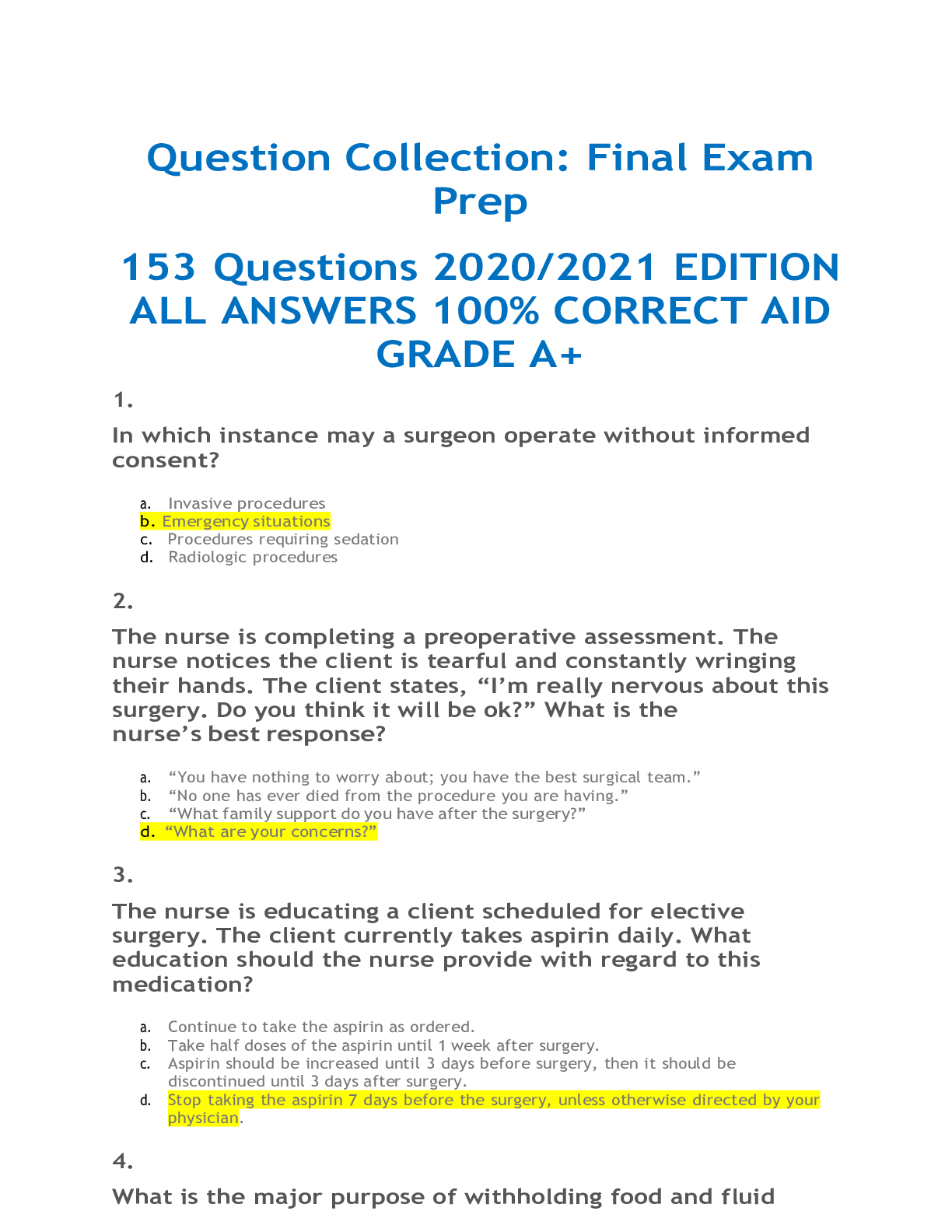
*NURSING > EXAM > ADULT HEALTH NUR3241_ 2021 / NUR3241 Question Collection: Final Exam Prep 153 Questions and answers_ (All)
ADULT HEALTH NUR3241_ 2021 / NUR3241 Question Collection: Final Exam Prep 153 Questions and answers_ 2021
Document Content and Description Below
1. In which instance may a surgeon operate without informed consent? a. Invasive procedures b. Emergency situations c. Procedures requiring se dation d. Radiologic procedures 2. The nurse is completin... g a preoperative assessment. The nurse notices the client is tearful and constantly wringing their hands. The client states, “I’m really nervous about this surgery. Do you think it will be ok?” What is the nurse’s best response? a. “You have nothing to worry about; you have the best surgical team.” b. “No one has ever died from the procedure you are having.” c. “What family support do you have after the surgery?” d. “What are your concerns?” 3. The nurse is educating a client scheduled for elective surgery. The client currently takes aspirin daily. What education should the nurse provide with regard to this medication? a. Continue to take the aspirin as ordered. b. Take half doses of the aspirin until 1 week after surgery. c. Aspirin should be increased until 3 days before surgery, then it should be discontinued until 3 days after surgery. d. Stop taking the aspirin 7 days before the surgery, unless otherwise directed by your physician. 4. What is the major purpose of withholding food and fluid before surgery?a. Prevent overhydration b. Decrease urine output c. Prevent aspiration d. Decrease risk of constipation 5. During the admission history the client reports to the nurse of taking the usual dose of warfarin the previous day. What is an appropriate nursing action? a. Notify the surgeon that the client took warfarin the day before surgery. b. No action is needed, because the client takes warfarin on a continuing basis. c. Put a note on the preoperative checklist before sending the client into surgery. d. Tell the client to inform the circulating nurse before the anesthesia is administered. 6. The nurse is aware that a religious group that refuses blood transfusions for religious reasons is: a. Catholics b. Jehovah's Witnesses c. Jews d. Methodists 7. The nurse is monitoring a presurgical patient for electrolyte imbalance. Which classification of medication may cause electrolyte imbalance? a. Corticosteroids b. Diuretics c. Phenothiazines d. Insulin 8. The nurse is aware that which of the following nutrients promotes normal blood clotting? a. Magnesium b. Vitamin C c. Zinc d. Vitamin K 9.A registered nurse who is responsible for coordinating and documenting client care in the operating room is a a. circulating nurse. b. scrub nurse. c. anesthetist. d. anesthesiologist. 10. The surgical unit nurse is developing a postoperative plan of care. In which client’s plan of care would the nurse document interventions of coughing and deep breathing, gastrointestinal assessment, and effective regulation of temperature? a. A client with gastrointestinal surgery and general anesthesia b. A client having a knee replacement and regional anesthesia c. A client having lower extremity muscle repair and spinal anesthesia d. A client with spinal stenosis and a regional nerve blockade 11. A nurse on the surgical team has been assigned the role of scrub nurse. What action by the scrub nurse is appropriate? a. Leading the surgical team in a debriefing session b. Keeping all records and adjusting lights c. Handing instruments to the surgeon and assistants d. Coordinating activities of other personnel 12. A patient is scheduled to have a heart valve replacement with a porcine valve. Which patient does the nurse understand may refuse the use of any porcine-based product? a. A patient of Catholic faith b. A patient of Jewish faith c. A patient of Baptist faith d. A patient of Lutheran faith 13. In which position would a client undergoing a lumbar puncture be placed?a. Supine b. Semi-Fowler's c. Side-lying, knees to chest d. Trendelenburg 14. It is important for the nurse to assist a postsurgical client to sit up and turn the head to one side when vomiting in order to a. maximize comfort. b. avoid dizziness. c. avoid aspiration. d. help eliminate inhaled anesthetics. 