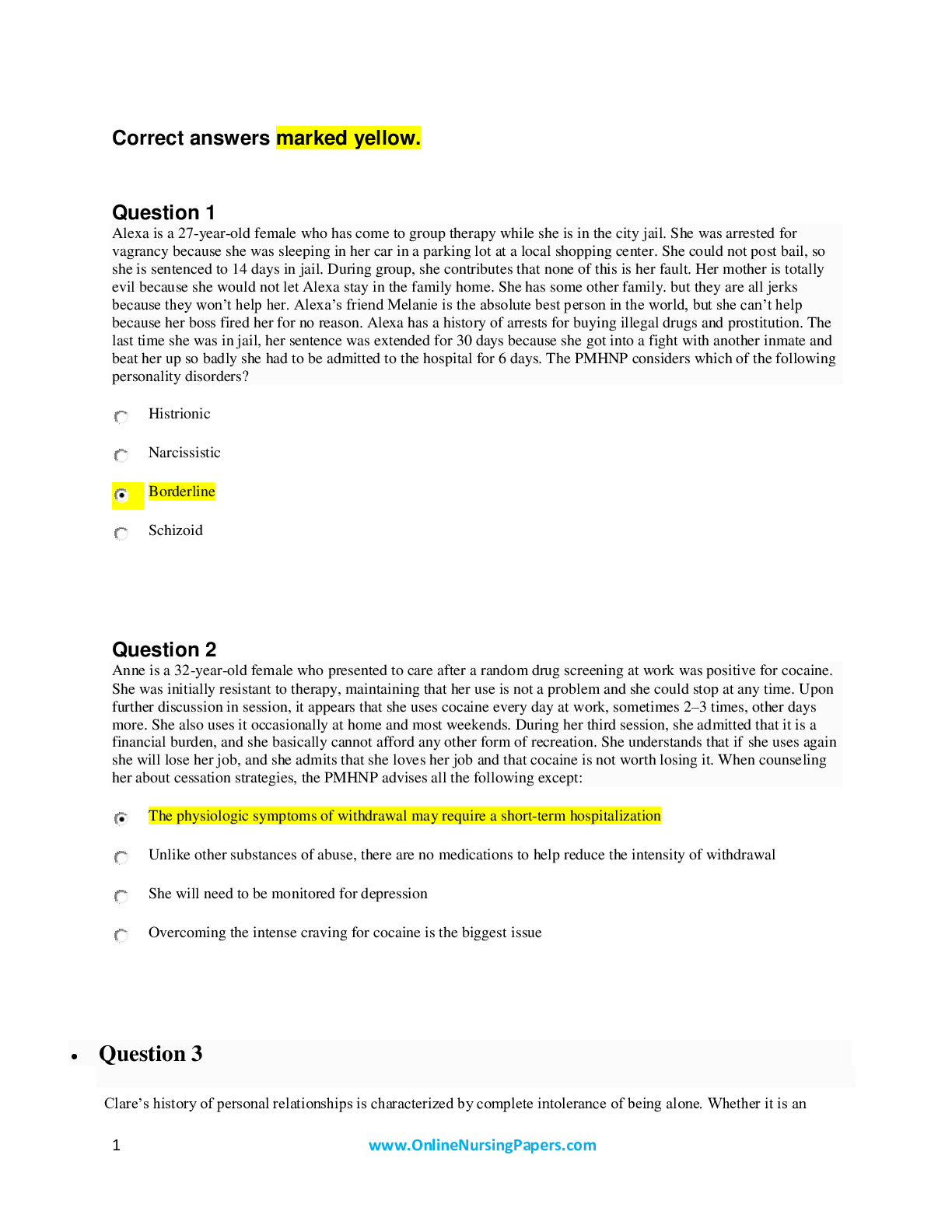
*NURSING > STUDY GUIDE > NUR 180 Final Exam Study Guide Download To prepare for an EXAM (All)
NUR 180 Final Exam Study Guide Download To prepare for an EXAM
Document Content and Description Below
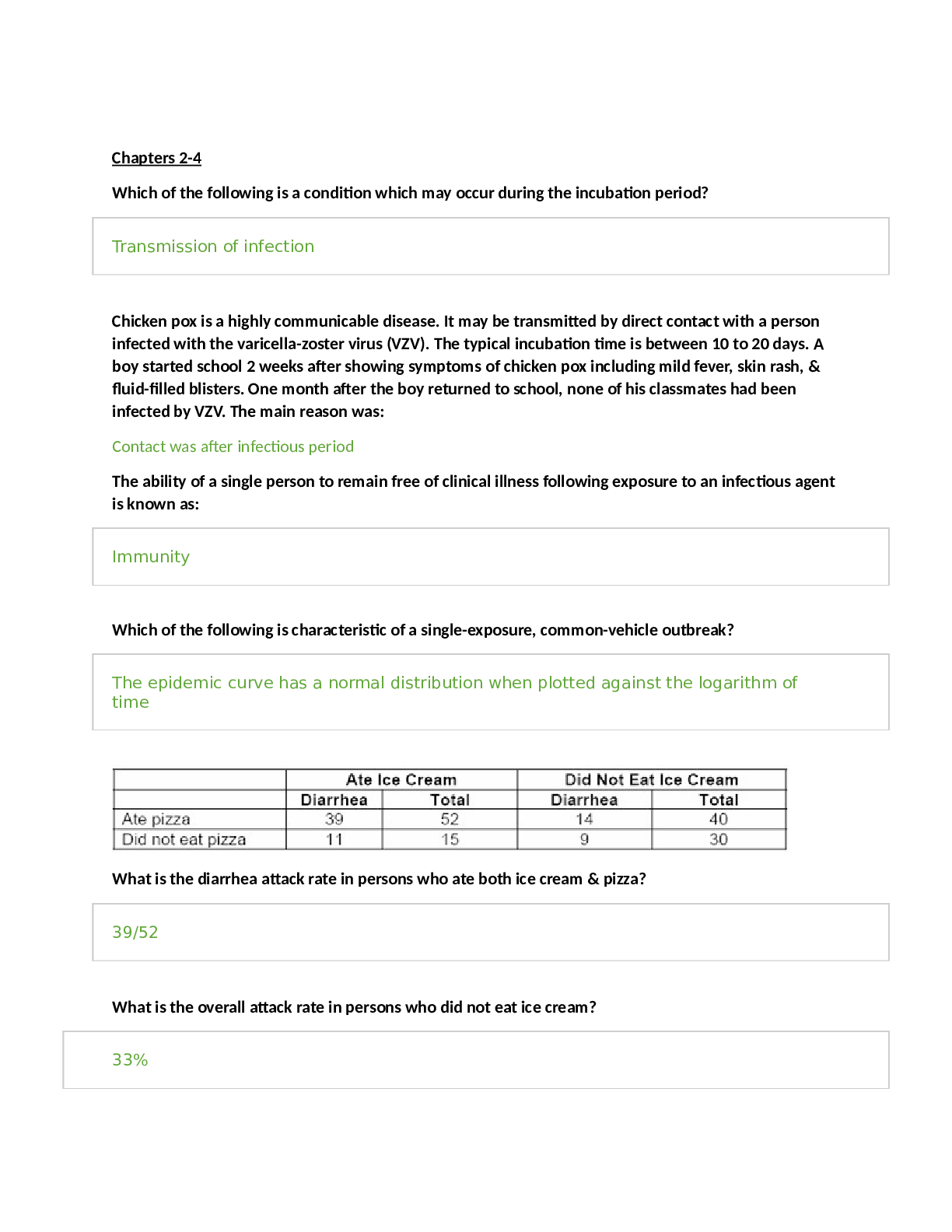
Oxygenation: COPD Oxygenation involves ventilation and perfusion o Ventilation is the process of the gas exchanging o O2 and CO2 exchanging in the lungs o Perfusion is the process of the oxygen an... d nutrients being carried to the tissue and the CO2 and toxins being removed from the tissues We assess: o Respiratory rate o Work of breathing o Pulse ox o Lung sounds o Color of the skin & lips & nailbeds In those with COPD we're going to see: o An increase in respiratory rate o An increase in work of breathing o Intercostal muscles o Nasal flaring o Labored respirations o Drop in the pulse ox o Cyanosis COPD: Patients will have an acid base imbalance – RESPIRATORY ACIDOSIS o Due to the retention of CO2 o Symptoms include irritable, headache, change in mental status, decrease in LOC o Can result in cardiac arrest or respiratory failure if not properly addressed Chronic obstructive pulmonary disease is comprised of 2 disease processes: Chronic bronchitis and emphysema o Chronic bronchitiso Persistent inflammation and edema ■ Continuous inflammation of the bronchioles and a low grade infection of the bronchi ■ This is responsible for most of the airflow obstruction ○ Excessive Bronchial Mucus Production ■ Increase in the size and number of goblet cells; causes a lot of mucous production as well as it impairs the ciliary ■ Ciliary is unable to function properly and cannot properly move the secretions up the bronchial tree ○ Chronic bronchitis is usually precipitated by a prolonged exposure to irritants (usually smoke) or an infection (viral or bacterial) ● Emphysema ○ Enlargement of alveoli secondary to the destruction of alveoli cell wall ■ Protease is released due to inflammation ■ Protease damages the cell wall (elastin) ■ Alveolar cell wall when damaged is unable to have O2 and CO2 gas exchange ■ Sometimes alveoli will “pop” - these alveoli become non-functioning Emphysema is like a cluster of grapes or balloons - Walls get damaged - Lose elasticity - Cannot recoil to fully empty the lungs - They could pop Alpha antitrypsin regulates protease so that there is no damage to the alveoli - Also produced when there is inflammation ***Cigarette smoke would be the number one irritant COPD Stages: o Classification is based on the severity (Stages 1-4) o Determined by forced expiratory volume and symptoms o FVE is the amount of air exhaled in one