Pathophysiology > EXAM > PATHOPHYSIOLOGY 6501 MIDTERM EXAM. Already Graded A (All)
PATHOPHYSIOLOGY 6501 MIDTERM EXAM. Already Graded A
Document Content and Description Below
Patho Midterm Chapter 1: Cellular Biology 1. Which statement best describes the cellular function of metabolic absorption? Ans: Cells can take in and use nutrients. 2. Most of a cell’s genetic i... nformation, including RNA and DNA, is contained in the: Ans: Nucleolus 3. Which component of the cell produces hydrogen peroxide (H2O2) by using oxygen to remove hydrogen atoms from specific substrates in an oxidative reaction? Ans: Peroxisomes 4. Which cell component is capable of cellular autodigestion when it is released during cell injury? Ans: Lysosomes 5. What is the sequence of steps in the development of a digestive enzyme by the pancreas cells from the initial transcription to the release from the cell? Ans: The enzyme is transcribed from DNA by RNA in the nucleus, proceeds to the ribosome for synthesis, and is transported in a secretory vesicle to the cell membrane. 6. During which phase of the cell cycle is DNA synthesized? Ans: S (synthesis) 7. What organic compound facilitates transportation across cell membranes by acting as receptors, transport channels for electrolytes, and enzymes to drive active pumps? Ans: Proteins 8. Understanding the various steps of proteolytic cascades, such as caspase-mediated apoptosis and complement cascades, may be useful in designing drug therapy for which human diseases? Ans: Autoimmune and malignant disorders 9. Which structure prevents water-soluble molecules from entering cells across the plasma membrane? Ans: Lipid bilayer 10. The fluid mosaic model explains: Ans: How a cell membrane functions 11. Which form of cell communication is used to communicate within the cell itself and with other cells in direct physical contact? Ans: Protein channel (gap junction) 12. Which mode of chemical signaling uses blood to transport communication to cells some distance away? Ans: Hormonal 13. Which mode of chemical signaling uses local chemical mediators that are quickly taken up, destroyed, or immobilized? Ans: Paracrine 14. Neurotransmitters affect the postsynaptic membrane by binding to: Ans: Receptors 15. How do cells receive communication from the extracellular fluid surrounding them? Ans: Chemical messengers such as ligands 16. When a second message is necessary for extracellular communication to be activated, it is provided by which one? Ans: Adenosine monophosphate (AMP) d. Guanosine diphosphate (GDP) 17. Under anaerobic conditions, what process provides energy for the cell? Ans: Glycolysis 18. What is the mechanism by which the energy produced from carbohydrates, proteins, and lipids is transferred to adenosine triphosphate (ATP)? Ans: Oxidative phosphorylation 19. Passive transport is best described with which statement? Ans: Being driven by osmosis, hydrostatic pressure, and diffusion 20. Active transport occurs across which type of membranes? Ans: Membranes that have receptors that are capable of binding with the substances to be transported 21. Which method of transport uses transmembrane proteins with receptors with a high degree of specificity for the substance being transported? Ans: Mediated 22. The movement of fluid across the arterial end of capillary membranes into the interstitial fluid surrounding the capillary is an example of which fluid movement process? Ans: Hydrostatic pressure 23. Why is osmolality preferred over osmolarity as the measurement of osmotic activity in the clinical assessment of individuals? Ans: More of the weight of plasma is influenced by solutes, such as protein and glucose, rather than by water. 24. A patient who has diarrhea receives a 3% saline solution intravenously to replace the sodium and chloride lost in the stool. What effect will this fluid replacement have on cells? Ans: Shrink 25. The transport of glucose from the blood to the cell is accomplished by which process? Ans: Passive-mediated transport (facilitated diffusion) 26. Potassium and sodium are transported across plasma membranes by: Ans: Adenosine triphosphatase (ATPase) enzyme 27. What occurs during exocytosis? Ans: Macromolecules can be secreted across eukaryotic cell membranes. 28. Why is it possible for potassium to diffuse easily into and out of cells? Ans: The resting plasma membrane is more permeable to potassium. 29. The cellular uptake of the nutrient cholesterol depends on which process? Ans: Receptor-mediated endocytosis 30. What causes the rapid change in the resting membrane potential to initiate an action potential? Ans: Sodium gates open, and sodium rushes into the cell, changing the membrane potential from negative to positive. 31. The action of platelet-derived growth factor is to stimulate the production of which cells? Ans: Connective tissue cells 32. The role of cytokines in cell reproduction is that they: Ans: Provide growth factor for tissue growth and development. 33. What is the process of cellular reproduction? Ans: Two diploid cells, called daughter cells, have been formed. 34. Which statement is true about eukaryotic cells? Ans: They contain compartments called organelles. 35. Which statement is true about phagocytosis? Ans: Phagocytosis involves the ingestion of bacteria. 36. A muscle cell possesses which specialized function? Ans: Movement 37. When a mucous gland cell creates a new substance from previously absorbed material, this process is known as which specialized cellular function? Ans: Secretion 38. All cells are capable of what process? Ans: Excretion 39. What are the major chemical components of the cell membranes? Ans: Lipids Proteins 40. Which cells lose their ability to replicate and divide? Ans: Nerves Lens of the eye Skeletal muscle 41. Which statements are true concerning the process of facilitated diffusion? Ans: Facilitated diffusion is also referred to as passive mediated transport. This process expends no metabolic energy. Moving solute molecules through cellular membranes are involved in this process. 42. Passive transport is dependent on: Ans: Semipermeable barrier membrane The process of osmosis Diffusion as a driving force Hydrostatic pressure 43. What is the primary function of proteins? Ans: Proteins are binding units. Proteins are transport channels. Proteins provide cell surface markers. Proteins are chemical reaction catalysts. Match the structure with its function. Answers may be used more than once. B. Ribosome 44. Packages and transports proteins. A. Endoplasmic reticulum 45. Fuses with the plasma membrane to release contents from the cell. C. Secretory vesicle 46. Synthesizes and transports lipids. A. Endoplasmic reticulum 47. Provides energy to digest proteins into amino acids. D. Lysosomes Match the structure with its function. Answers may be used more than once. 48. Movement of water C. Osmosis 49. Protein carrier B. Active-mediated transport 50. Facilitated diffusion A. Passive-mediated transport Chapter 2: Altered Cellular and Tissue Biology 1. Which type of cell adaptation occurs when normal columnar ciliated epithelial cells of the bronchial lining have been replaced by stratified squamous epithelial cells? Ans: Metaplasia 2. The loss of the adenosine triphosphate (ATP) during ischemia causes cells to: Ans: Swell because of the influx of sodium chloride (NaCl). 