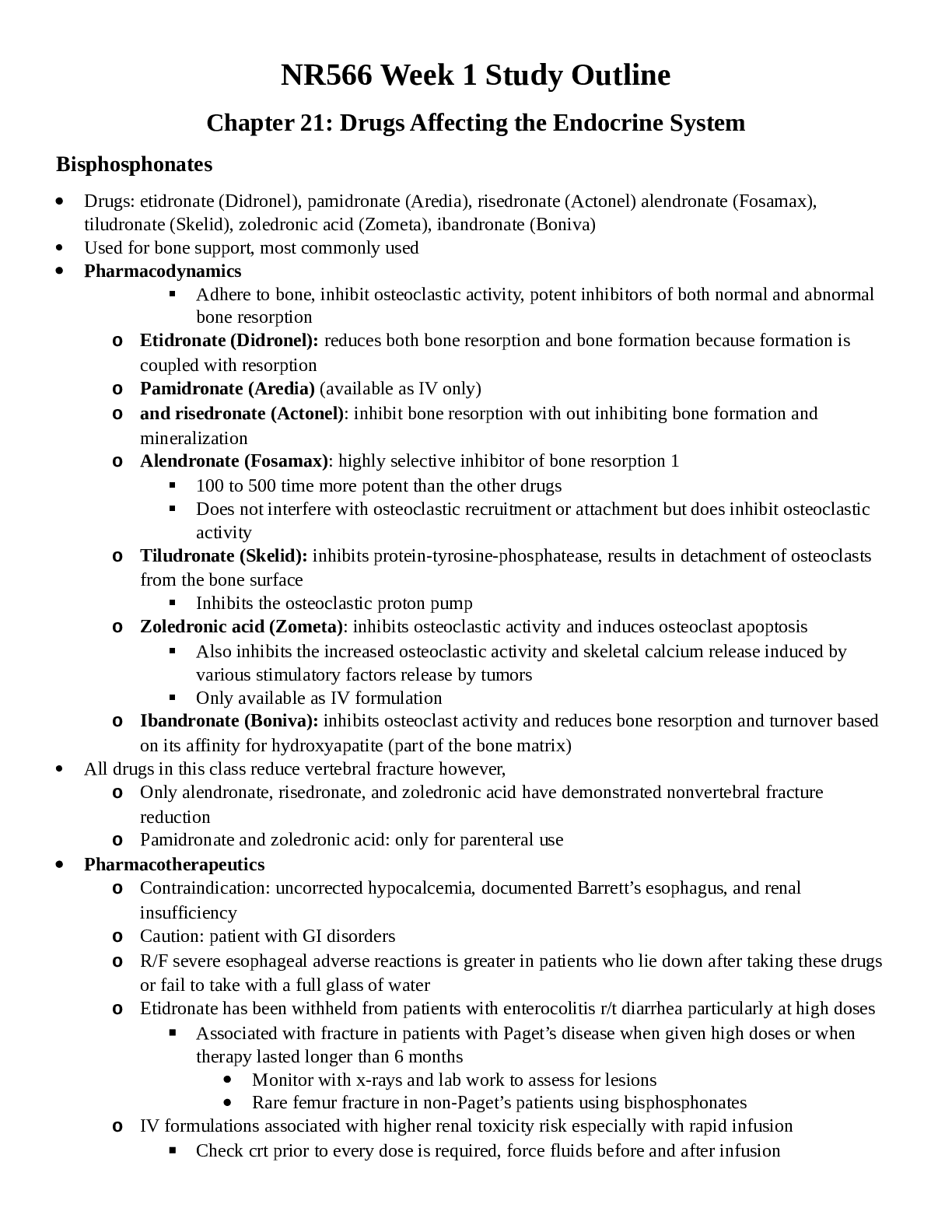
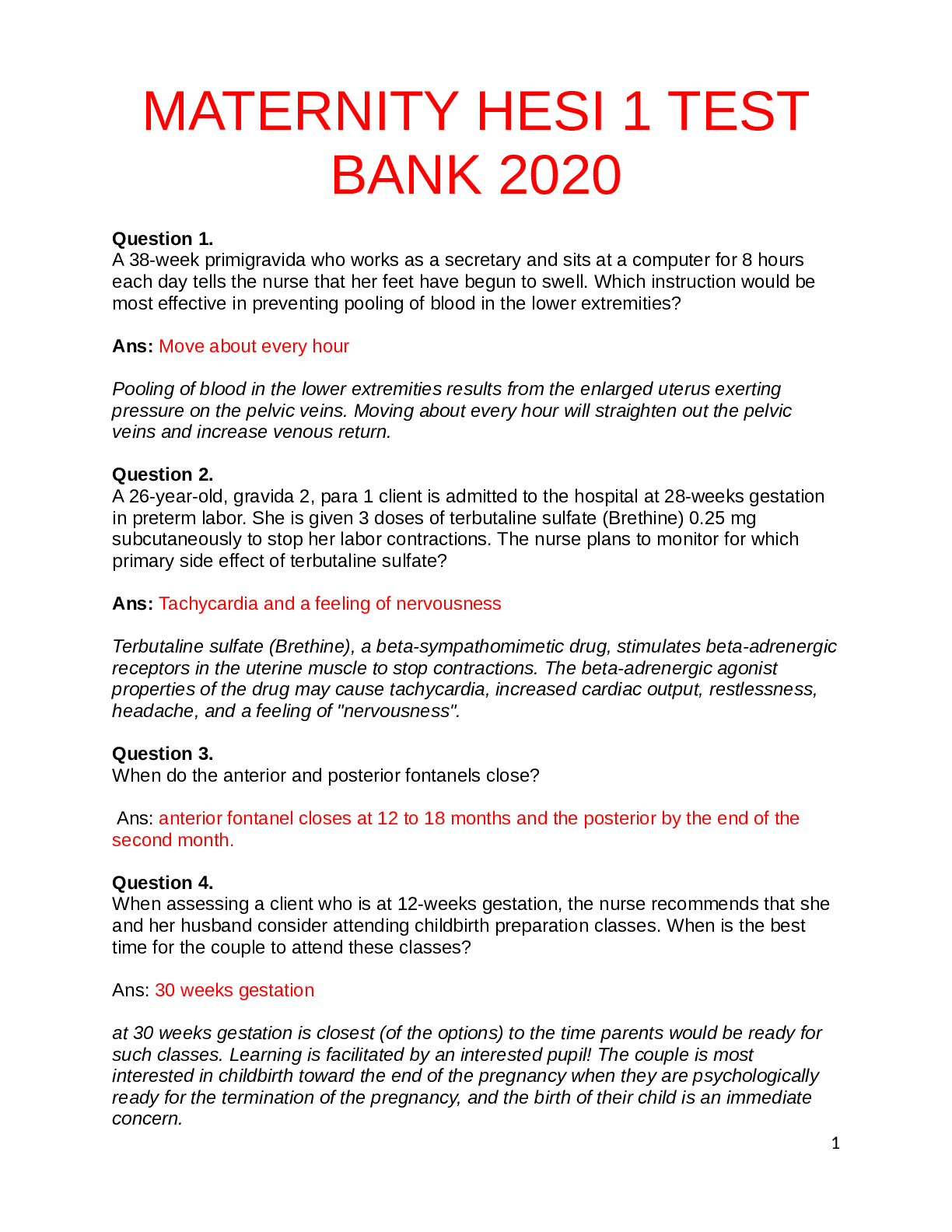
Chamberlain College: NR 566 wk 1 Completed Study Guide LATEST UPDATED Chapter 21: Drugs Affecting the Endocrine System Bisphosphonates • Drugs: etidronate (Didronel), pamidronate (Aredia), rise... dronate (Actonel) alendronate (Fosamax), tiludronate (Skelid), zoledronic acid (Zometa), ibandronate (Boniva) • Used for bone support, most commonly used • Pharmacodynamics ▪ Adhere to bone, inhibit osteoclastic activity, potent inhibitors of both normal and abnormal bone resorption o Etidronate (Didronel): reduces both bone resorption and bone formation because formation is coupled with resorption o Pamidronate (Aredia) (available as IV only) o and risedronate (Actonel): inhibit bone resorption with out inhibiting bone formation and mineralization o Alendronate (Fosamax): highly selective inhibitor of bone resorption 1 ▪ 100 to 500 time more potent than the other drugs ▪ Does not interfere with osteoclastic recruitment or attachment but does inhibit osteoclastic activity o Tiludronate (Skelid): inhibits protein-tyrosine-phosphatease, results in detachment of osteoclasts from the bone surface ▪ Inhibits the osteoclastic proton pump o Zoledronic acid (Zometa): inhibits osteoclastic activity and induces osteoclast apoptosis ▪ Also inhibits the increased osteoclastic activity and skeletal calcium release induced by various stimulatory factors release by tumors ▪ Only available as IV formulation o Ibandronate (Boniva): inhibits osteoclast activity and reduces bone resorption and turnover based on its affinity for hydroxyapatite (part of the bone matrix) • All drugs in this class reduce vertebral fracture however, o Only alendronate, risedronate, and zoledronic acid have demonstrated nonvertebral fracture reduction o Pamidronate and zoledronic acid: only for parenteral use • Pharmacotherapeutics o Contraindication: uncorrected hypocalcemia, documented Barrett’s esophagus, and renal insufficiency o Caution: patient with GI disorders o R/F severe esophageal adverse reactions is greater in patients who lie down after taking these drugs or fail to take with a full glass of water o Etidronate has been withheld from patients with enterocolitis r/t diarrhea particularly at high doses ▪ Associated with fracture in patients with Paget’s disease when given high doses or when therapy lasted longer than 6 months • Monitor with x-rays and lab work to assess for lesions • Rare femur fracture in non-Paget’s patients using bisphosphonates o IV formulations associated with higher renal toxicity risk especially with rapid infusion ▪ Check crt prior to every dose is required, force fluids before and after infusion • Clinical Use (Page 546 Dosing Chart) o Osteoporosis ▪ Prevention and treatment of osteoporosis and its risk for fracture in men and postmenopausal women (especially vertebral fractures) ▪ First line drugs: Alendronate, risedronate, and zolendronic acid with hip fracture reductions, FDA approved for this indication ▪ Second-line drug: Ibandronate ▪ Ibandronate and zoledronic acid come in IV form ▪ Alendronate PO solution (Binosto) and PO tablets ▪ Zoledronic acid: only alternative form that shows evidence of hip fracture reduction ▪ Prophylactic use in patients with early osteopenia r/t long term use of medications that contribute to bone loss • Includes (thyroid hormone, aromatase inhibitors, and glucocorticoids, PPIs, SSRIs) ▪ It is recommended that all adults taking more than 7.5 mg of prednisone or its equivalent for more than 3 weeks be given alendronate or risedrone ▪ In very high risk patients, maximum 2-year use of teriparatide (Forteo) (bone mass benefit disappears after d/c) a parathyroid hormone, may be more efficacious • Bisphosphonates: bone mass benefit does not decline for 5 years ▪ Alendronate and risedronate initial doses for prevention of bone loss: 5mg/day or 35mg/week ▪ For existing osteoporosis: alendronate 10mg/day or 70mg/week ▪ Risedronate: 75mg for 2 days or 150mg once a month o Paget’s Disease (Osteitis Deformans) ▪ All bisphosphonates are used to treat Paget’s disease when the alkaline phosphatase is at least twice the upper limit of normal ▪ Asymptomatic or at risk for future complications from their disease ▪ Symptomatic Paget’s best treated with etidronate ▪ Etidronate slows accelerated bone turnover in pagetic lesions and to a lesser extend in normal bone ▪ Reduced turnover causes symptomatic improvement: less bone pain and decreased fractures ▪ 5-10 mg/kg daily for up to 6 months or 11 to 20 mg/kg daily for 3 months ▪ For all drugs indications for retreatment are evidence of active disease or failure to normalize alkaline phosphatase levels ▪ Supplemental calcium and vitamin D if dietary intake is not adequate ▪ Space calcium supplements and bisphosphonates to prevent reduced bioavailability o Heterotopic Ossification ▪ Complications of THR ▪ Etidronate: first line ▪ Heterotopic ossification r/t spinal cord injury ▪ Use as soon as possible after injury • Drug Interactions o Adverse GI reactions, interact with drugs that affect the GI tract ▪ Histamine 2 blocking agents double alendronate bioavailability but the impact with unknow o Calcium supplements and antacids interfere with bisphosphonate absorption when taken within 1 hr o R/F GI bleeding is increased when ASA and NSAIDs are concomitantly taken o ASA may decrease the bioavailability of tiludronate by up to 50% when taken 2 hrs after the tiludronate o Indomethacin increases the bioavailability of tiludronate by 2- to 4- fold ▪ Diclofenac does not significantly alter bioavailability therefore each NSAID must be evaluated individually o Concurrent use of bisphosphonates and other drugs known to build bone density (estrogens and SERMs) have additive bone density however fracture reduction potential is unknown • ADRs o All bisphosphonates: musculoskeletal pain ▪ More common in Paget’s disease ▪ More common in those taking risedronate ▪ High doses of etidronate ▪ Rare reports of osteonecrosis of the jaw in active dental disease, invasive procedure, especially in CA patients • Can occur without dental issues in those receiving frequent high IV doses ▪ R/F A-fib • Bioavailability of bisphosphonate drugs and appropriate patient education o Absorption and bioavailability of oral doses are significantly reduced by the presence of food in the gut or other preparations containing divalent cations o To enhance absorption take with 8 oz of water, no other food or drink and remain upright for at least half an hr (1 hour with ibandronate) o Histamine 2 blocking agents double alendronate bioavailability but the impact with unknow o ASA may decrease the bioavailability of tiludronate by up to 50% when taken 2 hrs after the tiludronate o Indomethacin increases the bioavailability of tiludronate by 2- to 4- fold ▪ Diclofenac does not significantly alter bioavailability therefore each NSAID must be evaluated individually o Patient education: Take oral drugs first thing in the morning at least 30 minutes prior to other medications, beverages, or food (60 minutes for ibandronate) o Etidronate and tiludronate take 2 hours before food o Alendronate, ibandronate, risedronate, and tiludronate should be taken with 8 oz of plain water o Mineral water, coffee, OJ, and other drinks greatly reduce absorption o Supplemental calcium or antacids take the bisphosphonate at least 1 hr before these drugs o Skip missed daily doses and resume the next morning o Sit up for at least 30 mins after taking to decrease risk of esophageal irritation (1hr for ibandronate) • Adverse effects associated with long-term use o Etidronate: Fractures in patients with Paget’s disease when given high doses or when therapy lasted longer than 6 months o Oral drugs in this class: rare osteonecrosis of the jaw after 3 years of use (higher risk in IV drugs) Growth hormones • Drugs: somatropin (Nutropin and Nutropin AQ, Gentropin, Humatrope, Norditropin, Nutropin, Accretropi9n, Saizen, Serostim) and somatrem (Protropin) • Dosage of the various forms of somatropin varies by manufacturer • Pharmacodynamics o GHRH secreted by hypothalamus in response to decreased serum glucose o GHRH then binds to receptors in the anterior pituitary, secrets GH (somatotropin) o Passes through cell membrane, fosters proteins synthesis, fat breakdown, and tissue growth o Causes hyperglycemia by decreasing glucose utilization by cells and increases rate by which glycogen is broken down into glucose o Both GHRH and GH have been synthesized by recombinant DNA technology ▪ Synthetic hormones o Administration results in an insulin like effect o Increased growth of organs and skeletal, increased cellular protein synthesis o Children with GH deficiency sometimes experience hypoglycemia and it is improved by admin of these drugs o Reduction in fat