*NURSING > STUDY GUIDE > NR 511 Week 4 Midterm Question Bank (Newest 2020): Differential Diagnosis and Primary Care Practicum (All)
NR 511 Week 4 Midterm Question Bank (Newest 2020): Differential Diagnosis and Primary Care Practicum: Chamberlain | 100 % VERIFIED ANSWERS, GRADE A
Document Content and Description Below
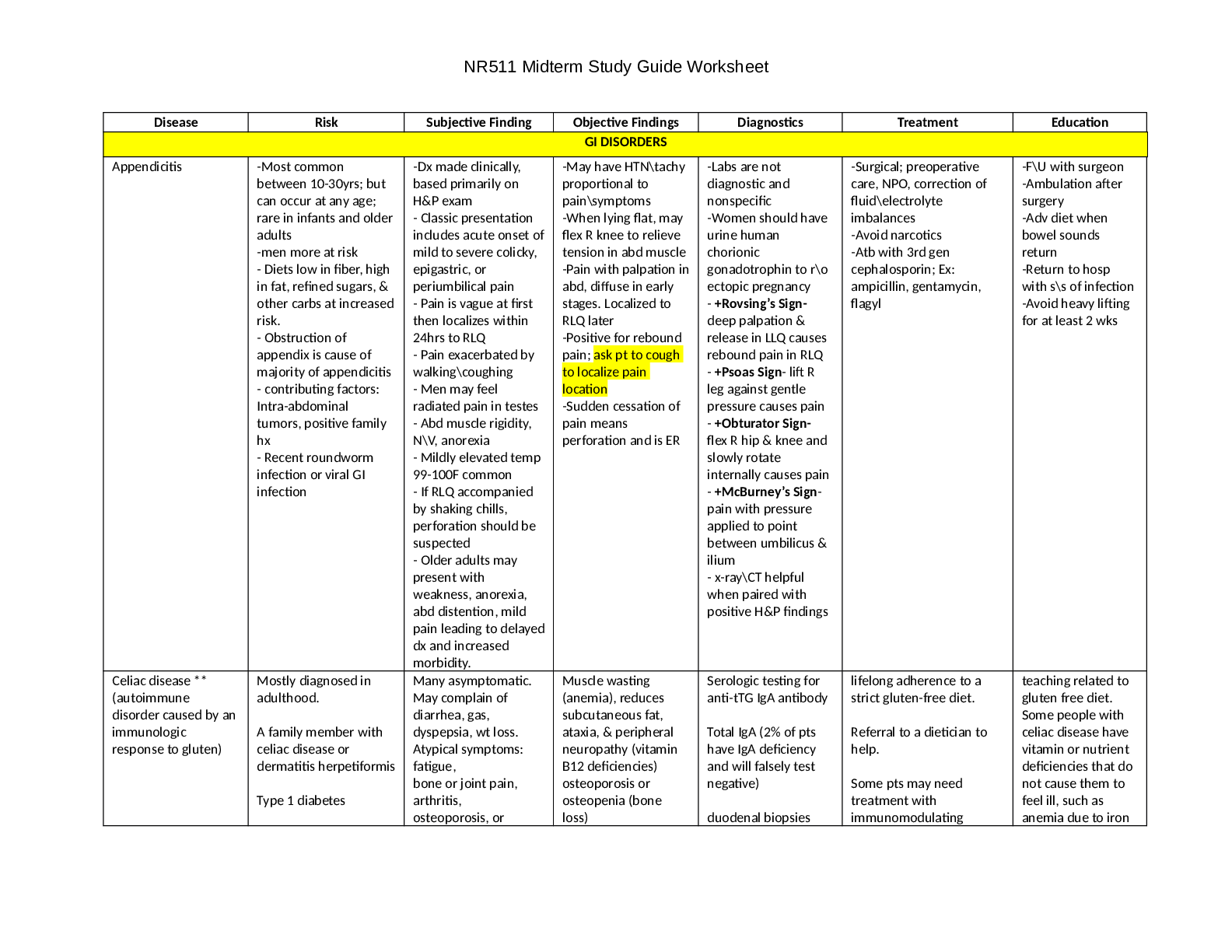
NR 511 Week 4 Midterm Question Bank Q bank questions Respiratory An adult has upper respiratory symptoms and cough for the past 14 days. What should be considered? (Pertussis) Pertussis should always ... be considered in adults who present with acute cough of greater than 5 days’ duration. The incubation period for pertussis is about 7-10 days. Patients present with URI symptoms for 1-2 weeks. The classic paroxysmal cough usually begins in the second week of the illness. The duration of symptoms and cough are about 3 months even when treated with antibiotics. This is highly infectious and is a reportable disease. Mycoplasma pneumoniae is: (a disease with extrapulmonary manifestations) Mycoplasma is an atypical pathogen and produces atypical pneumonia. It can be difficult to diagnose because symptoms can be varied and involve multiple body systems (extrapulmonary manifestations). Infection with Mycoplasma may present with a normal white blood cell count, maculopapular rash, GI symptoms, tender joints and aches, and, though rare, cardiac rhythm disturbances. Respiratory symptoms may not be pronounced. On chest X-ray there are some unique findings (peribronchial pattern) with Mycoplasma. These include thickened bronchial shadow, streaks of interstitial infiltration, and atelectasis. These are more likely to occur in the lower lobes. Which medication below is contraindicated in an asthma patient because it may increase risk of sudden death if used alone? (Long-acting bronchodilator) A long-acting bronchodilator can be used to treat asthma when it is used in combination with an inhaled steroid. Otherwise, using a long-acting bronchodilator like salmeterol is contraindicated. There is an increased risk of sudden death with asthma exacerbations when this class is used solo to treat asthma. The other choices can be used to treat asthma. Choices vary depending on the patient. A 75-year-old female with emphysema who has been treated with inhaled steroids for many years should: (should be screened for osteoporosis) Older females are at higher risk than others for osteoporosis. This female patient, who has used inhaled steroids and smokes, has multiple risk factors for osteoporosis. Additionally, she probably has emphysema because she smoked (or still smokes). If she is Asian or Caucasian, she has still another risk factor. Screening for osteoporosis should be considered when managing patients with multiple risk factors. A patient received the pneumonia immunization at age 60 years. He is 65 years old and presents to your clinic today. What recommendation should be made about the pneumococcal immunization? (He should receive another one today) This patient should receive another one today because he is 65 years old and at least 5 years has elapsed since his last one. The CDC does not recommend immunizing this patient every 5 years. Two immunizations are available, PCV13 and PPSV23. He needs both, but PCV13 should be administered today. PPSV23 should be administered at least 1 year later. Which of the following medications should be used cautiously in a patient who has asthma? (Timolol ophthalmic drops) Timolol is a beta blocker. This class of medications can precipitate bronchoconstriction in patients who have asthma. Even though timolol is being administered in the eye, it is absorbed through mucous membranes and can exert systemic effects. Beta blockers should be avoided in patients with asthma and used cautiously in patients with COPD. The other medications listed have no specific contraindications for patients with asthma. The most common symptom associated with acute bronchitis is: (Cough) Fever (temp > 101°F) is an unusual symptom associated with acute bronchitis. Cough is the most common symptom associated with acute bronchitis. Purulent sputum is identified in more than 50% of patients with acute bronchitis. The color imparted to the sputum is usually due to sloughing of epithelial cells, not bacterial infection. Concurrent upper respiratory symptoms are typical of acute bronchitis. Pharyngitis is common. Mild persistent asthma is characterized by: (symptoms occurring more than twice weekly) Mild persistent asthma is characterized by symptoms that occur more than twice weekly but not daily; or 3-4 nocturnal awakenings per month due to asthma. It is treated with an inhaled steroid daily, and a bronchodilator PRN for exacerbations. If symptoms occur more than twice weekly, therapy should be stepped up. Generally, a long-acting bronchodilator is added to the steroid when therapy is stepped up. The chest circumference of a 12 month-old is: (equal to head circumference) The chest circumference is not routinely measured at well-child visits, but is assessed if there is concern about the circumference of either the head or the chest. An exception to this observation can occur in premature infants where the head grows very rapidly. Normally, the head exceeds the chest circumference by 1-2 cm from birth until 6 months. Between 6 and 24 months the head and chest circumference should be about equal and by 2 years of age the chest should be larger than the head. The chest circumference is measured at the nipple line. A patient with cough and fever is found to have infiltrates on chest x-ray. What is his likely diagnosis? (Pneumonia) The finding of infiltrates on chest x-ray, in conjunction with clinical findings of fever and cough, should direct the examiner to consider pneumonia as the diagnosis. Other common clinical findings with pneumonia include chest pain, dyspnea, and sputum production. Though not common, some patients with pneumonia exhibit gastrointestinal symptoms like nausea, vomiting, and diarrhea. An uncommon symptom associated with acute bronchitis is: (temperature > 101°F) Fever is an unusual symptom associated with acute bronchitis. Cough is the most common symptom associated with acute bronchitis. Purulent sputum is identified in more than 50% of patients with acute bronchitis. The color imparted to the sputum is usually due to sloughing of epithelial cells, not bacterial infection. Concurrent upper respiratory symptoms are typical of acute bronchitis. Pharyngitis is common within the first 3 days of the illness. Patients who have cough-variant asthma: (all exhibit cough) One of the most common causes of cough in adults is asthma. Cough due to asthma is often accompanied by episodic wheezing or dyspnea, though some patients who have asthma only cough. This is termed “cough-variant asthma.” The clinical presentation of asthma varies but hyper-responsiveness of the airways is a typical finding. The most common cause of atypical pneumonia in adults is: (Mycoplasma pneumonia) In patients who have atypical pneumonia, Mycoplasma is the most common pathogen. M. pneumoniae is so named because of its atypical appearance on chest X-ray. This organism is responsible for “walking pneumonia” that is prevalent in a young adult population. This accounts for about 15% of pneumonia and is transmitted via respiratory droplet. Which patient might be expected to have the worst FEV1? (A 65-year-old with emphysema) FEV 1 stands for “forced expiratory volume in 1 second.” This is the volume of air that is forcefully exhaled in the first second of exhalation after a deep breath. Patients with emphysema are not able to do this efficiently because their alveoli are stretched, and mostly contain trapped air. FEV 1 is used to assess airway obstruction. An asthma patient in the green zone would be expected to have a normal (compared to himself) FEV1. An FEV1 measurement or pulmonary function tests would not be performed on a patient with pneumonia or bronchiectasis because he would have diminished respiratory capacity related to his infection. A patient who has asthma presents with chest tightness, wheezing, coughing, and fever. He has wheezing and diminished breath sounds