*NURSING > EXAM > CRIT 480 EXAM 1 Critical Care Practice Questions and Answers (RATED A+) Solutions | (100 out of 100) (All)
CRIT 480 EXAM 1 Critical Care Practice Questions and Answers (RATED A+) Solutions | (100 out of 100) | Download To Score An A
Document Content and Description Below
CRIT 480 EXAM 1 Critical Care Practice Questions and Answers A college heath nurse interprets the peak expiratory flow rate for a student who has asthma and fluids that student is in the yellow zon... e of his asthma action plan. The nurse should base her actions on which of the following information? (select all that apply.) a. The nurse should use his quick-relief inhaler b. The students asthma is not well controlled c. The students peek flow is 50% to 80% of his best peak flow d. The nurse should obtain a second expiratory flow rate A nurse is caring for a client who is receiving mechanical ventilation and has an ideal weight of 60 kg. The nurse should expect the tidal volume to be set at which of the following? a. 480 mL (The average tidal volume is 7-9 (60kg x 8ml/kg =480) A nurse in the PACU is assessing a client who has an endotracheal tube (ET) tube in place and observes the absence of left-sided chest wall expansion upon respiration. Which of the following complications should the nurse suspect? a. Movement of the ET into the right main bronchus. ( During intubation the staff can misplace the ET tube in the right stem bronchus. The nurse should identify absence of chest wall movement or breath sounds on a single sliding scale as indicating ET tube displacement, and should notify appropriate personnel to reposition the tube) A nurse is assessing the respiratory pattern of an older adult client who is receiving end of life care. Which of the following assessment findings should the nurse identify as Cheyne-stokes respirations? a. Breathing ranging from very deep to very shallow with periods of apnea. (The Cheyne-stokes respirations is an indication that the client is approaching death.) A nurse is caring for a client who is receiving mechanical ventilation via tracheostomy tube. The nurse should recognize that which of the following complications is associated with long-term mechanical ventilation? a. Stress ulcers (stress ulcers in clients who are receiving long-term mechanical ventilation are caused by elevated levels of hydrochloric acid in the stomach. Stress ulcers increase the risk for systemic infections and require pharmacological treatment.) A nurse is caring for a client following extubation of her endotracheal tube 10 min ago. Which of the followings should the nurse report to the provider immediately? a. Stridor A nurse in an emergency department is planning care for a client who has a flail chest on the right side following a MVA accident. Which of the following should the nurse plan to take? a. Prepare the client for positive pressure ventilation. (The nurse should prepare the client for positive pressure ventilation to promote lung expansion and stabilize the pressure within the clients chest. The nurse should also administer analgesics to alleviate pain while breathing to achieve lung re-expansion.) A nurse is suctioning the endotracheal tube of a client who is on a ventilator. The clients heart rate increases from 86/min to 110/min and becomes irregular. The nurse should know that the client requires? a. Pre-oxygination prior to suctioning. (Suctioning should be performed on the endotracheal tube of a client who is mechanically ventilated to remove accumulated secretions from the airways. Possible complications of the procedure includes hypoxemia (Manifested by tachycardia and arrhythmia) and tissue injury. An increased, irregular heart rate while suctioning is evidence that the client is becoming hypoxic. In preparation for suctioning, and to prevent hypoxemia the client should be pre-oxyginated with a manual resusotator bag set at 100% oxygen) A nurse is assessing a client immedietaly after the provider removes the clients endotracheal tube. Which of the following findings should the nurse report to the provider? a. Stridor Alternating periods of hyperventilation and apnea is Cheyne-stokes breathing. A nurse understands that there are three ways to decrease ventilator-assisted pneumonia called a “ventilator bundle”. Which of the following three nursing actions are included in the clients care bundle? a. Hand hygiene, oral care, and HOB elevation A nurse is caring for a client who has respiratory failure, is intubated, and is mechanically ventilated. The client pulls out the edotrachial tube. Which of the following is the priority action? a. Ensure the airway is open A nurse is assessing a clients wife how to take a blood pressure. Which of the following actions by the wife indicates a need for further instructions? a. Place the clients arm above the level of the heart A nurse is monitoring a post-operative client who is unable to respond to questions. Which of the following behviors should the nurse recognize as an indicator of pain? (select all) a. Resltlessness b. Grimacing c. Clenching A nurse is assisting with the discharge plan of a client who has a permanent tracheostomy. The nurse should verify the availability of which of the following equipment? (select all) a. Oxygen b. Suction machine c. Replacement canula A nurse is giving shift report using SBAR to the oncoming nurse on a client who has traumatic brain injury. When reporting information about the client, which of the following are included in the situation of SBAR? a. History of the injury SBAR examples: 1. Gaslow coma scales falls under assessment 2. Intercranial pressure readings falls under assessment 3. Medication that is needed falls under recommendations A nurse is monitoring the cardiac output of a client who has left sided heart failure using pulse pressure analysis. Which of the following findings can compromise the reading? a. The client is experiencing premature atrial contractions. A nurse in the ICU is providing teaching for a client proior to the removal of an endotracheal tube. Which of the following instructions should the nurse include in the teaching? a. Avoid speaking for long periods A nurse is caring for a client who has severe head injuries and is declared brain dead. The transplant coordinator has spoken with the clients family about organ donation. The clients spouce states she is confused and does not know what she should do. Which of the following responses by the nurse is appropriate? a. What do you think your spouse would have wants? A client is performing nasotrachial suctioning for a client who has COPD and an artificial airway. Which of the following actions should the nurse take? a. Preoxygenate the clients with 100% oxygen for up to 3 min. A charge nurse has access to the faciliteies electronic records. It is appropriate for the charge nurse to share her personal password with whom? a. No one A nurse is assessing a group of clients for hospice services. The nurse should recommend hospice care for which of the following clients? a. A client who has terminal cancer and needs assistance with pain management. A nurse is planning to delegate tasks to a LPN. Which of the following entitles is important for the nurse to understand when delegating to a LPN? a. The state nurse practice act A nurse receives a wrong medication. The nurse who made the medication error should take which of the following actions first? a. Assess the client A charge nurse is observing the actions of an assistive persoel (AP). Which of the following actions by the AP is appropriate? a. Logging off the computer after entering a clients intake and output A nurse is caring for a client 1 day postoperative who has developed atelectasis. Which of the following manifestations is an expected finding for this condition? a. Hypoxemia or cyanosis A nurse enters a clients room and finds the clients pulseless. The family has requested a DNR order from the provider, but he has not written the order yet. Which of the following actions should the nurse take first? a. Call the emergency response team A nurse is assessing a client for hypoxemia during an athsma attack. Which of the following manifestations should the nurse expect? a. Agitation A nurse is evaluating the CVP of a client who has sustained multiple traumas. Which of the following interpretations of a low CVP should the nurse make? a. Hypovolemia (A low cvp indicates right ventricular preload, which can be seen in clients who are experiencing hypovolemia, excessive blood loss, or overdiuressis) A nurse in the ICU is caring for a client who has heart failure and is receiving a dobutamine drip. The nurse should identify that which of the following findings indicates that the medication is effective? a. Increased urinary output (Doubtamine is administered to clients who have heart failure to improve their hemodynamic status.) A nurse in a ICU caring for a client who is post-op following a right pneumonectomy. After extubation from the ventilator. Which of the following positions should the client be placed? a. Semi-fowlers A nurse is preparing a client for transfer to the ICU for a placement of a pulmonary artery catheter. The nurse should explain to the client that this catheter is used to monitor which of the following conditions? a. Hemodynamic status A nurse is caring for a client who has a new diagnosis of CKD. Which of the following statements should the nurse identify as an indication of anticipatory grieving? a. I just cant believe that this dialysis is going to ruin my whole life. (Anger and fear of the upcoming loss) A nurse is caring for a client who is receiving positive-pressure mechanical ventilation. Which of the following interventions should the nurse implement to prevent complications? (select all) a. Elevate the hob 30 b. Administer pantoprazole as prescribed c. Reposition the endotracheal tube opposite of the mouth daily A nurse is caring for a client who has named a person to serve as his health care proxy. The client states he needs clarification about this type of advanced directives. Which of the following statements by the client indicates a need for clarification? A. I have to choose a family member as my health proxy. (the client needs to choose someone they can trust for end of life care, should be a family member, but doesn’t have to be a family member.) A nurse in the emergency department is caring for a client who has compression fracture of a spinal vertebra. During transport to the facility, the client was medicated with intravenous morphine. On arrival, the neurosurgeon determined determined urgent surgical intervention is indicated for the fracture. Staff members have been unable to reach the clients family. Which of the following actions should the nurse anticipate the neurosurgeon taking? a. Invoking implied consent A nurse is admitted to the emergency room with a respiratory rate of 7/min. ABG reveals the following values. Which of the following is an appropriate analysis of the ABG’s? a. Respiratory acidsis A nurse is caring for a female client in the ER who reports SOB and pain in the lung area. She states that she started taking birth control 3 weeks ago and that she smokes. (the question too long to type) a. Administer oxygen via face mask A nurse is planning care for a client who as acute respiratory distress syndrome ARDS. Which of the following should the nurse include in the plan? a. Place in prone position A nurse in a dialysis center caring for a client who has a new diagnosis of ESKD. When he arrives he tells the nurse I decided to come today, but “I am not sure if I need to come back after today.” (too long to type) a. Denial phase of grieving A nurse is caring for an older adult client who was alert and orientated at admission, but now seems increasingly restless and intermittently confused. Which of the following actions should