store, increased lean muscle mass, and decreased mean cholesterol o Treats lipodystrophy in HIV patients – helps to reduce wasting and cachexia o In over abundance of GH, surgical intervention is primary intervention however recurrence may require use of somatostatin analogues such as octreotide or lancreotide ▪ GH suppressive agents • Pharmacotherapeutics o Contraindication: patients with closed epiphyses and those with evidence of active tumore growth o Caution: o intracranial tumors increased r/f tumor growth o Patients with coexisting adrenocorticotropic hormone deficiency may experience increased symptoms o Increased serum levels of inorganic phosphorus, alkaline phosphatase, and parathyroid hormone o TH level changes have occurred ▪ Makes managing thyroid disorders more difficult ▪ Untreated hypothyroidism prevents optimal response to GH therapy o May induce insulin resistance o Use cautiously with diabetic patients, those with glucose intolerance, or risk for metabolic syndrome ▪ Lipid benefits may negate this risk o Safety and efficacy of synthetic GH not established in pregnancy or lactation, Category C, only if clearly needed • Clinical Use (Dosing Schedule: Pg 551) o Growth Failure Associated with Chronic Renal Insufficiency ▪ GH is used to treat children with growth failure up to the time of renal transplantation • Dosages are higher than normal r/t hormone resistance ▪ After transplantation use is restricted to children 2 standard deviations below the mean for their gender without epiphyseal closure ▪ GH increased the side effects of cyclosporine, so typically evaluated 1 year after transplant for continued use ▪ To optimize therapy for those receiving hemodialysis, injections are given at night prior to going to sleep or at least 3 to 4 hrs after dialysis to prevent hematoma formation caused by the heparin ▪ For those with peritoneal dialysis: take injection in the morning after dialysis is completed ▪ Ambulatory peritoneal dialysis: injection in the evening at the time of the overnight exchange o Long-term Treatment of Growth Failure in Children who lack adequate Endogenous GH ▪ Somatrem and all forms of somatropin (except Serostim) used for this indication ▪ Titrated to individual patient response ▪ Younger children respond better than prepubertal adolescents ▪ High doses increase risk for excess human GH o Turner’s Syndrome ▪ Somatropin is approved for long-term treatment of short stature associated with TS ▪ Specific dosing schedule is individualized ▪ Relative hormone resistance is common (higher doses to obtain growth) o Somatropin Deficiency ▪ Patients must meet strict criteria to receive GH, prescribed by endocrinology team • Drug Interactions o Glucocorticoid therapy and estrogens may inhibit the growth-promoting effect of GH o Anticonvulsants may have more severe side effects o Insulin may lose its effectiveness • ADRs o 30-40 % of patients on somatrem and 2-4.7% of patients on somatropin develop persistent antibodies, making them less likely to response to the drug o Other adverse reactions are rare and include pain at the injection site, hyperglycemia, hypothyroidism, and edema secondary to retained sodium o Rare instances of death • Monitoring o Prior to initiating and throughout therapy, hepatic and renal function studies are done o Patient with thyroid dysfunction, DM, or glucose intolerance have their disease processes more carefully monitoring o A target heigh goal is set at the 75th percentileor a calculated genetic target height calculated from the parents o X-rays to monitor bone growth and watch epiphyseal plate o Risk for abuse or misuse: illegal athletic performance enhancement and non-FDA-approved antiaging properties • Patient Education o Usually injected at home by a family member or self-administration o Educate patient and person who will administer the drug o Proper use and disposal of needles and syringes o Consistent dosing yields consistent results however stopping the drug does not induce any major adverse issues o Differences in dosing between brand name drugs Pancreatic enzymes • Drugs: pancrelipase (Creon delayed release caps, Pancreaze Delayed Release Caps, Pertzye delayed release caps, ultressa delayed release caps, Viokase, ZEN-pep Delayed release capsules) o Only 6 FDA approved drugs, can be expensive • The various brands are not bioequivalent o Each drug varies in the number of units of lipase, protease, and amylase o If new drug started monitor the effect of the new drug on endpoints o Treatment failure has been reported in CF when grand name products were replaced by generics or switched to another drug • Exocrine function of the pancreas: section of enzymes into the gut for digestion • Two major disorders: o cystic fibrosis (malabsorption of protein, fat, and carbs) results in failure to thrive and growth impairment and o pancreatitis (acute and chronic characterized by inflammation that results in swelling and obstruction of the pancreatic ducts leads to activated enzymes digesting the pancreas malabsorption) • Some bariatric procedures may induce the need for enzymatic supplementation • Pancreatic CA and short bowel syndrome patients may also benefit • Caution: pancreatic endocrine insufficiency can coexist with pancreatic exocrine issues • Pharmacodynamics o Pancrelipase contains principally lipase with some amylase and protease o Hydrolyzes fats to glycerol and fatty acids, proteins into peptides and amino acids, and converts starch into dextrin and sugars • Pharmacotherapeutics o Caution: The enzymes increase uric acid levels, issue for those with gout or renal impairment o Do not use during acute exacerbation of acute pancreatitis o Fetal harm not known in pregnant women, Pregnancy Category C • Clinical Use (Dosage Schedule Pg. 554) o Enzyme Replacement in Patients with Deficient Exocrine Pancreatic Secretions, CF, Chronic Pancreatitis, Pancreatic Insufficiency and Steatorrhea of Malabsorption Syndromes, and Post- Gastrectomy ▪ Dosing and schedule for CF is the same for each of the FDA-approved enzymes ▪ Adult dosing for pancreatic insufficiency is individualized and based on stool output and consistency ▪ Prescribed in units of lipase ▪ Infants under 1 initiate therapy with 3,000 units of lipase per bottle or brast feed ▪ Capsules must be opened and sprinkled directly into the infants mouth or on applesauce ▪ Cannot be dissolved ▪ Chi9ldren 1-4 years old initiate therapy with 4,000 to 8,000 units of lipase sprinkled on acidic foods o Post-Pancreatectomy and Ductal Obstructions Caused by CA of the Pancreas or Common Bile Duct ▪ The dosing schedule for these indications starts with low values and can be taken at 2 hr intervals ▪ In severe deficiencies, dose may be increased to a large number of units with meals ▪ Frequency of administration may be increased to hourly intervals unless nausea, cramps, or diarrhea occurs • Drug Interactions o Calcium and magnesium based antacids will decrease the effectiveness of the enzymes o The ability of oral iron to increase serum iron levels may be reduced o Alkaline foods destroy the coating of EC products, destruction of the enzymes by gastric acids • ADRs o High doses associated with GI symptoms: nausea, cramping ABD pain, diarrhea, and colonic strictures ▪ Viokase must be administered with a PPI to protect the gastric lining o Irritation of the skin and mucous membranes occurs less commonly o Local irritation from powder inside capsules ▪ Inhalation can cause an asthma attack • Specifics about administration and education regarding pancreatic enzymes o Doses are taken immediately before or with meals or snacks with a fatty component o Fruit, hard candy, fruit juice like drinks, tea or coffee or popsicles do not require enzymes o Capsules may be opened and sprinkled on food o Capsules with EC beads should not be chewed ▪ Sprinkle on soft acidic food that is not hot and that can be swallowed without chewing (applesauce or gelatin) o Swallow immediately (proteolytic enzymes may irritate the mucosa) o Follow with a glass of water or juice or eating immediately after taking the drug helps to ensure that the medication is swallowed and does not remain in contact with the mouth and esophagus for long periods o Pancrelipase is destroyed by acid, PPI, sodium bicarbonate, or aluminum based antacids may be used with preparations without EC to neutralize gastric pH ▪ Calcium and magnesium based antacids should not be used for this purposed (interfere with MOA) o EC formulations should not be mixed with alkaline food (destroys the enteric coating) o Adverse reactions are usually GI ▪ Use lowest effective dose to minimize nausea, stomach cramps, ABD pain, or diarrhea o Dosages or brands may need to be changed if symptoms persist o Wash off powder in contact with the skin o Powder may irritate the nasal mucosa and