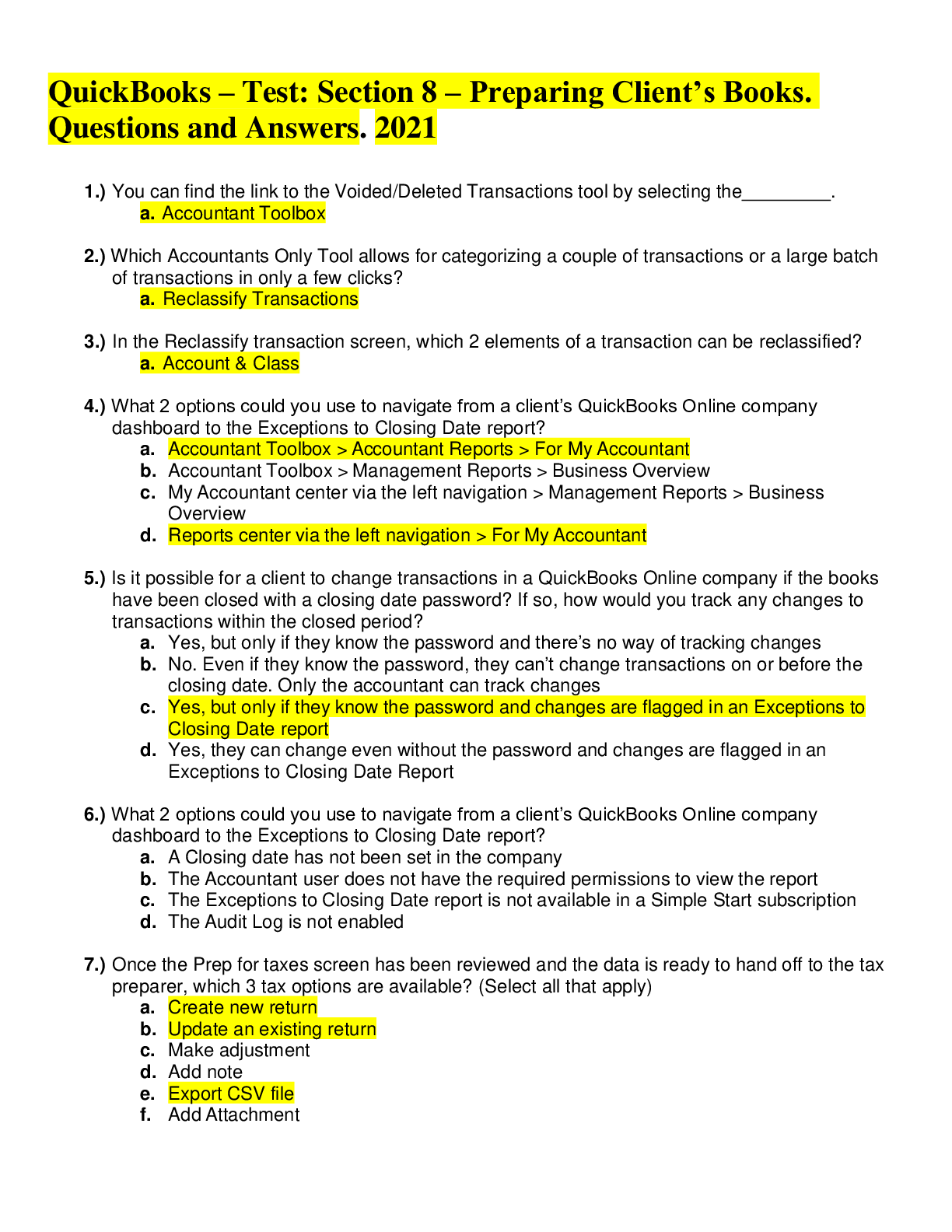
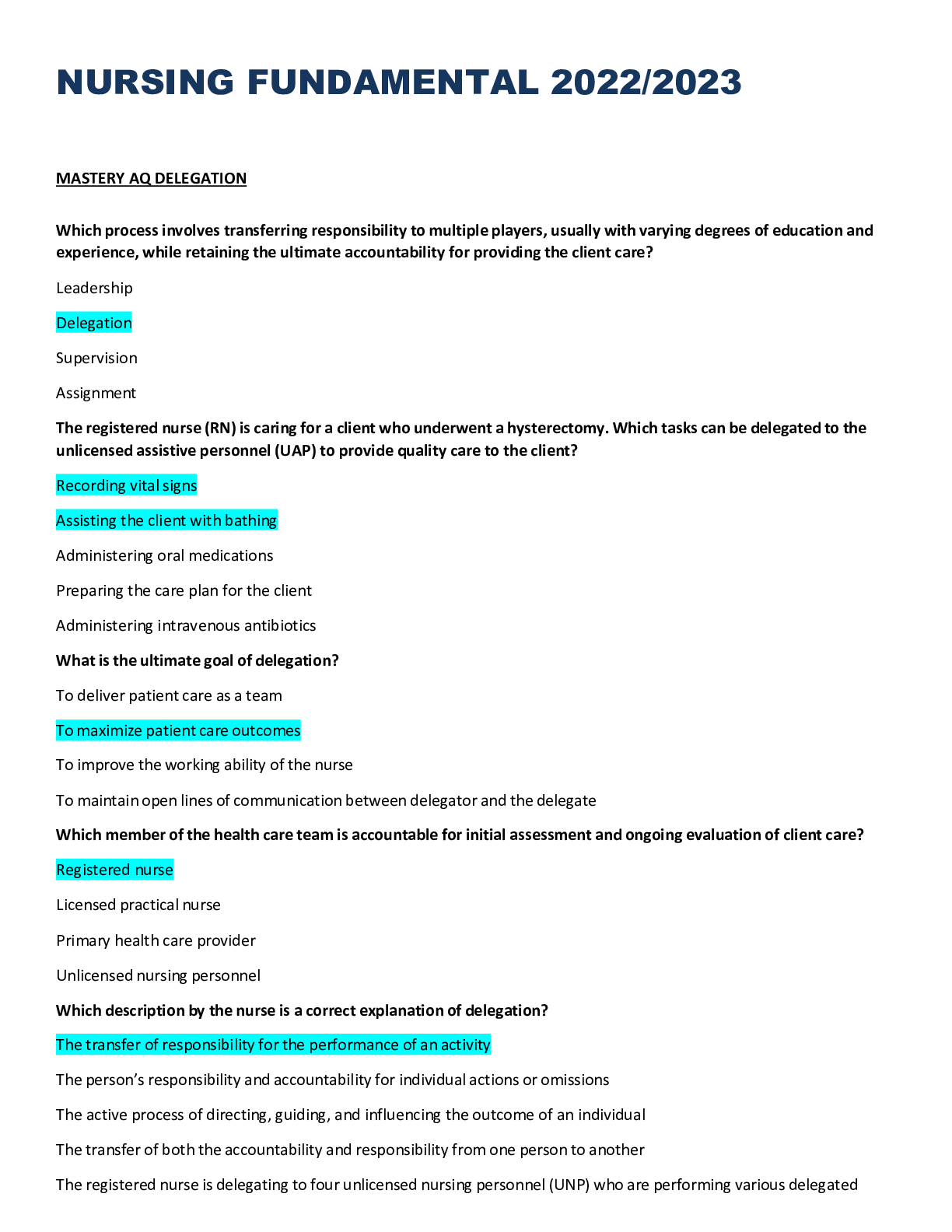
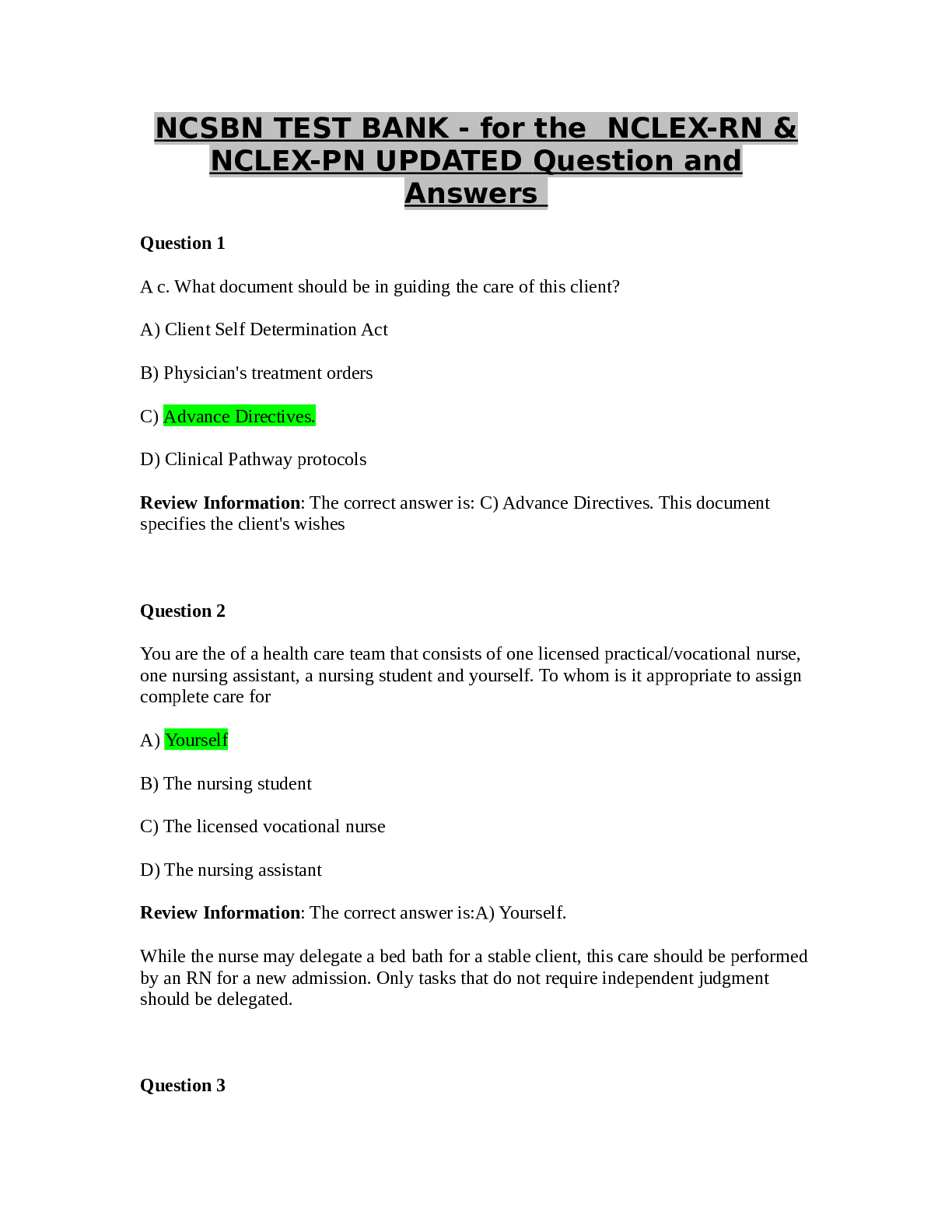
*NURSING > QUESTIONS & ANSWERS > Concorde Career Colleges NURSING 240 Questions and Answers (All)
Concorde Career Colleges NURSING 240 Questions and Answers
Document Content and Description Below
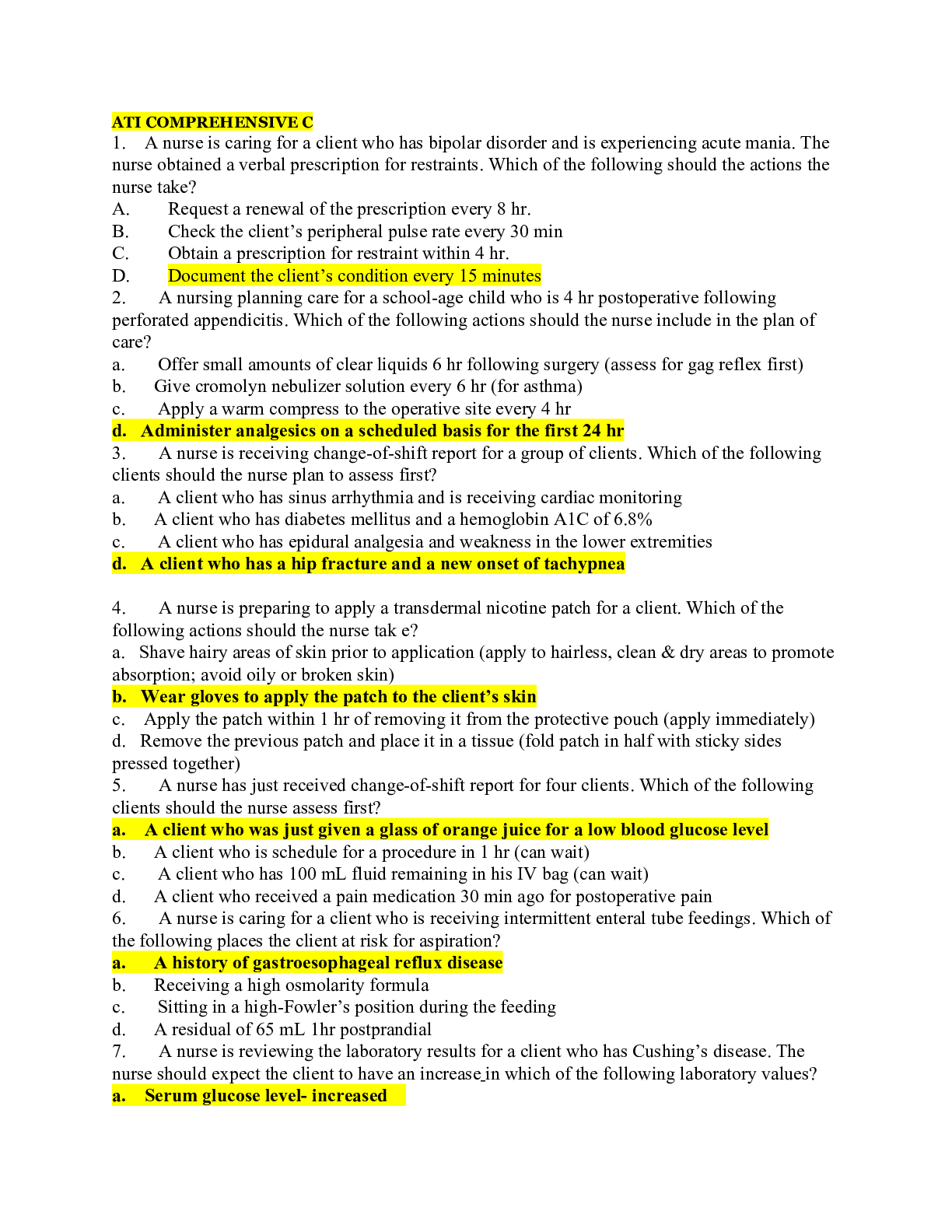
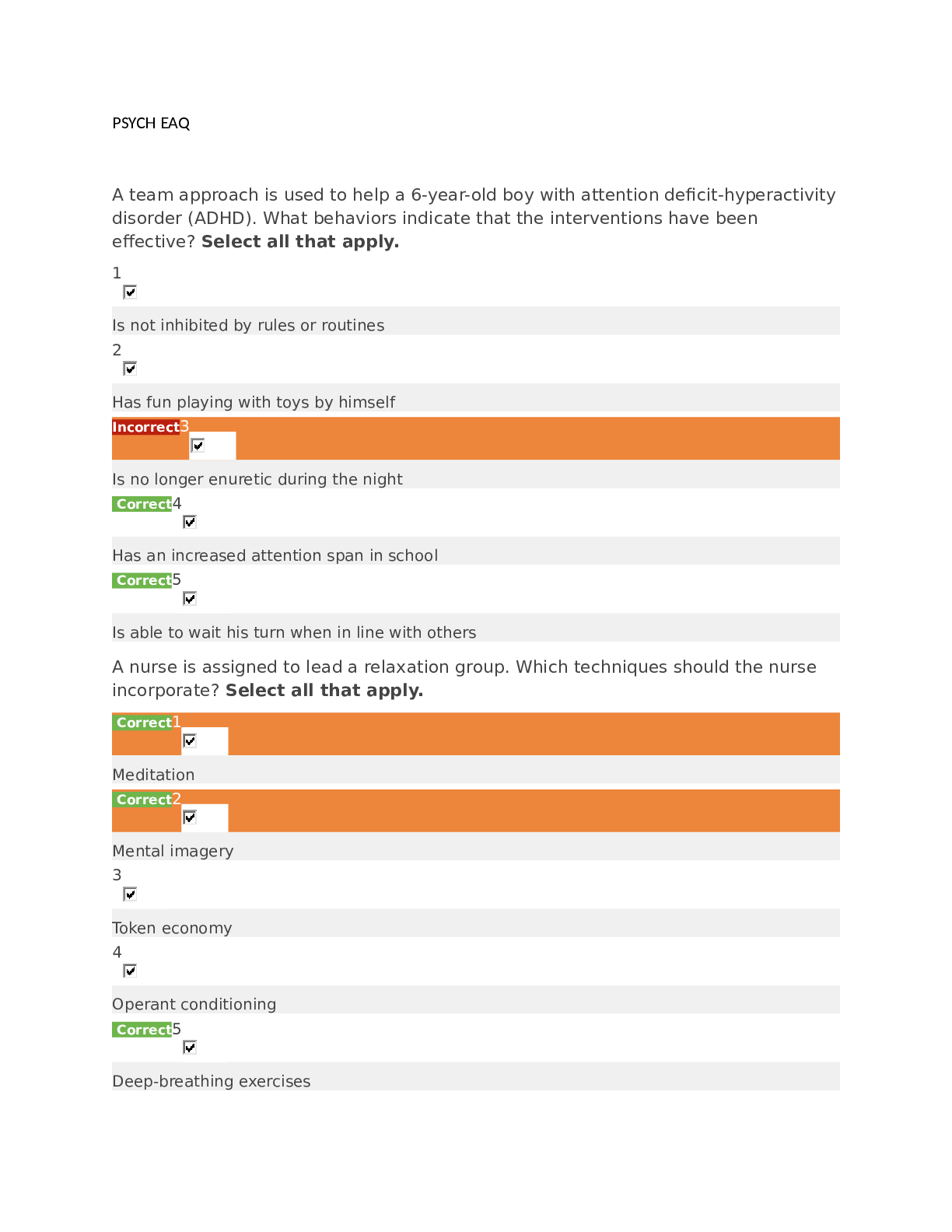
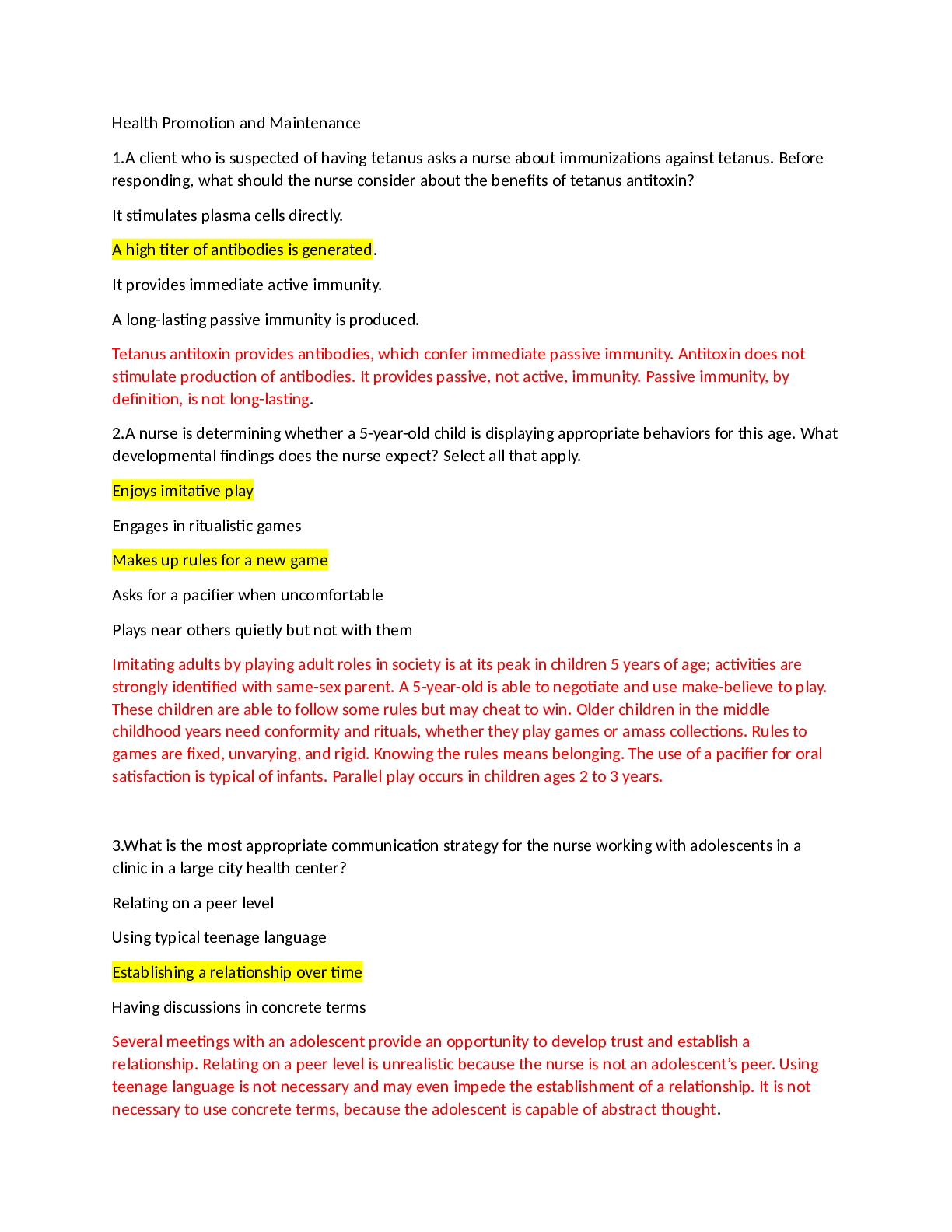
1. A home care nurse is instructing a client with hyperemesis gravidarum about measures to ease the nausea and vomiting. The nurse tells the client to: A. Eat foods high in calories and fat B. Lie ... down for at least 20 minutes after meals C. Eat carbohydrates such as cereals, rice, and pasta Correct D. Consume primarily soups and liquids at mealtimes Rationale: Low-fat foods and easily digested carbohydrates such as fruit, breads, cereals, rice, and pasta provide important nutrients and help prevent a low blood glucose level, which can cause nausea. Soups and other liquids should be taken between meals to avoid distending the stomach and triggering nausea. Sitting upright after meals reduces gastric reflux. Additionally, food portions should be small and foods with strong odors should be eliminated from the diet, because food smells often incite nausea. A nurse is caring for a client with preeclampsia who is receiving a magnesium sulfate infusion to prevent eclampsia. Which finding indicates to the nurse that the medication is effective? E. Clonus is present. Incorrect F. Magnesium level is 10 mg/dL. G. Deep tendon reflexes are absent. H. The client experiences diuresis within 24 to 48 hours. Correct Rationale: Magnesium sulfate is effective in preventing seizures (eclampsia) if diuresis occurs within 24 to 48 hours of the start of the infusion. As part of the therapeutic response, renal perfusion is increased and the client is free of visual disturbances, headache, epigastric pain, clonus (the rapid rhythmic jerking motion of the foot that occurs when the client’s lower leg is supported and the foot is sharply dorsiflexed), and seizure activity. Hyperreflexia indicates cerebral irritability. Clonus is normally not present. The therapeutic magnesium level is 4 to 8 mg/dL. Reflexes range from 1+ to 2+ but should not be absent. A client with preeclampsia who is receiving magnesium sulfate in an intravenous infusion exhibits signs of magnesium toxicity. The nurse immediately prepares for the administration of: I. Vitamin K J. Protamine sulfate Incorrect K. Calcium gluconate Correct L. Naloxone hydrochloride Rationale: Calcium gluconate is the antidote to magnesium sulfate because it antagonizes the effects of magnesium at the neuromuscular junction. It should be readily available whenever magnesium is administered. Vitamin K is the antidote in cases of hemorrhage induced by the administration of oral anticoagulants such as warfarin sodium (Coumadin). Protamine sulfate is theantidote in cases of hemorrhage induced by the