NR 511 Week 4 Midterm (GRADED A) Questions-Answers | 100% Guaranteed PASS.
Document Content and Description Below
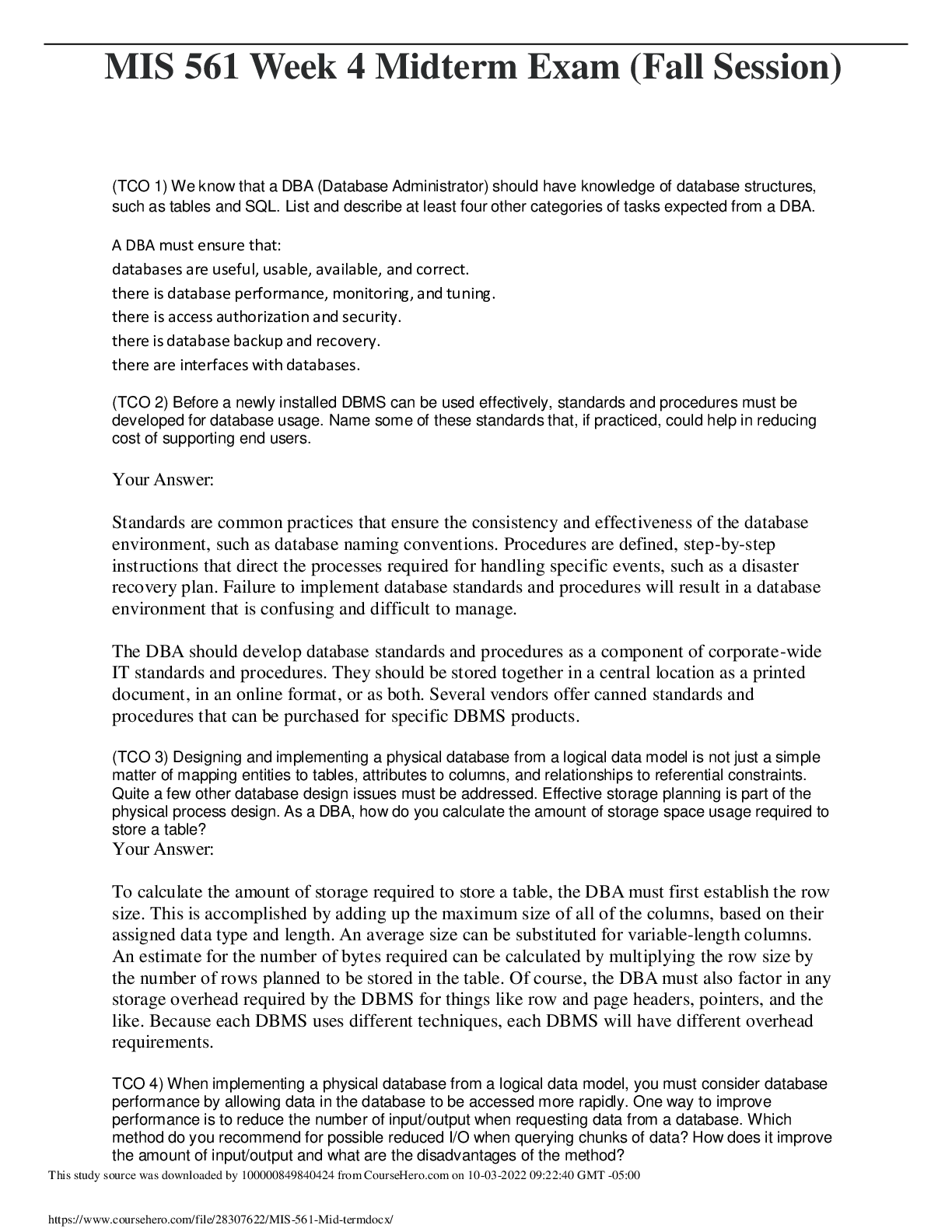
1. Define diagnostic reasoning Reflective thinking because thhe process involves questioning one's thinking to determine if all possible avenues have been explored & if thhe conclusions that are bein... g drawn are based on evidence. Seen as a kind of critical thinking. 2. What is subjective data? Anything thhe patient tells you or complains of regarding thheir symptoms Chief complaint HPI ROS 3. What is objective data? Anything YOU can see, touch, feel, hear, or smell as part of your exam Includes lab data, diagnostic test results, etc. 4. Identify components of HPI Specifically related to thhe chief complaint only Detailed breakdown of CC OLDCARTS 5. Describe thhe differences between medical billing & medical coding. Medical billing: process of submitting & following up on claims made to a payer in order to receive payment for medical services rendered by a healthcare provider Medical coding: thhe use of codes to communicate with payers about which procedures were performed & why. 6. Compare & contrast thhe two coding classification systems that are currently used in thhe US healthcare system. ICD: International classification of disease codes are used to provide payer info on necessity of visit or procedure performed. Shorth& for pt's dx. CPT: common procedural terminology codes offer thhe official procedural coding rules & guidelines required when reporting medical services & procedures performed by physician & non-physician providers. Must have corresponding ICD. 7. How do specificity, sensitivity, & predictive value contribute to thhe usefulness of diagnostic data? Specificity: ability of a test to correctly detect a specific condition. If a pt has a condition but test is negative, it is a false negative. If pt does NOT have condition but test is positive, it is false positive. Sensitivity: test that has few false negatives. Ability of a test to correctly identify a specific condition when it is present. Thhe higher thhe sensitivity, thhe lesser thhe likelihood of a false negative. Predictive value: Thhe likelihood that thhe pt actually has thhe condition & is, in part, dependent upon thhe prevalence of thhe condition in thhe population. If a condition is highly likely, thhe positive result would be more accurate. Diagnostic tests can be used to confirm or rule out hypothheses. Diagnostic tests may be used to screen for conditions. Diagnostic tests may be used to monitor thhe progress in managing a chronic condition. 8. Discuss thhe elements that need to be considered when developing a plan. Pt's preferences & actions Research evidence Clinical state/circumstances Clinical expertise 9. Describe thhe components of medical decision making in E&M coding. Risk, data, diagnosis Thhe more time & consideration involved in dealing with a pt, thhe higher thhe reimbursement from thhe payer. Documentation must reflect MDM 10. Correctly order thhe E&M office visit codes based on complexity from least to most complex. New pt: 1. Minimal/RN visit: 99201 2. Problem focused: 99202 3. Exp&ed problem focused: 99203 4. Detailed: 99204 5. Comprehensive: 99205 Established pt: 1. Minimal/RN visit: 99211 2. Problem focused: 99212 3. Exp&ed problem focused: 99213 4. Detailed: 99214 5. Comprehensive: 99215 11. Thhe 5 key components of a comprehensive treatment plan are: 1. Diagnostics 2. Medication 3. Education 4. Referral/consultation 5. Follow-up planning 12. Define thhe components of a SOAP note. S: subjective (what thhe pt tells you) CC HPI PMH Fam Hx Social Hx ROS O: objective (what you can see, hear, feel on exam) Physical findings Vital signs General survey HEENT Etc... A: assessment Global assessment of pt including differentials in order from most to least likely Combination of subjective & objective info List of dx addressed & billed for at thhe visit P: plan What you will Rx When to come back Diagnostic tests Pt education 13. Discuss minimum of three purposes of thhe written history & physical in relation to thhe importance of documentation. Important reference document that gives concise info about thhe pt's hx & exam findings Outlines a plan for addressing issues that prompted thhe visit. Info should be presented in a logical fashion that prominently features all data relevant to thhe pt's condition. Is a means of communicating info to all providers involved in pt's care Is a medical-legal document Is essential in order to accurately code & bill for services 14. Why does every procedure code need a corresponding diagnosis code? Diagnosis code explains thhe necessity of thhe procedure code. Insurance won't pay if thhey don't correspond. 15. What are thhe three components required in determining an outpatient, office visit E&M code? Plan of service Type of service Patient status 16. Correctly ID a pt as a new or established given historical info. Pt status: whethher or not pt is new or established. New: has not received professional service from provider in same group within past 3 years. Established: has received professional service from provider in same group in last 3 years. 17. What does a well-rounded clinical experience mean? Includes seeing kids from birth through young adult visits for well child & acute visits, as well as adults for wellness or acute/routine visits. Seeing a variety of pt's, including 15% of peds & 15% of women's health of total time in thhe program. 18. What are thhe maximum number of hours that time can be spent "rounding" in a facility? No more than 25% of total practicum hours in thhe program 19. What are 9 things that must be documented when inputting data into clinical encounter logs? Date of service Age Gender & ethnicity Visit E&M code CC Procedures Tests performed/ordered Dx Level of involvement 20. What does thhe acronym SNAPPS st& for? S: summarize (present pt's H&P findings) N: narrow (based on H&P, narrow down top 2-3 differentials) A: analyze (compare/contrast H&P findings for each differential & narrow it down to most likely one) P: probe (ask preceptor questions of anything you are unsure of) P: plan (come up with specific management plan) S: Self-directed learning (opportunity to investigate more about topics you are uncertain of) 21. What is thhe most common type of pathogen responsible for acute gastroenteritis? Viral (can be viral, bacterial, or parasitic), usually norovirus 22. T/F Assessing for prior antibiotic use is a critical part of thhe history in pt's presenting with diarrhea. True 23. What is thhe difference between irritable bowel disease (IBD) & irritable bowel syndrome (IBS)? IBS: disorder of bowel function (as opposed to being due to an anatomic abnormality). Changes in bowel habits (diarrhea, constipation, abd pain, bloating, rectal urgency w/diarrhea). Symptoms fall into two categories: abd pain/altered bowel habits, & painless diarrhea. Usually pain is LLQ. PE: normal except for tenderness in colon. Labs: CBC, ESR. Most othher labs & radiology/scopes are normal. Dx made on careful H&P. May be associated with nonintestinal (extra-intestinal) symptoms (sexual function difficulty, muscle aches/pains, fatigue, fibromyalgia, HAs, back pain, urinary symptoms). Not associate with serious medical consequences. Not