15. The client complains of weakness and dizziness as the nurse assists the client to sit on the side of the bed. The nurse recognizes the client is experiencing: a. acute pain b. anxiety c. incisional pain d. orthostatic hypotension 16. A client who had abdominal surgery 4 days ago reports that "something gave way" when he sneezed. The nurse observes a wound evisceration. Which nursing action is the first priority? a. Applying a sterile, moist dressing b. Monitoring vital signs c. Inserting a nasogastric (NG) tube d. Putting the client on nothing-by-mouth (NPO) status 17. What intervention by the nurse is most effective for reducing hospital-acquired infections? a. Administration of prophylactic antibiotics b. Aseptic wound care c. Control of upper respiratory tract infections d. Proper hand-washing techniques18. Which action should a nurse perform to prevent deep vein thrombosis when caring for a postsurgical client? a. Reinforce the need to perform leg exercises every hour when awake b. Massage the calves or thighs c. Instruct the client to cross the legs or prop a pillow under the knees d. Maintain bed rest 19. A client has undergone surgery to repair a hernia, with no complications. In the immediate postoperative period, which action by the nurse is most appropriate? a. Monitor vital signs every 15 minutes b. Measure arterial blood gas every 5 minutes c. Measure urinary output every 15 minutes d. Assess pupillary response every 5 minutes 20. Which of the following sets of clinical data would allow the nurse to conclude that the nursing actions taken to prevent postoperative pneumonia have been effective? a. Vital signs within normal limits; absence of chills and cough b. Alert and oriented; peripheral pulses present and strong c. Bladder non—distended; Foley catheter draining clear, yellow urine d. Bowel sounds present and active; denies nausea and vomiting 21. A client receiving moderate sedation for a minor surgical procedure begins to vomit. What should the nurse do first? a. Roll the client onto his or her side. b. Suction the mouth. c. Provide a basin. d. Administer an antiemetic medication. 22. A nurse is monitoring a client recovering from moderate sedation that was administered during a colonoscopy. Which finding requires the nurse's immediate attention? a. Heart rate of 84 beats/minuteb. Oxygen saturation (SaO2) of 85% c. Decreased cough and gag reflexes d. Blood-tinged stools 23. The nurse is teaching the client about usual side effects associated with spinal anesthesia. Which of the following should the nurse include when teaching? a. Sore throat b. Itching c. Seizures d. Headache 24. The nurse understands that the purpose of the “time out” is to: a. verify all necessary supplies are available. b. identify the client’s allergies. c. clarify the roles of the OR personnel. d. maintain the safety of the client. 25. A client undergoing coronary artery bypass surgery is subjected to intentional hypothermia. The client is ready for rewarming procedures. Which action by the nurse is appropriate? a. Temporarily set the OR temperature to 30°C. b. Place warm damp drapes on the client, replacing them every 5 minutes. c. Administer IV fluids warmed to room temperature. d. Apply a warm air blanket, gradually increasing body temperature. 26. Which statement by the client indicates further teaching about epidural anesthesia is necessary? a. "I will become unconscious." b. "I will lose the ability to move my legs." c. "I will be able to hear the surgeon during the surgery." d. "A needle will deliver the anesthetic into the area around my spinal cord." 27.The nurse caring for a client receiving a transfusion notes that 15 minutes after the infusion of packed red blood cells (PRBCs) has begun, the client is having difficulty breathing and complains of severe chest tightness. What is the most appropriate initial action for the nurse to take? a. Notify the client's health care provider b. Stop the transfusion immediately. c. Remove the client's IV access. d. Assess the client's chest sounds and vital signs. 28. The nurse begins a routine blood transfusion of packed red blood cells (PRBCs) at 1100. To ensure client safety, the unit of blood should be completely transfused by what time? a. 1115 b. 1500 c. 1530 d. 1600 29. For a client diagnosed with pernicious anemia, the nurse emphasizes the importance of lifelong administration of a. Vitamin A b. Vitamin C c. Folic acid d. Vitamin B12 30. The nurse is caring for four clients on the medical-surgical unit of the hospital. What client is mostly likely to be receiving treatment for sickle cell crisis? a. A 29-year-old Caucasian male b. A 19-year-old African American male c. A 24-year-old Native American female d. A 36-year-old Eastern European female 31. Which type of hemolytic anemia is categorized as inherited disorder?a. Sickle cell anemia b. Autoimmune hemolytic anemia c. Cold agglutinin disease d. Hypersplenism 32. The nurse is caring for an older adult client who has a hemoglobin of 9.6 g/dL and a hematocrit of 34%. To determine where the blood loss is coming from, what intervention can the nurse provide? a. Observe stools for blood. b. Observe the gums for bleeding after the client brushes teeth. c. Observe the sputum for signs of blood. d. Observe client for facial droop. 