administration of heparin. Naloxone hydrochloride is administered to treat opioid-induced respiratory depression. A nurse instructs a pregnant client about foods that are high in folic acid. Which item does the nurse tell the client is the best source of folic acid? M. Milk N. Steak O. Chicken P. Lima beans Correct Rationale: The best sources of folic acid are liver; kidney, pinto, lima, and black beans; and fresh dark-green leafy vegetables. Other good sources of folic acid are orange juice, peanuts, refried beans, and peas. Milk is high in calcium. Chicken and steak are high in protein. A nurse is providing instructions to a mother of an infant with seborrheic dermatitis (cradle cap) about treatment of the condition. The nurse tells the mother to: Q. Avoid the use of shampoo on the infant’s scalp Incorrect R. Apply oil to the affected area on the infant’s scalp Correct S. Wash the infant’s scalp daily, using only tepid water T. Shampoo the infant’s scalp, avoiding the anterior fontanel area Rationale: Seborrheic dermatitis, a chronic inflammation of the scalp or other areas of the skin, is characterized by yellow, scaly, oily lesions. It sometimes results when parents do not wash over the anterior fontanel carefully for fear that they will hurt the infant. Treatment includes the application of oil (e.g., mineral oil) to the area to help soften the lesions followed by gentle removal of the scaly lesions with a comb before the head is shampooed. The nurse should teach the mother how to shampoo the scalp and explain that she will not damage the fontanel with normal gentle shampooing. The scalp should be rinsed well to remove all soap, which could cause irritation. A nurse is monitoring a client who was given an epidural opioid for a cesarean birth. The nurse notes that the client’s oxygen saturation on pulse oximetry is 92%. The nurse first: U. Notifies the registered nurse V. Documents the findings W. Instructs the client to take several deep breaths Correct X. Administers 100% oxygen by way of face mask Incorrect Rationale: If the client has been given an epidural opioid, the nurse should monitor the client’s respiratory status closely. If the oxygen saturation falls below 95%, the nurse instructs the client to take several deep breaths to increase the level. Although the finding would be documented, action is required to increase the oxygen saturation level. It is not necessary to contact the registered nurse. Ifthe deep breaths fail to increase the oxygen saturation level, the registered nurse is notified and may prescribe oxygen. A client who delivered a healthy newborn 11 days ago calls the clinic and tells the nurse that she is experiencing a white vaginal discharge. The nurse tells the client: Y. To perform a vaginal douche Z. To come to the clinic for a checkup Incorrect AA. That this is an indication of an infection AB. That this is a normal postpartum occurrence Correct Rationale: For the first 3 days following childbirth, lochia consists almost