*NURSING > CASE STUDY > NR 601 Week 2: COPD Case Study Part 2 ( With Purpose, Discussion Format) (All)
NR 601 Week 2: COPD Case Study Part 2 ( With Purpose, Discussion Format)
Document Content and Description Below
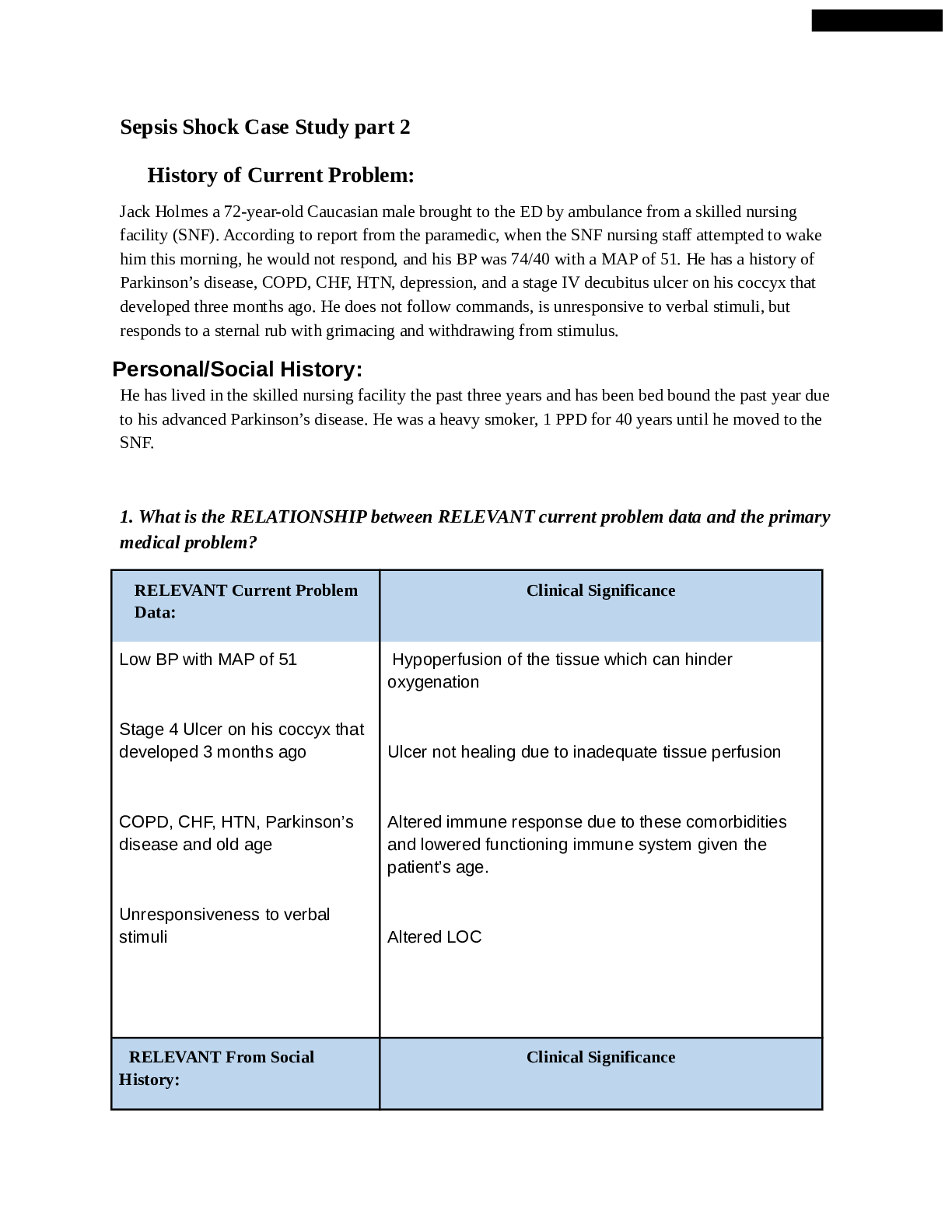
Purpose Problem-based learning is a methodology designed to help students develop the reasoning process used in clinical practice through problem solving actual patient problems in the same manner as... they occur in practice. The purpose of this activity is to develop students’ clinical reasoning skills using a case-based learning exercise. Through participation in an online discussion forum, students identify learning issues in a self-directed manner which facilitates learning for the entire group. Activity Learning Outcomes Through this discussion, the student will demonstrate the ability to: 1. Demonstratecompetenceintheevaluationandmanagementofcommonrespiratory problems(WO2.1)(CO2,3,4,5) 2. Distinguish between obstructive and restrictive lung disease (CO 2, 4) Develop a management plan for the case study patient based on identified primary, secondary and differential diagnoses. (WO 2.2) (CO 2,4) 3. Interpret pulmonary function test results. (WO 2.3) (CO 2, 4) Due Date: Student enters initial post to part one by 11:59 p.m. MT on Thursday; responds substantively to at least one topic-related post of a peer including evidence from appropriate sources AND all direct faculty questions in parts one by Sunday, 11:59 p.m. MT. A 10% late penalty will be imposed for discussions posted after the deadline on Thursday 11:59pm MT, regardless of the number of days late. NOTHING will be accepted after 11:59pm MT on Sunday (i.e. student will receive an automatic 0). Week 8 discussion closes on Saturday at 11:59pm MT. Total Points Possible: 50 Case Study - Part 2 You ordered a CXR and spirometry at the previous visit and he returns today to review the results. Physical exam and symptoms are unchanged since last visit. Vital signs at this visit are: Temp-98.3, P-68, RR-20, BP 152/90, Height 68.9in., Weight 258 pounds, O2sat 94% on RA CXR Result: No acute infiltrates or consolidations are seen. Cardiac and mediastinal silhouettes are normal. No hilar enlargement is evident. Osseous thorax is intact. Spirometry Results: Pre-Bronchodilator Post-Bronchodilator Predicted Actual %Predicted Actual % Predicted % Change FVC (L) 4.52 3.01 67 3.08 68 2 FEV1 (L) 3.40 1.58 46 1.60 47 1 FEV1/FV .75 .52 --- .52 --- 0 Requirements/Questions: 1. What is your primary (one) diagnosis for this patient at this time? (support the decision for your diagnosis with pertinent positives and negatives from the case) 2. Identify the corresponding ICD-10 code. 3. Provide a treatment plan for this patient's primary diagnosis which includes: o Medication* o Any additional testing necessary for this particular diagnosis* o Patient education o Referral o Follow up 4. Provide an active problem list for this patient based on the information given in the case. 5. Arethereanychangesthatyouwouldalsomaketothispatient’soveraltreatmentplanat thistime?MustprovideanEBPargumentforeachtreatmentortestingdecision. *If part of the plan does not warrant an action, you must explain why. ALL medication and testing decisions (or decisions not to treat with medication or additional testing) MUST be supported with an evidence-based practice (EBP) argument. Over-the-counter (OTC) and RXs must be written in full as if handing a script to the patient in the office. Over-the-counter (OTC) and RXs must be written in full as if handing a prescription to the patient in the office. Example: Amoxicillin 500 mg capsule 1 tab po BID q 10 days Disp #20 no refills DISCUSSION CONTENT Category Points % Description 1. Student chooses one appropriate diagnosis for the patient; AND 2. Diagnosis is supported with strong pertinent positive and negative subjective and objective data from parts 1 & 2; AND 3. The ICD code for the diagnosis is correct; AND 4. Treatment plan for primary diagnosis includes medication, additional testing, patient education, and referral; AND Application of Course Knowledge 15 5. 