33. While assessing a client, the nurse will recognize what as the most obvious sign of anemia? a. Pallor b. Tachycardia c. Flow murmurs d. Jaundice 34. A client diagnosed with a cataract comes into the clinic. What assessments should the nurse observe in this client? a. A burning sensation and the sensation of an object in the eye b. Blurred or cloudy visual image c. Inability to produce sufficient tears d. A swollen lacrimal caruncle 35. A colleague has been splashed in the eye with cleaning solution. Which of the following would be the priority? a. Finding out what the substance was b. Irrigating the eye immediately with tap water c. Covering the eye with a clean sterile dressing d. Instilling a local anesthetic into the eye 36. Which of the following eye disorders is caused by an elevated intraocular pressure (IOP)?a. Glaucoma b. Cataracts c. Hyperopia d. Myopia 37. A patient has had cataract extractions and the nurse is providing discharge instructions. What should the nurse encourage the patient to do at home? a. Maintain bed rest for 1 week. b. Lie on the stomach while sleeping. c. Avoid bending the head below the waist. d. Lift weights to increase muscle strength. 38. An older adult patient has noticed a significant amount of vision loss in the last few years. What does the nurse recognize as the most common cause of visual loss in older adults? a. Macular degeneration b. Ocular trauma c. Retinal vascular disease d. Uveitis 39. Some clients with acoustic neuromas have vertigo. What is a priority nursing action for clients with vertigo? a. Protect the client from injury. b. Provide small meals of tepid food. c. Mobilize the client at every opportunity. d. Provide ice to the affected ear. 40. A client who comes to the ambulatory care facility states, "It feels like things are moving or spinning around me." The nurse interprets this as indicating which of the following? a. Dizziness b. Nystagmus c. Vertigo d. Motion sickness41. The nurse caring for a client with Ménière's disease needs to assist with what when the client is experiencing an attack? a. Sleeping b. ADLs c. Coughing d. URIs 42. Which nursing diagnosis takes highest priority for a client admitted for evaluation for Ménière's disease? a. Acute pain related to vertigo b. Imbalanced nutrition: Less than body requirements related to nausea and vomiting c. Risk for deficient fluid volume related to vomiting d. Risk for injury related to vertigo 43. The nurse is developing a plan of care for a client with Meniere's disease and identifies a nursing diagnosis of excess fluid volume related to fluid retention in the inner ear. Which intervention would be most appropriate to include in the plan of care? a. Limit foods that are high in sodium. b. Encourage intake of caffeinated fluids. c. Administer prescribed antihistamine. d. Restrict high-potassium foods. 44. A patient is scheduled for a test with contrast to determine kidney function. What statement made by the patient should the nurse inform the physician about prior to testing? a. “I don’t like needles.” b. “I am allergic to shrimp.” c. “I take medication to help me sleep at night.” d. “I have had a test similar to this one in the past.” 45. Which term describes painful or difficult urination? a. Oliguriab. Anuria c. Nocturia d. Dysuria 46. When the bladder contains 400 to 500 mL of urine, this is referred to as a. anuria. b. specific gravity. c. functional capacity. d. renal clearance. 47. When fluid intake is normal, the specific gravity of urine should be: a. 1.000 b. Less than 1.010 c. Greater than 1.025 d. 1.010 to 1.025 48. The nurse is teaching a client with recurrent urinary tract infections (UTIs) ways to decrease risk for additional UTIs. The nurse includes which information? a. Take tub baths instead of showers. b. Void immediately after sexual intercourse. c. Increase intake of coffee, tea, and colas. d. Void every 5 hours during the day. 49. Which client is at highest risk for developing a hospitalacquired infection? a. A client with a laceration to the left hand b. A client who's taking prednisone (Deltasone) c. A client with an indwelling urinary catheter d. A client with Crohn's disease 50. The nurse is caring for a patient with dementia in the longterm care facility when the patient has a change in cognitivefunction. What should the nurse suspect this patient may be experiencing? a. A UTI b. A stroke c. An aneurysm d. Fecal impaction 51. A client has a suspected diagnosis of bladder stones. Stones may form in the bladder or originate in the upper urinary tract and travel to and remain in the bladder. What are some signs and symptoms that this client may be experiencing? Select all that apply. a. All choices are true. b. hematuria c. suprapubic pain d. difficulty starting urinary stream 52. A nurse is planning a group teaching session on the topic of urinary tract infection (UTI) prevention. Which point should the nurse include? a. Limit fluid intake to reduce the need to urinate. b. Take medication ordered for a UTI until the symptoms subside. c. Notify the physician if urinary urgency, burning, frequency, or difficulty occurs. d. Wear only nylon underwear to reduce the chance of irritation. 53. A client is complaining of problems with constipation. What dietary suggestion can the nurse inform the client may help facilitate the passage of stool? a. Increase the carbohydrate content of the diet. b. Increase dietary fat consumption. c. Increase dietary protein such as lean meats. d. Increase dietary fiber. 