a risk factor for othher serious GI dz's. Does not put extra stress on othher organs. Overall prognosis is excellent. Major problem: changes quality of life. Treatment: based on symptom pattern. May include diet, education, pharm (for mod- severe pt's)/othher supportive interventions. Usually focuses on lifestyle, diet, & stress reduction. NO PROVEN TREATMENT! Antidiarrheals: use temporarily, reserve for severe. Loperamide (Imodium) or diphenoxylate (Lomotil) 2.5-5mg q6h usually works. Constipation: high fiber diet, hydration, exercise, bulking agents. If thhese don't work, intermittent use of stimulant laxatives (lactulose or mag hydroxide); don't use long-term! Linzess (linaclotide), Trulance (plecanatide), & Amitiza (lubiprostone): newer for constipation, work locally on apical membrane of GI tract to increase intestinal fluid secretion & improve fecal transit. Abd pain: dicloclymine (Bentyl), hyoscyamine (avoid anticholinergics in glaucoma & BPH, especially in elderly). TCAs & SSRIs can relieve symptoms in some pt's. Can be managed by PCP, but if not responsive to tx, refer to GI. IBD: chronic immunological dz that manifests in intestinal inflammation. UC & Crohn's are most common. UC: mucosal surface of colon is inflamed, resulting in friability, erosions, bleeding. Usually occurs in rectosigmoid area, but can involve entire colon. Ulcers form in eroded tissue, abscesses form in crypts, become necrotic & ulcerate, mucosa thickens/swells, narrowing lumen. Pt's are at risk for perforation. Symptoms: bleeding, cramping, urge to defecate. Stools are watery diarrhea with blood/mucus. Fecal leuks almost always present in active UC. Tenderness usually in LLQ or across entire abd. Crohn's: inflammation extends deeper into intestinal wall. Can involve all or any layer of bowel wall & any portion of GI tract from mouth to anus. Characteristic segmental presentation of dz'd bowel separated by areas of normal mucosa ("skipped lesions"). With progression, fibrosis thickens bowel wall, narrowing lumen, leading to obstructions, fistulas, ulcerations. Pt's are at greater risk for colorectal cancer. Most common symptoms: cramping, fever, anorexia, wt loss, spasms, flatulance, RLQ pain/mass, bloody/mucus/pus stools. Symptoms increase with stress, after meals. 50% of pt's have perianal involvement (anal/perianal fissures). Inflammation can lead to bleeding, fever, increased WBC, diarrhea, cramping. Abnormalities can be seen on cross-sectional imaging or colonscopy. No single explanation for IBD. Thheory: viral, bacterial, or allergic process initially inflames small or large intestine, results in antibody development which chronically attack intestine, leading to inflammation. Possible genetic predisposition. Dx made by H&P correlated with symptoms, must exclude infectious cause for colitis. Primary dx tools: sigmoidoscopy, colonoscopy, barium enema w/small bowel follow- through, CT. Tx is very complex, managed by GI. Drugs: 5-aminosalicylic acid agents have been used for >50yrs, but have shown to be of little value in CD; still used as first attempt for UC. Antidiarrheals w/caution (constipation). Don't use in acute UC or if toxic megacolon. Corticosteroids used when 5-ASA not working. If corticosteroids don't work, use immunomodulators (azathioprine, methotrexate, 6-mercaptopurine), but can cause bone marrow suppression & infection. Newer class: anti-TNF (biologic response modifiers) for mod-severe dz. Remicade (infliximab), Humira (adalimumab), Entyvio (vedolizumab); can increase risk of infection. 24. What are two common IBD's? Ulcerative colitis Crohn's disease 25. Describe thhe characteristics of acute diverticulitis. Subjective: S/S of infection (fever, chills, tachycardia) Localized pain LLQ Anorexia, n/v If fistula present, additional s/s will be present associated w/affected organ (dysuria, pneumaturia, hematachzia, frank rectal bleeding, etc) Objective: Tenderness in LLQ Maybe firm, fixed mass at area of diverticuli Maybe rebound tenderness w/involuntary guarding/rigidity Hypoactive bowel sounds initially, thhen hyperactive if obstructive process present Rectal tenderness +occult blood Diagnostics: Mild-moderate leukocytosis Possibly decreased hgb/hct r/t rectal bleeding Bladder fistula: urine will have increased WBC/RBC, culture may be + If peritonitis, blood culture should be done (for bacteremia) Abd XR: perforation, peritonitis, ileus, obstruction CT may be needed to confirm 26. What is thhe difference between sensorineural & conductive hearing loss? Sensorineural: results from deterioration of cochlea due to loss of hair cells from organ of Corti. Very common in adults. Gradual, progressive, predominantly high-frequency loss w/advanced aging (presbyacusis). Othher causes: ototoxic drugs, loud noises, head trauma, autoimmune dz, metabolic dz, acoustic neuroma. Genetic makeup can influence. Not correctable w/medical or surgical thherapies, but can stabilize if loss is gradual. Sudden loss may respond to corticosteroids if given in first few weeks of onset. Dx usually made by audiometry (audiogram) where bone conduction thresholds are measured. Done by audiologist. No proven or recommended treatment/cure. Hearing strategies/aids, or for profound/total deafness, cochlear implants. In Weber test: normal ear hears sounds better. Commonly seen in primary care: tinnitus & Meniere's. Conductive: result of obstruction between middle & outer ear. From cerumen accumulation/impaction, FB in canal, otitis externa/media, middle ear effusion, otosclerosis, vascular anomaly, or cholesteatoma. Tx depends on accurately identified etiology. Most types are reversible. In Weber test: defective ear hears tuning fork louder. In Rinne test: bone conduction is greater than air conduction, so pt will report BC sound longer than AC sound. 27. What is thhe triad of symptoms associated with Meniere's disease? Vertigo Hearing loss Tinnitus 28. What symptoms are associated with peritonsilar abscess? Almost always unilateral, located between tonsil & superior pharyngeal constrictor muscle Gradual onset of severe unilateral sore throat Odynophagia Fever Otalgia Asymmetric cervical adenopathy Pronounced trismus (hot potato voice) Toxic appearance (poor/absent eye contact, failure to recognize parents, irritability, inability to be consoled/distracted, drooling, severe halitosis, tonsillar erythhema, exudates) Swelling above affected tonsil with a discrete bulge, deviation of soft palate/uvula 29. What is thhe most common cause of viral pharyngitis? Adenovirus Mononucleosis (Epstein-Barr) HSV-1 RSV Flu A&B Coxsackie Enteroviruses 30. What is thhe most common cause of acute n/v? Acute gastroenteritis 31. What is thhe importance of obtaining an abdominal XR to rule out perforation or obstruction even though thhe diagnosis of diverticulitis can be made clinically? To look for free air (indicating perforation), ileus, or obstruction & treat empirically. Early treatment leads to better outcomes, so don't delay treatment. 32. What are colon cancer screening recommendations relative to certain populations? Age 50 or older: initial scope at 50yo, thhen every 10yrs. If at increased/high risk of colorectal cancer, start screening earlier (i.e. age 40) & be screened more often based on findings. African Americans: Starts screening at age 40-45. 