respiratory tract ▪ Super-sensitive patients may need to use a mark during preparation o Pancreatic enzyme replacement is only part of the treatment regimen o Adherence to the rest of the treatment regimen is required o Dietary recommendations are dependent upon the reason the replacement is needed o Typically, high calorie, high protein, and low fat o For children with CF: high calorie, high protein, and high fat o Dosage of the enzyme is based on fat content of the diet, consistent amounts of fat in each meal o Small frequent meals especially in CF, post op gastrectomy, or bariatric procedure o Use the same brand consistently Insulin • A small protein secreted by the beta cells of the pancreas • Essential to the utilization of glucose by all body cells • Disorders of insulin secretion and utilization are found in DM, and the primary use of insulin as a drug is the treatment for this disorder • Type 1 DM is exclusively treated with exogenous insulin • Untreated leads to DKA, weight loss, muscle wasting, and death may occur • Pharmacodynamics • Naturally insulin is released at a constant low basal rate with intermittent bursts in response to a variety of stimuli o Stress, vagal activity, and high blood glucose levels • Binds to receptors on the cell membrane, changes occur within the cell in response, glucose transporters move to cell surface, the transporter facilitates the intake of glucose by the cell • Insulin promotes the storage of fat as well as glucose and influences cell growth and metabolic functions o Action on Glucose Transporters ▪ GLUT 1 insulin transporter is found in all tissue • Associated with basal uptake of glucose and transport of glucose across the BBB ▪ GLUT 2 transporter is found in beta cells of the pancreas, liver, kidney, and get • Regulates insulin release and glucose homeostasis • Defects in this receptor are thought to contribute to the reduced insulin secretion seen in type 2 DM ▪ GLUT 3 transporter is located in the brain, kidney, and placenta • Related to uptake of glucose in neurons and some other tissues ▪ GLUT 4 transporter is located in muscle and adipose tissue • Most associated with lowering blood glucose levels and is the primary influence in glucose uptake especially during exercise • Most associated with insulin resistance in type 2 DM ▪ GLUT 5 transporter are found in the gut and kidney • Associated with intestinal absorption of fructose ▪ The total number of receptors can be suppressed by factors such as obesity and long-standing hyperglycemia • This may explain why weight reduction can be a significant factor in DM management o Action on the Liver ▪ Increases storage of glucose as glycogen and resets the liver after food intake by reversing the amount of catabolic activity ▪ Decreases urea production, protein catabolism, and cAMP in the liver ▪ Promotes triglyceride synthesis ▪ Increases K and phosphate uptake by the liver o Action on Muscle Cells ▪ Promotes protein synthesis by increasing amino acid transport and stimulating ribosomal activity ▪ Promotes glycogen synthesis to replace glycogen stores used during muscle activity o Action on Adipose Tissue ▪ Reduces the circulation of free fatty acids and promotes the store of triglycerides in adipose tissue ▪ Suppression of cAMP production and dephosphorylation of the lipases in fat cells • Types of Insulin o Rapid-Acting (RAI): lispro, insulin aspart, insulin glulisine ▪ Onset of action 15 minutes, peak 1 hr ▪ Not compatible with NPH ▪ Used as bolus doses to correct hyperglycemia or to cover food eaten as meals o Short-Acting (SAI): regular, regular U-500 ▪ Onset of action 30 minutes duration of 8 to 12 hours ▪ Used as bolus insulin to correct hyperglycemia or to cover food eaten at meals o Intermediate-Acting (IAI): Neutral protamine Hagedorn (NPH) or isophane ▪ Onset of action is delayed by combining the insulin with protamine ▪ Onset of action is 1 to 1.5 hours and duration is 12 to 24 hours ▪ Used as basal insulin in both types 1 and 2 DM o Long-Acting (LAI): insulin glargine, insulin detemir ▪ No peak ▪ Used in types 1 and 2 DM as basal insulin ▪ Typically given HS but can be given at other times of day o Inhaled Insulin: Afrezza ▪ Inhaled powder ▪ Most rapid acting type of insulin ▪ Peak 12 to 15 minutes duration 2-3 hours ▪ Given with meals ▪ No indication for treating diabetic emergencies ▪ If used in type 1 DM, a long-acting insulin must also be used • Pharmacotherapeutics o Contraindications: hypoglycemia and hypersensitivity to product ingredients o Dose adjustments with renal dysfunction o Dose adjustments with hepatic impairment o Hypothyroidism: may require less insulin to treat diabetes o Hyperthyroidism: may increase the renal clearance of insulin ▪ Both require more frequent monitoring of glucose levels when insulin is used o Insulin resistance: occurs in type 2 DM ▪ Results in increased rate of endogenous glucose production secondary to increased glucagon levels r/t liver cells not receiving feedback messages ▪ Obesity, acanthosis nigricans, ketoacidosis, or endocrinopathies • Clinical Use (Dosage Schedule Pg. 562) o Type 1 DM ▪ These patients do not produce insulin ▪ Wide variety of regimens are utilized including • Regular insulin via insulin pump • Split-mix regimens • Intensive insulin therapy • Mixture of SAI and IAI or • SAI or RAI and LAI given 2-4 times a day o Type 2 DM ▪ These patients produce insulin but not enough to meet the body’s needs ▪ Have insulin receptor defects, insulin resistance, and altered hepatic glucose metabolism ▪ Insulin is Rx when adequate control not achieved by dietary, exercise, weight reduction, and oral agents ▪ Multiple regimens may be used o Dosing ▪ Average insulin doses are 0.6 to 0.8 units/kg/day ▪ Starting doses are 0.3 to 0.5 units/kg/d ▪ Obese patients may require more than 100 units per day ▪ Volumes approaching 200 units per injection triggers a switch to concentrated U-500 formulation ▪ Type 2 DM: LAI initiated at 0.1 unit/kg/day while simultaneously starting a PO agent o Mixing ▪ Mixing insulin is common practice but not all are compatible ▪ LAI insulin cannot be mixed with other insulin, requires are additional injection ▪ When mixing always draw clear insulin into the syringe first “Clear to cloudy” o Switching insulins ▪ Every insulin has unique characteristics and neither brand of insulin nor type of syringe nor needle should be changed without monitoring by the health care provider o Hyperkalemia ▪ IV infusion of glucose and insulin produce a shift of K into cells and lower serum K levels ▪ This Tx is usually reserved for hospitalized patients with very high K levels or those ARF cardiac arrhythmias o Pregnancy ▪ Gestational DM and management of patient with DM who become pregnant insulin is usually the drug of choice • Drug Interactions o Beta blockers can increase insulin resistance, producing hyperglycemia, can mask the s/s of hypoglycemia ▪ Do not mask diaphoresis, teach patients to check BG whenever they sweat • ADRs o Hypoglycemia: too much insulin or not enough food ▪ s/s of hypoglycemia: decreased LOC, hunger, diaphoresis, weakness, dizziness, and tachycardia ▪ BG <70 ▪ Treatment “rule of 15”consumer 15 gr of CHO, wait 15 minutes, and check BG ▪ Or if unable to ingest IM or SC glucagon or concentrated IV glucose o Diabetic ketoacidosis: too little insulin ▪ May result from stress, illness, infection, or insulin omission ▪ May develop slowly after a long period of adequate BG control ▪ Children with undiagnosed type 1 DM may present with DKA at the time of Dx ▪ S/s: drowsiness, dim vision, Kussmaul respirations, sweet smelling breath ▪ Indications of hyperglycemia that may precipitate DKA: polyuria, polydipsia, polyphagia, weight loss and fatigue, vomiting, dehydration, ketone odor to the breath, and ABD pain ▪ Tx requires hospitalization, IV fluids, correction of acidosis and hypotension, low dose regular insulin SC or IV o Inhaled insulin: bronchospasm o Do not Rx to patients with lung CA or Hx of lung CA Oral hypoglycemic agents • Many classes • Most prevalent type of DM is type 2 • Physiological alterations of type 2: insulin resistance suboptimal response of insulin sensitive tissues (liver, muscle, adipose tissue) to insulin • Results in 4 alterations in glucose metabolism o 1) insufficient production of endogenous insulin by beta cells o 2) tissue insensitivity to insulin o 3) impaired response of beta cells to BG levels o 4) excessive production of glucose by the liver secondeary to increased glucagon levels • Do not have an absence of insulin secretion • Liver and incretin hormone system are major organs in type 2 • Few and nonspecific pancreatic changes • Adipose tissue does not take up glucose in response to insulin, results in obesity • Increased visceral fat inversely related to insulin Biguanides: metformin (Glucophage) o Tx