54. A client presents to the emergency department with complaints of acute GI distress, bloody diarrhea, weightloss, and fever. Which condition in the family history is most pertinent to the client's current health problem? a. Ulcerative colitis b. Hypertension c. Gastroesophageal reflux disease d. Appendicitis 55. Crohn's disease is a condition of malabsorption caused by which pathophysiological process? a. Inflammation of all layers of intestinal mucosa b. Infectious disease c. Disaccharidase deficiency d. Gastric resection 56. It is important for the nurse to monitor serum electrolytes in a patient with acute diarrhea. Select the electrolyte result that should be immediately reported. a. Chloride of 100 mEq/L b. Sodium of 136 mEq/L c. Calcium of 9 mg/dL d. Potassium of 2.8 mEq/L 57. The nurse is admitting a client with a diagnosis of diverticulitis and assesses that the client has a board-like abdomen, no bowel sounds, and reports of severe abdominal pain. What is the nurse's first action? a. Start an IV with lactated Ringer’s solution. b. Notify the health care provider. c. Administer a retention enema. d. Administer an opioid analgesic. 58. The nurse teaches a client scheduled for a colonoscopy. Which instruction should be included as part of the preparation for the procedure? a. Consume at least 3 quarts of water 30 minutes before the test. b. Do not void for at least 30 minutes before the test. c. Follow the dietary and fluid restrictions and bowel preparation procedures.d. Spray or gargle with a local anesthetic. 59. The nurse is collecting a stool specimen from a patient. What characteristic of the stool indicates to the nurse that the patient may have an upper GI bleed? a. Clay-colored b. Greasy and foamy c. Tarry and black d. Threaded with mucus 60. A client was diagnosed with pernicious anemia. Which vitamin cannot be absorbed without an intrinsic factor? a. Vitamin A b. Vitamin B12 c. Vitamin C d. Vitamin D 61. A client reports having red stools lately. What will the nurse ask during assessment questioning? a. "Have you been eating beets?" b. "Have you been drinking grape juice?" c. "Have you been eating spinach?" d. "Have you been taking an iron supplement?" 62. The nurse assesses bowel sounds and hears one to two bowel sounds in 2 minutes. How should the nurse document the bowel sounds? a. normal b. hyperactive c. hypoactive d. absent 63. A nurse is caring for a client who needs a nasogastric (NG) tube for a tube feeding. What is the safe method for thenurse to use to measure the appropriate length of the NG tube? a. A length of 50 cm (20 in) b. The distance measured from the nose to the xiphoid process c. The distance measured from the tip of the nose to the earlobe and from the earlobe to the xiphoid process d. The distance measured from the tragus of the ear to the xiphoid process 64. A client receives tube feedings after an oral surgery. The nurse manages tube feedings to minimize the risk of aspiration. Which measure should the nurse include in the care plan to reduce the risk of aspiration? a. Change the tube feeding container ,tubing, and adjust patient head of bed . b. Avoid cessation of feedings and adjust patient head of bed. c. Use semi-Fowler position during, and 60 minutes after, an intermittent feeding. d. Administer 15 to 30 mL of water before and after medications and feedings. 65. The client is on a continuous tube feeding. The nurse determines the tube placement should be checked every a. shift. b. hour. c. 12 hours. d. 24 hours. 66. A client with a peptic ulcer is about to begin a therapeutic regimen that includes a bland diet, antacids, and famotidine. Before the client is discharged, the nurse should provide which instruction? a. "Eat three balanced meals every day." b. "Stop taking the drugs when your symptoms subside." c. "Avoid aspirin and products that contain aspirin." d. "Increase your intake of fluids containing caffeine." 67. The nurse is assessing a client with a bleeding gastric ulcer. When examining the client's stool, which characteristic would the nurse be most likely to find?a. Green color and texture b. Bright red blood in stool c. Black and tarry appearance d. Clay-like quality 68. Which of the following medications is classified as a proton pump inhibitor (PPI)? a. Omeprazole b. Nizatidine c. Cimetidine d. Famotidine 69. A client taking metronidazole for the treatment of H. pylori states that the medication is causing nausea. What teaching should the nurse provide to the client to alleviate the nausea? a. Discontinue the use of the medication. b. Ask the healthcare provider to prescribe another type of antibiotic. c. Take the medication with meals to decrease the nausea. d. Crush the medication and put it in applesauce. 