*NURSING > STUDY GUIDE > NR566 Week 2 Study Outline Ch 17: Drugs Affecting the Respiratory System Bronchodilators :LATEST,100 (All)
NR566 Week 2 Study Outline Ch 17: Drugs Affecting the Respiratory System Bronchodilators :LATEST,100% CORRECT
Document Content and Description Below
NR566 Week 2 Study Outline Ch 17: Drugs Affecting the Respiratory System Bronchodilators :LATEST ... Beta 2 Receptor Agonists (B2RA): Short and long acting beta agonists • B2RA widely used in all ages to treat reversible bronchoconstriction caused by reactive airway disease (RAD) or COPD • Bronchodilators • Short-acting beta agonists: Albuterol (ProAir, Ventolin, Proventil) , metaproterenol (Alupent), terbutaline (Brethine, Brethaire), bitolterol (Tornalate), pirbuterol (Maxair), and levalbuterol (Xopenex) • Long-acting beta agonists: arformoterol (Brovana), salmeterol (Serevent), formoterol (Foradil), and indacaterol (Arcapta Neohaler) • Drug of choice during pregnancy for asthma Pharmacodynamics • Act on smooth muscle to reverse bronchospasm, decreases airway resistance and residual volume and increasing VC and airflow • Stimulate beta 2 adrenergic receptors in the lungs to increase cAMP production which relaxes bronchial smooth muscle and inhibits mediators from hypersensitivity cells (mast cells) • All beta agonists stimulate beta 1 activity (increased HR, tremor)f Short Acting Beta Agonists • Albuterol o Selective beta2 agonist with minor beta1 activity o Often first-line drug r/t less ADRs than the other drugs in this class o Increases HR by stimulating beta 2 receptors in the heart and vascular smooth muscle • Levalbuterol: (similar to albuterol), where the (S)-isomer from racemic albuterol is removed • Pirbuterol: selective beta 2 agonist, similar to albuterol • Terbutaline: similar to albuterol, selective beta 2 with minor beta 1 activity o Known to inhibit uterine contractions • Metaproterenol: beta 2 selective with some beta 1 activity, less selective than albuterol or terbutaline • Bitolterol: hydrolyzed by esterase in the lung to colterol, or terbutylnorepinephrine, selective beta 2 Long Acting Beta Agonists (Salmeterol, formoterol, indacaterol, and aformoterol) • Salmeterol is more selective for beta2 receptors than albuterol and has minor beta1 activity. o 12 hour half-life o Formoterol: 200-fold greater agonist activity at B2 than albuterol and has minor B1 activity o Aformoterol (R,R)-enantiomer of formoterol, twice as potent as formoterol o Indacaterol: 24 fold greater B2 activity than B1 o Salmeterol and formoterol exert long-lasting broncho protection against allergen, exercise, histamine, and methacholine caused bronchospasm Pharmacokinetics • Contraindications: Cardiac arrhythmias (tachycardia or heart block caused by digitalis intoxication, angina, narrow-angle glaucoma, organic brain damage (epi only), and shock during general anesthesia with halogenated agents • Monitor closely: HTN, ischemic heart disease, coronary insufficiency, CGH, and Hx of stroke and/or cardiac arrhythmias • Diabetics: potential drug-induced hyperglycemia, insulin dose may need increased • Hyperthyroidism: ADRs are more likely to occur with use of bronchodilators • Digoxin: require close monitoring, albuterol increases the volume of distribution of dig and can cause decreased dig blood levels • Pheochromocytoma: avoid, severe HTN may occur • Older adults: Lower doses r/t increased sympathomimetic sensitivity • Black Box warning for LABAs: The risks of salmeterol (Serevent) and formoterol (Foradil) outweighed the benefits and should not be used singly in asthma for all ages o Two-fold increase in catastrophic events (asthma-related intubations and death) o The use of LABAs is contraindicated without the use of an asthma controller medication such as an inhaled corticosteroid o Only use long-term in patients who asthma cannot be adequately controlled on asthma controller medications o Use for the shortest duration of time required to achieve control, then maintain on an asthma controller medication o Pediatric and adolescent patient who require addition of a LABA to an inhaled corticosteroid should be a combination product containing both an inhaled ICS and a LABA, to ensure compliance with both medications • Terbutaline pregnancy category B (prevent contractions) (others category C) • Albuterol safe for all age children • Metaproterenol can be used in young children • Levalbuterol, as young as 2 (drug insert says 6) • Salmeterol should not be used in children less than age 4 years and never singly. • Formoterol age 5 and older • Indacaterol and aformoterol are used for COPD, not for use in children or adolescents Drug and Food Interactions o Many drug interactions o Digitalis glycosides: increased risk of dysrhythmia o Beta adrenergic blocking agents (Beta Blockers): direct competition for beta sites resulting in mutual inhibition of therapeutic effects o Including beta blocker eye drops o Tricyclic antidepressants and MAOIs potentiate effects of beta agonist on vascular system ADRs o Usually transient o Stopping the med is not usually needed, reduce dose then slowly increase o Supraventricular and ventricular ectopic beats have occurred o Tachycardia and palpitations o Some central nervous system (CNS) excitation effects o Tremors, dizziness, shakiness, nervousness, and restlessness o Headaches, rarely insomnia, post inhalation cough o Salmeterol has an increased risk of exacerbation of severe asthma symptoms if the patient is deteriorating o Overuse can lead to seizures, hypokalemia, anginal pain and HTN o Stimulant like effects o GI upset, take po meds with food Clinical Use and Dosing Bronchospasm • Bronchodilators are used primarily in the treatment of bronchospasm associated with asthma, bronchitis (acute or chronic), and chronic obstructive pulmonary disease (COPD) o Albuterol ▪ MDI dose children over 4 and adults is 2 puffs every 4 to 6 hours o Nebulizer dose children over age 12 and adults is 2.5 mg/dose ▪ For younger children over 15 kg, dose is 0.1 to 0.15 mg/kg/dose o Dose may be repeated once after 5 to 10 minutes, up to 2 times, three doses total during exacerbations o Oral dose in adults is 2 to 4 mg 3 or 4 times a day ▪ For children 6 to 12, 2 mg albuterol 3 to 4 times a day (PO form rarely used in children) ▪ Oral syrup: children under age 6, 0.1 mg/kg 3 times a day (rarely used) o May combine with ipratropium o Aformoterol (Brovana): nebulizer 15 mcg/ by inhalation BID (not approved for use in children) o Indacaterol (Arcapta Neohaler): powder via a Neohaler device ▪ adults with COPD, one capsule one daily with a Neohaler device o Levalbuterol (Xopenex): inhalation solution (nebulizer) in adolescents over age 12 and adults is 0.63 mg TID (every 6 to 8 hours) ▪ Children: 6 to 11: 0.31 mg TID, do not exceed 0.63 mg TID ▪ Children 4 and younger: 0.31 to 1.25 mg every 4 to 6 hours ▪ Inhaler: one to two puffs repeated every 4 to 6 hours o Metaproterenol (Alupent): MDI, inhalation solution, and syrup forms o Terbutaline: MDI (Brethaire), PO tablets (Brethine), or parenteral form for SC injection o Pirbuterol: only available as MDI (Maxair Autohaler) o Bitolterol (Tornalate): MDI: acute bronchospasm two puffs 1 to 3 minutes apart o Salmeterol (Serevent DISKUS): 1 puff BID o Do not use alone for persistent asthma, combine with an inhaled corticosteroid o Packaged with Fluticasone (Advair DISKUS) differing doses o Formoterol: 12 mcg, single use dry powder capsule o Ipratropium: inhaled anticholinergic, may be used in combination with albuterol to treat asthma exacerbation in the ER ▪ Bronchodilator of choice3 in patients taking beta blockers or who do not tolerate beta 2 agonists Exercise-induced bronchospasm (EIB) o Albuterol or other SABA and salmeterol o Albuterol MDI: 2 puffs 15 minutes before exercise, lasts 2-3 hours o Salmeterol: 2 puffs 30 to 60 minutes before exercise, duration 10 to 12 hours o Cromolyn or nedocromil may be used before exercise, not as effective o Leukotriene modifiers taken daily may decrease EIB symptoms in 50% of patients, but patient will still need to use albuterol before exercise Xanthine derivatives o Methylxanthines have declined in importance in the Tx of asthma, but some patients may still benefit from the use of theophylline o Theophylline and Caffeine o Bronchodilator Pharmacodynamics o Bronchial smooth muscle relaxation o CNS stimulants o CV effects o Increased gastric acid production o Stimulate skeletal muscle o Increased renal blood flow and GFR o Work directly by an unknown mechanism: mediated by selective inhibition of specific phosphodiesterase o Increased production of cAMP=bronchial smooth muscle and pulmonary vessel relaxation o Theophylline and caffeine: powerful CNS stimulants (insomnia and excitability) o Theophylline has a greater effect on the cardiovascular system o Theophylline directly stimulates the myocardium and increases myocardial contractility and HR o Relaxes vascular smooth muscle, dilates the coronary, pulmonary, and systemic blood vessels o Both theophylline and caffeine: increase gastric acid production (may cause NV) o Stimulate skeletal muscle: tremors o Theophylline: Acts directly on the renal tubules to cause increased sodium and chloride excretion o Both cause diuresis r/t action on the kidneys (increased blood flow to kidneys) Pharmacotherapeutics o Contraindications to theophylline: hypersensitivity to xanthine, PUD, and underlying seizure disorder o Contraindications to caffeine: hypersensitivity to caffeine or use of caffeine sodium benzoate formulation in neonates o Use Caution: HTN, ischemic heart disease, coronary insufficiency, CHF, or Hx of stroke and cardiac arrhythmias r/t effects on CV system o Toxicity: levels above 25 mcg/mL ▪ May occur if clearance is decreased (hepatic impairment, chronic lung disease, cardiac failure, patients older than 55, and infants under 1) o Theophylline: Pregnancy Category C, crosses placenta, newborns may have therapeutic serum levels if maternal levels are high-normal range (tachycardia, irritability, and vomiting) o May be used in children: infants younger than 1 have decreased theophylline clearance and closely monitor levels should be a range of 5 to 10 mcg/mL o Caffeine citrate is used to treat apnea of prematurity o Pregnancy Category C Theophylline: Drug and Food Interactions o Many drug interactions due to metabolism via CYP 450 isoenzyme CYP1A2, CYP2E1, and CYP 3A3/4 o Increase serum theophylline: allopurinol, VVs, CCBs, cimetidine, cipro, oral contraceptives, corticosteroids, disulfiram, ephedrine, flu vaccine, interferon, macrolides, quinolones, THs, carbamazepine, IZD, loop diuretics o Decrease serum theophylline: aminoglutethimide, barbiturates, charcoal, hydantoins, ketoconazole, rifampin, smoking, sulfinpyrazone, beta agonists, carbamazepine, isoniazid, loop diuretics, lansoprazole, primidone, ritonavir o Lithium: theophylline may increase renal clearance of lithium=reduced levels o Smoking tobacco increases theophylline clearance (may take months to 2 years to normalize theophylline clearance after quitting) o Benzodiazepines are antagonized by theophylline o Beta Blockers may cause additive toxicity o Elimination is effected by diet o Low-CHO/high-protein diet increases clearance (shortens half-life) o High in CHOs and low in protein decreases elimination (lengthens