*NURSING > CASE STUDY > NR 601 Week 2: COPD Case Study Part 1 - Download to View Proper Discussion Format And Attain That Hi (All)
NR 601 Week 2: COPD Case Study Part 1 - Download to View Proper Discussion Format And Attain That High Score.
Document Content and Description Below
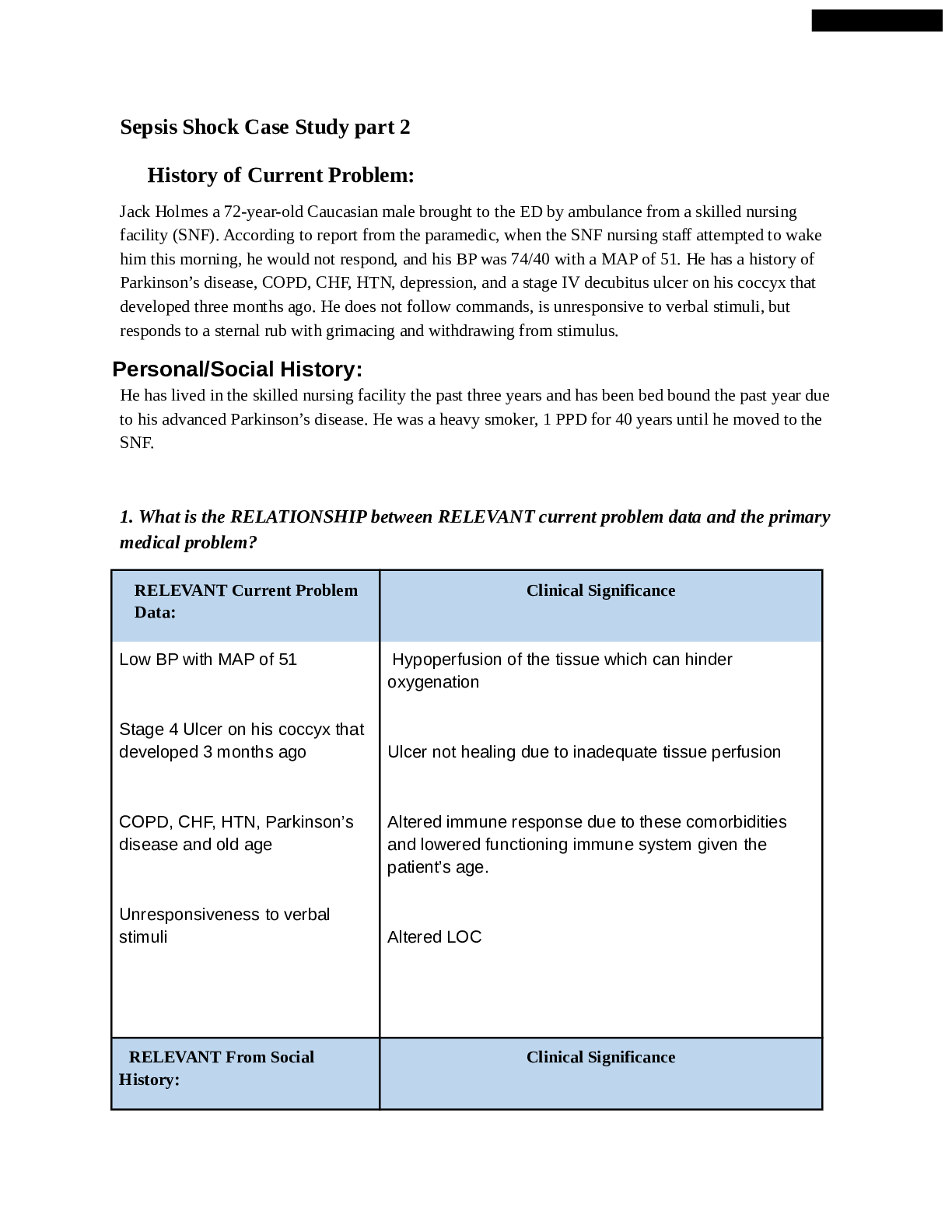
Purpose Problem-based learning is a methodology designed to help students develop the reasoning process used in clinical practice through problem solving actual patient problems in the same manner as... they occur in practice. The purpose of this activity is to develop students’ clinical reasoning skills using a case-based learning exercise. Through participation in an online discussion forum, students identify learning issues in a self-directed manner which facilitates learning for the entire group. Activity Learning Outcomes Through this discussion, the student will demonstrate the ability to: 1. Demonstratecompetenceintheevaluationandmanagementofcommonrespiratory problems(WO2.1)(CO,2,3,4,5) 2. Distinguish between obstructive and restrictive lung disease (CO 2, 4) Develop a management plan for the case study patient based on identified primary, secondary and differential diagnoses. (WO 2.2) (CO 2,4) 3. Interpret pulmonary function test results. (WO 2.3) (CO 2, 4) Due Date: Student enters initial post to part one by 11:59 p.m. MT on Tuesday; responds substantively to at least one topic-related post of a peer including evidence from appropriate sources AND all direct faculty questions in parts one by Sunday, 11:59 p.m. MT. A 10% late penalty will be imposed for discussions posted after the deadline on Tuesday 11:59pm MT, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Sunday (i.e. student will receive an automatic 0). Total Points Possible: 50 Case Study - Part 1 Date of visit: November 20,2019 A 62 year-old Caucasian male presents to the office with persistent cough and recent onset of shortness of breath. Upon further questioning you discover the following subjective information regarding the chief complaint. Physical exam reveals the following: Requirements/Questions: 1. Briefly and concisely summarize the history and physical (H&P) findings as if you were presenting it to your preceptor using the pertinent facts from the case. May use approved medical abbreviations. Avoid redundancy and irrelevant information. 2. Provide a differential diagnosis (minimum of 3) which might explain the patient's chief complaint along with a brief statement (2-3 sentences) of pathophysiology for each. 3. Analyze the differential by using the pertinent findings from the history and physical to argue for or against a diagnosis. 4. Rank the differential in order of most likely to least likely. 5. Identify any additional tests and/or procedures that you feel is necessary or needed to help you narrow your differential. All testing decisions must be supported with an evidence-based practice (EBP) argument as to why it is necessary or pertinent in this case. If no testing is indicated or needed, you must also support this decision with EBP evidence. DISCUSSION CONTENT Category Points % Description Application of 15 30% 1. A brief AND concise summary of the history and physical (H&P) findings is presented without redundancy or irrelevant information; AND Three (3) appropriate diagnoses in the differential are presented which can explain the patient’s chief complaint; AND A brief statement of pathophysiology is included for each diagnosis; AND Each diagnosis in the differential is analyzed using pertinent positive and negative subjective and objective findings as support; AND The differential is ranked in order from most likely to least likely; AND Clinical reasoning skills are demonstrated by linking testing to diagnoses as applicable; AND Testing decisions are well supported with Course Knowledge 2. 