in the upper right lobe. His cough is nonproductive, and he denies nasal symptoms. Which symptom is not likely related to his asthma? (Fever) Wheezing is typical of asthma, but one must consider pneumonia in any patient who presents with diminished breath sounds in only one lobe. Fever is not typical of asthma or an exacerbation. Ipratropium is very widely used in the treatment of COPD. Which of the following statements about ipratropium is correct? (It decreases parasympathetic tone and produces bronchodilation) Ipratropium is the most widely studied anticholinergic medication used to treat patients with COPD. It produces its helpful effects by reducing cholinergic tone in the lungs. It may be used with a beta agonist if shortness of breath is present. However, beta agonists increase side effects like tachycardia and tremor and do not improve efficacy. An 80-year-old has Stage 3 COPD. He is most likely to have concomitant: (anxiety or depression) About 40% of older patients who have COPD have concomitant anxiety and/or depression. It should be treated because it affects the overall management of COPD. COPD is characterized by airflow limitation and dyspnea. This may contribute to feelings of chronic anxiety. Additionally, many chronic diseases are associated with depression. This is the case with COPD. A 6-year-old child who has moderate persistent asthma is diagnosed with pneumonia after chest X-ray and laboratory studies. He developed a sudden onset of fever with chills. He is in no distress. What is the preferred treatment for him? (Amoxicillin) In children who are older than 5 years of age, the most common bacterial pathogen is an atypical pathogen. Because this child has asthma and uses an inhaled steroid daily, the most likely pathogen is Streptococcus pneumoniae. An abrupt onset of fever and chills is suggestive of Streptococcal pneumonia. Amoxicillin is usually chosen first for its efficacy, cost, and tolerability. The higher dose (80-100 mg/kg/d) is chosen because of the prevalence of resistant Streptococcus pneumoniae. Azithromycin would be chosen if an atypical pathogen was more likely. Doxycycline is not an appropriate choice because it has poor Strep coverage and it is contraindicated in children younger than 8 years. What disease is usually managed with a short-acting or long-acting inhaled anticholinergic medication? (COPD) First-line treatment for patients with COPD who have intermittent symptoms of shortness of breath is an anticholinergic medication because it improves lung function. Alternatively, a short-acting beta agonist may be used. Anticholinergic medications are not used as a lone agents to manage symptoms of asthma; inhaled steroids usually are. Bronchitis is a viral infection that is self-limited and usually does not require an inhaled medication. Bronchiectasis is a disease in which the respiratory tubules are permanently enlarged. Symptoms include chronic production of purulent mucous. A patient with pneumonia reports that he has rust-colored sputum. What pathogen should the nurse practitioner suspect? (Streptococcus pneumonia) Clinical descriptions of mucus do not really help in clinical decision-making regarding pneumonia, but certain clinical characteristics are associated with specific types of pneumonia. Strep pneumonia, also known as pneumococcal pneumonia, is associated with rust-colored sputum. Scant or watery sputum is associated with atypical pathogens like Mycoplasma and Chlamydophila pneumonia. Thick, discolored sputum may be associated with bacterial pneumonia. A 44-year-old nonsmoker is diagnosed with pneumonia. He is otherwise healthy and does not need hospitalization at this time. Which antibiotic can be used for empirical treatment of pneumonia according to the most recent Infectious Diseases Society of America/American Thoracic Society guidelines? (Azithromycin) The guidelines recommend macrolide use or doxycycline for initial treatment of uncomplicated pneumonia in outpatients who are otherwise healthy and have not had recent antibiotic exposure. The initial choices can be any of these: azithromycin, clarithromycin, or doxycycline. These agents are chosen because they cover atypical pathogens, the most likely pathogen in this population. Fluoroquinolones are commonly used first line in these patients; however, the guidelines strongly recommend using fluoroquinolones for patients with comorbidities or patients who have recent antibiotic exposure. The gold standard for diagnosing pneumonia on chest X-ray is the presence of: (Infiltrates) The finding of infiltrates on chest X-ray, in conjunction with clinical findings of fever, chest pain, dyspnea, and sputum production on clinical exam, should direct the examiner to consider pneumonia as the diagnosis. An 83-year-old healthy adult is diagnosed with pneumonia. He is febrile but in no distress. What is the preferred treatment for him? (Levofloxacin) At age extremes, the most common pathogen is Streptococcus pneumoniae. Because of the age of the patient and the consequences of potential treatment failure, a respiratory quinolone should be considered. Quinolone antibiotics can produce QT prolongation and should be used cautiously in older adults. Azithromycin or doxycycline would be chosen if an atypical pathogen was suspected. This is unlikely in this patient because of his age. The pneumococcal immunization in infants has: (shifted the pathogenesis to fewer cases of S. pneumonia) The heptavalent pneumococcal conjugate vaccine (PCV13), Prevnar, protects children from 13 types of pneumococcal bacteria. It has reduced the incidence of ear infections caused by S. pneumo and has reduced the incidence of recurrent ear infections and tube placement by 10-20%. The pathogenesis of acute otitis media has shifted to more cases of H. influenzae, but this organism is less likely to become resistant, as Strep pneumo has. A 78-year-old adult who has a 50 pack year smoking habit asks the nurse practitioner about the benefits of quitting “at my age.” What should the nurse practitioner reply? (This will decrease your risk of all cause mortality 5 years after stopping) Smoking cessation at any age is beneficial to the person engaging in smoking cessation. Data demonstrates that after 5 years of smoking cessation, there is a significant decrease in the risk of death from coronary disease, cancer, and COPD. The patient already has COPD if he has a 50 pack year habit. All patients should be counseled to quit smoking regardless of age. M. pneumoniae and C. pneumoniae are respiratory pathogens that: (cause atypical pneumonia) These two organisms are common causes of pneumonia. They are called atypical pathogens because they produce atypical pneumonia. They are transmitted via respiratory droplets from the nose and throat of infected people. Prolonged close contact is probably needed for transmission to occur. Patients are usually contagious for 10 days or so. Most commonly, these infections occur in younger patients, but all ages may be affected. Generally, the atypical pathogens are eradicated with macrolide antibiotics or tetracyclines. An 18-month-old child is diagnosed with bronchiolitis. His respiratory rate is 28 breaths per minute. Which choice below is most appropriate for patient management? (Antipyretics) Bronchiolitis is a viral infection and antibiotics would be inappropriate for management. Since fever commonly accompanies bronchiolitis, antipyretics such as acetaminophen and ibuprofen are commonly used. Bronchiolitis is characterized by wheezing. A normal respiratory rate for an 18-month-old is 20-30 breaths/minute. Bronchodilators, especially nebulized, and inhaled/oral steroids are commonly employed to decrease respiratory effort. However, these interventions lack proven benefit, increase the cost of care, and have many side effects. How should a 20-year-old college age student who presents with cough, night sweats, and weight loss be screened for TB? (A TB skin test) Screening for TB in this patient should take place with a skin test known as the Mantoux. A chest X-ray is typically performed after a positive skin test. A sputum specimen is used for diagnosis, not screening. A questionnaire is used for