the nurse take to address the clients safety needs? a. Move the client to a room closer to the nursing station A nurse is monitoring the pulomary artery wedge pressure PAWP for a client. The nurse should identify that a reading of 15 mm Hg is an identification of which of the following conditions? a. Mitral regurgitation ( hemodynamic monitoring allows the nurse to monitor the pressure within the heart and the great vessels. The PAWP reflects left atrial pressure.) A nurse is caring for a client who has meningitis, a temperature of 93.7 C (103.5F), and is prescribed a hypothermia blanket, while using this therapy the nurse must carefully observe for? a. Shivering A nurse in an ER is assessing a client who was bitten by on the left leg by a poisonous snake. The client has placed elastic bandages snuggly above and below the bite marks and is in no apparent distress. Which of the following actions should the nurse take? a. Obtain a prescription for the appropriate anti-venom A nurse enters a clients room and finds him unresponsive. After notifying the rapid response team, which of the following actions should the nurse take first? a. Check for a carotid pulse A nurse is caring for a client who is brought into the emergency department immediately following a snake bite to his forearm. The client suspects the snake to be venomous. Which of the following should the nurse take? a. Place the extremity in a dependent position A nurse in the ICU is caring for a client who has heart failure and is receiving a dobutamine drip. The nurse should identify that which of the following findings indicate that the medicine is effective? a. Increased urine output (shows their hemodynamic status is improved) A nurse enters an adult’s room and finds him unresponsive. After determining that the client is not breathing and does not have a pulse, which of the following actions should the nurse take first? a. Summon the code team A nurse is caring for a client who develops an airway obstruction from a foreign body but remains conscious. Which of the following actions should the nurse take first? a. Administer the abdominal thrust maneuver Life threatening emergency steps 1. Open airway using jaw maneuver 2. Determine effectiveness of ventilator 3. Establish IV access 4. Perform gaslows coma scale 5. Remove clothing for a thorough assessment A nurse is teaching a group of clients about emergency care for a snake bite. Which of the following information should the nurse include in the teaching? a. Immobilize the affected area with a splint A nurse is assessing a client while suctioning the client tracheostomy tube. Which of the following indicates the client is experiencing hypoxia? a. Increased heart rate If patient has an extubation from the ventilator place the client in semi-fowlers position. A nurse is receiving a transfer report from a client who has had a head injury. The client has a Gaslows Coma Scale score of 3 for opening eyes, 5 for best verbal response, and 5 for best motor response. Which of the following is a conclusion of this data? a. The client opens his eyes when spoken to A nurse is assessing a client who has a 8 gaslows coma scale to evaluate LOC. Which of the following statements accurately describes the score? a. Indicates the need for total nursing care A client with right ventricular has a central venous pressure monitoring catheter in place (CVP). The nurse should expect which of the CVP measurements? a. 7 mm HG (a CVP above 6 indicates a reduced right ventricular preload, typically from hypovolemia) A nurse is caring for a client who is immedietly postoperative following a thoracic surgery. The nurse administers a narcotic analgesic to the client frequently for pain. Which of the following should the nurse recognize as the primary reason for this action? a. It facilitates the clients deep breathing A nurse is in a cardiac care unit is caring for a client with acute heart failure. Which of the findings should the nurse expect? a. Elevated CVP pressure A nurse is caring for a client who has shallow rapid respirations, paradoxal pulse, CVP 4 cm H20, BP 90/50 mm Hg, skin cold and pale, and urinary output 55ml over the last 2 hours. From these findings, the nurse concludes that he may be developing which of the following? a. Hypovolemic shock A nurse in the emergency department is implementing a plan of care for a conscious patient who has a suspected cervical cord injury. Which of the following immediate interventions should the nurse implement? (select all) a. Assess adequacy of RR b. Obtain vitals c. Stabilize head and neck d. Assess for visceral damage A nurse is responding to a client who has esophageal varicies from portal hypertension. The client has IV fluids infusing and has a blood pressure of 68/48 after vomiting up 500ml of blood. Which of the following actions may the nurse plan to do first? a. Increase IV fluid rate A nurse in an urgent care center is assessing a client who reports a sudden onset of irregular palpitations, fatigue, and dizziness. The nurse finds a rapid and irregular heart rate with a significant pulse deficit. Which of the following dysrhythmias should the nurse expect to find on the ECG? a. Atrial fibrillation The nurse is caring for a client who just had cardiac catherization. The post procedure nursing care of plan for this client should include which of the following nursing interventions? a. Have the client rest in bed for 2-6 hours (Clients who had manual or mechanical pressure after catheter removal require 6hr of bed rest.) A nurse is caring for a client who has hypovolemic shock. Which of the following should the nurse expect? a. Oluguria A nurse is caring for a client who has quadriplegia from a spinal cord injury who reports having a “severe headache”. Upon assessment the nurse obtains a blood pressure reading of 210/108mm Hg. Suspecting that the client is experiencing autonomic dysresflexia. Which of the following actions should the nurse perform first? a. Place the client in high-fowlers position (this will help decrease the clients b/p) A nurse in an ICU unit is caring for a client with acute respiratory distress syndrome ARDS and is receiving mechanical venetaltion via and endotracheal tube. The provider plans to extubate her within the next 24 hours. Which of the following is an important criteria when extubating this client? a. Adequate tidal volume without positive pressure (typical weaning criteria include the ability to maintain adequate vital capacity, tidal volume, and minute ventilation without positive pressure or any othe manually assisted breaths) A nurse is dining at a restaurant when a woman begins to scream that her husband is choking. Which of the following should the nurse do first? a. Ask the victim can he speak Hypovolemic shock indication – HR suddently increases ex: ( goes from 88-110) A nurse enters an adult clients room and finds him unresponsive. After determining that the client is not breathing and does not have a pulse , which of the following actions should the nurse take first? a. Summon the code team A nurse is preparing home instructions for a client who has epilepsy. Which of the following should the nurse include in the teaching? a. Eat food high in fiber to have daily bowel movements Patient taking “LOL” beta blockers monitor blood pressure standing, sitting, lying BiPAP education is done by the respiratory therapist A nurse is assessing a clients wife on how to take a blood pressure. Indication for further teaching when she states? a. Place the clients arm above the level of the heart A nurse is assessing a client who has a urine output of 250ml in a 24 hour period. Which of the following terms should the nurse include in the documentation of the electronic medical record? a. Oliguria Comfort Care for a postoperative client (select all) a. Keep bed linens smooth b. Monitor TENS therapy c. Give back massage d. Teach relaxation techniques A nurse is monitoring cardiac output for a client who has left side HF using a pulse pressure analysis. Which of the followings can compromise this reading? a. The client is experiencing premature atrial contractions Teaching for removal of endotracheal tube a. Avoid speaking for long periods How does airway pressure release ventilation (APRV) work related to respiratory support? a. patient and ventilator work together breath expelled by the lung's own natural recoil How does PEEP work related to respiratory support? a. preset pressure on expiration added to treat persistent hypoxemia How does pressure support ventilation (PSV) work r/t respiratory support? a. greater oxygenation, makes the work of breathing easier, prevents alveolar collapse How do you document the placement of a tube for mechanical ventilation? a. in cm at the client's teeth or lips For an ET tube what should the cuff be set at? how often should you adjust the cuff pressure? a. 20 mm Hg q 8 h A nurse is caring whose arterial blood gas results show a pH of 7.3 and a PaCO2 of 50 mm Hg. The nurse correctly determines that the client has a. respiratory acidosis A nurse is planning care for a client who has a suspected myocardial infarction. Which of the following should the nurse administrator? a. Oxygen Airway Obstruction a. Tachycardia b. Retractions c. Restlessness Metabolic acidosis- below 7.35 Narcotics for pain facilitate deep breathing Client brought into the airway following MVA accident priority is airway Breath sounds determine left side heart failure If nurse suspects anaphylaxis when giving an antibiotic priority- count RR rate Occupational therapist- assist with self-care, fine-motor skills, coordination, Physical Therapist- assist with ambulating, transfers, toileting, gross motor skills Speech therapist- check for dysphagia, swallowing problems A nurse is providing care for a patient on a medical surgical unit. A nurse from another unit asks about the surgeons medical diagnosis. The nurse responds that he is unable to provide the information requested. The nurse is displaying which ethical principle? a. Non-malificence To determine in patient experiencing MI – put 12 ECG leads A nurse is caring for a client who has a central venous catheter and suddenly develops chest pain, dypnea, dizziness, and tachycardia. The nurse suspects air embolism and clamps the catheter immediately. What other action should the nurse take at this time? a. Place the client on his left-side in trenlendenburg Pulmonary embolism- Heparin When client scheduled for physical therapy- identify their pain level and medicate as needed Hypovolemic shock- increased HR Left side heart failure- hacking cough Indication of dehydration- skin turgor present Find client unresponsive 1. Notify Rapid response 2. Check carotid pulse Right ventricular failure- hepatomelagy When checking a clients capillary refill and the client has a cap refill of 10 this indicates a. Arterial insufficiency Client develops airway obstruction from a foreign body but remains conscious priority- administer the abdominal thrush maneuver Use chlorohexidine to wash hands after providing care for immunocompromised patient. A nurse is caring for a client who has an arterial line. Which of the following should the nurse take? a. Place pressure bag around the flush solution Placing central venous catheter place patient in trenlendslendenburg A nurse is caring for a client who has a central venous catheter and develops SOB. Which of the following actions should the nurse take first? a. Clamp the catheter Pulmonary Embolism (select all) a. Assess leg for redness b. Apply elastic compression stockings c. Perform passive ROM A client who has left ventricular failure and a high pulmonary cap wedge pressure PCWP is receiving dopamine IV to improve ventricular function. Which of the following indocates the medicine is having therapeutic effects? a. Systolic blood pressure increases A