70. A nurse is caring for a client who is undergoing a diagnostic workup for a suspected gastrointestinal problem. The client reports gnawing epigastric pain following meals and heartburn. What would the nurse suspect this client has? a. peptic ulcer disease b. ulcerative colitis c. appendicitis d. diverticulitis 71. A nurse is teaching a group of middle-aged men about peptic ulcers. When discussing risk factors for peptic ulcers, the nurse should mention: a. a sedentary lifestyle and smoking. b. a history of hemorrhoids and smoking. c. alcohol abuse and a history of acute renal failure. d. alcohol abuse and smoking.72. The nurse is conducting a community education class on gastritis. The nurse includes that chronic gastritis caused by Helicobacter pylori is implicated in which disease/condition? a. Pernicious anemia b. Systemic infection c. Peptic ulcers d. Colostomy 73. A client is in the hospital for the treatment of peptic ulcer disease. The client reports vomiting and a sudden severe pain in the abdomen. The nurse then assesses a board-like abdomen. What does the nurse suspect these symptoms indicate? a. Ineffective treatment for the peptic ulcer b. A reaction to the medication given for the ulcer c. Gastric penetration d. Perforation of the peptic ulcer 74. When caring for a client with an acute exacerbation of a peptic ulcer, the nurse finds the client doubled up in bed with severe pain in the right shoulder. What is the initial appropriate action by the nurse? a. Notify the health care provider. b. Irrigate the client's NG tube. c. Place the client in the high-Fowler's position. d. Assess the client's abdomen and vital signs. 75. A patient has been diagnosed with acute gastritis and asks the nurse what could have caused it. What is the best response by the nurse? (Select all that apply.) a. “It can be caused by ingestion of strong acids.” b. “You may have ingested some irritating foods.” c. “Is it possible that you are overusing aspirin.” d. “It is a hereditary disease.” e. “It is probably your nerves.” 76.A client realizes that regular use of laxatives has greatly improved bowel patterns. However, the nurse cautions this client against the prolonged use of laxatives for which reason? a. The client may develop inflammatory bowel disease. b. The client may develop arthritis or arthralgia. c. The client's natural bowel function may become sluggish. d. The client may lose his or her appetite. 77. A nurse conducts the Romberg test on a client by asking the client to stand with the feet close together and the eyes closed. As a result of this posture, the client suddenly sways to one side and is about to fall when the nurse intervenes and saves the client from being injured. How should the nurse interpret the client's result? a. Positive Romberg test, indicating a problem with level of consciousness b. Negative Romberg test, indicating a problem with body mass c. Negative Romberg test, indicating a problem with vision d. Positive Romberg test, indicating a problem with equilibrium 78. A client the nurse is caring for experiences a seizure. What would be a priority nursing action? a. Restrain the client during the seizure. b. Insert a tongue blade between the teeth. c. Protect the client from injury. d. Suction the mouth during the convulsion. 79. A client is having a tonic-clonic seizure. What should the nurse do first? a. Elevate the head of the bed. b. Restrain the client's arms and legs. c. Place a tongue blade in the client's mouth. d. Take measures to prevent injury. 80.A client with meningitis has a history of seizures. Which activity should the nurse do while the client is actively seizing? a. Place a cooling blanket beneath the client b. Provide oxygen or anticonvulsants, whichever is available c. Turn the client to the side during a seizure and do not restrain movements d. Suction the client's mouth and pharynx 81. The nurse is caring for a patient with an altered LOC. What is the first priority of treatment for this patient? a. Assessment of pupillary light reflexes b. Determination of the cause c. Positioning to prevent complications d. Maintenance of a patent airway 82. A home care nurse makes a visit to a client with Parkinson's disease who is being cared for by his spouse. During the visit, the spouse says, "I'm just so tired. I have to do just about everything for him." Which response by the nurse would be most appropriate? a. "You're doing a great job. Just keep it up." b. "It must be difficult for you to see your husband like this." c. "Are you upset about how your husband is doing?" d. "You sound a bit overwhelmed. Tell me more about what's happening." 83. A nurse is providing care to a client with Parkinson's disease. The nurse understands the client's signs and symptoms are related to a depletion of which of the following? a. Serotonin b. Acetylcholine c. Dopamine d. Norepinephrine 84. A client with Parkinson's disease asks the nurse what their treatment is supposed to do since the disease is progressive. What would be the nurse's best response?a. “Treatment aims at keeping you independent as long as possible.” b. “Treatment really doesn't matter; the disease is going to progress anyway.” c. “Treatment for Parkinson's is only palliative; it keeps you comfortable.” d. ”Treatment aims at keeping you emotionally healthy by making you think you are doing something to fight this disease.” 