screening patients who have had a history of a positive TB skin test. If symptoms are acknowledged on the questionnaire, a chest X-ray may be performed. The questionnaire is used to prevent inappropriate exposure to radiation in patients in whom regular screening is required, like healthcare providers. An example of a short-acting beta agonist is: (levalbuterol) An example of a short-acting beta agonist is albuterol or levalbuterol. These provide rapid dilation of the bronchioles and can give immediate relief for shortness of breath; hence the term for this class of medications: rescue medications. Salmeterol is a long-acting beta agonist. These should never be used without an inhaled steroid to treat a patient with asthma. Mometasone and beclomethasone are steroids commonly used to treat patients with asthma. A patient with asthma uses one puff twice daily of fluticasone and has an albuterol inhaler for PRN use. He requests a refill on his albuterol inhaler. His last prescription was filled 5 weeks ago. What action by the NP is appropriate? (Increase the dose of the inhaled steroid, refill the albuterol) The patient is using his short-acting bronchodilator excessively if he needs a refill of his inhaler in only 5 weeks. Inhalers typically contain 200 puffs. They should be used two or fewer times per week. His inhaled steroid dose should be increased and his albuterol inhaler should be refilled. In fact, he should not be without a prescription for the albuterol. Consideration could be given to prescribing a long-acting bronchodilator and increasing the steroid, but this is not the best choice because this does not include a refill of the albuterol and this patient cannot be without access to a rescue inhaler. Patients with asthma: (can cough or wheeze) The second leading cause of cough in adults is asthma. Cough due to asthma is often accompanied by episodic wheezing or dyspnea, though some patients with asthma only cough. This is termed “cough variant asthma.” The clinical presentation of asthma varies but hyper-responsiveness of the airways is a typical finding. A 26-year-old being treated for community-acquired pneumonia (CAP) has been taking azithromycin (standard dose) in therapeutic doses for 72 hours. His temperature has gone from 102° F to 101° F. What should be done? (Stop azithromycin and initiate a respiratory quinolone) A 26-year-old with CAP should show improvement in symptoms in 24-48 hours if he is on appropriate antibiotic therapy. Azithromycin treats atypical pathogens like Mycoplasma and Chlamydophila, but, has poor Streptococcus coverage. The most likely pathogen in this age group that causes pneumonia is an atypical pathogen, but at this point the most common typical pathogen, Streptococcus pneumoniae, must be considered. The best choice is to consider Streptococcus pneumoniae as the pathogen and treat with a respiratory quinolone. Specifically, this patient should receive a respiratory quinolone because of the increased incidence of resistant Streptococcus pneumoniae (DRSP). A 60-year-old patient newly diagnosed with COPD presents to your office. He would like to get the influenza immunization. He has no evidence of having had the pneumococcal immunization. What statement is correct? (He should receive both influenza and pneumococcal immunizations today) This patient has COPD. He should receive the pneumococcal immunization today. He belongs to a group of patients with chronic illness who are between the ages of 19 and 64 years and so, should be immunized for pneumonia. The flu immunization should be given to him annually. Which of the following is NOT part of the differential for a patient who complains of cough? (Obesity) All of the other conditions listed, heart failure, GERD, and asthma, are associated with cough. Obesity does not produce cough and is not associated with cough. A 65-year-old has been diagnosed with asthma. Older patients who have newly diagnosed asthma: (are more likely to cough) Asthma is usually diagnosed in children or young adults. Diagnosis after age 65 years is unusual, but 5-10% of newly diagnosed asthma patients are part of this age group. The most common presentation is cough, not wheezing. Exacerbations are much less variable than in younger adults. This is often initially misdiagnosed because the patient presents with symptoms that seem more like heart failure or COPD. A 67-year-old patient with COPD presents an immunization record that reflects having last received the pneumococcal immunization (PPSV23) when he was 60 years old. Which statement below reflects the current standard of practice recommended by CDC for this patient? (He should be vaccinated today with PCV13) The recommendation by CDC is pneumococcal immunization once at age 65 years regardless of other diseases present. However, if the initial immunization was given prior to age 65 years and 5 years has elapsed since the initial one, he should be revaccinated today. Two immunizations are available, PCV13 and PPSV23. He needs both, but PCV13 should be administered today. PPSV23 should be administered at least 1 year later. A 24-year-old college student who does not smoke is diagnosed with pneumonia. He is otherwise healthy and does not need hospitalization at this time. What antibiotic represents the best choice for treatment for him? (Clarithromycin) A macrolide (like azithromycin or clarithromycin) or a tetracycline (like doxycycline) is used for initial treatment of uncomplicated pneumonia in outpatients who are otherwise healthy and have not had recent antibiotic exposure. These agents are chosen because they cover atypical pathogens (the organism most likely to have infected him) and provide coverage against nondrug-resistant forms of Streptococcus. Fluoroquinolones are commonly used first line in these patients. However, guidelines strongly recommend using fluoroquinolones for patients with comorbidities and/or those who have suspected macrolide resistant strains of Streptococcus. Inappropriate use of fluoroquinolones will promote development of fluoroquinolone-resistant pathogens. What does a peak flow meter measure? (Expiratory flow) A peak flow meter measures peak expiratory flow; that is, air flow out of a patient’s lungs. Peak flow is sensitive to changes in the respiratory tubules and so reflects narrowing of the airways. The utility of a peak flow meter is especially important for patients with asthma because of the rapid changes that occur prior to the onset of an asthma exacerbation. There is minimal to no benefit of measuring these airway changes in patients with COPD and pneumonia. The major laboratory abnormality noted in patients who have pneumococcal pneumonia is: (leukocytosis) An increased white count is typical in patients with bacterial pneumonia such as pneumococcal pneumonia. Eosinophils can be increased in patients who develop pneumonia secondary to exposure to a very irritating substance like a toxic gas. Gram stain can demonstrate gram-positive or negative pathogens. Leukopenia is an ominous finding, especially in older patients. This indicates a poor prognosis because it means that the immune system is not responding to a potentially fatal pathogen. Which drug class is never used to treat chronic obstructive pulmonary disease (COPD)? (Leukotriene blockers) There is no data to suggest efficacy in treating COPD patients with leukotriene blockers like zafirlukast or montelukast. A long-acting bronchodilator (used twice daily) like salmeterol is commonly used. The long-acting anticholinergic medication tiotropium can be used once daily. Systemic steroids may be used for exacerbations of COPD. A patient who has asthma presents with chest tightness, wheezing, coughing, and fever. He has wheezing and diminished breath sounds in the upper right lobe. His cough is non-productive, and he denies nasal symptoms. Which symptom is most likely related to pneumonia? (Fever) The presence of fever should trigger the practitioner to consider pneumonia. The other symptoms are most likely secondary to asthma. Coughing may be due to asthma and pneumonia. A patient with COPD has been using albuterol with good relief for shortness of breath. He is using it 3-4 times daily over