of type 2 DM o First line therapy in adults and children older than 10 y/o o Directly addresses the major pathological defects in type 2 DM o Monotherapy with metformin is effective as initial drug therapy ▪ If monotherapy with metformin is not effective it is used as combination therapy with other drugs or insulin o Significant effect on pre-diabetes or glucose intolerance (not FDA approved for this indication) ▪ Pharmacodynamics • Increases peripheral glucose uptake and utilization (insulin sensitivity), decreases hepatic glucose production, and decreases intestinal absorption of glucose • These actions address the patho defects to improve glucose tolerance and lower basal and postprandial glucose levels • Does not typically produce hypoglycemia • Does not cause hyperinsulinemia • Does not cause weight gain, patients often lose weight o Important drug action r/t obesity and DM • Inhibits platelet aggregation and reduces blood viscosity o factor in metabolic syndrome use • Those with higher BG levels for longer periods of time have more complications • African Americans with DM have higher BG: metformin can be twice as effective in this population as compared to whites • Modestly favorable impact on lipids r/t actions in the liver o Lowers mean fasting serum triglycerides, total cholesterol, and LDL, and increased HDL ▪ Pharmacotherapeutics • Two major contraindications: renal disease or dysfunction and metabolic acidosis • R/t Renal elimination of the drug o GFR above 30 is the cutoff (moderate kidney disease) • Chronic metabolic acidosis or high RF lactic acidosis r/t tissue hypoperfusion or hypoxia (severe dehydration, HF, respiratory failure, ETOH abuse with liver damage) • Do not use with hepatic disease • Cautious use in patients over 80 y/o r/t decreased renal function • Test CCr prior to initiating therapy and annually • Withhold 48 hours prior to and 48 hours after undergoing radiological studies that involve iodine-based contrast medium r/t altered renal function and associated with lactic acidosis o Only start after renal function is found to be normal • Withhold from patients undergoing surgical procedures when fluid will be withheld r/t RF dehydration and hypoperfusion, ARF lactic acidosis • Decreased B12 levels have been reported o If prior anemia fix that first before starting metformin • Possible link to dementia • Increased RF low TSH levels, first 6 months of use o Does not occur in those with normal thyroid, occurs in those with hypothyroid • Pregnancy Category B, use requires obstetric or endocrinology consultation • Use cautiously in breast feeding mothers, may cause hypoglycemia in the infant • Can be used in children with type 2 DM ages 10-16 y/o • African Americans are extremely responsive to the drug, clinically significant decrease in HbA1c o Clinical Use (Dosage Schedule Pg. 571) • Type 2 DM • Indicated for monotherapy for those who cannot control BG with healthy eating, increased activity, and weight loss o First line drug therapy for Type 2 DM ▪ Start therapy with ▪ Adults: • 500 mg BID with the morning and evening meal • or 850 mg BID with the morning and evening meal ▪ Children: • 500 mg BID with morning and evening meal ▪ Increase in increments of 500 mg every other week for adults ▪ Max dose adults 2,550 mg/day and 2,000 mg/day for children ▪ Max dose should be divided and given TID to reduce GI reactions ▪ HbA1c reduction achieved in 1.5% ▪ Especially useful in obese patients r/t weight loss produced by the drug ▪ Positive effect on lipids: especially those with HLD ▪ Sulfonylureas and metformin potentiate each other • Both fasting and postprandial BG levels • Monitor BG closely when adding a drug to the treatment regimen • Avoid hypoglycemia ▪ Available in intermediate and ER formulations and oral solution (500mg/5mL) o Concomitant Metformin and Sulfonylurea Therapy in Adults ▪ In patients not responsive to monotherapy after 3 months, PO med or insulin should be added ▪ Formulation of metformin plus glipizide (Metaglip) and metformin plus glyburide (Glucovance) ▪ If BG and HbA1c goals not met in 3 months add a third drug ▪ Endocrinologist referral o Concomitant Metformin and Thiazolidinediones ▪ Can be added with metformin alone or with other drugs ▪ Starting dose is based on current regimen of each drug ▪ Combination formulations metformin plus pioglitazone (ActoPlus Met and ActoPlus Met XR) and metformin plus rosiglitazone (Avandament) o Concomitant Metformin and Meglitinides ▪ Combination formulation of metformin plus repaglinide (PrandiMet) o Concomitant Metformin and Gliptins ▪ Combination formulation sitagliptin plus metformin (Janumet) • Given twice daily with meals and gradual dose escalation to reduce GI reactions ▪ Fewer hypoglycemic risks than combinations of glipizide (Metaglip) and metformin ▪ Possible worsening of renal impairment and pancreatitis o Concomitant Metformin and Insulin Therapy ▪ Initiate metformin IR or ER 500 mg once daily with patients on insulin therapy ▪ For inadequate response increase dose of metformin by 500 mg daily after 1 week and by 500 mg daily every week thereafter until adequate glycemic control is achieved ▪ Insulin should be decreased by 10-25% when FBG is less than 120 o Concomitant Metformin and SGLT2 medications ▪ No long term data for this combination ▪ Dapagliflozin/metformin ER (Xigduo XR) o Metabolic Syndrome ▪ Inhibition of platelet aggregation and decreases blood viscosity ▪ Recommended along with an ACE inhibitor or ARBS and statins in the Tx of insulin resistance syndrome ▪ Syndrome which includes obesity, HTN, HLD, and insulin resistance o Prevention of Conversion of Prediabetes to Diabetes ▪ First line drug for this indication ▪ Drug Interactions • Many drug interactions • Carbonic anhydrase inhibitors increase r/f lactic acidosis • Drugs may compete for tubular excretion o Digoxin, morphine, quinidine, trimethoprim, vanc o Dosage adjustments may be needed in metformin or interacting drugs • Cimetidine and furosemide increase peak metformin plasma levels • Avoid ETOH: potentiates effect of metformin on lactate metabolism • Beta blockers (mask s/s of hypoglycemia) and nifedipine (increases effects of metformin) ▪ ADRs • GI disturbances: ABD bloating, NVD, and metallic taste o Usually transient and resolve in 2 weeks of therapy • May be reduced by starting with low dose and titrating up slowly • Hypoglycemia is rare but can occur in reduction of calories, strenuous exercise not compensated with caloric intake, or concurrent use of another glucose-lowering drug or ETOH • Older adults, debilitated and malnourished patients and those with adrenal or pituitary insufficiency are at increased r/’f hypoglycemia ▪ Monitoring • Assess renal function before initiating therapy and at least annually o Crt and CCR • Patients at risk for metabolic acidosis should be assessed for evidence of ketoacidosis or lactic acidosis o Serum electrolytes and ketones, BG, and blood pH, lactate levels • LFTs prior to initiating therapy • Monitor response to therapy: o daily to weekly monitoring of fasting and postprandial BG and monitoring HbA1c Q 3 months or fructosamine Q 2 months • During initial therapy and with increases, FBG is used to evaluate response • After stabilized on a specific dose monitoring with FBG and A1C level Q 6 months • Some patients with inadequate B12 or calcium intake or absorption may be ARF developing subnormal B12 levels o RBC at initiation of therapy and every 2-3 years after that ▪ Patient Education • Take at the same time each day • Swallow pills whole • Use a card or calendar to remind patients of schedule for titrating doses • Take with food to decrease GI irritation • GI disturbances usually resolve in 2 weeks • If the patient develops vomiting or diarrhea or develops a fever, the drug is stopped • Dehydration may cause increased r/f lactic acidosis and decreased renal function • Teach s/s of lactic acidosis o Chills, dizziness, low BP, muscle pain, sleepiness, trouble breathing, slow heart rate, and weakness and report immediately • Stop drug when an iodine based contrast medium or surgery in which fluid will be withheld Sulfonylureas Drugs: • First generation: chlorpropamide, tolazamide, tolbutamide (Orinase) • Second generation: glipizide (Glucotrol and Glucotrol XL) • Glyburide: Glyburide (DiaBeta, Micronase), glynase (micronized formulation), glimepiride (Amaryl) • First oral drug to treat type 2 DM • Used in combo therapy • Only useful with patients with some endogenous insulin • R/f hypoglycemia and limited action on insulin resistance o Pharmacodynamics ▪ Increased endogenous insulin section by beta cells related to increased cAMP generation ▪ Improve binding between insulin and insulin receptors or increase the number of receptors ▪ Hypoglycemic effects r/t increased endogenous insulin production and