*NURSING > STUDY GUIDE > NR 222 Week 8 Final Exam Study Guide | 100% GUARANTEED ACE. (All)
NR 222 Week 8 Final Exam Study Guide | 100% GUARANTEED ACE.
Document Content and Description Below
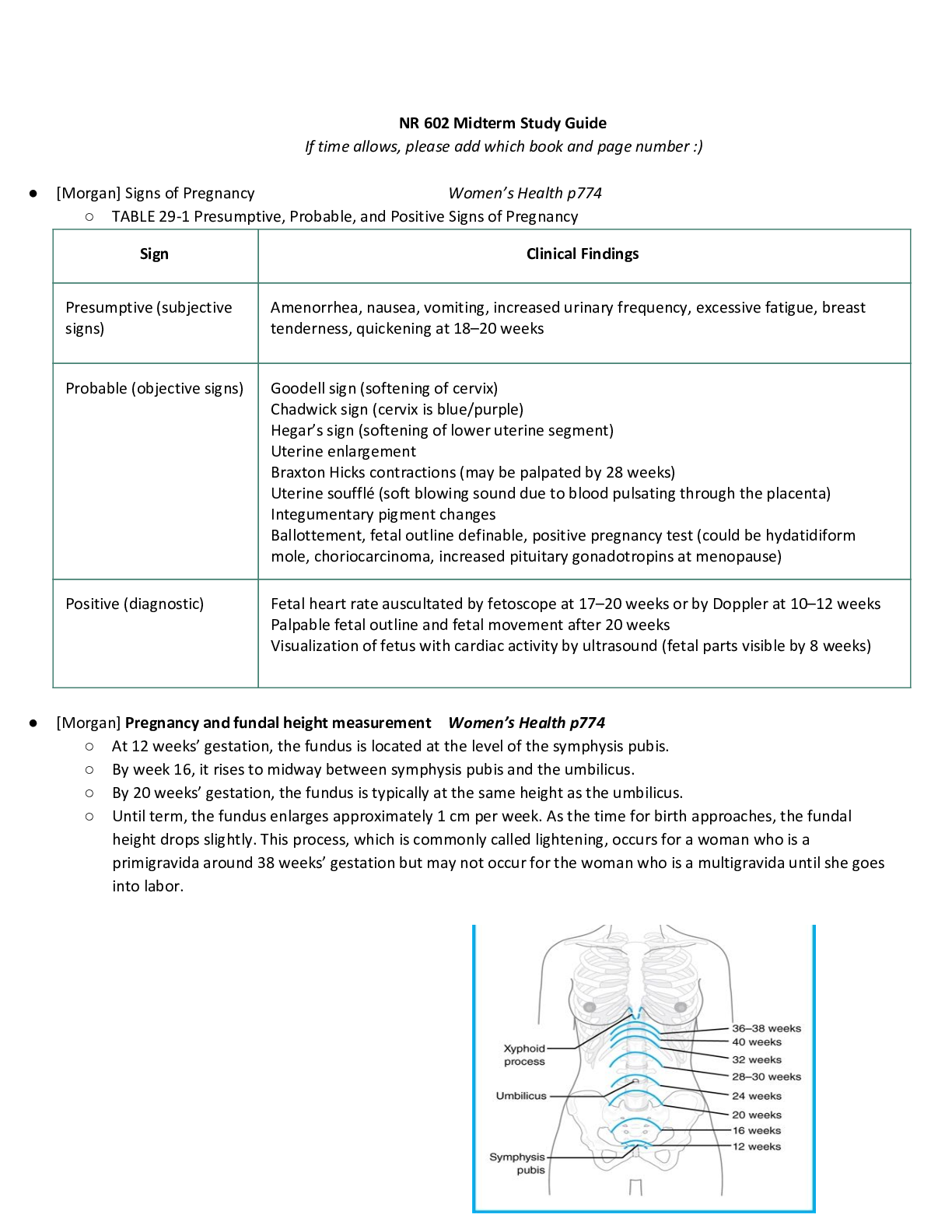
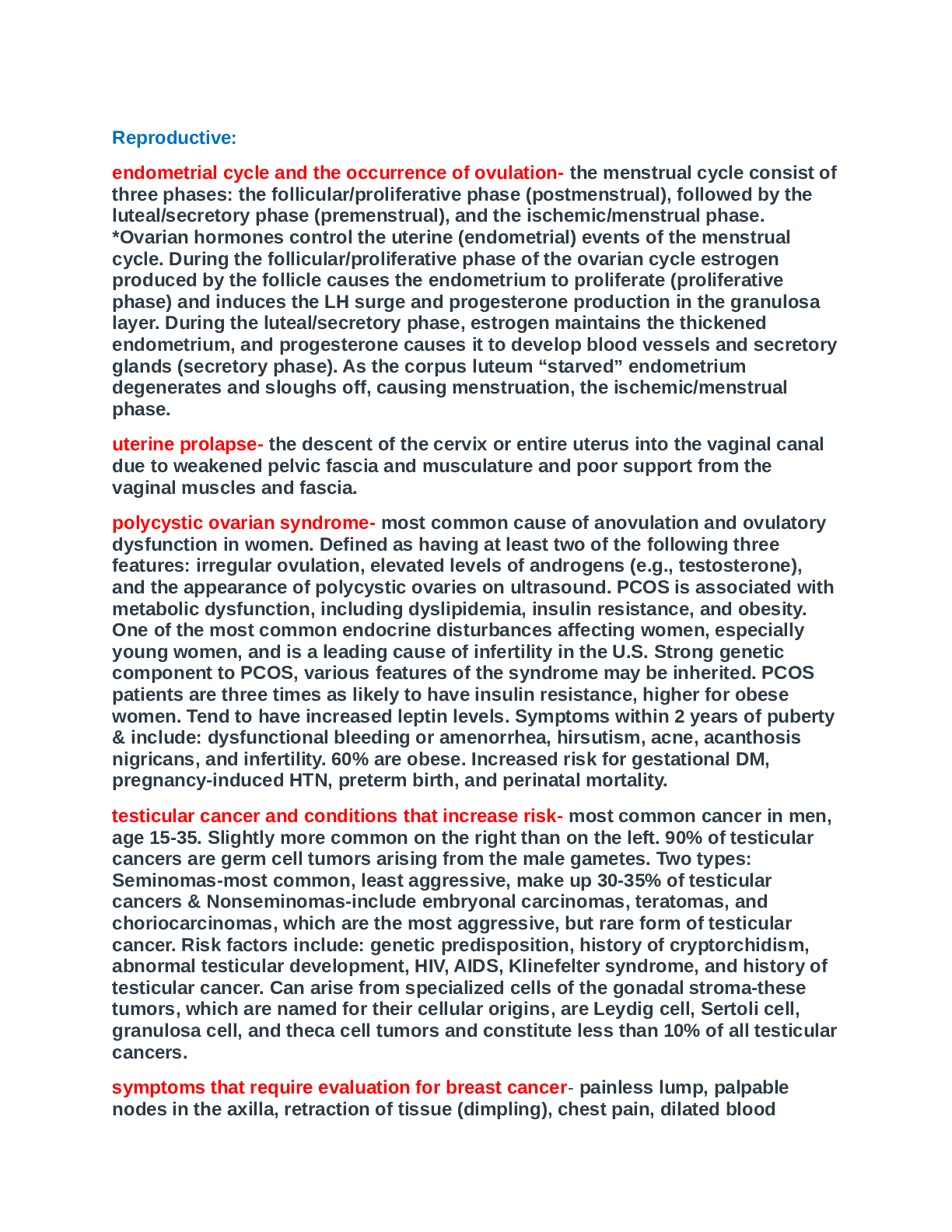
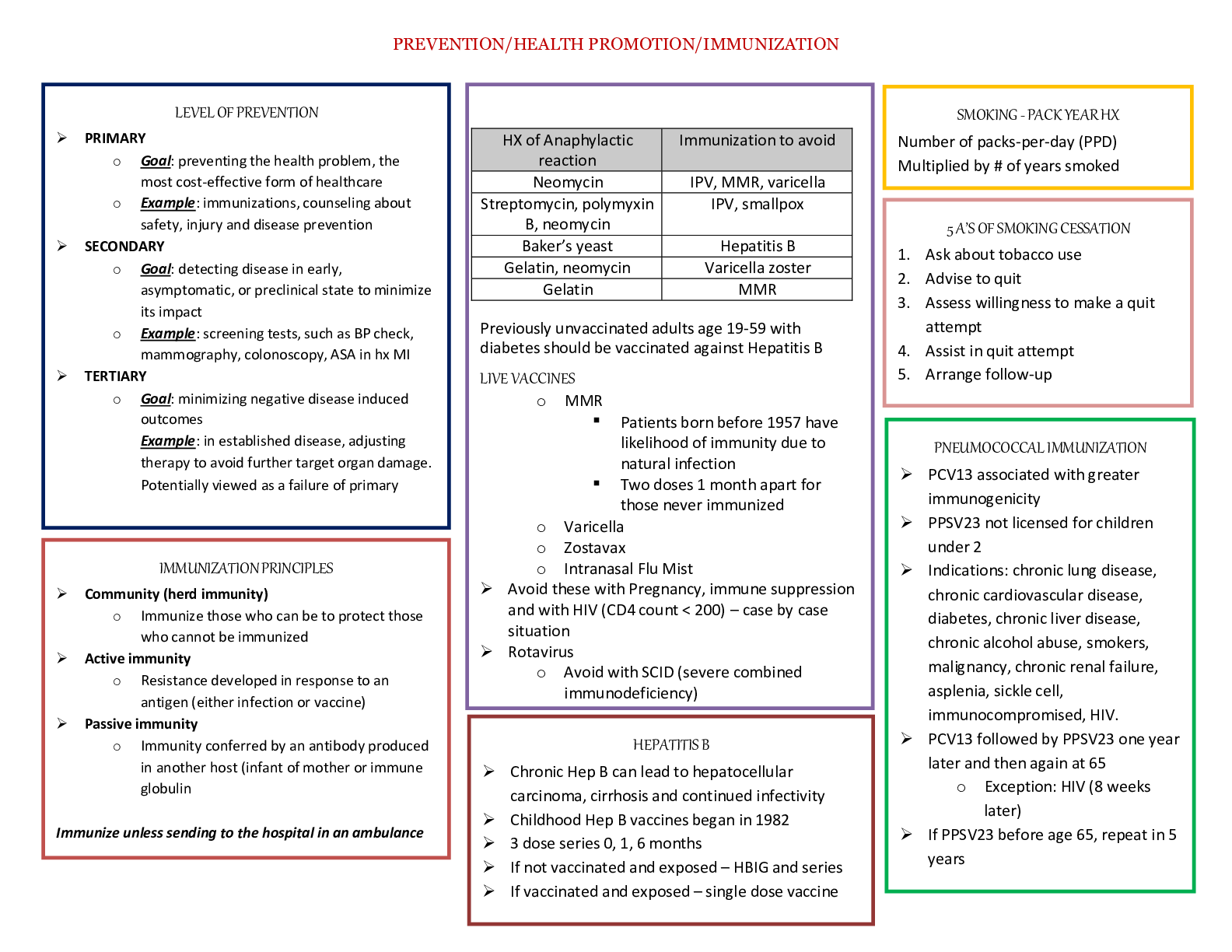
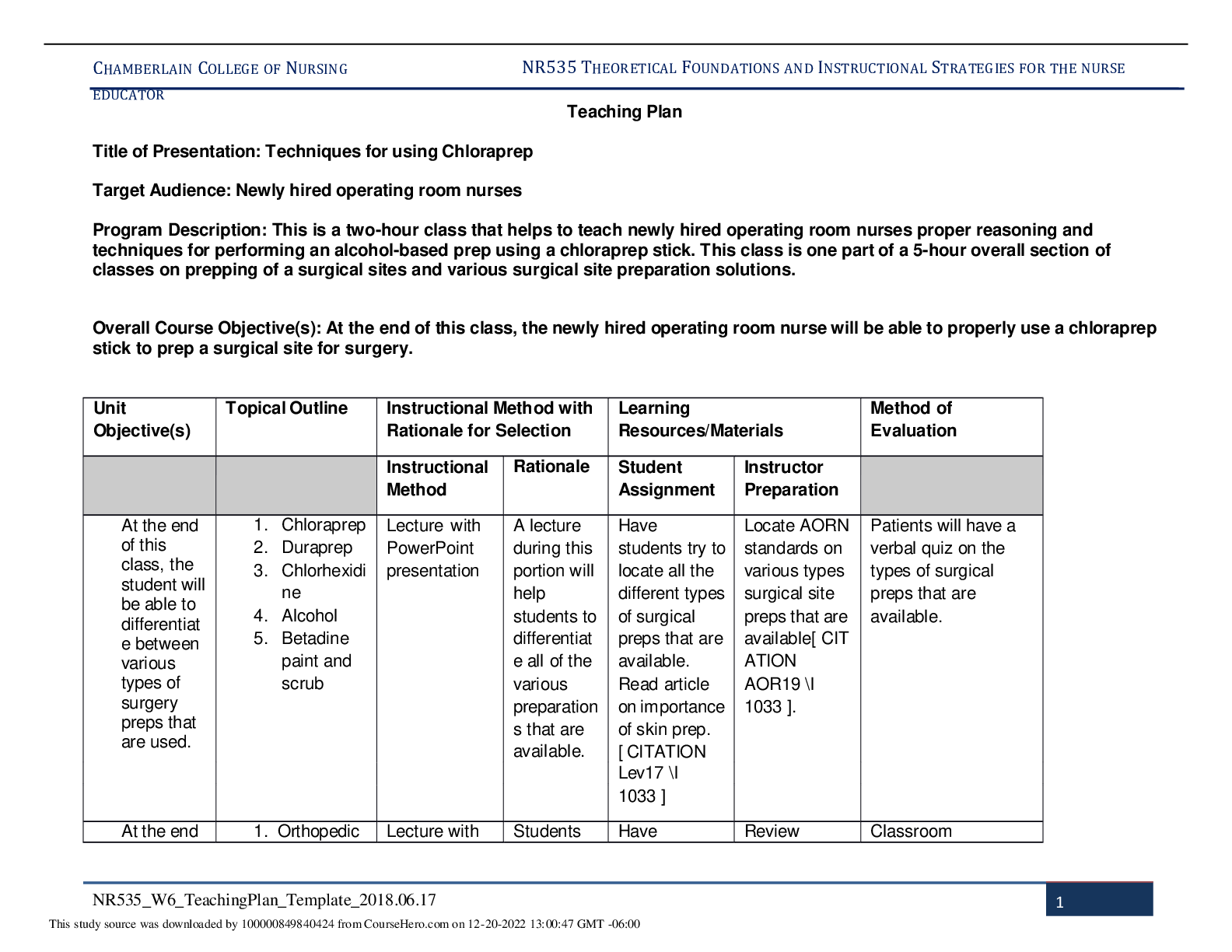
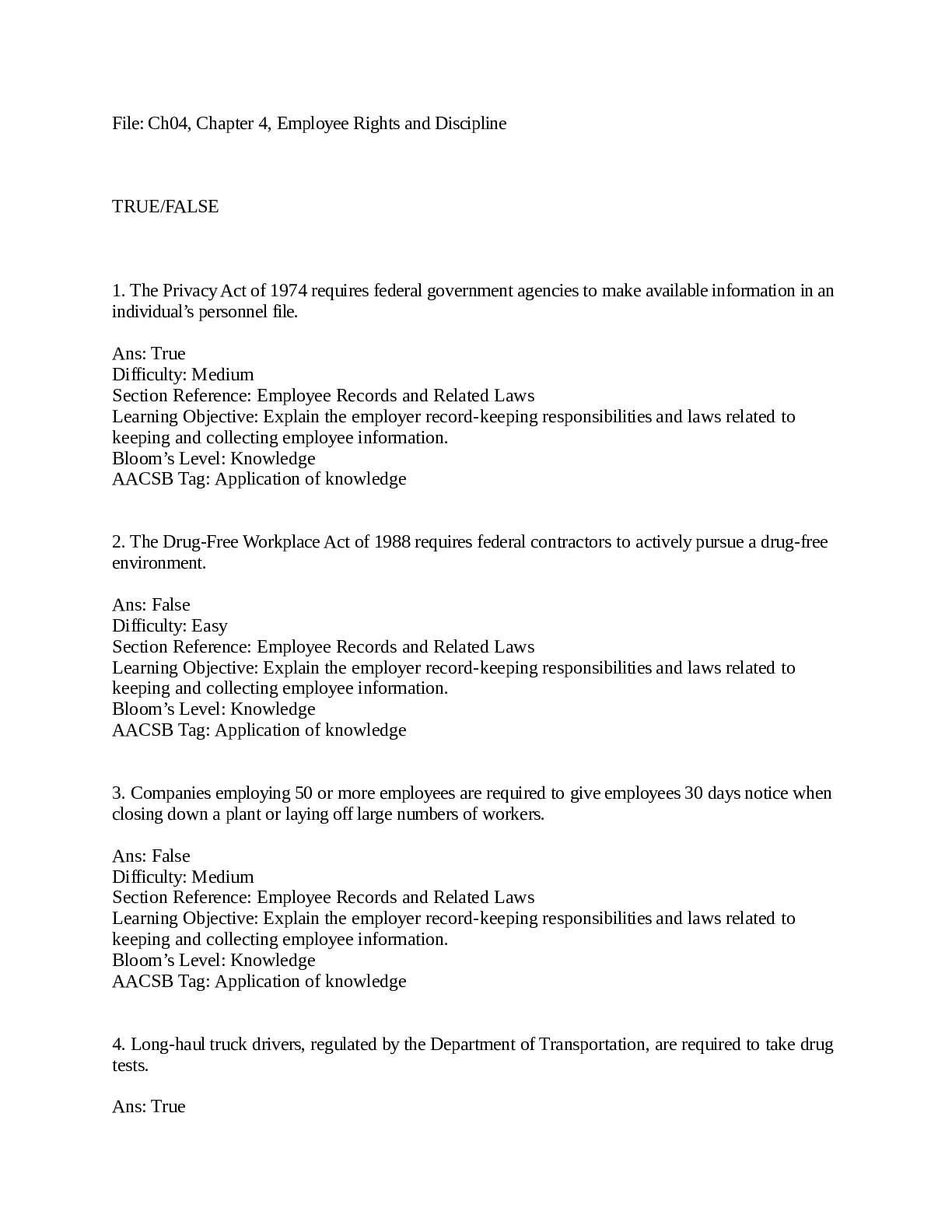
NR 222 Health and Wellness Study Guide Final NR 222 Models of Health: Clinical: • Defined by the absence of illness, signs, and symptoms of disease. • May not seek preventative care or ser... vices. • People who use this model may not seek preventive health services or they may wait until they are very ill to seek care. • You go to the hospital if you need immediate help (such as a broken something not a cold you caught). Role Performance945, with performance based on societal expectations. • Illness would be the failure to perform roles at the ////////////////////////////////////////////////////////////////////////////level of others in society. o EX: If you are sick, you get medicine to help you get back up and running Adaptive: • The ability to adjust positively to social, mental, and physiological change • Illness occurs when the person is unable to adapt o Go through a traumatic injury and then you get help with adapting to a new injury (takes a slow process). Eudemonistic: • Emphasizes the interactions between physical, social, psychological, and spiritual aspects of life • Goal attainment and meaning • May seek out alternative therapies, council of priest, rabbi, or minister • Strive for equilibrium o A person dying of cancer may still be healthy if that person is finding meaning in life at this stage of development. Reasons why the Eudemonistic model is a better, more cost effective model to use today? • This was adopted by the healthcare system because it pays the hospitals, doctors, etc more money because people only come when they are in dire need of medical care thus needing more tests, medicine, procedures done to them and since every little thing costs money the hospital or facility gets paid either from the patient or insurance company. It is more expensive for the patient. Also it was adopted because people think they are healthy or they do not have enough money to go to the doctor for every little thing that happens to them. Why the Affordable Care Act can move America towards a Eudemonistic model? • This model is better because you are focusing on your health as a whole and emphasizes the interactions within social, spiritual, physical, and psychological aspects of life. You seek out alternative therapies such as ministers, rabbis, etc. It is a more holistic approach to medicine and therefore costs less since you are using different types of holistic treatments instead of the big medications from the big pharmaceutical companies. They don't let their illness slow them down. Healthy People 2020: What are the Overarching goals? 1. Attain high-quality, longer lives free of preventable disease, disability, injury, and premature death. 2. Achieve health equity, eliminate disparities, and improve the health of all groups. 3. Create social and physical environments that promote good health for all. 4. Promote quality of life, health development, and healthy behaviors across all life stages What is the differences from Healthy People 2010? • Healthy people 2010 had only two goals. Healthy 2010 is very vague. In Healthy People 2010, it was to eliminate, not just reduce, health disparities. In Healthy People 2020, that goal was expanded even further: to achieve health equity, eliminate disparities, and improve the health of all groups. Define these terms and give two examples of each: Primary Prevention • Health promotion Specific Protection • Catch it before it starts and make people aware of it. o Examples: Periodic examinations, massive immunizations, nutritional awareness and practice, exercise, safety precautions at workplace. Secondary Prevention: • Early Diagnosis, Prompt Treatment, and Disability limitation • Screenings (MRI, BP measurement, Dental Examinations, mammographs, diagnostic tests, HIV testing) Tertiary Prevention: • Restoration= highest level of functioning possible despite the limitation caused by injury. • Rehabilitation o Rehabilitative care, hospice, outreach programs, palliative care • Goal: prevent further disabilities or deduced functioning when possible Define these terms and give an example related to nursing for each: Fidelity • Agreement to keep a promise • Nurses need to follow through actions and interventions • Unwilling to abandon patients regardless of circumstances o Even though you promised and cannot make it send someone else to do it Non-maleficence • Avoiding of harm • Healthcare professionals try to balance risks and benefits of care while striving at the same time to do the least harm o Ex: stopping a medication that would not benefit the patient Autonomy • The right of independence- making decisions for themselves • Right to say no • Include patients in decisions • Providers need to inform patients about risks and benefits of treatment plans • Ensure that patient understands and agree to treatment • Always take the time to explain to patient what you are doing o Ex: Letting the patient go home even though it is against orders. Justice • Fairness • Often used in discussing about healthcare resources, including distribution of scarce resources o Examples: health insurance, hospital locations and services be fair with all of the patients, have no favorites Veracity • Devotion to the truth • People whose health is in question are to various degrees reliant on the person who possesses the knowledge and skills to bring these to bear on their behalf. o Ex: Always being straight up with the patient and telling the truth. Beneficence • Best interest for the patient and NOT self interest • Positive actions for others Understand the difference between these three types of insurance and how people gain access to these health insurances in the Private Sector: HMO • Deliver comprehensive health maintenance and treatment services to a group of enrolled individuals who prepay a fixed fee. • The employer pays a monthly or annual rate directly to the HMO. • The individual may also have out-of-pocket expenses such as copayments. • Go to primary doctor and get a referral for a specialty doctor • Can’t go to doctors outside HMO physicians PPO • Contracted providers provide services for discounted price • Additional costs if a provider outside the PPO is used. • To control costs, the provider must receive preauthorization from the PPO for a member to be hospitalized or for some procedures or tests, and second opinions are usually required before major procedures or surgical operations are performed. POS • POS plans allow members, for an additional fee and higher copayment, to use providers outside the individual HMO network. IPA • Independent physicians in solo or group practices who provide health care services to members of an HMO • Group practice model: HMO contracts with all physicians and