*NURSING > QUESTIONS & ANSWERS > Chamberlain College of Nursing - ADVANCED P NR509WEEK 7 SOAP. Notes and Exam. All Done and Graded A (All)
Chamberlain College of Nursing - ADVANCED P NR509WEEK 7 SOAP. Notes and Exam. All Done and Graded A
Document Content and Description Below
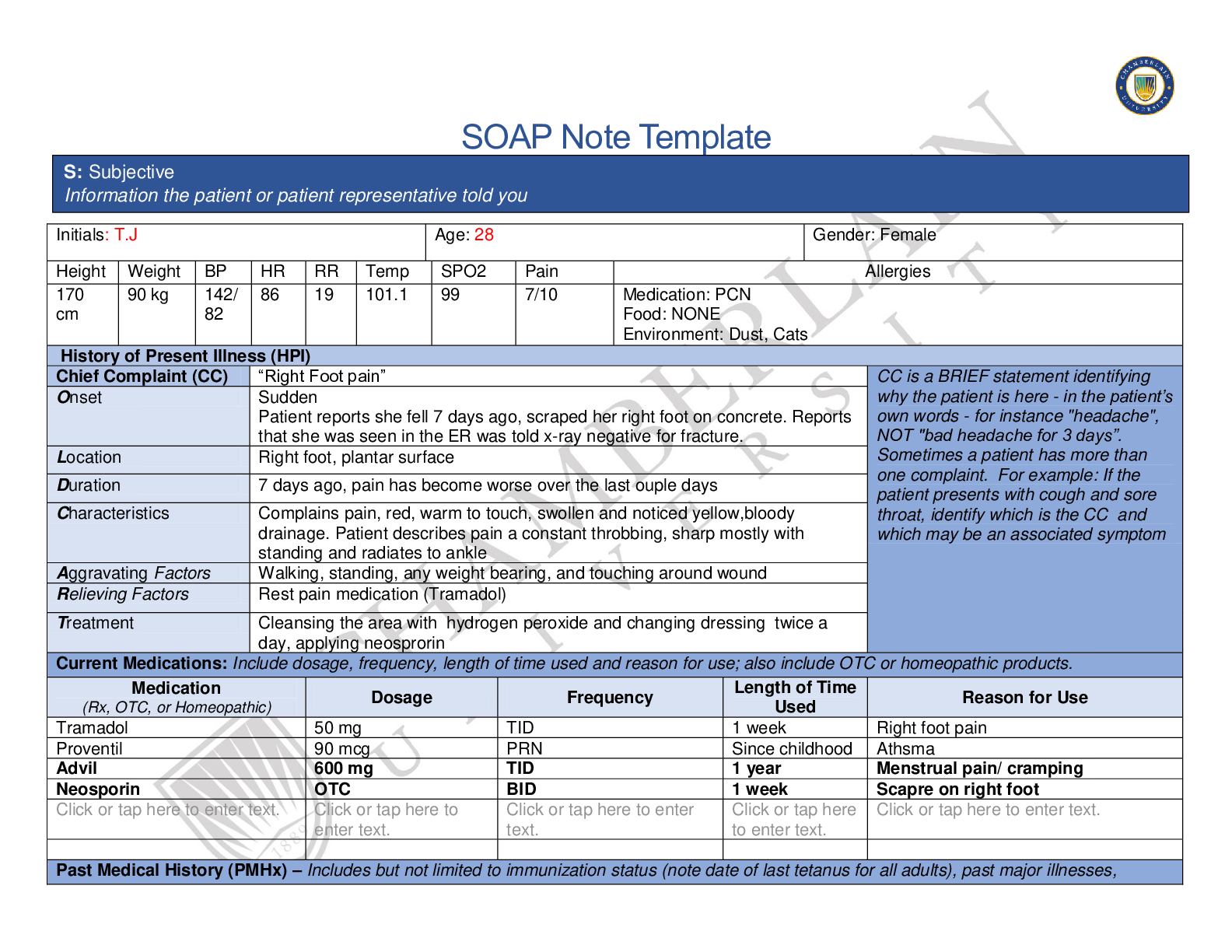
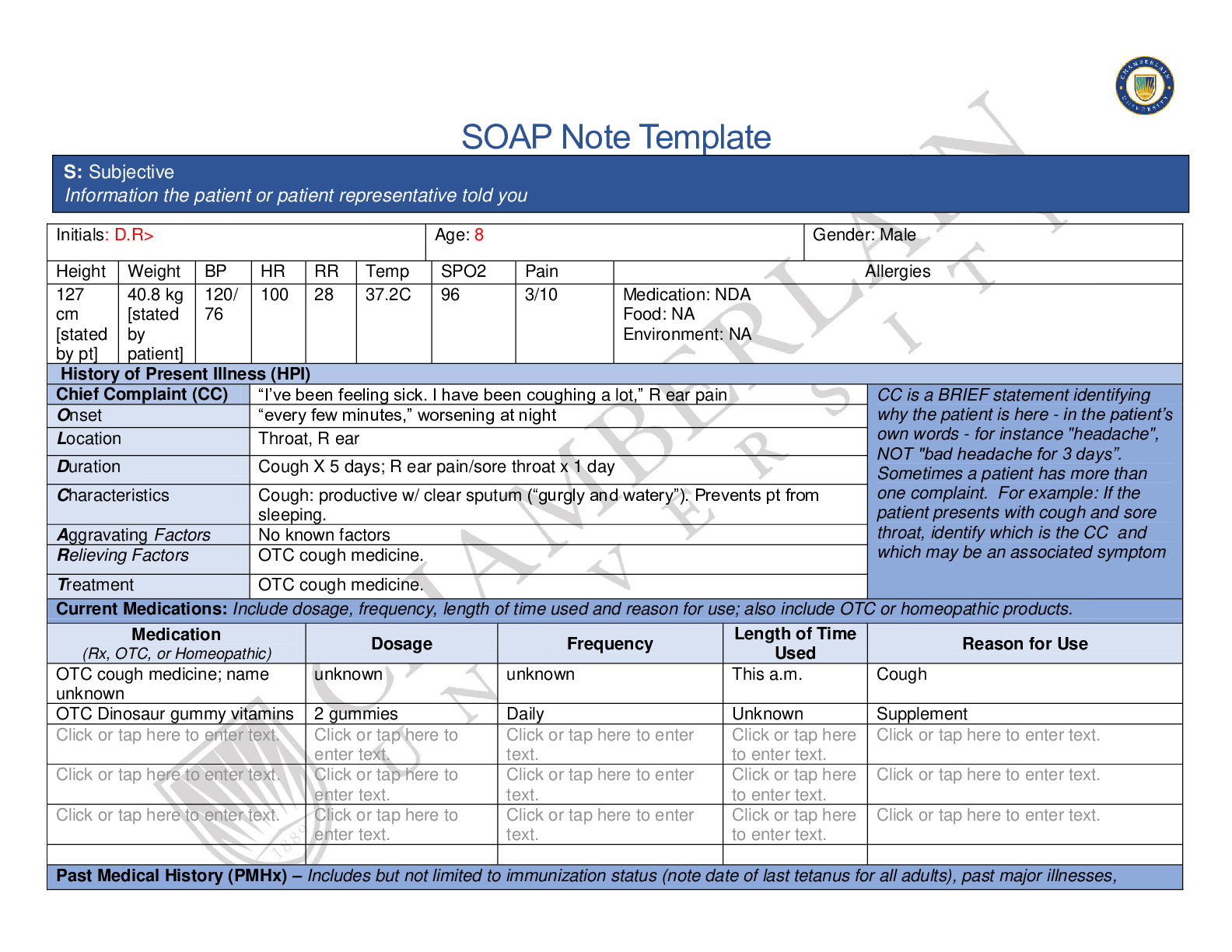
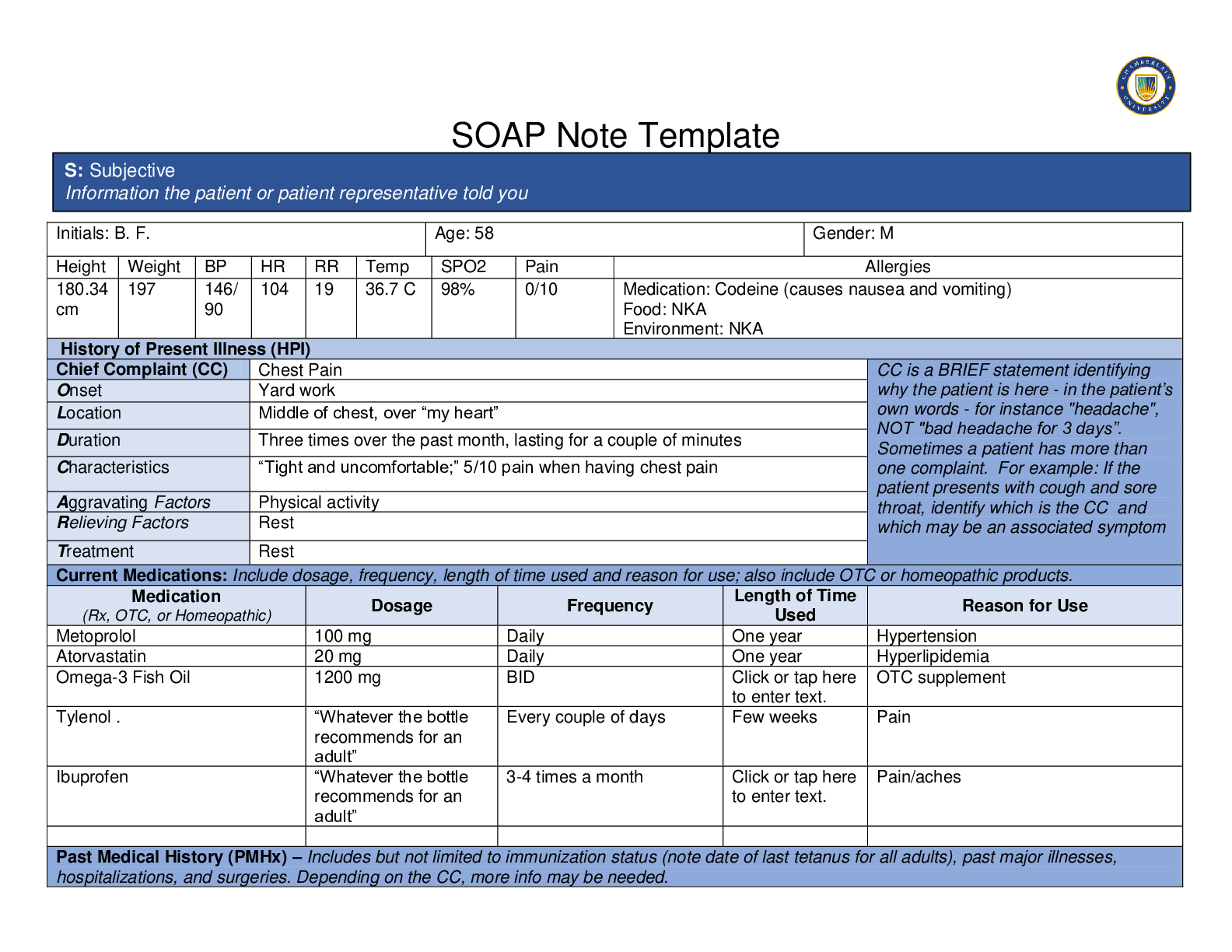
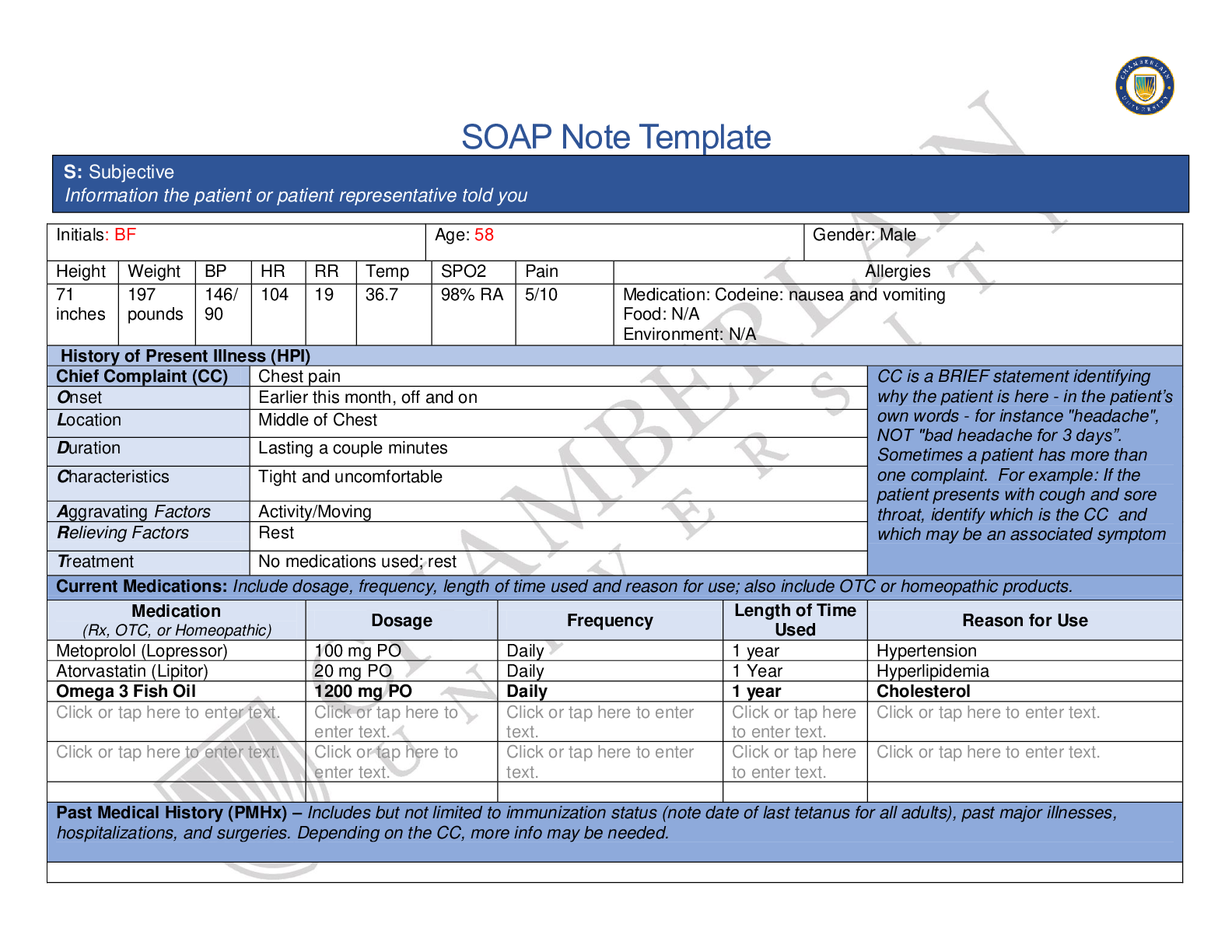
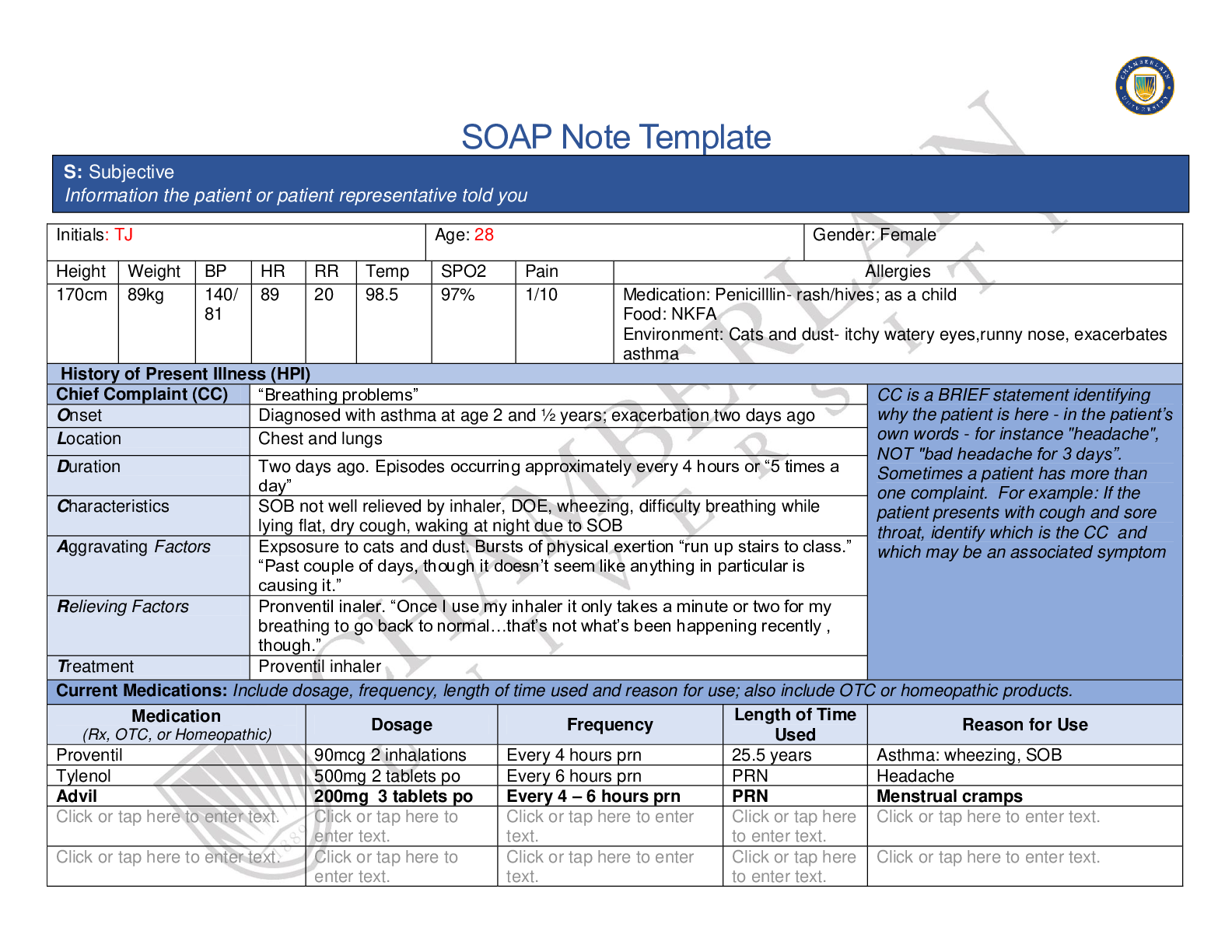
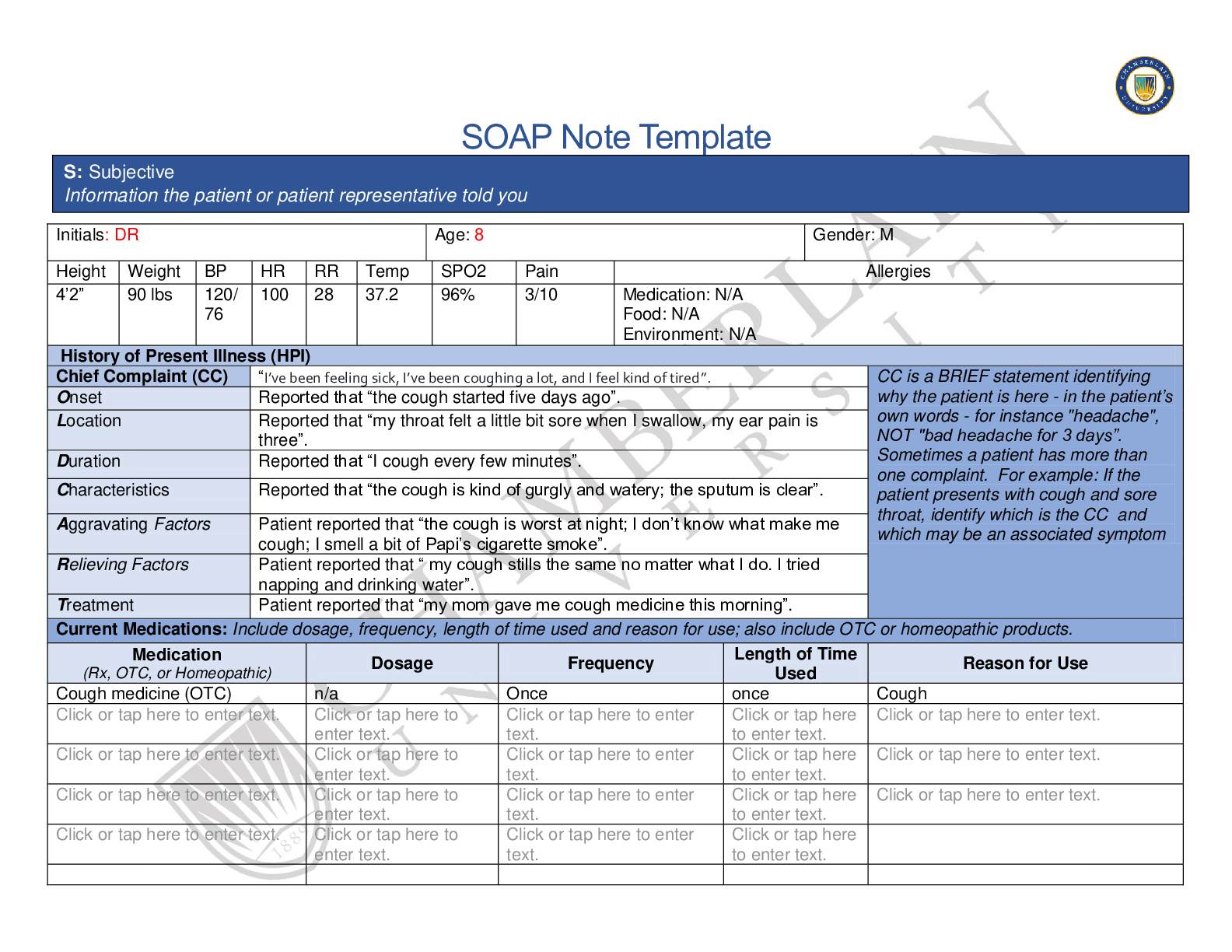
SOAP Note Template Initials: DR Age: 8 Gender: M Height Weight BP HR RR Temp SPO2 Pain Allergies 4’2” 90 lbs 120/ 76 100 28 37.2 96% 3/10 Medication: N/A Food: N/A Environment: N/A History... of Present Illness (HPI) Chief Complaint (CC) “I’ve been feeling sick, I’ve been coughing a lot, and I feel kind of tired”. CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Reported that “the cough started five days ago”. Location Reported that “my throat felt a little bit sore when I swallow, my ear pain is three”. Duration Reported that “I cough every few minutes”. Characteristics Reported that “the cough is kind of gurgly and watery; the sputum is clear”. Aggravating Factors Patient reported that “the cough is worst at night; I don’t know what make me cough; I smell a bit of Papi’s cigarette smoke”. Relieving Factors Patient reported that “ my cough stills the same no matter what I do. I tried napping and drinking water”. Treatment Patient reported that “my mom gave me cough medicine this morning”. Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Cough medicine (OTC) n/a Once once Cough Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. S: Subjective Information the patient or patient representative told youPast Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Mr. Rivera