3. The mammary glands enlarge during pregnancy primarily as a consequence of hormonal: Ans: Hyperplasia 4. Free radicals play a major role in the initiation and progression of which diseases? Ans: Cardiovascular diseases such as hypertension and ischemic heart disease 5. Free radicals cause cell damage by: Ans: Giving up an electron, which causes injury to the chemical bonds of the cell membrane 6. What is a consequence of plasma membrane damage to the mitochondria? Ans: Influx of calcium ions halts ATP production. 7. What is a consequence of leakage of lysosomal enzymes during chemical injury? Ans: Enzymatic digestion of the nucleus and nucleolus occurs, halting DNA synthesis. 8. Lead causes damage within the cell by interfering with the action of: Ans: Calcium 9. Which statement is a description of the characteristics of apoptosis? Ans: Programmed cell death of scattered, single cells 10. Lead poisoning affects the nervous system by: Ans: Interfering with the function of neurotransmitters 11. Carbon monoxide causes tissue damage by: Ans: Binding to hemoglobin so that it cannot carry oxygen 12. Acute alcoholism mainly affects which body system? Ans: Central nervous 13. During cell injury caused by hypoxia, an increase in the osmotic pressure occurs within the cell because: Ans: Sodium chloride enters the cell. 14. Which statement is true regarding the difference between subdural hematoma and epidural hematoma? Ans: A subdural hematoma is often the result of shaken baby syndrome, whereas an epidural hematoma rapidly forms as a result of a skull fracture. 15. What physiologic change occurs during heat exhaustion? Ans: Hemoconcentration occurs because of the loss of salt and water. 16. In hypoxic injury, sodium enters the cell and causes swelling because: Ans: ATP is insufficient to maintain the pump that keeps sodium out of the cell. 17. What is the most common site of lipid accumulation? Ans: Liver 18. What mechanisms occur in the liver cells as a result of lipid accumulation? Ans: Increased synthesis of triglycerides from fatty acids and decreased synthesis of apoproteins 19. Hemoprotein accumulations are a result of the excessive storage of: Ans: Iron, which is transferred from the cells to the bloodstream 20. Hemosiderosis is a condition that results in the excess of what substance being stored as hemosiderin in cells of many organs and tissues? Ans: Iron 21. What is the cause of free calcium in the cytosol that damages cell membranes by uncontrolled enzyme activation? Ans: Depletion of ATP normally pumps calcium from the cell. 22. What two types of hearing loss are associated with noise? Ans: Acoustic trauma and noise-induced 23. What type of necrosis results from ischemia of neurons and glial cells? Ans: Liquefactive 24. What type of necrosis is often associated with pulmonary tuberculosis? Ans: Caseous 25. What type of necrosis is associated with wet gangrene? Ans: Liquefactive 26. Current research supports the believe that, after heart muscle injury, the damage: Ans: Is repaired by newly matured cardiomyocytes. 27. After ovulation, the uterine endometrial cells divide under the influence of estrogen. This process is an example of hormonal: Ans: Hyperplasia 28. The abnormal proliferation of cells in response to excessive hormonal stimulation is called: Ans: Pathologic hyperplasia 29. Removal of part of the liver leads to the remaining liver cells undergoing compensatory: Ans: Hyperplasia 30. What is the single most common cause of cellular injury? Ans: Hypoxic injury 31. During cell injury caused by hypoxia, sodium and water move into the cell because: Ans: The pump that transports sodium out of the cell cannot function because of a decrease in ATP levels. 32. In decompression sickness, emboli are formed by bubbles of: Ans: Nitrogen 33. Which is an effect of ionizing radiation exposure? Ans: DNA aberrations 34. What is an example of compensatory hyperplasia? Ans: Hepatic cells increase cell division after part of the liver is excised. 35. It is true that nondividing cells are: Ans: Found in gastrointestinal lining 36. Dysplasia refers to a(n): Ans: Modification in the shape of a specific cell type 37. Current research has determined that chemical-induced cellular injury: Ans: Is often the result of the damage caused by reactive free radicals. 38. Which organs are affected by lead consumption? Ans: Bones Nerves 39. What effect does fetal alcohol syndrome have on newborns? Ans: Cognitive impairment Facial anomalies 40. What organs are affected by the type of necrosis that results from either severe ischemia or chemical injury? Ans: Kidneys Heart 41. It is true that melanin is: Ans: Found in cells called keratinocytes, which are present in the retina A factor in the prevention of certain types of cancer Accumulated in specific cells found in the skin 42. Examples of adaptive cellular responses include: Ans: Atrophy Hypertrophy Hyperplasia Metaplasia 43. Blunt force injuries would include a: Ans: Bruise to the upper arm, resulting from a fall Simple tibia fracture sustained in a skiing accident Spleen laceration caused by a punch during a physical fight 44. Which statements are true regarding the effects of marijuana use? Ans: Smoking the drug results in greater absorption that eating it. Heavy use can result in psychomotor impairments. Smoking four “joints” a day equals smoking approximately 20 cigarettes. Chapter 3: The Cellular Environment: Fluids and Electrolytes, Acids and Bases 1. Infants are most susceptible to significant losses in total body water because of an infant’s: Ans: Kidneys are not mature enough to counter fluid losses 2. Obesity creates a greater risk for dehydration in people because: Ans: Adipose cells contain little water because fat is water repelling. 3. A patient’s blood gases reveal the following findings: pH, 7.3; bicarbonate (HCO3) 27 mEq/L; carbon dioxide (CO2), 58 mm Hg. What is the interpretation of these gases? Ans: Respiratory acidosis 4. Water movement between the intracellular fluid (ICF) compartment and the extracellular fluid (ECF) compartment is primarily a function of: Ans: Osmotic forces 5. In addition to osmosis, what force is involved in the movement of water between the plasma and interstitial fluid spaces? Ans: Hydrostatic pressure 6. Venous obstruction is a cause of edema because of an increase in which pressure? Ans: Capillary hydrostatic 7. At the arterial end of capillaries, fluid moves from the intravascular space into the interstitial space because the: Ans: Capillary hydrostatic pressure is higher than the capillary oncotic pressure. 8. Low plasma albumin causes edema as a result of a reduction in which pressure? Ans: Plasma oncotic 9. Secretion of antidiuretic hormone (ADH) and the perception of thirst are stimulated by a(n): Ans: Increase in plasma osmolality 10. Thirst activates osmoreceptors by an increase in which blood plasma? Ans: Osmotic pressure 11. It is true that natriuretic peptides: Ans: Decrease blood pressure and increase sodium and water excretion. 12. When changes in total body water are accompanied by proportional changes in electrolytes, what type of alteration occurs? Ans: Isotonic 13. Which enzyme is secreted by the juxtaglomerular cells of the kidney when circulating blood volume is reduced? Ans: Renin 14. What mechanism can cause hypernatremia? Ans: Hypersecretion of aldosterone 15. What causes the clinical manifestations of confusion, convulsions, cerebral hemorrhage, and coma in hypernatremia? Ans: High sodium in the blood vessels pulls water out of the brain cells into the blood vessels, causing brain cells to shrink. 