second Pathology of COPD- ● Both Chronic Bronchitis and Emphysema result in airway obstruction, air trapping, dyspnea, and frequent infections ● With both disease processes the airway is narrowed whether it be from bronchial edema, secretions, or inflammation ● Hypoxemia is low oxygen level in the blood; Hypoxia is low level of oxygen in the tissues ● COPD causes a decreased amount of oxygen in the blood; this results in increased vasoconstriction; vasoconstriction of the pulmonary artery results in the blood unable to leave the right side of the heart; results in right sided heart failure (because it gets backed up) ● Alpha-1-antitrypsin regulated the amount of Protease that an individual has; the inability to control that Protease results in damage to the alveoli wall; alveoli wall loses its elasticity (alveoli are hyperinflated); alveoli do not empty; resulting in air trapping In this photo: Top alveoli is normal in function: o Blood flow and perfusion going around alveoli o So that O2 and CO2 can exchange and carry O2 out to the body. o There is good ventilation and there is no blockage Second is physiologically shunting: o There is blood flow o The airway is narrow o Impairing ventilation o Disrupting gas exchange Third alveoli are dead space: o Blood is coming in, but the blood can’t get to alveoli and complete gas exchange because of the obstruction. o Nothing is taking place. o Ventilation, but no perfusion so no gas exchange is taking place Patient Presentation: Chronic Bronchitis- (cough lasting 3 or more months in two consecutive years) o Chronic cough with mucous production o Dyspnea o Tachycardia o Narrowed airway passages o Wheezing o Air trapping (due to the narrow passageway, secretions and inflammation making it hard for air to get out) Emphysema- (characterized more by respiratory distress, not as many secretions) o Air trapping o alveoli not recoiling to for emptying o Decreased breath sounds o Possible wheezing o Dyspnea o Barrel chest ● Alveoli lose elasticity; alveoli are stretched; alveoli unable to recoil to squeeze out the CO2; alveoli stay hyperinflated; changes the dimensions of the chest cavity o Pursed lip breathing o Patient wants to prolong exhalation o Tripod position (hands on knees) Nursing Interventions: o Encourage stopping smoking o Administer bronchodilators o Provide supplemental O2 (want an oxygen saturation of at least 90%) o But remembering not to give too much to mess with their drive to breath o COPD patients become desensitized to the CO2 levels in their body o Instead, a low O2 level will drive their body to breath o Usually a pulse ox around 90% with activity § Resting at 92 or 93 o Encourage fluid intake to try and thin secretion o This will also help with their insensible loss from the breathing through their mouth, drying out the mouth o Effective coughing techniques to rid some secretions o Postural changes o Raise HOB o Monitor ABG’s o Monitor for high CO2 levels o Pt with COPD are commonly in respiratory acidosis o Mechanical ventilation o Ventilator ○ CPAP (pushes in a breath; patient does not need to use muscles to take a breath; decreases the amount of work that the patient needs to breath; can have a set rate) ■ Patient initiates a breath and the machine pushes the breath in; pressure stops; patient naturally exhales ○ BiPAP (pressure for inspiration, as well as pressure for expiration; pressure increases when the patient initiates a breath; pressure decreases to allow expiration) § This instills a volume of oxygenated air to take the work load off the patient o Nutrition o They are typically malnourished o When they have a hard time breathing, there is less concern with food. They are more focused on liquids due to the loss of insensible fluids when breathing o We want them on low Na diets o High Protein o Decrease carbs o Promote snacking with snacks at the bedside Issues of Concern: o SOB and can’t breathe comfortably o Can make these pt hard to work with § Grumpy and irritable o Just try and be kind and supportive ● Appreciate and understand that these individuals may be in a bad mood; do not take it personally ○ Chronic illnesses are hard to live with What should we do: o Airway o Monitor ABG’s for hypoxemia (low O2) and hypercapnia (high CO2/ respiratory acidosis) o Asses RR, WOB, Cough, sputum, lung sounds o Pt will be in respiratory acidosis o Monitor I&O (especially due to their insensible loss) § But, be frugal so that they are not drinking lots of fluids before a meal, making them feel full, then they do not get to eat, even though their caloric demand is higher from the COPD o Position in semi or high fowlers orthoptic position or a position that promotes optimal breathing o Encourage activity as tolerated § We want them to do what they can and then we help with the rest o Provide tissues and trash can for secretions o Administer steroids, bronchodilators and or expectorants o Provide that supplemental or two o Teach the Huff cough o Monitor vitals o Breathing o Monitor RR and HR o Monitor ABG § Making sure CO2 is coming down and O2 is at an acceptable rate o Provide rest § To prevent fatigue because activity increases oxygen demand o Administer bronchodilators and anti-inflammatory agents that will help their breathing o Activity o Assess patients