85. Which topic is most important for the nurse to include in the teaching plan for a client newly diagnosed with Parkinson’s disease? a. Involvement with diversion activities b. Enhancement of the immune system c. Establishing balanced nutrition d. Maintaining a safe environment 86. Which is a by-product of fat breakdown in the absence of insulin and accumulates in the blood and urine? a. Ketones b. Creatinine c. Hemoglobin d. Cholesterol 87. When referred to a podiatrist, a client newly diagnosed with diabetes mellitus asks, "Why do you need to check my feet when I'm having a problem with my blood sugar?" The nurse's most helpful response to this statement is: a. "The physician wants to be sure your shoes fit properly so you won't develop pressure sores." b. "The circulation in your feet can help us determine how severe your diabetes is." c. "Diabetes can affect sensation in your feet and you can hurt yourself without realizing it." d. "It's easier to get foot infections if you have diabetes." 88. A client with newly diagnosed type 2 diabetes is admitted to the metabolic unit. The primary goal for this admission is education. Which goal should the nurse incorporate into her teaching plan? a. Maintenance of blood glucose levels between 180 and 200 mg/dlb. Smoking reduction but not complete cessation c. An eye examination every 2 years until age 50 d. Weight reduction through diet and exercise 89. A client has type 1 diabetes. Her husband finds her unconscious at home and administers glucagon, 0.5 mg subcutaneously. She awakens in 5 minutes. Why should her husband offer her a complex carbohydrate snack as soon as possible? a. To decrease the possibility of nausea and vomiting b. To restore liver glycogen and prevent secondary hypoglycemia c. To stimulate her appetite d. To decrease the amount of glycogen in her system 90. An older adult patient that has type 2 diabetes comes to the emergency department with second-degree burns to the bottom of both feet and states, "I didn't feel too hot but my feet must have been too close to the heater." What does the nurse understand is most likely the reason for the decrease in temperature sensation? a. A faulty heater b. Autonomic neuropathy c. Peripheral neuropathy d. Sudomotor neuropathy 91. Which would be included in the teaching plan for a client diagnosed with diabetes mellitus? a. An elevated blood glucose concentration contributes to complications of diabetes, such as diminished vision. b. Sugar is found only in dessert foods. c. The only diet change needed in the treatment of diabetes is to stop eating sugar. d. Once insulin injections are started in the treatment of type 2 diabetes, they can never be discontinued. 92. A client is admitted to the health care center with abdominal pain, nausea, and vomiting. The medical reports indicate a history of type 1 diabetes. The nurse suspects the client’ssymptoms to be those of diabetic ketoacidosis (DKA). Which action will help the nurse confirm the diagnosis? a. Assess the client's ability to take a deep breath b. Assess the client's ability to move all extremities c. Assess the client's breath odor d. Assess for excessive sweating 93. A diabetic nurse is working for the summer at a camp for adolescents with diabetes. When providing information on the prevention and management of hypoglycemia, what action should the nurse promote? a. Always carry a form of fast-acting sugar. b. Perform exercise prior to eating whenever possible. c. Eat a meal or snack every 8 hours. d. Check blood sugar at least every 24 hours. 94. A client with diabetes mellitus is receiving an oral antidiabetic agent. The nurse observes for which symptom when caring for this client? a. Polyuria b. Hypoglycemia c. Blurred vision d. Polydipsia 95. A client with diabetes comes to the clinic for a follow-up visit. The nurse reviews the client's glycosylated hemoglobin test results. Which result would indicate to the nurse that the client's blood glucose level has been well-controlled? a. 6.5% b. 7.5 % c. 8.0% d. 8.5% 96. Which information should be included in the teaching plan for a client receiving glargine, a “peakless” basal insulin?a. Administer the total daily dosage in two doses. b. Draw up the drug first, then add regular insulin. c. It is rapidly absorbed and has a fast onset of action. d. Do not mix with other insulins. 