16. Vomiting-induced metabolic alkalosis, resulting in the loss of chloride, causes: Ans: Retention of bicarbonate to maintain the anion balance 17. The pathophysiologic process of edema is related to which mechanism? Ans: Lymphatic obstruction 18. Insulin is used to treat hyperkalemia because it: Ans: Transports potassium from the blood to the cell along with glucose. 19. A major determinant of the resting membrane potential necessary for the transmission of nerve impulses is the ratio between: Ans: Intracellular and extracellular K+ 20. During acidosis, the body compensates for the increase in serum hydrogen ions by shifting hydrogen ions into the cell in exchange for which electrolyte? Ans: Potassium 21. Causes of hyperkalemia include: Ans: Renal failure and Addison disease 22. In hyperkalemia, what change occurs to the cells’ resting membrane potential? Ans: Hypopolarization 23. The calcium and phosphate balance is influenced by which three substances? Ans: Parathyroid hormone, calcitonin, and vitamin D 24. It is true that Kussmaul respirations indicate: Ans: A compensatory measure is needed to correct metabolic acidosis. 25. Chvostek and Trousseau signs indicate which electrolyte imbalance? Ans: Hypocalcemia 26. An excessive use of magnesium-containing antacids and aluminum-containing antacids can result in: Ans: Hypophosphatemia 27. The most common cause of hypermagnesemia is: Ans: Renal failure 28. Physiologic pH is maintained at approximately 7.4 because bicarbonate (HCO3) and carbonic acid (H2CO3) exist in a ratio of: Ans: 20:1 29. Which arterial pH will initiate the formation of ammonium (NH4) from ammonia (NH3), referred to as academia, in the tubular lumen of the kidney? Ans: 7.25 30. Two thirds of the body’s water is found in its: Ans: Intracellular fluid compartments 31. It is true that when insulin is administered: Ans: The liver increases its potassium levels. 32. Increased capillary hydrostatic pressure results in edema because of: Ans: Sodium and water retention 33. The existence of hyperkalemia is likely to result in which changes to a person’s ECG? Ans: Peaked T waves 34. Which groups are at risk for fluid imbalance? Ans: Infants Obese persons Older adults 35. Dehydration can cause which result? Ans: Weak pulses Tachycardia Weight loss 36. Causes of hypocalcemia include: Ans: Repeated blood administration Pancreatitis 37. The electrolyte imbalance called hyponatremia exhibits which clinical manifestations? Ans: Headache Seizures Confusion Lethargy 38. The electrolyte imbalance hypercalcemia exhibits which clinical manifestations? Ans: Calcium based kidney stones Lethargy Bradycardia 39. The electrolyte imbalance hypokalemia exhibits which clinical manifestations? Ans: Paralytic ileus Sinus bradycardia Atrioventricular block 40. A third of the body’s fluid is contained in the extracellular interstitial fluid spaces that include: Ans: Urine Intraocular fluids Lymph Sweat 41. An imbalance of potassium can produce which dysfunctions? Ans: Weakness skeletal muscles Cardiac dysrhythmias Smooth muscle atony 42. Which statements regarding total body water (TBW) are true? Ans: During childhood, TBW slowly decreases in relationship to body weight. Men tend to have greater TBW as a result of their muscle mass. Estrogen plays a role in female TBW. Older adults experience a decrease in TBW as a result of decreased muscle mass. Match the electrolytes with the corresponding descriptions. Terms may be used more than once. D. Magnesium 43. Regulates osmolality in the extracellular fluid (ECF) space. A. Sodium 44. Is inversely related to HCO3 concentration. B. Chloride 45. Is a major determinant of resting membrane potential. C. Potassium 46. An intracellular metabolic form is adenosine triphosphate (ATP). E. Phosphate 47. Changes in hydrogen ion concentration affect this electrolyte. C. Potassium Chapter 4: Genes and Genetic Diseases 1. Inserting bone marrow cells into an individual who produces abnormal erythrocytes is an example of what type of therapy? Ans: Somatic cell 2. DNA replication requires the enzyme DNA polymerase to: Ans: Travel along the single DNA strand, adding the correct nucleotide to the new strand 3. Transcription is best defined as a process by which: Ans: RNA is synthesized from a DNA template. 4. The purpose of a staining technique of chromosomes such as Giemsa is to: Ans: Allow for the numbering of chromosomes and the identification of variations. 5. An amniocentesis indicates a neural tube defect when an increase in which protein is evident? Ans: Alpha fetoprotein 6. An amniocentesis is recommended for pregnant women who: Ans: Have a family history of genetic disorders 7. The most clinically useful technique for prenatal diagnosis of chromosomal abnormalities at 3 months’ (12 weeks’) gestation is: Ans: Chorionic villus sampling 8. The term for an error in which homologous chromosomes fail to separate during meiosis or mitosis is: Ans: Nondisjunction 9. Which clinical manifestations would be expected for a child who has complete trisomy of the twenty-first chromosome? Ans: An IQ of 25 to 70, low nasal bridge, protruding tongue, and flat, low-set ears 10. What is the most common cause of Down syndrome? Ans: Maternal nondisjunction 11. What syndrome, characterized by an absent homologous X chromosome with only a single X chromosome, exhibits features that include a short stature, widely spaced nipples, and webbed neck? Ans: Turner 12. A person with 47, XXY karyotype has the genetic disorder resulting in which syndrome? Ans: Klinefelter 13. What is the chromosomal variation that causes Klinefelter syndrome? Ans: Nondisjunction of X chromosome in the mother 14. What is the second most commonly recognized genetic cause of mental retardation? Ans: Fragile X syndrome 15. What is the blood type of a person who is heterozygous, having A and B alleles as codominant? Ans: AB 16. A couple has two children diagnosed with an autosomal dominant genetic disease. What is the probability that the next child will have the same genetic disease? Ans: One half 17. When a child inherits a disease that is autosomal recessive, it is inherited from: Ans: Both parents 18. People diagnosed with neurofibromatosis have varying degrees of the condition because of the genetic principle of: Ans: Expressivity 19. Which genetic disease has been linked to a mutation of the tumor-suppressor gene? Ans: Retinoblastoma 20. Cystic fibrosis is caused by what type of gene? Ans: Autosomal recessive 21. Which is an important criterion for discerning autosomal recessive inheritance? Ans: Consanguinity is sometimes present. 22. Consanguinity refers to the mating of persons: Ans: Having common family relations 23. Males, having only one X chromosome (as is expected), are said to be: Ans: Hemizygous 24. Males are more often affected by which type of genetic disease? Ans: Sex-linked recessive 25. An X-linked recessive disease can skip generations because: Ans: The disease can be transmitted through female carriers. 