specialists needed by the HMO enrollees, but physicians remain independent. • Some contracts are exclusive, requiring physicians to restrict care to members of an individual HMO, • Other variations allow physicians to care for members outside the HMO. • Network model: HMOs contract with individual physicians and with physician groups for both primary and specialty services. Understand the difference between Medicare and Medicaid: Who gains access? Medicare: -Federal Program -Paid through taxes -For people over 65 -Disabilities -End stage renal failure - Hospice • Part A o Inpatient care in hospitals, skilled nursing facilities home health care, hospice • Part B o Supplementary voluntary coverage o Pays doctor’s visits o Should not have a co-pay • Part D o Pharmaceutical costs ▪ Multiple plans available ▪ Medication is not covered ▪ Need supplemental plans (extra insurance etc. anta Blue cross blue shield) to cover meds. ▪ This company will not move medicate pays for something first • Challenged o Growth in elderly population o Depletion of Medicare resources (trust fund) o Uncovered services (glasses, hearing aids) Medicaid: • Federal +State funds • Cost up to 50% of state budgets • Available o Certain low-income individuals o No age requirements o Families with children: 5-year lifetime limit • Services o Inpatient and outpatient hospital care o Prenatal care o Physicians’ services o Nursing facility services for persons >2 o Family planning services o Rural health clinic services o Laboratory and radiologic tests o Pediatric, FNP, and nurse midwife services o Certain federally qualified ambulatory & health center services o Home health services Definition of the Individual How do you correctly write a nursing diagnosis? What are the three main parts? 1. Problem statement 1. What is the issue/problem with this client (always prioritize. Remember ABCs). Ex. Pain or SOB 2. Based on assessment of client b. Etiology 1. what’s causing/contributing to the client’s problem? Ex. What is causing this problem 2. Determine what the problem is caused by or related to b. Defining Characteristics (AEB) 1. what’s the evidence of the problem? Ex. Patient report or nurses’ assessment. 2. Then state as evidenced by(AEB) the specific facts the evidence is based on b. Risk for as evidenced by (Risk Factors). What makes a goal a SMART goal? S- specific M-measurable A-attainable R-relevant T-time bound Transtheoretical Model of Change o Precontemplation ▪ Research stage, you are thinking about it ▪ Example: Looking for the right nursing schools, you are researching online for the top 5 best schools ▪ Nursing Example: Nurse talks to a patient that comes in with cholesterol o Contemplation ▪ Thinking about it, and then taking the next step ▪ Talk to nursing schools ▪ Nursing Example: Looking at the discharge papers and do more research about the medications and thinking about taking the medication. o Planning or Preparation ▪ Getting all the paperwork, documentation, you are on your ways ▪ Nursing Example: Taking the prescription to the pharmacy o Action ▪ In class and navigating what needs to be done (in regards to school work) ▪ Nursing Example: Taking the prescription o Maintenance ▪ Doing/turning in assignments on time ▪ Reading the book ▪ Nursing Example: Taking the prescription every night before bed and continuing to do so for couple days Screening: Significance • Primary Objective: Detection of a disease in its early stages in order to treat it and deter its progression • Secondary Objective: Reduce cost of disease management by avoiding costly interventions required at later stages • The significance of a disease is the level of priority assigned to the disease or disorder as a public health concern • Determinants of Significance o Quality of Life ▪ Subjective; difficult to estimate o Quantity of Life ▪ Disease-specific mortality rates ▪ Prevalence Rates: Existing Cases (chronic disease) ▪ Incidence Rates: New Cases (acute disease) • Cost to treat Benefits vs. Risk What is the Health Belief Model? • Individual perceptions of readiness for change • The value of health compared to other aspects of living • Perceived susceptibility to a health problem o Don’t understand what is going on and they will continue to do it • Perceived seriousness of the disease level • Risk factors to a disease o What are some of the risk factors of the disease • Perceived benefits of health action • Perceived barriers to promotion action • Example: A person needs to recognize a link for coronary artery disease, a person may not see this as serious and not really care or the opposite, the patients reaction to whether or not he/she sees this disease to be serious will determine what changes they will make or not make to help them. • This model focuses on the relation of perception and compliance with therapy • Between the person belief and health behaviors HIPAA: • Has the privacy rule to set standards for the protection of health information • In practice you cannot share information about a patient's medical condition or personal information to anyone not involved in the care of the patient. Roles of the Nurse: Advocate • Be the voice for the patience • Know the patient’s rights o Get what they are entitled to in health care • Make sure system is responsible for patient and community needs • Help people develop advocating skills • Everyone receives high quality care, cost efficient appropriate care Care manager • Looking at all aspects and pulling it all together for the Pt. • Safety and reduce cost • Maintain quality Consultant • Provide knowledge for health promotions and disease preventions • Providing more education to the PT • Some nurses may specialize in areas Deliverer of services • Direct service such as o Health education o Influenza vaccinations o Counselling in health promotions • Home/Health nursing Educator • Teaching patient about diagnosis • To teach effectively nurses must know facts about how people learn and teaching process Healer • Emotional support • Help individuals integrate and balance the various parts of their lives • Ability to look at the individuals inside to sense what is important to the patient and add specific care to help that patient Researcher • Evidence based practice • Looking for a better way to do something. Evidence based practice Adult learning Principles. How do adults learn? • Adults are internally motivated and self-directed • Adults bring life experiences and knowledge to learning experiences • Adults are goal oriented • Adults are relevancy oriented • Adults are practical • Adult learners like to be respected Three domains of learning 1. Cognitive 1. Development of new facts or concepts b. Psychomotor 1. Developing physical skills from simple to complex actions a. Affective 1. Recognition of values, religious and spiritual beliefs, family interaction patterns and relationships Code of Ethics Provisions 8.3: Obligations • Nurses work with others to change unjust structures and processes that affect both the individuals and communities • Nurses educate the public o Facilitate informed choices o Identify