97. A client with diabetes mellitus must learn how to selfadminister insulin. The physician has ordered 10 units of U- 100 regular insulin and 35 units of U-100 isophane insulin suspension (NPH) to be taken before breakfast. When teaching the client how to select and rotate insulin injection sites, the nurse should provide which instruction? a. "Inject insulin into healthy tissue with large blood vessels and nerves." b. "Rotate injection sites within the same anatomic region, not among different regions." c. "Administer insulin into areas of scar tissue or hypertrophy whenever possible." d. "Administer insulin into sites above muscles that you plan to exercise heavily later that day." 98. Which particular area(s) should be examined to assess peripheral edema? a. Upper arms b. Under the sacrum c. Lips, earlobes d. Feet, ankles 99. A nurse is caring for a client who is recovering from a myocardial infarction (MI). The cardiologist refers the client to cardiac rehabilitation. Which statement by the client indicates an understanding of cardiac rehabilitation? a. "When I finish the rehabilitation program I'll never have to worry about heart trouble again." b. "I won't be able to jog again even with rehabilitation." c. "Rehabilitation will help me function as well as I physically can." d. "I'll get rest during these rehabilitation classes. All I have to do is sit and listen to the instructor." 100. A nurse teaches a client with angina pectoris that he or she needs to take up to three sublingual nitroglycerin tablets at 5-minute intervals and immediately notify the health careprovider if chest pain doesn't subside within 15 minutes. What symptoms may the client experience after taking the nitroglycerin? a. Nausea, vomiting, depression, fatigue, and impotence. b. Sedation, nausea, vomiting, constipation, and respiratory depression. c. Headache, hypotension, dizziness, and flushing. d. Flushing, dizziness, headache, and pedal edema. 101. A nurse is educating a community group about coronary artery disease. One member asks about how to avoid coronary artery disease. Which of the following items are considered modifiable risk factors for coronary artery disease? Choose all that apply. a. Hyperlipidemia b. Gender c. Obesity d. Race e. Tobacco use 102. A nurse is developing a nursing care plan for a client with peripheral arterial disease. Which of the following will be the priority nursing diagnosis? a. Ineffective peripheral tissue perfusion b. Impaired tissue integrity c. Ineffective thermoregulation d. Ineffective self-health management 103. A client with venous insufficiency is instructed to exercise, apply elastic stockings, and elevate the extremities. Which is the primary benefit for this nursing management regime? a. Improve arterial flow b. Strengthen venous valves c. Increase venous congestion d. Improve venous return 104.A nurse is teaching a client who will soon be discharged with a prescription for warfarin (Coumadin). Which statement should the nurse include in discharge teaching? a. "Eat more yogurt and broccoli." b. "This drug will dissolve any clots you may still have." c. "If you miss a dose, double the next dose." d. "Don't take aspirin while you're taking warfarin." 105. A nurse is teaching a client newly diagnosed with arterial insufficiency. Which term should the nurse use to refer to leg pain that occurs when the client is walking? a. Dyspnea b. Orthopnea c. Thromboangiitis obliterans d. Intermittent claudication 106. Health teaching for a patient diagnosed with Raynaud's phenomenon would include advising the patient to avoid the most common factor known to trigger episodes. Which of the following is the most common factor? a. Allergens b. Strenuous exercise c. Cold and stress d. Jobs/hobbies that involve vibrations 107. A nurse is reviewing self-care measures for a client with peripheral vascular disease. Which statement indicates proper self-care measures? a. "I like to soak my feet in the hot tub every day." b. "I walk only to the mailbox in my bare feet." c. "I stopped smoking and use only chewing tobacco." d. "I have my wife look at the soles of my feet each day." 108. A nurse is assessing a client's right lower leg, which is wrapped with an elastic bandage. Which signs and symptoms suggest circulatory impairment?a. Numbness, cool skin temperature, and pallor b. Swelling, warm skin temperature, and drainage c. Numbness, warm skin temperature, and redness d. Redness, cool skin temperature, and swelling 109. A client with venous insufficiency asks the nurse what they can do to decrease their risk of complications. What advice should the nurse provide to clients with venous insufficiency? a. Elevate the legs periodically for at least an hour. b. Avoid foods with iodine. c. Elevate the legs periodically for at least 15 to 20 minutes. d. Refrain from sexual activity for a week. 110. A client with systemic lupus erythematosus (SLE) complains that his hands become pale, blue, and painful when exposed to the cold. What disease should the nurse cite as an explanation for these signs and symptoms? a. Peripheral vascular disease b. Raynaud's disease c. Arterial occlusive diseases d. Buerger's disease 111. The nurse is monitoring a patient who is on heparin anticoagulant therapy. What should the nurse determine the therapeutic range of the international normalized ratio (INR) should be? a. 2.0–3.0 b. 4.0–5.0 c. 5.0–6.0 d. 7.0–8.0 112. The nurse is caring for a client newly diagnosed with hypertension. Which statement by the client indicates the need for further teaching?a. “If I take my blood pressure and it is normal, I don’t have to take my blood pressure pills.” b. “I think I’m going to sign up for a yoga class twice a week to help reduce my stress.” c. “When getting up from bed, I will sit for a short period before standing up.” d. “I will consult a dietician to help get my weight under control.” 