nurse is caring for a client who is receiving mechanical ventilation when the low pressure alarm sounds. Which of the following situations should the nurse recognize as a possible cause of the alarm? a. Artificial airway cuff leak A nurse is caring for a client in acute respiratory failure who is receiving mechanical ventilation. Which of the following assessments is the best method for the nurse to determine the effectiveness of the current treatment regimen? a. Arterial blood gas If chest tube comes out- put tip in sterile water (more helpful info) https://quizlet.com/172754756/critical-care-ati-flash-cards/ https://quizlet.com/71508111/hemodynamics-ati-nclex-flash-cards/ https://quizlet.com/124257127/hemodynamic-monitoring-ati-flash-cards/ https://quizlet.com/148806919/ati-nasogastric-intubation-flash-cards/ https://quizlet.com/101469310/ati-chapter-53-airway-managementoxygen-therapy- flash-cards/ https://quizlet.com/71508111/hemodynamics-ati-nclex-flash-cards/ https://quizlet.com/124257127/hemodynamic-monitoring-ati-flash-cards/ https://quizlet.com/172754756/critical-care-ati-flash-cards/ https://www.caccn.ca/pdfs/CACCN%20Certification%20Study%20Guide %20Answers%202010.pdf https://www.glowm.com/section_view/heading/Hemodynamic%20Monitoring %20of%20the%20Critically%20Ill%20Patient/item/211 https://quizlet.com/361980054/chapter-65-critical-care-hemodynamic-monitoring- flash-cards/ Chapter 1 1. The nurse completes an admission database and explains that the plan of care and discharge goals will be developed with the patient’s input. The patient states, “How is this different from what the doctor does?” Which response would be most appropriate for the nurse to make? a. “The role of the nurse is to administer medications and other treatments prescribed by your doctor.” b. “The nurse’s job is to help the doctor by collecting information and communicating any problems that occur.” c. “Nurses perform many of the same procedures as the doctor, but nurses are with the patients for a longer time than the doctor.” d. “In addition to caring for you while you are sick, the nurses will assist you to develop an individualized plan to maintain your health.” ANS: D This response is consistent with the American Nurses Association (ANA) definition of nursing, which describes the role of nurses in promoting health. The other responses describe some of the dependent and collaborative functions of the nursing role but do not accurately describe the nurse’s role in the health care system. DIF: Cognitive Level: Understand (comprehension) REF: 3 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 2. The nurse describes to a student nurse how to use evidence-based practice guidelines when caring for patients. Which statement, if made by the nurse, would be the most accurate? a. “Inferences from clinical research studies are used as a guide.” b. “Patient care is based on clinical judgment, experience, and traditions.” c. “Data are evaluated to show that the patient outcomes are consistently met.” d. “Recommendations are based on research, clinical expertise, and patient preferences.” ANS: D Evidence-based practice (EBP) is the use of the best research-based evidence combined with clinician expertise. Clinical judgment based on the nurse’s clinical experience is part of EBP, but clinical decision making should also incorporate current research and research-based guidelines. Evaluation of patient outcomes is important, but interventions should be based on research from randomized control studies with a large number of subjects. DIF: Cognitive Level: Remember (knowledge) REF: 15 TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 3. The nurse teaches a student nurse about how to apply the nursing process when providing patient care. Which statement, if made by the student nurse, indicates that teaching was successful? a. “The nursing process is a scientific-based method of diagnosing the patient’s health care problems.” b. “The nursing process is a problem-solving tool used to identify and treat patients’ health care needs.” c. “The nursing process is used primarily to explain nursing interventions to other health care professionals.” d. “The nursing process is based on nursing theory that incorporates the biopsychosocial nature of humans.” ANS: B The nursing process is a problem-solving approach to the identification and treatment of patients’ problems. Diagnosis is only one phase of the nursing process. The primary use of the nursing process is in patient care, not to establish nursing theory or explain nursing interventions to other health care professionals. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 4. A patient has been admitted to the hospital for surgery and tells the nurse, “I do not feel comfortable leaving my children with my parents.” Which action should the nurse take next? a. Reassure the patient that these feelings are common for parents. b. Have the patient call the children to ensure that they are doing well. c. Gather more data about the patient’s feelings about the child-care arrangements. d. Call the patient’s parents to determine whether adequate child care is being provided. ANS: C Because a complete assessment is necessary in order to identify a problem and choose an appropriate intervention, the nurse’s first action should be to obtain more information. The other actions may be appropriate, but more assessment is needed before the best intervention can be chosen. DIF: Cognitive Level: Apply (application) REF: 6 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 5. A patient who is paralyzed on the left side of the body after a stroke develops a pressure ulcer on the left hip. Which nursing diagnosis is most appropriate? a. Impaired physical mobility related to left-sided paralysis b. Risk for impaired tissue integrity related to left-sided weakness c. Impaired skin integrity related to altered circulation and pressure d. Ineffective tissue perfusion related to inability to move independently ANS: C The patient’s major problem is the impaired skin integrity as demonstrated by the presence of a pressure ulcer. The nurse is able to treat the cause of altered circulation and pressure by frequently repositioning the patient. Although left-sided weakness is a problem for the patient, the nurse cannot treat the weakness. The “risk for” diagnosis is not appropriate for this patient, who already has impaired tissue integrity. The patient does have ineffective tissue perfusion, but the impaired skin integrity diagnosis indicates more clearly what the health problem is. DIF: Cognitive Level: Apply (application) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Physiological Integrity 6. A patient with a bacterial infection has a nursing diagnosis of deficient fluid volume related to excessive diaphoresis. Which outcome would the nurse recognize as appropriate for this patient? a. Patient has a balanced intake and output. b. Patient’s bedding is changed when it becomes damp. c. Patient understands the need for increased fluid intake. d. Patient’s skin remains cool and dry throughout hospitalization. ANS: A This statement gives measurable data showing resolution of the problem of deficient fluid volume that was identified in the nursing diagnosis statement. The other statements would not indicate that the problem of deficient fluid volume was resolved. DIF: Cognitive Level: Apply (application) REF: 7 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 7. A nurse asks the patient if pain was relieved after receiving medication. What is the purpose of the evaluation phase of the nursing process? a. To determine if interventions have been effective in meeting patient outcomes b. To document the nursing care plan in the progress notes of the medical record c. To decide whether the patient’s health problems have been completely resolved d. To establish if the patient agrees that the nursing care provided was satisfactory ANS: A Evaluation consists of determining whether the desired patient outcomes have been met and whether the nursing interventions were appropriate. The other responses do not describe the evaluation phase. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Evaluation MSC: NCLEX: Safe and Effective Care Environment 8. The nurse interviews a patient while completing the health history and physical examination. What is the purpose of the assessment phase of the nursing process? a. To teach interventions that relieve health problems b. To use patient data to evaluate patient care outcomes c. To obtain data with which to diagnose patient problems d. To help the patient identify realistic outcomes for health problems ANS: C During the assessment phase, the nurse gathers information about the patient to diagnose patient problems. The other responses are examples of the planning, intervention, and evaluation phases of the nursing process. DIF: Cognitive Level: Understand (comprehension) REF: 5 TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment 9. Which nursing diagnosis statement is written correctly? a. Altered tissue perfusion related to heart failure b. Risk for impaired tissue integrity related to sacral redness c. Ineffective coping related to response to biopsy test results d. Altered urinary elimination related to urinary tract infection ANS: C This diagnosis statement includes a NANDA nursing diagnosis and an etiology that describes a patient’s response to a health problem that can be treated by nursing. The use of a medical diagnosis as an etiology (as in the responses beginning “Altered tissue perfusion” and “Altered urinary elimination”) is not appropriate. The response beginning “Risk for impaired tissue integrity” uses the defining characteristic as the etiology. DIF: Cognitive Level: Understand (comprehension) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Safe and Effective Care Environment 10. The nurse admits a patient to the hospital and develops a plan of care. What components should the nurse include in the nursing diagnosis statement? a. The problem and the suggested patient goals or outcomes b. The problem with possible causes and the planned interventions c. The problem, its cause, and objective data that support the problem d. The problem with an etiology and the signs and symptoms of the problem ANS: D When writing nursing diagnoses, this format should be used: problem, etiology, and signs and symptoms. The subjective, as well as objective, data should be included in the defining characteristics. Interventions and outcomes are not included in the nursing diagnosis statement. DIF: Cognitive Level: Remember (knowledge) REF: 7 TOP: Nursing Process: Diagnosis MSC: NCLEX: Safe and Effective Care Environment 11. A nurse is caring for a patient with heart failure. Which task is appropriate for the nurse to delegate to experienced unlicensed assistive personnel (UAP)? a. Monitor for shortness of breath or fatigue after ambulation. b. Instruct the patient about the need to alternate activity and rest. c. Obtain the patient’s blood pressure and pulse rate after ambulation. d. Determine whether the patient is ready to increase the activity level. ANS: C UAP education includes accurate vital sign measurement. Assessment and patient teaching require registered nurse education and scope of practice and cannot be delegated. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 12. A nurse is caring for a group of patients on the medical-surgical unit with the help of one float registered nurse (RN), one unlicensed assistive personnel (UAP), and one licensed practical/vocational nurse (LPN/LVN). Which assignment, if delegated by the nurse, would be inappropriate? a. Measurement of a patient’s urine output by UAP b. Administration of oral medications by LPN/LVN c. Check for the presence of bowel sounds and flatulence by UAP d. Care of a patient with diabetes by RN who usually works on the pediatric unit ANS: C Assessment requires RN education and scope of practice and cannot be delegated to an LPN/LVN or UAP. The other assignments made by the RN are appropriate. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 13. Which task is appropriate for the nurse to delegate to a licensed practical/vocational nurse (LPN/LVN)? a. Complete the initial admission assessment and plan of care. b. Document teaching completed before a diagnostic procedure. c. Instruct a patient about low-fat, reduced sodium dietary restrictions. d. Obtain bedside blood glucose on a patient before insulin administration. ANS: D The education and scope of practice of the LPN/LVN include activities such as obtaining glucose testing using a finger stick. Patient teaching and the initial assessment and development of the plan of care are nursing actions that require registered nurse education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 14. A nurse is assigned as a case manager for a hospitalized patient with a spinal cord injury. The patient can expect the nurse functioning in this role to perform which activity? a. Care for the patient during hospitalization for the injuries. b. Assist the patient with home care activities during recovery. c. Determine what medical care the patient needs for optimal rehabilitation. d. Coordinate the services that the patient receives in the hospital and at home. ANS: D The role of the case manager is to coordinate the patient’s care through multiple settings and levels of care to allow the maximal patient benefit at the least cost. The case manager does not provide direct care in either the acute or home setting. The case manager coordinates and advocates for care but does not determine what medical care is needed; that would be completed by the health care provider or other provider. DIF: Cognitive Level: Apply (application) REF: 9 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 15. The nurse is caring for an older adult patient who had surgery to repair a fractured hip. The patient needs continued nursing care and physical therapy to improve mobility before returning home. The nurse will help to arrange for transfer of this patient to which facility? a. A skilled care facility c. A transitional care facility b. A residential care facility d. An intermediate care facility ANS: C Transitional care settings are appropriate for patients who need continued rehabilitation before discharge to home or to long-term care settings. The patient is no longer in need of the more continuous assessment and care given in acute care settings. There is no indication that the patient will need the permanent and ongoing medical and nursing services available in intermediate or skilled care. The patient is not yet independent enough to transfer to a residential care facility. DIF: Cognitive Level: Apply (application) REF: 8 TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 16. A home care nurse is planning care for a patient who has just been diagnosed with type 2 diabetes mellitus. Which task is appropriate for the nurse to delegate to the home health aide? a. Assist the patient to choose appropriate foods. b. Help the patient with a daily bath and oral care. c. Check the patient’s feet for signs of breakdown. d. Teach the patient how to monitor blood glucose. ANS: B Assisting with patient hygiene is included in home health-aide education and scope of practice. Assessment of the patient and instructing the patient in new skills, such as diet and blood glucose monitoring, are complex skills that are included in registered nurse education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 17. The nurse is providing education to nursing staff on quality care initiatives. Which statement is an accurate description of the impact of health care financing on quality care? a. “If a patient develops a catheter-related infection, the hospital receives additional funding.” b. “Payment for patient care is primarily based on clinical outcomes and patient satisfaction.” c. “Hospitals are reimbursed for all costs incurred if care is documented electronically.” d. “Because hospitals are accountable for overall care, it is not nursing’s responsibility to monitor care delivered by others.” ANS: B Payment for health care services programs reimburses hospitals for their performance on overall quality-of-care measures. These measures include clinical outcomes and patient satisfaction. Nurses are responsible for coordinating complex aspects of patient care, including the care delivered by others, and identifying issues that are associated with poor quality care. Payment for care can be withheld if something happens to the patient that is considered preventable (e.g., acquiring a catheter-related urinary tract infection). DIF: Cognitive Level: Apply (application) REF: 4 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 18. The nurse documenting the patient’s progress in the care plan in the electronic health record before an interprofessional discharge conference is demonstrating competency in which QSEN category? a. Patient-centered care c. Evidence-based practice b. Quality improvement d. Informatics and technology ANS: D The nurse is displaying competency in the QSEN area of informatics and technology. Using a computerized information system to document patient needs and progress and communicate vital information regarding the patient with the interprofessional care team members provides evidence that nursing practice standards related to the nursing process have been maintained during the care of the patient. DIF: Cognitive Level: Apply (application) REF: 13 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. Which information will the nurse consider when deciding what nursing actions to delegate to a licensed practical/vocational nurse (LPN/LVN) who is working on a medical-surgical unit (select all that apply)? a. Institutional policies b. Stability of the patient c. State nurse practice act d. LPN/LVN teaching abilities e. Experience of the LPN/LVN ANS: A, B, C, E The nurse should assess the experience of LPN/LVNs when delegating. In addition, state nurse practice acts and institutional policies must be considered. In general, whereas the LPN/LVN scope of practice includes caring for patients who are stable, registered nurses should provide most of the care for unstable patients. Because the LPN/LVN scope of practice does not include patient education, this will not be part of the delegation process. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 2. The nurse is administering medications to a patient. Which actions by the nurse during this process are consistent with promoting safe delivery of care (select all that apply)? a. Throws away a medication that is not labeled b. Uses a hand sanitizer before preparing a medication c. Identifies the patient by the room number on the door d. Checks laboratory test results before administering a diuretic e. Gives the patient a list of current medications upon discharge ANS: A, B, D, E National Patient Safety Goals have been established to promote safe delivery of care. The nurse should use at least two reliable ways to identify the patient such as asking the patient’s full name and date of birth before medication administration. Other actions that improve patient safety include performing hand hygiene, disposing of unlabeled medications, completing appropriate assessments before administering medications, and giving a list of the current medicines to the patient and caregiver before discharge. DIF: Cognitive Level: Apply (application) REF: 12 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment OTHER 1. The nurse uses the Situation-Background-Assessment-Recommendation (SBAR) format to communicate a change in patient status to a health care provider. In which order should the nurse make the following statements? (Put a comma and a space between each answer choice [A, B, C, D].) a. “The patient needs to be evaluated immediately and may need intubation and mechanical ventilation.” b. “The patient was admitted yesterday with heart failure and has been receiving furosemide (Lasix) for diuresis, but urine output has been low.” c. “The patient has crackles audible throughout the posterior chest, and the most recent oxygen saturation is 89%. Her condition is very unstable.” d. “This is the nurse on the surgical unit. After assessing the patient, I am very concerned about increased shortness of breath over the past hour.” ANS: D, B, C, A The order of the nurse’s statements follows the SBAR format. DIF: Cognitive Level: Apply (application) REF: 11 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment Chapter 9 1. The nurse is caring for an unresponsive terminally ill patient who has 20-second periods of apnea followed by periods of deep and rapid breathing. Which action by the nurse would be appropriate? a. Suction the patient’s mouth. b. Administer oxygen via face mask. c. Document Cheyne-Stokes respirations. d. Place the patient in high Fowler’s position. ANS: C Cheyne-Stokes respirations are characterized by periods of apnea alternating with deep and rapid breaths. Cheyne-Stokes respirations are expected in the last days of life and are not position dependent. There is also no need for supplemental oxygen by face mask or suctioning the patient. DIF: Cognitive Level: Apply (application) REF: 132 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 2. The nurse is caring for an adolescent patient who is dying. The patient’s parents are interested in organ donation and ask the nurse how the health care providers determine brain death. Which response by the nurse accurately describes brain death determination? a. “If CPR does not restore a heartbeat, the brain cannot function.” b. “Brain death has occurred if there is not any breathing or brainstem reflexes.” c. “Brain death has occurred if a person has flaccid muscles and does not awaken.” d. “If respiratory efforts cease and no apical pulse is audible, brain death is present.” ANS: B The diagnosis of brain death is based on irreversible loss of all brain functions, including brainstem functions that control respirations and brainstem reflexes. The other descriptions describe other clinical manifestations associated with death but are insufficient to declare a patient brain dead. DIF: Cognitive Level: Apply (application) REF: 131 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 3. A patient in hospice is manifesting a decrease in all body system functions except for a heart rate of 124 beats/min and a respiratory rate of 28 breaths/min. Which statement, if made by the nurse to the patient’s family member, is most appropriate? a. “These vital signs will continue to increase until death finally occurs.” b. “These vital signs are an expected response now but will slow down later.” c. “These vital signs may indicate an improvement in the patient’s condition.” d. “These vital signs are a helpful response to the slowing of other body systems.” ANS: B An increase in heart and respiratory rate may occur before the slowing of these functions in a dying patient. Heart and respiratory rate typically slow as the patient progresses further toward death. In a dying patient, high respiratory and pulse rates do not indicate improvement or compensation, and it would be inappropriate for the nurse to indicate this to the family. DIF: Cognitive Level: Apply (application) REF: 132 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 4. A patient who has been diagnosed with inoperable lung cancer and has a poor prognosis plans a trip across the country “to settle some issues with family members.” The nurse recognizes that the patient is manifesting which psychosocial response to death? a. Protesting the unfairness of death b. Anxiety about unfinished business c. Fear of having