ability to meet ADLs o Encourage activities o Create an exercise plan § plan activities with them so that you and they're both clear what they're going to do and what they're going to need help with o Nutrition o Monitor weight o Document intake o Might want to consult dietician o Want small frequent meals and snacks at bedside o Foods that are easy to chew o Mouth care before meals o Anxiety o High CO2 causes anxiety o Anxiety can in RR o Stress from not being able to breathe o May have medication to alleviate anxiety (ativan, valium, xanax) o Coping o Be supportive o COPD patients’ emotions may vary o Encourage smoking cessation Oxygenation in relation to other concepts: ● Increased CO2 = Vasodilation ○ Resulting in increased ICP and increased HR (Acid-Base), respiratory Acidosis, headache, irritability, decreased LOC, flushed skin ■ High CO2 does NOT cause vasodilation; decrease in oxygen causes vasodilation; this only occurs in the brain; body has a low oxygen; body vasodilates the brain to try to get blood and oxygen to the brain ■ The rest of the body vasoconstricts; this is directly related to high CO2 because we want to shunt the blood from the body to the core organ so that gas exchange can happen and the oxygen that we do have can go to the brain ○ Increased CO2 can cause respiratory acidosis related to the acid-base ○ Nursing intervention: Need to know how the patient slept the night before (are they lethargic because they are tired or have an increase in CO2) ● Decreased O2 = Increased systemic workload and shunts blood from periphery to vital organs (cellular regulation) ○ Resulting in fatigue, palor, jaundice, tachycardia ○ Patient’s without enough oxygen lead to the heart working harder, body will have to vaso constrict, shunt the blood to get whatever oxygen you do have to the brain ● Decreased O2 = Changes in cognition and LOC (cognition) ● Decreased O2 = Decreased O2 to tissues ○ Resulting in pain (comfort), increased HR, increased RR, increased BP, restlessness, anxiety, diaphoresis, PT report ■ Peripheral arterial disease or Frostbite - when enough arterial blood cannot get to the toes it is painful for the patient ● Decreased O2 = decreased O2 to organs (perfusion) ○ Peripheral pulses diminished, nail beds >3 seconds CRT, color (not pink), body positions for comfort, orientation Patient Experiencing Difficulty Exhaling ● Increased volume of trapped air results in hyperinflation of the alveoli ● Lungs remain in a hyper-expanded state ● Expiration becomes a muscular act ○ Patients must “bear down” to try to exhale ○ Patient tries to constrict the diaphragm to compress the lungs to get an