improved beta cell sensitivity to BG or suppression of glucose release by the liver ▪ Potentiate the effect of antidiuretic hormone and produce mild diuresis ▪ Lowers A1c ▪ Effect is rapid to compared to other agents o Pharmacotherapeutics ▪ Contraindicated in patients with hypersensitivity to the drugs or the compounds in which they are mixed ▪ Cross-sensitivity may occur with other sulfonamides including thiazide diuretics ▪ Pregnancy Category C (glyburide is Preg Cat B) • Can cause prolonged hypoglycemia in the infant at time of birth • If it must be used d/c 2 to 4 weeks prior to delivery date ▪ Chlorpropamide and tolbutamide: enter breast mild, ▪ Contraindicated in nursing mothers ▪ Safety and efficacy in children not established ▪ Do not use in type 1 DM, DKA or diabetic coma, and uncontrolled infection, burns or trauma ▪ Patients with adrenal or pituitary insufficiency are especially susceptible to hypoglycemia ▪ Sever hepatic impairment may decrease hepatic release of glucose in response to hypoglycemia ▪ Renal impairment may cause decreased elimination leads to accumulation of drug and hypoglycemia ▪ Use with extreme caution in patient s with hepatic or renal impairment (Monitor frequently) ▪ Old adults and debilitated patients susceptible to the hypoglycemia action of the drugs ▪ Avoid long acting agents and use short acting agents with caution ▪ All sulfonylureas carry a warning that states that the administration of oral hypoglycemic drugs has been reported to be associated with increased cardiovascular mortality compared to Tx with diet alone or diet plus insulin • Study conducted by the University Group Diabetes Program o Clinical Use (Dosage Schedule Pg. 576) ▪ Type 2 DM • Both first and second generation drugs • Second-line therapy in patients who have previously used diet, exercise, weight control, and metformin • Therapeutic doses vary from 1 mg to 1,000 mg depending on the drug • All drugs are once daily doses and highly individualized based on BG readings o Higher doses may be divided BID • Start with lowest dose and increase every 4 to 7 days, based on BG control • If BG level goal is not achieved in one-half the maximum dose, consider adding a drug from a different class o Drug Interactions ▪ Interact with many drugs that either increase or decrease their hypoglycemia effect ▪ ETOH: produces a disulfiram like syndrome • facial flushing, occasional breathlessness but without nausea, vomiting, and hypotension o ADRs ▪ All sulfonylureas may produce sever hypoglycemia • Second generation drugs are less likely than first generation drugs ▪ Weight gain • Increased insulin secretion associated with weight gain and hyperinsulinemia • Combination with metformin reduces these adverse effects ▪ Dose related GI disturbances (nausea, epigastric fullness, heartburn) • Most common ADRs • Typically disappear when the dose is reduced • Glipizide: diarrhea, tolbutamide: taste alterations • Cholestatic jaundice is rare but requires d/c ▪ Dermatological reactions: rashes, pruritis, erythema, and urticaria • Transient and may disappear despite continued use of the drug • Photosensitivity (sunblock and clothing to cover skin in sunlight) ▪ SIADH (syndrome of inappropriate secretion of antidiuretic hormone especially in those with HF or hepatic cirrhosis • These drugs stimulate ADH release, augments hypothalamic pituitary release of ADH • Results in excessive water retention and dilutional hyponatremia ▪ Hemolytic anemia, agranulocytosis, leukopenia, and thrombocytopenia (rare) ▪ Initial and annual CBC o Rational drug selection ▪ Avoid in older adults ARF sever hypoglycemia ▪ Not approved for use in children ▪ Renal impairment: glipizide and tolbutamide, glyburide, tolazamide (CCr less than 30) ▪ Second generation drugs best to minimize drug interactions ▪ Once daily administration: reduced dosing complexity and improved adherence ▪ Glimepiride binds to different receptors than the other drugs and may be effective when others are not • Also associated with lower incidence of hypoglycemia o Monitoring ▪ HbA1c preferred tool for monitoring long term glycemia control ▪ Fructosamine (short term control monitoring) goal: 325 mmol or less goal for intensive therapy of 287 o Patient Education ▪ Take as prescribed the same time each day preferably before or with the morning meal ▪ All may be taken with food except glipizide ▪ Glipizide must be taken 30 minutes before a meal to prevent reduced absorption ▪ Don’t take a dose if the patient is unable to eat ▪ GI ADRs • Doses may be divided ▪ Most serious ADR: hypoglycemia ▪ Teach s/s and how to treat it ▪ Avoid concurrent use of other drugs before talking to provider ▪ Report sore throat, rash, or unusual bruising or bleeding ▪ Report unusual weight gain, swelling of the ankles, drowsiness, or SOB Alpha-Glucosidase Inhibitors o Drugs: acarbose (Precose) and meglitol (Glyset) o Oral antihyperglycemic drugs for type 2 DM o Reduce BG both as added therapy who cannot achieve control on diet alone and as added therapy for patients who BG cannot be controlled by lifestyle modification and other ora antihyperglycemic agents o Not typically monotherapy: adjunct to other therapy o Pharmacodynamics ▪ Do not act directly on any of the defects in metabolism ▪ Competitively inhibit the absorption of CHO from the small bowel ▪ Digestive enzymes activity is diverted from CHO digestion while trying to digest the alpha glucosidase inhibitor ▪ Delays digestion of CHOs ▪ The process of enzyme induction takes weeks to months patients may experience intestinal flatus and ABD distention ▪ No inhibitory activity against lactase (does not induce lactose intolerance) ▪ Lower BG after meals: the higher the postprandial BG level the larger the reduction will be that the drug can provide ▪ Also reduce glycosylated hemoglobin levels ▪ Do not enhance pancreatic beta cell secretion of insulin ▪ Do not produce hypoglycemia ▪ Not associated with weight gain ▪ Reduce the weight increasing effects of sulfonylureas when given in combination with them ▪ Effective on any CHO food intake, including liquid diets via NG tube o Pharmacotherapeutics ▪ Do not use in patients with bowel diseases (IBD, bowel obstruction or risk factors for it, chronic intestinal disease associated with marked digestive disorders, or conditions that may deteriorate because of increased gas in the intestine) ▪ Severe renal impairment increases plasma concentrations of alpha-glucosidase inhibitors • Dosage adjustments are not possible because the drug acts locally • Treatment is not recommended ▪ Safety in pregnancy not established, Pregnancy Category B ▪ Do not use unless clearly needed ▪ Should not be used in lactating women ▪ Safety and efficacy in children have not been established o Clinical Use (Dosage Schedule Pg. 580) ▪ Management of type 2 DM ▪ Useful for patients with high postprandial BG ▪ Initial dose of both drugs is 25 mg TID taken with the first bite of each meal ▪ Taking the dose with the first bit is critical ▪ Dose is increased in increments of 25 mg with each mean at 4 to 8 week intervals ▪ Maintenance dose 50 mg TID ▪ Weight considerations ▪ No higher than 50 mg TID for patients less than 60 kg and ▪ The 100 mg TID dose should be reserved for patient weight more than 60 kg ▪ Max dose 100 mg TID o Drug Interactions ▪ Acarbose may decrease serum digoxin levels ▪ Enhance the hypoglycemia effects of acarbose and miglitol • Neomycin, selective serotonin uptake inhibitors, salicylates, and MAO inhibitors ▪ Diminish hypoglycemia effects • Somatropin, loop and thiazide diuretics, and corticosteroids ▪ Both drugs may have therapeutic effects reduced by concurrent admin with digestive enzymes or intestinal absorbents o ADRs ▪ GI symptoms are the most common ADR • Flatulence (leading reason for discontinuance), Diarrhea, ABD pain • GI ADRs can be reduced by slow titration to maximal dose ▪ Do not cause hypoglycemia alone but may do so in combination with other drugs • This hypoglycemia cannot be treated with typical Tx (Rule of 15) r/t MOA which slows the absorption of sugars ▪ Reversible increases in ALT and AST have occurred with acarbose greater than 200 mg TID • Hepatic abnormalities improve or resolve with d/c of the drug o Monitoring ▪ Before starting therapy and at least annually assess renal function • Not recommended for patients with renal impairment • Serum electrolytes, BUN, and crt ▪ Assess liver function for those taking acarbose • Acarbose associated with reversible elevation in transaminase • Assess every three months for the first year ▪ After regimen established FPG and HbA1C every 3 to 6 months o Patient Education ▪ Take with the first bite of each meal ▪ Timing of administration is stressed because taking it too soon reduces its effect and taking it after a meal has no effect ▪ GI ADRs: slow titration