is an 8-yr. old male who came because of feeling sick, being tired, and coughing a lot. His grandmother is with him at bedside. Mr. Rivera denies previous hospitalizations and surgery. Mr. Rivera was only treated for pneumonia last year. He denies having any asthma. His immunization record shows that he did not have an influenza vaccine for the last 12 months. His hepatitis A, hepatitis B, pneumococcal, DTap, MMR, Varicella, and Polio vaccines are complete. Mr. Rivera was given cough medicine by his mother before he came to the clinic. He said that the cough medicine was purple and was given a spoonful. Mr. Rivera reported that the cough medicine just given him a temporary relief. Mr. Rivera denies any seasonal allergies, food allergies, medication allergies, allergies to animals, and latex allergy. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Mr. Rivera lives with his parents. His grandma take care of him while his parents are at work. He is in grade 3. His record shows that he was absent for two weeks last year because of pneumonia. English is a primary spoken language and some Spanish. He said that his father smokes cigarettes and sometimes forget to take his cigarettes outside. He reported that sometimes he could smell his father’s cigarette smoke. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Mr. Rivera’s mother has type 2 DM, HTN, hypercholesteremia, spinal stenosis and obesity. His father has asthma when he was a child, a smoker, hypertension, and hypercholesteremia. His maternal grandmother has type 2 DM, and HTN. His maternal grandfather is also a smoker and has eczema. His paternal grandmother died of a car accident when the grandmother was 52. His paternal grandfather has no known history. He denies any allergies affecting the family. He also reported that they do not have any pet at home. Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☒Fatigue feel tires and need to rest more often ☒Weakness Click or tap here to enter text. ☒Fever/Chills T=100.2 ☐Weight Gain none ☐Itching none ☐Rashes none ☐Nail Changes none ☐Skin Color Changes NONE ☐Other: ☐Diplopia none ☐Eye Pain none ☐Eye redness none ☐Vision changes NONE ☐Photophobia none ☐Eye discharge none ☒Earache 3/10 ☐Tinnitus none ☐Epistaxis none ☐Vertigo none ☐Hearing Changes none ☐Hoarseness none ☐Oral Ulcers none ☒Sore Throat 3/10 ☐Congestion none ☐Rhinorrhea NONE ☐Other:☐Weight Loss none ☐Trouble Sleeping none ☐Night Sweats none ☐Other: n/a Click or tap here to enter text. Click or tap here to enter text. Respiratory Neuro Cardiovascular ☒Cough Click or tap here to enter text. ☐Hemoptysis none ☐Dyspnea none ☐Wheezing none ☐Pain on Inspiration none ☒Sputum Production White Small Thin ☐Other: n/a ☐Syncope or Lightheadedness none ☐Headache NONE ☐Numbness none ☐Tingling none ☐Sensation Changes . ☐Speech Deficits none ☐Other: Click or tap here to enter text. ☐Chest pain none ☐SOB none ☐Exercise Intolerance none ☐Orthopnea none ☐Edema none ☐Murmurs none ☐Palpitations none ☐Faintness none ☐OC Changes none ☐Claudications none ☐PND none ☐Other: n/a MSK GI GU PSYCH ☒Pain 3/10 throat and ear ☐Stiffness none ☐Crepitus none ☐Swelling none ☐Limited ROM . ☐Redness none ☐Misalignment none ☐Other: n/a ☐Nausea/Vomiting none ☐Dysphasia none ☐Diarrhea once ☐Appetite Change Click or tap here to enter text. ☐Heartburn none ☐Blood in Stool none ☐Abdominal Pain none ☐Excessive Flatus Click or tap here to enter text. ☐Food Intolerance none ☐Rectal Bleeding none ☐Other: none ☐Urgency none ☐Dysuria none ☐Burning none ☐Hematuria none ☐Polyuria none ☐Nocturia none ☐Incontinence none ☐Other: none ☐Stress