conditions and circumstances that contribute to the illness o Injury and disease o Foster healthy lifestyles o Participate in institutional and legislative effort of protecting and promoting health • Nurses address barriers to health • Nurses must collaborate to create a moral milieu that is sensitive to diverse cultural values and practices Standards of Practice Standard 8 Culturally Congruent Practice Therapeutic Relationships Types of communication • Verbal Communication o Vocabulary o Pacing o Clarity/Brevity (length of time) o Timing/Relevance • Nonverbal Communication o Personal appearance o Posture o Facial Expression o Eye Contact o Gestures Mechanisms of Communication • Intrapersonal o Occurs within an individual • Interpersonal o One-to-one interaction between two people • Public o Interaction with an audience • Electronic o EMR (emails, social media) • Small Group o Interactions with a small number of people • Transpersonal o Interaction within a person’s spiritual domain Barriers to communication • Transference o Client comparing you somehow to something from the past • Countertransference o “You remind me of my 16 year old daughter” Therapeutic Communication Techniques • DON'T SAY “I’M SORRY” • Using touch o Careful if its a rape victim, sociocultural • Using silence o Silence = GOLDEN(and if you don't know) • Providing information o ALWAYS telling them what’s next • Clarifying o Saying it differently if they don't understand the first time (most effective) • NEVERsay.. (in fact, always restate what they’re thinking in a better way) o “Why..” o “I know exactly how you feel..” o “You should..” o “Am I gonna die?” Therapeutic Strategies/Relationship phases 1. Pre-interaction 1. Occurs before meeting the patient 1. Look at the room, medications, charts, available data, medical and nursing history b. Orientation 1. When the nurse and the patient meet and get to know each other 1. Should have some information about them at this time 2. Introduction 3. Prioritize the patient's problems and identify his or her goals. 4. Assess the patient's health status. 5. Let the patient know when to expect the relationship to be terminated. 6. Form contracts with the patient that specify who will do what. a. Working i. When the nurse and the patient work together to solve problems and accomplish goals 1. Encourage and help the patient express feelings about his or her health. 2. Encourage and help the patient with self-exploration. 3. Provide information needed to understand and change behavior. 4. Encourage and help the patient set goals. 5. Take action to meet the goals set with the patient. 6. Use therapeutic communication skills to facilitate successful interactions. 7. Use appropriate self-disclosure and confrontation. a. Termination i. Occurs at the end of a relationship 1. Did you achieve the goals or outcomes Nontherapeutic Communication Techniques • Giving personal opinions o Because no one really cares • Changing the subject • Automatic responses o Patient: “I’m gonna be alright” o You: “Yeah!” • False reassurance (stay away from!!) o “Looking at your labs/results..” o Get a physician if you don’t know (play it safe) • Defensive responses o “I’m coming chill” Stages of Communication SOLAR • S: Sit facing the patient o Getting on their level • O: Observe an open posture o EX: “Tell me what’s wrong” • L: Lean toward patient • E: Establish/maintain eye contact • R: Relax Emerging Populations and Health Identify the emerging populations in the United States. • Asian Americans/Pacific Islanders • Blacks/African Americans • Latinos/Hispanic Americans • Native Americans • Arab Americans • Homeless persons • Persons with HIV/AIDS Identify health care issues/disparities specific to each population • Asian Americans/Pacific Islanders o Health Issues ▪ Hesitancy to seek early diagnosis/screening ▪ Higher rate of tuberculosis (closer proximity) ▪ Mental health problems due to adjustments issues ▪ Lower rate of obesity, hypertension o Barriers ▪ Poverty ▪ Stress in intergenerational relationships ▪ Cultural norms that prevent health care seeking ▪ Loss of social networking ▪ Poor access to services • Blacks/African Americans o Health Issue ▪ Higher cancer deaths ▪ HIV(drug abuse) ▪ Hypertension ▪ Obesity ▪ Mental health concerns o Barriers ▪ Poverty ▪ Lack of health insurance ▪ Inadequate or unsafe environments • Latinos/Hispanic Americans o Health Issues ▪ Stomach cancer ▪ Diabetes mellitus ▪ Cardiovascular disease ▪ HIV(higher LGBTQ) o Barriers ▪ Highest uninsured rate of any U.S. racial/ethnic group ▪ Use/receive less preventative health care ▪ Lack of interpreter services in health care ▪ Lack culturally appropriate health care services ▪ Reliance on folk systems of healing • Native Americans o Health Issues ▪ Linked to social and economic conditions ▪ Smoking, substance abuse ▪ Deaths: unintentional injuries, cirrhosis, homicide, suicide, pneumonia, diabetes o Barriers ▪ Difficult access to care ▪ Underserved population • Arab Americans o Health Issues ▪ Adult-Onset Diabetes Mellitus ▪ Coronary artery disease ▪ Roles of acculturation- hard assimilating to the US ▪ Mental health ▪ Teenage smoking o Barriers ▪ Religious belief and practices ▪ Cultural norm/modesty ▪ Gender issues regarding providers ▪ Communication difficulty ▪ Folk remedies ▪ Lack of cultural competent providers • Homeless persons o Health Issues ▪ Exposure to extreme temperatures, unsanitary living conditions, crowded shelters, poor nutrition ▪ Lack of healthcare access ▪ Lack of preventative care ▪ Mental health ▪ Substance abuse ▪ STIs o Individual Causes ▪ Child and adult victimization ▪ Mental illness ▪ Substance Abuse ▪ Low levels of education ▪ Poor or no work history ▪ Too early childbearing ▪ Fastest growing population = families with children • Persons with HIV/AIDS Specific Emerging Populations Define cultural competence and explain its role in health promotion. 1. Respecting patient’s health beliefs and understanding the effect of beliefs on care delivery 2. Shifting a model of understanding a patient’s experience from a disease happening in the patient’s organ systems to that of an illness occurring in the context of culture 3. Ability to elicit a patient’s explanation of an illness and its causes 4. Ability to explain to a patient the HC provider’s perspective on the illness and its perceived causes 5. Being able to negotiate a mutually agreeable, safe, and effective treatment plan • Culture may have impact on people’s o Health o Healing o Wellness belief systems o Perceived causes of illness and disease o Behaviors of seeking health care o Attitudes towards health care providers. Describe the nursing profession’s response to health disparities. Voluntary • Immigrants come for positive experience • Quest of the individual of group for one or more goals o Education o Economic o Social improvements o Political or Religious freedom Involuntary Migration • Fleeing or being forced out of homeland • Natural disasters • Indentured Servitude • Refugees Folk healing • Reflect beliefs, values, treatment of cultural group Culturally congruent