of dose to reduce • Usually resolve in 2 weeks ▪ Treat hypoglycemia with dextrose ▪ Severe hypoglycemia Tx with IV glucose or glucagon ▪ Wear a med bracelet stating the drug and where dextrose is located (purse, pocket) Thiazolidinediones (TZDs) o Drugs: pioglitazone (Actos) and rosiglitazone (Avandia) o Action lowers BG as monotherapy for patients who cannot achieve BG control with diet alone o Successful as added therapy for patients who cannot be controlled by lifestyle modifications or other antihyperglycemic agents o Not part of initial therapy o Used cautiously r/t potential for cardiovascular problems (especially rosiglitazone) o Pharmacodynamics ▪ Improve insulin sensitivity (a major patho problem of type 2 DM) ▪ Depend on the presence of insulin for their action ▪ Highly selective activators of a receptors that regulates gene transcriptions, results in proteins that express improved insulin action in the cell ▪ Increased utilization of available insulin by the liver and muscle cell and adipose tissue ▪ Reduce hepatic glucose production ▪ All of these actions improve glucose tolerance and lower both basal and postprandial BG ▪ Do not produce hypoglycemia ▪ Do not cause hyperinsulinemia: do not stimulate insulin release ▪ Modest impact on lipids r/t actions in the liver o Pharmacotherapeutics ▪ Chronic liver disease: increased plasma concentrations of metabolites • Must check transaminase at the start of therapy and frequently during therapy • Do not initiate in patients with ALT greater than 2.5 times the upper limit of normal • d/c if jaundice develops or labs suggest liver injury (ALT greater than 3 times the upper limit of normal) ▪ Fluid retention with increase in body weight and decrease in hemoglobin • Contraindicated in patients with NYHA class II or IV HF ▪ Black Box Warning: Cardiotoxicity ▪ In premenopausal anovulatory patients with insulin resistance TZD may result in resumption of ovulation ▪ No studies in pregnant women, unknown if excreted in breast milk ▪ Safety and efficacy in children have not been established o Clinical Use (Dosage Schedule Pg. 582) ▪ Monotherapy • Pioglitazone (Actos): initial dose 15-30 mg/day, max dose 45 mg/day • Rosiglitazone (Avandia): 4 mg/day single dose or in divided doses BID, max dose 8 mg/day ▪ Combination Therapy with Oral Agents • When added to sulfonylurea, initiate pioglitazone with either 15 or 30 mg dose • Rosiglitazone: initiate therapy at 4 mg/day in single or divided doses • If glycemic control is inadequate increase the TZD at 8 to 12 weeks ▪ Combination Therapy with Insulin • For patients stabilized on insulin, continue the insulin dose • For pioglitazone: initiate at 15 to 30 mg once daily • Rosiglitazone: 4mg once daily and do not increase this dose • For both drugs, decrease the insulin dose by 10-25% if hypoglycemia or FBG decreases to less than 100 o Drug Interactions ▪ Pioglitazone with an oral contraceptive that contains ethinyl estradiol and norethindrone reduces plasma concentrations of both drugs by 30% • A higher dose of OC or an alternative birth control method may be needed ▪ Pioglitazone is metabolized by the CYP450 3A4 system • No specific formal pharmacokinetics interaction studies have been conducted • Avoid these drug combinations or carefully monitor o ADRs ▪ Generally well tolerated (exception of cardio events, weight gain, HTN, HF, and MI) ▪ Some patients experience increases in total cholesterol, HDL, and LDL, and weight gain o Monitoring ▪ ALT levels must be checked at the start of therapy • Recheck every 2 months for the first 12 months • Recheck weekly if ALT increases ▪ D/c if ALT is more than 3 times the upper limit of normal ▪ D/c if jaundice occurs ▪ Cardiac function evaluated on a regular basis: look for indications of MI or HF o Patient Education ▪ Pioglitazone: once daily in the morning ▪ Rosiglitazone: may be taken once or twice daily ▪ Do not change dosing schedule without talking to your doctor ▪ Generally well tolerated and ADRs are rare ▪ ADR: hepatocellular injury • Immediately report s/s of hepatic dysfunction (nausea, vomiting, ABD pain, fatigue, anorexia, jaundice, or dark urine) • Explain that hepatic function must be carefully monitored ▪ Hypoglycemia is not a risk with monotherapy but may occur when TZDs are given with other glucose lowering drugs ▪ Report immediately CP, SOB, peripheral edema, or indications of impending stroke ▪ Female patients using oral contraceptives: possible need to increase dose of OC or choose alternative birth control method Meglitinides o Drugs: repaglinide (Prandin) and nateglinide (Starlix) o Phenylalanine derivatives that are short acting insulin secretagogues o Act by stimulation of insulin secretion to lower postprandial BG o DO not direct affect FBG or the other pathological defects in metabolism o Most useful in patients whose primary glucose alteration is postprandial hyperglycemia and the amount of insulin released depends on existing BG levels o Used as adjunct therapy o Pharmacodynamics ▪ Close ATP dependent K channels in the beta cell membrane by binding at specific receptor sites ▪ The potassium channel blockade depolarized the beta cell and leads to an opening of calcium channels ▪ The influx of calcium increases the secretion of insulin o Pharmacotherapeutics ▪ Use with caution in hepatic impairment: metabolized by the CYP450 system • Longer intervals between dosage ▪ Caution in patients with sever renal impairment and adrenal/pituitary impairment: • may exert more glucose lowering effects ▪ Repaglinide and nateglinide are Pregnancy Category C, no adequate trials, do not use in pregnancy ▪ No safety and efficacy for these drugs in children o Clinical Use (Dosage Schedule Pg. 585) ▪ Monotherapy • Nateglinide: initial and maintenance dose 120 mg TID, 1 to 30 minutes prior to each meal • If the A1C is less than 7 dosing may be started at 60 mg TID • Repaglinide: A1C less than 8 or not previously treated 0.5 mg before each meal for A1C greater than 8 or patient is being switching from another oral agent initial dose is 1 to 2 mg TID ▪ Combination Therapy • May be given in conjunction with metformin or TZDs • Not currently on the ADA treatment algorithm for type 2 DM • Ecause more frequent dosing and less glucose lowering effectiveness than other drugs ▪ For Both Uses • Dosage changes are based on FPG and A1C o Drug Interactions ▪ CYP450 system: CYP2C9 and CYP3A4 ▪ Antifungals and antimicrobials may increase the risk for hypoglycemia: increase blood levels of the drug ▪ Meglitinides can potentiate the action of highly protein bound drugs by competing for their binding sites (warfarin, beta blockers, NSAIDS) o ADRs ▪ Hypoglycemia ▪ Patients with hepatic insufficiency, older adults, and debilitated and malnourished patient are high risk for hypoglycemia ▪ Frequency of hypoglycemia greater with A1c less than 8 ▪ Careful timing of administration with regard to meals lessens ADRs ▪ May cause weight gain o Monitoring ▪ Periodic monitoring of FPG and A1C every three months o Patient Education ▪ Always administer 0 to 30 minutes prior to each meal, omit if meal skipped ▪ If extra meals are eaten, extra doses should be taken ▪ Timing of drug in relation to food is critical ▪ ADR: hypoglycemia ▪ Teach how to prevent, recognize, and treat hypoglycemia Dipeptidyl Peptidase-4 Inhibitors ▪ Known as gliptins ▪ DRUGS: sitagliptin, saxagliptin, linagliptin, and alogliptin ▪ Incretin hormones: act on the incretin hormone system and have an indirect effect on increasing insulin production ▪ Only moderate glycemic control ▪ Well tolerated, low r/f hypoglycemia, weight neutral ▪ Approved for monotherapy, best used as add on therapy in combination with metformin as second line therapy o Pharmacodynamics ▪ GLP-1 found in the gut, significantly reduced in type 2 DM ▪ DPP-4 inhibitors extends the action of any GLP-1 still present in the system and interferes with its rate of breakdown ▪ Reduce pre and postprandial glucose levels, reduces A1C, and promotes weight loss o Pharmacotherapeutics ▪ Use with caution with renal impairment r/t renal excretion ▪ Risk for toxicity with ESRD and moderate to severe renal impairment ▪ Dosage adjustments are needed for renal impairment (except linagliptin) ▪ Caution in older adults r/t decreased renal function ▪ Pregnancy Category B: new drugs no long term data ▪ Safety and efficacy in children not established o Clinical Use (Dosing Schedule Pg 587) ▪ Mono or combo therapy ▪ Especially useful for obese patients because they are not associated with weight gain ▪ Preferred over GLP-1 medications (injection averse) ▪ Monotherapy • Sitagliptin: once daily 100 mg • Saxagliptin: once daily between 2.5 to 5 mg • Linagliptin dosage: 5 mg once daily • Sitagliptin and saxagliptin are reduced for decreased creatinine clearance ▪ Combination Therapy • All are