entirely of blood, with small particles of decidua and mucus, and is called lochia rubra because of its red color. The amount of blood decreases by about the fourth day, and which time the lochia changes from red to pink or brown-tinged; this stage is called lochia serosa. By about the 11th day, the erythrocyte component of lochia has decreased and the discharge becomes white or cream-colored. This final stage is known as lochia alba. Lochia alba contains leukocytes, decidual cells, epithelial cells, fat, cervical mucus, and bacteria. It is present in most women until the third week after childbirth but may persist for as long as 6 weeks. Lochia alba is a normal finding during the postpartum course, and no intervention is required, so the other options are incorrect. A rubella antibody screen is performed in a pregnant client, and the results indicate that the client is not immune to rubella. The nurse tells the client that: AC. A rubella vaccine must be administered immediately Incorrect AD. A rubella vaccine must be administered after childbirth Correct AE. She will not contract rubella if she is exposed to the disease AF. She does not need to be concerned about being exposed to rubella Rationale: A prenatal rubella antibody screen is performed in every pregnant woman to determine whether she is immune to rubella, which can cause serious fetal anomalies. If she is not immune, rubella vaccine is offered after childbirth to keep her from contracting rubella during subsequent pregnancies. The vaccine is a live virus, and defects might occur in the fetus if the vaccine were administered during pregnancy or if the mother were to become pregnant soon after it was administered. Administering a rubella vaccine immediately places the fetus at risk. Telling the client that she does not need to be concerned about being exposed to rubella is incorrect, because the possibility of exposure, which could be harmful to the fetus, does exist. A nurse is monitoring a client who delivered a healthy newborn 12 hours ago. The nurse takes the client’s temperature and notes that it is 38° C (100.4° F). The most appropriate nursing action would be to: AG. Notify the registered nurse AH. Recheck the temperature in 1 hour IncorrectAI. Encourage the intake of oral fluids Correct AJ. Tell the client that antibiotics will be prescribed Rationale: A temperature of 38° C (100.4° F) is common during the 24 hours after childbirth. It may be the result of dehydration or normal postpartum leukocytosis. If the increased temperature persists for longer than 24 hours or exceeds 38° C, infection is a possibility, and the fever is reported to the registered nurse. Because the client delivered her baby just 12 hours ago, the most appropriate nursing action is to encourage the intake of oral fluids. A nurse is assessing the uterine fundus of a client who has just delivered a baby and notes that the fundus is boggy. The nurse massages the fundus, and then presses to expel clots from the uterus. To prevent