care • Transcultural nursing o A comparative study of cultures to understand their similarities and differences · Culturally congruent care o Care that fits a person’s life patterns, values and system of meaning Diversity and Health Teaching • Eliminating disparities in health require that nurses provide culturally appropriate health education and health promotion. • Prevention strategies must be culturally and linguistically appropriate in order to be effective. • The nurse endeavors to provide culturally sensitive education. • Make an effort to analyze educational interventions that are acceptable and satisfying to the individual Care of the Family Family structure • Family composition including roles/relationship o a family member may have a relationship with a spouse, child, employer, and work colleagues. ▪ Each relationship has different demand and roles ▪ Multiple relationship and expectation often the source of stress • Rigid structures specifically dictate who accomplishes different tasks and also limit the number of people outside the immediate family allowed to assume these tasks. o Mother = only acceptable to provide person will emotional support and do household chores o Father = only acceptable to financial support and do yard Health considerations Advantages and disadvantages of screening • Advantage o The simplicity of some screening procedures decreases the time and cost of the health care personnel involved, especially when compared with the cost of treating the disease after symptoms appear, and enables less skilled technicians to administer the test. o Apply the screening process to both individuals and larger populations. ▪ Individual:one person is tested by a health professional who has selected the individual as high risk (such as prior hypertension). ▪ Group: a target population is selected on the basis of an increased incidence of a condition or a recognized element of high risk within an identified group. ▪ For example, the target population may be invited to a central location on a designated day to be tested for the selected disorders (elevated levels of lipids and cholesterol, hypertension, osteoporosis, elevated blood glucose level) • Ability to provide one-test disease- specific screening or multiple test screenings. ▪ is the administration of a single test that searches for a characteristic that indicates a high risk of developing a disorder. ▪ An example of this would be blood pressure screening to evaluate hypertension • Creates an opportunity for providing health education • Disadvantage o Uncertainties in scientific evidence, which sets normal testing ranges and therefore also ranges of error for screening tests. ▪ False positives ▪ False negative Family Violence • The intentional intimidation, abuse, or neglect of children, adults, or elders by a family member, intimate partner, or caretaker in order to gain power and control over the victim. • The use of physical force by one family member against another, with the intent to hurt, injure, or cause death • Emotional, physical, or sexual abuse of one family member by another The Nurse’s Role • Acts as role model • Collaborates with family • Provides information • Assists with decision-making,problem solving • Serves as liaison for services • Report abuse Nursing process and the family as a unit • Assess o Physical surroundings o Unit rituals o Roles o Relationships • Assessment o Factors that may influence o Nurse’s perception of family o Theoretical knowledge o Norms o Standards o Communication ability o Family cooperation o Health-Promotion plans • Analyzing the Data o Presence of risk factors predicts potential dysfunction o Developmental risk and risk arising from dysfunctional health patterns increase whole family risk o Identify an appropriate Family Nursing Diagnosis • Planning, Implementation, Evaluation o Nursing process occurs mutually with families, not for families o Collaborative process o Constantly changing and evolving Wellness practices and Indicators of Healthy families Family Forms • Nuclear Family o The nuclear family consists of a married couple (and perhaps one or more children). • Extended Family o The extended family includes relatives (aunts, uncles, grandparents, and cousins) in addition to the nuclear family. • Single Parent Family o The single-parent family is formed when one parent leaves the nuclear family because of death, divorce, or desertion or when a single person decides to have or adopt a child • Blended Family o The blended family is formed when parents bring unrelated children from prior adoptive or foster parenting relationships into a new, joint living situation. • Alternative Family o Relationships include multi-adult households, “skip-generation” families (grandparents caring for grandchildren), communal groups with children, “nonfamilies” (adults living alone), and cohabitating partners. Care of the Community Structure and Function of a community • Structure: System or subsystem consists of a formal or informal arrangement of parts, including both animate and inanimate properties. o Health agencies, schools, fire departments, and governmental bodies are examples of structural parts. • Function: Process of dynamic change with adaptation in the system’s parts and the ways that community systems and subsystems interact. Community strengths and Health Concerns Community nursing interventions • Promote the health of the population • Develop essential relationships • Supply educational information Overview of Growth and Development Erikson’s Eight Stages of Human Development 1. Infancy to birth (birth to 18 months) • Basic conflict: Trust vs. Mistrust • Important events: feeding • Outcome: Children develop sense of trust when caregivers provide reliability, care, and affection. Lack of this will lead to mistrust 2. Early childhood (2-3 years) • Basic Conflict: Autonomy vs. Shame and Doubt • Important events: Toilet training • Outcome: Children need to develop sense of personal control over physical skills and sense of independence. Success leads to feelings of autonomy and failure leads to feelings of shame and doubt. 3. Preschool (3-5 years) • Basic conflict: Initiative vs. Guilt • Important events: Exploration • Outcome: Children need to start asserting control and power over environment. Success in this stage leads to a sense of purpose. Children who exert too much power experience disapproval and have a sense of guilt 4. School age (6-11 years) • Basic conflict: Industry vs. Inferiority • Important events: School • Outcome: Children need to cope with new social and academic demands. Success leads to sense of competence and failure results in feeling inferior 5. Adolescence (12-18 years) • Basic conflict: Identity vs. Role confusion • Important events: Social relationships • Outcome: Develop sense of self and personal identity. Success leads to ability to stay true to yourself and failure leads to role confusion and weak sense of self 6. Young Adulthood (19-40) • Basic conflict: Intimacy vs. Isolation • Important events: Relationships • Outcome: Need to form intimate, loving, relationships with other people. Success leads to strong relationships and failure results in loneliness and isolation. 