Surgery > STUDY GUIDE > PAEA Surgery Study Guide | PAEA Surgery Blueprint Gastrointestinal/Nutritional ; ABDOMINAL PAIN. (All)
PAEA Surgery Study Guide | PAEA Surgery Blueprint Gastrointestinal/Nutritional ; ABDOMINAL PAIN.
Document Content and Description Below
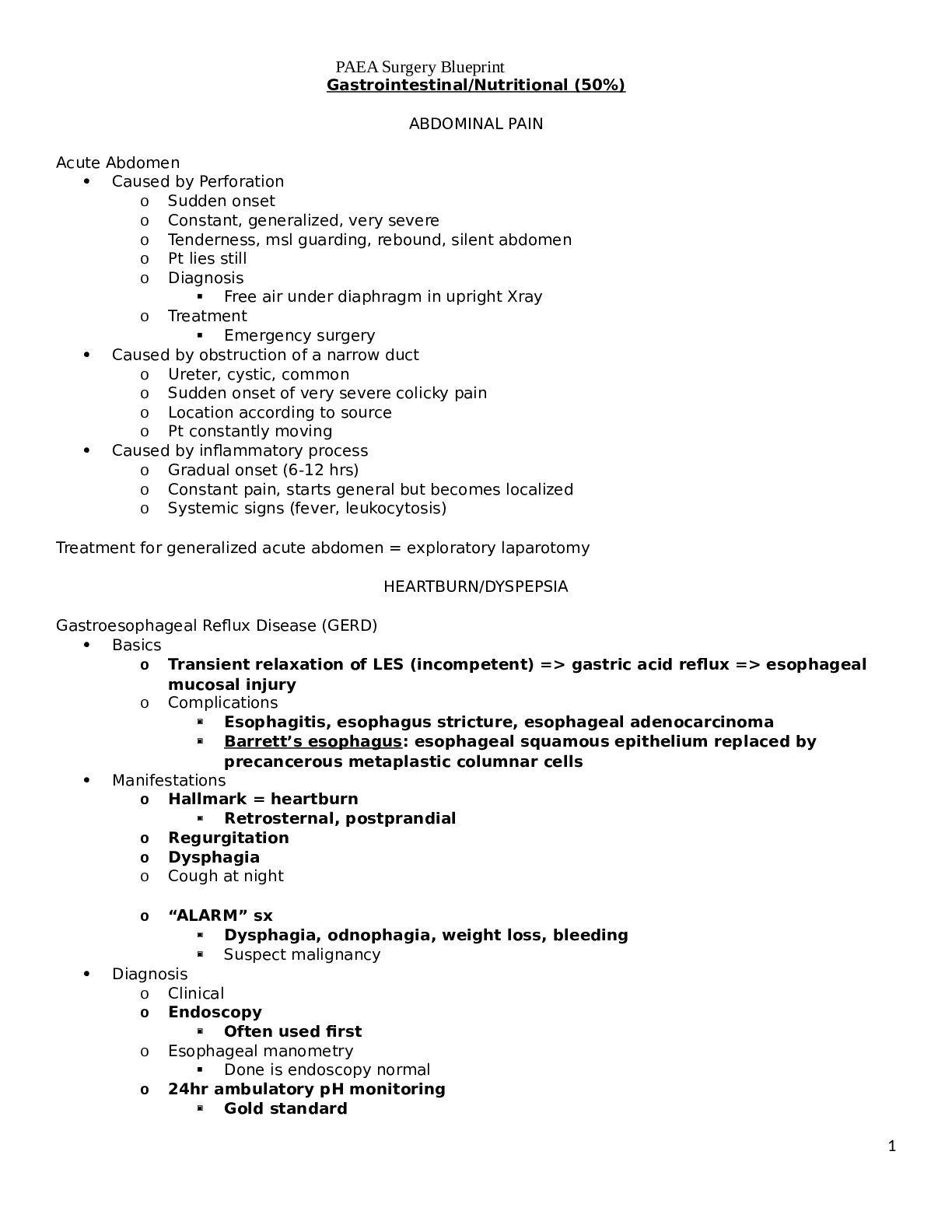
PAEA Surgery Blueprint Gastrointestinal/Nutritional (50%) ABDOMINAL PAIN Acute Abdomen Caused by Perforation o Sudden onset o Constant, generalized, very severe o Tenderness, msl guarding, ... rebound, silent abdomen o Pt lies still o Diagnosis Free air under diaphragm in upright Xray o Treatment Emergency surgery Caused by obstruction of a narrow duct o Ureter, cystic, common o Sudden onset of very severe colicky pain o Location according to source o Pt constantly moving Caused by inflammatory process o Gradual onset (6-12 hrs) o Constant pain, starts general but becomes localized o Systemic signs (fever, leukocytosis) Treatment for generalized acute abdomen = exploratory laparotomy HEARTBURN/DYSPEPSIA Gastroesophageal Reflux Disease (GERD) Basics o Transient relaxation of LES (incompetent) => gastric acid reflux => esophageal mucosal injury o Complications Esophagitis, esophagus stricture, esophageal adenocarcinoma Barrett’s esophagus: esophageal squamous epithelium replaced by precancerous metaplastic columnar cells Manifestations o Hallmark = heartburn Retrosternal, postprandial o Regurgitation o Dysphagia o Cough at night o “ALARM” sx Dysphagia, odnophagia, weight loss, bleeding Suspect malignancy Diagnosis o Clinical o Endoscopy Often used first o Esophageal manometry Done is endoscopy normal o 24hr ambulatory pH monitoring Gold standard 1 PAEA Surgery Blueprint Not done often Management o Stage 1: Lifestyle Modifications Elevation of the head of the bed Avoid recumbence for three hours after eating Eat small meals Avoid certain foods (fatty, spicy, citrus, chocolate, caffeine) Decrease fat & ETOH intake Weight loss Smoking cessation o Stage 2: As Needed” Pharmacological Therapy Antacids OTC H2 receptor antagonists (“-tidine”) ***If “ALARM” sx, do endoscopy o Stage 3: Scheduled Pharmacologic Therapy Meds H2RA Proton Pump Inhibitors (“-azole”) o Drug of choice in severe disease Cisapride Nissen Fundoplication If refractory Achalasia Basics o Loss of Aurbach’s plexus => increased LES pressure Failure of LES relaxation Manifestations o Dysphagia to BOTH solids & liquids o Weight loss o Regurgitation of undigested food o Chest pain o Cough Diagnosis o Esophageal manometry (gold standard) Increased LES pressure (> 40 mmHg) o Double-contrast esophagram Bird’s beak appearance Management o Decrease LES pressure Botox injection (temporary relief) Nitrates CCBs Dilation of LES Esophagomyomectomy JAUNDICE Basics Yellowing of skin, nail beds, sclera o Due to tissue bilirubin distribution *Not a disease but a sign of disease Occurs when bilirubin > 2.5 mg/dL 2 PAEA Surgery Blueprint Types Hemolytic o Low level (6-8) o Elevated bilirubin is unconjugated (indirect) o Work up should determine what is causing issue with RBCs Hepatocellular o Elevated bilirubin (conjugated & unconjugated), transaminases, alk phos (modest) o Hepatitis (direct workup this way) Obstructive o Elevated bilirubin (conjugated & unconjugated), transaminases, alk phos (v. high) o Workup => U/S Look for obstruction HEMATEMESIS Denotes upper GI source Diagnosis: UGI endoscopy Corrosive Esophagitis Basics o Etiology: ingestion of corrosive substance Manifestations o Odynophagia, dysphagia, hematemesis, dyspnea Diagnosis o Endoscopy Management o Supportive o Pain meds o IV fluids Boerhaave’s Syndrome Basics o Full thickness rupture of distal esophagus o Associated with repeated vomiting (bulimia), iatrogenic perforation Manifestations o Retrosternal chest pain worse with deep breathing and swallowing o Hematemesis o PE: crepitus on chest auscultation due to pneumomediastinum Diagnosis o Chest CT Management o Surgical repair Mallory-Weiss Syndrome (Tears) Basics o UGI bleeding due to longitudinal mucosal lacerations @ gastroesophageal junction or gastric cardia (superficial) o Sudden rise in intragastric pressure or gastric prolapse into esophagus Persistent retching/vomiting Alcohol binge Bulimia 3 PAEA Surgery Blueprint Manifestations o Retching/vomiting => hematemesis after an alcohol binge o Melena, hematochezia, syncope, ab pain, hydrophobia Diagnosis o Upper endoscopy Management o Supportive if no active bleeding o Active bleeding => epi injection, sclerosing agent, band ligation, hemo-clipping or balloon tamponade [Show More]
Last updated: 1 year ago
Preview 1 out of 67 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 24, 2022
Number of pages
67
Written in
Additional information
This document has been written for:
Uploaded
May 24, 2022
Downloads
0
Views
28