the past 4 weeks. How should the NP manage this? (Add a long-acting beta agonist) The patient is using albuterol too frequently. It should be used no more than twice weekly because it will lose its effectiveness over time (tachyphylaxis). Albuterol should be used as a rescue medication only. This patient’s medication regimen needs adjusting. The best choice is to consider adding a long-acting beta agonist (or long acting inhaled anticholinergic) and have him use albuterol as a rescue medication only. Which of the following may be used to diagnose COPD? (Pulmonary function tests or spirometry) Spirometry or pulmonary function tests (PFTs) are essential to diagnose COPD. The most important measures are the FEV1 (forced expiratory volume in one second) and FVC (forced vital capacity). Chest radiograph has a poor sensitivity in diagnosing COPD. Only about half of patients with moderately severe COPD can be diagnosed using chest radiography alone. CT scan is able to identify emphysema, but not chronic bronchitis. Arterial blood gases demonstrate hypoxia, but a specific cause is not able to be determined from this test alone. A patient with acute bronchitis was diagnosed at an urgent care center 10 days ago. He reports that he received an antitussive for nighttime cough, a steroid injection and oral steroids, and an antibiotic. Which of these interventions was of greatest benefit in resolution of his symptoms? (None of them) Acute bronchitis is almost always due to a viral infection. The antibiotic had no effect in symptom resolution. Unfortunately, antibiotics are commonly given for acute bronchitis. There is no evidence to support use of steroids as they do not result in quicker resolution of symptoms than placebo. In fact, multiple studies have failed to demonstrate benefit. Time is of greatest benefit in resolution of acute bronchitis symptoms. A 65-year-old patient has COPD. She receives a prescription for an albuterol inhaler. What medication information should be provided to this patient? (This may cause tachycardia) An example of an inhaled beta agonist is albuterol or levalbuterol. These agents stimulate the beta receptors in the lungs and in the heart. This helps the patient breathe better because it produces bronchodilation, but it potentially can produce arrhythmias or angina because beta receptors in the heart can become stimulated too. The dose for a patient with underlying cardiac problems is half the dose (and used with caution). Common side effects of these agents are jitteriness, tremor, nervousness, and potentially hypokalemia if used on a regular basis. A patient presents with symptoms of influenza during influenza season. He has not received the immunization against influenza. What should be used to help diagnose influenza in him? (A nasal swab) Influenza is diagnosed based on the results of a flu swab and the patient’s clinical presentation. A patient with influenza usually demonstrates influenza A (the most predominant strain during an outbreak) or influenza B (the strain identified occasionally during flu season but more often, throughout the rest of the year) if he is infected. The most common cause of pneumonia in people of all ages is: (S. pneumonia) Streptococcus pneumoniae (S. pneumo) is the most common pathogen in community-acquired pneumonia (CAP) worldwide. It is more common in age extremes (the very young and very old) and during winter months. Group A Strep can cause a fulminant pneumonia even in patients who are immunocompetent. Mycoplasma is the most common atypical pathogen that causes pneumonia. Staphylococcus pneumonia is more common postinfluenza in the very young and very old. A patient recently received levofloxacin for 7 days to treat pneumonia. His respiratory symptoms have resolved, but today he calls the office. He reports having severe watery diarrhea, abdominal cramping, and low-grade fever. What should be done? (Order a stool specimen) This history of recent antibiotic exposure suggests C. difficile. A stool specimen should be ordered to assess for infection with C. difficile. Some clinicians will initiate treatment for C. difficile based on this history, especially if the patient’s symptoms are severe or the patient is elderly/debilitated. A 20-year-old college age student has a positive TB skin test. Which choice listed below provides definitive diagnosis of tuberculosis? (A sputum specimen) Screening for TB is performed with a skin test known as the Mantoux. A chest X-ray is typically performed after a positive skin test, but is not diagnostic since TB can affect organs other than the lungs. A sputum specimen is used for definitive diagnosis. A questionnaire is used for screening patients who have had a history of a positive TB skin test. If symptoms are acknowledged on the questionnaire, generally, a chest X-ray is performed. The questionnaire is used to prevent too frequent exposure to radiation in patients in whom regular screening is required, like healthcare providers. A patient has cough, pharyngitis, nasal discharge, and fever. He has been diagnosed with acute bronchitis. Which symptom is least likely in the first 3 days of this illness? (Cough) Cough is the most common symptom associated with acute bronchitis and almost always appears after day 3 of the illness. In the first few days of acute bronchitis, upper respiratory symptoms predominate. In fact, it may be impossible to distinguish upper respiratory infection from acute bronchitis. Pharyngitis and nasal discharge/congestion are common on days 1-3. Acute bronchitis is suggested when cough lasts longer than 5 days. Fever is a relatively uncommon symptom of acute bronchitis. When fever appears along with cough, pneumonia should be strongly considered. Which of the following characteristics is always present in a patient with COPD? (Obstructed airways) COPD, chronic obstructive pulmonary disease, is characterized by obstructed airways. The obstruction is NOT completely reversible even with medication use. Productive cough is likely present in patients with chronic bronchitis but not necessarily emphysema. Shortness of breath does not have to be present (or perceived in patients with COPD). Hypercapnia is more prevalent in patients with emphysema since air trapping occurs. “Good control” of asthma is measured by the number of times weekly a patient uses a rescue inhaler. What choice below indicates “good control”? (Once weekly) Good asthma management is characterized by using short-acting bronchodilators (rescue medication) no more than twice weekly during daytime or twice monthly at nighttime. Using short-acting inhaled bronchodilators 2 times weekly necessitates use of prophylactic medications such as inhaled steroids and possible use of long-acting bronchodilators in conjunction with inhaled steroids. Mr. Smith has smoked for 45 years. Which of the following medications may worsen one of his diseases? (Propanolol) Propanolol is a nonselective beta blocker and might be potentially more harmful in a patient who has COPD than a cardioselective beta blocker. Metoprolol is a cardioselective beta blocker. Typically, cardioselective beta blockers exert their effect on the beta receptors in the heart, but not always. Sometimes there is effect on the beta receptors in the lungs. This could produce shortness of breath and would be described as a drug-disease interaction. Noncardioselective beta blockers like propanolol have a worse effect than cardioselective ones. In any event, beta blocker use should be avoided or used with caution in patients who have lower airway disease. The most common sequela of influenza in older adults is: (Pneumonia) More than 90% of deaths associated with influenza occur in older adults. Pneumonia is the most common cause of death and most common reason for hospital admission in older patients with influenza. Annual influenza immunization is recommended for all adults in the United States. A healthy 7-year-old child is diagnosed with atypical pneumonia. He is febrile but not in distress. What is the preferred treatment for him? (Azithromycin) In this age group (> 5 years), the most common atypical pathogens are Mycoplasma or Chlamydophila. Therefore, a macrolide antibiotic