7. Middle Adulthood (40-65 years) • Basic conflict: Generativity vs. Stagnation • Important events: Work and Parenthood • Outcome: Need to create or nurture things that will outlast them often by having children. Success leads to feelings of usefulness and accomplishment and failure leads to shallow involvement in the world. 8. Maturity (65 to death) • Basic conflict: Ego integrity vs. Despair • Important events: Reflection on life. • Outcome: Need to look back on life and feel sense of fulfillment. Success leads to feelings of wisdom and failure leads to feelings of regret, bitterness, and despair Piaget’s Stages of Cognitive Development Kohlberg’s theory of Moral Development Stage1:physical aspects (young children) Stage 2: different people have different viewpoints Stage 3: Norm of groups, thinking other people’s account into consideration Stage 4: Wider rules of society Stage 5: individual rights and greater good Stage 6: Own morals = own your actions Infant Identify Key growth and development markers (box 17-2) Anticipatory guidance • The main focus centers on stimulation, because each of the infant’s senses is receptive to environmental stimulation. o This activity helps the infant learn from the environment. • Parents are the primary providers of pleasurable and stimulating experiences for the infant. Immunizations • Birth o Hep B(first dose) • Two months o DTaP (first dose), Hib (first dose), PV (first dose), PCV (first dose), RV (first dose), Hep B(second dose, between 1 and 2 months) • 4 months o DTaP (second dose), Hib (second dose), PV (second dose), PCV (second dose), RV (second dose) • 6 months o DTaP (third dose), Hib (third dose), HepB(third dose), PV (third dose), PCV (third dose), RV (third dose), and influenza vaccine • 12 months o MMR, PCV (fourth dose), Hib (fourth dose), varicella vaccine, HepA (first dose) • 15 months o DTaP (fourth dose) • 18 months o Hep A(second dose) Injuries/Safety guidelines Environmental process • Leading cause of death • Falls (SAFETY, SAFETY, SAFETY) o Most common after 4 months (rolling over) o Do not leave unattended on raised surface o Raise crib rails ▪ Rails should be no more that 2inch o Restrain in high chair o Avoid walkers near stairs o Gate stairs o Safe shoes, pants not touching the floor • Burns o Deaths from smoke/toxic gasses o Install smoke detectors o Check formula & bath temp o Guard fireplace or heater • Swallowing/choking on foreign objects o Potential: any small object in mouth o Childproof environment o Infant CPR: parents & caregivers ▪ Babies respiratory arrest o Inspect toys for small parts o No nuts, seeds, hot dogs o Specific incidentals in age groups Cancer o Leading cause of death from disease o Nurse’s role: Risk-factor identification, screening, assessment, community education Toddler Identify Language, Speech, and Hearing Ability Growth Patterns Environmental Processes • High risk for accidental injury • Structural hazards o Baby-proof” environment o Inspect for hazards in unfamiliar environments o Appropriate supervision • Toys o Inspect toys o Risk of small removable parts, batteries, toxic paint, sharp edges • Sports o Improper storage of guns, heavy equipment o Need for bike helmets • Drowning: Highest risk ages 1 to 3 o Can drown in water if covers nose/mouth o Danger: pools, tubs, toilets, pails of water • Burns o Hot liquids, electrical cords, fireplaces o Lower water heater to 120° to 125° F Poisoning Preschool-School Aged Children Environmental Processes • Drowning o Fewer incidents than younger children; racial differences o Prevention: water safety teaching • Signs of abuse: inconsistent recall of injury between child & caregiver/parent o lack of emotional response from child to playground injury • Burns o House fires (Christmas trees, space heaters) o Prevention: smoke detectors; fire safety practices • Firearms(school age) o Gun accidents; adolescent shootings o Prevention: locked guns, gun safety • Sports and recreation o Risk: musculoskeletal injuries with competitive sports o Playground equipment safety o Prevention: protective devices, hydration, conditioning exercises, match child to activity • Mechanical o Bicycle accidents become a greater source of injury during the preschool years. o Motor vehicle Injury Prevention/Unintentional Injuries • Preschool • Household furniture and fixtures also remain a hazard for preschoolers, as do structural features such as stairs and windows. • Nursery and toy injuries decrease during the preschool years. • Sports and recreational injuries increase markedly. o This elevated incidence likely reflects a change in many preschoolers being involved in group sports, riding bicycles, and using playground equipment • Preschoolers need a broad range of play areas and experiences. Conscientious parents supply age-appropriate limits and supervision. • Preschoolers lack the skill or judgment to ride bicycles in the street. Health Promotion Needs and Risks o Increase risk for cardiovascular diseases, diabetes, sleep apnea o Psychosocial: Ridicule, discrimination Health screening considerations • Health promotion o Nutrition o Sleep o Vision Adolescents Environmental Processes • Accidents o Motor vehicle accidents: 20 times more likely than in other age groups o Inexperience, drugs/ETOH, distracted driving • Sports injuries o Vulnerable: Immature coordination, judgment, musculature, epiphyses o Performance enhancing substances • Violence o Risk from carrying weapons, testing limits, witnessing/observing violence, music lyrics o Unresolved fear: Increase in violent behavior Erikson’s Identity vs Role Confusion Recognition/Assessment of Abuse Patterns • inconsistent recall of injury between child & caregiver/parent Screening and Intervention for the Adolescents Young Adults Health Monitoring Behavioral Health Physical Health Sexually Transmitted Disease recognition/screening Education on Contraceptive Methods Adult Immunization and Communicable diseases Erikson’s Theory Middle Aged Adults Erikson’s Theory Life Expectancy Mortality Rates • Leading causes: Heart disease and cancer • Morbidity and mortality: Influenced by lifestyle behaviors Health Promotion and Disease Prevention Screening Recommendations • Females: o Mammography, clinical breast exam, and SBE o Fecal occult blood and colonoscopy o Pap smear o Alcohol/substance use o BP, Chol,Ht,Wt o Vision and hearing • Males: o Fecal occult blood and colonoscopy o Digital rectal exam o Prostate specific antigen (PSA) o Alcohol/substance use o BP, Chol,Ht,Wt o Vision and hearing Physical System Changes Determinants of Health Nursing Assessment and Application Older Adults Erikson’s Theory Health Promotion/Health Education • Heart disease • Cancer • Chronic lung disease • Stroke • Smoking • Alcohol abuse • Nutrition • Dental problems • Exercise • Falls • Sensory impairments • Pain • Medication use Safety • Safety at home o Modifications and tips for home safety ▪ General ▪ Stair use ▪ Kitchen ▪ Bathroom o Monitoring devices • Medication