113. A client diagnosed with hypertension begins drug therapy using an antihypertensive agent. The nurse instructs the client’s spouse to remove any objects in the home that can lead to falls. Which client statement confirms that the teaching has been successful? a. "Antihypertensive drugs can lead to falls." b. "Constant thirst is a common side effect of antihypertensive therapy." c. "Insomnia is a common side effect of antihypertensive medications." d. "Antihypertensives can lead to memory loss." 114. When interpreting the results of a Mantoux test, the nurse explains to the client that a reaction occurs when the intradermal injection site shows a. redness and induration. b. drainage. c. tissue sloughing. d. bruising. 115. A nurse caring for a client with deep vein thrombosis must be especially alert for complications such as pulmonary embolism. Which findings suggest pulmonary embolism? a. Nonproductive cough and abdominal pain b. Hypertension and lack of fever c. Bradypnea and bradycardia d. Chest pain and dyspnea 116. Which is the most important risk factor for development of chronic obstructive pulmonary disease (COPD)? a. Occupational exposure b. Cigarette smoking c. Air pollutiond. Genetic abnormalities 117. When developing a preventative plan of care for a patient at risk for developing chronic obstructive pulmonary disease (COPD), which of the following should be incorporated? a. Smoking cessation b. Weight reduction c. Cholesterol management d. Cancer prevention 118. Which vaccine should a nurse encourage a client with chronic obstructive pulmonary disease (COPD) to receive? a. Varicella b. Influenza c. Hepatitis B d. Human papilloma virus (HPV) 119. For a client with chronic obstructive pulmonary disease, which nursing intervention helps maintain a patent airway? a. Restricting fluid intake to 1,000 ml/day b. Enforcing absolute bed rest c. Teaching the client how to perform controlled coughing d. Administering ordered sedatives regularly and in large amounts 120. The nurse is caring for a client with extensive respiratory disease. Which is a late sign of hypoxia the client may experience? a. Restlessness b. Cyanosis c. Hypotension d. Somnolence 121. The nurse is teaching the client in respiratory distress ways to prolong exhalation to improve respiratory status. The nurse tells the client toa. Sit in an upright position only. b. Initially inhale through the mouth. c. Purse the lips when exhaling air from the lungs. d. Hold the breath for 5 seconds and then exhale. 122. At 11 p.m., a client is admitted to the emergency department. He has a respiratory rate of 44 breaths/minute. He's anxious, and wheezes are audible. The client is immediately given oxygen by face mask and methylprednisolone (Depo-Medrol) I.V. At 11:30 p.m., the client's arterial blood oxygen saturation is 86%, and he's still wheezing. The nurse should plan to administer: a. alprazolam (Xanax). b. propranolol (Inderal). c. morphine. d. albuterol (Proventil). 123. Which of the following is the hallmark symptom for peripheral arterial disease (PAD) in the lower extremity? a. Intermittent claudication b. Acute limb ischemia c. Dizziness d. Vertigo 124. Which elements of assessment of a traumatic musculoskeletal injury should be included when a client is evaluated. Select all that apply. a. All should be included. b. Observe for swelling, external bleeding, or bruising. c. Palpate the peripheral pulses. d. Check the sensation of the injured part. 125. The nurse is reading the admission note for a client with a bone fracture that requires surgery. The note indicates the presence of crepitus. The nurse interprets this as being a. bleeding. b. a crackling sound. c. ecchymosis.d. a closed fracture. 126. A client is in Buck's traction after fracturing his right hip. The nurse should include which action in the care plan? a. Removing the weights once every shift b. Maintaining the bed in the knee gatch position c. Keeping the client in semi-Fowler's position d. Maintaining correct body alignment 127. Primary prevention of osteoporosis includes: a. placing items within the client's reach. b. installing grab bars in the bathroom to prevent falls. c. optimal calcium intake and estrogen replacement therapy. d. using a professional alert system in the home in case a client falls when she's alone. 128. Which common problem of the upper extremity results from entrapment of the median nerve at the wrist? a. Ganglion b. Carpal tunne [Show More]
Last updated: 1 year ago
Preview 1 out of 36 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 13, 2021
Number of pages
36
Written in
Additional information
This document has been written for:
Uploaded
Oct 13, 2021
Downloads
0
Views
57


.png)

 ORGMED ORGANIC PHARMACEUTICAL PHARMACY.png)



.png)