*NURSING > STUDY GUIDE > NR 601Comprehensive Final exam study guide and practice questions (Final review) (All)
NR 601Comprehensive Final exam study guide and practice questions (Final review)
Document Content and Description Below
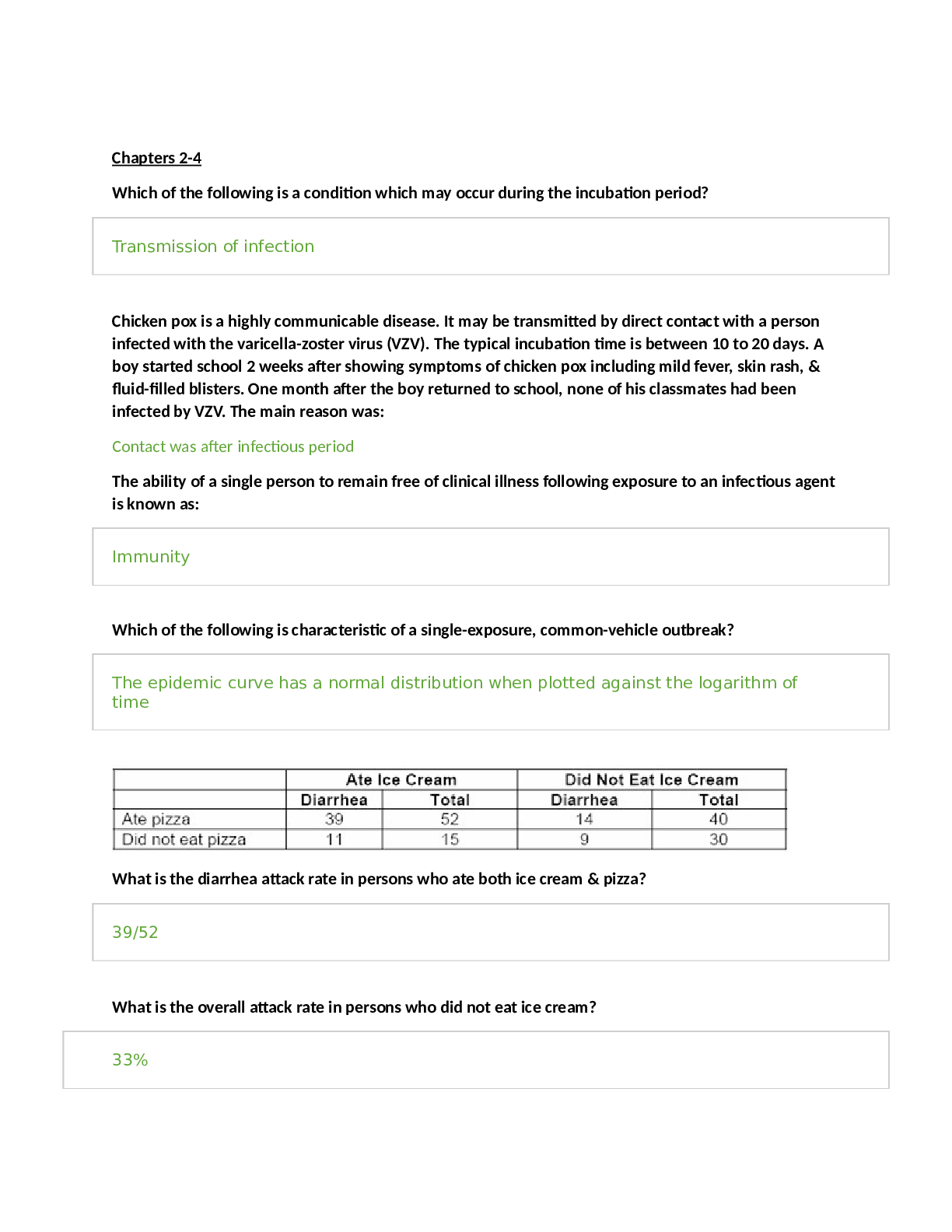
NR 601 final review.docx NR 601 Comprehensive Final exam study guide and practice questions DISCLAIMER- None of this is my original work. The first 11 pages are the completed study guide from a prev... ious class. Pages 11 through 13 are the NR 601 course final exam review topics in outline form (Thanks Lisa Trevino!). Page 13-46 includes my notes from class and YouTube videos, Kennedy-Malone text (minimal), lessons, and some external research. When the information came from an external article, I included a link so that you do not use it as a test resource. Hopefully this is helpful for us as both a test and boards review. I kinda sorta (but not really because I’m over it) apologize for any typos. How to conduct Mini-Cog- The Mini-Cog has been demonstrated to have comparable psychometric properties to the MMSE The primary advantage of the Mini-Cog is that it is shorter than the MMSE and measures executive function. It is composed of a three-item recall and the Clock Drawing Test (CDT) and takes about 3 minutes to administer The Mini-Cog is a short dementia assessment that combines three-word recall with clock-drawing capability. Patients are given a total score reflecting accuracy in clock drawing and recollection of the given three words. A score of 0 to 2 is a positive screen for dementia Causes of delirium in elderly- Causes of delirium are numerous and in elderly hospitalized patients there are often multiple etiologies, including metabolic, infection, cardiac, neurological, pulmonary, sensory impairments, medications, and toxins. Regardless of cause, a consistent finding is significant reduction in regional cerebral perfusion during periods of delirium in comparison with blood flow patterns after recovery. A possible neurological common pathway may involve acetylcholine and dopamine, and the disruption in the sleep-wake cycle in delirium indicates melatonin as a possible factor. (Kennedy-Malone 59) Agnosia Loss of ability to identify objects ADA criteria for diagnosing DM- FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h.* 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75-g anhydrous glucose dissolved in water.* A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay.* In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L). • Urinary incontinence- Involuntary loss of urine from the bladder ▪ So common in women many consider it normal ▪ Common in older men w/ enlarged prostate o Can affect quality of life o Significance-One of the most common complains w/ older adults, Distress & embarrassment, Cost burden to pt & society as a whole, Not life-threatening, may effect QOL, PCP essential to educating individuals o Epidemiology- Increased prevalence w/ age in men & women, Nursing home population – 40-70%, Often a factor in placement ▪ URGENCY UI is greater in men ▪ STRESS UI is greater in women o Terminology ▪ UI- Unintentional voiding, loss or leakage of urine ▪ Continuous incontinence-Continuous loss or leak of urine ▪ Increased daytime frequency-More frequent during day than considered normal ▪ Nocturia-Interruption of sleep one or more times due to the need to urinate – increases in frequency after age 50 ▪ Urgency-Sudden, compelling desire to pass urine that’s difficult to prevent ▪ Overactive bladder syndrome- Urgency, frequency, nocturia w/ or w/o incontinence o Risk Factors-Aging,Obesity,Smoking, Caffeine,Uncontrolled DM, Constipation,Use of diuretics o Risk Factors by gender-Women:Aging, obesity, smoking, caffeine intake, DM, pregnancy, multiparity, estrogen