like azithromycin is the preferred agent. It is usually chosen first for its coverage of atypical pathogens. Doxycycline is not an appropriate choice because it is contraindicated in children younger than 8 years, however, it does provide coverage against the atypical pathogens. Amoxicillin provides no coverage of atypical pathogens and so it is a poor choice. A 30-year-old patient with intermittent asthma is using his “rescue” medication once daily. How should this be managed? He should receive a prescription for a(n): (an inhaled steroid) The patient is using his bronchodilator (“rescue” medication) more than twice weekly. This is a signal to the healthcare provider that the patient’s asthma is not well controlled and another medication needs to be used. The next step for this patient is a trial of an inhaled steroid. This should relieve his symptoms and decrease the use of his rescue medication. If an inhaled bronchodilator is overused, it will not continue to produce bronchodilation over time. Which choice below most appropriately differentiates acute bronchitis from pneumonia in a patient who has a productive cough? (Chest X-ray) Nearly all cases of pneumonia can be identified on chest X-ray by the presence of infiltrates. Patients with bronchitis have a normal chest X-ray unless there are other underlying pathologies. CBCs help distinguish bacterial from viral infections. Fever is not used to differentiate acute bronchitis from pneumonia. Sputum specimens are indicated when there is a need to identify organisms in the sputum. The most common cause of pneumonia in an otherwise healthy 3-year-old child is: (a viral infection) In children who are 6 months to 5 years of age, the most common cause of pneumonia is a viral pathogen. Rarely are studies performed to identify viral pathogens, however one of the most common viral pathogens is respiratory syncytial virus (RSV). S. pneumoniae is a common cause of pneumonia in very young children, it is also implicated in older adults as a causative agent in pneumonia. In young and middle adults, Mycoplasma is a common pathogen. Which medication below should be avoided in a patient with stage 3 COPD? (Cough suppressant with codeine) Codeine should be avoided (or used with extreme caution) because the sedative effect of codeine or any narcotic can potentially worsen respiratory depression and worsen hypercapnia. A patient with acute bronchitis and cough for 5 days calls to report that his cough is productive of discolored sputum. He has no other new symptoms. How should the nurse practitioner manage this? (Continue the original plan of care) This is the typical course of acute bronchitis. Acute bronchitis is characterized by cough lasting greater than 5 days, but usually less than 20 days. More than 50% of patients report discolored sputum. Since the overwhelming majority of cases of acute bronchitis are secondary to viral causes, antibiotics are not indicated. Discolored sputum is related to sloughing of epithelial cells and is the reason for the discoloration. Discolored sputum does not indicate bacterial infection. The CDC recommends treating acute bronchitis with antibiotics ONLY when the etiology is pertussis. In all other cases, the patient should be treated with supportive and symptomatic management only. A patient has received a prescription for lisinopril. Which side effect most commonly occurs with this medication? (Dry cough) A common side effect of ACE inhibitors is dry cough. Though estimates vary, 5-20% of patients who receive ACE inhibitors develop a cough. Angiotensin converting enzyme is believed to be responsible for metabolism of bradykinin in the lungs. Bradykinin is thought to be responsible for the cough because it induces production of arachidonic acid metabolites and nitric oxide. These substances may promote cough. The cough associated with ACE inhibitors appears to be a class effect. A 24-year-old presents with fever, rhinorrhea, and paroxysmal, high-pitched cough. This is: (Pertussis) Pertussis is also called “whooping cough.” This is a highly communicable respiratory disease caused by Bordetella pertussis. There are three recognized stages of pertussis: the catarrhal phase, the paroxysmal phase, and convalescence. More adults than children have contracted pertussis in the last decade. Since the outbreak of pertussis in Iowa in 2005, diminished titers were recognized and adolescents are being given a booster with TdaP at 11-12 years of age. A 60-year-old patient reports chronic cough and sputum production. He has a long history of exposure to secondhand cigarette smoke from his wife. What diagnosis is most likely? (COPD) This patient’s exposure to secondhand cigarette smoke from his wife represents a risk factor for COPD even though this patient does not smoke. COPD must be considered in anyone with a history of chronic cough and sputum production, dyspnea at rest or exertion, and history of exposure to tobacco smoke. A patient is diagnosed with asthma. Which question is most important to ask when deciding on medication management? (How often do your symptoms occur?) Diagnosis of asthma, as well as pharmacologic management of asthma, is based on frequency of occurrence of symptoms (wheezing, shortness of breath, cough, etc.). Bronchodilators, both short and long-acting, and inhaled steroids, represent the cornerstone of management of most patients who have asthma. Not all patients with asthma wheeze, therefore, asking that question might not be of great help. Severity of symptoms is subjective. Smoking cessation is important, but not a determinant in selecting medications for asthma management. Breath sounds auscultated over the periphery of the lung fields are quiet and wispy during the inspiratory phase followed by a short, almost silent expiratory phase. These breath sounds are considered: (Vesicular) The three normal breath sounds are vesicular, bronchovesicular, and bronchial. Vesicular breath sounds consist of a quiet, wispy inspiratory phase followed by a short, almost silent expiratory phase. They are heard over the periphery of the lung fields. Bronchial breath sounds consist of a full inspiratory and expiratory phase with the inspiratory phase usually being louder. They are normally heard over the trachea and larynx. Bronchovesicular breath sounds consist of a full inspiratory phase with a shortened and softer expiratory phase. They are normally heard over the hilar region. Crackles are adventitious sounds heard in the lungs and may be due to abnormalities in the lungs. GI The two tests that can indicate current infection with hepatitis B are: (presence of hepatitis B surface antigen and IgM) The earliest serologic marker that indicates acute hepatitis B infection is the presence of hepatitis B surface antigen. It becomes positive about 1-10 weeks after infection, but usually before symptom onset. A positive IgM indicates current infection. The presence of hepatitis B core antibody identifies hepatitis B infection (present or past) with certainty. It does not indicate timing of infection. A mother of a 4-week-old infant visits your office. She states that her baby is vomiting after feeding and then cries as if he is hungry again. What should the nurse practitioner assess? (His abdomen for an olive shaped mass) The symptoms likely reflect pyloric stenosis. The most common time for this to occur is 3-6 weeks. It rarely occurs after 12 weeks of age. Babies who have episodes of projectile vomiting and who demand to be refed are called “hungry vomiters” and a diagnosis of pyloric stenosis should be considered. The olive-shaped mass, if found, probably represents hypertrophy of the lateral edge of the rectus abdominus muscle. It is most easily felt immediately after vomiting. This diagnosis is made much earlier now than it used to be, so problems with dehydration are not as common as decades ago. A patient has the following laboratory value. (anti-HAV IgG: positive). What is the clinical interpretation? (He has immunity to hepatitis A) This patient is immune to hepatitis because he has a positive immunoglobulin G (IgG). This signifies immunity secondary to: (1) past infection, or (2) immunization. A negative IgG signifies