*NURSING > STUDY GUIDE > walden university-NURS 6512n midterm-compilation-study-guide-2020/2021 rated-A (All)
walden university-NURS 6512n midterm-compilation-study-guide-2020/2021 rated-A
Document Content and Description Below
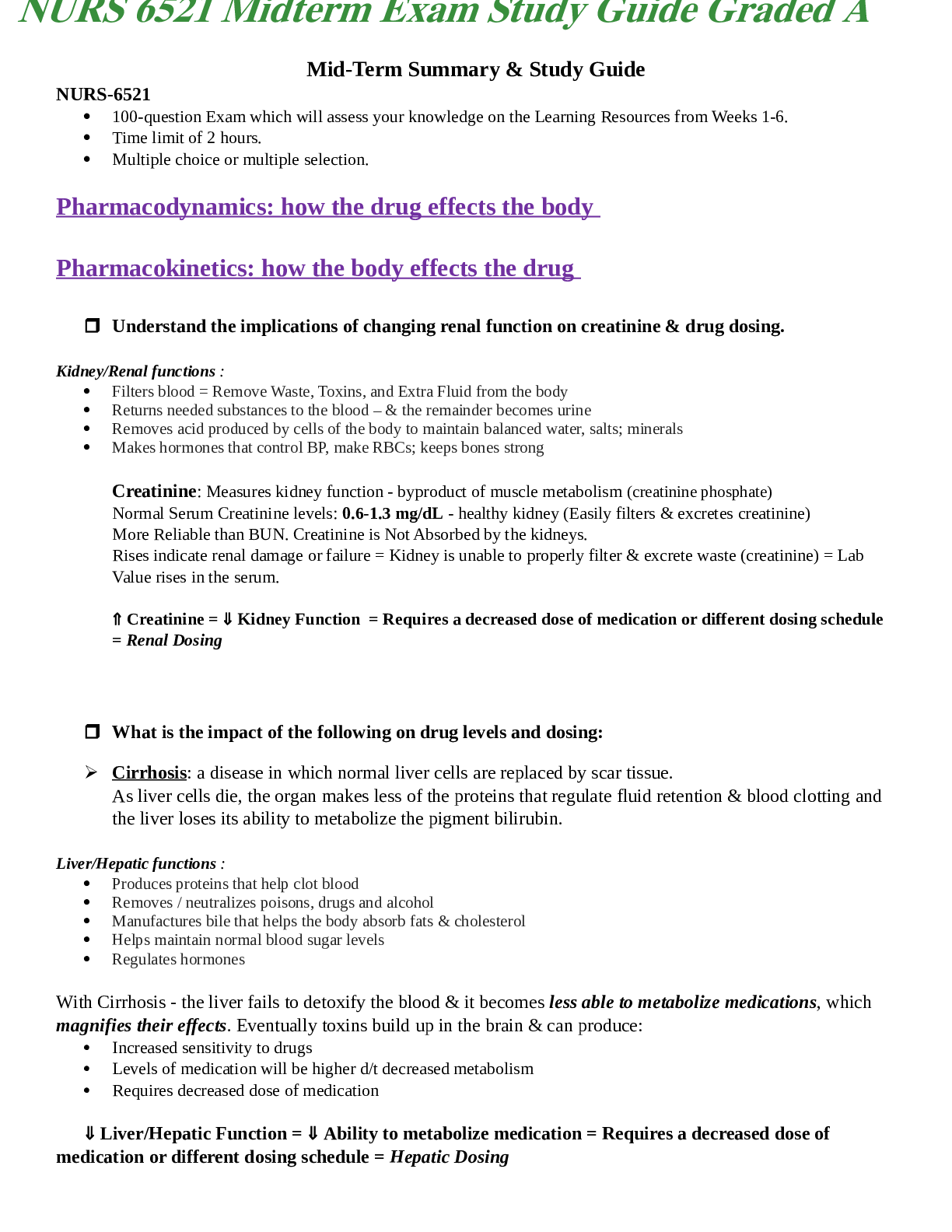
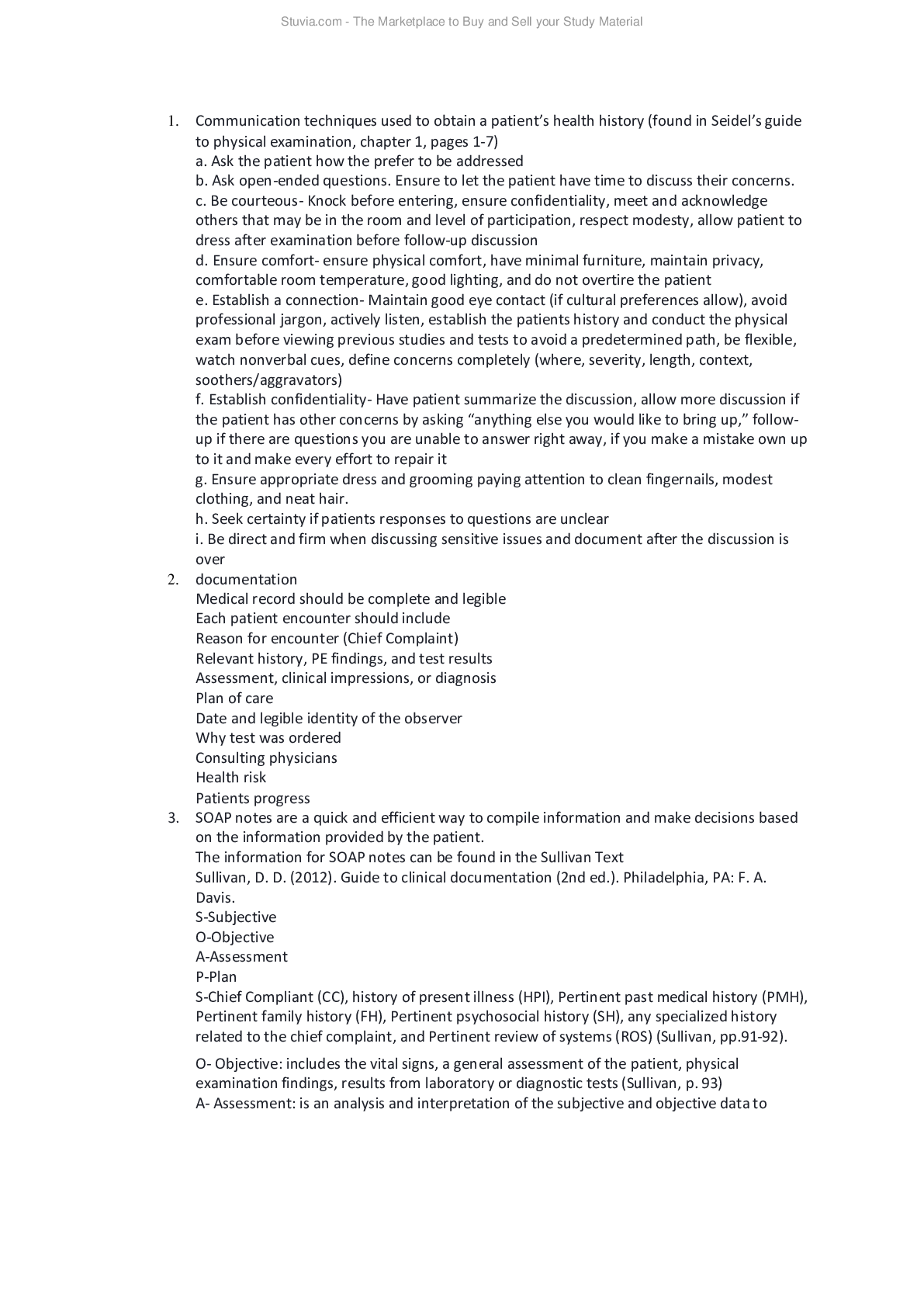
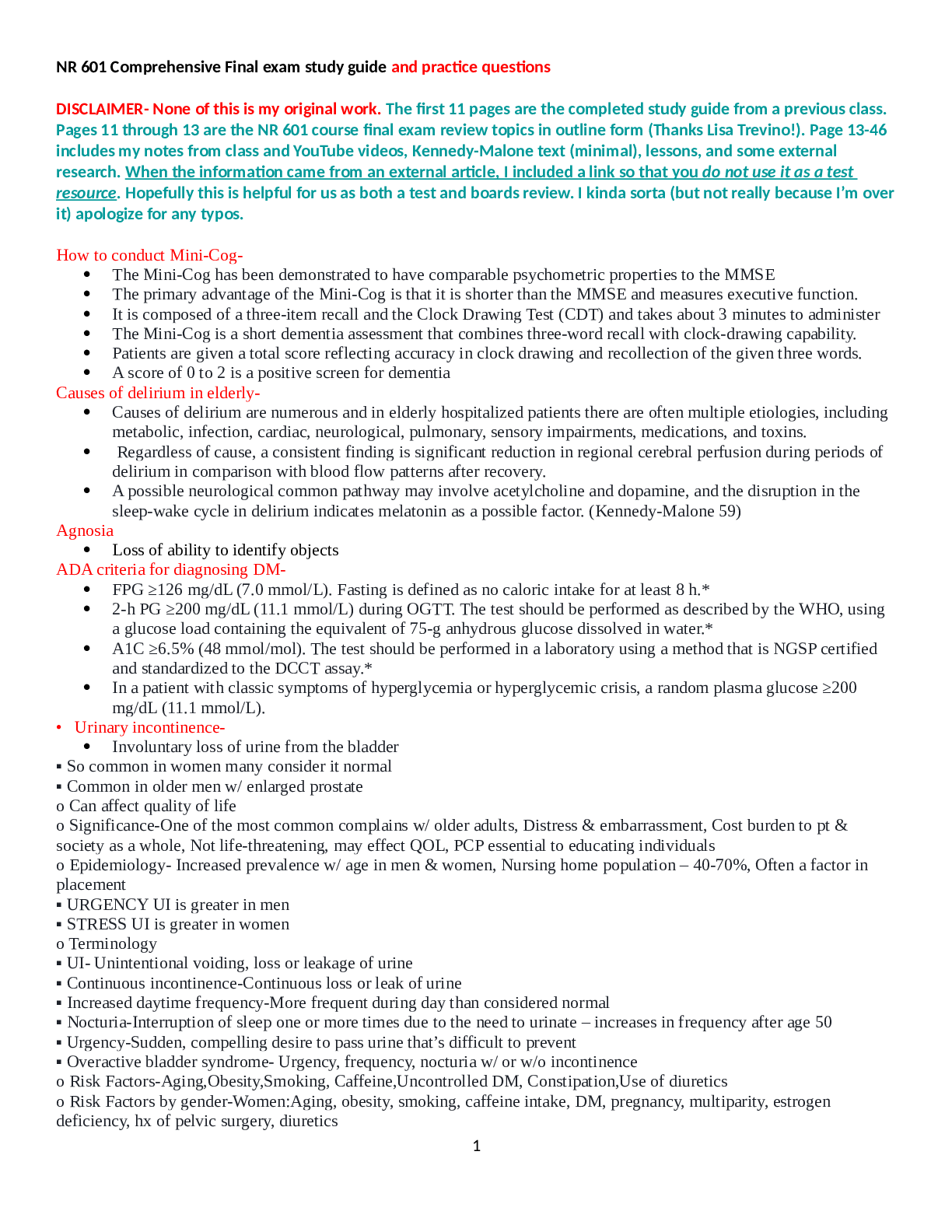
Communication techniques used to obtain a patient’s health history (found in Seidel’s guide to physical examination, chapter 1, pages 1-7) a. Ask the patient how the prefer to be addressed b. Ask ... open-ended questions. Ensure to let the patient have time to discuss their concerns. c. Be courteous- Knock before entering, ensure confidentiality, meet and acknowledge others that may be in the room and level of participation, respect modesty, allow patient to dress after examination before follow-up discussion d. Ensure comfort- ensure physical comfort, have minimal furniture, maintain privacy, comfortable room temperature, good lighting, and do not overtire the patient e. Establish a connection- Maintain good eye contact (if cultural preferences allow), avoid professional jargon, actively listen, establish the patients