lived a meaningless life d. Restlessness about the uncertainty of prognosis ANS: B The patient’s statement indicates that there is some unfinished family business that the patient would like to address before dying. There is no indication that the patient is protesting the prognosis, feels uncertain about the prognosis, or fears that life has been meaningless. DIF: Cognitive Level: Apply (application) REF: 132 TOP: Nursing Process: Assessment MSC: NCLEX: Psychosocial Integrity 5. A patient with terminal cancer is being admitted to a family-centered inpatient hospice. The patient’s spouse visits daily and cheerfully talks with the patient about wedding anniversary plans for the next year. When the nurse asks about any concerns, the spouse says, “I’m busy at work, but otherwise things are fine.” Which provisional nursing diagnosis is appropriate for the patient’s spouse? a. Ineffective coping related to lack of grieving b. Anxiety related to complicated grieving process c. Hopelessness related to knowledge deficit about cancer d. Caregiver role strain related to spouse’s complex care needs ANS: A The spouse’s behavior and statements indicate the absence of anticipatory grieving, which may lead to impaired adjustment as the patient progresses toward death. The spouse does not appear to feel overwhelmed, hopeless, or anxious. DIF: Cognitive Level: Apply (application) REF: 133 TOP: Nursing Process: Diagnosis MSC: NCLEX: Psychosocial Integrity 6. As the nurse admits a patient in end-stage renal disease to the hospital, the patient tells the nurse, “If my heart or breathing stop, I do not want to be resuscitated.” Which action should the nurse take first? a. Place a “Do Not Resuscitate” (DNR) notation in the patient’s care plan. b. Invite the patient to add a notarized advance directive in the health record. c. Advise the patient to designate a person to make future health care decisions. d. Ask if the decision has been discussed with the patient’s health care provider. ANS: D A health care provider’s order should be written describing the actions that the nurses should take if the patient requires CPR, but the primary right to decide belongs to the patient or family. The nurse should document the patient’s request but does not have the authority to place the DNR order in the care plan. A notarized advance directive is not needed to establish the patient’s wishes. The patient may need a durable power of attorney for health care (or the equivalent), but this does not address the patient’s current concern with possible resuscitation. DIF: Cognitive Level: Apply (application) REF: 136 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 7. A young adult patient with metastatic cancer, who is very close to death, appears restless. The patient keeps repeating, “I am not ready to die.” Which action is best for the nurse to take? a. Remind the patient that no one feels ready for death. b. Sit at the bedside and ask if there is anything the patient needs. c. Insist that family members remain at the bedside with the patient. d. Tell the patient that everything possible is being done to delay death. ANS: B Staying at the bedside and listening allows the patient to discuss any unresolved issues or physical discomforts that should be addressed. Stating that no one feels ready for death fails to address the individual patient’s concerns. Telling the patient that everything is being done does not address the patient’s fears about dying, especially because the patient is likely to die soon. Family members may not feel comfortable staying at the bedside of a dying patient, and the nurse should not insist that they remain there. DIF: Cognitive Level: Analyze (analysis) REF: 138 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 8. The nurse is caring for a terminally ill patient who is experiencing continuous and severe pain. How should the nurse schedule the administration of opioid pain medications? a. Plan around-the-clock routine administration of analgesics. b. Provide PRN doses of medication whenever the patient requests them. c. Suggest small analgesic doses to avoid decreasing the respiratory rate. d. Offer enough pain medication to keep the patient sedated and unaware of stimuli. ANS: A The principles of beneficence and nonmaleficence indicate that the goal of pain management in a terminally ill patient is adequate pain relief even if the effect of pain medications could hasten death. Administration of analgesics on a PRN basis will not provide the consistent level of analgesia the patient needs. Patients usually do not require so much pain medication that they are oversedated and unaware of stimuli. Adequate pain relief may require a dosage that will result in a decrease in respiratory rate. DIF: Cognitive Level: Apply (application) REF: 140 TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 9. The nurse is caring for a patient with lung cancer in a home hospice program. Which action by the nurse is appropriate? a. Discuss cancer risk factors and appropriate lifestyle modifications. b. Teach the patient about the purpose of chemotherapy and radiation. c. Encourage the patient to discuss past life events and their meanings. d. Accomplish a thorough head-to-toe assessment several times a week. ANS: C The role of the hospice nurse includes assisting the patient with the important end-of-life task of finding meaning in the patient’s life. Frequent head-to-toe assessments are not needed for hospice patients and may tire the patient unnecessarily. Patients admitted to hospice forego curative treatments such as chemotherapy and radiation for lung cancer. Discussion of cancer risk factors and therapies is not appropriate. DIF: Cognitive Level: Apply (application) REF: 139 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 10. A hospice nurse who has become close to a terminally ill patient is present in the home when the patient dies and feels saddened and tearful as the family members begin to cry. Which action should the nurse take at this time? a. Contact a grief counselor as soon as possible. b. Cry along with the patient’s family members. c. Leave the home quickly to allow the family to grieve privately. d. Consider leaving hospice work because patient losses are common. ANS: B It is appropriate for the nurse to cry and express sadness in other ways when a patient dies, and the family is likely to feel that this is supportive. Contacting a grief counselor, leaving the family to grieve privately, and considering whether hospice continues to be a satisfying place to work are all appropriate actions as well, but the nurse’s initial action at this time should be to share the grieving process with the family. DIF: Cognitive Level: Apply (application) REF: 142 TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 11. A middle-aged patient tells the nurse, “My mother died 4 months ago, and I just can’t get over it. I’m not sure it is normal to still think about her every day.” Which nursing diagnosis is most appropriate? a. Hopelessness related to inability to resolve grief b. Complicated grieving related to unresolved issues c. Anxiety related to lack of knowledge about normal grieving d. Chronic sorrow related to ongoing distress about loss of mother ANS: C The patient should be reassured that grieving activities such as frequent thoughts about the deceased are considered normal for months or years after a death. The other nursing diagnoses imply that the patient’s grief is unusual or pathologic, which is not the case. DIF: Cognitive Level: Apply (application) REF: 133 TOP: Nursing Process: Diagnosis MSC: NCLEX: Psychosocial Integrity 12. The son of a dying patient tells the nurse, “Mother doesn’t really respond any more when I visit. I don’t think she knows that I am here.” Which response by the nurse is appropriate? a. “Cut back your visits for now to avoid overtiring your mother.” b. “Withdrawal can be a normal response in the process of dying.” c. “Most dying patients don’t know what is going on around them.” d. “It is important to stimulate your mother so she can’t retreat from you.” ANS: B Withdrawal is a normal psychosocial response to approaching death. Dying patients may maintain the ability to hear while not being able to respond. Stimulation will tire the patient and is not an appropriate response to withdrawal in this circumstance. Visitors are encouraged to be “present” with the patient, talking softly and making physical contact in a way that does not demand a response from the patient. DIF: Cognitive Level: Apply (application) REF: 138 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 13. Which patient should the nurse refer for hospice care? a. A 70-yr-old patient with lymphoma whose children are unable to discuss issues related to dying b. A 60-yr-old patient with chronic severe pain as a result of spinal arthritis and vertebral collapse c. A 40-yr-old patient with AIDS-related dementia who needs palliative care and pain management d. A 50-yr-old patient with advanced liver failure whose family members can no longer provide care in the home ANS: C Hospice is designed to provide palliative care such as symptom management and pain control for patients at the end of life. Patients who require more care than the family can provide, whose families are unable to discuss important issues related to dying, or who have severe pain are candidates for other nursing services but are not appropriate hospice patients. DIF: Cognitive Level: Apply (application) REF: 130 OBJ: Special Questions: Multiple Patients TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 14. The nurse admits a terminally ill patient to the hospital. What is the first action that the nurse should complete when planning this patient's care? a. Determine the patient’s wishes regarding end-of-life care. b. Emphasize the importance of addressing any family issues. c. Discuss the normal grief process with the patient and family. d. Encourage the patient to talk about any fears or unresolved issues. ANS: A The nurse’s initial action should be to assess the patient’s wishes at this time. The other actions may be implemented if the patient or the family express a desire to discuss fears, understand the grief process, or address family issues, but they should not be implemented until the assessment indicates that they are appropriate. DIF: Cognitive Level: Analyze (analysis) REF: 135 OBJ: Special Questions: Prioritization TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity 15. Which action is most important for the nurse to take to ensure culturally competent care for an alert, terminally ill Filipino patient? a. Let the family decide how to tell the patient about the terminal diagnosis. b. Ask the patient and family about their preferences for care during this time. c. Obtain information from Filipino staff members about possible cultural needs. d. Remind family members that dying patients prefer to have someone at the bedside. ANS: B Because cultural beliefs may vary among people of the same ethnicity, the nurse’s best action is to assess the expectations of both the patient and family. The other actions may be appropriate, but the nurse can only plan for individualized culturally competent care after assessment of this patient and family. DIF: Cognitive Level: Analyze (analysis) REF: 134 TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment MULTIPLE RESPONSE 1. Which nursing actions for the care of a dying patient can the nurse delegate to a licensed practical/vocational nurse (LPN/LVN) (select all that apply)? a. Provide postmortem care to the patient. b. Encourage the family members to talk with and reassure the patient. c. Determine how frequently physical assessments are needed for the patient. d. Teach family members about commonly occurring signs of approaching death. e. Administer the prescribed morphine