26. The presence of a zygote having one chromosome with the normal complement of genes and one with a missing gene is characteristic of which genetic disorder? Ans: Cri du chat 27. A child with which genetic disorder has a characteristic cry? Ans: Cri du chat 28. Which statement is true regarding X-linked recessive conditions? Ans: These conditions are passed from affected father to all of his female children. 29. DNA formation occurs in which of the cell’s structures? Ans: Nucleus 30. What is the risk for the recurrence of autosomal dominant diseases? Ans: 50% 31. An individual’s genetic makeup is referred to as his or her: Ans: Genotype 32. Which disorders have similar modes of inheritance? Ans: Duchenne muscular dystrophy Becker muscular dystrophy 33. The key to accurate DNA replication depends on which complementary base pairs? Ans: Adenine with thymine Guanine with cytosine 34. Chromosomal abnormalities are the leading known cause of: Ans: Mental retardation Fetal miscarriage 35. Examples of prenatal diagnostic studies include: Ans: Chorionic villus sampling (CVS) Amniocentesis Preimplantation genetic diagnosis (PGD) 36. The advantage derived from human genome sequencing on genetic disorders focuses on: Ans: Identification of the mutated gene Diagnosis of the existing disorder Appropriate treatment Match the genetic terms with the corresponding diseases. Terms may be used more than once. C. X-linked dominant 37. Cystic fibrosis B. Autosomal recessive 38. Duchenne muscular dystrophy D. X-linked recessive 39. Sickle cell disease B. Autosomal recessive 40. Huntington disease A. Autosomal dominant Chapter 5: Genes, Environment-Lifestyle, and Common Diseases 1. The data reporting that sickle cell disease affects approximately 1 in 600 American blacks is an example of which concept? Ans: Prevalence 2. The ratio of the disease among the exposed population to the disease rate in an unexposed population is referred to as what type of risk? Ans: Relative 3. Empirical risks for most multifactorial diseases are based on: Ans: Direct observation 4. What is the cause of familial hypercholesterolemia (FH)? Ans: Reduction in the number of low-density lipoprotein (LDL) receptors on cell surfaces 5. Which risk factor for hypertension is influenced by genetic factors and lifestyle? Ans: Obesity 6. What percentage of all cases of breast cancer are identified as an autosomal dominant form? Ans: 5 7. When a woman has one first-degree relative with breast cancer, her risk of developing breast cancer is how many times greater? Ans: 2 8. Adoption studies have shown that the offspring of an alcoholic parent when raised by nonalcoholic parents have what amount of an increased risk of developing alcoholism? Ans: Fourfold 9. Studies have identified several genes that play a role in the prevention of obesity by affecting what? Ans: Regulation of appetite 10. The BRCA1 and BRCA2 mutations increase the risk of which cancer in women? Ans: Ovarian 11. Blood pressure variations are associated with: Ans: The renin-angiotensin system’s effect on vasoconstriction 12. The two most important risk factors for type 2 diabetes are: Ans: Obesity and positive family history 13. A major characteristic of type 1 diabetes mellitus is that there is: Ans: An autoimmune cause factor 14. Obesity acts as an important risk factor for type 2 diabetes mellitus by: Ans: Increasing the resistance to insulin by cells 15. Traits caused by the combined effects of multiple genes are referred to by which term? Ans: Polygenic 16. Regarding type 2 diabetes, obesity is considered to be what type of risk? Ans: Modifiable 17. Which disease form is identified on the basis of empirical risk observation? Ans: Multifactorial 18. The number of persons living with a specific disease at a specific point in time is referred to by which term? Ans: Prevalence 19. Which type of cancer is said to aggregate among families? Ans: Breast 20. Which dietary lifestyle choice has been associated with a decreased risk for developing colon cancer? Ans: Decreased consumption of foods high in fat 21. It is currently believed that the risk for developing Alzheimer disease: Ans: Doubles among those with an affected first-degree relative. 22. The number of new cases of a disease reported during a specific period divided by the number of individuals in the population is defined as which characteristic of a disease? Ans: Incidence rate 23. Cancers that cluster strongly in families include: Ans: Breast Colon Ovarian 24. Which genes are responsible for an autosomal dominant form of breast cancer? Ans: BRCA1 BRCA2 25. Lifestyle modifications that affect health-related risk factors include: Ans: Diet Exercise Stress reduction 26. What factors are typically considered when assessing an individual’s risk for developing such common diseases as hypertension? Ans: Age Diet Exercise habits Family history 27. Examples of multifactorial diseases associated with adults include: Ans: Breast cancer Coronary heart disease Diabetes mellitus Schizophrenia Match the terms with the corresponding descriptions. 28. Traits caused by the combined effects of multiple genes E. Polygenic 29. Number of persons living with the disease C. Prevalence rate at which some diseases occur 30. Yields an increased risk for some diseases B. Gene-environment interaction 31. Modifiable risk factor for many diseases D. Obesity 32. Number of new cases (persons) detected with the disease A. Incidence rate effect of multiple genes 33. Measure of the effect of a specific risk factor G. Relative risk 34. Risks based on direct observation of data F. Empirical risk Chapter 7: Innate Immunity: Inflammation 1. Which action is a purpose of the inflammatory process? Ans: To prevent infection of the injured tissue 2. How do surfactant proteins A through D provide innate resistance? Ans: Promote phagocytosis. 3. Which secretion is a first line of defense against pathogen invasion that involves antibacterial and antifungal fatty acids, as well as lactic acid? Ans: Sebaceous gland sebum 4. Which bacterium grows in the intestines after prolonged antibiotic therapy? Ans: Clostridium difficile 13. In the coagulation (clotting) cascade, the intrinsic and the extrinsic pathways converge at which factor? Ans: X 14. Which chemical interacts among all plasma protein systems by degrading blood clots, activating complement, and activating the Hageman factor? Ans: Plasmin 15. The chemotactic factor affects the inflammatory process by: Ans: Directing leukocytes to the inflamed area 16. What affect does the process of histamine binding to the histamine-2 (H2) receptor have on inflammation? Ans: Inhibition 17. Frequently when H1 and H2 receptors are located on the same cells, they act in what fashion? Ans: Antagonistically 18. Some older adults have impaired inflammation and wound healing because of which problem? Ans: Underlying chronic illness(es) exists. 19. Which chemical mediator derived from mast cells retracts endothelial cells to increase vascular permeability and to cause leukocyte adhesion to endothelial cells? Ans: Platelet-activating factor 20. What is the inflammatory effect of nitric oxide (NO)? Ans: Decreases mast cell function, and decreases platelet aggregation. 