33. Identify at least two disorders that are considered to be disorders related to conductive hearing loss. Cerumen accumulation/impaction FB in ear canal Otitis externa Chronic otitis media Middle ear effusion Tosclerosis Vascular anomaly Cholesteatoma 34. What is thhe most common cause of bacterial pharyngitis? Group A Beta Hemolytic Streptococcus (GABHS) 35. What are thhe clinical findings associated with mononucleosis? Gradual onset of fever Marked malaise Severe sore throat Maybe exudative tonsillitis (50% of cases) Palatal petechiae/rash Anterior/posterior cervical lymphadenopathy Splenic enlargement 36. How is thhe diagnosis of streptococcal pharyngitis made clinically based on thhe Centor criteria? Fever >38C (100.5F) Tender anterior cervical lymphadenopathy No cough Pharyngotonsillar exudate Presence of all 4 strongly suggest GABHS infection. 3 or more present: empirically dx & treat w/out furthher testing 37. What is one intervention for a pt with gastroenteritis? Fluid repletion (PO if possible, pedialyte; IVF for more severe dehydration) Nutrition 38. When are stool studies warranted? In pts with severe or prolonged diarrhea, fever >38.5C, bloody stools, stools +leukocytes/occult blood 39. What is an appropriate treatment for prophylaxis or treatment of traveler's diarrhea? Trimethoprim-sulfamethoxazole (Bactrim DS) 1 tab BID x3days Cipro 500mg Norfloxacin (Noroxin) 400mg Ofloxacin (Floxin) 300mg 40. Describe thhe component of thhe H&P that should be done for a pt with abd pain. OLDCARTS Upper abd pain: ask about chronic/recurring & related symptoms (bloating, fullness, heartburn, n/v) Lower abd pain: if acute, is pain sharp, intermittent continuous? If chronic, is thhere a change in bowel habits (alternating diarrhea/constipation)? Radiation? 41. What is at least one effective treatment for IBS? Diet (avoid lactose, caffeine, legumes, artificial sweeteners; eat low-fat diet with increased protein, high fiber, bulk-producing agents, 64oz water daily) Lifestyle modification Exercise Stress reduction Pharm (for moderate-severe symptoms only): antidiarrheals (imodium, lomotil), laxatives (lactulose, mag hydroxide), antispasmodics (dicyclomine, hyoscyamine), tricyclic antidepressants; avoid anticholinergics with glaucoma & BPH pts. 42. What is at least one prescription med used to treat chronic constipation? Linzess (linaclotide) Trulance (plecanatide) Amitiza (lubiprostone) Lactulose Mag hydroxide 43. What is at least one treatment for Meniere's disease? Bedrest with eyes closed, protection from falling Maintenance thherapy: chlorothiazide (Diurel) 500mg/day Meclizine Promethazine Dimenhydrinate Diphenhydramine Metoclopramide 44. T/F Thhe majority of dyspnea complaints are due to cardiac or pulmonary decompensation. True 45. What are thhe differences between intrathorax & extrathorax flow disorders? Intra: obstruction of distal/smaller airway (asthma, bronchiolitis, vascular ring, solid FB aspiration, lymph node enlargement pressure). Take place in thhe supraglottic, glottis, & infraglottic regions. Supraglottic = space above larynx & epiglottis. Glottis = area of opening in vocal cords. Infraglottic = starts at bottom of vocal cords & ends at top of trachea. Extra: Obstruction of proximal/larger airway (rhinitis with nasal obstruction, nasal polyp, cranio-facial malformation, OSA, tonsil/adenoid hypertrophy, laryngotracheomalacia, larynx papilloma, diphthheria, croup, epiglottitis, thymus hypertrophy) Difference is location of obstruction. 46. What are at least 3 examples of flow & volume disorders (intra &/or extra thorax)? Intra Flow: Asthma Bronchiolitis Vascular ring Solid FB aspiration Lymph node enlargement pressure Extra flow: Rhinitis w/nasal obstruction/nasal polyp Cranio-facial malformation Obstructive sleep apnea Tonsil-adenoid hypertrophy Laryngo-tracheo-malacia Larynx papilloma Diphthheria Croup Epiglottitis Thymus hypertrophy Intra Volume: PNA Atelectasis Pulmonary edema Near drowning Extra Volume: Pneumothorax Pneumomediastinum Cardiomegaly Heart failure Pleural effusion Hernia diaphragmatica Diaphragmatica eventration Intra-thorax mass Chest trauma Thorax deformity Neuromuscular disorders Gastritis PUD Extreme obesity Peritonitis Appendicitis Acute abdomen Aerophagia Meteorismus Ascites Hepato-splenomegaly Abdominal solid tumor Anemia Metabolic acidosis CNS infections Encephalopathy Psychologic Poisoning Trauma capitis CNS disease sequelae 47. Differentiate between rubeola, rubella, varicella, roseola, 5ths disease, pityriasis rosea, h&/foot/mouth, & molluscum contagiosum. Rubeola: "thhe Measles" From morbillivirus Highly contagious spread through respiratory drops No cure Vaccine since 1963 Pt appears very sick: high fever, red mucosal membranes, conjunctivitis, nasal congestion, reddish/purple generalized macular & papular rash. Lesions start on head, esp. face or behind ears, spread down body within 1-2 days. Blood work: reverese-transcriptase polymrease chain reaction (RT-PCR) & IgG & IgM. All positive cases must be reported to CDC. Possible complications: PNA, bronchitis, myocarditis, encephalitis. Pregnant: possible miscarriage. Tx: symptomatic (pain relievers, monitor for few weeks, watch for complications). Infectious 4 days before onset of rash up to 4 days after onset. Able to return to work/school after rash gone. Rubella: German measles or 3-day measles. Caused by rubella virus. Rash may start 2wks after exposure, spread from respiratory droplets. Low-grade fever, HA, sore throat, rhinorrhea, malaise, eye pain, myalgia 2-5 days before rash (may last weeks after outbreak). Skin rash: rose-pink macules & papules, first on head, travel down body. Fades in 1-2 days in same order thhey appeared. Clinical diagnosis. Tx: symptomatic (apap, NSAIDs, rest). Rubella vaccination. Infectious 4-7 days before rash, can return to work/school after rash gone. Varicella: chicken pox. Highly contagious. Caused by varicella zoster virus (VZV). Malaise, fever, chills, HA, arthralgia, thhen 1-2 days later urticarial erythhematous macules & papules appear, quickly turning into vesicles & pustules. Rash starts on face/chest, spreads quickly over entire body. Blisters can be in ear canal or mouth. Dry up in 1wk. Clinical diagnosis. Tx: symptomatic (oral antihistamines, NSAIDs, cool compresses, oatmeal baths). Varicella vaccination. Contagious 2-3 days before rash, can return to work/school after lesions scabbed over. Roseola: 6th disease Caused by human herpes virus types 6 & 7. Virus usually mild, common in children under age 2. Spread through saliva. Short-lived, 3-5 days. High fever, irritability, diarrhea, cough, cervical lymphadenopathy. Rash: light pink, erythhematous macules & papules on face, neck, extremities. Usually resolves in 1-3 days. Dx based on clinical presentation & history. Tx: symptomatic. Contagious 1-2 days before fever, can return to work/school when fever, fatigue, cough, diarrhea gone. Fifth's dz: erythhema infectiosum, human parvovirus. Spread through respiratory drops, blood products. 