none ☐Anxiety none ☐Depression none ☐Suicidal/Homicidal Ideation none ☐Memory Deficits none ☐Mood Changes none ☐Trouble Concentrating none ☐Other: noneGYN ☐Rash none ☐Discharge normal ☐Itching none ☐Irregular Menses NONE ☐Dysmenorrhea NONE ☐Foul Odor none ☐Amenorrhea none ☐LMP: last month ☐Contraception none ☐Other: Body System Positive Findings Negative Findings General . Patient looks tired, weak, and feverish. Patient is alert and oriented. The patient is calm and cooperative. Ms. Rivera gave personal information without hesitation. He is dress according to the weather. Skin . Unable to Assess Skin color is usual for ethnicity, dry, elastic, intact, without any lesions, and without tenting. HEENT . The right external auditory canal and tympanic membrane is erythemic. Nasal cavities has clear discharge. Tonsils is +2 erythemic; posterior pharynx is cobblestoning and erythemic Lymph node is palpable in right anterior cervical. Head is symmetric and midline; face do not have any lesions nor edema. Eye conjunctiva is pink, moist, and no discharge; sclera is clear, white, and no visible deformities. Ear is symmetric and without any lesions; Right auditory canal has no fluid no discharge.Tympanic membrane has no visible abnormal findings, the cone of light is at 5:00; Left external auditory canal is pink, no discharge, and no abnormal findings; tympanic membrane is pearly gray and the cone of light is at 7:00. Nose is midline, no lesions, no fracture and nasal mucosa is pink and moist, turbinates are pink and intact, septum is O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings.midline, pink and moist. Lips is pink and moist; teeth are intact and no decay; tongue is midline, pink and moist without any lesions; buccal mucosa is pink and moist without any lesions; hard palate and