approved for use in combo therapy • DPP-4s in two drug combinations with metformin and three drug combos with sulfonylureas, TZDs, or insulin o Drug Interactions ▪ ACE inhibitors associated with risk of angioedema ▪ Digoxin increases in concentration ▪ Limited CYP 3A4 and CYP2C8 metabolism o ADRs ▪ Typically well-tolerated ▪ Most common ADRs: edema, HA, and UTI ▪ Hypoglycemia can occur with combination therapy (insulin) ▪ Acute pancreatitis, caution in patient with Hx of pancreatitis or at greater risk o Monitoring ▪ Assess renal function: crt and CCr and then crt annually ▪ Assessed by daily to weekly FPG and postprandial BG and A1C or fructosamine o Patient Education ▪ Taken once daily in the AM ▪ Hypoglycemia with combo therapy Selective Sodium Glucose Co-Transporter 2 (SGLT-2) inhibitors Drugs: canagliflozin (Invokana), dapglifoxin (Farxiga), and empagliflozin (Jardiance) ▪ Novel inhibitors of renal SGLT-2, block reabsorption of glucose in the kidney, and promote excretion of excess glucose in the urine ▪ Mono or combo therapy o Pharmacodynamics ▪ Inhibition of SGLT-2 lowers reabsorption of plasma glucose concentration in the kidneys, results in increased glucose excretion and reduction of plasma glucose ▪ Works in the proximal tubule to absorb about 90% of the glucose in the ultrafiltrate o Pharmacotherapeutics ▪ Contraindicated in patients with severe renal impairment (GFR less than 30), ESRD, or who are on dialysis ▪ Modification of the dose is suggested when GFR is less than 45 ▪ Severe hypersensitivity reactions have been reported ▪ Can cause volume depletion and symptomatic hypotension ▪ Decrease insulin dose if being taken with insulin ▪ May be kidney protective when started early ▪ ARF hyperkalemia o Clinical Use (pg. 592) ▪ Type 2 DM • Adjunct to diet and exercise o Drug Interactions ▪ Canagliflozin should not be taken with pimozide ▪ Increases digoxin ▪ Can increase the effect of ACE and ARBs, aliskiren, aripiprazole, duloxetine, eplerenone, and potassium sparing diuretics o ADRs ▪ Genital fungal infections, UTI, and increased urination most common ▪ Female genital mycotic infection or male genital mycotic infections ▪ Dose related LDL increase ▪ Volume depletion in older adults, GFR less than 60, and patients on loop diuretics ▪ Bladder CA (too few cases to take action by FDA): do not Rx with Hx of bladder CA ▪ Glucose causes osmotic diuretic effect ▪ Use with caution in CB or DVT patients ARF o Monitoring ▪ Renal function, electrolytes, genital mycotic infections ▪ Urine dip sticks are expected to show positive for glucose (intended consequence) ▪ Anticipated increase in hematocrit ▪ Increases in both LDL and inorganic phosphorus is possible o Patient Education ▪ Canagliflozin (Invokana) should be taken at the same time each day before the first meal ▪ Dapaglifloxin and empagliflozin taken without regard to meals ▪ S/s dehydration: dizziness, hypotension, weakness) ▪ genital yeast infections (itching, redness/swelling, thick white discharge) • easily treated but usually recur ▪ allergic reactions can occur and cause an emergency Amylin Agonists Drugs: pramlintide (Symlin) ▪ Synthetic analogue of the beta cell hormone amylin for use as adjunct therapy in both type 1 and type 2 DM to help reduce BG after eating ▪ Acts on glucagon secretion, slowing gastric emptying and suppressing appetite o Pharmacodynamics ▪ Co-located and co-secreted with insulin in response to eating ▪ Amylin affects postprandial glucose by slowing gastric emplying, suppression of glucagon section, and centrally mediated modulation of appetite ▪ Decreases in A1C and weight o Pharmacotherapeutics ▪ Contraindicated: Confirmed Dx of gastroparesis or required use of drugs to stimulate GI motility ▪ Do not use in patient with Hx of nausea ▪ Risk for hypoglycemia when given with insulin ▪ Do not use in patients with poor compliance with insulin regimen and/or BG monitoring or recurrent episodes of hypoglycemia ▪ Use with caution in the elderly r/t renal metabolism ▪ No good studies in pregnant women ▪ o Clinical Use (pg 595) ▪ Type 1 DM • Initiate at 15 mcg and titrate up in 15 mcg increments as tolerated every 3 days, to a 30 to 60 mcg maintenance dose • If nausea is clinically significant at 60 reduce to 30 • Adjust insulin ▪ Type 2 DM • Initiate at 60 mcg immediately before meals • Increase to 120 mcg when no clinically significant nausea has occurred for 3 to 7 days • If significant nausea persists at 120 decrease back to 60 mcg • Adjust insulin dose o Drug Interactions ▪ Based largely on other drugs that increase or decrease the actions of pramlintide ▪ Drugs that alter GI motility and PO drugs dependent on gastric emptying for absorption ▪ Anticholinergic effects of drugs enhanced by pramlintide ▪ Avoid ETOH increases r/f hypoglycemia ▪ Garlic, chromium, and gymnema increase hypoglycemic effects o ADRs ▪ Pramlintide Black Box Warning: increased risk for severe hypoglycemia when used in conjunction with insulin ▪ Use with caution with Beta blockers that may mask s/s of hypoglycemia ▪ Most ADRs are GI disturbances ▪ Nausea and decreased with time ▪ Gradual titration to reduce nausea o Patient Education ▪ SQ in thigh or ABD not arm ▪ Given immediately before each major meal containing at least 250 kcal or 30 g of carbs ▪ Cannot be mixed with other insulin ▪ Administer in a separate syringe ▪ At least two inches away from injection site used for insulin ▪ Room temperature Glucagon-like peptide Agonists (GLP-1) or incretin mimetics Drugs: exenatide (immediate and ER), liraglutide, dulaglutide, and albiglutide o Acts on the incretin system o GLP 1 is a naturally occurring peptide produced in the small intestine: potentiates glucose stimulated insulin section o Bind directly to receptors in the beta cell and act as an incretin mimetic o Used with other meds o Low risk for hypoglycemia o Given by injection, weekly dosing with exenatide and albiglutide o Recommended in two step therapy on metformin and in three drug with metformin and a sulfonylurea or TZD or insulin o GLP 1 receptors must be present in the gut to act o In Loss of receptor number in DM o Promotes satiety and weight loss o Reduction of systolic pressure and lower triglycerides o Pharmacodynamics ▪ Moderates glucose secretion and lowering glucagon concentrations during periods of hyperglycemia ▪ Lead to decreased hepatic glucose output and decreased insulin demand ▪ slow gastric emptying and reduce appetite o Pharmacotherapeutics ▪ Severe GI disease: UC, Crohn’s) should not use r/t drugs effect on gastric emptying ▪ Pancreatitis: report persistent, severe ABD pain, may be accompanied by vomiting ▪ C cell thyroid tumors or hyperplasia ▪ Not recommended for use in those with moderate renal impairment or ESRD ▪ ARF and exacerbations of CRF have been reported ▪ May be r/t dehydration ▪ Increased LFTs (prior liver or gallbladder disease) ▪ Pregnancy Category C: no studies in pregnant women o Clinical Use ▪ Combo therapy dosages page 597 ▪ Not indicated for monotherapy ▪ If given with metformin or TZD keep the metformin or TZD dose the same ▪ If given with a sulfonylurea, reduce sulfonylurea dose to reduce r/f hypoglycemia o Drug Interactions ▪ Separate administration of the interacting drug and the incretin mimetic will usually resolve the problem ▪ INR increases with warfarin: do not use concurrently o ADRs ▪ High frequency of GI disturbances: NVD ▪ Tend to subside over time ▪ ER formulation has more transient nausea prfile ▪ Liraglutide has few reports of GI distress ▪ Consult with an endocrinologist if antiemetic use is considered ▪ Slow and low titration may reduce GI ADRs o Patient education ▪ Administer in thigh, ABD, or arm ▪ Give IR exenatide 60 minutes before morning and evening meals at least 6 hours apart Glucagon o Hormone secreted by the pancreas o Used clinically to elevate BG o Pharmacodynamics ▪ Accelerates liver glucogenolysis by stimulating cAMP synthesis and increasing phosphorylase kinase activity ▪ Results in increased breakdown of glycogen to glucose and inhibition of glycogen synthesis ▪ End result is elevation in BG o Pharmacotherapeutics ▪ Only contraindication is hypersensitivity to it ▪ Use with caution in patient with insulinoma or pheochromocytoma ▪ May cause initial BG increase but then may cause subsequent hypoglycemia ▪ Stimulates catecholamine release: increased BP in patient with pheochromocytoma ▪ Positive inotropic and chronotropic effects ▪ Pregnancy Category B: no well controlled studies in pregnant women o Clinical Use (pg 599) ▪ Reversal of hypoglycemia ▪ Action is dependent on the presence of glycogen in the liver • Little or no help in starvation, adrenal insufficiency, or chronic hypoglycemia o Drug Interactions ▪ Increased anticoagulation effects of oral anticoagulants r/f bleeding o ADRs ▪ NV ▪ Rare allergic reactions (phenol