half-life) o Charcoal-broiled foods accelerate the hepatic metabolism of theophylline o Caffeine is metabolized by CYP1A2, CYP2E1, and CYP3A3/4 o Cimetidine, ketoconazole, fluconazole, mexiletine, and phenylpropanolamine (impair metabolism) o Caffeine elimination increased by phenobarbital and phenytoin ADR o Some patients have toxic effects at 15 to 20 mcg/mL (greater than 25 mcg/mL is toxicity) o CNS effects: irritability, restlessness, seizures, insomnia o GI effects: reflux, worsening heart burn o Cardiac effects: palpitations, tachycardia, hypotension, and life-threatening arrhythmias o Others: rash, diuresis, and tachypnea o Toxicity (greater than 20 mcg/mL): NVD, HA, insomnia, and irritability o Toxicity (greater than 35 mcg/mL): hyperglycemia, hypotension, cardiac arrhythmias, tachycardia, seizures, brain damage, and death o Caffeine: cardiac arrhythmias, tachycardia, insomnia, agitation, irritability, NA, NV, gastric irritation Clinical Use and Dosing Theophylline and COPD o Second or Third line drug for asthma and COPD o Recommended for long-term control of asthma and an “alternative, not preferred” therapy in step 2 of asthma care o Alternative treatment in combination with inhaled corticosteroids o Try LABA with ICS before theophylline r/t toxicity issues with theophylline o Dose for asthma and COPD based on weight and serum theophylline levels o Adult (16 and older) is started on 6 mg/kg/24 hours or 400 mg/24 hours o Dose is increased by 25% every 3 days until serum theophylline levels are 10 to 20 mcg/ml o Maximum dose 12-16 years old is 13 mg/kg/day and 10 mg/kg/day in healthy adolescents older than 16 and adults o The initial dose for children ages 5 or older is 16 mg/kg/day up to a maximum of 400 mg/day Apnea of Prematurity o Loading dose of caffeine citrate 10 to 20 mg/kg o Maintenance dose of 5mg/kg/day o If theophylline has been given to the patient in the previous 3 days. the loading dose is decreased by 50-70% o Theophylline: loading dose of 4 mg/kg/dose o Maintenance dose: 4 mg/kg/day o Total daily dose is divided and administered every 12 hours o Both drugs are equally effective in deceasing apnea spells in infants less than 33 weeks gestation Precautions and testing for xanthine derivatives o If serum concentration is between 10 to 15 mcg/mL, maintain dosage if tolerated and recheck at 6 to 12 month intervals o Check levels frequently until therapeutic range is met or adjusting doses (Q 3 days) o Monitor closely for s/s of toxicity o Check theophylline if a new medication is added to the treatment regimen or health status change o Levels need to be timed to measure peak levels of the drug o A serum theophylline level should be drawn 1 to 2 hours after immediate release formulas and 5 to 9 hours after sustained-release formulas o Check when changing brands (bioavailability varies) o Contraindications to theophylline: hypersensitivity to xanthine, PUD, and underlying seizure disorder o Contraindications to caffeine: hypersensitivity to caffeine or use of caffeine sodium benzoate formulation in neonates o Use Caution: HTN, ischemic heart disease, coronary insufficiency, CHF, or Hx of stroke and cardiac arrhythmias r/t effects on CV system o Toxicity: levels above 25 mcg/mL ▪ May occur if clearance is decreased (hepatic impairment, chronic lung disease, cardiac failure, patients older than 55, and infants under 1) o Theophylline: Pregnancy Category C, crosses placenta, newborns may have therapeutic serum levels if maternal levels are high-normal range (tachycardia, irritability, and vomiting) o May be used in children: infants younger than 1 have decreased theophylline clearance and closely monitor levels should be a range of 5 to 10 mcg/mL o Caffeine citrate is used to treat apnea of prematurity Inhaled Anticholinergics o Drugs: ipratropium bromide (Atrovent), ipratropium with albuterol (Combivent), tiotropium bromide (Spiriva), and aclidinium bromide (Tadorza Pressair) o Treatment of COPD o Cause bronchial smooth muscle relaxation (bronchodilator) o Ipratropium may be used in combination with albuterol as the emergent Tx of an asthma exacerbation or when a patient is intolerant to B2Ras o Second-line bronchodilators for asthma and COPD o Use a spacer device and rinse mouth with water after administration to help decrease the incidence of ADRs Pharmacodynamics o Action of each drug is similar o Ipratropium: blocks the muscarinic cholinergic receptors by antagonizing the action of acetylcholine, this decreases the formation of cGMP, which leads to decreased contractility of the smooth muscle of the lungs (action of cGMP on intracellular calcium) o When inhaled ipratropium’s actions are confined to the mouth and airways o Tiotropium and aclidinium bromide: inhibit the muscarinic M3 receptors in the lungs (smooth muscle bronchodilation) Pharmacotherapeutics o Contraindication: hypersensitivity to atropine or atropine derivatives and those with bromide sensitivity o Patients with milk protein hypersensitivity should not be prescribed aclidinium bromide o Tiotropium: contraindication in patients with hypersensitivity to ipratropium or tiotropium o The inhaled anticholinergics (aclidinium, ipratropium and tiotropium), should not be used for the treatment of acute bronchospasms (except ipratropium mixed with albuterol) o Avoid in patients with urinary retention, bladder neck obstruction, or prostatic hypertrophy r/t anticholinergic effects o May increase intraocular pressure in patients with closed-angle glaucoma o Ipratropium bromide is Pregnancy Category B o Aclidinium and tiotropium and Pregnancy Category C o Safety and effectiveness of ipratropium in children under age 12 have not been established o May use in younger children as an adjunct to beta agonist (albuterol) therapy in acute exacerbations of asthma o Aclidinium and tiotropium are only approved for COPD, safety in children not established ADRs o Ipratropium: most common ADR is cough o Hoarseness, throat irritation, and dysgeusia o NV and dyspepsia (r/t anticholinergic effects constipation and urinary retention), and xerostomia (dry mouth) o Inhaled tiotropium (Spiriva HandiHaler): dry mouth is the most common ADR o Mouth irritation, pharyngitis, nasal congestion, sinusitis, HA, and URI o Aclidinium: HA most common ADR o Nasopharyngitis, cough, and rhinitis o Anticholinergic effects: urinary retention, dizziness, drowsiness, and constipation o Urinary retention is increased with the use of inhaled anticholinergics, particularly patients with BPH o If Ipratropium is sprayed in the eyes, may experience temporary eye irritation, pain, mydriasis, blurred vision, cycloplegia (paralysis of the ciliary muscle), irritant conjunctivitis, and visual disturbances o Rare allergic and anaphylactoid reactions may occur o Urticaria, maculopapular rash, bronchospasm, pruritis, laryngospasm, oropharyngeal edema, and angioedema of the tongue, lips, and face o Use with caution in patients with Hx of sensitivity to other drugs and soybeans, legumes, or soy lecithin appears to be correlated with hypersensitivity to ipratropium bromide o Patients with milk protein hypersensitivity should not be prescribed aclidinium bromide Drug Interactions o Ipratropium and tiotropium are minimally absorbed into systemic circulation after inhalation, no major drug interactions o Do not mix cromolyn sodium and ipratropium bromide via nebulizer because a precipitate will form Clinical Use and Dosage COPD o Ipratropium MDI: 18 mcg/spray: Two inhalations (36 mcg) 4 times a day (total of eight sprays/day) o If needed may take up to 12 puffs/day (maximum of 216 mcg/24 hours) o Ipratropium Nebulizer: one unit dose vial (500 mcg) 3 to 4 times/day via nebulizes, doses are 6 to 8 hours apart o Ipratropium may be mixed with albuterol (must be used within 1 hour) o Aclidinium bromide (Tadorza Pressair): inhalation powder administered via inhaler, 400 mcg/spray o One inhalation BID o Tiotropium (Spiriva) is a dry powder capsule given via HandiHaler device o Two inhalation of a single 18 mcg capsule once daily o Ipratropium/albuterol combination (Combivent): second-line use for patients with COPD o 2 puffs QID o Prescribed for patients already on a bronchodilator who continue to have bronchospasms who may benefit from a second bronchodilator o Each inhalation is 103 mcg of albuterol sulfate and 18 mcg of ipratropium bromide Two inhalations four times a day o May take addition inhalations must not exceed 12 inhalations in 24 hours o Very economical for patients who need both meds Asthma o Ipratropium for asthma maintenance is two to three inhalations 4 times a day o Should not be used for EIA o For children under 12, one or two inhalations every 6 hours o Ipratropium solution: o Adults 250 mcg via nebulizer four times a day o Children under 12 is 250 to 500 mcg every 8 hours o Infants are dosed at 125 to 25o mcg three times a day o Acute exacerbation of asthma: ipratropium mixed with albuterol o Ipratropium/albuterol (Combivent): second-line quick relief mediation in asthma o 103 mcg of albuterol sulfate and 18 mcg of ipratropium bromide o Dose in adults two to three inhalations four times a day o Children under 12 one to two inhalations every 6 hours o Nebulizer solution of albuterol (2.5 mg/3 mL) and ipratropium (0.5 mg/3 mL) o 3 mL every 4 to 6 hours for adults o Children under 12: 1.5 to 3 mL every 8 hours Leukotriene Modifiers o Induces numerous effects that contribute to inflammatory process o Smooth muscle contractions o Decrease inflammation o Leukotriene-receptor agonists (LTRAs) and 5-lipoxygenase pathway inhibitors were developed under the theory that cysteinyl leukotriene play a significant role in the chronic inflammation associated with asthma and allergy o Leukotrienes induce numerous effects that contribute to the inflammatory process (smooth muscle contractility, neutrophil aggregation, degranulation, and chemotaxis, vascular permeability, and lymphocytes o Drugs for use in asthma: zafirlukast (Accolate), zileutin (Zyflo, Zyflo CR), and montelukast (Singular) Pharmacodynamics Leukotriene-Receptor Agonists (Zafirlukast and Montelukast) o Zafirlukast: synthetic, selective, and competitive LTRA of leukotriene D4 and E4 o Have been identified as component of slow reacting substance of anaphylaxis o Montelukast: selective LTRA that inhibits cysteinyl leukotriene receptor (CysLT1) o Binds with high affinity and selectivity to the receptor (CysLT1) o Evidence that cysteinyl leukotriene contribute to the pathophysiology of asthma and allergy o Contribute to: Airway edema, smooth muscle constriction, and cellular changes associated with inflammatory process 5- Lipoxygenase Pathway Inhibitors (Zileuton) o Zileuton in an inhibitor of 5-lipoxygenase (enzyme that catalyzes the formation of leukotrienes from arachidonic acid o By inhibiting 5-lipoxygenase zileuton inhibits the formation of LTB4, LTC4, and LTE4 (component of slow reacting substance of anaphylaxis) Pharmacotherapeutics o Do not use for primary treatment of an acute asthma attack Contraindications: o Hypersensitivity to any of the components of the medication o Chewable montelukast: phenylketonuria the product contains phenylalanine o Zileuton Contraindicated in patients with active liver disease o Zafirlukast: use with caution in patients with hepatic dysfunction r/t extensive metabolized by