effective exhale Increased AP Diameter ● Barrel chest; patient in state of hyperinflation; typical of COPD patients ● Alveoli have lost their elasticity; unable to recoil, rebound, and squeeze CO2 out Diagnostics: o PFTS (pulmonary function tests) o Tests breathing in, taking a deep breath in, taking a breath out, and taking a deep breath out o Used to evaluate and diagnose the progression of the disease o Ventilation perfusion scans § Looks to see if the lung tissue is being ventilated or the gases are exchanging and perfusion to see if there's blood flow ○ Patient will inhale a radioactive isotope allowing everything to “light up”; the areas that light up are indication of what has been breathed in entering into the blood; as the blood perfuses the lungs it will “light up”; areas in the scan that do not “light up” indicate that the blood is not arriving there (that area is not getting oxygen) · Used also in diagnosing a PE (pulmonary emboli). If there is a clot in the lung, the the area that's not getting the blood flow is going to to darken so the ventilation perfusion scan is really done to rule out any type of perfusion issue o Serum anti trypsin level o if you have that an Alpha antitrypsin deficiency then your protease enzyme can't be regulated or controlled § That causes damage to the alveolae and causes emphysema so that's a way to tell if this emphysema is caused by that Alpha antitrypsin deficiency resulting in that proteasome sign not being able to be regulated or controlled and that results in damage of the alveoli cell wall o ABGs o monitor that acid base balance § CO2 levels coming down § O2 level is staying acceptable o Pulse ox o Make sure that that oxygen level that's being carried in the blood is acceptable we want it to be at least 90 o realize that if we want it to be at least 90 with activity, then that means that rest it could be a little bit higher o you might see a pulse ox 93, 94, 95 but again when it comes to the oxygen, we want to be careful we don't want to provide too much oxygen § We don't want to suppress their drive to breathe o Chest X Rays o Typically, a chest x-ray is ordered to determine if there's pneumonia or not o a lot of times what brings patients with COPD into the hospital is the fact that they've acquired pneumonia and that's put them over the edge & they've gone into respiratory distress [Show More]
Last updated: 1 year ago
Preview 1 out of 168 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 18, 2021
Number of pages
168
Written in
Additional information
This document has been written for:
Uploaded
May 18, 2021
Downloads
0
Views
27




 Rasmussen College.png)