deficiency, hx of pelvic surgery, diuretics Men:Aging, obesity, smoking, caffeine, DM, prostate dx, hx of prostate surgery, hx of UTIs, diuretics o Physical changes w/ aging that contribute to UI ▪ Lower urinary tract-Detrusor muscle over activity,Decrease in detrusor contractility, Increase in post void residual,Decrease in urethral blood flow ▪ Women – decrease in urethral closure pressure,Low estrogen following menopause - leads to atrophy of ureteral mucosal epithelium & increase in urethral sensation ▪ Men can experience constriction of urethra due to BPH which may result in bladder outlet obstructing symptoms - Initial clinical workup for UI in Men o PMH, PE, UA, DRE: Eval of prostate,PSA w/ new onset in men - UI workup in women:Exclude underlying causes,PMH, PE, UA, Pelvic exam, vaginal exam, perineal, Identify estrogen status of pt, Pelvic prolapse, fistula, -Cough test, Integrity of pelvic musculature, leaking of urine ▪ Full bladder ▪ Standing position ▪ Asked to cough ▪ If urine leak is observed, stress incontinence is confirmed - Red flags in males o Higher level of suspicion for serious diseases, Refer to urology if Previous pelvic surgery, Pelvic radiation, Pelvic pain, Severe incontinence, Severe UTI symptoms, Recurrent urologic infection,Abnl Prostate exam,Elevated PSA o Be alert to these with NEW ONSET UI- Hematuria,Pelvic pain,Abdominal mass, Dysuria, Proteinuria, Glucosuria, CVA tenderness,Nodular prostate,Any new neuro symptoms - Goals of treatment: Reduce symptoms, Improve QOL, Increase social activity, Reduce leakage volumes, increase dryness, use less protection; Increase independence in incontinence management; Decrease caregiver burden - 1st line management guidelines o AHRQ guidelines for management of UI in women ▪ Behavioral therapy ▪ Lifestyle modification ▪ Try for 3 months before pharm management o Weight loss, Smoking cessation(Tobacco is a bladder irritant),Less coughing o Dietary changes-Alcohol, soda, coffee with or without caffeine, acidic foods and spicy foods o Maintain adequate fluid balance to reduce constipation, provide adequate flow to kidneys - Behavioral strategies:Bladder training, Bladder control strategies,Timed voiding,Kegels, Pelvic floor training - 2nd line management - Medication o Antimuscarinic medication: 1st line for women ▪ Block the parasympathetic muscarinic receptors ▪ Inhibit involuntary detrusor contractions ▪ Side effects due to the effects on other muscarinic receptors o Outcomes unpredictable and side effects common o Common s/e: Dry mouth**, Blurred vision, Constipation,Nausea,Dizziness, Headache o AntimuscarinicsMechanism of action ● Blocks acetylcholine at muscarinic receptors, relaxes bladder smooth muscle, inhibits involuntary detrusor contractions (anticholinergic) ● CYP3A4 substrates ▪ Indications: UI and OAB ▪ Contraindications: Untreated/uncontrolled narrow angle glaucoma,Gastric retention, Urinary retention ▪ Precautions:CNS depression,Caution in elderly ● Renal dosing o CrCl <30 o Beta 3 Adrenergic Agonist – Mirabegron (Myrbetriq) ▪ Also approved for UI and OAB ▪ Clinical trials – significant reduction in incontinence and micturations ● No anticholinergic s/e ▪ Mech of action ● Selectively stimulates beta-3 adrenergic receptors ● Relaxes smooth muscle – bladder ▪ Contraindications/caution: HTN- Do not use if SBP >180, DBP >100 ▪ Avoid severe renal/liver disease ▪ Dose – 25-50mg PO QD ▪ CrCl <30 – max 25mg - 2nd line of UI in Males – Alpha 1 blockers o Men, not women! o Alpha 1 blockers antagonize peripheral alpha 1 adrenergic receptors o Used in men d/t high incidence of BPH in aging men o Alpha antagonists ▪ Alpha 1A – prostatic smooth muscle relaxation ▪ 1B – vascular smooth muscle contraction ▪ 1D – bladder muscle contraction and sacral spinal cord innervation o Meds ▪ Doxazosin SE: Dizziness, dyspnea, edema, fatigue, somnolence ▪ Terazosin SE: Asthenia, dizziness, postural hypotension ▪ Tamsulosin SE:Abnormal ejaculation, asthenia, back pain, dizziness, increased cough ▪ Alfuzosin- CrCl <30 use with caution, SE: Dizziness, URI ▪ Silodosin SE- Retrograde ejaculation Differentials as cause for erectile dysfunction- Differential diagnosis: o Vascular, Endocrine, Neurological, Neurovascular, Substance abuse, End-organ disease, Psychogenic, Social causes (Kennedy-Malone 376) Elder abuse Types- o Physical, Emotional, Sexual, Neglect, Exploitation, Abandonment, Self-Neglect Risk Factors- o Age, Gender, Cognitive Impairment, Living Arrangement, Social Isolation Signs of abuse- o bruises, slap marks, unexplained burns, increased accidents, lack of hygiene, failure to meet medical needs, weight loss, decubiti, changes in personality, decreased interaction, unexplained STD Provider responsibility in reporting abuse o If you suspect elder abuse perform a physical exam and order any necessary tests. o Include a cognitive screen. o Document your findings. This includes what the patient says and your objective findings. o You may need to interview your patient and the caregiver separately to see if the stories are the same. o Be aware of your state laws regarding mandatory reporting of suspected abuse. Differentials as cause for hematuria- Differentials per class notes Dietary substances o Caffeine, spices, Tomatoes, chocolate, alcohol, Citrus, soy sauce, & some herbal meds Medication o Beta-lactam antibiotics, sulfonamide, NSAIDs, Cipro, allopurinol, Tagamet, & dilantin Anticoagulation and papillary necrosis o Coumadin, Heparin, aspirin, & NSAIDs Glomerular nephritis Hydrocarbons (glue, paint) NSAIDs Urolithiasis menses Terazosin use(s)- Alpha blocker for BPH. 1-10 mg P.O. nightly. Caution in those with cataracts and in elderly. Side effects o hypotension, priapism, dizziness, dyspnea, tachycardia. 2nd Line Management of UI in males ***Alpha 1 Blockers Pharmacologic agents for men with urinary incontinence differ from women; Alpha 1 blocker antagonize peripheral alpha-1 adrenergic receptors and commonly referred to as alpha 1 blockers *Lifestyle changes and Behavioral Management are first-line but when not effective alpha 1 blocker is initiated; *This difference in choice of medication for men is due to the high incidence of BPH associated with aging men Alpha 1 Adrenergic Receptor antagonists Alpha 1A- Prosthetic smooth muscle relaxation Alpha 1B- Vascular smooth muscle contraction Alpha 1D -Bladder muscle contraction and sacral spinal cord innervation UTIs in men and women UTI treatment guidelines BPH- Progressive, benign hyperplasia of prostate gland tissue Etiology/incidence- o Cause is uncertain, About 50% of men have it by 60, By age 85, 90% have it o Most common cause of bladder outlet obstruction in men over 50 Symptoms are attributed to mechanical obstruction of the urethra by the enlarged prostate gland Signs/Symptoms- o Gradual worsening of the following, Frequency, urgency, urge incontinence, Nocturia, dysuria, Weak urinary stream, dribbling, hesitancy, Sensation of full bladder even after voiding, Retention Diff Dx- o Urethral stricture, Prostate or bladder cancer, Neurogenic bladder, Bladder calculus, Acute or chronic prostatitis, Bladder neck contractor, Medications that affect micturition Physical findings- o Abdomen,May have distended bladder secondary to retention; Prostate,Nontender w/ asymmetric or symmetrical enlargement, gross enlargement atypical, Consistency is smooth, rubbery (eraser), Nodules may be present Differentiation from BPH and CA needs biopsy Tests/Findings o UA-No hematuria or UTI, Urinary flow rate, Voided volume and peak urinary flow rate (uroflowmetry) may detect obstruction flow, Abdominal