the liver o In ETOH cirrhosis, clearance of zafirlukast is reduced 50-60% o No dose adjustment with montelukast in patients with mild to moderate hepatic insufficiency because elimination is only slightly prolonged o Avoid in patients with severe liver disease o Should not be abruptly substituted for inhaled or oral steroids o Use caution as systemic corticosteroids are reduced o Reports of eosinophilia, vasculitis rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting as Chur-Strauss syndrome (systemic eosinophilic rash o Neuropsychiatric events have been reported in adults, adolescent, and pediatric patients o Agitation, aggression, anxiousness, dream abnormalities, hallucinations, depression, insomnia, irritability, restlessness, suicidal thinking, and behavior (including suicide), and tremor o Sleep disorders o Zafirlukast and montelukast are Pregnancy Category B o Zileuton is Pregnancy Category C o Safety and efficacy of zafirlukast has been established in children 5 and older o Montelukast may be prescribed for children as young as 12 months for chronic asthma o The safety and effectiveness of Zileuton in pediatric patients younger then 12 has not been established o Caution in lactating women: effects on infants are unknown ADRs o Zafirlukast: most common ADR is HA o GI upset, myalgias, and fever (small percentage of patients) o Respiratory infections in patients older than 55 taking zafirlukast o Mild to moderate infections associated with coadministration of inhaled corticosteroids o Zileuton: dyspepsia o Hepatic injury, including hepatitis and death, with patients exhibiting elevated ATL Drug Interactions o Zafirlukast: use with caution with any drug that is metabolized by CYP2C9 and CYP3A3/4 ▪ ASA: 45% increase in plasma zafirlukast ▪ Erythromycin 40% decrease in plasma zafirlukast levels ▪ Terfenadine: decreased plasma zafirlukast ▪ Warfarin and zafirlukast: clinically significant increase in PT o Montelukast: CYP2A6, CYP2C9, and CYP3A3/4 (phenobarbital, rifampin) o Zileuton: CYP3A4 ▪ Zileuton and theophylline: may elevate theophylline levels ▪ A reduction of the theophylline dose by 50% is recommended ▪ Terfenadine is increased and clearance reduced when administered with zileuton ▪ Warfarin: increased PT ▪ Propranolol: Increased propranolol concentration Clinical Use and Dosing o Zafirlukast: treatment of chronic asthma in children aged 5 years and older and adults ▪ 20 mg BID in children 12 years and older and adults ▪ 10 mg BIG for children 5-11 ▪ Take on an empty stomach o Montelukast: treatment of persistent asthmas for patients aged 12 months or older ▪ May be prescribed for the prevention of exercise induced bronchoconstriction, in adolescents age 15 years or older and adults ▪ May be used to treat seasonal allergic rhinitis in patients 2 years or older and perennial allergic rhinitis in patients 6 months and older ▪ Adults dose (15 years and older): 10 mg once a day in the evening ▪ Children 6-14: 5 mg once a day in the evening ▪ Children 2 to 5: 4 mg once daily in the evening ▪ 12 to 24 months: 4 mg oral granules ▪ Can be taken without regard to food ▪ Dosed the same for allergy as for asthma o Zileuton: treatment of persistence asthma in children aged 12 years and older and adults ▪ 600 mg 4 times a day or two 600 mg ER tablets BID ▪ Take 1 hour after meals Respiratory Inhalants: Inhaled Corticosteroids o Drugs: beclomethasone dipropionate (QVAR), triamcinolone acetonide (Azmacort), budesonide (Pulmicort), flunisolide (AeroBid), mometasone furoate (Asmanex Twisthaler), fluticasone (Flovent), and ciclesonide (Alvesco) o Long-term drug of choice in pregnancy o Most potent and effective anti-inflammatory medication currently available o Reduce severity of asthma symptoms, increase peak flow readings, and decrease airway hyperresponsiveness o Safe and well tolerated at recommended dosages o Preventative therapy, not rescue therapy o Generally safe and well tolerated and can be used by children and adults o Can be used intranasally for allergic rhinitis o Beclomethasone (Beconase), triamcinolone (Nasacort AQ), budesonide (Rhinocort Aqua), flunisolide (Nasalide, Nasarel), mometasone (Nasonex), fluticasone (Flonase), and ciclesonide (Omnaris) o Rinse mouth after use to avoid oral candidiasis o May take 3 to 7 days for effects to start o An expert panel does not recommend one ICS over another: choice based on ease of dosing, indications, and ADRs o No generic equivalent formulas o Monitor blood glucose, K, and growth in young children o If using a bronchodilator and an ICS: Use the bronchodilator first and wait several minutes before using the ICS: enhances the absorption of the steroid Pharmacodynamics o Primary actions are anti-inflammatory o Inhibit IgE and mast-cell mediated migration of inflammatory cells into the bronchial tissue (last-phase allergic reaction) o Relax smooth muscle: MOA unknown o Intranasal corticosteroids apply topical and local anti-inflammatory effects without any systemic effects Pharmacotherapeutics o Contraindication: Acute status asthmaticus or when intensive acute therapy is warranted o Not used for relief of acute bronchospasm o Use caution when substituting any of the ICS for oral corticosteroid therapy ▪ Deaths have been reported due to adrenal insufficiency in asthmatic patients who were switched from oral to inhaled corticosteroids ▪ Avoid in Cushing’s syndrome o Use with caution with ocular herpes simplex infections, TB, oral or nasal surgery or trauma, healing nasal septal ulcers, and untreated respiratory infections (viral, fungal, or bacterial) o All are Pregnancy Category C: no well controlled studies o High dose in children may inhibit growth but so can poorly controlled asthma ▪ Closely monitor growth o Triamcinolone: do not prescribe to children under 6 (safety and efficacy not established) o Budesonide: can be used in children as young as 6 months o Fluticasone: use with caution to children under 4, can inhibit growth o Mometasone nasal spray: may be prescribed for children as young as 2, but oral inhalation powder for asthma has not been established for children younger than 12 o Flunisolide: not for use under age 6 o Ciclesonide (Omnaris): safe and effective in children 6 and older o Inhaled ciclesonide (Alvesco), safe but not effective in children younger than 12 Drug Interactions o No known drug interactions with inhaled triamcinolone, flunisolide, mometasone, beclomethasone, or ciclesonide o Ritonavir: significantly increases fluticasone and may lead to increased corticosteroid effects o Ketoconazole: increased concentration of fluticasone and budesonide ▪ Due to CYP3A4 o Monitor for corticosteroid related side effects if co-administered with drugs known to inhibit CYP3A4 ▪ Anastrozole (Arimidex), delavirdine (Rescriptor), erythromycin, fluconazole (Diflucan), fluoxetine (Prozac), itraconazole (Sporanox) mibefradil, nefazodone, nelfinavir, ritonavir, and zileuton ADRs • Xerostomia, hoarseness, tongue and mouth irritation, flushing, dysgeusia (altered taste sensation) and dysmenorrhea • Less common: oral candidiasis, cataracts bronchospasm, HPA suppression, pulmonary infiltrates with eosinophilia, nasal irritation, itching, sneezing, and dryness, bloody nasal mucus or epistaxis Clinical Use and Dosing Asthma o Inhaled corticosteroids are the preferred long term control medications for managing the inflammatory process associated with asthma o Dosages vary with the specific produce and delivery method o Mild persistent asthma: start on a low dose of inhaled corticosteroids (ICS) ▪ Children older than 12 may be treated with cromolyn, nedocromil, leukotriene modifiers, or theophylline as alternative therapy o Moderate persistent asthma: daily low to medium dose ICS combined with an LABA ▪ Alternative Tx: medium dose ICS or a combination of low to medium dose ICS and a leukotriene modifier o Severe persistent asthma: daily high dose inhaled corticosteroid and LABA o Children with persistent asthma require daily anti-inflammatory therapy o Young children with mild persistent asthma: started on step 2 therapy, a low dose inhaled corticosteroid (via neb or MDI) with an alternative therapy being cromolyn or montelukast o Child with moderate persistent asthma: low dose ICS combined with montelukast or LABA ▪ The alternative treatment for a LABA would be medium dose ICS or low dose ICS combined with a leukotriene modifier (montelukast) o Child with severe persistent asthma: High dose inhaled steroids combined with a LABA or montelukast Allergic Rhinitis o Nasal corticosteroids are used to manage the inflammatory response associated with seasonal or perennial allergies o May be used 1-2 times daily Inhaled Anti-Inflammatory Agents • Drugs: cromolyn sodium and nedocromil (only available as ophthalmic solution) • Cromolyn: synthetic compound that inhibit antigen induced bronchospasms, block the release of histamine, and stabilize mast cells • Used in the treatment of asthma and (Nasalcrom) used to treat allergic rhinitis Pharmacodynamics • Inhibits mast cell degranulation which prevents the release of histamine and slow reacting substance of anaphylaxis • Prevents the release of leukotrienes • With continued use, reduces bronchi hyperreactivity to stimuli such as cold air, allergens, and environmental irritants Pharmacotherapeutics • Contraindicated in the treatment of acute bronchospasm or status asthmaticus • Pregnancy Category B and should be used with caution in lactating mothers • Safe for use in children as young as 2 ADRs • Generally, well tolerated • Inhaled cromolyn may cause bronchospasm which can be avoided by pre-administering a beta agonist bronchodilator • Throat irritation and cough • Intranasal: may produce nasal irritation and cause sneezing Drug Interactions • No clinically significant drug interactions • Nebulizer solution will form a precipitate if mixed with ipratropium solution Clinical Use and Dosing Asthma • Alternative long term control drug for the treatment of mild persistent asthma • Available in inhaled form and nebulizer solution • Cromolyn MDI for children older than 5 and adults: 2 sprays inhaled QID at regular intervals • Cromolyn Nebulizer: one ampule (20 mg) QID at regular intervals • May be decreased after the patient is stabilized (usually after 4 weeks) to two or three doses a day • If used concurrently with bronchodilators, the bronchodilator should be administered first • May be mixed with albuterol in a nebulizer cup to simplify dosing • Effectiveness depends on using it regularly • Oral cromolyn: used for systemic mast-cell disease (Mastocytosis) and IBD o Mastocytosis: o 200 mg of Gastrocrom oral concentrate 4 times a day in adults o 100 mg 4 times a day in children 2 to 12 • Adult dosing for IBD is 200 mg QID of Gastrocrom, may be doubled if not responding after 2 to 3 weeks to 400 mg QID • Children aged 2 to 12 with IBD dosed at 100 mg QID , dose may be doubled but should not exceed 40 mg/kg/day Bronchospasm Prophylaxis • Exercise induced bronchospasm or individuals who have bronchospasm with known precipitating factors (pets) • Cromolyn MDI for children 5 years or older and adults: 2 inhalations 10 to 15 minutes before exercise • If exercise is prolonged, the dose may be repeated • Cromolyn nebulizer dosing in children aged 2 years and older and adults: one ampule via neb not more