3. 4. 5. 6. 7. EBP arguments that are in-line with the clinical scenario and appropriate for the primary care setting (7 critical elements) 1. Discussion post is supported with appropriate, scholarly sources; AND 2. Sources are published within the last 5 years Support from Evidence-Based Practice (EBP) 15 30% 3. 4. (unless it is the most current CPG); AND Reference list is provided and in-text citations match; AND All testing decisions are fully supported with an appropriate EBP argument (4 critical elements) 1. Student provides a substantive* response to at least one topic-related post of a peer; AND 2. Evidence from appropriate scholarly sources are included; AND 3. Reference list is provided and in-text citations Interactive Dialogue 10 20% 4. match; AND Student responds to all direct faculty questions (*) A substantive post adds new content or insights to the discussion thread and information from student’s original post is not reused in peer or faculty response (4 critical elements) Total CONTENT Points= 40 pts DISCUSSION FORMAT Category Points % Description 1. Case study response is presented in a logical format, AND 2. Responses are in sequence with the numbered Organization 5 10% 3. questions AND The case study response is understandable and easy to follow AND 4. All responses are relevant to the case topic (4 critical elements) Grammar, Syntax, 5 10% Discussion post has minimal grammar, syntax, spelling, Spelling & Punctuation punctuation, or APA format errors* Total FORMAT Points= 10 pts DISCUSSION TOTAL= 50 pts due Sunday) PE-Upon exam patient is afebrile with a BP of 156/94, HR 66, RR 20 and o2 sat 94% on room air. His BMI is 39.23. No has clear nasal drainage. S1 and S2 with no murmurs. Lungs are clear bilaterally with faint forced expiratory wheezes in bilateral bases. Respirations unlabored. Legs without edema. Differential Diagnosis ranked most likely to least likely: #1 COPD COPD is a persistent respiratory condition that is common and preventable. Cigarette smoking is the most significant risk factor. COPD is characterized by chronic airflow limitation due to inflammation. Structural changes and destruction of the lung parenchyma take place leading to loss of alveolar attachments to the small airways and a reduction in lung elastic recoil. These changes decrease the ability of the airways to remain open during expiration (GOLD, 2020). Analysis: Pertinent positives- chronic cough (6 months), progressive decrease in activity tolerance due to shortness of breath wheezing, history of smoking and was exposed to smoke as a child since his father smoked Pertinent negatives-afebrile, nasal turbinates without redness or edema, Oropharynx moist, no lesions or exudate, denies sore throat, no family history of COPD #2 Asthma Asthma is a chronic inflammatory disorder of the airways. The inflammation is associated with bronchial hyperresponsive, constriction of the airways, and variable airflow obstruction that is reversible. This causes wheezing, shortness of breath, chest tightness, and coughing. Contributing factors include exposure to allergens, environmental