safety o Extent of medication usage o Polypharmacy ▪ Drug interaction possibilities o Medication guidelines ▪ Medication list • Safety in driving o Ability o Elderly drivers and accidents o Risk factors affecting driving safety Biological and Chemical Agents • Effects of aging o Drug absorption, metabolism, excretion • Side effects of medication • Drug-drug interactions o Good medication history o Start with lowest effective dose • Ability of older adults to self-administer • Medication affordability • Use of illegal drugs Polypharmacy • Go to different doctors and the doctors will prescribe medication without talking to the patients other doctors Long-Term Care Housing/Assessment (Table 24-4) Stress Management Stressors • Any psychological, social, environmental, or physiological or spiritual stimulus that disrupts homeostasis, thereby requiring change • 3 Categories of Stressors o Extrinsic Factors ▪ Out of the individuals control (Death of a spouse, Traffic) o Modifiable Factors ▪ By changing social interactions, behaviors, environment etc. o Intrinsic Factors ▪ Stressors related or exacerbated by individuals response to stress (Poor time management/procrastinating, negative thinking) Assessment of Warning Signs Symptoms of Stress • Headaches • Low energy • Insomnia • Pain/tense muscles • Colds/infections • Headaches o Tension, migraine • Change in appetite o Food cravings o Sweet, salty, fatty Goals • To improve quality of life by increasing healthy, effective coping, thereby reducing unhealthy consequences of distress Sources and Coping Mechanisms • Mind, Body, Spirit, Cognitive/Emotional states and Behavior Consequences of Stress Physiological • Neuroendocrine activation/Behavior changes o Fight-or-flight stress response: Adaptive, acute, short-term • Hypothalamus signals to SNS (sympathetic nervous system): Epi/NorEpi release • Increased Metabolism, PP, BP, RR, Muscle Tension • Maladaptive o Causes or exacerbates disease/symptoms Psychological • Contributory role on negative moods o Anxiety, Depression, Hostility, Anger • Elevated Cortisol levels: (Immune System Response) • Affects outcomes in key populations o EX: Elderly, Terminally Ill, Caregivers, etc ▪ Quality of life ▪ Depressive symptoms ▪ Degree of suffering Sociobehavioral Effects • Stress response: based on individual reliance on less healthy behaviors o Overeating (unhealthy) o alcohol/drugs o Isolation o Smoking o Unhealthy behaviors associated with increased morbidity/mortality Spiritual • Spirituality: “Feelings, thoughts, experiences and behaviours that arise from a search for meaning” o Note: Spirituality and Religion are NOT the same thing • Stress Response o Often feel disconnected from life’s meaning/purpose • Promoting connection with life meaning and purpose: Health Benefit Health Benefits • Promoting stress management is key to disease management and better health outcomes. • “Caregiver stress/ Burden” = Major concern stemming from the taxing nature of being a caregiver o “Sandwich generation” - Those caring for elders/parents while caring/raising children at the same time o BURNOUT is a consequence Stress Management Interventions • Primary Appraisal(positive or negative outcomes. get to the bottom of it) o Perceived actual/potential positive & negative outcomes ▪ Negative Outcomes: Harm (physical injury, disease, death) ▪ Positive Outcomes: Challenges individual perceives can be overcome (graduation, promotion) • Secondary Appraisal(no choice, but to learn to cope) o Individual’s choices to cope with stress o Choices: Internal/external resources/responses Communication and Techniques for Effective management • Self awareness o One of the most effective stress management tools. o Increases sense of control. o Interactions between mind, body and spirit o Monitor stress warning signs/symptoms. o Relaxation Response ▪ Repetition of word/prayer/activity/sound/thought ▪ Passive disregard for everyday thoughts o Mini-Relaxations ▪ Can be used throughout the day ▪ Keep initial stress symptoms from intensifying ▪ Stop and breathe. Slow down. o Expressive writing ▪ Transferring thoughts/emotions into writing (EX: journal, diary etc) ▪ Improves processing and disclosing information ▪ Improves mental and physical health o Healthy Diet ▪ Health, physical performance, state of mind = positive influence ▪ Balance diet (improves functioning) o Physical Activity ▪ Comprehensive wellbeing while decreasing stress o Sleep Hygiene ▪ Altered sleep patterns can result in stress issues ▪ Sleep techniques can improve quality of life ▪ Sleep Deprivation = depression/fatigue o Cognitive Behavioral Restructuring ▪ Modifies negative, exaggerated thoughts ▪ STOP, break the cycle, take a breath (relax), reflect, choose a more different/rational method/approach. o Affirmations ▪ Positive thoughts that are meaningful to a person. o Social Support ▪ Have good relationships with close family, friends, co-workers, professionals, supporters. o Assertive Communications ▪ Non-judgmental, expressive feelings and opinions, reaffirms perceived rights. ▪ Format: “I Feel [Emotion], When you [Behaviour] Because [Explanation]” o Empathy ▪ Considering another person’s perspective & communicate understanding back to them ▪ Reduces emotional arousal, defensive behavior, and conflict o Engaging in Healthy Pleasures ▪ Activities that bring a person happiness/joy/peace o Spiritual Practice ▪ Activities a person finds meaningful, purpose, connection. o Clarifying Values and Beliefs ▪ Identifying what is important/meaningful o Realistic Goals ▪ SMART goals: Help to increase control and reduce stress. o Humor ▪ Laughter: physiological effects similar to exercise ▪ Opens different perspectives on problems (reframes perceptions) Nutrition Counseling for Health Promotion Dietary supplementation • Include vitamins, minerals, herbs, botanicals/plant-derived substances, amino acids, metabolites, constituents, and extracts • Unregulated by FDA: more research needed • Dietary supplementation indicated for specific populations, examples include: o Folic acid, iron during pregnancy o Calcium, vitamin D for elderly • Vitamin Toxicity: Excessive use of supplements o Highest risk: fat-soluble vitamins (A, D, E, K) Folic acid deficiencies • Folic acid intake is particularly important for DNA synthesis and the growth of red blood cells. • Folic Acid is very important for women who are pregnant • Inadequate intake can lead to fetal neural tube defects, anencephaly, or maternal megaloblastic anemia • Women of childbearing age need to consume 400 mcg of folic acid daily, increasing to 600 mcg daily during pregnancy. Ca Deficiencies • Osteoporosis Vitamin Toxicity High Risk Vitamins • Excessive use of supplements Foodborne illness (E COLI vs Salmonella) • E. coli : damages intestines, hemolytic uremic syndrome, avoid undercooked meat, unpasteurized milk, unwashed foods o The illness is characterized by severe abdominal cramping, watery to bloody diarrhea, dehydration, nausea, and vomiting with or without low- grade fever. o Hemorrhagic colitis is usually self-limited and lasts for an average of 8 