than 1 hr prior to exercise • For maximum effectiveness, the time between the use of inhaled cromolyn sodium and exercise should be as brief as possible Allergic Rhinitis • Cromolyn sodium nasal inhalation spray in children aged 6 years and older and adults is one spray in each nostril 3 to 4 times a day • Dose may be increased to 6 times a day if needed • Two to four weeks of therapy may be needed to produce relief from perennial rhinitis Inhaled Antihistamines • Drugs: azelastine (Astelin, Astepro) and olopatadine (Patanase) • Azelastine and olopatadine are the intranasal H1 blockers in the US • Used to treat seasonal allergic rhinitis and vasomotor rhinitis Pharmacodynamics • Azelastine is an H1 agonist and potent inhibitor of histamine release from mast cells • Azelastine and its metabolite desmethylazelastine inhibit the effects of histamine by competing with histamine for H1 binding sites • Azelastine may also interfere with histamine and leukotriene induced bronchospasm • Olopatadine is a selective H1 receptor antagonist Pharmacotherapeutics • Some patients may experience somnolence and should be cautioned not to drive or operate heavy equipment while using it • Should not use ETOH or other CNS depressants while using azelastine • Olopatadine is contraindicated in patients with nasal diseases other than allergies • Avoid spraying in eyes • Pregnancy Category C • Azelastine: safety in children under age 5 not established • Olopatadine: safety in children under age 12 not established ADRs • Most common ADR to azelastine is bitter taste o Somnolence, HA, weight gain, and myalgia o Local effects: nasal irritation, epistaxis, sneezing, and rhinitis • Olopatadine: bitter taste, HA, and epistaxis Drug Interactions • Azelastine: Additive CNS depression when taken with other CNS depressants • Azelastine should be used cautiously with other antihistamines • Theoretical additive CNS depression when olopatadine is administered with other CNS depressants or ETOH Clinical Use and Dosing Allergic Rhinitis • Azelastine is approved for use in seasonal allergic rhinitis o Used to treat rhinorrhea, sneezing, and nasal pruritus o Two sprays (137 mcg/spray) per nostril BID o Children 5-12: one spray per nostril BID • Olopatadine: two sprays in each nostril BID in children older than 12 and adults Oxygen • Basic element essential for human life, deprivation leads to death • Therapy with O2 is needed for life in several disease that interfere with normal oxygenation of blood and tissues • Delivered from steel containers and is 99% pure Pharmacodynamics • Prescribed to treat hypoxia, or tissue deprivation of oxygen • Hypoxia from inadequate supply of oxygen to the lungs due to poor ventilation or inadequate partial pressure of inspired O2 • VQ mismatch, low cardiac output, or anemia Pharmacotherapeutics • Contraindication: concurrent smoking while oxygen is running, flammable gas and will ignite • Should be Rx to patients with chronic carbon dioxide retention with extreme caution and close monitoring • Hypoxemia may be the primary stimulus for respiratory in these patients, the lowest possible concentration of O2 to avoid serious tissue hypoxia should be used • In patients with hypercapnia, the sudden increases in PaCO2 produced by oxygen may result in cessation of respiration ADRs • Most common: dry nasal passages (humidified O2 by mask or keeping flow rate low, less than 5 to 6 L/min) • Toxicity: occurs when inspired concentrations of O2 exceed those of air for prolonged periods of time o Cell membrane damage and death are thought to be caused by increased production of reactive species such as superoxide anion, singlet oxygen, hydroxyl radical, and hydrogen peroxide o The respiratory tract, CNS, and retina are sensitive to high oxygen concentration Drug Interactions: There are no drug interactions with O2 Clinical Use and Dosing • Administered to treat hypoxia as determined by pulse oximetry or arterial or mixed venous blood gases • Usually a symptom or manifestation of an underlying disease, not curative, provides symptomatic and temporary improvement • Underlying cause needs to be treated Correction of Hypoxia • Delivered via a variety of systems • Delivery system based on the fraction or percentage of oxygen (FIO2) that is desired for treatment • Goal of treatment is to maintain O2Sat above 90% • NC will deliver an FIO2 of 0.24 to 0.35 if the flow of oxygen is at 5 to 6 L o Higher flow rates via NC dry out nasal mucosa and will not achieve higher FIO2 o Percentage of O2 is 22-44% • Masks: allow for a higher concentration of O2 o Flow rate above 5 L, flow rate of 8 to 10 L is recommended • Simple face mask (allows room air to dilute the O2) delivers 40 to 60 % oxygen • A face mask with an oxygen reservoir provides a constant flow of oxygen at above 60% concentration • Venture mask allows for controlled percentages of oxygen to be delivered can be adjusted o Used on patients with chronic hypercapnia (COPD) to tightly control the amount of oxygen delivered and avoid respiratory depression associated with high oxygen concentrations in these patients • Hood or tent-unknown concentration o Flow rates must be high enough to prevent accumulation of carbon dioxide Chapter 30: Asthma and COPD Diagnosis and classification of asthma • Diagnosis: • Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role: in particular, mast cells, eosinophils, neutrophils (especially in sudden onset, fatal exacerbations, occupational asthma, and patients who smoke), T lymphocytes, macrophages, and epithelial cells. • According to the American Lung Association: spirometry, health Hx, physician exam, allergy testing, exhaled nitric oxide or FeNO test, challenge tests (methacholine). • According to the Asthma and Allergy Foundation of America: medical Hx, physical exam, lung function tests, chest, or sinus x-ray. LFTs: spirometry, peak airflow, FeNO tests, provocation tests. • Spirometry is used as the most definitive diagnostic tool: test is performed before and after a SABA and results compared. Spirometry also measures reactivity. • Classification of asthma in children 12 years or older and adults: • 1. Mild intermittent asthma: Symptoms occur less often than twice a week and the patient are asymptomatic between exacerbations; nighttime symptoms occur less than twice a month; and peak expiratory flow (PEF) is greater than 80% predicted. The use of short-acting beta2 agonists (SABA) should be less than twice a week, unless used for exercise-induced bronchospasm (EIB). • 2. Mild persistent asthma: Symptoms occur more often than twice a week but less often than once a day and exacerbations may affect activity; nighttime symptoms occur 3 to 4 times a month; and PEF is greater than 80% predicted. Patients with mild persistent asthma may use their short-acting beta2 agonists more than twice a week but not daily, and not more than once daily. • 3. Moderate persistent asthma: The patient is having daily symptoms; requires daily use of a beta2 agonist; exacerbations affect normal activity; nighttime symptoms occur more often than once a week; and PEF is greater than 60% to less than 80%. • 4. Severe persistent asthma: The patient has some degree of symptoms all the time; extremely limited physical activity and frequent exacerbations; frequent nighttime symptoms, often 7 days a week; and decreased lung function (PEF less than 60% predicted). Table 30-1 Pg. 916 outlines the classifications of asthma severity in patients aged 12 years or older. In children: classification of asthma is based on severity and frequent of symptoms • 1. Mild intermittent asthma: Symptoms occur less often than twice a week and the patient are asymptomatic between exacerbations. Children aged 0 to 4 years have no nighttime symptoms, and children aged 5 to 11 years have nighttime symptoms less than twice a month and PEF are greater than 80% predicted. The use of short-acting beta2 agonists should be less than twice a week, unless using for EIB. Exacerbations requiring oral systemic corticosteroids occur no more than once a year. • 2. Mild persistent asthma: Symptoms occur more often than twice a week but less often than once a day and exacerbations may affect activity. In children aged 0 to 4 years, nighttime symptoms occur 1 to 2 times a month, and in children aged 5 to 11 years, nighttime symptoms occur 3 to 4 times a month; PEF is greater than 80% predicted. Patients with mild persistent asthma may use their short-acting beta2 agonists more than twice a week but not daily, and not more than once daily. Children younger than age 4 years with mild persistent asthma have more than two exacerbations in 6 months requiring systemic steroids or four episodes of wheezing in a year lasting more than a day and risk factors for persistent asthma. Children aged 5 to 11 with mild persistent asthma have exacerbations 2 or more times a year. • 3. Moderate persistent asthma: The child is having daily symptoms; requires daily use of a beta2 agonist; and exacerbations affect normal activity. In children aged 4 years or younger, nighttime symptoms occur 3 or 4 times a month, and in children aged 5 to 11 years nighttime symptoms occur more than once a week but not nightly; PEF is greater than 60% to less than 80%. Children with moderate persistent asthma have exacerbations 2 or more times a year. • 4. Severe persistent asthma: The patient has some degree of symptoms all the time; extremely limited physical activity; frequent nighttime symptoms (more than once a week in children younger than age 4 years and in older children often occurring 7 days a week); and decreased lung function (PEF less than 60% predicted). Children aged 5 to 11 with severe persistent asthma have exacerbations 2 or more times a year. Risk factors for fatal asthma attacks • Those having previous severe exacerbations requiring intubation or ICU, two or more hospitalizations or more than 3 ER visits in the last years, use of more than 2 SABA canisters per month, difficulty perceiving airway obstruction or worsening asthma, or low socioeconomic status or inner city residence Asthma step therapy and goals of step therapy Step therapy: • Stepwise approach to the pharmacological management of asthma • Can begin at a higher level and gradually step down or start low and move up, depending on the patient’s status when beginning treatment • Medications categorized into two general classes: long term control medications to achieve and maintain control of persistent asthma and quick relief medications to treat acute symptoms and exacerbations • Asthma severity determines the amount and frequency of medication, with suppression of airway inflammation the goal • Patient cooperation in keeping an asthma symptoms log is important • Patient self-assessment: enables provider to track the effectiveness of therapy and make treatment decisions based on medication use, nighttime symptoms, and PEF • Individualize therapy based on individual circumstances and response to therapy • Requires ongoing monitoring to assess degree of control • Mild intermittent Asthma: Step 1: Treatment with SABA as needed for symptoms (triggers, EIA, and infants and children who wheeze with viral URIs, exercise can be mild intermittent, need an annual flu shot • Mild Persistent Asthma: Step 2: one long term control medication daily, primary