absence of immunity to hepatitis A and susceptibility if exposed. The early signs and symptoms of appendicitis in an adult: (are subtle) The most consistent findings in adults with early presentation of acute appendicitis are subtle and difficult to identify. Symptoms may be as vague as indigestion, flatulence, and a feeling of ill-being. Initially, pain can be in the general abdomen, then become periumbilical, and finally localize to the lower right quadrant. Early symptoms are difficult to identify, especially in older adults. A 70-year-old presents to the nurse practitioner’s office for a well exam today. What medication probably has no effect on screening for occult blood in the stool? (Acetaminophen) The exam for occult blood is a screen for colorectal cancer. Aspirin, clopidogrel, NSAIDs, warfarin all decrease the positive predictive value of the test because they all can exacerbate bleeding if it is occurring in the colon secondary to a polyp or tumor. Ideally, the medications mentioned (except acetaminophen) would be stopped prior to the exam to increase the likelihood of test sensitivity, but this is not always possible. Symptoms of uncomplicated reflux disease in older adults should be treated: (with empiric treatment) In older patients without signs of complicated GERD (choking, cough, shortness of breath, pain with swallowing or in the chest), empiric treatment is appropriate. Empiric treatment can take place using proton pump inhibitors or H2 blockers. If H2 blockers are used, famotidine and nizatidine are preferred because of their efficacy and low risk of drug-drug interactions. If symptoms of GERD persist despite initial treatment, or if symptoms are severe, patients should have testing to rule out esophageal cancer, Barrett’s esophagitis, or other conditions of the esophagus and throat. Which symptom is INCONSISTENT with irritable bowel syndrome in older adults? (Onset after 50 years of age) Irritable bowel syndrome (IBS) is common in adults and lasts into older adulthood, but symptoms start prior to age 50 years. Typical symptoms of IBS are diarrhea and constipation intermittently, abdominal pain (one of the criteria for diagnosis), and bloating. Other symptoms that are inconsistent with IBS are associated weight loss, blood in the stool, rectal bleeding, and nocturnal diarrhea. These are more indicative of inflammatory disease or carcinoma of the bowel. A 20-year-old female patient presents with tenderness at McBurney’s point. Appendicitis is considered. What laboratory test should be done initially to determine the etiology of this patient’s abdominal pain? (Serum pregnancy test) A serum pregnancy test should be performed since this patient could have an ectopic pregnancy. Once pregnancy is ruled out, other etiologies can be evaluated. CBC with an elevated white count may indicate that an infection is present. It does not indicate a specific location of the infection. Urinalysis could help determine if the etiology is a urinary tract infection. Symptoms can mimic an appendicitis. Positive vaginal swabs could indicate pelvic inflammatory disease as the cause of the pain. A patient with a suspected inguinal hernia should be examined: (standing) The patient should be examined while he is standing. He should be asked to bear down, cough, or strain during the exam. Though hernias are far more common in males, they can be found in females too. In males, the patient should be asked to stand. The examiner should put his 2nd or 3rd finger through the scrotum and into the external ring. When the patient is asked to cough, a “silky” feel will butt up against the examiner’s finger, and the hernia can be easily felt. A healthcare provider (“the HCP”) was stuck with a needle from a patient suspected to be infected with HIV (“the patient”). A rapid HIV test was performed on the patient and found to be positive. This means that: (the HIV status of the patient requires further testing) The rapid HIV is always performed on the source patient (“the patient”). It is known as an ELISA (enzyme linked immunosorbent assay). In the patient suspected of being HIV positive, it is performed to establish whether or not he was positive at the time of the needle stick. In this case, it was found to be positive, but, this is a screening test, and false positives can occur. Therefore, a confirmatory test, the western blot, is routinely performed on the patient’s specimen to confirm the findings of the ELISA. The healthcare provider will usually be tested with a rapid HIV but it is done to establish HIV status at the time of the needlestick. The results of a rapid test can be performed in less than 20 minutes. A patient has had right upper quadrant pain that has lasted for the past 3 days, but the pain has become acute in the past 12 hours. He has low-grade fever. Which lab test(s) will be elevated if he has pancreatitis? (Serum amylase) Serum amylase levels begin to rise 6-12 hours after pancreatic insult and remain elevated for 3-5 days. The other tests described may be abnormal but are not specific for pancreatitis. A patient presents with complaints of bright red stools over the past week. This symptom could be consistent with: (cancer of the sigmoid colon) Bright red blood in the stools is more characteristic of left-sided colon cancer (descending and sigmoid colon) or rectal hemorrhoids. If blood occurs in the stool in right-sided colon cancers (ascending colon) or gastric ulcers, the stool will be black and tarry. A 24-year-old female presents with pain and tenderness in the right lower abdominal quadrant. Her pelvic exam and urinalysis are within normal limits. Her WBC is elevated and her urine pregnancy test is negative. What is part of the differential diagnosis? (Appendicitis) A CBC with a mild elevation in white cell count indicates that infection is likely. This finding is present in most patients who have acute appendicitis. Right lower quadrant abdominal pain, anorexia, and nausea/vomiting are considered classic symptoms of acute appendicitis. Pelvic inflammatory disease is characterized by cervical motion and adnexal tenderness on bimanual examination. Purulent endocervical discharge may be present. This is unlikely in the presence of a normal pelvic exam. Acute pelvic pain and a positive pregnancy test in women of childbearing age may suggest ectopic pregnancy. The patient’s pregnancy test is negative. Symptoms of a urinary tract infection (UTI) can mimic appendicitis, but this can be ruled out with the patient’s normal urinalysis report. What medication used to treat patients who have GERD provides the fastest relief of heartburn symptoms? (Calcium carbonate) Calcium carbonate is an antacid. It provides rapid changes in gastric pH. This provides relief that can be noticed immediately. The increase in pH lasts for about 30 minutes and corresponds with resolution of symptoms. However, as pH decreases within 30 minutes, symptoms may return. Ranitidine is an H2 blocker. It provides relief in 1-2 hours. This usually lasts for about 6-12 hours. Amantadine is an antiviral not used to treat GERD. Pantoprazole is a proton pump inhibitor. This provides relief after several hours or days of daily consumption. A patient with gall bladder disease has classic symptoms. Which symptom below is NOT classic of gallbladder disease? (Pain that occurs when the stomach empties) The pain associated with cholecystitis is usually constant and may or may not occur in relation to meals, but it rarely occurs after the stomach has emptied (takes several hours) or with fasting. Initial pain is usual after a fatty meal. The pain is usually in the upper right quadrant but is nearly as common in the mid abdomen. The pain can mimic a myocardial infarction and so it must be treated as cardiac pain until proven otherwise. The pain is usually caused by contraction of the gallbladder after a meal. The contraction may force a stone or sludge against the gallbladder outlet. Discomfort can last for several hours. Most patients who have acute hepatitis B infection: (have varied clinical presentations) Most patients with hepatitis B (70%) have subclinical hepatitis. Development of cirrhosis is rare following hepatitis B infection unless