days. o Are food-borne and associated with undercooked or raw ground beef, unpasteurized fruit juices and milk, alfalfa sprouts, lettuce, spinach, and fruits. o Outbreaks can be caused by secondary person-to-person contamination in homes, day care centers, nursing homes, and hospitals. ▪ Another mode of transmission of E. coli O157:H7 is by hand-to- mouth contact with animals or contaminated surfaces at petting zoos and agricultural fairs. o Children and older adults are more susceptible. • Salmonellosis: o Most reported food born illness o Contamination may also occur from unsanitary handling of foods and utensils by infected food handlers and contact with the feces of some pets, especially those with diarrhea. o Symptoms ▪ Abdominal cramping, mild to severe diarrhea, nausea, vomiting, and fever within 8 to 72 hours after infection. ▪ Symptoms may resolve within 4 to 7 days without treatment ▪ However, infections can become life threatening for people with weakened immune systems such as infants with an immature immune system, young children, pregnant women, older adults, and people with autoimmune disorders or those being treated for cancer. • Prevention: o Avoid uncooked egg dishes, undercooked meat, shellfish, and unpasteurized milk and juice. o Adherence to sanitary regulations, as well as proper food handling Food Safety Practices • Clean: o Wash hands, utensils, and cutting boards before and after contact with raw meat, poultry, seafood, and eggs o Wash all parts of the hands thoroughly with running warm water with soap and friction for approximately 20 to 30 seconds. o Clean all surfaces with warm, soapy water often (including all appliances, knobs, and handles) and clean up spills immediately. o At least once a week, discard refrigerated foods that should no longer be eaten. ▪ Cooked leftovers should be discarded after 4 days; raw poultry and ground meats should be discarded after 1 to 2 days • Separate o Do not cross-contaminate. ▪ Keep raw meat and poultry separated from foods that will not be cooked while shopping, preparing, or storing foods o Rinse fresh fruits and vegetables thoroughly with running water before eating, cutting, or cooking them • Cook o Cook food to the proper temperatures and use a food thermometer. • Chill o Refrigerate food promptly within 2 hours, or in 1 hour for environments that are 90°F or hotter. ▪ This includes groceries, food being prepared, and leftovers and takeout foods. ▪ Keep the refrigerator at 40°F or less and the freezer at 0°F or less and monitor temperatures with a thermometer. o Danger zone 33°F -140°F ▪ Harmful bacteria can grow rapidly o Thaw food properly to avoid any bad bacteria ▪ In the refrigerator; in cold water, such as in a leak-proof bag ▪ Changing the water for cold water every 30 minutes ▪ or in the microwave oven, never on the countertop. • Risk: Greatest in persons without mature, healthy immune systems • Food contaminants may be categorized as biological, chemical, or physical. o Biological contaminants include bacteria, viruses, parasites, and fungi (yeasts and molds). o Chemical contamination refers to the presence of pesticides, kitchen- cleaning supplies, and toxic chemicals in food that have been leached from worn metal cookware and equipment. o Physical contamination includes dirt, glass chips, crockery, wood, splinters, stones, hair, jewelry, and metal shavings from dull can openers. ▪ Another unintended physical contaminant may be an unintended allergen added to a food product that typically does not include that ingredient (such as peanuts) during food processing in the same location. Nutrition Screening Risk factors • Discover characteristics or risk factors associated with dietary/nutrition problems • Tool objective data to measure o height, weight, weight change, primary diagnosis, and the presence of other co-morbidities o Combine multiple objective measures with subjective measures related to nutrition to adequately screen for nutritional problems. • Identification of risk factors such as unintentional weight loss, presence of a modified diet, or the presence of altered nutritional symptoms (i.e., nausea, vomiting, diarrhea, and constipation) requires nutritional consultation. • Older adults at disproportionate risk • Referral criteria examples o Involuntary decrease of >10 lb in 6 months o Problems complying with a special diet o Dependent for eating o Elevated serum cholesterol Nutrition Risk Factors • Avoid cardiovascular disease (CHD, CVA, HTN) o Balanced diet with emphasis on fruits/vegetables/grains o Limit ▪ High-calorie foods ▪ Trans-fatty acids ▪ Salt: <6g/day; DASH diet o Alcohol o Cholesterol: <300 mg/day (200 mg if at risk) • Presence of cardiovascular risk factors o Therapeutic Lifestyle Changes (TLC) as per ATP III guidelines Obesity • Associated with nutrition-related causes of death • BMI used to screen for risk health/nutritional disorders o Healthy BMI = 18.5 =underweight o 19-25 healthy o 25-30 overweight o obese = ≥30 • Focus of nutritional counseling o Balanced diet and appropriate serving sizes o Incorporate exercise to help in weight control o LEARN acronym: Steps to help with behavior change o Avoid fad diets, repeated weight gain/loss cycles Diabetes • Minority & Elderly disproportionately affected • Medical nutrition therapy (MNT) (this should be individualized) o Most critical/pivotal component of DM care o Purpose: Delay/prevent complications o MNT individualized—ongoing monitoring of metabolic parameters ▪ Tailored meal plan dependent on person’s energy needs to determine number food choices ▪ Evaluate/adjust through outcome measures ▪ Referral to dietician/registered diabetes educator HIV Recommendations • Purpose: Minimize nutritional consequences of disease (EX: severe weight loss, effects from depression) • Initial nutritional assessment needed • Nutrient-dense, protein-rich, well-balanced • Vitamin and mineral supplement • Focus on food sanitation • Consider nutrition need for comorbidities • Avoid breastfeeding (vertical HIV transmission) My Plate (nutritional portion method of education) • Five food groups o Grains ▪ Whole or refined grains, cereals, pasta, rice o Vegetables ▪ 2 ½ cups o Fruits o Protein ▪ Complete ▪ Fish, Chicken, Soybean, Turkey, Cheese ▪ Incomplete ▪ Legumes(beans,peas), vegetables o Diary Learn how to calculate BMI • Weight/ height^2 Vitamin C absorbs Iron Exercise Effects of Exercise: Aging • Improves functional independence o Decreases fails o Hospitalizations • Improves blood lipid profiles • Reduces fat • Prevents osteoporosis (increase BMD) • Improves functions o Cardiovascular o Cardiopulmonary o Metabolic Functions Cardiac Risk factors(minimizes heart attack) • CHD (Coronary Heart Disease) o Both primary/secondary prevention ▪ Primary: Catch it before it starts & make people aware of it ▪ EXs: Periodic exams, exercise, safety precautions, immunizations ▪ Secondary: Early diagnosis, prompt treatment, disability limitation ▪ EXs: Screenings, MRI, dental examinations, diagnostic tests, HIV testing o Less likely to develop CHD o Decreases cardiac mortality in heart failure