treatment is inhaled anti- inflammatory medications. Treatment is started with inhaled low dose corticosteroids (ICS) for all ages o Suggested beginning dose of inhaled steroids is 80 to 240 mcg/day of beclomethasone HFA (QVAR) or 180 to 600 mcg/day of budesonide (Pulmicort Turbuhaler) or equivalent o Alternative therapy: sustained release theophylline to serum concentrations of 5 to 15 mcg/mL (monitor closely) o Inhaled SABA: used as needed to relieve symptoms, if using 2 or more days per week, step up in therapy o If symptoms persist, ICS should be increased to 240 to 480 mcg/day of beclomethasone (QVAR) (three to six puffs/day of 80 mcg/puff or equivalent o If patient requires daily Beta agonists and is using the meds correctly then step 3 therapy is indicated o Alternative to ICS: ▪ Mast cell stabilizers cromolyn (Intal) and nedocromil (Tilade) • Especially useful in EIB or mild persistent asthma • Take weeks to reach full effectiveness for asthma ▪ Leukotriene modifiers: montelukast (Singular), zafirlukast (Accolate) and zileuton (Zyflo) • Moderate Persistent Asthma: Step 3: Long term preventive medication to maintain control of asthma o Medium dose ICS: 240 to 480 mcg of beclomethasone (3 to 6 puffs/day of 80 mcg/puff) o or low-dose ICS combined with a LABA (Advair) ▪ The long acting beta agonist salmeterol (Serevent) should not be Rx without the concurrent use of ICS because of increased risk of catastrophic events (asthma related intubations and death o Quick relief of symptoms with SABA o More severe exacerbation may require oral corticosteroids o If control of symptoms is not achieved and the patient is adhering to the plan, increasing to step 4 is indicated o Keeping a record of medication use and symptoms is critical at this step o Referral to an asthma specialist is indicated if thew patient needs step 4 therapy • Severe Persistent Asthma: Requires step 4, 5, or 6 therapy o Step 4 (Refer to an asthma specialist) ▪ Daily medium dose ICS (240 to 480 mcg/d of beclomethasone or equivalent ▪ Plus LABA (arformoterol, formoterol, indacaterol, and salmeterol) ▪ Alternative: medium dose ICS and a leukotriene modifier or theophylline o Step 5 ▪ Daily high dose ICS combined with daily LABA ▪ ICS: high dose, greater than 480 mcg of beclomethasone (more than 6 puffs/d at 80 mcg/puff) o Step 6 ▪ High dose ICS combined with daily LABA and oral corticosteroids ▪ If long term oral corticosteroids are required use lowest dose possible • Doses 2 mg/kg/d, not to exceed 60 mg/day ▪ ICS are preferable to systemic corticosteroids and the maximum dose should be used before long term systemic therapy is initiated ▪ Exacerbations require short bursts of high dose systemic corticosteroids o Step 5 or step 6: ▪ If associated with allergies may benefit from omalizumab (Xolair) ▪ Binds to free IgE and prevents them from responding to relevant allergens ▪ Administered every 2 to 4 weeks via SQ ▪ Has demonstrated reduced exacerbations and total ER visits Goals of therapy: • Reduce Impairment 1. Prevent chronic and troublesome symptoms (coughing or breathlessness in the night, in the early morning, or after exertion) 2. Require infrequent use (less than twice a week) of inhaled SABA for relief of symptoms (not including use for EIB) 3. Maintain (near) “normal” pulmonary function 4. Maintain (near) normal activity levels 5. Mett patients’ and families’ expectations of and satisfaction with asthma care • Reduce Risk 1. Prevent recurrent exacerbations of asthma and minimize the need for emergency department visits or hospitalizations 2. Prevent loss of lung function, for children, prevent reduced lung growth 3. Provide optimal pharmacotherapy with minimal or no adverse effects COPD therapy and goals of treatment • Goal of Therapy: Slow the disease process and maintain quality of life • Rational drug selection: • Maintenance monotherapy: LABA, long acting inhaled muscarinics (inhaled anticholingeric), or ICS • Bronchodilators • Treat the reversible component of COPD to maximize airflow by relaxing the airway smooth muscle and improving lung emptying during tidal breathing • Beta 2 agonists: mainstay, SABA for acute symptomatic relief • LABA as monotherapy or in combination with an Anticholinergic or ICS • LABA: salmeterol (Serevent) or formoterol (Preformist) can be Rx singly or in combination with an ICS (Advair or Symbicort) or long acting muscarinic antagonist (Tiotropium) • Use albuterol (SABA) and ipratropium (anticholinergic) together • ULABA: once daily when combined with a long acting muscarinic antagonist, the benefit is additive, resulting in improved respiratory symptoms • Anticholinergic drugs • Ipratropium bromide (Atrovent) and tiotropium (Spiriva), Acridinium bromide (Tudorza Pressair) • Reduce volume of sputum without changing the viscosity and bronchodilation • Drugs of choice for COPD • Spiriva: long acting muscarinic antagonists (LAMA): dry powder once daily • Reduces exacerbations and hospitalizations • Combining albuterol and ipratropium (Combivent) or formoterol and tiotropium (Symbicort) produces a greater change in spirometry over 3 months • Combination therapy for COPD if FEV1 is less than 60% of predicted • More convenient and economical • Albuterol and ipratropium are available in solution for nebulizer (DuoNeb) • Acridinium bromide (Tudorza Pressair): recently approved LAMA for COPD, dry powder BID • Methylxanthines (theophylline) • Second line drug, low dose theophylline reduces exacerbations of COPD • Risk for toxicity • Corticosteroids • Nonspecific anti-inflammatory activity • Effects are less dramatic in COPD than in asthma • Daily ICS has mixed results • Decrease exacerbations of COPD and improve health status • Start on moderate to high dose ICS • Combo therapy of ICS and LABA such as Advair (salmeterol/fluticasone) is more effective in decreasing exacerbations • Slow onset of action, rinse mouth after ICS, reports of pneumonia • Oral corticosteroids are useful in short term treatment of acute COPD exacerbations • Prednisone 30 to 40 mg/day x 10 days Respiratory drug interactions with digoxin • Beta 2 Receptor Agonists (B2Ras) o Albuterol: digoxin serum levels may be decreased, decrease dose of albuterol may be needed o Levalbuterol: digoxin levels may be decreased, decreased dose of albuterol may be needed Patient education for treatment of asthma • Mild intermittent: introducing the patient and family to the use of medication and teaching them about asthma, proper inhaler technique if appropriate, care during exacerbation of symptoms, and environmental controls to known allergens • Mild persistent: self-monitoring and developing and reviewing the self-management plan • Written asthma action plan: discussion of overall treatment plan, specific to drug therapy, reasons for taking the drugs, drugs as part of the total treatment regimen, and adherence issues • Establish and maintain a partnership • Asthma education is cost effective and can reduce morbidity for both adults and children Use of oral corticosteroids in the treatment of COPD and asthma • Temporary increase in anti-inflammatory therapy may be needed to reestablish control or treat exacerbations • Need for oral steroids is characterized by increased need for SABA or decreased PEF (20% or greater), reduced tolerance to activity, and increased nocturnal symptoms • A short burst of oral prednisone is often effective o Adults: 40 to 60 mg/d single or divided BID x 5 to 10 days o 1 to 2 mg/kg in children to maximum of 60 mg/day x 3 to 10 days • If the steroid is successful the PEF returns to normal and symptoms improve, no other treatment needed • If the steroid is not successful, then a step up to a higher level is indicated • If frequent bursts of steroids are required, then higher level care is needed Chapter 42: Pneumonia Etiology, diagnosis, classification, and risk factors • Pneumonia affects more than 5 million people a year in the United States, making it one of the more commonly seen medical problems and the eighth leading cause of death in the United States • Pneumonia develops when an organism invades the lung parenchyma, and the host defenses are depressed. o Chronically ill patients of all ages are more prone to pneumonia, usually because of their underlying medical problem. • There may be other origins of pneumonia besides bacterial organisms, such as viral, fungal, rickettsial, and parasitic organisms; inflammatory processes; and inhalation of toxic substances. • Pneumonia should be considered in any patient who presents with respiratory symptoms such as cough, dyspnea, or sputum production o Fever or abnormal breath sounds (crackles) would strengthen the suspicion • Chest radiographs assist in confirming the Dx of pneumonia versus other respiratory disorders (r/o lung abscess or TB) o Diagnostic testing has limitations therefore CAP is treated empirically • Predominant organism depends upon the patients age and health status • All ages (except neonates) Streptococcus pneumoniae is the organism most commonly found in pneumonia (60-75% of adults confirmed via sputum culture) o Non-typeable Haemophilus influenzae and Moraxella catarrhalis are common pathogens in patients with underlying lung disease o Staphylococcus aureus has become a common co pathogen in influenza associated pneumonia o Mycoplasma pneumonia, difficult to detect on Gram stain or culture, is another common cause of pneumonia o In up to 50% of CAP the organism is not identified o Neonates: coliform bacteria, cytomegalovirus, enterovirus, GBS, herpes virus, mycoplasma hominis, unreaplasma urealyticum o Infants 4-16 weeks: cytomegalovirus, influenza virus, parainfluenza virus, RSV, chlamydia trachomatis, H. influenzae, S. aureus, S. pneumoniae, U. urealyticum o Children up to 5 years: adenovirus, GAS, FLU, RSV, H. influenzae, S. aureus, S. pneumoniae o Children over 5 years through adolescence: Flu, varicella, chlamydia pneumoniae, H. influenzae, Legionella pneumophila, Mycoplasma pneumoniae, S. pneumoniae o Adults group I (no cardiopulmonary disease and no modifying factors): Respiratory viruses, C. pneumoniae, H. influenzae, M. pneumoniae, S. pneumoniae, endemic fungi, Legionella spp., Mycobacterium tuberculosis, S. aureus o Adults group II (with cardiopulmonary disease and/or modifying factors): Aerobic gram-negative bacilli, resp viruses, H. influenzae, S. aureus, S. pneumoniae (DRSP), endemic fungi, Legionella Moraxella catarrhalis, TB, Mycoplasma pneumoniae, mixed infection • Typical: S. pneumoniae, H. influenzae, S. aureus, or gram-negative bacteria o The presentation of typical pneumonia included fever, chills, yellow or green sputum, pleuritic chest pain, and lobar consolidation on chest x-rays • Atypical: M. pneumoniae, Legionella pneumophila, or a viral infection o The presentation of atypical pneumonia included a gradual onset of cough, no or scant sputum, low-grade fever, myalgias, arthralgias, and lack of consolidation on x-rays. Pneumonia therapy and goals of treatment • The goal of treatment for all patients is the return to the respiratory status they had before the illness. • Initially, patients who are responding to empirical antibiotic therapy should show improved clinical condition in 48 to 72 hours. • Fever should resolve in 2 to 4 days, and leukocytosis usually resolves by day 4 of treatment • The patient's chest x-ray