soft palate is moist and intact; uvula is midline, pink and intact. Fronal sinuses and maxillary simuses has no tenderness. Supraclavicular and Axillary lymph node are non-palpable. Respiratory . Unable to Assess Chest is symmetric and no abnormal deformities. Lung sounds is present in all lobes and are clear. No adventitious sounds heard. Fremitus is equal bilaterally. Bronchophony is equal bilaterally. All areas are resonant upon percussion. FEV1 =3.15L FVC= 3.91L (FEV1/FVC:80.5) Neuro . Unable to Assess Patient is alert and oriented. His speech is clear and vocabulary is appropriate. Cardiovascular . Unable to Assess S1, S2 heart sounds are heard in aortic, pulmonic, erb’s point, tricuspid, and mitral valve Musculoskeletal . Unable to Assess Upper extremities and lower extremities does not have any redness lesions, nor edema Gastrointestinal . Abdomen is flat and symmetric. No redness, bulging nor lesions are observed.All quadrants has normoactive sounds. Right renal, left renal, right iliac, left iliac, right femoral, and left femoral artery have no bruits. No flatness, or dullness heard upon percussion. The liver is nonpalpable. Spleen is non- palpable. No tenderness nor masses was palpated.Problem List 1. Cough 6 11 Click or tap here to enter text. 2 feeling tired 7 12 Click or tap here to enter text. 3 earache 8 13 Click or tap here to enter text. 4 sore throat 9 14 Click or tap here to enter text. 5 fever 10 15 Genitourinary . Unable to Assess Genitourinary tract has no redness, masses, nor lesions; bladder is non-palpable; kidneys are non-palpable; No tenderness below the posterior CVA. Urine is amber, clear, acidic, and negative for other substances. Psychiatric . Unable to Assess Patient is calm and cooperative. Gynecological . Unable to Assess No tenderness, lesions, irritations, discharge, bleeding, masses or growth noted in the genital or pelvic area. Diagnosis ICD-10 Code Pertinent Findings Streptococcal pharyngitis J02.0 Patient has erythemic posterior pharynx with cobblestoning. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.Diagnostics: List tests you will order this visit Test Rationale/Citation Rapid Strep test The most commonly used diagnostic test to see if the sore throat is cause by group A streptococcal bacteria (Stead, 2019). Although we have been taught in class that there is a guideline we could follow to eliminate rapid strep test, I will just post this test for the sake of discussion. Throat culture The throat culture is more accurate than the rapid strep test. The throat culture swab is collected Viral Pharyngitis J02.9 Patient has erythemic posterior pharynx with cobblestoning. Otalgia H92.09 Patient is suffering from ear pain 3/10. P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention.together with the rapid strep test swab (Stead, 2019). Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation For individuals without Penicillin allergy Penicillin V Or Amoxicillin Or Benzathine Penicillin G, intramuscular 250 mg daily PO 2-3 times per day 50 mg/kg PO q24hrs, or, 25 mg/kg PO q12hrs <27 kg= 0.6 M units IM; >27 kg = 1.2M units IM 10 days 10 days once Penicillin is an antibiotic of choice to treat strep throat. Penicillin could be given in a pill form or a liquid form 2-4 times per day in 10days. People who are allergic to penicillin could be given another form of antibiotics (UpToDate, 2019; CDC, 2019) Antibiotics for individuals with penicillin allergy Cephalexin 20 mg/kg/dose PO q12 hours; max of 500 mg/dose 10 days Cephalexin is a cephalosporin antibiotic that is used to treat bacterial infections. Caution if patient