30% Prescription and OTC medications are written appropriately as a RX and all components are correct; AND 6. Treatment decisions (medication, additional testing, referrals) are supported with appropriate EBP arguments; AND 7. An accurate problem list is presented based on case information; AND 8. Student discusses changes (or not) to the overall treatment plan for the patient for pertinent issues; AND 9. An appropriate F/U plan is provided (9 critical elements) 1. Discussion post is supported with appropriate, scholarly sources AND 2. Sources are published within the last 5 years Support from Evidence-Based Practice (EBP) 15 30% 3. 4. (unless the most current CPG is used) AND A reference list is provided with in-text citations that match AND All testing decisions are fully supported with an appropriate EBP argument (4 critical elements) Interactive Dialogue 10 20% 1. Student provides a substantive* response to at 2. 3. 4. least one topic-related post of a peer AND Includes evidence from appropriate scholarly sources AND Provides a reference list which match in-text citations AND Student responds to all direct faculty questions (4 critical elements) Total CONTENT Points= 40 pts DISCUSSION FORMAT Category Points % Description 1. Case study response is presented in a logical format, AND 2. Responses are in sequence with the numbered Organization 5 10% 3. questions AND The case study response is understandable and easy to follow AND 4. All responses are relevant to the case topic (4 critical elements) Grammar, Syntax, Spelling & Punctuation 5 10% Discussion post has minimal grammar, syntax, spelling, punctuation, or APA format errors* Total FORMAT Points= 10 pts DISCUSSION TOTAL= 50 pts due Sunday) Jan 14, 2020Jan 14 at 7:14pm Manage Discussion Entry Primary Diagnosis The primary diagnosis for this patient is moderate COPD (GOLD group 2). The patient has multiple key indicators for the diagnosis of COPD. He has shortness of breath that has increased over time, a cough for 6 months. and wheezing. He is a previous smoker and his father smoked, which increases his exposure to smoke (GOLD, 2020). Pertinent negatives are that the patient denied fever or chills, which rules out an infectious process. He has no redness or edema in his nasal turbinates and his throat has no lesions or exudate. He also denies any sore throat. This helps rule postnasal drip or sinus issues that could be causing the chronic cough. Looking at the diagnostic testing, the chest x-ray was negative: there was no fluid in the lungs or enlargement of the heart. Therefore, the differential diagnosis of heart failure can be ruled out. The pre and post bronchodilator spirometry results did not show a response to the treatment. The bronchodilator did not open the narrowed airways, so the differential diagnosis of asthma can be ruled out. The FEV1/FVC ratio before and after the bronchodilator showed an improvement of 0%. This result would need to be an improvement of 12% or above to indicate reversible airway obstruction (Bringham & West, 2015). For this patient the Fev1/FVC= 52%. The FEV1, the amount of air exhaled with force in the first second, is 1.60 which is 47% of the predicted This is less than 50% of the predicted. Since the FEV1/FVC percentage is over 50% but less than 80%, this patient has a GOLD classification of moderate COPD, GOLD group 2 (GOLD, 2020). ICD 10 code- J44.9 Treatment plan: Medication Since the patient is in group 2, he will be prescribed a short acting bronchodilator (SABA) and a long acting bronchodilator (LABA). I would prescribe a Stiolto inhaler which is a combination of Oladaterol and Tiotropium. This is a combination of a long-acting bronchodilator (Oladaterol) and an anticholinergic (Tiotropium). These medications relax and open the airways to improve breathing. Tiotropium inhibits mucus hypersecretion (Mosely, Smith, & Dutton, 2016). The anticholinergic would be beneficial for this patient’s cough. The benefit of this inhaler is that it only has to be used once a day which increases compliance. It is also steroid free. We