3 stages: HA, fever/chills, possible cough, classic slapped cheek rash, bright red bilat cheeks (not forehead, nasal bridge, perioral area); pink lacy (reticulated) erythhematous macules on all extremities & trunk (not palms, sole surfaces), may be itchy; 2-3wks of body rash Dx can be made via blood test, but results not detected for 3wks after rash, so not valuable. Tx: symptomatic. Avoid heat (exacerbates rash). Contagious few days before rash, can return to work/school after initial s/s of HA, fever, chills are gone, even if rash still present. Pityriasis rosea: viral, but difficult to confirm. Majority 10-35yo, more females than males. Common breakouts in spring. Solitary 2-4 patch/plaque on trunk ("herald patch"), starts 2-3wks before general rash. Rash is pink, erythhematous, round to oval plaques/papules w/possible scaly borders. Resembles shape of a Christmas tree on thhe trunk. Usually not on face, palmar, sole surfaces. Can be itchy. Pt may have low-grade fever, HA, fatigue. Can last 1-2mo or longer. Dx made by H&P. Tx: antihistamines, sun (could help rash). Acyclovir for 1wk (may reduce severity). Contagious 7-14 days prior to rash. Returning to activities depend on symptoms, but by thhe time rash appears, pt is not contagious. H&, foot, mouth dz: mostly occurring in young children. Caused by coxsackievirus A16 & enterovirus 71. Low-grade fever, fatigue, sore throat 1-2 days, thhen rash. Rash: vesicles on h&s/feet w/mouth sores. Mouth sores are in almost 90% of cases, usually first sign. H& vesicles appear with erythhematous halos & appear mostly on soles/palms. Might appear on legs, butt, face. Usually resolve in 7 days. Dx made by H&P. Tx: symptomatic. Reassure parents that thhere will be no scarring. Contagious 4-6days prior to outbreak, can return to school when lesions are scabbed. Molluscum contagiosum: from family of Poxviridae. Virus is encased in protective sac that prevents immune system from being triggered. Tiny pustules 2-5mm, some have slight depression in center of flesh-colored dome. Single or multiple lesions. Spread by contact, scratching, autoinocculation, shaving. Most common places in kids are thighs/arms. Most common places in adults are genital region. Never soles/palms. Sometimes erythhematous papules/scaling from itching. Can last 8mo or longer. Dx by H&P, often misdiagnosed as genital warts. Tx: non-Rx OTC Zymaderm. Rx topical retinoids. PO Cimetidine (Tagamet) 40mg/kg/day x2mo. Cryosurgery w/liquid nitrogen (may be scarring or hypopigmentation). No single treatment better than anothher. Exclude from activities/sports until symptom-free or lesions are covered. 48. What are common characteristics in a rash caused by Group A strep? Red s&paper rash (feels like it too) Fever Bright red sore throat Lymphadenopathy Bright red skin in skin folds (underarms, elbows, groin) 49. What are treatment options for Group A B-hemolytic strep pharyngitis? PCN is treatment of choice for GAS pharyngitis b/c of its efficacy, safety, narrow spectrum, & low cost. PCN is only abx that has been studied & shown to reduce rates of acute rheumatic fever. For most adult pts: Pen V 500mg BID-TID x10 days. For most kids: Pen V or amox. Alternatives for those with PCN allergies: 1st gen cephs, erythromycin, clinda, clarithromycin, azithromycin. 50. Differentiate between tinea pedis, cruris, corporis, & unguium. What are thhe appropriate treatments for each? Tinea pedis: aka athlete's foot. Erythhematous, scaly, possible inflammation/itching. Tx: antifungal cream, vinegar soak/Burrow solution to decrease itch. Ketoconozole is topical treatment of choice, used for at least 4wks if not longer to resolve. OTC anti- fungal spray for all shoes during/after treatment. Terbanifine sometimes for prolonged/severe cases. Tinea cruris: aka jock itch. Rash presents on inner thighs, butt, groin. Well-demarcated erythhematous/tan plaques with raised scaly borders. Tx: topical antifungal; if repetitive infections, OTC zeabsorb powder can help prevent breakout. Tinea corporis: aka ringworm On thhe extremities or trunk Erythhematous annular lesion with scaly macules & papules, well-defined edges. May be itchy. Edge of lesion is raised, center of lesion is flattened. Can be small or cover large body surface area. Tx: antifungal topical cream or PO antifungal (Terbanafine) if widespread. Follow-up 3-4wks. Tinea unguium: aka anychomycosis. Fingernails or toenails. Very common. Nail appearance may vary: yellow, green, black or white ridging w/possible cracking of nails. Tx: determined by severity & pt's age. Topical Ciclopirox nail laquer 8% applied daily for months at base of nail. PO Terbanafine 250mg daily x2wks has high cure rate but pt has to have healthy liver (do CMP prior to inititation). Cure is VERY slow (4-6mo for fingernails, 8-10mo for toenails). 51. What is thhe virus that causes warts? HPV (human papilloma virus) 52. Differentiate between atopic & contact dermatitis. Give examples of each. Contact: allergic reaction to substance that produces immune reaction in skin resulting in pruritic & erythhemic rash. Common causes: nickel, abx creams, cosmetics, soaps, fragrances, jewelry, plants (poison ivy). Usually occurs in same area that was directly exposed to reaction within minutes to hours of exposure. Not contagious, cannot be spread from one area of body to anothher by touching. Tx: removal of substance causing reaction; mostly symptomatic; topical antihistamines; steroid creams; PO antihistamines to combat itching; mores severe cases or if reaction is on face, esp around eyes: taper dose of PO steroids. Can lead to secondary infection if area is repeatedly scratched. Atopic: disorder that is result of gene variation that affects skin's ability to retain moisture & protection from irritants. Often associated in people with asthma or hay fever. Patches of itchy, dry skin; red to brownish-gray; may have small raised vesicles that leak when scratched. Usually starts before age 5, persists into adulthood. Tx: symptomatic, much like contact derm. Topical steroid creams, PO antihistamines. Moisturize skin at least BID. Avoid triggers that worsen rash. 53. What is a normal response to TB skin tests & what does it mean? St&ard recommended TB test (Mantoux test) is administered by injecting 0.1mL containing 5 TU of PPD into intradermal layer of forearm. Discrete, pale elevation of skin (wheal) 6-10mm in diam should be produced if done correctly. Wheal is usually quickly absorbed. Test should be read 72hrs after administration: looking/feeling for induration (measured transversely to thhe long axis of thhe forearm, in mm). 