may deteriorate and not return to baseline for weeks or months. • The best indicator of improvement in clinical status is that the overall clinical manifestations of pneumonia (e.g., fever and increased white blood cell [WBC] count) should improve. Common bacterial pathogens • Predominant organism depends upon the patients age and health status • All ages (except neonates) Streptococcus pneumoniae is the organism most commonly found in pneumonia (60-75% of adults confirmed via sputum culture) o Non-typeable Haemophilus influenzae and Moraxella catarrhalis are common pathogens in patients with underlying lung disease o Staphylococcus aureus has become a common co pathogen in influenza associated pneumonia o Mycoplasma pneumonia, difficult to detect on Gram stain or culture, is another common cause of pneumonia o In up to 50% of CAP the organism is not identified o Neonates: coliform bacteria, cytomegalovirus, enterovirus, GBS, herpes virus, mycoplasma hominis, unreaplasma urealyticum o Infants 4-16 weeks: cytomegalovirus, influenza virus, parainfluenza virus, RSV, chlamydia trachomatis, H. influenzae, S. aureus, S. pneumoniae, U. urealyticum o Children up to 5 years: adenovirus, GAS, FLU, RSV, H. influenzae, S. aureus, S. pneumoniae o Children over 5 years through adolescence: Flu, varicella, chlamydia pneumoniae, H. influenzae, Legionella pneumophila, Mycoplasma pneumoniae, S. pneumoniae o Adults group I (no cardiopulmonary disease and no modifying factors): Respiratory viruses, C. pneumoniae, H. influenzae, M. pneumoniae, S. pneumoniae, endemic fungi, Legionella spp., Mycobacterium tuberculosis, S. aureus o Adults group II (with cardiopulmonary disease and/or modifying factors): Aerobic gram-negative bacilli, resp viruses, H. influenzae, S. aureus, S. pneumoniae (DRSP), endemic fungi, Legionella Moraxella catarrhalis, TB, Mycoplasma pneumoniae, mixed infection Clinical practice guidelines for treatment of CAP • Initial management of adults with CAP that discuss the diagnosis, assessment of severity, and initial antimicrobial therapy. • Basically, the practitioner needs to take into consideration the comorbidities of the patient (cardiopulmonary disease), the severity of the illness at initial presentation, and the treatment setting (outpatient or hospital) • 1. Previously healthy outpatients with no history of cardiopulmonary disease and no modifying factors such as risk for drug-resistant streptococcal pneumonia (DSRP) (excludes those with HIV). o Treat with Macrolide (azithromycin, clarithromycin, or erythromycin) or doxycycline o No issues treat with macrolide or with doxycycline if patient allergic , Azithromycin 500 mg on day 1, followed by 250 mg/d for days 2 to 5 o clarithromycin 250 to 500 mg twice a day for 7 to 10 days o Erythromycin 500 mg given PO QID for 7 to 10 days is the least expensive o Length of treatment with community-acquired pneumonia should be for a minimum of 5 days (level I evidence) and the patient should be afebrile for 48 to 72 hours with vital signs, including oxygen saturation, within normal limits • 2. Outpatients with cardiopulmonary disease (congestive heart failure or chronic obstructive pulmonary disease [COPD]), diabetes, liver or renal disease, alcoholism, malignancies, asplenia, immunosuppression, use of antimicrobials in the past 3 months, and/or modifying factors (risk factors for DSRP [age greater than 65] or gram-negative bacteria). o Treat with a respiratory fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin) or a b-lactam plus a macrolide (high dose amoxicillin or amoxicillin/clavulanate preferred) o Issues like comorbidities, and antibiotics etc. then alternative treatment in patients with comorbidities is a beta lactam plus a macrolide (level I evidence). o High-dose amoxicillin (1 gm TID) or amoxicillin/clavulanate (Augmentin) is the preferred o Alternatives include cefpodoxime, cefuroxime, or parenteral ceftriaxone followed by oral cefpodoxime. Doxycycline • healthy, appropriately immunized infants, preschool, school-aged, and adolescent children, high-dose amoxicillin (90 mg/kg daily, divided in two doses) is the drug of choice for 7 to 10 days of outpatient treatment (Bradley et al, 2011)). If highly resistant pneumococci are in the community, the practitioner may choose between IV or IM ceftriaxone (50 mg/kg in one daily dose) or cefotaxime (150 mg/kg/d every 8 hours) followed by appropriate oral therapy after 1 or 2 doses • Mycoplasma pneumonia is the most common type in children over age 5 years, with approximately 10% of school-age children presenting with symptoms consistent with atypical or mycoplasma infection (AAP, 2012b). The disease is usually mild. The typical history includes upper respiratory symptoms, fever, dry cough, malaise, sore throat, headache, and possibly chills. Symptoms often last for 3 to 4 weeks (AAP, 2012b). A maculopapular rash o the treatment of choice for mycoplasma pneumonia is a macrolide. Z-pak CAP treatment in pregnancy pregnant women should get the PVC 13 vaccine • Pregnant women are at a slightly higher risk for infections than are other women because of diminished lymphocyte function and decreased functional residual capacity of the lung • women with pneumonia may require hospitalization, treatment with the appropriate antimicrobial/antiviral, and consultation with a peri-natologist as occult onset of preterm labor may occur • the macrolides erythromycin, azithromycin, and clarithromycin are safe during pregnancy, although erythromycin or azithromycin is the first choice, as each is Pregnancy Category B, whereas clarithromycin is Pregnancy Category C. • Doxycycline, a tetracycline, is not used during pregnancy because it may cause discoloration of deciduous teeth in neonates. • Fluoroquinolones are avoided during pregnancy due to concerns for fetal malformations, based on animal studies. • Women with comorbid conditions or recent antibiotics should be treated with a beta lactam plus a macrolide Radiologic findings during CAP treatment Radiographic improvement usually requires more time and is not an indicator of improvement. If the chest x- ray worsens yet the patient shows clinical improvement, that is the natural progression of the disease. Up to 15% of patients do not respond to appropriate initial empiric antibiotic therapy (Mandell et al, 2007). In severe CAP, if the radiographic findings worsen and the clinical picture worsens, then that is a predictor of increased morbidity and mortality. Treatment of chlamydial pneumonia Infants who are 2 to 19 weeks old and who present as afebrile, with a repetitive staccato cough and tachypnea, cervical adenopathy, and rales, are likely to have chlamydial pneumonia. Wheezing is rare. Chest x-ray will show hyperinflation and bilateral diffuse infiltrates. The patient may also have nasal stuffiness and otitis media. Diagnosis is confirmed by detecting chlamydia-specific immunoglobulin M (IgM) in serum • The standard treatment for infants with confirmed chlamydial pneumonia is erythromycin (EryPed) 50 mg/kg daily for 14 days or oral azithromycin (Zithromax) 20 mg/kg/d for 3 days. • These infants can usually be treated as outpatients if they are able to eat and maintain hydration. • An association between the use of erythromycin and hypertrophic pyloric stenosis in infants less than 6 weeks of age has been reported • The AAP continues to advise use of erythromycin for treatment of diseases caused by C. trachomatis • A diagnosis of C. trachomatis infection in an infant should prompt treatment of the mother and her sexual partner Chapter 43: Smoking Cessation Patient instructions for use of nicotine replacement medications Although the patient can self-treat with the OTC products, the health-care provider should educate the patient regarding their proper use to ensure successful treatment. Nicotine replacement does not achieve the same peak levels of nicotine as does smoking, but it does achieve a level high enough to suppress nicotine withdrawal symptoms. Nicotine replacement therapy is recommended for patients who smoke more than 20 cigarettes per day (one pack), patients who smoke within 30 minutes of awakening in the morning, and patients who have tried to quit previously and have failed because of strong withdrawal symptoms and craving within the first week of quitting. Patient education: overall treatment plan, specific to drug therapy, reasons for taking the drugs, drugs as part of the total treatment regimen, adherence issues Common side effects associated with smoking cessation therapy • Nicotine Withdrawal Syndrome: craving, nervousness, irritability, impatience, hostility, labile mood, difficulty concentrating, restlessness, and anxiety • Decreased HR, increased appetite, and weight gain averaging 8 to 11 pounds • Myalgia, HA, constipation, and fatigue • adherence issues often relapse 2-3 times, development of mouth ulcers Contraindications for smoking cessation therapy • Pregnancy and lactation • Bupropion and Chantix are not recommended during pregnancy • gum in pregnancy, patch is pregnancy D • children should never receive nicotine replacement products • contraindicated immediately after a stroke • Nicotine replacement therapy is contraindicated for people with a hypersensitivity to nicotine and should be used with caution in persons immediately after MI and in patients with life-threatening arrhythmias and severe or worsening angina pectoris because of increases in heart rate. Nicotine replacement medications: pharmacodynamics, pharmacotherapeutics, ADRs, drug interactions, clinical use, and dose Nicotine replacement therapy • Five forms: gum, lozenge, TD patch, inhaler, and nasal spray • Nicotine gum: nicotine polacrilex (a nicotine resin complex), bound to an ion exchange resin and released during chewing, chew 5-8 times and then place gum in buccal mucosa, use over 30 minutes (chewing and parking), excessive chewing can cause nausea, throat irritation, and hiccoughs, avoid smoking r/t toxicity (NV, HA), not first line for TMJ or PUD r/t ADRs, 2 to 4 mg/hr when beginning, acidic foods (coffee, soft drinks, juice) interfere with buccal absorption, gradually wean from the gum after 6 weeks • Nicotine lozenge: nicotine polacrilex lozenge an adjunct to quit, dose is 2 to 4 mg lozenge, based on how early in the day the smoker smoked the first cigarette, if a smoker has first cig 30 minutes or more after awakening 2 mg is indicated, 4 mg for those who smoke their first cig within 30 minutes of waking up, dissolves over 20 to 30 minutes, do not chew or swallow (r/t significant first pass metabolism), 1 lozenge every 1 to 2 hours for the first 6 weeks, 9/day with max of 20/day. Taper dose over several weeks. • TD patch: Slow, cutaneous absorption of nicotine over many hours, applied to clean, nonhair skin on the upper body or arm while awake, different strengths available, more ADRS sleep disruption, delivers a steady state that prevents withdrawal symptoms, ease of administration and once daily dosing, wean off by decreased dose of the patch on a schedule, disadvantage: unable to self-regulate the dose if they are exhibiting withdrawal symptoms=less effective for highly dependent smoking, refrain from smoking r/t life threatening dysrhythmias or MI, ADR skin irritation, change site every day do not reuse the site within a week, sleep disturbance or insomnia, delayed onset of sleep, toxicity (NV, HA) if toxicity occurs remove patch and rinse with water do not use soap it can increase absorption from the site, brand name and generics available • Nicotine Nasal Spray: Dose 1to 2 sprays in each nostril per hour, not to exceed 5 doses (10 sprays) per hour and not to exceed 40 doses (80 sprays) per day. Advantage: speed of delivery (increased rate of absorption). Do not inhale, swallow, or sniff the spray. ADR nasopharyngeal and ocular mucosa irritation, can cause serious arrhythmias and elevated BP, avoid immediately after MI may cause angina. If any CV symptoms abruptly d/c. Potential for abuse: patients report a head rush and sensation of feeling good. Three months of therapy max. • Nicotine Inhaler: Patient puffs continuously on the inhaler for 20 minutes, equivalent of two cigarettes. 