and glycerin in some products) o Patient Education ▪ Patients at high risk for hypoglycemia: keep the medication with you and make sure someone with you knows how to reconstitute it and give it Thyroid Agents o Pharmacodynamics ▪ TH effect all body processes: lack of it slows the processes down ▪ Synthetic TH produce the same effects on tissues as endogenous TH o Pharmacotherapeutics ▪ CVD (CAD) may worsen however increased risk of death from HF in African Americans with even mild hypothyroidism should not dissuade cautious use ▪ Contraindicated after recent MI ▪ Decreased bone density with long term therapy ▪ TH therapy in patients with DI or adrenal insufficiency exacerbates the intensity of their symptoms • Downward TH adjustments ▪ Severe or prolonged hypothyroidism can lead to decreased adrenocortical function • Can cause adrenocortical insufficiency • Requiring supplemental adrenocorticosteroids o Clinical Use ▪ Hypothyroidism • Start slow and titrate slowly • Levothyroxine: o Adults: start at 50 mcg daily and increased in increments of 25 mcg/d at 2 to 4 week intervals to 100-150 mcg daily o Target dose is based on TSH levels and is approximately 1.7 mcg/kg/day o Older adults may require less than 1 mcg/kg/day as their target o Initial dose for elders: 25 to 50 mcg/day with gradual dosage increases of 12.5 to 25 mcg/d at 6 to 8 week intervals • Liothyronine (T3) start at 25 mcg/d increased by 12.5 to 25 mcg/day at 1 to 2 week intervals until maintenance dose of 25 to 50 mcg is reached • Indicated for use in infants, children, adults, and geriatric patients o Drug Interactions ▪ Bile acid sequestrants, iron salts, and antacids decrease absorption ▪ Estrogens decrease response to TH ▪ SSRIs may require dosage adjustments of TH ▪ TH decreases effectiveness of warfarin, digoxin, and beta blockers o ADRs ▪ Hyperthyroidism due to overdose (increased HR, arrhythmias, CP, tremors, nervousness, insomnia, irritability, diarrhea, vomiting, weight loss, menstrual irregularity, or heat intolerance) assess TSH and make dosage adjustments o Monitoring ▪ TSH and free T4 • Elevations in TSH indicate insufficient TH • TSH levels below desired levels indicate excessive TH ▪ Checked initially and at 6 weeks after the first adjustment ▪ Recheck at 4 to 6 months after achieving euthyroid ▪ Steady state takes 4 to 6 weeks to achieve ▪ After stable: TSH annually ▪ Infants must be checked every 1 to 2 months ▪ Children should be monitored every 3 to 6 months ▪ Diagnostic TSH levels are not the same as therapeutic levels • 0.5 to 5.0, most patients best maintained between 1.0 to 2.5 o Patient Education ▪ Single daily dose in the AM before breakfast ▪ Take levothyroxine on an empty stomach to enhance absorption ▪ If more than three doses are missed notify HC provider ▪ Do not change brands, differences between brands must be re-titrated ▪ Measure pulse rate, if greater than 100 bpm at rest hold dose and notify provider ▪ May indicate excessive TH ▪ Report nervousness, CP, HTN and unexplained weight loss of more than 2 lbs in 1 week ▪ Some children on TH may experience partial air loss ▪ Usually temporary ▪ Elders at higher risk of developing A fib ▪ Chronic illnesses managed with self monitoring of symptoms and drug therapy ▪ Medications needed for life unless patho is transient in nature (pregnancy) Antithyroid Agents • Drugs: propylthiouracil and methimazole • Inhibit synthesis of TH or destroy thyroid gland tissue • Used to treat hyperthyroidism (thyrotoxicosis): excessive TH • Graves’ disease • Dramatic increase in iodine uptake and thyroid gland metabolism • Thyroid storm: life threatening situation • Heat intolerance, increased sensitivity to stimulation of SNS o Pharmacodynamics ▪ Inhibit synthesis of TH ▪ Do not inactivate existing thyroxine and tri iodothyronine store in the thyroid gland or circulating in the blood o Pharmacotherapeutics ▪ I131 is contraindicated (Category X) in pregnancy r/t impact on the infant when it crosses the placenta and into breast milk ▪ Methimazole is associated with birth defects ▪ Propylthiouracil in early pregnancy as clinically necessary ▪ Methimazole and propylthiouracil can cause goiter and cretinism in the fetus o Clinical Use ▪ Hyperthyroidism/Graves’ Disease • Propylthiouracil 150 to 300 mg TID • 300 to 900 mg/day • Methimazole started at 10 to 15 mg daily • For moderate disease methimazole is 30 to 40 mg/day and for severe disease dose is 60 mg/day ▪ Toxic Goiter • Require higher doses • Methimazole 60 mg/d TID • Propylthiouracil 600 to 900 mg/day o Drug Interactions ▪ Any drug that causes bone marrow suppression have an additive effect with antithyroid drugs ▪ Additive antithyroid effects with lithium, potassium iodide, or sodium iodide o ADRs ▪ Agranulocytosis and possible aplastic anemia ▪ Risk is higher for patients with decreased bone marrow reserve, older than 40, and receiving more than 40 mg/day ▪ d/c drug if this ADR occurs ▪ Drug induced hepatitis and abnormal hair loss ▪ Black Box Warning: propylthiouracil and liver failure ▪ Drowsiness, HA, paresthesia, vertigo, diarrhea, nausea, arthralgia, and pruritic skin rash o Monitoring ▪ TSH and free T4 evaluated prior to initiating therapy • Aromatase inhibitors • Drugs: o Pharmacodynamics o Naturally occurring enzyme involved with estrogen synthesis o Inhibition of the enzyme is the major role of the class o Approved for post breast CA treatment in women o Men can take the medication if they have estrogen sensitive breast CA or to resolve gynecomastia or fertility issues r/t imbalance of testosterone to estradiol ratio o Pharmacotherapeutics o Used as adjuvant therapy in estrogen receptor positive postmenopausal breast CA patients o Added to the plan after 3 to 5 years of tamoxifen therapy and for at least 5 years o Used as first line Tx in cases of advanced metastatic CA o Unlabeled uses for ovarian CA and to stimulate ovulation in anovulatory women o Oral agents taken once daily o Anastrozole 1 mg tablet, exemestane is 25 mg, and letrozole come in a 2.5 mg dose o Require special handling and disposal o Contraindicated in pregnancy and breast feeding o Clinical Use o Breast CA in post-menopausal women and some indications in men o Drug Interactions ▪ Do not take with tamoxifen or an estrogen product ▪ Anastrazole cannot be taken with pimozide ▪ Anastrazole and letrazole decrease the effect of digoxin and Vit K antagonists o ADRs/ Common adverse effects with aromatase inhibitors ▪ Various pain syndromes, vertigo, insomnia resulting in daytime sleepiness and confusion, increased risk of blood clots, and hair loss ▪ Loss of bone mass ▪ All patients should be on Vit D ▪ Relative leukopenia has occurred ▪ HTN ▪ Life threatening increase in blood clotting can result in MI, stroke, or pulmonary embolus ▪ Intense hot flashes Chapter 33: Diabetes Mellitus • Clinical signs & symptoms • Risk factors & associated complications • Diagnostic criteria • Criteria for screening asymptomatic adults • Differentiate between onset, peak and duration of insulin and oral hypoglycemic agents (table 33-4) • Know treatment algorithms • A1C treatment goal • Calculate an appropriate daily dose of insulin for initiation of insulin therapy • Insulin treatment algorithm for Type 1 DM • A1C monitoring during oral or insulin diabetes management • Correlate mean plasma glucose level according to A1C (table 33-6) • Clinical manifestations of diabetic autonomic neuropathy • Hypoglycemia treatment (amount of carbohydrates and examples) • Storage of insulin • Drug monitoring with metformin • Antidiabetic medications associated with photosensitivity • Antidiabetics to avoid in the elderly & why • Improving patient compliance with diabetes treatment • Diabetic medications to avoid when taking digoxin • Classes of diabetes medications • Diabetic medications with need for renal dose adjustment • Diabetic medications associated with increased risk for genital mycotic infections Chapter 41: Hyperthyroidism and Hypothyroidism • Clinical signs & symptoms, risk factors, associated symptoms and diagnosis • Time anticipated for total reversal of hyperthyroid symptoms with methimazole • Other drugs used to provide symptomatic relief • Routine testing with drug therapy • Recommended dietary iodine intake • Drugs that increase metabolism of T4 • Symptoms of hyperthyroidism and hypothyroidism • Hyperthyroid drugs with risk for hepatic toxicity • Bile acid sequestrants absorption and administration • Levothyroxine administration instructions • Differentiate between primary and secondary hypothyroidism and hyperthyroidism [Show More]
Last updated: 1 year ago
Preview 1 out of 57 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 09, 2022
Number of pages
57
Written in
Additional information
This document has been written for:
Uploaded
Mar 09, 2022
Downloads
0
Views
39

.png)