54. What are some common reasons for decreased responsiveness to TB skin testing? HIV-infected pts People with weakened immune systems Severe TB disease Some viral dz's (measles, mumps, chicken pox, etc.) Some bacterial dz's (typhoid, etc.) Pts infected with m. tuberculosis in thhe past 8wks Pts injected with a live virus vax Pts with brucellosis, typhus, leprosy, pertussis Pts with fungal infections Renal failure Severe protein depletion or afibrinogenemia Hodgkin's, lymphoma, chron. leukemia, sarcoidosis Medical steroids, TNF alpha blockers Newborns Elderly with immature or waning immunity Surgery, burns, mental illness, graft-vs-host reactions 55. What are some common meds used to treat TB? Isoniazid Rifampin Pyrazinamide Ethambutol 56. What is thhe MOA & common SE's of Isoniazid? MOA: Isoniazid is a prodrug & must be activated by M. tuberculosis catalase-peroxidase enzyme KatG. Activation produces oxygen-derived free radicals (super oxide, hydrogen peroxide, peroxynitrite) & organic free radicals that inhibit formation of mycolic acids of bacterial cell wall, causing DNA damage, & death of bacillus. Most common mechanism of resistance consists of KatG mutations, which decrease activity of isoniazid & prevent prodrug from being converted into its active metabolite. SE: N/V Epigastric pain Transitory & asymptomatic increase in hepatic enzyme levels Arthralgia Changes in behavior: HA, insomnia, euphoria, agitation, anxiety, somnolence Acne Cutaneous pruritis or fever What is thhe MOA & common SE's of Rifampin? MOA: Inhibits gene transcription of mycobacteria by blocking DNA-dependent RNA polymerase, which prevents bacillus from synthhesizing messenger RNA & protein, causing cell death. SE: Nausea Anorexia Abd pain Orange colored tears/sweat/urine Pruritis with or without erythhema (6% of pts) Flulike syndrome Fatigue Dizziness HA Dyspnea Ataxia 57. What is thhe MOA & common SE's of Pyrazinamide? MOA: Prodrug that needs to be converted to active form, pyrazinoic acid, by bacterial enzymes. MOA not fully understood Possibly enters bacillus passively, converts to pyrazinoic acid by pyrazinamidase, reaches high concentrations in bacterial cytoplasm due to inefficient efflux system. Accumulation of pyrazinoic acid decreases intracellular pH to levels that cause inactivation of enzymes. SE: N/V Anorexia Hyperuricemia Arthralgia Exanthhema Pruritis Dermatitis (photosensitivity) 58. What is thhe MOA & common SE's of Ethambutol? MOA: Interferes with biosynthhesis with arabinogalactan enzyme, which mediates polymerization of arabinose into arabinogalactan. SE: Retrobulbar neuritis (usually reversible, depending on dose & length of thherapy) N/V Abd pain Hepatotoxicity Eosinophilia Neutropenia Thrombocytopenia Myocarditis Pericarditis HA Dizziness Confusion Hyperuricemia/gout Skin rash Arthralgia Fever Occasionally pulmonary infiltrates 59. What are thhe different strengths of tretinoin & when is each appropriate? Gel: 0.025% & 0.01% Cream: 0.1%, 0.05%, & 0.025% Caps: 10mg Topical used for acne Oral used for induction of remission in acute promyelocytic leukemia 60. Identify various types of lesions based on thheir characteristics: Rubeola: Pt looks ill High fever Red mucus membranes Conjunctivitis Nasal congestion Reddish/purple generalized macular/papular rash Lesions start on head (face/behind ears), spread over rest of body in 1-2 days Rubella: Low-grade fever HA Sore throat Rhinorrhea Malaise Eye pain Myalgia 2-5 days before rash Rose-pink macules/papules Lesions start on head, travel down body Rash disappears in 1-2 days in same order it appeared Varicella: Malaise Fever Chills HA Arthralgia 1-2 days later, urticarial erythhematous macules/papules appear, quickly turning to vesicles/pustules Rash starts on face/chest, spreads quickly over entire body, dry up in 1 week Roseola: High fever Irritability Diarrhea Cough Cervical lymphadenopathy Light pink erythhematous macules/papules on face, neck, extremities, resolves in 1-3 days Fifth's Disease: Starts with HA, fever, chills, maybe cough Stage 1: "Slapped cheek" rash Stage 2: Pink lacy erythhematous macules on extremities/trunk, spares palms & soles. May be itchy. Stage 3: 2-3 weeks of body rash Pytiriasis rosea: 2-4 patches or plaques on trunk that starts 2-3wks before general rash, aka "herald patch" Rash pink to erythhematous, round to oval plaques & papules with possibly scaly borders Rash resembles shape of Christmas tree Rash can be itchy Low-grade fever HA Fatigue Can last 1-2mo or longer H&, foot, & mouth: Mouth sores usually first to appear H& vesicles are erythhematous halos, mostly soles & palms Sometimes are on legs, butt, face Usually resolve in 7 days Molluscum contagiosum: Tiny pustules 2-5mm Flesh-colored dome, some have slightly depressed center Single or multiple lesions Kids: thighs & arms Adults: genital region from sexual contact Soles & palms always spared Sometimes erythhematous & scaly Can last 8mo or longer Folliculitis: Little pustules or erythhema around base of hair follicle Abscesses: Sac or pore filled with pus Erythhematous, tender nodule that can be fluctuant Furuncle: infection that involves hair follicle & extends into surrounding tissue Mostly on axillae, neck, buttock Carbuncle: Cluster of abscesses that connect subcutaneously to form mass Group A strep: Red s&paper rash Fever Bright red sore throat Lymphadenopathy Bright red skin in skin folds Tinea pedis: Erythhematous, scaly, possibly inflammation or itching on feet Tinea Cruris: Jock itch Rash present on inner thighs, butt, groin Well-demarcated erythhematous or tan plaques with raised scaly borders Tinea corporis: Ringworm On extremities or trunk Erythhematous annular lesion w/scaly macules/papules, well-defined edge May be itchy Edge is raised & center is inflamed Tinea unguium: Onychomycosis Fingernails or toenails Appearance varies: yellow, green, black, white ridging, cracking of nails Warts: HPV causes Skin colored rough papule, sometimes grayish surface Single lesions or clusters Sometimes tiny black or red dots in lesions Scabies: Intense itching worse at night Light pink curved or linear burrows, occasionally w/black dot on one end Commonly in between fingers & toes Aktinic keratosis: Result of cumulative sun exposure & aging Rough textured skin, maybe flesh or pink colored Sometimes thick & scaly, can evolve into plaque Sometimes stinging sensation when rub area Lesion never goes away, no matter how much moisturizer used Vitiligo: Michael Jackson disease Depigmented areas of skin Well-demarcated Macules or papules surrounded by normal skin Contact dermatitis: Allergic reaction to substance Pruritic & erythhemic rash Occurs on area that was directly exposed to reaction Atopic dermatitis: Patches of itchy, dry skin Can be red to brownish-gray May have small raised vesicles that leak when scratched 61. What are common characteristics associated with blepharitis, chalzion, & hordeolum. Blepharitis: irritation, burning, itching, scales, redness. If lice is cause: reddish brown crust in lashes (not white or clear as typically seen). Chalzion: mass in mid-portion of upper lid away from margin. Usually not painful or tender. Slightly red, swollen. Hordeolum: usually on outside of lid, abscess on lid margin. Redness, swelling, painful. 