21. What is the correct sequence in phagocytosis? Ans: Recognition, engulfment, fusion, destruction 22. When considering white blood cell differentials, acute inflammatory reactions are related to elevations of which leukocyte? Ans: Neutrophils 23. In the later stages of an inflammatory response, which phagocytic cell is predominant? Ans: Monocytes 24. In regulating vascular mediators released from mast cells, the role of eosinophils is to release: Ans: Histaminase, which limits the effects of histamine during acute inflammation 25. What is the role of a natural killer (NK) cells? Ans: Elimination of malignant cells 26. Which cytokine is produced and released from virally infected host cells? Ans: IFN-α 27. IFN-α is secreted from which cells? Ans: Macrophages 28. Which manifestation of inflammation is systemic? Ans: Fever and leukocytosis 29. The acute inflammatory response is characterized by fever that is produced by the hypothalamus being affected by: Ans: Endogenous pyrogens 30. What occurs during the process of repair after tissue damage? Ans: Nonfunctioning scar tissue replaces destroyed tissue. 31. The role of fibroblasts during the reconstructive phase of wound healing is to: Ans: Synthesize and secrete collagen and the connective tissue proteins. 32. A keloid is the result of which dysfunctional wound healing response? Ans: Collagen matrix assembly 33. Which solution is best to use when cleaning a wound that is healing by epithelialization? Ans: Normal saline 34. Many neonates have a transient depressed inflammatory response as a result of which condition? Ans: Complement and chemotaxis are deficient. 35. During phagocytosis, what is occurring during the step referred to as opsonization? Ans: Phagocytes recognize and adhere to the bacteria. 36. Fusion is the step in phagocytosis during which: Ans: Lysosomal granules enter the phagocyte. 37. During the process of endocytosis, the phagosome step results in: Ans: An intracellular phagocytic vacuole is formed. 38. When cellular damage occurs and regeneration is minor with no significant complications, the process of returning the cells to preinjury function is referred to as: Ans: Resolution 39. Newborns often have deficiencies in collectin-like proteins, making them more susceptible to what type of infection? Ans: Respiratory 40. Which cell is the body’s primary defense against parasite invasion? Ans: Eosinophil 41. Which chemical mediators induce pain during an inflammatory response? Ans: Prostaglandins Bradykinin 42. Sebaceous glands protect the body from infection by secreting: Ans: Antibacterial fatty acids Antifungal fatty acids Lactic acid 43. Which body fluid has the ability to attack the cell walls of gram-positive bacteria? Ans: Perspiration Tears Saliva 44. The main function of NK cells includes: Ans: Recognizing virus-infected cells Eliminating virus-infected cells Eliminating previously identified cancer cells 45. Normal bacterial flora found in the intestines produce vitamin K to assist in the absorption of which of the following? Ans: Calcium Iron Magnesium 46. An individual’s acquired immunity is dependent on the function of which cells? Ans: T lymphocytes B lymphocytes Macrophages 47. An example of a pathogen capable of surviving and even multiplying inside a macrophage is known as: Ans: Mycobacterium tuberculosis (tuberculosis) Mycobacterium leprae (leprosy) Salmonella typhi (typhoid fever) Brucella abortus (brucellosis) 48. An older adult is particularly susceptible to infections of which body parts? Ans: Lungs Skin Bladder Match each step of phagocytosis with its function. 49. Microorganisms are ingested. B. Engulfment 50. Microorganisms are killed and digested. E. Destruction 51. Phagocytes gain enhanced recognition and adherence of bacteria. A. Opsonization 52. Lysosomal granules enter the phagocyte. D. Fusion 53. Intracellular phagocytic vacuole is formed. C. Phagosome Chapter 8: Adaptive Immunity 1. Which primary characteristic is unique for the immune response? Ans: The immune response is specific to the antigen that initiates it. 2. In which structure does B lymphocytes mature and undergo changes that commit them to becoming B cells? Ans: Bone marrow 3. What is the term for the process during which lymphoid stem cells migrate and change into either immunocompetent T cells or immunocompetent B cells? Ans: Clonal diversity 4. Which type of immunity is produced by an individual after either natural exposure to the antigen or after immunization against the antigen? Ans: Active-acquired immunity 5. What type of immunity is produced when an immunoglobulin crosses the placenta? Ans: Passive-acquired immunity 6. The portion of the antigen that is configured for recognition and binding is referred to as what type of determinant? Ans: Epitope 7. Which characteristic is the most important determinant of immunogenicity when considering the antigen? Ans: Foreignness 8. When antigens are administered to produce immunity, why are different routes of administration considered? Ans: Each route stimulates a different lymphocyte-containing tissue, resulting in different types of cellular and humoral immunity. 9. The functions of the major histocompatibility complex (MHC) and CD1 molecules are alike because both: Ans: Are antigen-presenting molecules. 10. Where are antibodies produced? Ans: Plasma cells 11. Which immunoglobulin is present in blood, saliva, breast milk, and respiratory secretions? Ans: IgA 12. Which antibody initially indicates a typical primary immune response? Ans: IgM 13. An individual is more susceptible to infections of mucous membranes when he or she has a seriously low level of which immunoglobulin antibody? Ans: IgA 14. The B-cell receptor (BCR) complex functions uniquely by: Ans: Communicating information about the antigen to the cell nucleus 15. The generation of clonal diversity occurs primarily during which phase of life? Ans: Fetal 16. The generation of clonal diversity includes a process that: Ans: Takes place in the primary (central) lymphoid organs. 17. Which statement is true concerning clonal selection? Ans: This theory involves antigens that select those lymphocytes with compatible receptors. 18. Which is an example of an endogenous antigen? Ans: Cancer 19. Which cytokine is needed for the maturation of a functional helper T cell? Ans: IL-2 20. Th2 cells produce IL-4 and suppress which cells? Ans: Th1 cells 21. Which statement is believed to be true concerning Th1 cells? Ans: They are induced by antigens derived from cancer cells. 22. Which statement is believed to be true concerning Th2 cells? Ans: Th2 cells are induced by antigens derived from allergens. 23. When a person is exposed to most antigens, antibodies can be usually detected in his or her circulation within: Ans: 6 days 24. Vaccinations are able to provide protection against certain microorganisms because of the: Ans: Level of protection provided by IgG 25. Why is the herpes virus inaccessible to antibodies after the initial infection? Ans: The virus does not circulate in the blood. 26. Increased age may cause which change in lymphocyte function? Ans: Increased production of antibodies against self-antigens 27. How do antibodies protect the host from bacterial toxins? Ans: Binding to the toxins to neutralize their biologic effects 28. Which T cell controls or limits the immune response to protect the host’s own tissues against an autoimmune response? Ans: Regulatory T (Treg) cells 29. Evaluation of umbilical cord blood can confirm that which immunoglobulin level is near adult levels? Ans: IgG 30. Which statement is true concerning the IgM? Ans: IgM is the first antibody produced during the initial response to an antigen. 