6 cartridges/day for 3 to 6 weeks. Rude dose gradually maximum of 6 months of treatment. ADRs: coughing, mouth and throat irritation, and dyspepsia Antidepressants: bupropion, doxepin, and nortriptyline • Bupropion (Zyban), antidepressant, 7-12 weeks of therapy, only FDA approved antidepressant o Chemically unrelated to other antidepressants o MOA in smoking cessation unknown, Presumed action as a weak inhibitor of neuronal uptake of dopamine and norepinephrine o Started 1 to 2 weeks before quitting o Dose: 150 mg/day x 3 days and then increases to 150 mg BID (8 hrs apart at least), avoid bedtime dosing o On the quit day, the patient can quit cold turkey or use nicotine replacement therapy o Bupropion and the patch are a successful combo o Continue therapy for 7 to 12 weeks, may be extended for up to 6 months o Contraindicated in patients with seizure disorders, bulimia, and anorexia and within 14 days of an MAOI o Do not use in patients with Hx of stroke, brain tumor, brain surgery, or closed head injury o Reduce dose in renal failure o Use with caution with hepatic cirrhosis (150 mg every other day) o Pregnancy Category B: not recommended during pregnancy or for use in children under 18 o Monitor for HTN: if used with nicotine replacement therapy o Contraindicated: bupropion (Zyban) and Wellbutrin o ADRs: insomnia, dizziness, and dry mouth, constipation, increase fiber and fluid during Tx o Black Box Warning: increased risk of suicide ideation and suicidality in children, adolescents, and young adults Nicotinic Receptor Partial Agonists • Varenicline (Chantix), nicotine receptor partial agonist, 12 weeks of therapy • Affinity and selectivity for alpha 4 beta 2 nicotinic acetylcholine receptors • MOA: action as an agonist on the A4B2 receptors, as well as an antagonist preventing nicotine from binding t • Highly selective to A4B2 and moderately selective to 5-HT3 receptor • By blocking nicotine to the nicotinic receptors, there is less dopaminergic reinforcement and reward for smoking, decreased withdrawal symptoms • Choose a quit date and the drug is started 1 week before that • Titration up to 1 mg BID is required, manufacturer suggests schedule of 0.5 mg once a day for 3 days, then 0.5 mg BID on days 4 to 7 • Dose may be increased to 1 mg BID on day 8 and continue through Tx • Administer with a full glass of water after eating • If successful an addition 12 weeks of therapy is thought to increase the long term likelihood of quitting • ADR: nausea, insomnia, HA, behavior changes: agitation, depressed mood, suicidal ideation, and actual suicidal behavior • Pregnancy Category C and is not recommended during pregnancy or in nursing women • Do for use in children under 18 • Dose adjusted in older patients with decreased renal function Alpha 2 Adrenergic Agonists • Clonidine: second line treatment for smoking cessation, Not FDA approved for this indication • Available in tablets and patch • 0.1 mg/day increasing slowly to maximum of 0.3 mg/day • ADRs: dry mouth, sedation, dizziness, and hypotension Chapter 45: Tuberculosis Etiology, diagnosis, and risk factors Tuberculosis (TB) presents a serious threat to global health, with 8.6 million people developing TB and 1.3 million deaths in 2012 • TB is an infectious disease caused by M. tuberculosis, an organism that is inhaled into the alveolus, where it is ingested by the pulmonary macrophage. • The bacilli multiply and spread to local pulmonary areas and to extra thoracic organs via the lymphatic system. • The infected macrophage releases a substance that attracts T lymphocytes. • The infected macrophage presents antigens from the phagocytosed bacilli to the lymphocytes, producing a series of committed immune effector cells. • This causes a delayed hypersensitivity and, combined with the newly activated macrophages, leads to intracellular killing of the bacilli and granuloma formation. • M. tuberculosis and most of the other mycobacteria grow quite slowly, with a doubling time of 18 hours. • Thus, skin test reactivity does not occur until 4 to 6 weeks after infection, with longer intervals noted. • Colonies on culture media do not appear for 3 to 5 weeks, creating delays in culture confirmation and testing for drug susceptibility. • Infection is spread almost exclusively by aerosolization of contaminated lung secretions, in air for many hrs • Primarily affects the pulmonary tissue, although extrapulmonary TB is not uncommon, especially in immunocompromised patients. • Pulmonary TB: cough with productive, purulent secretion, often with blood streaks, wide temperature variations, malaise, fatigue, wasting, CP, dyspnea, and night sweats • Extra-pulmonary TB: more problematic symptoms often mimicking other diseases • Lymphatic TB: unilateral, painless, cervical lymphadenopathy • GU, bones or joints, meninges, GI tract, and pericardium • When extrapulmonary sites are infected symptoms are often vague and difficult to define • Diagnosis: Tuberculin skin test (TST) (negative 20-25% of the time) or interferon-gamma release assays (diagnoses latent and active TB), chest x-ray, sputum culture (nucleic acid amplification test monthly), biopsy, CT scan, bronch, blood test, HIV testing is recommended • Risk factors: foreign born (Mexico, the Philippines, India, Vietnam, and China), Asians have high rates of infection than whites, medically underserved, low income populations, including high risk racial or ethnic minority populations, people who are homeless, blacks, Hispanics, and Native Americans/Canadian aboriginal people, LTC residents, immune compromised patients, healthcare providers Rationale drug selection for special populations • Kids up to 4 years, infirm elderly, immunocompromised especially those with HIV or AIDs, or organ transplant recipients • Pregnancy and lactation: Initial Tx regimen: INH and RIF, EMB x 6 months. Pyridoxine (vitamin B6) 25 mg/d should be added to decrease incidence of peripheral neuropathy associated with INH. Streptomycin and other aminoglycosides are contraindicated r/t harmful effects on the fetus. Breastfeeding is not contraindicated during Tx (feed prior to taking dose, trace amounts in breast milk) • Pediatric patients: Difficult to Dx r/t positive screening test but asymptomatic, CXR may be normal or demonstrate minimal abnormalities. • Pediatric drug therapy depends on the infection or disease category (Asymptomatic infection with positive skin test only-9 month regimen: INH daily, Pulmonary disease-6 or 9 month regimen, Extrapulmonary TB- 12 month regimen (INH, RIF, PZA, and streptomycin daily for 2 months (meningitis, military, bone and joint), Extrapulmonary TB-same as for pulmonary disease (other than meningitis, military, bone or join)) • Peds: RIF and INH can be administered to children safety (LFTs) • EMB can cause ocular toxicity: do not Rx for children under 6 (vision cannot be properly tested) • Streptomycin in place of EMB (monitor for ototoxicity and nephrotoxicity) • PZA is safe in children • Infants: TST (4 to 6 weeks and at 3 to 4 months old), if TB status of household cannot be evaluated the infant may be started on INH (10 mg/kg/day) for 3-4 months. May receive BCG vaccine (decreased severity of disease) • HIV positive patients: Same for other adults except: one weekly RIF should not be used in any HIV patient and twice weekly INH RIF or rifabutin should not be used for patients with CD4 counts lower than 100/mcL Criteria for resistant TB diagnosis • Resistance to at least isoniazid and rifampin • If not chest x-ray improvement within 3 months of Tx, then either resistance or inaccurate Dx • Primary (patient who has never been treated for TB) or acquired (previous Tx for TB) • Can only be proved via susceptibility testing Risk factors for fatal hepatitis with INH use • Pregnant patients have a 2.5 fold higher risk of INH induced hepatitis than other patients (LFTs) • Age related (50-64 y/o), daily ETOH use, chronic liver disease, and IV drug use • Black and Hispanic women as well as any woman during the postpartum period who takes INH have increased risk of fatal hepatitis • s/s anorexia, NV, dark urine, icterus, rash, persistent paresthsias of hands or feet, fatigue, weakness, fever longer than 3 days, ABD tenders especially RUQ Prophylactic treatment of TB for high risk patient • A person who is in a high incidence group with a skin test reaction of 10 mm or more is a candidate for preventive therapy, even without any risk factors • TB prevention: combination of INH and rifapentine: “12 dose regimen” • INH 15 mg/kg (max 900 mg) and rifapentine (RPT) 900 mg (for adults more than or equal to 50kg) administered once weekly utilizing DOT Drug Therapy • Treatment regimen consists of multiple drugs, drugs must be taken regularly, drug therapy must continue for a sufficient period, never add a single drug to a failure treatment regiment • Many combinations of drugs and frequencies of administration are possible • Initial treatment phase: critical in preventing drug resistance and improve outcomes, last 2 months • Continuation phase: 4 to 7 months • Six month regimen: for those who adhere to Tx and have fully susceptible organisms • 2 months of 4 drugs daily: isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) followed by 4 months of INH and RIF • Alternative regimens for the first 2 months: (regimen 2) INH, RIF, PZA, and EMB given daily for 2 weeks followed by twice weekly for 6 weeks, or (regimen 3) three times a week for 8 weeks • This four drug therapy is effective even when organism is resistant to INH • Streptomycin is substituted for EMB in children too young to be monitored for visual acuity • Can be used in HIB • Nine month regimen: INH and RIF used for patients who cannot take PZA or have resistance to PZA. EMB (streptomycin in young children) should be included for the first 2 months, followed by INH and RIF given daily or twice weekly for 7 months ➢ Mycobacteria- among the most difficult to cure (e.g. tuberculosis [TB]) o They grow slowly and are relatively resistant to drugs that are largely dependent on how rapidly cells are dividing o Have a lipid-rich cell wall relatively impermeable to many drugs o Are usually intracellular and inaccessible to drugs that does not have good intracellular penetration o Have the ability to go into a dormant state o Easily develop resistance to any single drugs o Pregnancy categories: ▪ Isoniazid: Pregnancy category A ▪ Streptomycin: Pregnancy category D (congenital deafness) ▪ The rest: Pregnancy