uterine inversion during this procedure, the nurse: AK. Has the client void before the uterine assessment AL. Tells the woman to bear down during fundal message AM. Simultaneously provides pressure over the lower uterine segment Correct AN. Asks the client to take slow, deep breaths during fundal assessment Incorrect Rationale: After massaging a boggy fundus until it is firm, the nurse presses the fundus to expel clots from the uterus. The nurse must also keep one hand pressed firmly just above the symphysis (over the lower uterine segment) the entire time. Removing the clots allows the uterus to contract properly. Providing pressure over the lower uterine segment prevents uterine inversion. Having the client void before uterine assessment will not prevent uterine inversion. Telling the woman to bear down while the nurse performs fundal message and asking the client to take slow, deep breaths during fundal assessment also will not prevent uterine inversion. A nurse is monitoring a client after vaginal delivery notes a constant trickle of bright-red blood from the client’s vagina. In which order would the nurse perform the following actions? Assign the number 1 to the first action and the number 5 to the last. Incorrect A. Assessing the client’s fundus B. Checking the client’s vital signs C. Changing the client’s peripads D. Contacting the physician E. Documenting the findings The correct order is: F. Assessing the client’s fundus G. Checking the client’s vital signs H. Contacting the physician I. Changing the client’s peripads J. Documenting the findings Rationale: A constant trickle of bright-red blood may indicate abnormal bleeding and requires immediate attention. The nurse first checks the client’s fundus. Once it has been determined that thebleeding is not the result of a boggy uterus, the nurse should check the vital signs to determine whether the blood loss has compromised the client’s condition. Next the nurse would contact the physician and report the bleeding, fundal height and condition, and vital signs. After contacting the physician the nurse would attend to the client’s comfort needs, including, in this case, frequent changes of peripads. The nurse would document the findings once assessment and implementation had been completed and the client’s condition was considered stable. A nonstress test is performed, and the physician documents “accelerations lasting less than 15 seconds throughout fetal movement.” The nurse interprets these findings as: A. Normal B. Reactive Incorrect C. Nonreactive Correct D. Inconclusive Rationale: A reactive nonstress test is a normal, or negative, result and indicates a healthy fetus. The result requires two or more fetal heart rate accelerations of at least 15 beats/min lasting at least 15 seconds from the beginning of the acceleration to the end, in association with fetal movement, during a 20-minute period. A nonreactive test is an abnormal test, showing no accelerations or accelerations of less than 15 