is hypersensitive toCefadroxil 30 mg/kg PO once a day 10 days penicillin. Caution is patient is having GI disorders and renal impairment (Epocrates, 2019). Cefadroxil is also a cephalosporin. It fights bacteria in your body (Epocrates, 2019). Clindamycin 7 mg/kg/dose PO 3 times daily (max = 300 mg/dose) 10 days Clindamycin is use to kill bacteria in your body. Clindamycin should be drink with a full galss of water to prevent throat irritation (Epocrates, 2019). Azithromycin 12 mg/kg once PO (max = 500 mg), then 6 mg/kg PO (max=250 mg) once daily 5 days Azithromycin is used to treat infections in the throat. You should not use azithromycin in patients who have liver problems. (Epocrates, 2019) Acetaminophen 10 ml PO q4H PRN for fever Adjunctive medication should be used to treat mild to sever fever. Acetaminophen could also be used for pain (American Family Physician, 2013). Referral/Consults: Primary care Doctor Rationale/Citation If symptoms persist, the patient need to go back and see his primary care doctor, especially if drooling is involved, difficulty swallowing and breathing, Temperature of more than 101 F, swelling of the neck, inability or unwillingness to drink, difficulty opening the mouth, muffled voice and stiff neck (UpToDate, 2019). Education: Medication/Treatment regimen Rationale/Citation The clinician should educate the patient about the medication regimen. Patient should take theHandwashing Monitor for dehydration Alternative therapy such as oral rinses The time to return school/work drug exactly as prescribed and not skip or double doses (Woo & Robertson, 2016). Patient should also be educated on the adverse reaction of drugs and appropriate responses to it (Woo & Robertson, 2016). The best prevention for the spread of Step throat is handwashing. Patient should