patients and improves metabolic/functional indicators o Positive effects: ▪ cholesterol levels, blood pressure, glucose tolerance, obesity, platelet function • Hypertension (need to control it if you want to prevent it) o Decreases blood pressure (control blood pressure by exercise) o Dilates peripheral blood vessels, decreases systemic vascular resistance • Hyperinsulinemia and Glucose Tolerance o Increases insulin sensitivity o Decreases obesity o Improves glycemic control o Helps prevent progression of DMI II during early disease stages Obesity • Promotes negative energy balance • Increases metabolic rate for extended period • Increases metabolic efficiency for burning calories (increases lean body mass) • Counteracts decrease in metabolic rate by preserving lean body mass • Alternative to stress eating • Exercise Guidelines o Low-impact aerobic exercise, increase in daily activities, and resistance training o 5-7 times a week for 40-60 minutes daily o Keep telling people to do small activity/exercise ▪ ENCOURAGE IT! Osteoporosis(pressure & pain of BIG joints usually at hip/knee) • Increases BMD • Related to intensity of physical activity and degree to which activity stresses the bone o Weight bearing, aerobic, and resistance training important o Goal: Increase mechanical stress on bone • Exercise Guidelines • Osteoarthritis o “I know you’re sore, but you can do it” Arthritis(pressure/pain/inflammation of SMALL joints) • Improves/help strengthen joint function/muscles • Increases muscle strength and aerobic fitness: Enhances ADLs • Improves psychological state • Decreases loss of bone mass/risk of chronic disease • Yoga and Tai Chi can help • Exercise Guidelines o Daily: Develop joint flexibility • Rheumatoid Arthritis o “I know you’re sore, you can take a break” Low back pain • Bony vertebrae and disk health depends on movement to maintain muscle strength/flexibility and prevent strain/joint dysfunction • Exercise reduces pain, improves function, decreases loss of work days • Exercise Guidelines o Goal: Prevent debilitation from inactivity ▪ Improve endurance, strength, and flexibility o Individualized Program ▪ Trunk and extremity muscle strengthening ▪ Aerobic conditioning Holistic Health/Complementary Alternative Medicine (CAM) Allopathic Medicine • Western Medicine • Mainstream medical use of pharmacologically active agents or physical interventions to treat or suppress symptoms or pathophysiologic processes of diseases or conditions Clinical Practice Guidelines Holistic Nursing/Roles and responsibilities • Holistic nursing regards and treats the mind-body-spirit of the patient • Uses holistic nursing interventions such as relaxation therapy, music therapy, touch therapies, and guided imagery Risks vs Benefits of Alternative practice • Traditional Chinese Medicine Helps with (Benefits): o Substance Abuse o Detoxification o Insomnia o Musculoskeletal Pain of the knee o Reduces nausea and vomiting • Touch Therapies helps with: o Decreases anxiety o Decreases depression, fatigue, pain, and blood pressure o Improvement in quality of life score o Improved pain control Complementary/Alternative Therapies • Acupuncture (Ancient Chinese) o Needles are placed at specific points in the body o Helps to reduce pain, prevent/manage disorders • Hypnosis (Greek) o Helps with consciousness, relaxation o Used for conditions such as smoking, anxiety, pain • Reiki (Japanese) o Life force energy fields to affect health • Energy Therapies • Healing touch o Biofield therapy; uses gentle touch directly on or close to body to influence and support the human energy system and bring balance to the whole body (physical, spiritual, emotional, and mental); a formal educational and certification system provides credentials for practitioners • Reiki therapy o Biofield therapy derived from ancient Buddhist rituals; practitioner places hands on or above a body area and transfers “universal life energy,” providing strength, harmony, and balance to treat a patient's health disturbances • Therapeutic touch o Biofield therapy involving direction of a practitioner's balanced energies in an intentional manner toward those of a patient; practitioner's hands lay on or close to a patient's body • Manipulative and Body-Based Methods (Involve Movement of Body with Focus on Body Structures and Systems) • Acupressure o Applying digital pressure in a specified way on designated points on the body to relieve pain, produce analgesia, or regulate a body function • Chiropractic medicine o Manipulating the spinal column; includes physiotherapy and diet therapy • Craniosacral therapy o Assessing the craniosacral motion for rate, amplitude, symmetry, and quality and attuning/aligning the spinal column, cerebrospinal fluid, and rhythmic processes, releasing restrictions or abnormal barriers to motion • Massage therapy o Manipulating soft tissue through stroking, rubbing, or kneading to increase circulation, improve muscle tone, and provide relaxation • Mind-Body Interventions(Honor Connections Between Thoughts and Physiological Functioning Using Emotion to Influence Health and Well-Being) • Biofeedback o Process providing a person with visual or auditory information about autonomic physiological functions of the body such as muscle tension, skin temperature, and brain wave activity through the use of instruments • Breathwork o Using a variety of breathing patterns to relax, invigorate, or open emotional channels • Guided imagery o Concentrating on an image or series of images to treat pathological conditions • Meditation o Self-directed practice for relaxing the body and calming the mind with focused rhythmic breathing • Music therapy o Using music to address physical, psychological, cognitive, and social needs of individuals with disabilities and illnesses; improves physical movement and/or communication, develops emotional expression, evokes memories, and distracts people who are in pain. • Tai chi o Incorporating breath, movement, and meditation to cleanse, strengthen, and circulate vital life energy and blood; stimulate the immune system; and maintain external and internal balance • Yoga o Focuses on body musculature, posture, breathing mechanisms, and consciousness; goal is attainment of physical and mental well-being through mastery of body achieved through exercise, holding of postures, proper breathing, and meditation • Movement Therapies (Eastern or Western Approaches to Promote Well-Being) • Dance therapy o Intimate and powerful medium because it is a direct expression of the mind and body; treats people with social, emotional, cognitive, or physical problems • Pilates o Method of body movement used to strengthen, lengthen, and improve the voluntary control of muscles and muscle groups, especially those used for posture and core strengthening Therapeutic Responses [Show More]
Last updated: 1 year ago
Preview 1 out of 40 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 18, 2021
Number of pages
40
Written in
Additional information
This document has been written for:
Uploaded
Nov 18, 2021
Downloads
0
Views
49
.png)




 Rasmussen College.png)