sulfate sublingual as necessary for pain control. ANS: A, B, E Medication administration, psychosocial care, and postmortem care are included in LPN/LVN education and scope of practice. Patient and family teaching and assessment and planning of frequency for assessments are skills that require registered nurse level education and scope of practice. DIF: Cognitive Level: Apply (application) REF: 142 OBJ: Special Questions: Delegation TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment Chapter 65 1.A patient who has been in the intensive care unit for 4 days has disturbed sensory perception from sleep deprivation. Which action should the nurse include in the plan of care? a. Administer prescribed sedatives or opioids at bedtime to promote sleep. b. Cluster nursing activities so that the patient has uninterrupted rest periods. c. Silence the alarms on the cardiac monitors to allow 30- to 40-minute naps. d. Eliminate assessments between 2200 and 0600 to allow uninterrupted sleep. ANS: B Clustering nursing activities and providing uninterrupted rest periods will minimize sleep-cycle disruption. Sedative and opioid medications tend to decrease the amount of rapid eye movement (REM) sleep and can contribute to sleep disturbance and disturbed sensory perception. Silencing the alarms on the cardiac monitors would be unsafe in a critically ill patient, as would discontinuing all assessments during the night. DIF: Cognitive Level: Apply (application) REF: 1556 TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity 2. Which hemodynamic parameter best reflects the effectiveness of drugs that the nurse gives to reduce a patient’s left ventricular afterload? a. Mean arterial pressure (MAP) b. Systemic vascular resistance (SVR) c. Pulmonary vascular resistance (PVR) d. Pulmonary artery wedge pressure (PAWP) ANS: B SVR reflects the resistance to ventricular ejection, or afterload. The other parameters may be monitored but do not reflect afterload as directly. DIF: Cognitive Level: Apply (application) REF: 1560 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 3. While close family members are visiting, a patient has a respiratory arrest, and resuscitation is started. Which action by the nurse is best? a. Tell the family members that watching the resuscitation will be very stressful. b. Ask family members if they wish to remain in the room during the resuscitation. c. Take the family members quickly out of the patient room and remain with them. d. Assign a staff member to wait with family members just outside the patient room. ANS: B Evidence indicates that many family members want the option of remaining in the room during procedures such as cardiopulmonary resuscitation (CPR) and that this decreases anxiety and facilitates grieving. The other options may be appropriate if the family decides not to remain with the patient. DIF: Cognitive Level: Analyze (analysis) REF: 1558 TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 4. After surgery for an abdominal aortic aneurysm, a patient’s central venous pressure (CVP) monitor indicates low pressures. Which action should the nurse take? a. Administer IV diuretic medications. b. Increase the IV fluid infusion per protocol. c. Increase the infusion rate of IV vasodilators. d. Elevate the head of the patient’s bed to 45 degrees. ANS: B A low CVP indicates hypovolemia and a need for an increase in the infusion rate. Diuretic administration will contribute to hypovolemia and elevation of the head or increasing vasodilators may decrease cerebral perfusion. DIF: Cognitive Level: Apply (application) REF: 1564 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 5. When caring for a patient with pulmonary hypertension, which parameter will the nurse use to directly evaluate the effectiveness of the treatment? a. Central venous pressure (CVP) b. Systemic vascular resistance (SVR) c. Pulmonary vascular resistance (PVR) d. Pulmonary artery wedge pressure (PAWP) ANS: C PVR is a major contributor to pulmonary hypertension, and a decrease would indicate that pulmonary hypertension was improving. The other parameters may also be monitored but do not directly assess for pulmonary hypertension. DIF: Cognitive Level: Apply (application) REF: 1560 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 6. The intensive care unit (ICU) nurse educator determines that teaching a new staff nurse about arterial pressure monitoring has been effective when the nurse a. balances and calibrates the monitoring equipment every 2 hours. b. positions the zero-reference stopcock line level with the phlebostatic axis. c. ensures that the patient is supine with the head of the bed flat for all readings. d. rechecks the location of the phlebostatic axis with changes in the patient’s position. ANS: B For accurate measurement of pressures, the zero-reference level should be at the phlebostatic axis. There is no need to rebalance and recalibrate monitoring equipment every 2 hours. Accurate hemodynamic readings are possible with the patient’s head raised to 45 degrees or in the prone position. The anatomic position of the phlebostatic axis does not change when patients are repositioned. DIF: Cognitive Level: Apply (application) REF: 1560 TOP: Nursing Process: Evaluation MSC: NCLEX: Safe and Effective Care Environment 7. When monitoring the effectiveness of treatment for a patient with a large anterior wall myocardial infarction, the most pertinent measurement for the nurse to obtain is a. central venous pressure (CVP). b. systemic vascular resistance (SVR). c. pulmonary vascular resistance (PVR). d. pulmonary artery wedge pressure (PAWP). ANS: D PAWP reflects left ventricular end diastolic pressure (or left ventricular preload) and is a sensitive indicator of cardiac function. Because the patient is high risk for left ventricular failure, the PAWP must be monitored. An increase will indicate left ventricular failure. The other values would also provide useful information, but the most definitive measurement of changes in cardiac function is the PAWP. DIF: Cognitive Level: Apply (application) REF: 1563 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 8. Which action should the nurse take when the low pressure alarm sounds for a patient who has an arterial line in the left radial artery? a. Fast flush the arterial line. b. Check the left hand for pallor. c. Assess for cardiac dysrhythmias. d. Re-zero the monitoring equipment. ANS: C The low pressure alarm indicates a drop in the patient’s blood pressure, which may be caused by cardiac dysrhythmias. There is no indication to re-zero the equipment. Pallor of the left hand would be caused by occlusion of the radial artery by the arterial catheter, not by low pressure. There is no indication of a need for flushing the line. DIF: Cognitive Level: Apply (application) REF: 1564 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 9. Which nursing action is needed when preparing to assist with the insertion of a pulmonary artery catheter? a. Determine if the cardiac troponin level is elevated. b. Auscultate heart sounds before and during insertion. c. Place the patient on NPO status before the procedure. d. Attach cardiac monitoring leads before the procedure. ANS: D Dysrhythmias can occur as the catheter is floated through the right atrium and ventricle, and it is important for the nurse to monitor for these during insertion. Pulmonary artery catheter insertion does not require anesthesia, and the patient will not need to be NPO. Changes in cardiac troponin or heart and breath sounds are not expected during pulmonary artery catheter insertion. DIF: Cognitive Level: Apply (application) REF: 1564 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 10. While assisting with the placement of a pulmonary artery (PA) catheter, the nurse notes that the catheter is correctly placed when the balloon is inflated and the monitor shows a a. typical PA pressure waveform. b. tracing of the systemic arterial pressure. c. tracing of the systemic vascular resistance. d. typical PA wedge pressure (PAWP) tracing. ANS: D The purpose of a PA line is to measure PAWP, so the catheter is floated through the pulmonary artery until the dilated balloon wedges in a distal branch of the pulmonary artery, and the PAWP readings are available. After insertion, the balloon is deflated and the PA waveform will be observed. Systemic arterial pressures are obtained using an arterial line, and the systemic vascular resistance is a calculated value, not a waveform. DIF: Cognitive Level: Understand (comprehension) REF: 1564 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 11. Which assessment finding obtained by the nurse when caring for a patient with a right radial arterial line indicates a need for the nurse to take action? a. The right hand feels cooler than the left hand. b. The mean arterial pressure (MAP) is 77 mm Hg. c. The system is delivering 3 mL of flush solution per hour. d. The flush bag and tubing were last changed 2 days previously. ANS: A The change in temperature of the right hand suggests that blood flow to the right hand is impaired. The flush system needs to be changed every 96 hours. A mean arterial pressure (MAP) of 75 mm Hg is normal. Flush systems for hemodynamic monitoring are set up to deliver 3 to 6 mL/hr of flush solution. DIF: Cognitive Level: Apply (application) REF: 1565 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 12. The central venous oxygen saturation (ScvO2) is decreasing in a patient who has severe pancreatitis. To determine the possible cause of the decreased ScvO2, the nurse assesses the patient’s a. lipase level. c. urinary output. b. temperature. d. body mass index. ANS: B Elevated temperature increases metabolic demands and O2 use by tissues, resulting in a drop in O2 saturation of central venous blood. Information about the patient’s body mass index, urinary output, and lipase will not help in determining the cause of the patient’s drop in ScvO2. DIF: Cognitive Level: Apply (application) REF: 1565 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 13. An intraaortic balloon pump (IABP) is being used for a patient who is in cardiogenic shock. Which assessment data indicate to the nurse that the goals of treatment with the IABP are being met? a. Urine output of 25 mL/hr b. Heart rate of 110 beats/minute c. Cardiac output (CO) of 5 L/min d. Stroke volume (SV) of 40 mL/beat ANS: C A CO of 5 L/min is normal and indicates that the IABP has been successful in treating the shock. The low SV signifies continued cardiogenic shock. The tachycardia and low urine output also suggest continued cardiogenic shock. DIF: Cognitive Level: Apply (application) REF: 1569 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 14. The nurse is caring for a patient who has an intraaortic balloon pump in place. Which action should be included in the plan of care? a. Avoid the use of anticoagulant medications. b. Measure the patient’s urinary output every hour. c. Provide passive range of motion for all extremities. d. Position the patient supine with head flat at all times. ANS: B Monitoring urine output will help determine whether the patient’s cardiac output has improved and also help monitor for balloon displacement blocking the renal arteries. The head of the bed can be elevated up to 30 degrees. Heparin is used to prevent thrombus formation. Limited movement is allowed for the extremity with the balloon insertion site to prevent displacement of the balloon. DIF: Cognitive Level: Apply (application) REF: 1569 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 15. While waiting for heart transplantation, a patient with severe cardiomyopathy has a ventricular assist device (VAD) implanted. When planning care for this patient, the nurse should anticipate a. preparing the patient for a permanent VAD. b. administering immunosuppressive