category C ▪ Fetal death- d/t TB: isoniazid + rifampin + ethambutol for TB tx if pregnant and if drug resistance is a possibility. • Spectrum of coverage for various organisms/Pharmacodynamics o Isoniazid - most active drug for tx of TB ▪ Bactericidal- against susceptible mycobacteria (intracellular and extracellular organisms) ▪ Interferes with lipid and nucleic acid biosynthesis in growing organisms. ▪ Isoniazid and ethambutol- inhibits synthesis of mycolic acid (important constituents for mycobacteria cell walls and are not found in mammalian cells). o Rifamycin – rifampin, rifabutin, rifapentine ▪ Bactericidal- against susceptible mycobacteria ▪ Bind to the beta subunit of mycobacteria DNA-dependent RNA polymerase and inhibit RNA synthesis -> destruction of both multiplying and inactive bacilli. ▪ Readily penetrate most tissues and can kill bacteria that are poorly accessible to many drugs. ▪ Rifampin and rifabutin: N. gonorrhoeae, staphylococci, streptococci, Mycobacterium leprae, MAC, and H. influenzae type B. ▪ Rifampin-resistance develop rapidly when used as monotherapy- should be combined with another active abx for tx of established infections. o Ethambutol ▪ Bacteriostatic- against susceptible mycobacteria (M. tuberculosis, M. avium, M. kansasii) ▪ Inhibits synthesis of arabinogalactan (an essential component of mycobacteria cells walls). ▪ Arrests cell multiplication -> cell death ▪ Enhances the activity of lipophilic drugs (rifampin and ofloxacin) that cross the mycobacteria cell wall primarily in lipid portions of this cell wall. o Pyrazinamide- an analogue of nicotinamide ▪ Bactericidal – against M. tuberculosis in an acidic environment (pH <5.6). ▪ Useful in tx of TB ▪ Exhibits good activity within macrophages and plays a key role in killing intracellular organisms. ▪ Shortening therapy and preventing relapses ▪ Exact action is UNKNOWN. o Streptomycin – aminoglycoside, used now almost exclusively to treat M. tuberculosis infections. ▪ Bactericidal in alkaline extracellular environment ▪ Added as the 4th drug to the regimen for TB ▪ Sensitive to M. avium and M. kansasii; resistant to all mycobacterium ▪ Irreversible inhibitor of protein synthesis. ▪ Penetrates cells poorly o Ethionamide- similar binding site and mechanism of action as isoniazid. ▪ Ultimately blocks the synthesis of mycolic acids. ▪ Bacteriostatic – M. tuberculosis ▪ Can inhibit some other Mycobacterium species. o Capreomycin – peptide abx ▪ Bactericidal to susceptible mycobacteria. ▪ Inhibits RNA synthesis -> decreasing replication of M. tuberculosis. ▪ Resistance easily develops when given as monotherapy (should be given as part of multidrug regimen) o Bedaquiline – unique antimycobacterial, approved by FDA in 2012 ▪ For tx of multidrug resistant TB ▪ Inhibits mycobacterial adenosine triphosphate (ATP) synthesis ▪ Active against replicating and dormant mycobacteria ▪ Black-box warning: increased mortality as compared with a placebo tx group. ▪ Only to be used when an effective tx regimen cannot otherwise be provided. o Para-amino salicylic acid- structurally similar to PABA and sulfonamides ▪ Folate synthesis antagonist ▪ Active almost exclusive against M. tuberculosis. ▪ Bacteriostatic ▪ Not used frequently – primary resistance is common, and other drugs are better tolerated and less expensive. • Pharmacokinetics o Oral antimycobacterial drugs are rapidly and well absorbed in GI tract after PO administration. o Isoniazid- 90% bioavailable but should be taken on an empty stomach ▪ Readily diffuses into all body fluids including CSF (90% of serum levels), pleural, and ascitic fluids ▪ Readily diffuses into tissues, organs, saliva, sputum, and feces ▪ Crosses placenta and breastmilk ▪ Metabolism is extensive and highly variable and dependent on acetylator status. ⟶ Primarily acetylated by the liver 50% of both blacks and whites are slow acetylators Alaskan and Asians- majority are rapid acetylators Fast acetylators metabolize this drug 5 to 6 times faster than slow acetylators ⟶ Rate of acetylator does not affect effectiveness but may increase risk for toxic reactions with slow acetylators. ▪ Excreted in the urine- metabolites, and unchanged drug ▪ Elimination is largely dependent on renal function o Rifamycin’s and ethambutol penetrate and concentrate in most body fluids. ▪ Food slow the rate of absorption of rifamycin’s but not the extent of absorption (may be taken with or without food) ▪ Adequate CSF penetration occurs only in the presence of inflamed meninges. ▪ Potent inducers of liver metabolism ▪ Rifampin and rifapentine- metabolized in the liver by deacetylation. ⟶ Metabolites are active against M. tuberculosis. ⟶ t1/2 life decreases with repeated administration ▪ excreted primarily in the bile -> enterohepatic recirculation -> feces, urine (small amount) ▪ hepatic insufficiency and age slightly affect metabolism of rifabutin ▪ Renal insufficiency- reduced drug distribution and faster drug elimination -> decreased drug concentrations. o Pyrazinamide- widely distributed in body tissues and fluids including the liver and lung. ▪ Reaches high concentrations in CSF ▪ Crosses the placenta and enter breastmilk in small amounts ▪ Poor CSF penetration (good penetration if meninges are inflamed) ▪ 70% excreted in urine by glomerular filtration ▪ Hydrolyzed by the liver to a metabolite that also has antimycobacterial activity ▪ Prolonged t1/2 - significant on impaired hepatic and renal functions. o Streptomycin and capreomycin ▪ widely distributed through extracellular fluid ▪ Cross placenta and enter breast milk ▪ Poor CSF penetration except in the presence of inflamed meninges ▪ Excreted almost exclusively by the kidneys o Ethionamide- widely distributed to body tissues and fluids- CSF and serum concentrations are equal ▪ 35% metabolized by the liver ▪ Majority of the drug excreted in the urine as inactive metabolites o Ethambutol- mainly excreted as unchanged drug in the urine. ▪ 20% metabolized by the liver ▪ Marked accumulation may occur in renal failure • Pharmacotherapeutics o Isoniazid- careful monitoring for hepatotoxicity (ETOH drinkers, chronic liver disease, severe renal function, >35y/o, drug abuse, pregnant, immediately postpartum) ▪ Peripheral neuropathy, neurotoxicity may occur ⟶ Special caution: patients with preexisting peripheral neuropathy, pregnancy, and (+) HIV. o Ethambutol, streptomycin, capreomycin ▪ Cautious use for patient with renal impairment ▪ Dose adjustments may be required o HEPATOTOXIC: rifamycin’s, Isoniazid, Pyrazinamide, Ethionamide (RIPE) o Ethionamide: use with caution with DM, hepatitis is more likely with these patients o Thrombocytopenia and anemia: rifampin and isoniazid o Gouty arthritis attacks: ethambutol and pyrazinamide (should not be used during a flare up) o Visual disturbances, irreversible blindness- ethambutol (cautious use with eye disorders such as diabetic retinopathy, cataracts, optic neuritis) o CYP enzyme: ▪ Rifamycin’s- potent inducers of liver metabolism ▪ Medications metabolized by CYP enzyme- may lead to subtherapeutic concentrations -> tx failure may occur. • Clinical indications & dosing o See textbook pp.766-769 • ADRs/Monitoring: o Hypersensitivity reactions o Isoniazid ▪ Peripheral neuropathy – isoniazid (give Pyridoxine (vit.b6) for prevention) ▪ Hepatitis, Elevated LFTs- jaundice, fatigue – MONITOR LFTs ▪ Isoniazid + rifampin = increased risk for liver damage (4-folds!) ▪ Blood dyscrasias ▪ Metabolic acidosis ▪ Drug fever ▪ Gynecomastia o Rifamycins- mostly GI s/sx (n/v/d, anorexia, flatulence, abd pain) ▪ Hepatotoxicity occurs with isoniazid- MONITOR LFTs ▪ Orange-red discoloration of the body fluids including tears, saliva, urine, sweat, CSF, and feces (harmless) ▪ Hematuria- sign of hypersensitivity reaction (not to be confused with urine discoloration!!!) ▪ Blood dyscrasias ▪ h/a, drowsiness, inability to concentrate ▪ pruritic rash (1%-11% of patients) ▪ visual disturbances ▪ lupus erythematosus ▪ exudative conjunctivitis ▪ thrombocytopenia and neutropenia- observed with rifabutin o Ethambutol – mostly GI s/sx ▪ Common: optic neuritis (serious)- dose related (reversible if drug is dc’d) ⟶ Decreased visual acuity, loss of vision ⟶ Red-green color blindness ⟶ Diminished visual fields ⟶ Generally reversible when drug is d/c promptly ⟶ May take up to 1 year to recover ⟶ Vision tests before, during, and after therapy ▪ Gouty arthritis attacks- elevated uric acid- CHECK/MONITOR URIC ACID ▪ Transient impairment of liver function- MONITOR LFTs ▪ Infrequent peripheral neuropathy o Pyrazinamide – HEPATOTOXICITY (dose related) ▪ Monitor LFTs ▪ Monitor s/sx of hepatotoxicity (jaudince, fatigue) ▪ Hyperuricemia often occurs- may precipitate gouty arthritis attacks ⟶ The drug inhibits renal excretion of urates o Streptomycin, capreomycin- OTOTOXICITY ▪ Damage of the CN-VIII (Cranial Never 8)- vertigo, n/v, loss of hearing ▪ Increased risk -> higher doses and longer duration of therapy ▪ Nephrotoxicity- common among aminoglycosides ⟶ Dose adjustment, monitor kidney function ⟶ Dose of 2-3 times weekly (rather than daily)- may reduce the risk for toxicity o Ethionamide ▪ Few ADRs ▪ GI distress (NVD) ▪ Metallic taste ▪ Hepatitis (rare), optic neuritis, and peripheral neuritis (common) ⟶ Treat neurological symptoms with pyridoxine o Cycloserine ▪ Neurological effects ⟶ Somnolence, psychosis, and suicidal ideation • Patient education o Multidrug therapy is essential for TB- to prevent resistance, and achieve tx success o Directly observed therapy (DOT)- each dose is observed by an HCP or other designated person (strategy to promote compliance) o GI upset is relatively common in the first few weeks of initial phase therapy o First-line drugs, especially Rifampin, must not be d/c’d because of minor adverse effects o May be administered with food o Do not split doses o rifamycin’s may discolor urine, tears, saliva, and sweat o Clothes, dentures, or contacts may become stained o Patients on ethambutol contact provider if eye pain or visual disturbances occur o Good nutrition, rest, appropriate exercise o Monitoring of ADRs, hypersensitivity, resolution of s/sx (is the tx working?) Antimycobacterial guideline for TB ➢ TB disease can be treated by taking several drugs for 6-9 months ➢ 10 drugs approved by the USDA and FDA for treating TB ➢ First-line treatment (R-I-P-E)- for dosing, see textbook pp. 1242-1243 o Rifampin (RIF) o Isoniazid (INH) o Pyrazinamide (PZA) o Ethambutol (EMB) ➢ Second-line treatment- for dosing, see textbook pp. 1242-1243 o Cylcoserine o Ethionamide o Moxifloxacin o Gatifloxacin o Bedaquiline ➢ Treatment regimens include initial phase and continuation phases. ➢ Initial phase has four drugs o isoniazid (INH) rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) o Given for 2 months ➢ Followed by continuation phases, o usually two drugs INH and another drug, most often RIF o Given 4-7 months ➢ Tx of TB begins with accurate diagnosis. [Show More]
Last updated: 1 year ago
Preview 1 out of 75 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 05, 2022
Number of pages
75
Written in
Additional information
This document has been written for:
Uploaded
Mar 05, 2022
Downloads
0
Views
28

.png)






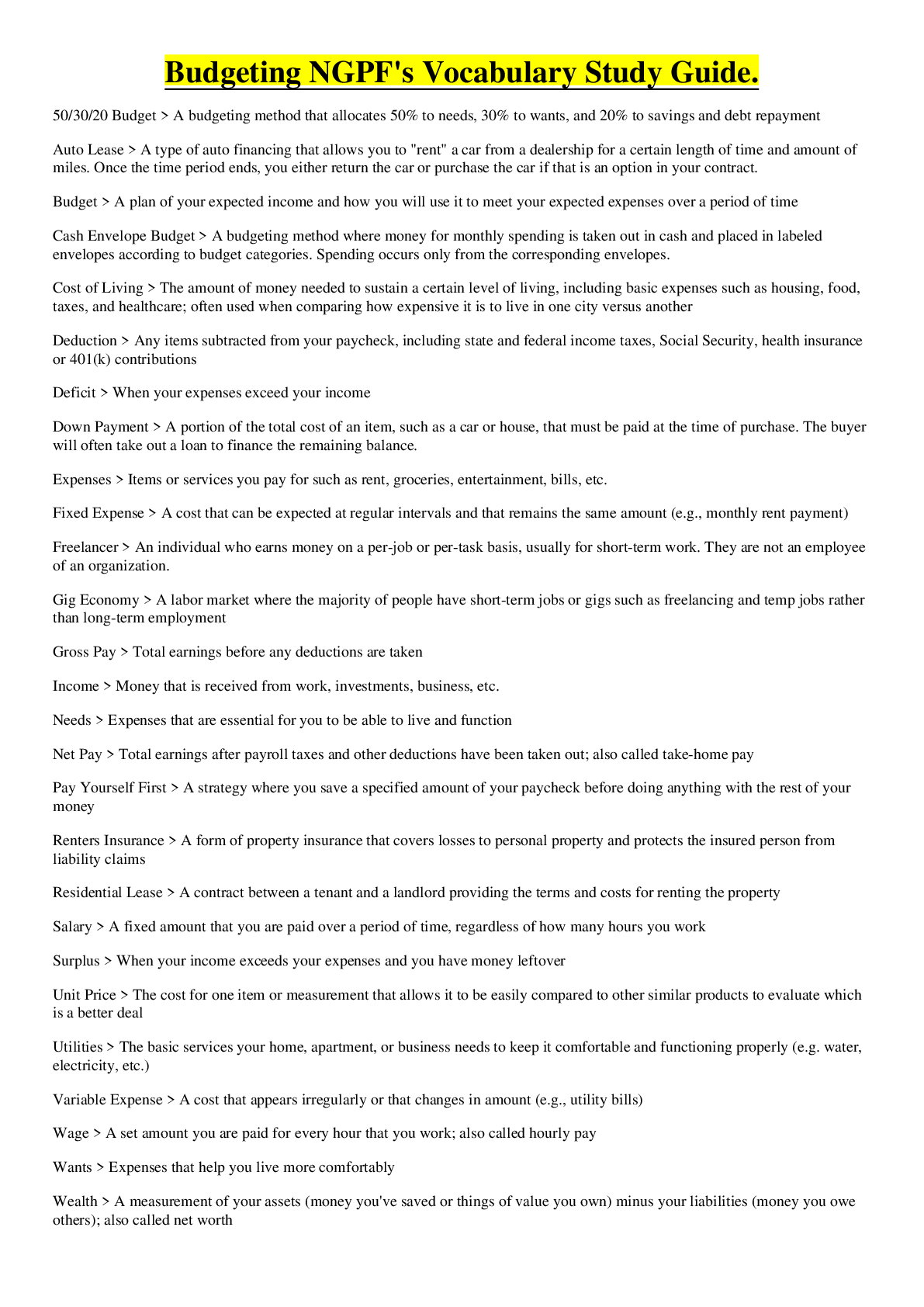

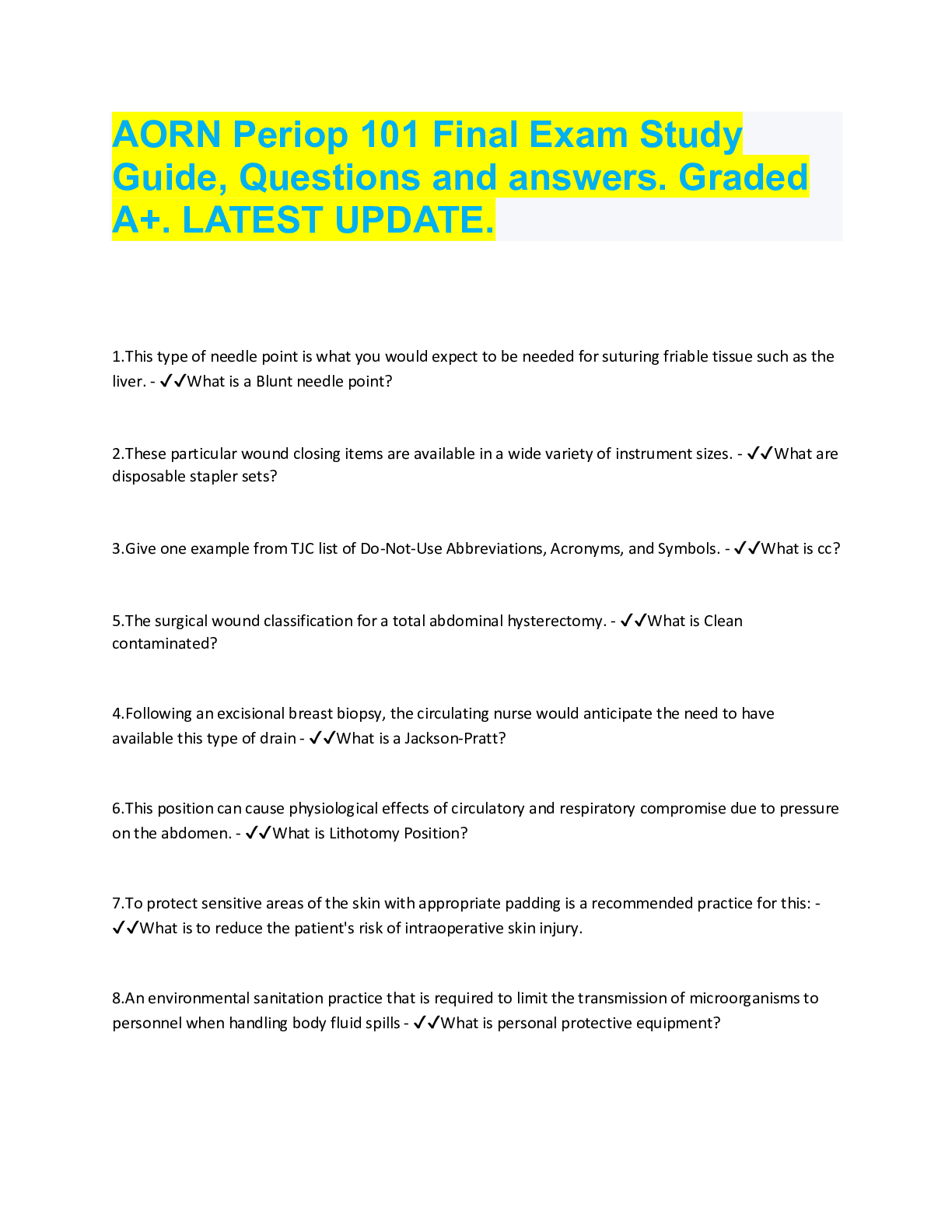
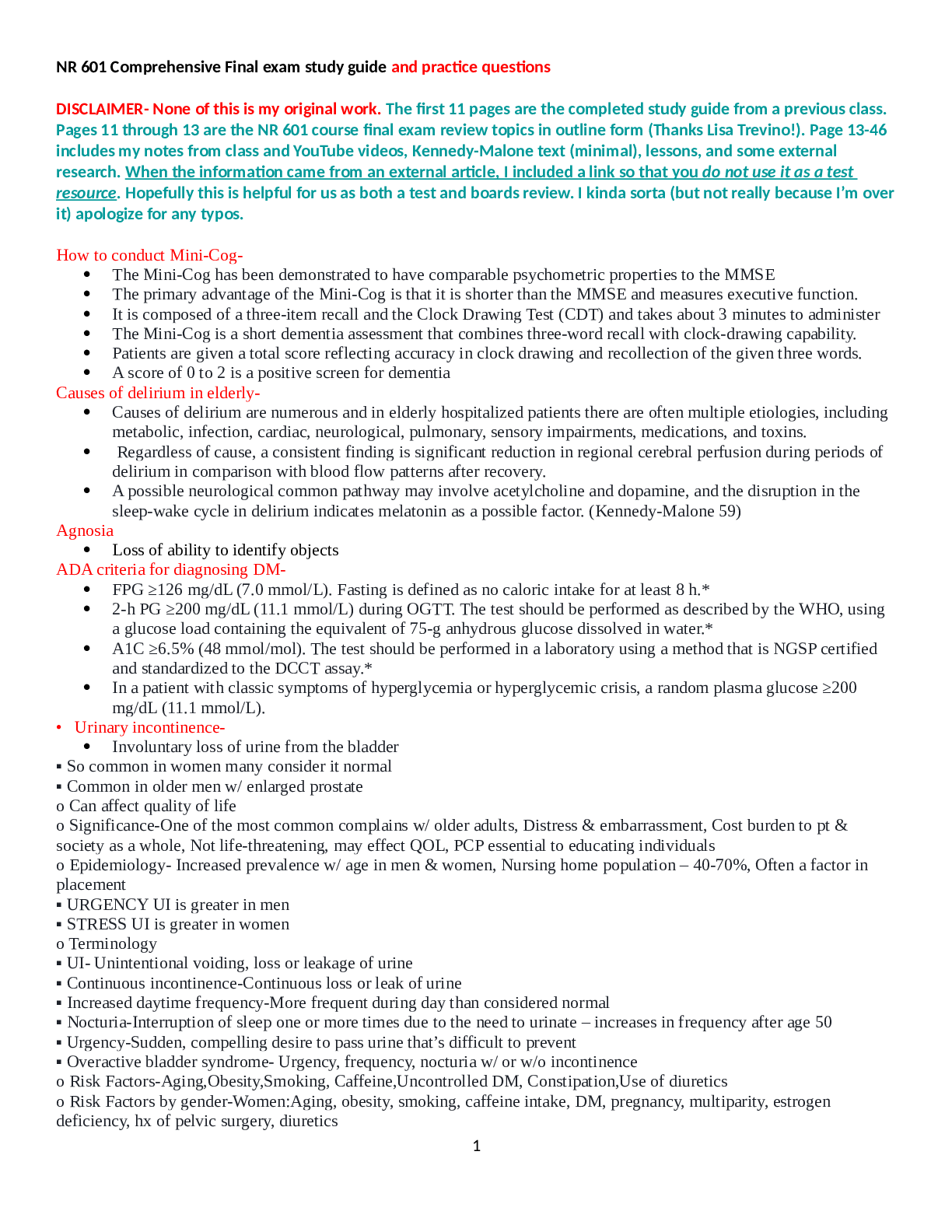



.png)