have multiple free samples of Stiolto at the office I am at, so it would be free for the patient. From my experience, most insurances cover this inhaler. Patients I have prescribed Stiolto to like that it is a mist and not a powder. The patient would be prescribed ProAir as a rescue inhaler. I would also change this patient’s blood pressure medication to. This patient’s blood pressure was elevated at 154/94 on two separate occasions. He is currently on Toprol XL, which is not controlling his blood pressure. Toprol XL is a beta blocker, which has the side effect of bronchospasms. It is cardioselective, the danger of bronchoconstriction is still present. The patient does not have any known irregular heart rhythms or chest pain that would indicate the need for a beta blocker. Use of blood pressure lowering medication is recommended for primary prevention of cardiovascular disease in patients with a systolic BP over 140 and a diastolic blood pressure over 90. This patient would be classified as stage 2 hypertension (Whelton, Carey, & Aronow, 2017). COPD patients are at increased risk of developing cardiovascular disease, so it is important to manage modifiable risk factors of heart disease such as blood pressure. Prescriptions for this patient: Stiolto Respimat inhaler 2.5mch/2.5mcg Disp- 1 inhaler Sig- inhale 2 puffs every morning RF 1 ProAir HFA 90mcg per actuation Disp- 1 inhaler Sig- 2 puff inhaled every 4-6 hours as needed for shortness of breath RF 1 Lisinopril 10mg tablets Disp- 30 tablets Sig- take one tablet daily RF 1 Additional testing- CAT score--Patient will be assisted with filling out COPD assessment test (CAT). This is a comprehensive assessment of symptoms that will be done with each visit (GOLD, 2020). EKG-is recommended as a baseline in patients with COPD (GOLD, 2020). Lipid profile and Hgb A1c. This patient’s father had a history of heart failure, MI, and diabetes. The results of the lipid panel and identifying if the patient is diabetic will allow for calculation of the patients ASCVD. Assessment of ASCVD is beneficial for primary prevention of cardiovascular disease (Arnett, Blumenthal, Albert, 2019). This patient has major risk factors of cardiovascular disease such as his family history, HTN, and obesity. Patient education Explain to patient what COPD is and his symptoms and diagnostic results that led to his diagnosis. Providing written information, like a pamphlet, would be helpful. He also needs to know how to prevent exacerbations. Exposure to smoke, air pollution, and dust can cause an exacerbation (GOLD, 2020). He needs an understanding of the medications he has been prescribed including purpose, side effects, and how to take them. The patient needs to be educated on how to use the inhalers. The teach-back method should be used. The patient needs to understand that the ProAir is used for an exacerbation, which is a acute worsening of respiratory symptoms (GOLD, 2020). The Stiolto is to be used every day. It is used to prevent exacerbations. Patient will need to stay current with the influenza and pneumonia vaccination (PPSV23). These vaccinations decrease lower respiratory track infections (GOLD, 2020). COPD involves inflammation of the lungs. Exacerbations of COPD are precipitated by respiratory tract infections. Patient needs to understand the importance of attending pulmonary rehab. This will teach him management of the disease. It includes nutrition counseling, exercises that promote energy conservation, nutritional counseling, breathing modifications, and medication education. (GOLD, 2020). He should also be referred to local support groups to prevent anxiety and depression, which is common with COPD patients. Explanation that patient needs to work towards decreasing BMI with diet and exercise. He needs education on DASH diet. This diet is high in fruit, vegetables, and low-fat dairy foods. It has been shown to lower blood pressure as well as LDL (Chiu et al., 2016). [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 01, 2023
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Feb 01, 2023
Downloads
0
Views
61