medications. c. teaching the patient the reason for complete bed rest. d. monitoring the surgical incision for signs of infection. ANS: D The insertion site for the VAD provides a source for transmission of infection to the circulatory system and requires frequent monitoring. Patients with VADs are able to have some mobility and may not be on bed rest. The VAD is a bridge to transplantation, not a permanent device. Immunosuppression is not necessary for nonbiologic devices such as the VAD. DIF: Cognitive Level: Apply (application) REF: 1569 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 16. To verify the correct placement of an oral endotracheal tube (ET) after insertion, the best initial action by the nurse is to a. obtain a portable chest x-ray. b. use an end-tidal CO2 monitor. c. auscultate for bilateral breath sounds. d. observe for symmetrical chest movement. ANS: B End-tidal CO2 monitors are currently recommended for rapid verification of ET placement. Auscultation for bilateral breath sounds and checking chest expansion are also used, but they are not as accurate as end-tidal CO2 monitoring. A chest x-ray confirms the placement but is done after the tube is secured. DIF: Cognitive Level: Analyze (analysis) REF: 1570 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 17. To maintain proper cuff pressure of an endotracheal tube (ET) when the patient is on mechanical ventilation, the nurse should a. inflate the cuff with a minimum of 10 mL of air. b. inflate the cuff until the pilot balloon is firm on palpation. c. inject air into the cuff until a manometer shows 15 mm Hg pressure. d. inject air into the cuff until a slight leak is heard only at peak inflation. ANS: D The minimal occluding volume technique involves injecting air into the cuff until an air leak is present only at peak inflation. The volume to inflate the cuff varies with the ET and the patient’s size. Cuff pressure should be maintained at 20 to 25 mm Hg. An accurate assessment of cuff pressure cannot be obtained by palpating the pilot balloon. DIF: Cognitive Level: Understand (comprehension) REF: 1571 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 18. The nurse notes premature ventricular contractions (PVCs) while suctioning a patient’s endotracheal tube. Which next action by the nurse is indicated? a. Plan to suction the patient more frequently. b. Decrease the suction pressure to 80 mm Hg. c. Give antidysrhythmic medications per protocol. d. Stop and ventilate the patient with 100% oxygen. ANS: D Dysrhythmias during suctioning may indicate hypoxemia or sympathetic nervous system stimulation. The nurse should stop suctioning and ventilate the patient with 100% O2. There is no indication that more frequent suctioning is needed. Lowering the suction pressure will decrease the effectiveness of suctioning without improving the hypoxemia. Because the PVCs occurred during suctioning, there is no need for antidysrhythmic medications (which may have adverse effects) unless they recur when the suctioning is stopped and patient is well oxygenated. DIF: Cognitive Level: Apply (application) REF: 1571 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 19. Which assessment finding obtained by the nurse when caring for a patient receiving mechanical ventilation indicates the need for suctioning? a. The patient was last suctioned 6 hours ago. b. The patient’s oxygen saturation drops to 93%. c. The patient’s respiratory rate is 32 breaths/min. d. The patient has occasional audible expiratory wheezes. ANS: C The increase in respiratory rate indicates that the patient may have decreased airway clearance and requires suctioning. Suctioning is done when patient assessment data indicate that it is needed and not on a scheduled basis. Occasional expiratory wheezes do not indicate poor airway clearance, and suctioning the patient may induce bronchospasm and increase wheezing. An O2 saturation of 93% is acceptable and does not suggest that immediate suctioning is needed. DIF: Cognitive Level: Apply (application) REF: 1571 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 20. The nurse notes thick, white secretions in the endotracheal tube (ET) of a patient who is receiving mechanical ventilation. Which intervention will most directly treat this finding? a. Reposition the patient every 1 to 2 hours. b. Increase suctioning frequency to every hour. c. Add additional water to the patient’s enteral feedings. d. Instill 5 mL of sterile saline into the ET before suctioning. ANS: C Because the patient’s secretions are thick, better hydration is indicated. Suctioning every hour without any specific evidence for the need will increase the incidence of mucosal trauma and would not address the etiology of the ineffective airway clearance. Instillation of saline does not liquefy secretions and may decrease the SpO2. Repositioning the patient is appropriate but will not decrease the thickness of secretions. DIF: Cognitive Level: Apply (application) REF: 1572 TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 21. Four hours after mechanical ventilation is initiated, a patient’s arterial blood gas (ABG) results include a pH of 7.51, PaO2 of 82 mm Hg, PaCO2 of 26 mm Hg, and HCO – of 23 mEq/L (23 mmol/L). The nurse will anticipate the need to a. increase the FIO2. c. increase the respiratory rate. b. increase the tidal volume. d. decrease the respiratory rate. ANS: D The patient’s PaCO2 and pH indicate respiratory alkalosis caused by too high a respiratory rate. The PaO2 is appropriate for a patient with COPD and increasing the respiratory rate and tidal volume would further lower the PaCO2. DIF: Cognitive Level: Analyze (analysis) REF: 1571 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 22. A patient with respiratory failure has arterial pressure–based cardiac output (APCO) monitoring and is receiving mechanical ventilation with peak end-expiratory pressure (PEEP) of 12 cm H2O. Which information indicates that a change in the ventilator settings may be required? a. The arterial pressure is 90/46. b. The stroke volume is increased. c. The heart rate is 58 beats/minute. d. The stroke volume variation is 12%. ANS: A The hypotension suggests that the high intrathoracic pressure caused by the PEEP may be decreasing venous return and (potentially) cardiac output. The other assessment data would not be a direct result of PEEP and mechanical ventilation. DIF: Cognitive Level: Apply (application) REF: 1571 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 23. A nurse is weaning a 68-kg patient who has chronic obstructive pulmonary disease (COPD) from mechanical ventilation. Which patient assessment finding indicates that the weaning protocol should be stopped? a. The patient’s heart rate is 97 beats/min. b. The patient’s oxygen saturation is 93%. c. The patient respiratory rate is 32 breaths/min. d. The patient’s spontaneous tidal volume is 450 mL. ANS: C Tachypnea is a sign that the patient’s work of breathing is too high to allow weaning to proceed. The patient’s heart rate is within normal limits, but the nurse should continue to monitor it. An O2 saturation of 93% is acceptable for a patient with COPD. A spontaneous tidal volume of 450 mL is within the acceptable range. DIF: Cognitive Level: Apply (application) REF: 1582 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 24. The nurse is caring for a patient receiving a continuous norepinephrine IV infusion. Which patient assessment finding indicates that the infusion rate may need to be adjusted? a. Heart rate is slow at 58 beats/min. b. Mean arterial pressure (MAP) is 56 mm Hg. c. Systemic vascular resistance (SVR) is elevated. d. Pulmonary artery wedge pressure (PAWP) is low. ANS: C Vasoconstrictors such as norepinephrine will increase SVR, and this will increase the work of the heart and decrease peripheral perfusion. The infusion rate may need to be decreased. Bradycardia, hypotension (MAP of 56 mm Hg), and low PAWP are not associated with norepinephrine infusion. DIF: Cognitive Level: Apply (application) REF: 1560 TOP: Nursing Process: Evaluation MSC: NCLEX: Physiological Integrity 25. When evaluating a patient with a central venous catheter, the nurse observes that the insertion site is red and tender to touch and the patient’s temperature is 101.8° F. What should the nurse plan to do? a. Discontinue the catheter and culture the tip. b. Use the catheter only for fluid administration. c. Change the flush system and monitor the site. d. Check the site more frequently for any swelling. ANS: A The information indicates that the patient has a local and systemic infection caused by the catheter, and the catheter should be discontinued to avoid further complications such as endocarditis. Changing the flush system, continued monitoring, or using the line for fluids will not help prevent or treat the infection. DIF: Cognitive Level: Apply (application) REF: 1562 TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity 26. An 81-yr-old patient who has been in the intensive care unit (ICU) for a week is now stable and transfer to the progressive care unit is planned. On rounds, the nurse notices that the patient has new onset confusion. The nurse will plan to a. give PRN lorazepam (Ativan) and cancel the transfer. b. inform the receiving nurse and then transfer the patient. c. notify the health care provider and postpone the transfer. d. obtain an order for restraints as needed and transfer the patient. ANS: B The patient’s history and symptoms most likely indicate delirium associated with the sleep deprivation and sensory overload in the ICU environment. Informing the receiving nurse and transferring the patient is appropriate. Postponing the transfer is likely to prolong the delirium. Benzodiazepines and restraints contribute to delirium and agitation. DIF: Cognitive Level: Apply (application) REF: 1557 TOP: Nursing Process: Planning MSC: NCLEX: Psychosocial Integrity 27. The family members of a patient who has been admitted to the intensive care unit (ICU) with multiple traumatic injuries have just arrived in the ICU waiting room. Which action should the nurse take first? a. Explain ICU visitation policies and encourage family visits. b. Escort the family from the waiting room to the patient’s bedside. c. Describe the patient’s injuries and the care that is being provided. d. Invite the family to participate in an interprofessional care conference. ANS: C Lack of information is a major source of anxiety for family members and should be addressed first. Family members should be prepared for the patient’s appearance and the ICU environment before visiting the patient for the first time. ICU visiting should be individualized to each patient and family rather than being dictated by rigid visitation policies. Inviting the family to participate in a multidisciplinary conference is appropriate but should not be the initial action by the nurse. DIF: Cognitive Level: Analyze (analysis) REF: 1558 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Psychosocial Integrity 28. The nurse is caring for a patient who has an arterial catheter in the left radial artery for arterial pressure–based cardiac output (APCO) monitoring. Which information obtained by the nurse requires a report to the health care provider? a. The patient has a positive Allen test result. b. There is redness at the catheter insertion site. c. The mean arterial pressure (MAP) is 86 mm Hg. d. The dicrotic notch is visible in the arterial waveform. ANS: B Redness at the catheter insertion site indicates possible infection. The Allen test is performed before arterial line insertion, and a positive test result indicates normal ulnar artery perfusion. A MAP of 86 mm Hg is normal, and the dicrotic notch is normally present on the arterial waveform. DIF: Cognitive Level: Apply (application) REF: 1562 OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 