31. Which cell has the ability to recognize antigens presented by the MHC class I molecules? Ans: CD 8 32. Which cell has a role in developing cell-mediated immunity? Ans: Th1 33. How does the aging process of the T-cell activity affect older adults? Ans: Tendency to develop various infections 34. Which statement is true regarding maternal antibodies provided to the neonate? Ans: The antibodies enter into the fetal circulation by means of active transport. 35. Antibodies that are associated with mucosal immune system, such as immunoglobulins, function to prevent which type of infections? Ans: Infections that focus on epithelial surfaces of the body 36. Cytokines are vital to a cell’s ability to do which function? Ans: Communicate 37. Which is an example of a bacterial toxin that has been inactivated but still retains its immunogenicity to protect the person? Ans: Tetanus Diphtheria 38. Which statements are true concerning the humoral immune response? Ans: The response has IgG and IgM produced during each of its phrases. It has a greater presence of IgG than IgM in one of its phases. The humoral immune response is produced in reaction to the presence of an antigen. Phases differ in their response time as a result of the effect of memory cells. 39. CD4 is a characteristic surface marker and a result of which of the following? Ans: Activity in the primary lymphoid organs Process of cellular differentiation Alterations to T cells Changes to B cells 40. What are the necessary components of an adaptive immune response? Ans: Antigen Lymphocyte surface receptors Antibody Match each immunoglobulin with its characteristic or function. Each immunoglobulin can be used only once. 41. Crosses the placenta. C. IgG 42. Is predominantly found in the blood and body secretions. A. IgA 43. Mediates many common allergic responses B. IgE Chapter 9: Alterations in Immunity and Inflammation 1. Hypersensitivity is best defined as a(an): Ans: Altered immunologic response to an antigen that results in disease 2. A hypersensitivity reaction that produces an allergic response is called: Ans: Anaphylaxis 3. The common hay fever allergy is expressed through a reaction that is mediated by which class of immunoglobulins? Ans: IgE 4. Which type of antibody is involved in type I hypersensitivity reaction? Ans: IgE 5. Blood transfusion reactions are an example of: Ans: Alloimmunity 6. During an IgE-mediated hypersensitivity reaction, which leukocyte is activated? Ans: Eosinophils 7. During an IgE-mediated hypersensitivity reaction, what causes bronchospasm? Ans: Smooth muscle contraction caused by histamine bound to H1 receptors 8. During an IgE-mediated hypersensitivity reaction, the degranulation of mast cells is a result of which receptor action? Ans: Histamine bound to H2 9. What characteristic do atopic individuals have that make them genetically predisposed to develop allergies? Ans: Greater quantities of IgE 10. What is the mechanism that results in type II hypersensitivity reactions? Ans: Antibodies bind to the antigens on the cell surface. 11. When mismatched blood is administered causing an ABO incompatibility, the erythrocytes are destroyed by: Ans: Complement-mediated cell lysis 12. When antibodies are formed against red blood cell antigens of the Rh system, the blood cells are destroyed by: Ans: Phagocytosis in the spleen 13. When soluble antigens from infectious agents enter circulation, tissue damage is a result of: Ans: Neutrophil granules and toxic oxygen products 14. How are target cells destroyed in a type II hypersensitivity reaction? Ans: Natural killer cells 15. Graves’ disease (hyperthyroidism) is an example of which type II hypersensitivity reaction? Ans: Modulation 16. Type III hypersensitivity reactions are a result of which of the following? Ans: Antibodies binding to soluble antigens that were released into body fluids and the immune complexes being deposited in the tissues 17. A type IV hypersensitivity reaction causes which result? Ans: Lymphokine-producing Th1 cells directly attacking and destroying cellular targets 18. In a type III hypersensitivity reaction, the harmful effects after the immune complexes that are deposited in tissues are a result of: Ans: Complement activation 19. Raynaud phenomenon is classified as a type III hypersensitivity reaction and is due to: Ans: Immune complexes that are deposited in capillary beds, blocking circulation 20. Deficiencies in which element can produce depression of both B- and T-cell function? Ans: Zinc 21. When the maternal immune system becomes sensitized against antigens expressed by the fetus, what reaction occurs? Ans: Alloimmunity 22. Tissue damage caused by the deposition of circulating immune complexes containing an antibody against the host DNA is the cause of which disease? Ans: Systemic lupus erythematosus 23. Why does tissue damage occurs in acute rejection after organ transplantation? Ans: Th1 cells release cytokines that activate infiltrating macrophages, and cytotoxic T cells directly attack the endothelial cells of the transplanted tissue. 24. Which blood cell carries the carbohydrate antigens for blood type? Ans: Erythrocytes 25. A person with type O blood is likely to have high titers of which anti-antibodies? Ans: A and B 26. Which class of immunoglobulins forms isohemagglutinins? Ans: IgM 27. Which component of the immune system is deficient in individuals with infections caused by viruses, fungi, or yeast? Ans: T cells 28. In which primary immune deficiency is there a partial-to-complete absence of T-cell immunity? Ans: DiGeorge syndrome 29. How many months does it take for the newborn to be sufficiently protected by antibodies produced by its own B cells? Ans: 6 to 8 30. Considering the effects of nutritional deficiencies on the immune system, severe deficits in calories and protein lead to deficiencies in the formation of which immune cells? Ans: T cells 31. Urticaria are a manifestation of a which type of hypersensitivity reaction? Ans: I 32. Graves’ disease is a result of: Ans: Autoantibodies binding to thyroid-stimulating hormone (TSH)-receptor sites 33. Raynaud phenomenon is an example of which type of hypersensitivity? Ans: III 34. Which statement is true concerning an atopic individual? Ans: They tend to produce more Fc receptors. 35. Which statement is true regarding immunodeficiency? Ans: Immunodeficiency is generally not present in other family members. 