beats/min or lasting less than 15 seconds during a 40-minute observation. An inconclusive result is one that cannot be interpreted because of the poor quality of the fetal heart rate recording. A stillborn infant was delivered a few hours ago. After the birth, the family remains together, holding and touching the baby. Which statement by the nurse is appropriate? E. “I know how you feel.” F. “This must be hard for you.” Correct G. “Now you have an angel in heaven.” H. “You’re young. You can have other children.” Rationale: Therapeutic communication helps the mother, father, and other family members express their feelings and emotions. “This must be hard for you” is a caring and empathetic response, focused on feelings and encouraging communication. The other options are nontherapeutic and may devalue the family members' feelings. A nurse is providing nutritional counseling to pregnant client with a history of cardiac disease. What does the nurse advise the client to eat? I. Water and pretzels J. Low-fat cheese omelet Incorrect K. Nachos and fried chicken L. Apple and whole-grain toast CorrectRationale: The pregnant woman needs a well-balanced diet high in iron and protein and adequate in calories for weight gain. Iron supplements that are taken during pregnancy tend to cause constipation. Constipation causes the client to strain during defecation, inadvertently performing the Valsalva maneuver, which causes blood to rush to the heart and overload the cardiac system. The pregnant woman, then, should increase her intake of fluids and fiber. An unlimited intake of sodium (pretzels, cheese, nachos) could cause overload of the circulating blood volume and contribute to the cardiac condition. A nurse is reviewing the records of the clients admitted to the maternity unit during the past 24 hours. Which of the following clients does the nurse recognize as being at risk for the development of disseminated intravascular coagulation (DIC)? Select all that apply. M. A client with septicemia Correct N. A client with mild preeclampsia Incorrect O. A client with diabetes mellitus who delivered a 10-lb baby Incorrect P. A client who had a cesarean section because of abruptio placentae Correct Q. A client who delivered 12 hours ago and has lost 475 mL of blood Rationale: DIC is a pathologic form of clotting that is diffuse and consumes large amounts of clotting factors, including platelets, fibrinogen, prothrombin, and factors V and VII. In the obstetric population, DIC occurs as a result of abruptio placentae, amniotic fluid embolism, dead fetus syndrome (in which the fetus has died but is retained in utero for at least 6 weeks), severe preeclampsia, septicemia, cardiopulmonary arrest, or hemorrhage. A loss of 475 mL is not considered hemorrhage .A mild case of preeclampsia is not a risk factor for DIC. It is not unusual for a client with diabetes mellitus to deliver a large baby, and this condition is unrelated to DIC. A delivery room nurse is preparing a client for a cesarean