history and conduct the physical exam before viewing previous studies and tests to avoid a predetermined path, be flexible, watch nonverbal cues, define concerns completely (where, severity, length, context, soothers/aggravators) f. Establish confidentiality- Have patient summarize the discussion, allow more discussion if the patient has other concerns by asking “anything else you would like to bring up,” follow- up if there are questions you are unable to answer right away, if you make a mistake own up to it and make every effort to repair it g. Ensure appropriate dress and grooming paying attention to clean fingernails, modest clothing, and neat hair. h. Seek certainty if patients responses to questions are unclear i. Be direct and firm when discussing sensitive issues and document after the discussion is over 2. documentation Medical record should be complete and legible Each patient encounter should include Reason for encounter (Chief Complaint) Relevant history, PE findings, and test results Assessment, clinical impressions, or diagnosis Plan of care Date and legible identity of the observer Why test was ordered Consulting physicians Health risk Patients progress 3. SOAP notes are a quick and efficient way to compile information and make decisions based on the information provided by the patient. The information for SOAP notes can be found in the Sullivan Text Sullivan, D. D. (2012). Guide to clinical documentation (2nd ed.). Philadelphia, PA: F. A. Davis. S-Subjective O-Objective A-Assessment P-Plan S-Chief Compliant (CC), history of present illness (HPI), Pertinent past medical history (PMH), Pertinent family history (FH), Pertinent psychosocial history (SH), any specialized history related to the chief complaint, and Pertinent review of systems (ROS) (Sullivan, pp.91-92). O- Objective: includes the vital signs, a general assessment of the patient, physical examination findings, results from laboratory or diagnostic tests (Sullivan, p. 93) A- Assessment: is an analysis and interpretation of the subjective and objective dat [Show More]
Last updated: 1 year ago
Preview 1 out of 49 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 25, 2021
Number of pages
49
Written in
Additional information
This document has been written for:
Uploaded
Apr 25, 2021
Downloads
0
Views
37

_removed.png)

.png)







.png)