US – rules out upper tract patho, PSA, Consider PVR urine volume, Cr to assess renal function, elevated levels suggest urinary retention or underlying renal disease – refer this patient Treatment/Management- o Refer men who have the following, Refractory urinary retention who have failed one attempt at cath removal, Recurrent infection, recurrent retention, refractory hematuria, bladder stone, large bladder, diverticula, or renal insufficiency related to BPH, Consider referral if complications exist or if patients have severe symptoms Management- o Men who have no indications for surgery, Discuss risks/benefits of all options, Watchful waiting (observation), Behavioral techniques to reduce symptoms, Limit fluid after dinner, Avoid medications such as Antidepressants, Antiparkinson drugs, Antipsychotics, Antispasmodics, Cold meds, Diuretics Medication Treatments o Alpha adrenergic blocker – for smaller prostates o 5-alpha adrenergic blocker – larger prostates o Combo therapy is an alpha-adrenergic blocker and finasteride is used now for men w/ large prostates Surgery has the best chance for relief of symptoms, but greater risks Follow up: o Teach signs/symptoms of retention and obstruction, o If observing for now, recheck every 6-12 months, o In use of meds, recheck in 4-6 weeks, o If post surgery follow up is at the discretion of the urologist Acanthosis nigricans A sign of insulin resistance that can be seen in African Americans associated with colon cancer, obesity and DM Delirium treatment- (Kennedy p. 560). Identify causes, prevent delirium though complications of identified disorders. \ Focus on safety. Frequent reassurance and re-orientation. First generation --haloperidol. Second generation (olanazapine, risperidone, ziprasidone and quitiapine) antipsychotics to control behavioral symptoms. Essential tremor vs. Parkinson’s Disease Essential tremor is an action tremor 6 to 8 Hz, Parkinson’s tremor is a resting tremor which is 3 to 6 Hz. (Kennedy p. 425) Seizure causes In older adults stroke is the most common underlying cause of seizures. Other causes include neurodegenerative disorders, brain tumors and head injuries. (Kennedy p 438) Hospice & palliative care- Hospice: o Last 6 mos of life. Uses palliative care principles to support pt and family. Includes bereavement services. Covered by Medicare/Medicaid, most private insurance. Interdisciplinary care, medical service, supplies, drugs Palliative Care: o To relieve pain and improve QOL. Used early in dz process. Interdisciplinary Care. Provides care for the entire dz process, from diagnosis to death, including bereavement services. Pain- Pain assessment tools: o Visual Analogue Scale o Numerical Analogue Scale o Wong Baker FACES o Pain Assessment in Advanced Dementia scale Types of pain: o Somatic, o Visceral, o Neuropathic Framework for pharmacological interventions for pain: The WHO Step Ladder o 1st step: NSAIDs and Tylenol for mild pain o 2nd step: Opioids added, usually with APAP for moderate to severe pain with functional impairment and or decreased QOL o 3rd step: Opioid pain meds, sometimes around the clock for severe pain Adjuvant meds: o Tricyclic antidepressants, Nortriptyline, Desipramine, Duloxetine, Gabapentin, Pregabalin, Lidocaine 5% patch, Capsaicin cream, Corticosteroids, Calcitonin, Baclofen Pain management in elderly Delirium vs. dementia- Delirium- o rapid onset (hours to days). o Poor memory, disorientation, speech disturbance, perceptual disturbance. o Typically fluctuates over course of day. [Show More]
Last updated: 1 year ago
Preview 1 out of 75 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 31, 2021
Number of pages
75
Written in
Additional information
This document has been written for:
Uploaded
Aug 31, 2021
Downloads
0
Views
45



 Rasmussen College.png)