delivery. The client is placed on the delivery room table, and the nurse positions the client: R. Prone S. In a semi-Fowler position T. In the Trendelenburg position U. Supine with a wedge under the right hip Correct Rationale: The pregnant client is positioned so that the uterus is displaced laterally to prevent compression of the inferior vena cava, which causes decreased placental perfusion. This is accomplished by placing a wedge under the hip. Positioning for abdominal surgery necessitates a supine position. The Trendelenburg position places pressure from the pregnant uterus on the diaphragm and lungs, decreasing respiratory capacity and oxygenation. A semi-Fowler or prone position is not practical for this type of abdominal surgery. A nurse is preparing to perform the Leopold maneuvers on a pregnant client. The nurse should first: V. Locate the fetal heart toneW. Position the woman supine X. Ask the client to empty her bladder Correct Y. Count the fetal heart rate for 1 minute Rationale: In preparation for the Leopold maneuvers, the nurse first asks the woman to empty her bladder, which will contribute to the woman’s comfort during the examination. Next the nurse positions the client supine with a wedge placed under the hip to displace the uterus. Often the Leopold maneuvers are performed to aid the examiner in locating the fetal heart tones. Counting the fetal heart rate is not associated with Leopold maneuvers. A nurse is assessing the lochia of a client who delivered a viable newborn 1 hour ago. Which type of lochia would the nurse expect to note at this time? Z. Lochia alba AA. Lochial clots Incorrect AB. Lochia serosa AC. Dark-red lochia rubra Correct Rationale: When the perineum is assessed, the lochia is checked for amount, color, and the presence of clots. The color of the lochia during the fourth stage of labor (1 to 4 hours after birth) is dark red (rubra). This is an expected occurrence until the third day after delivery. Then, from days 4 through 10, the discharge is brownish pink (serosa). Alba is a white discharge that occurs on days 11 to 14. A nurse provides instructions to a breastfeeding mother who is experiencing breast engorgement about measures for treating the problem. The nurse tells the mother to: AD. Take a cool shower just before breastfeeding AE. Avoid breastfeeding during the night time hours to ensure adequate rest AF. Gently massage the breasts during breastfeeding to help empty the breasts Correct AG. Apply heat packs to the breasts for 15 to 20 minutes between feedings to reduce swelling Rationale: Gently massaging the breasts during breast feeding will help empty the breasts. The mother should not avoid breastfeeding during the night; instead, she should breastfeed every 2 hours or pump the breasts. The nurse instructs the woman to apply ice packs, not heat packs, to the breasts between feedings to reduce swelling. It may be helpful for the mother to stand in a warm shower just before feeding to foster relaxation and