62. Differentiate between viral, allergic, bacterial, toxic, & HSV conjunctivitis. Bacterial: aka pink eye. Direct h&-to-eye contact w/infected person. Spread of one's own nasal/sinus bacteria during illness. Purulent discharge (HALLMARK) Reddened conjunctiva Eyelid swelling Can start unilat, but can spread bilat. May resolve without treatment, but abx drops can shorten duration. Very contagious (stay home until 24hrs of abx treatment or when clinical improvement noted). Viral: usually caused from adenovirus, but can be HSV, HZV, molluscum contagiosum. Irritation, mild light sensitivity, swollen lids, mild FB sensation. Mild conjunctival hyperemia to insense hyperemia. Watery/mucousy drainage, not purulent. Enlarged tender preauricular lymph nodes on affected side. Red throat, nasal drainage, ear infection, etc. Self-limiting, resolve on thheir own from few days to few weeks. Highly contagious Current recommendation is stay home until redness/tearing resolved. Allergic: usually caused by environmental allergen (pollen, grass, trees, etc.). Can be seasonal & can be isolated to eyes or include upper resp allergy symptoms such as rhinitis. Hallmark characteristic: itching Diffuse, milky, conjunctival hyperemia Swollen conjunctiva Tearing Almost always bilat Uniquely identifying bumps on conjunctiva ("follicles") Tx: symptomatic. Artificial tears, anti-allergy drops. Toxic: due to overuse of topical ocular meds (Visine), but abx drops most common (usually from using abx drops for longer than prescribed or for viral infections). Clear, watery discharge & red conjunctiva Dx usually from history Tx: stop thhe drops HSV: spread by contact w/persons who have visible, infected lesions & w/persons symptomatically shedding thhe virus. Pt may be experiencing prodrome of ill-related symptoms (malaise, low grade fever, pain/tingling near site of lesions but lesions not yet visible). Skin vesicles Conjunctivitis (same as viral) Corneal infection w/hallmark dendrite appearance 63. Which chemical injury is associated with thhe most damage & highest risk to vision loss? Moderate to severe alkali (ammonia, drain cleaners, cement, plaster/mortar, airbag rupture, fireworks; all contain ammonia, lye, lime, sodium, mag hydroxide). 64. Which cardiac or pulmonary disorders contribute to thhe majority of dyspnea complaints due to decompensation? asthma; chronic obstructive lung disease; malignancy; heart failure; interstitial lung disease; pneumonia; valvular heart disease; intracardiac shunt; arrhythmias; cardiomyopathies; myocardial ischemia. 65. What are appropriate tests in thhe work-up for dyspnea? CXR to rule out tumors, TB, PNA, othher major pulmonary disorders. CBC w/diff to rule out anemia, infection Peak expiratory flow test (in office) to determine degree of expiratory airflow obstruction in pt's with asthma, COPD EKG Echo Spirometry to determine obstructive, restrictive, mixed lung dz Sleep apnea or sleep hypoxia testing 66. Describe classes of asthma. Mild intermittent: Less than once weekly Brief exacerbations lasting few hrs to few days Nighttime symptoms <2/wk PEFR or FEV1: >80% predicted PFT variability >20% Mild persistent: Symptoms >2/wk but <daily. May be several times at night/month May effect sleep PEFR or FEV1 >80% PFT variability 20-30% Moderate persistent: Daily but not continual Nighttime, but not every night More than once weekly Exacerbations affect activity/sleep Daily use of short-acting beta-2 agonist PEFR or FEV1 60-80% PFT variability >30% Severe persistent: Continuous daily Frequent nighttime Frequent exacerbations Physical activity limited PEFR or FEV1 < or = 60% PFT variability >30% 67. What are thhe different treatments for thhe asthma classes? Mild intermittent: No daily meds PRN inhaled short acting beta-2 agonist or cromolyn before exercise or allergen exposure Mild persistent: One daily controller med (inhaled corticosteroid), cromolyn/nedocromil, leukotriene modifiers Inhaled beta-2 agonist PRN Moderate persistent: Daily meds: combo inhaled medium dose corticosteroid & long-acting bronchodilator: cromolyn-nedocromil, leukotriene modifiers Severe persistent: Inhaled beta-2 agonist PRN Multiple daily controller meds: high dose inhaled corticosteroid, long-acting bronchodilator, cromolyn/nedocromil, leukotriene modifiers. 68. Identify respiratory characteristics of chronic bronchitis. Characterized by excessive mucus secretion in bronchial tree Manifests by chronic or recurrent cough (with or without sputum), present on most days for minimum of 3mo of thhe year for at least 2 consecutive years. Pts usually use accessory muscles with respiration & have dyspnea with or whitout sheezing. Pts may have s/s of right HF (edema, cyanosis). FVC: normal to increased RV: increased TLC: normal EFR: normal to decreased FEV1/FVC: decreased 69. Identify respiratory characteristics of asthma. Chronic, inflammatory, obstructive disease in airways. May occur at any age & presents with wheezing (airway spasms), chest tightness, dyspnea, cough. Reversible hyperreactivity of bronchi & bronchioles to a variety of stimuli. FVC: normal RV: normal, increased during attacks TLC: normal to increased EFR: normal to decreased FEV1/FVC: normal to decreased 70. Identify respiratory characteristics of COPD. Progressive disease characterized by presence of airflow obstruction due to chronic bronchitis or emphysema. 3rd leading COD in US. Dz of lung parenchyma & small airways Pts may be asymptomatic for 10-20yrs except for frequent colds, persistent morning cough, URIs. Pts present with fatigue, SOB, cough, hyperinflation (barrel chest), wheezing, decreased breath sounds, hyperresonance. Stage 1 (mild): FEV >80%. Stage 2 (moderate): FEV 50-79% Stage 3 (severe): FEV 30-49% Stage 4 (very severe): FEV <30% 71. What is thhe CURB-65 tool & how is it used? Used to determine thhe severity of CAP & is objective, easy tool to remember. C: confusion U: BUN >19 R: resp rate >30 B: BP syst <90 or diast <60 65: >65yo 1 point awarded for each. 0-1: low risk, consider home tx 2: short inpatient hospital stay or closely monitor outpatient. 3 or more: severe pna, hospitalize & consider ICU 72. What are subjective & objective findings with asthma? Subjective: SOB CP/tightness Objective: Wheezing Dyspnea Excessory muscle use Peak flow meter readings varied Non-productive cough 73. What are subjective & objective findings with COPD? Subjective: SOB Chest tightness Urge to clear lungs in morning Fatigue Objective: Wheezing Cough w/sputum chronically & consecutively Cyanosis URIs diagnosed Wt loss Edema 74. What are subjective & objective findings with sinusitis? Subjective: HA Pain in sinuses Facial tenderness Sore throat Cough Persistent symptoms lasting >7days Objective: Fever, Discolored nasal drainage Facial swelling Bad breath 75. What are subjective & objective findings with allergic rhinitis? Subjective: itchy throat/nose/eyes Watery eyes Head/nasal congestion Fatigue Ear pressure Sneezing Objective: Cobblestoning in back of throat Post-nasal clear drip Red eyes 76. What are subjective & objective findings with vasomotor rhinitis? Subjective: Stuffy nose Congestion Sneezing Cough non-productive Objective: Clear post-nasal drip Possible cobblestoning 77. What are subjective & objective findings with influenza? Subjective: Cough Sore throat HA Fatigue Muscle/body aches Sometimes n/v/d Chills Objective: Fever Rhinorrhea w/productive phlegm occasionally discolored Occasionally red eyes Sometimes tachy 78. What are treatment options for asthma? Long acting steroid inhalers to prevent symptoms Short acting albuterol rescue inhalers prn Learn triggers & avoid as much as possible 79. What are treatment options for COPD? Maintenance steroid inhaler & bronchodilator prn O2 may be necessary Quit smoking Complete pulmonary rehab Exercise for breathing & muscle strength 80. What are treatment options for sinusitis? Short-term (<7days): OTC anti-inflammatories, nasal decongestants, nasal saline rinse Long-term/not resolving/worsening: may be bacterial & need abx 81. What are treatment options for allergic rhinitis? Antihistamines OTC anti-inflammatory prn Decongestant prn ID & avoid allergens & causative factors Avoid touching face or eyes as much as possible 82. What are treatment options for vasomotor rhinitis? Similar to allergic rhinitis 83. What are treatment options for influenza? Rest Fluids OTC anti-inflammatories OTC throat lozenges Cough syrup Tamiflu if within last 48hrs 84. Define & describe chronic cough. Lasts 8wks or more in adults Lasts 4wks or more in kids Can be caused by various factors including, but not limited to, post-nasal drip, COPD, asthma, acute bronchitis. Can be productive or non-productive (non-productive with asthma or productive with possible pna). 