36. A person with type O blood is considered to be the universal blood donor because type O blood contains which of the following? Ans: No antigens 37. Immunoglobulin E (IgE) is associated with which type of hypersensitivity reaction? Ans: I 38. Graves’ disease is an autoimmune disease that results in which maternal antibody? Ans: Affecting the receptor for TSH, causing neonatal hyperthyroidism 39. When a tuberculin skin test is positive, the hard center and erythema surrounding the induration are a result of which of the following? Ans: T lymphocytes Macrophages 40. Exposure to which of the following could result in a type IV hypersensitivity reaction? Ans: Poison ivy Nickel Neomycin Detergents 41. Which disorders are considered autoimmune? Ans: Crohn disease Systemic lupus erythematosus Addison disease Rheumatoid arthritis 42. Which statements best define acute rejection? Ans: Acute rejection is a cell-mediated immune response. Immunosuppressive drugs delay or lessen the intensity of an acute rejection. Acute rejection is associated with the body’s response to an organ transplant. Acute rejection is a response against unmatched human leukocyte antigens (HLAs). Chapter 10: Infection 1. What is a significant cause of morbidity and mortality worldwide? Ans: Infectious disease 2. What is the first stage in the infectious process? Ans: Colonization 3. Which type of microorganism reproduces on the skin? Ans: Bacteria and fungi 4. Phagocytosis involves neutrophils actively attacking, engulfing, and destroying which microorganisms? Ans: Bacteria 5. Once they have penetrated the first line of defense, which microorganisms do natural killer (NK) cells actively attack? Ans: Viruses 6. Which statement concerning exotoxins is true? Ans: Exotoxins are released during bacterial growth. 7. Which statement is true concerning a fungal infection? Ans: Phagocytes and T lymphocytes control fungal infections. 8. Cytokines are thought to cause fevers by stimulating the synthesis of which chemical mediator? Ans: Prostaglandin 9. Considering the hypothalamus, a fever is produced by: Ans: Endogenous pyrogens acting directly on the hypothalamus. 10. Which statement about vaccines is true? Ans: Vaccines require booster injections to maintain life-long protection. 11. Vaccines against viruses are created from: Ans: Live organisms weakened to produce antigens 12. Which statement is a characteristic of HIV? Ans: HIV is a retrovirus. 13. What is the role of reverse transcriptase in HIV infection? Ans: It converts RNA into double-stranded DNA. 14. After sexual transmission of HIV, a person can be infected yet seronegative for how many months? Ans: 6 to 14 15. Which cells are primary targets for HIV? Ans: CD4+ Th cells, macrophages, and natural killer cells 16. What area in the body may act as a reservoir in which HIV can be relatively protected from antiviral drugs? Ans: Central nervous system 17. AIDS produces a striking decrease in the number of which cells? Ans: CD4+ Th cells 18. HIV antibodies appear within how many weeks after infection through blood products? Ans: 4 to 7 19. What is the final stage of the infectious process? Ans: Spread 20. Toxigenicity is defined as the: Ans: Pathogen’s ability to produce disease by the production of a soluble toxin 21. The ability of the pathogen to invade and multiply in the host is referred to as: Ans: Infectivity 22. Some bacterial surface proteins bind with the crystalline fragment (Fc) portion of an antibody to: Ans: Produce a protective “self” protein 23. Which organism is a common sexually transmitted bacterial infection? Ans: Treponema pallidum 24. Which disease is an example of a rickettsial infection? Ans: Rocky Mountain spotted fever 25. Which secretion transmits HIV? Ans: Semen Breast milk 26. Which infection is fungal? Ans: Ringworm Candida Athlete’s foot Aspergillus 27. Which statement is true regarding the development of HIV symptoms? Ans: T cells levels, particularly those of memory T cells, progressively decrease. Untreated infected individuals may remain asymptomatic for up to10 years. Secondary lymphoid organs experience damage and resulting malfunction. 28. Which statements are true regarding endotoxins? Ans: Endotoxins are lipopolysaccharides. Endotoxins are located in the walls of bacteria. Endotoxins are found in gram-negative microorganisms. Endotoxins are released during the destruction of its host. 29. Which statements are true regarding viruses? Ans: Viruses are capable of producing messenger RNA (mRNA). Viruses penetrate plasma membranes via endocytosis. Viruses are capable of uncoating cytoplasmic nucleocapsid. 30. Which of the following play a role in the control of fungal infections? Ans: Cytokines Macrophages Neutrophils T lymphocytes 31. Complications of AIDS include: Ans: Kaposi sarcoma Cytomegalovirus retinitis Herpes simplex infection Match each term with its definition. 32. Ability of the pathogen to invade and multiply in the host B. Infectivity 33. Capacity of a pathogen to cause severe disease D. Virulence 34. An important factor in determining a pathogen’s ability to produce disease by the production of a soluble toxin A. Toxigenicity 35. Ability of an agent to produce disease C. Pathogenicity Chapter 11: Stress and Disease 1. Exhaustion occurs if stress continues when which stage of the general adaptation syndrome is not successful? Ans: Adaptation 2. Which organ is stimulated during the alarm phase of the general adaptation syndrome (GAS)? Ans: Hypothalamus 3. During an anticipatory response to stress, the reaction from the limbic system is stimulated by the: Ans: Paraventricular nucleus of the hypothalamus 4. Which hormone prompts increased anxiety, vigilance, and arousal during a stress response? Ans: Norepinephrine 5. Perceived stress elicits an emotional, anticipatory response that begins where? Ans: Limbic system 6. During a stress response, the helper T (Th) 1 response is suppress by which hormone? Ans: Cortisol 7. What is the effect that low-serum albumin has on the central stress response? Ans: Impaired circulation of epinephrine and norepinephrine 8. Stress-age syndrome directly results in depressed function of which system? Ans: Immune 9. Stress-induced sympathetic stimulation of the adrenal medulla causes the secretion of: Ans: Epinephrine and norepinephrine 10. Stress-induced norepinephrine results in: Ans: Peripheral vasoconstriction 11. Released stress-induced cortisol results in the stimulation of gluconeogenesis by affecting which structure? Ans: Adrenal cortex 12. What is the effect of increased secretions of epinephrine, glucagon, and growth hormone? Ans: Hyperglycemia 13. Which hormone increases the formation of glucose from amino acids and free fatty acids? Ans: Cortisol 14. What effect do androgens have on lymphocytes? Ans: Suppression of B- and T-cell responses 15. Which gland regulates the immune response and mediates the apparent effects of circadian rhythms on immunity? Ans: Pineal 16. Which cytokines initiate the production of corticotropin-releasing hormone (CRH)? Ans: IL–1 and IL-6 17. The release of which cytokines is triggered by bacterial or viral infections, cancer, and tissue injury that, in turn, initiate a stress response? Ans: IFN, TNF-ß, and IL-6 18. The action of which hormone helps explain increases in affective anxiety and eating disorders, mood cycles, and vulnerability to autoimmune and inflammatory diseases in women as a result of stimulation of the CRH gene promoter and central norepinephrine system? Ans: Estrogen 19. What effect does estrogen have on lymphocytes? Ans: Depression of T-cell functions and enhancement of B-cell functions 20. Which statement is true concerning the differences between stress-induced hormonal alterations of men and women? Ans: Androgens appear to induce a greater degree of immune cell apoptosis after injury, creating greater immunosuppression in injured men than in injured women. 