pollution, tobacco smoke, and obesity (GINA, 2019)). Analysis: Pertinent positives- wheezing, on beta blocker, obesity, previous smoker and exposed to smoke as a child since father smoked, cough worse in morning, activity intolerance due to shortness of breath Pertinent negatives-respirations unlabored, no occupational exposure (senior accountant), no known environmental allergies, no family history of asthma #3 Heart Failure Heart failure (HF) is a complex syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. Risk factors include HTN, elevated cholesterol, obesity, diet, and physical inactivity. Symptoms of HF include dyspnea, fatigue, fluid retention, and exercise intolerance. These clinical symptoms result from disorders of the pericardium, myocardium, endocardium, heart valves, or from certain metabolic abnormities (Yancy et al., 2013). Analysis: Pertinent positives- shortness of breath, progressive activity intolerance, persistent productive cough, wheezing, HTN (155/94) Risk factors present: male, 62 yrs. old, history of HTN and smoking- Father has history CHF Pertinent negatives- no edema in extremities, no JVD, heart rate 66 (no tachycardia) Additional test or procedures: Pulse oximetry- a simple non-invasive way to assess the patient’s arterial oxygen saturation. (GOLD, 2020). A decreased oxygen saturation may be present with COPD, Asthma, or HF. It is important to evaluate to determine if supplemental oxygen is needed. Spirometry- Airflow limitation can be measure with spirometry. It is the most widely available and reproducible test of lung function (GOLD, 2020). This is a simple lung function test that can be used to diagnose asthma or COPD. An improvement of 12% and 200lm in the FEV1/FVC ratio after a bronchodilator indicates reversible airway obstruction. This would be helpful to differentiate asthma from COPD (Bringham & West, 2015). Chest x ray- A chest-xray will not diagnose asthma or COPD, but it will be used exclude the presence of some other pulmonary or cardiac diseases (GOLD, 2020). It can show heart enlargement and fluid in the lungs which would help diagnose HF. CBC- A CBC will check for anemia, (which occurs in advanced COPD with hypoxemia), infection, or eosinophilia which would indicate an allergic or asthmatic component (GOLD, 2020). BNP-A lower BNP can exclude the presence of HF and a higher result has a reasonably high predictive value to diagnose HF (Yancy et al., 2013). Reference: Bringham, E. West, N., (2015). Diagnosis of asthma: Diagnostic testing. International Forum of Allergy & Rhinology, 5 (1). 527-530. doi: 10.1022/air.21597 Global Initiative for Asthma. Management and prevention for adults and children over 5 years old. (2019). Retrieved from https://ginasthma.org/gina- reports/ Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2020). Retrieved from https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2- 03Dec19_WMV.pdf Yancy, C. W., Jessup, M., Butler, J., Drazner, M., Geraci, S., Januzzi, J., Kasper, E., Masoudi, F., McMurray, J., Peterson, P., Sam, F., Tang, W., Wilkoff, B. (2013). 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology Foundation/ American Heart Association task force on practice guidelines. Retrieved from http://www.onlinejacc.org/content/accj/62/16/e147.full.pdf? _ga=2.28012988.1211871446.1578704549-315720946.1563672617 [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 01, 2023
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Feb 01, 2023
Downloads
0
Views
52