letdown. When, during the normal postpartum course, would the nurse expect to note the fundal assessment shown in the figure?AH. 4 days after delivery Incorrect AI. The day after delivery AJ. Immediately after delivery Correct AK. When the client’s bladder is full Rationale: Immediately after delivery, the uterine fundus should be at the level of the umbilicus or one to three fingerbreadths below it and in the midline of the abdomen. Location of the fundus above the umbilicus may indicate the presence of blood clots in the uterus that need to be expelled by means of fundal massage. A fundus that is not located in the midline may indicate a full bladder. The fundus descends 1 or 2 cm every 24 hours, so it should be located farther below the umbilicus with every succeeding postpartum day. A nurse assists the primary healthcare provider in performing an amniotomy on a client in labor. In which order should the nurse perform the following actions after the amniotomy? Assign the number 1 to the first action and the number 5 to the last action. Incorrect A. Determining the fetal heart rate B. Taking the client’s temperature, pulse, and blood pressure C. Noting the quantity, color, and odor of the amniotic fluid D. Replacing soiled underpads from beneath the client’s buttocks E. Planning evaluation of the client for signs and symptoms of infection The correct order is: F. Determining the fetal heart rate G. Noting the quantity, color, and odor of the amniotic fluid H. Taking the client’s temperature, pulse, and blood pressure I. Replacing soiled underpads from beneath the client’s buttocks J. Planning evaluation of the client for signs and symptoms of infection Rationale: After amniotomy, the fetal heart rate is assessed for at least 1 full minute for changes associated with prolapse or compression of the umbilical cord and the characteristics of the fluid are noted as an indicator of fetal risk. After the fluid has been assessed, the next concern is evaluation of the maternal vital signs. The client’s comfort (i.e., the soiled underpads) is considered next. With the ruptured membranes comes an increased risk for maternal infection. For this reason, the client is frequently assessed for signs and symptoms of infection throughout the course of labor. A licensed practical nurse (LPN) is monitoring a client in labor for signs of intrauterine infection. Which sign, indicative of infection, would prompt the LPN to contact the registered nurse? A. Maternal fatigue B. Clear amniotic fluid C. Strong-smelling amniotic fluid Correct D. A fetal heart rate of 140 beats/minRationale: Signs associated with intrauterine infection includes fetal tachycardia (rising baseline or faster than 160 beats/min, a maternal fever (38° C or 100.4° F), foul or strong-smelling amniotic fluid, or cloudy or yellow amniotic fluid. The normal fetal heart rate is 110 to 160 beats/min. Clear amniotic fluid is normal. Maternal fatigue normally occurs during labor. A nurse in the labor room is