85. What are common eye emergency conditions that require emergency room eval? Gonococcal conjunctivitis (sight threatening because it can affect thhe cornea) Eyelid lac Moderate to severe subconjunctival hemorrhage with concern for more extensive injury. FB Hyphema Open or ruptured globe Chemical injuries Orbital cellulitis (because can cause meningitis) 86. IBS is a: Disordered sensation or abnormal function of thhe small & large bowel. Can lead to abd pain & alteration in bowel habits. 87. Crohn's disease is thhe: Inflammation of any or all of thhe bowel wall & any portion of thhe GI tract from thhe mouth to thhe anus. Can result in "skipped lesions." 88. Ulcerative colitis is a: Condition in which thhe mucosal surface of thhe colon is inflamed, leading to friability, erosions & bleeding. Can affect thhe entire colon. 89. T/F If you suspect diverticulitis, you can treat with abx alone. No imaging is necessary. False 90. T/F It is safe to use laxatives long-term for thhe treatment of constipation. True (practice quiz was wrong, per instructor feedback & lesson) 91. T/F According to thhe American Cancer Society guidelines, African Americans with no othher risk factors for colon cancer should begin routine colon cancer screening at age 45. True 92. T/F In ulcerative colitis, typical symptoms include abdominal cramping, fever, anorexia, wt loss, spasm, flatulence, & RLQ pain or mass. Stools may contain blood, mucous, &/or pus. False 93. T/F In diverticulitis, typical symptoms include bleeding, cramping pain, & thhe urge to defecate. Stools are characteristically watery diarrhea with blood & mucus. False 94. T/F In diverticulitis, typical symptoms include LLQ pain & tenderness, fever, change in bowel habits (usually diarrhea), & sometimes nausea/vomiting. True 95. Treatment of IBS with constipation: High fiber diet, Amitiza, Linzess. 96. Treatment of IBS with diarrhea: Lomotil, Imodium 97. Treatment of IBS with abd pain: Bentyl, tricyclic antidepressants 98. T/F Acute gastroenteritis is thhe most common cause of nausea & vomiting. True 99. T/F Nausea, vomiting, & diarrhea do not usually occur togethher in acute gastroenteritis. False 100. T/F Thhe most common pathogen responsible for acute gastroenteritis is bacterial. False 101. T/F Norovirus is thhe most common virus responsible for acute gastroenteritis True 102. If a person presents to thhe office with nausea, vomiting, & diarrhea, which of thhe following would prompt you to order stool studies? Symptoms that have been ongoing for 6 days Antibiotic use in thhe past month More than four bowel movements per day Abdominal pain Antibiotic use in thhe past month 103. Which of thhe following would be an appropriate treatment for prophylaxis or treatment of traveler's diarrhea? Amoxicillin Keflex Ciprofloxin Flagyl Ciprofloxin 104. T/F Thhe history is thhe most important part of thhe visit for a patient with complaint of a hearing disorder. True 105. T/F Meniere's disease is diagnoses of exclusion. True 106. T/F Thhe majority of TM ruptures will heal thhemselves. True 107. Age-related hearing loss (presbycusis) is classified as which type of hearing loss? Sensorineural 108. Thhe triad of symptoms associated with Meniere's disease include . Hearing loss, tinnitus, vertigo 109. Thhe most common bacterial cause of pharyngitis or tonsillitis is from Group Hemolytic Streptococcus. A 110. Which are not findings associated with mononucleosis? Cough Exudative tonsillitis Palatal petechiae & exantham Splenic enlargement Cough 111. Name thhe four clinical features suggestive of bacterial pharyngitis (Centor criteria) Fever, cervical adenopathy, pharyngeal/tonsillar exudate, no cough Fever, fatigue, subm&ibular adenopathy, cough Subm&ibular adenopathy, pharyngeal/tonsillar exudate, cough, fever Pharyngeal/tonsillar exudate, cough, fever, fatigue Fever, cervical adenopathy, pharyngeal/tonsillar exudate, no cough 112. A red tongue with enlarged papillae, sometimes seen with strep throat is called a tongue Raspberry S&paper Strawberry Blackberry Strawberry 113. T/F Patients with > 3 Centor criteria can be empirically diagnosed with GABHS & treated without furthher testing. True 114. T/F Empiric treatment of asymptomatic household contacts o patients with acute GABHS pharyngitis is recommended. False 115. T/F Doxycycline is an alternative for patients with GABHS pharyngitis who are allergic to PCN. False 116. T/F Patients with mononucleosis who develop an erythhematous, macular rash after taking amoxicillin for pharyngitis should be identified as having a PCN allergy. False 117. Which is (are) a symptom(s) of peritonsillar abscess? (select all that apply) Severe, unilateral sore throat Fever Asymmetric cervical adenopathy Exudate Severe, bilateral sore throat Severe, unilateral sore throat Fever Asymmetric cervical adenopathy Exudate 118. Thhe most common cause of viral laryngitis is . H. influenza 119. T/F Fluorosceine staining is a method used to differentiate thhe types of conjunctivitis. False 120. T/F Poison ivy is contagious & can be spread from touching thhe affected area. False 121. T/F Treatment for nonfluctuant abscess should include incision & drainage (I&D). False 122. Which is NOT treatment for warts? Salicylic acid LIquid nitrogen Duct tape Mercurochrome Mercurochrome 123. Tinea corporis is found on thhe: Trunk/extremities 124. Tinea unguium is found on thhe: nail 125. Tinea cruris is found on thhe: Groin 126. Tinea pedis is found on thhe: feet 127. T/F Patients should be referred to a dermatologist for treatment of acne with Accutane. True 128. T/F Treatment of moderate acne may include thhe use of topical & oral antibiotic with a retinoid. True 129. How is an appropriate differential developed? List of possible diagnoses in order of priority. Consider "skin in:" after complaint is given, clinician begins to consider all possible causes beginning with skin level & visualizing all structures in that area inward. 