other systemic factors are present, such as ethanol abuse, HIV infection, hepatitis C infection, etc. There is no predilection for this disease by gender. When patients are symptomatic, they typically develop nausea, jaundice, and flu-like symptoms with fever, body aches, and fatigue. A patient has been diagnosed with hepatitis A. The most common reported risk factor is: (international travel) Traveling internationally is the most common risk factor. Hepatitis A (HAV) is spread via the fecal-oral route (and is highly contagious), though most people have no recollection of eating or drinking contaminated food/drink. Mexico, Central and South America are countries with the highest reported rates of HAV. Other risk factors are contact with infected family or close contacts and homosexual activity among men. Hepatitis A has declined since vaccination in the US has become widespread. A 6-week-old male infant is brought to the nurse practitioner because of vomiting. The mother describes vomiting after feeding and feeling a “knot” in his abdomen especially after he vomits. The child appears adequately nourished. What is the likely etiology? (Pyloric Stenosis) This scenario is typical of an infant with pyloric stenosis. It is more common in males (88%) and usually is diagnosed before the child is 12 weeks old. The classic presentation is an infant who vomits immediately after eating. The “knot” in the abdomen is the typical “olive-shaped mass” palpable at the lateral edge of the rectus abdominus muscle in the right upper quadrant of the abdomen. The mass is best palpated immediately after vomiting. The differential should include GER, but no mass is palpable. Munchausen syndrome by proxy is the fabrication or induction of an illness in a child in order for the caregiver to receive attention. Which of the following is NOT a risk factor for developing hepatitis B? (Consuming contaminated water) Hepatitis B can be contracted by any of the choices listed except drinking contaminated water. Drinking contaminated water increases the risk of hepatitis A. An 83-year-old patient is diagnosed with diverticulitis. The most common complaint is: (left lower quadrant pain) Diverticular disease is more common in older adults. About 70% of patients diagnosed with diverticulitis have left lower quadrant pain. Rectal bleeding may have varied etiologies, such as rectal carcinoma or hemorrhoids. Bloating and cramping are often found in patients with diverticular disease (diverticulosis) but not specifically diverticulitis. Belching and flatulence are not specifically associated with diverticulosis. Which medication listed below can exacerbate the symptoms of GERD? (Verapamil) Verapamil is a calcium channel blocker. Calcium is needed for muscle contraction. Since the lower esophageal sphincter is opened and closed by muscles, the contraction of these muscles will be less forceful. GERD can be exacerbated in this case. Calcium channel blockers should be avoided in patients with severe GERD or in patients in whom calcium channel blockers exacerbate GERD symptoms. Choose the number on the image that most closely approximates the location of a direct inguinal hernia.(Above pubic bone) Hesselbach’s triangle is the area through which direct inguinal hernias occur. The boundaries of Hesselbach’s triangle are formed by the inguinal ligament, the rectus abdominis muscle, and the epigastric vein and artery. Weakness in the floor of the inguinal canal results in the protrusion of direct inguinal hernias. This weakness is commonly the result of connective tissue abnormalities, but may occur due to a deficiency in the musculature of the abdomen from chronic over-stretching or injury. A 70-year-old patient states that he had some bright red blood on the toilet tissue this morning after a bowel movement. He denies pain. What is the LEAST likely cause in this patient? (Anal fissure) Nearly 1 in 3 patients in this age group with acute lower gastrointestinal bleeding have bleeding secondary to diverticulitis. Nearly 1 in 5 have colorectal cancer or polyps, though, polyps usually do not bleed. Patients who have anal fissures often complain of a tearing pain during bowel movements. Regardless of the etiology, this patient needs referral for a colonoscopy to identify the cause of bleeding. He is at high risk for colon cancer because of his age. The appropriate recommendation is referral to gastroenterology for colonoscopy. GERD (gastroesophageal reflux disease) and physiologic reflux have similar characteristics. However, physiologic reflux: (rarely occurs at nighttime) GERD is usually associated with symptoms that produce injury to the mucosa. This rarely occurs in physiologic reflux. Characteristics typical of physiologic reflux are that it occurs primarily postprandial (like GERD), is usually asymptomatic, rarely occurs nocturnally, and is usually short-lived. In contrast, GERD usually occurs nocturnally, especially when there is lower esophageal sphincter disease. A 56-year-old male patient has been diagnosed with an inguinal hernia. What symptom would make the nurse practitioner suspect an incarcerated hernia? (Pain) A hernia is a weakened area in the muscle where loop of bowel protrudes through the abdominal wall. Normally, hernias are not frankly painful, though they may be tender. A painful hernia should be suspected as one that has become incarcerated or strangulated. Incarceration means that the hernia cannot be reduced; it is trapped. A strangulated hernia means that it is incarcerated and ischemia is present. A strangulated hernia is a surgical emergency. Emergency surgery should be performed within 4-6 hours to prevent loss of bowel. Dilated scrotal veins should cause the examiner to consider varicocele. A 48-year-old patient has the following laboratory values. (anti-HCV: reactive, HCV RNA: detectable). How should they be interpreted? (The patient has hepatitis C) This patient has hepatitis C. He has a reactive HCV antibody (anti-HCV). This is a positive screen for hepatitis C. The HCV RNA level is detectable, which confirms infection. When both the anti-HCV and HCV RNA are positive, the patient can be diagnosed with hepatitis C. At this time, there is no immunization for hepatitis C. Choose the number on the image that most closely approximates the location of an indirect inguinal hernia? (Inguinal fold) The internal inguinal ring is the most common site for development of an indirect inguinal hernia. These can occur in men and women. Though most are probably congenital, symptoms may not be obvious until later in life. Indirect hernias are: more common on the right side. Direct inguinal hernias occur through Hesselbach’s triangle. A patient presents with right upper quadrant and upper abdominal pain. Acute cholecystitis is suspected because the pain radiates to the: (right scapula area) Acute cholecystitis presents with right upper quadrant and/or upper abdominal pain radiating to the right scapular area. The pain is usually steady and aching. Pain in the epigastric area could be associated with a peptic ulcer or dyspepsia. Cancer of the stomach presents with epigastric pain. Acute mechanical colon obstruction presents with pain in the lower abdomen. A 63-year-old male has been your patient for several years. He is a former smoker who takes simvastatin, ramipril, and an aspirin daily. His blood pressure and lipids are well controlled. He presents to your clinic with complaints of fatigue and “just not feeling well” for the last few days. His vital signs and exam are normal, but his liver enzymes are elevated. His hepatitis panel is negative for infectious hepatitis. What is the most likely cause of his elevated liver enzymes? (Daily grapefruit consumption for the past 10 days) Grapefruit is a potent inhibitor of the cytochrome P450 enzyme system. Statins and calcium channel blockers are two infamous drug interactions that occur with grapefruit and grapefruit juice. Because they inhibit metabolism of the statin, the patient continues to have statin in circulation because he cannot significantly metabolize the medication. When the next day’s dose is taken, its effect is coupled with the effect of the previous day’s dose. The effect