preparing to care for a client with hypertonic uterine dysfunction. The nurse is told that the client is experiencing uncoordinated contractions that are erratic in their frequency, duration, and intensity. What is the priority nursing intervention in the care of this client? E. Providing pain relief Correct F. Preparing the client for amniotomy G. Monitoring the oxytocin (Pitocin) infusion closely Incorrect H. Encouraging the client to ambulate every 30 minutes Rationale: Management of hypertonic uterine dysfunction depends on the cause. Relief of pain is the primary intervention in promoting a normal labor pattern. Therapeutic management of hypotonic uterine dysfunction includes oxytocin augmentation and amniotomy to stimulate labor progression. The client with hypertonic uterine dysfunction would be encouraged to rest, not to ambulate every 30 minutes. A nurse is preparing to care for a client experiencing dystocia. To which of the following interventions does the nurse give priority? I. Monitoring fetal status Correct J. Providing comfort measures K. Changing the client’s position L. Informing the client’s partner of the progress of the labor Rationale: The priority intervention is monitoring fetal status. Once this is done, the nurse provides maternal comfort measures, including positioning the client, because this may decrease anxiety and hasten the progression of labor. Keeping the client’s partner informed of the progress of the labor is also an important aspect of client care during labor but is not an immediate priority. A postpartum client asks a nurse when she may safely resume sexual activity. The nurse tells the client that she may resume sexual activity: M. At any time Incorrect N. In 2 to 4 weeks Correct O. After the 6-week physician checkup P. When her normal menstrual period has resumed Rationale: Usually a woman may engage safely in sexual intercourse during the second to fourth week after childbirth as long as she experiences no discomfort during intercourse. The other options are incorrect. Engaging in intercourse too early in the postpartum course could result in further injuryto perineal tissues damaged during childbirth. It usually takes about 3 weeks for an episiotomy to heal; therefore, it is unnecessary to wait 6 weeks. Menstruation may not resume in a postpartum woman for 12 weeks to 6 months after childbirth. A pregnant woman reports to the clinic complaining of loss of appetite, weight loss, and fatigue, and tuberculosis is suspected. A sputum culture reveals Mycobacterium tuberculosis. The nurse, providing instructions to the mother regarding therapeutic management of the disease, tells the mother that: [Show More]
Last updated: 1 year ago
Preview 1 out of 45 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 12, 2021
Number of pages
45
Written in
Additional information
This document has been written for:
Uploaded
Sep 12, 2021
Downloads
0
Views
48

.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)

.png)

.png)
.png)
.png)