29. The nurse responds to a ventilator alarm and finds the patient lying in bed gasping and holding the endotracheal tube (ET) in her hand. Which action should the nurse take next? a. Activate the rapid response team. b. Provide reassurance to the patient. c. Call the health care provider to reinsert the tube. d. Manually ventilate the patient with 100% oxygen. ANS: D The nurse should ensure maximal patient oxygenation by manually ventilating with a bag-valve- mask system. Offering reassurance to the patient, notifying the health care provider about the need to reinsert the tube, and activating the rapid response team are also appropriate after the nurse has stabilized the patient’s oxygenation. DIF: Cognitive Level: Analyze (analysis) REF: 1573 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 30. The nurse notes that a patient’s endotracheal tube (ET), which was at the 22-cm mark, is now at the 25-cm mark, and the patient is anxious and restless. Which action should the nurse take next? a. Check the O2 saturation. b. Offer reassurance to the patient. c. Listen to the patient’s breath sounds. d. Notify the patient’s health care provider. ANS: C The nurse should first determine whether the ET tube has been displaced into the right mainstem bronchus by listening for unilateral breath sounds. If so, assistance will be needed to reposition the tube immediately. The other actions are also appropriate, but detection and correction of tube malposition are the most critical actions. DIF: Cognitive Level: Analyze (analysis) REF: 1573 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 31. The nurse educator is evaluating the care that a new registered nurse (RN) provides to a patient receiving mechanical ventilation. Which action by the new RN indicates the need for more education? a. The RN increases the FIO2 to 100% before suctioning. b. The RN secures a bite block in place using adhesive tape. c. The RN asks for assistance to resecure the endotracheal tube. d. The RN positions the patient with the head of bed at 10 degrees. ANS: D The head of the patient’s bed should be positioned at 30 to 45 degrees to prevent ventilator- associated pneumonia. The other actions by the new RN are appropriate. DIF: Cognitive Level: Apply (application) REF: 1579 OBJ: Special Questions: Supervision TOP: Nursing Process: Evaluation MSC: NCLEX: Safe and Effective Care Environment 32. A patient who is orally intubated and receiving mechanical ventilation is anxious and is “fighting” the ventilator. Which action should the nurse take next? a. Verbally coach the patient to breathe with the ventilator. b. Sedate the patient with the ordered PRN lorazepam (Ativan). c. Manually ventilate the patient with a bag-valve-mask device. d. Increase the rate for the ordered propofol (Diprivan) infusion. ANS: A The initial response by the nurse should be to try to decrease the patient’s anxiety by coaching the patient about how to coordinate respirations with the ventilator. The other actions may also be helpful if the verbal coaching is ineffective in reducing the patient’s anxiety. DIF: Cognitive Level: Analyze (analysis) REF: 1579 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 33. The nurse educator is evaluating the performance of a new registered nurse (RN) who is providing care to a patient who is receiving mechanical ventilation with 15 cm H2O of peak end- expiratory pressure (PEEP). Which action indicates that the new RN is safe? a. The RN plans to suction the patient every 1 to 2 hours. b. The RN uses a closed-suction technique to suction the patient. c. The RN tapes the connection between the ventilator tubing and the ET. d. The RN changes the ventilator circuit tubing routinely every 48 hours. ANS: B The closed-suction technique is used when patients require high levels of PEEP (>10 cm H2O) to prevent the loss of PEEP that occurs when disconnecting the patient from the ventilator. Suctioning should not be scheduled routinely, but it should be done only when patient assessment data indicate the need for suctioning. Taping connections between the ET and ventilator tubing would restrict the ability of the tubing to swivel in response to patient repositioning. Ventilator tubing changes increase the risk for ventilator-associated pneumonia and are not indicated routinely. DIF: Cognitive Level: Apply (application) REF: 1571 OBJ: Special Questions: Delegation TOP: Nursing Process: Implementation MSC: NCLEX: Safe and Effective Care Environment 34. The nurse is caring for a patient with a subarachnoid hemorrhage who is intubated and placed on a mechanical ventilator with 10 cm H2O of peak end-expiratory pressure (PEEP). When monitoring the patient, the nurse will need to notify the health care provider immediately if the patient develops a. O2 saturation of 93%. b. green nasogastric tube drainage. c. respirations of 20 breaths/minute. d. increased jugular venous distention. ANS: D Increases in jugular venous distention in a patient with a subarachnoid hemorrhage may indicate an increase in intracranial pressure (ICP) and that the PEEP setting is too high for this patient. A respiratory rate of 20, O2 saturation of 93%, and green nasogastric tube drainage are within normal limits. DIF: Cognitive Level: Apply (application) REF: 1579 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 35. A patient who is receiving positive pressure ventilation is scheduled for a spontaneous breathing trial (SBT). Which finding by the nurse is most likely to result in postponing the SBT? a. New ST segment elevation is noted on the cardiac monitor. b. Enteral feedings are being given through an orogastric tube. c. Scattered rhonchi are heard when auscultating breath sounds. d. hydromorphone (Dilaudid) is being used to treat postoperative pain. ANS: A Myocardial ischemia is a contraindication for ventilator weaning. The ST segment elevation is an indication that weaning should be postponed until further investigation and/or treatment for myocardial ischemia can be done. Ventilator weaning can proceed when opioids are used for pain management, abnormal lung sounds are present, or enteral feedings are being used. DIF: Cognitive Level: Apply (application) REF: 1582 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity 36. After change-of-shift report on a ventilator weaning unit, which patient should the nurse assess first? a. Patient who failed a spontaneous breathing trial and has been placed in a rest mode on the ventilator b. Patient who is intubated and has continuous partial pressure end-tidal CO2 (PETCO2) monitoring c. Patient who was successfully weaned and extubated 4 hours ago and has no urine output for the last 6 hours d. Patient with a central venous O2 saturation (ScvO2) of 69% while on bilevel positive airway pressure (BiPAP) ANS: C The decreased urine output may indicate acute kidney injury or that the patient’s cardiac output and perfusion of vital organs have decreased. Any of these causes would require rapid action. The data about the other patients indicate that their conditions are stable and do not require immediate assessment or changes in their care. Continuous PETCO2 monitoring is frequently used when patients are intubated. The rest mode should be used to allow patient recovery after a failed SBT, and an ScvO2 of 69% is within normal limits. DIF: Cognitive Level: Analyze (analysis) REF: 1582 OBJ: Special Questions: Prioritization | Special Questions: Multiple Patients TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment 37. After change-of-shift report, which patient should the progressive care nurse assess first? a. Patient who was extubated this morning and has a temperature of 101.4°F (38.6°C) b. Patient with bilevel positive airway pressure (BiPAP) for obstructive sleep apnea and a respiratory rate of 16 c. Patient with arterial pressure monitoring who is 2 hours post–percutaneous coronary intervention and needs to void d. Patient who is receiving IV heparin for a venous thromboembolism and has a partial thromboplastin time (PTT) of 101 sec ANS: D The findings for this patient indicate high risk for bleeding from an elevated (nontherapeutic) PTT. The nurse needs to adjust the rate of the infusion (dose) per the health care provider’s parameters. The patient with BiPAP for sleep apnea has a normal respiratory rate. The patient recovering from the percutaneous coronary intervention will need to be assisted with voiding and this task could be delegated to unlicensed assistive personnel. The patient with a fever may be developing ventilator-associated pneumonia, but addressing the bleeding risk is a higher priority. DIF: Cognitive Level: Analyze (analysis) REF: 1556 OBJ: Special Questions: Prioritization | Special Questions: Multiple Patients TOP: Nursing Process: Planning MSC: NCLEX: Safe and Effective Care Environment COMPLETION 1. A patient’s vital signs are pulse 90, respirations 24, and BP 128/64 mm Hg, and cardiac output is 4.7 L/min. The patient’s stroke volume is mL. (Round to the nearest whole number.) ANS: 52 Stroke volume = Cardiac output/heart rate 52 mL = (4.7 L x 1000 mL/L)/90 DIF: Cognitive Level: Understand (comprehension) REF: 1559 TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity OTHER 1. When assisting with oral intubation of a patient who is having respiratory distress, in which order will the nurse take these actions? (Put a comma and a space between each answer choice [A, B, C, D, E].) a. Obtain a portable chest-x-ray. b. Position the patient in the supine position. c. Inflate the cuff of the endotracheal tube after insertion. d. Attach an end-tidal CO2 detector to the endotracheal tube. e. Oxygenate the patient with a bag-valve-mask device for several minutes. ANS: E, B, C, D, A The patient is pre-oxygenated with a bag-valve-mask system for 3 to 5 minutes before intubation and then placed in a supine position. After the intubation, the cuff on the endotracheal tube is inflated to occlude and protect the airway. Tube placement is assessed first with an end-tidal CO2 sensor and then with chest x-ray examination. DIF: Cognitive Level: Analyze (analysis) REF: 1570 OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity 2. The nurse is caring for a patient who has an intraaortic balloon pump (IABP) after a massive heart attack. When assessing the patient, the nurse notices blood backing up into the IABP catheter. In which order should the nurse take the following actions? (Put a comma and a space between each answer choice [A, B, C, D].) a. Confirm that the IABP console has turned off. b. Assess the patient’s vital signs and orientation. c. Obtain supplies for insertion of a new IABP catheter. d. Notify the health care provider of the IABP malfunction. ANS: A, B, D, C Blood in the IABP catheter indicates a possible tear in the balloon. The console should shut off automatically to prevent complications such as air embolism. Next, the nurse will assess the patient and communicate with the health care provider about the patient’s assessment and the IABP problem. Finally, supplies for insertion of a new IABP catheter may be needed based on the patient assessment and the decision of the health care provider. DIF: Cognitive Level: Analyze (analysis) REF: 1568 OBJ: Special Questions: Prioritization TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity [Show More]
Last updated: 1 year ago
Preview 1 out of 47 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 30, 2021
Number of pages
47
Written in
Additional information
This document has been written for:
Uploaded
Jun 30, 2021
Downloads
0
Views
54



.png)
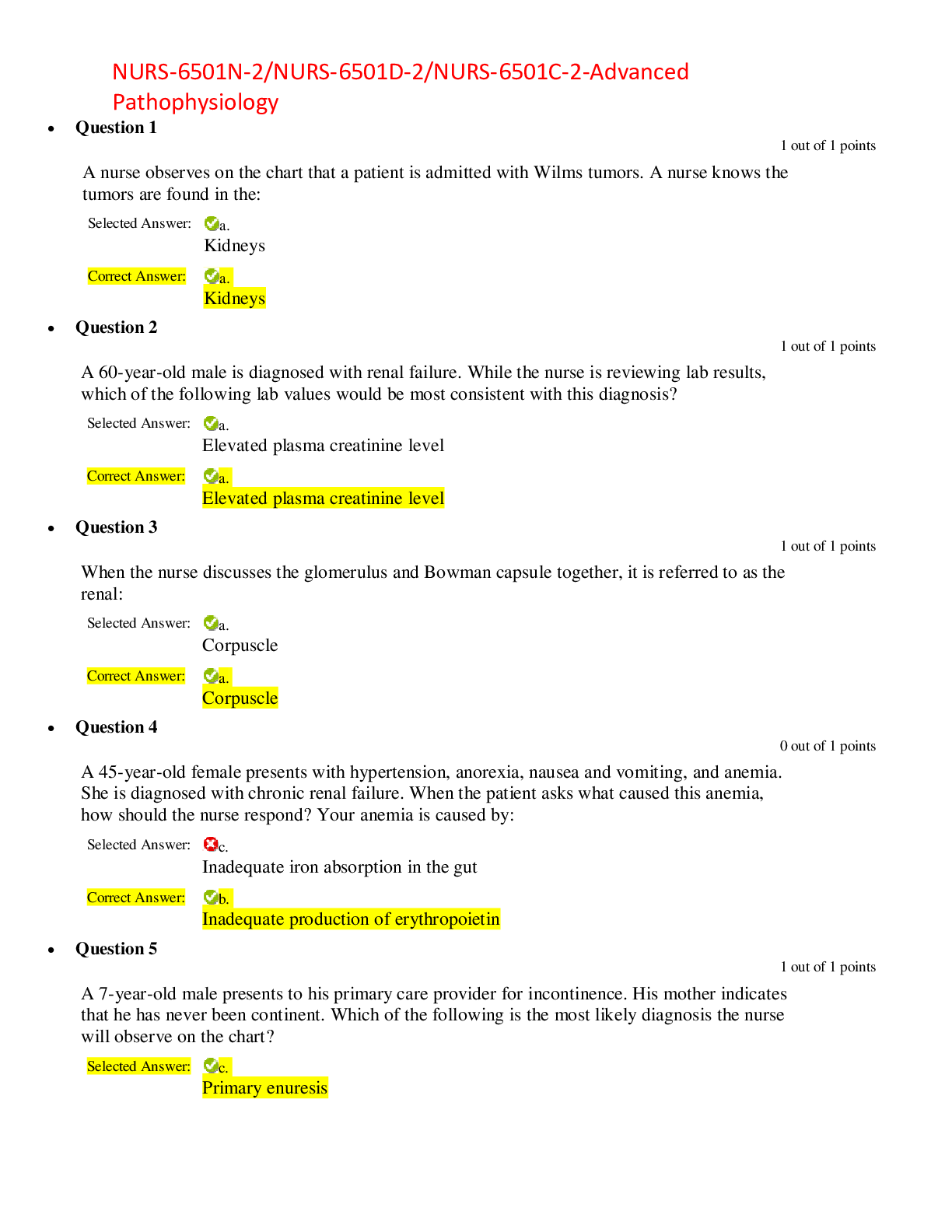
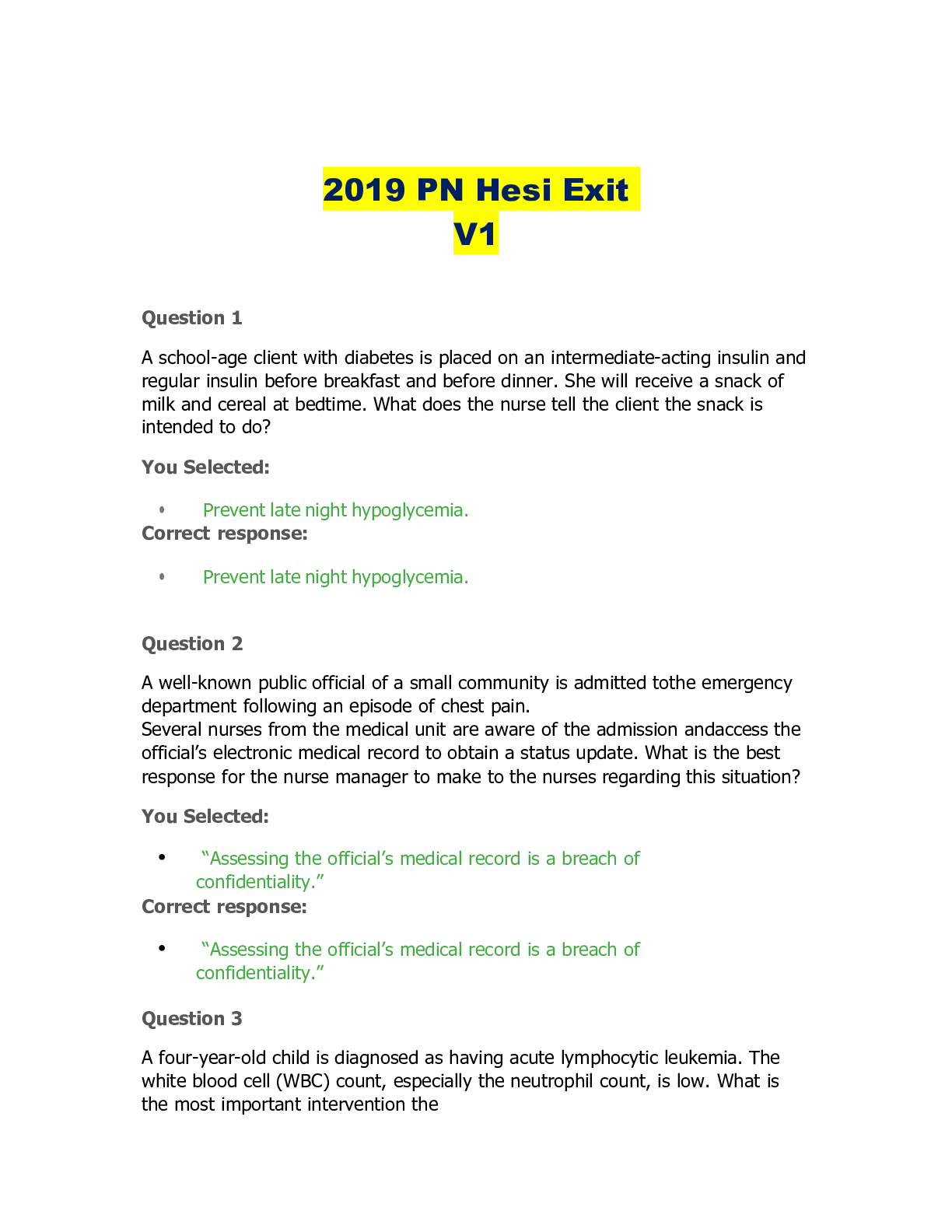

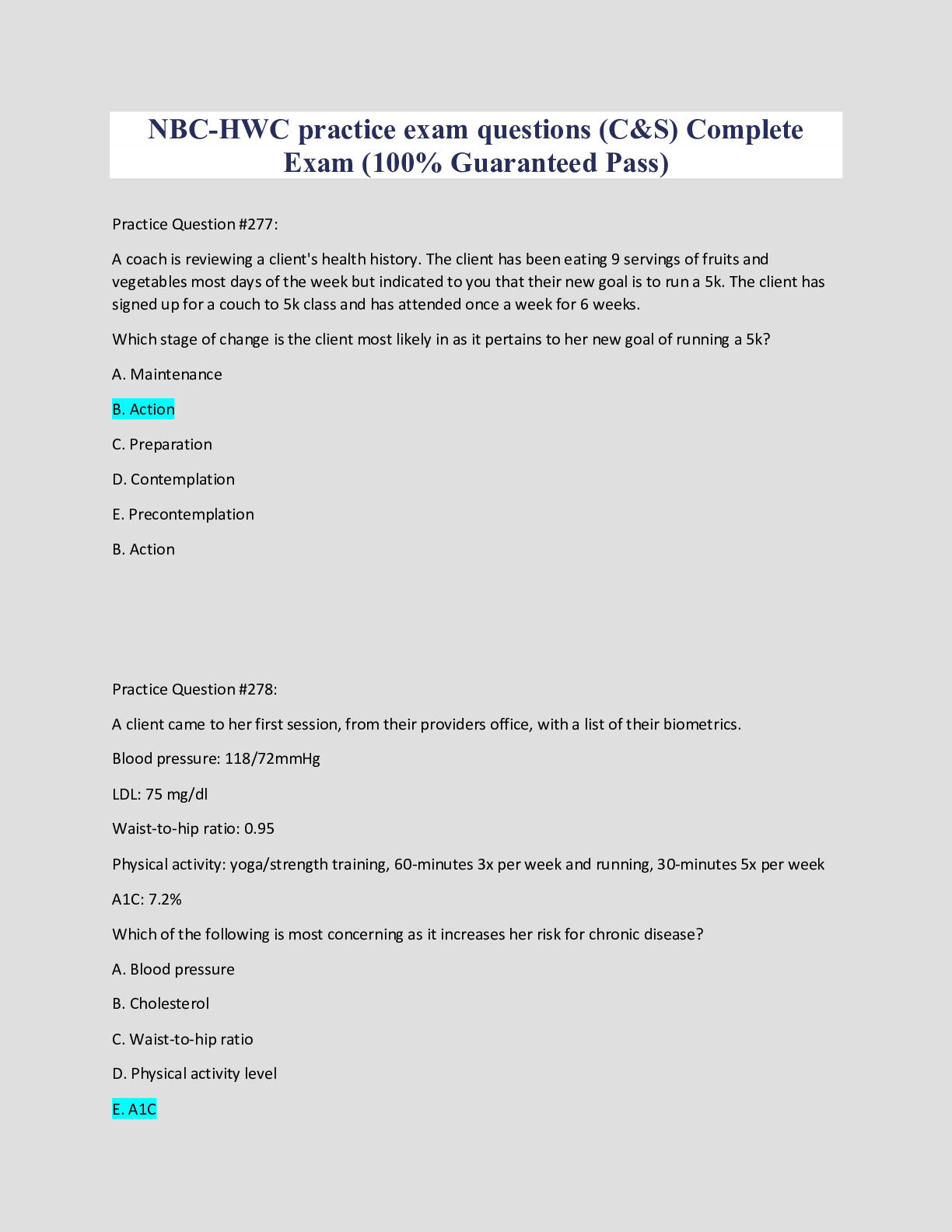
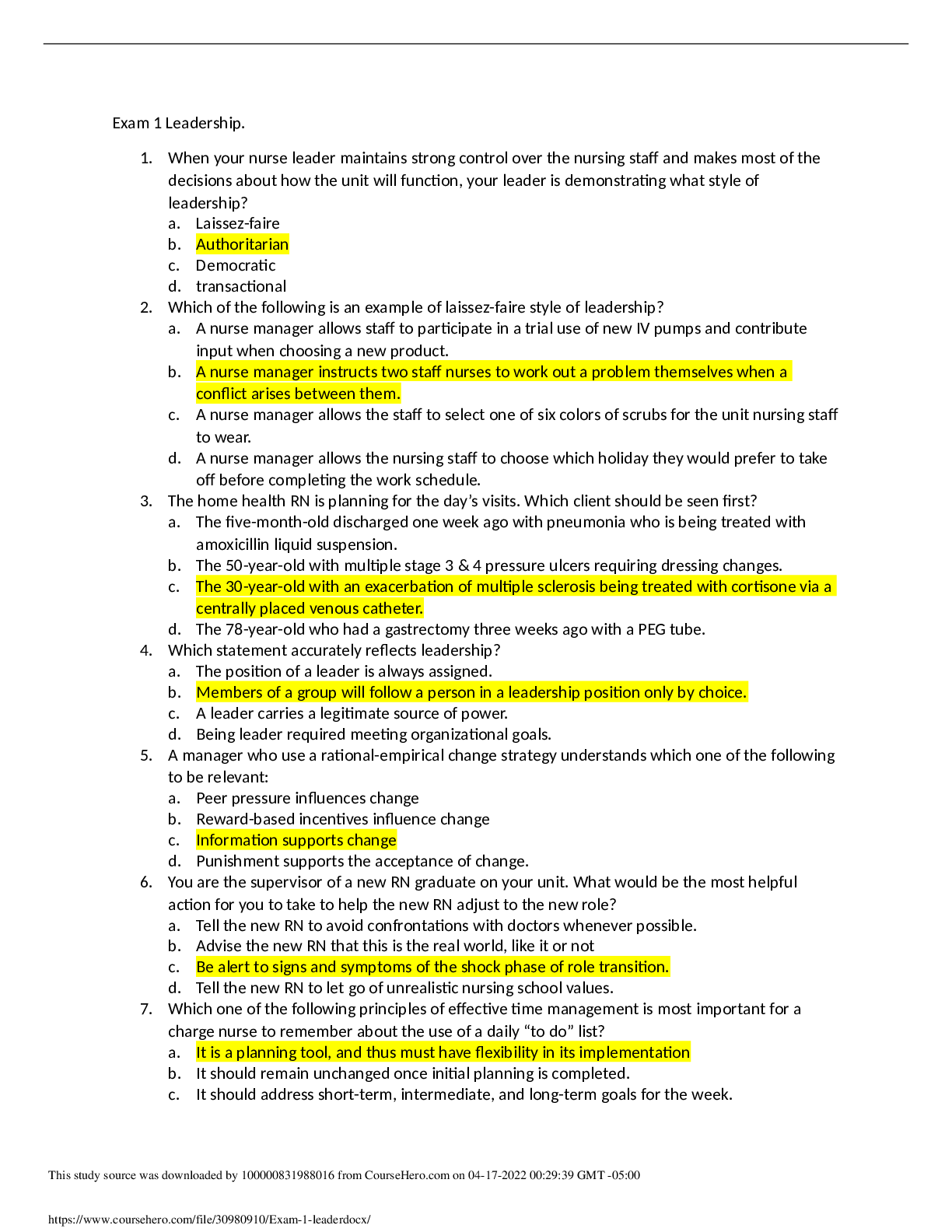
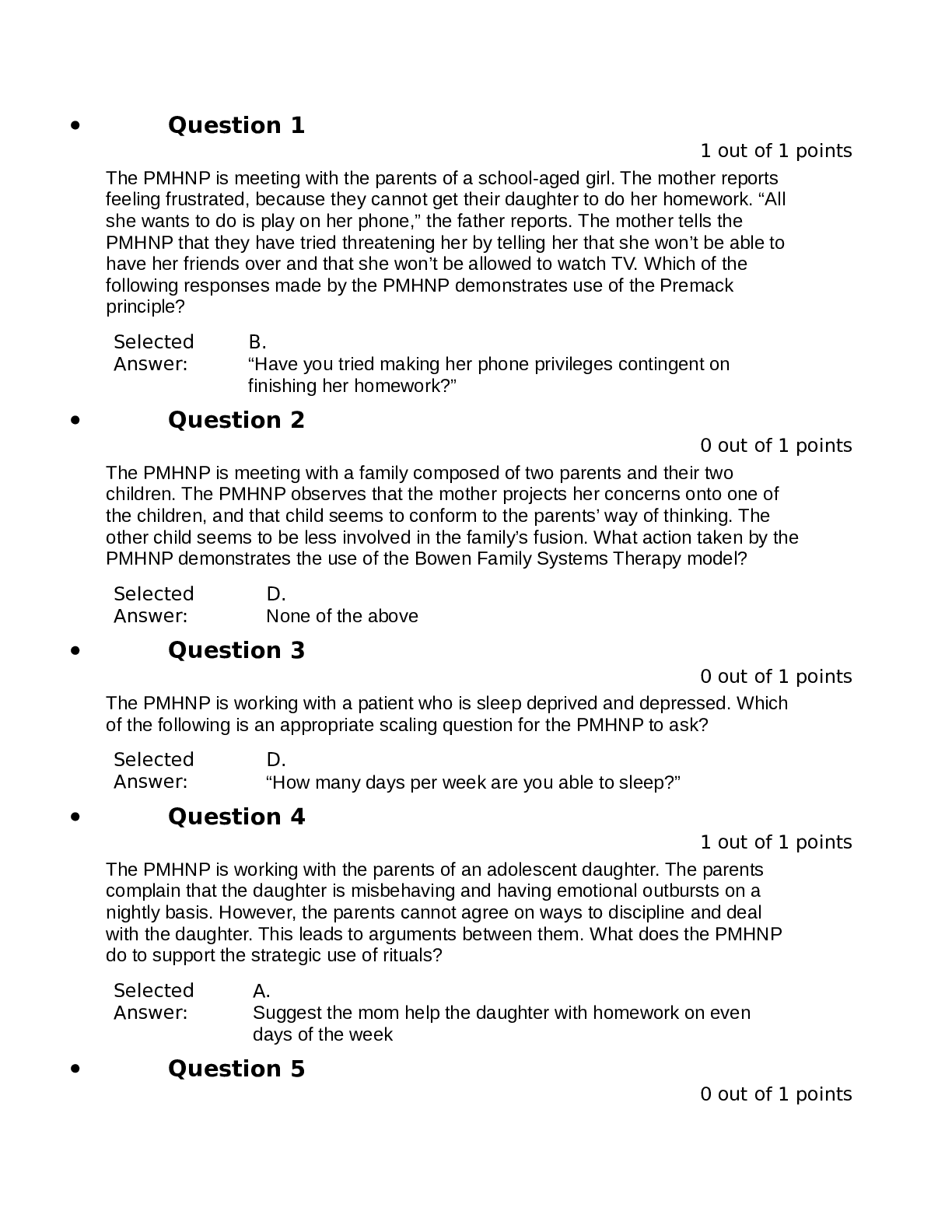
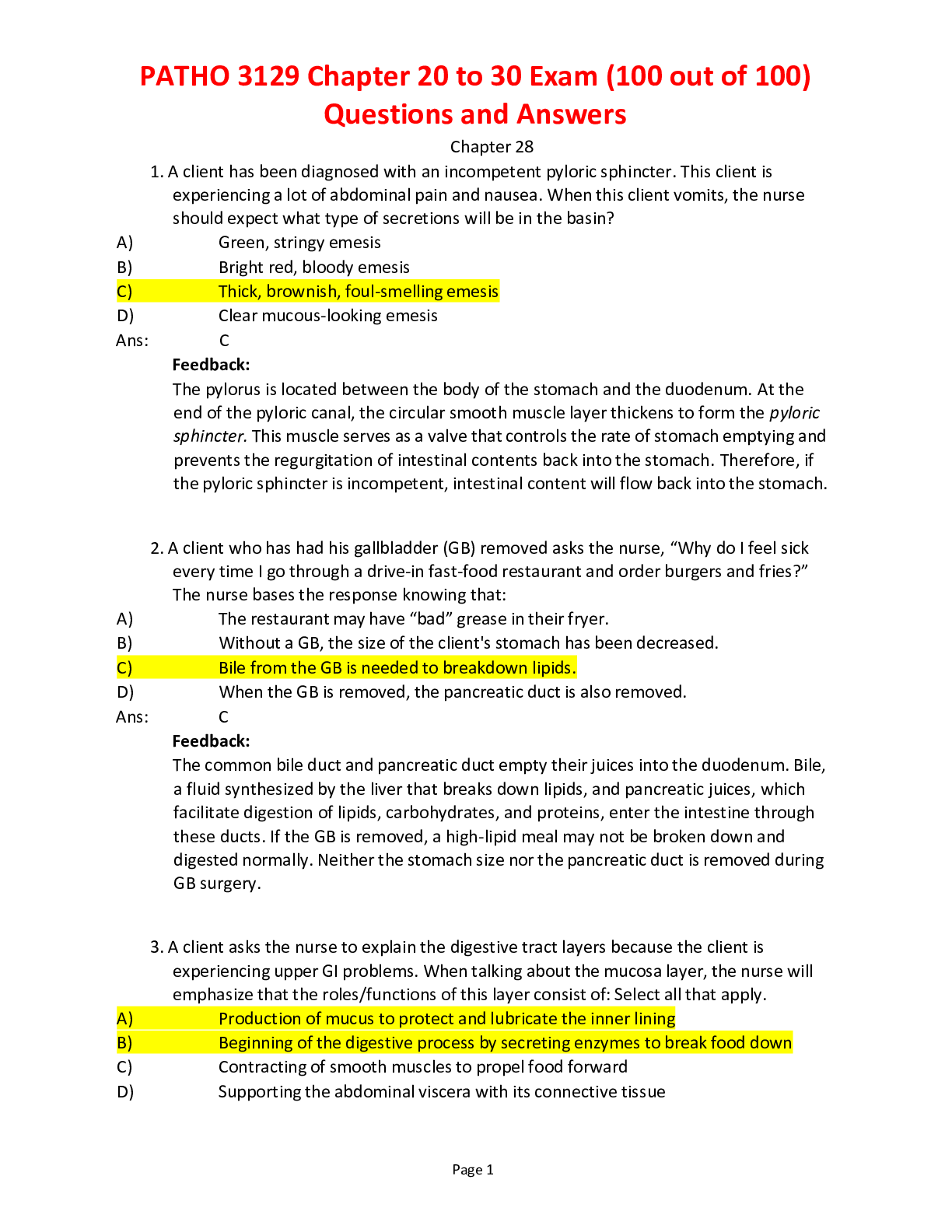
.png)
 (1).png)