be educated about handwashing. Alcohol rub is another best alternative. Handwashing should be done after counging, sneezing or blowing one’s nose (UpToDate, 2019). Some kids are reluctant to drink some fluids because of a sore throat. Ask parents to monitor for dehydration. Parents could also offer warm or cold liquid (UpToDate, 2019). Patient should be educated that oral rinses such as salt-water gargles could help getting rid of sore throat (UpToDate, 2019). Patient with strep throat could return to work or school 24 hours after antibiotic therapy (UpToDate, 2019). Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. One week Rationale/Citation It is essential to determine if thereare any complications brought by strep throat, such as streptococcal abscess, rheumatic fever and cervical lymph adenitis (UptoDate, 2019). References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. American Family Physician (AFP). (2013). IDSA updates guideline for managing Group A Streptococcal pharyngitis. 88(5), 338-340. Center for Disease Control. (2018). Pharyngitis (Strep Throat). Retrieved August 23, 2019, from https://www.cdc.gov/groupastrep/diseaseshcp/strep-throat.html UpToDate. 2019. Patient education : Sore throat in children (beyond the basics). Uptodate. Retrieved August 23, 2019, from https://www.uptodate.com/contents/sore-throat-in-children-beyond-the-basics?topicRef=4013&source=see_link Woo, T. M., Robinson, M. V. (2016). Pharmacotherapeutics for Advanced Practice Nurse Prescribers (4th ed.). Philadelphia, PA: F. A. Davis Company. Retrieved from https://ambassadored.vitalsource.com/#/books/9780803658110/ [Show More]
Last updated: 1 year ago
Preview 1 out of 11 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
11
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
61



.png)