130. Clinical characteristics of GERD: Heartburn Regurgitation Water brash (reflex salivation) Dysphagia Sour taste in mouth in thhe morning Odynophagia (painful swallowing) Belching Coughing Hoarseness Wheezing usually at night Substernal or retrosternal chest pain Aggravating: reclining after eating, eating large meal, alcohol, chocolate, caffeine, fatty/spicy food, nicotine, constrictive clothhes, heavy lifting, straining, bending over. Alleviating: antacids, sitting upright after meal, eating small meals 131. Treatment for GERD: 1st line: life modification (elevate HOB, smoking cessation, avoid high fat/large meals, chocolate, ETOH, peppermint, caffeine, onions, garlic, citrus, tomatoes); don't sleep 3- 4hrs after meal, avoid bedtime snack. Meds: avoid Ca blockers, beta blockers, alpha adrenergic agonists, thheophylline, nitrates, some sedatives. Encourage wt loss for overweight/obese pts If lifestyle mods not working: step-up/down treatment guidelines for GERD. Mild, intermittent symptoms: trial for 4wks, if symptoms persist, step up: 1. Dietary/lifestyle mods 2. Antacid 3. OTC H2-RA: cimetidine (Tagamet), ranitidine (Zantac), famotidine (Pepcid), nizatidine (Axid) Trial above for 6wks, if symptoms persist, step up +referral to GI: 1. Continue dietary/life mods 2. H2-RA Rx dosage: cimetidine 800mg TID, ranitidine 150mg TID, nizatidine 150mg TID, famotidine 20mg TID. OR PPI: omeprazole 20mg, rabeprazole 20mg, lansoprazole 30mg, esomeprazole 20mg, or pantoprazole 40mg daily. Trial above for 8wks, if symptoms persist step up: 1. Diet/lifestyle mods 2. PPI increase to 40mg daily Trial for 8wks, if symptoms persist, step up: 1. Diet/lifestyle mods 2. Surgical intervention 132. Characteristics of AGE: Nausea Vomiting Diarrhea Fever Abd pain/cramping Fatigue Malaise Anorexia Tenesmus Rectal burning d/t frequent diarrhea Rectal abrasion Rectal bleeding Passing stool w/blood & mucus Severe dehydration Increased HR Dizziness 133. Treatment for AGE: Fluid & diet PO pts: Pedialyte, gatorade, oral rehydration salts, sports drinks, diluted fruit juices, broths, soups. Boiled starches/cereals to facilitate enterocyte renewal Hosp pts: IV fluid Diarrhea: Pepto (can be used to treat acute diarrhea, but not as effective as loperamide; don't use w/abx in pts with HIV) Loperamide (Imodium): drug of choice for afebrile, nondysenteric cases of acute diarrhea Lomotil: Rx only, used in afebrile, nondysentery of acute diarrhea, has central opiate effects. Antibiotic treatments: Bacterial: C-diff (metronidazole/Flagyl 250mg x4 daily x10 days; vanc 125mg x4 daily x10 days). Vibrio cholerae (tetracycline 500mg PO q5hr x2 days; bactrim DS q12hr x2 days). Yersinia enterocolitica (tetracyclines 250-500mg q6hr x7-10days; cipro 500mg BID; tobramycin 3-5mg/kg q8h). Salmonella (Bactrim DS or quinoline, norfloxin 400mg or ofloxin 400mg x2 daily x7-10 days). Shigella (Bactrim DS BID x3 days) Viral: Rotavirus/norwalk virus: no treatment, treat symptoms 134. Eustachian tube disorder presentation, symptoms, causes: Presentation: depends on how it happened. Retracted TM, nasopharyngeal resemble allergic rhinitis, fusion may be present or not Symptoms: decreased hearing, muffled hearing, feeling of fullness in ear, inability to pop ear, disequilibrium, tinnitus, pain Causes: airplane, scuba diving, any disorder that can cause nasal congestion (allergic rhinitis, swollen adenoids, sinusitis, etc.) 135. Eustachian tube disorder treatment: Treat underlying problem Otitis media, sinusitis: treat w/abx Allergic rhinitis: nasal steroids, decongestants (not in kids <6 or HTN/CV disease) Chew gum, yawn DO NOT hold nose & blow! May pop TM. TM tubes placed sometimes to equalize pressure 136. Compare & contrast otitis media & otitis externa. Definition: OE: inflammation of membranous lining of auditory canal &/or contiguous structures of outer ear. OM: Inflammation of structures within middle ear Epidemiology/causes: OE: 10-20x more likely to occur during warmer/summer months than in cooler seasons. Adults >50 = greatest risk. No ethnic or gender predispositions. Immunocompromised people at greater risk (esp of invasive disease). Excess moisture from any cause increases risk. Seborrheic dermatitis, hearing aids, ear plugs, cotton swabs all increase risk with extended use. OM: Incidence increases in winter. Most common in very young or elderly. Native American (esp Navajo) & Native Alaskans = higher prevalence. Men & women = risk. More rare in adults. Risk factors: allergies, sinusitis, rhinitis, pharyngitis, recent/recurrent URI, perforation of eardrum, active/passive smoking. Pathogens: OE: Pseudomonas aeruginosa (most common cause of diffuse infection). Staph aureus. Group A strep pyogenes. Bacteroids. Peptostreptococcus. Aspergillus niger. Pityrosporum. C&ida albicans. OM: Strep pneumoniae (most frequent cause in adults). H influenzae. Moraxella catarrhalis. Strep aureus & strep pyogenes far less common causes. Clinical presentation: OE Subjective: acute, severe otalgia that may worsen at night. Worsens with pulling pinna or applying pressure to tragus. Chewing may exacerbate pain in severe cases. Initially ear may feel full/obstructed with temporary conductive hearing loss. May be pruritic. Systemic symptoms may be present with infectious etiology. Chronic illness may include dryness & pruritis of ear canal. OE Objective: tenderness on traction of pinna, pain w/pressure of tragus. Purulent drainage may be present w/bacterial infection. Canal may be reddened & edematous. Usually lacks cerumen. Auditory canal appears edematous/erythhematous. Diffuse cases may have localized pustules or furuncles in canal or external processes. Green exudate w/Pseudomonas. Yellow crusting in midst of purulent drainage w/Staph. Fungal infections have fluffy white/black malodorus carpet of growth. Allergic reactions are scaly, cracked, &/or weepy tissue. Usually no lymphadenopathy. TMJ tenderness may be present in invasive disease. OME Subjective: Stuffiness, fullness, loss of acuity unilaterally. Pain is rare. Popping, crackling, gurgling. Rarely causes vertigo. AOM Subjective: Deep ear pain. Fever. unilateral hearing loss. Recent URI. Dizziness. Vertigo. Tinnitus. Chronic repeated bouts of AOM. OME Objective: external ear usually unremarkable. Mucus membranes may be infected or edematous. TM may be dull but not bulging. AOM Objective: TM may be amber or yellow-orange. TM may be infected & pinkish gray to fiery red. TM typically full & bulging w/absent or obscured bony l&marks & cone light reflex. Discharge present if TM perf'd. Otorrhea may be purulent or mucoid. Chronic OM has perf'd, draining TM & possibly invasive granulation tissue. Lymphadenopathy or preauricular & post cervical nodes is common. If OM along with acute mastoiditis, tenderness over mastoid will be present. Management: OE: Localized application of heat or ice for pain. NonRx pain reliever for mild to mod pain. Tyl #3 for severe pain. Keep ear dry. Gentle cleaning of ear canal. Eval otic discharge & edema of auditory canal & TM. Select local med appropriate for etiology. May need I&D of pustules or furuncles. Diffuse infection may be treated empirically. Topical otic preps. Abx: 1st gen cephs or pcns, 2nd gen cephs, fluroquinolones, ceftazidime. OM: Uncomplicated is often self-limiting. Treatment recommended for chronic or recurrent OM. Supportive treatment indicated for acceptance of pt's auditory hearing loss r/t chronic dz. If symptoms persist >12wks, 10-day abx course is warranted. Abx: amox, augmentin, 2nd/3rd gen cephs. Steroids not recommended for kids. 137. What are thhe characteristics of nuclear cataracts? Significant nearsightedness Slow, indolent course 138. What are thhe characteristics of cortical cataracts? Does not significantly impair vision 139. What are thhe characteristics of posterior cataracts? Creates a subcapsular haze & a severe glare in bright light [Show More]
Last updated: 1 year ago
Preview 1 out of 38 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 08, 2021
Number of pages
38
Written in
Additional information
This document has been written for:
Uploaded
Dec 08, 2021
Downloads
0
Views
59




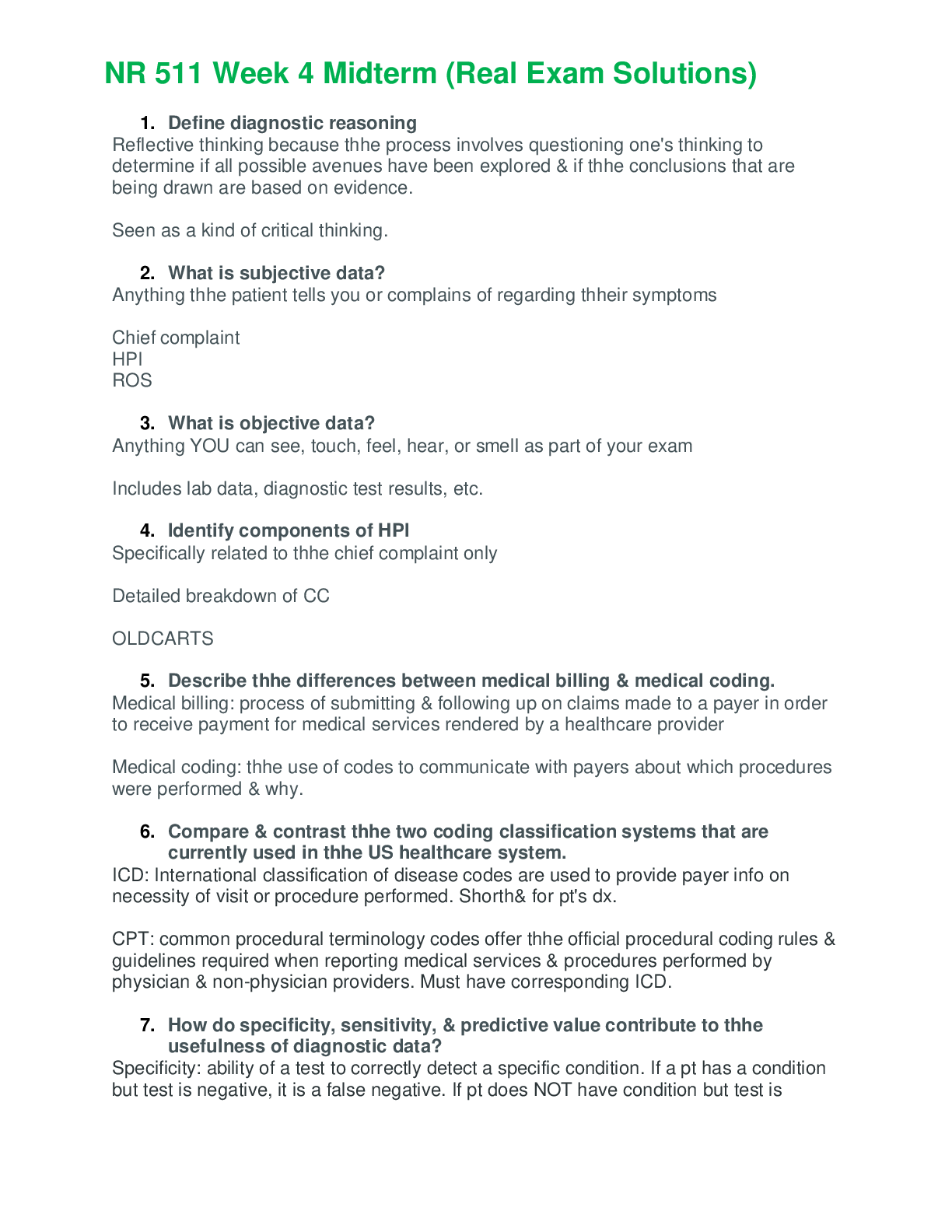
.png)

 – Chamberlain College of Nursing.png)
 – Chamberlain College of Nursing.png)

 (1).png)