is cumulative. Hepatoxicity can quickly develop. The simvastatin must be stopped immediately! The liver enzymes must be followed until they return to normal; which could take weeks, months or even longer. What is the simplest screen for nutritional adequacy in elderly patients? (Measure their weight) In older adults, serial weight is the simplest screen for assessment of nutritional adequacy. Weight loss in elderly patients is associated with greater mortality than weight maintenance. A 31-year-old patient is suspected of having hepatitis C. He reports possible exposure about a month ago. (anti-HCV: nonreactive, HCV RNA: not detectable).How should the nurse practitioner interpret his laboratory results? (The patient does not have hepatitis C) This patient does not have hepatitis C (HCV) infection. An HCV antibody test (anti-HCV) is recommended as the initial screen for infection. Development of detectable antibodies (anti-HCV) usually occurs between 2-6 months following exposure. The patient's HCV antibody test (anti-HCV) is nonreactive. Typically, subsequent evaluation to detect the presence of HCV RNA is not necessary following a nonreactive anti-HCV result. Because exposure occurred less than 6 months ago, he may lack detectible levels of anti-HCV antibodies, which warrants testing for HCV RNA. HCV RNA levels become detectible before reactive antibodies. HCV RNA was not detected in this patient. This confirms that this patient has a true negative screen for infection with HCV. A patient has been diagnosed with viral gastroenteritis. He has nausea and vomiting, and has started having lower abdominal cramps. What is the most effective intervention for him? (Oral rehydration) Patients with viral gastroenteritis should be treated symptomatically. The goal of therapy is to prevent dehydration and replace electrolyte losses. Antidiarrheals, antispasmodics, and antiemetics can decrease nausea, vomiting, abdominal cramping and symptoms of diarrhea, but should be used with extreme caution when given to older adults or children younger than 5 years of age. Clinical judgment should dictate when it is prudent to initiate these agents. A 35-year-old patient has the following laboratory values. How should they be interpreted? (HBsAG: negative, Anti-HBc: negative, Anti-HBs: negative)(The patient should consider Hepatitis B immunization) This patient has a negative hepatitis B surface antigen (HBsAg). Therefore, he does not have hepatitis B. The patient has a negative hepatitis B core antibody (anti-HBc). Therefore, he has never had hepatitis B. The patient has a negative hepatitis B surface antibody (anti-HBs). Therefore, he is not considered immune, and immunization should be considered. There is a remote possibility that this patient has been immunized but did not produce hepatitis B surface antibodies. If this were the case, he should consider immunization once again. An 85-year-old adult has chronic constipation. How should this be managed initially? (Avoid all constipating medications/foods when possible) Initially, all medications known to cause constipation should be stopped when possible. Symptoms should be reassessed. It is always preferable to stop a medication to correct a condition BEFORE adding a medication to correct a condition. If symptoms persist, a gradual increase in dietary fiber up to 25 grams daily should be added, along with increasing fluid intake. Physical activity should be increased as tolerated. Sorbitol solution and an oil retention enema could be initiated if other options mentioned were not helpful. Which is NOT an effective strategy for helping older adults gain weight? (Increase carbohydrate intake) When treating patients with weight loss, the goal is to increase the number of calories at each meal. Fats are more heavily laden with calories than carbohydrates. Carbohydrates (and proteins) provide only 4 calories per gram; fats provide 9 calories per gram. The addition of fats will increase calories much more quickly than increasing carbohydrate intake. All of the suggestions listed above will increase caloric intake. Daytime snacks should be offered too. Consider a vitamin B supplement because this can stimulate appetite. The relationship between duodenal ulcer disease and H. pylori infection is: (very likely) H. pylori is a gram-negative organism that is a major etiologic factor in development of duodenal ulcer disease, gastric adenocarcinoma and lymphoma of the stomach. Only about 10-15% of patients with H. pylori infection actually develop duodenal ulcer disease, but this is the largest contributor to duodenal ulcer development. Other etiologic factors in duodenal ulcer development are NSAID overuse and smoking. A 37-year-old has routine blood work performed during an annual exam. On exam he has a tender, enlarged liver. How should the nurse practitioner proceed? (Order a hepatitis panel) The differential for a patient with elevated liver enzymes can reflect many different etiologies. Since the liver is tender and liver enzymes are elevated, a likely etiology is hepatitis. The size and consistency of the liver should be ascertained. The spleen should be assessed. If it is palpable, it is enlarged also. Hepatitis panel should be performed and strong consideration given to referral to gastroenterology. Repeating liver enzymes might be considered if the rest of the exam was normal and the lab values were the only abnormal values. The results of a CBC will not change the differential. The patient’s abnormal labs and exam make this urgent, and waiting a week will delay diagnosis and possible treatment. A 19-year-old female presents with lower abdominal pain that began about 12 hours ago. She denies vaginal discharge. Which choice below is the least likely cause of her symptoms? (Renal stone) A renal stone can produce lower abdominal pain, but it is unlikely to produce fever. Low-grade fever might accompany appendicitis, UTI, or a ruptured ovarian cyst. Another diagnosis that must be considered because of her age is pelvic inflammatory disease. In this case, a pelvic exam should be performed. The most common place for indirect inguinal hernias to develop is: (the internal inguinal ring) The internal inguinal ring is the most common site for development of an indirect inguinal hernia. These can occur in men and women. Though most are probably congenital, symptoms may not be obvious until later in life. Indirect hernias are more common on the right side. Direct inguinal hernias occur through Hesselbach’s triangle. A 14 year-old male patient has an acute, painless groin swelling. Which tool would yield the most information to identify the etiology of the swelling?(Ultrasound of the scrotum) The patient has an acute swelling of the groin. Since the etiology could include several scrotal problems (inguinal hernia, hydrocele, or varicocele), an ultrasound will yield quick reliable information with a diagnostic accuracy of 93% for acute groin problems. The definitive treatment for inguinal hernia is surgical repair. Mrs. Lovely, an 84-year-old, complains of fecal incontinence. A likely cause is: (constipation) Underlying constipation is a common cause of fecal incontinence in older adults. However, typically it is multifactorial. Risk factors include: age > 80 years, impaired mobility, and neurologic disorders including dementia. Inactivity and poor fluid consumption may contribute to constipation but are not causes of fecal incontinence. A 40-year-old patient has the following laboratory values. How should they be interpreted? HBsAG: negative, anti-HBs: positive, anti-HBc: negative (The patient has been immunized) This patient has a negative hepatitis B surface antigen (HBsAg). Therefore, he does not have hepatitis B. The patient has a negative hepatitis B core antibody (anti-HBc). Therefore, he has never had hepatitis B. The patient has a positive hepatitis B surface antibody (anti-HBs). Therefore, he is considered i [Show More]
Last updated: 1 year ago
Preview 1 out of 73 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 31, 2020
Number of pages
73
Written in
Additional information
This document has been written for:
Uploaded
Jul 31, 2020
Downloads
0
Views
68







.png)
.png)