21. Diagnostic blood work on individuals who perceive themselves to be in a chronic stress state will likely demonstrate: Ans: Decreased Tc cells 22. What are the signs that a patient is in the adaptive stage of the general adaptation syndrome? Ans: The patient perceives his or her only options are to run away or fight back. 23. The most influential factor in whether a person will experience a stress reaction is his or her: Ans: Ability to cope 24. A reduction is an individual’s number of natural killer (NK) cells appears to correlate with an increased risk for the development of: Ans: Depression 25. A nurse is providing care to a terminally ill adult who has been with his life partner for over 56 years. Research supports the nurse’s assessment of the life partner for signs of: Ans: Severe stress reaction 26. The effect epinephrine has on the immune system during the stress response is to increase which cells? Ans: NK cells T cells 27. Which immune cells are suppressed by the corticotropin-releasing hormone (CRH)? Ans: Monocyte-macrophage cells Th cells 28. The increased production of proinflammatory cytokines is associated with which considerations? Ans: Elevated anxiety levels Immune disorders 29. Which statements are true regarding lymphocytes? Ans: Lymphocytes are involved in the production of the human growth hormone. Elevated catecholamine levels influence lymphocytes. Lymphocytes have receptors for the hormone prolactin. Match the hormone with its effects during a stress response. Hormones may be used more than once. 30. Constricts peripheral vessels to increase blood pressure. B. Norepinephrine 31. Increases cardiac output by increasing heart rate and myocardial contractility. A. Epinephrine 32. Increases gastric secretions. C. Cortisol Chapter 12: Cancer Biology 1. Which cancer originates from connective tissue? Ans: Osteogenic sarcoma 2. Carcinoma refers to abnormal cell proliferation originating from which tissue origin? Ans: Epithelial cells 3. Carcinoma in situ is characterized by which changes? Ans: Cells remain localized in the glandular or squamous cells. 4. Which term is used to describe a muscle cell showing a reduced ability to form new muscle while appearing highly disorganized? Ans: Anaplasia 5. What are tumor cell markers? Ans: Hormones, enzymes, antigens, and antibodies that are produced by cancer cells 6. The function of the tumor cell marker is to: Ans: Screen individuals at high risk for cancer. 7. Which statement supports the hypothesis that intestinal polyps are benign neoplasms and the first stage in the development of colon cancer? Ans: An accumulation of mutations in specific genes is required for the development of cancer. 8. Autocrine stimulation is the ability of cancer cells to: Ans: Secrete growth factors that stimulate their own growth. 9. Apoptosis is a(an): Ans: Normal mechanism for cells to self-destruct when growth is excessive 10. Many cancers create a mutation of ras. ras is a(an): Ans: Intracellular-signaling protein that regulates cell growth 11. Oncogenes are genes that are capable of: Ans: Undergoing mutation that directs the synthesis of proteins to accelerate the rate of tissue proliferation 12. Burkitt lymphomas designate a chromosome that has a piece of chromosome 8 fused to a piece of chromosome 14. This is an example of which mutation of normal genes to oncogenes? Ans: Chromosome translocation 13. In childhood neuroblastoma, the N-myc oncogene undergoes which type of mutation of normal gene to oncogene? Ans: Gene amplification 14. What aberrant change causes the abnormal growth in retinoblastoma? Ans: The tumor-suppressor gene is turned off. 15. Two “hits” are required to inactivate tumor-suppressor genes because: Ans: Each allele must be altered, and each person has two copies, or alleles, of each gene, one from each parent. 16. The ras gene converts from a proto-oncogene to an oncogene by: Ans: Altering one or more nucleotide base pairs 17. How do cancer cells use the enzyme telomerase? Ans: To switch on the telomerase to enable cells to divide indefinitely 18. What are characteristics of benign tumors? Ans: Benign tumors include the suffix -oma. 19. Which terms represent the correct nomenclature for benign and malignant tumors of adipose tissue, respectively? Ans: Lipoma, liposarcoma 20. What is the major virus involved in the development of cervical cancer? Ans: Human papillomavirus 21. The Papanicolaou (Pap) test is used to screen for which cancer? Ans: Cervical 22. What is the skin-related health risk induced by some types of chemotherapy? Ans: Infection 23. Which cancers are all associated with chronic inflammation? Ans: Colon, thyroid gland, and urinary bladder 24. Chronic inflammation causes cancer by: Ans: Releasing compounds such as reactive oxygen species that promote mutations 25. Inherited mutations that predispose to cancer are almost invariably what kind of gene? Ans: Tumor-suppressor genes 26. What is the consequence for cells when the functioning TP53 gene is lost as a result of mutation? Ans: Cells escape apoptosis. 27. Which gastrointestinal tract condition can be an outcome of both chemotherapy and radiation therapy? Ans: Stomatitis 28. What is the role of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) in cell metastasis? Ans: To develop new blood vessels to feed cancer cells 29. It has been determined that a tumor is in stage 2. What is the meaning of this finding? Ans: Cancer is locally invasive. 30. Which statement is true regarding pain and cancer? Ans: Pain is generally associated with late-stage cancer. 31. Which cancer may be treated with radiation delivered by brachytherapy? Ans: Cervical 32. The survival rate for stage IV Hodgkin disease can be as high as: Ans: 70% 33. What is the cause of anemia in a patient diagnosed with pancreatic cancer? Ans: Malabsorption of iron 34. By what process do cancer cells multiply in the absence of external growth signals? Ans: Autocrine stimulation 35. What is the role of caretaker genes? Ans: Maintenance of genomic integrity 36. In a normal, nonmutant state, an oncogene is referred to as a: Ans: Proto-oncogene 37. Which statement is true regarding pleomorphic cells? Ans: They are a result of anaplasia. 38. What is the most commonly reported symptom of cancer treatment? Ans: Fatigue 39. The most common site of metastasis for a patient diagnosed with prostate cancer is which location? Ans: Bones 40. Which statement concerning benign tumors is true? Ans: The cells are well-differentiated. 41. Normally, which cells are considered immortal (never die)? Ans: Germ Stem 42. What is the most common route for distant metastasis? Ans: Blood Lymphatic vessels 43. What cellular characteristics are affected by anaplasia? Ans: Size Ability to differentiate Tissue structure Shape 44. What are the most common causes of nosocomial infections among patients with cancer? Ans: Indwelling medical devices Visitor-introduced microorganisms Inadequate wound care 45. Which statements concerning aging and the occurrence of cancer are true? Ans: Decline in immunologic functions Predisposition to nutritional inadequacies Effects of immobility on the immune system Match the phrases with the corresponding terms. 46. Chemotherapy D. Takes advantage of specific vulnerabilities in specific cancer cells. 47. Radiation B. Is used to kill cancer cells while minimizing damage to normal structures. 48. Staging E. Provides a framework to determine treatment. 49. Angiogenesis A. Is the process of cancer cell growth. 50. Target agent C. Is guided by molecular analysis in specific diseases. Match the organism factor with the cancer it causes. 51. Cervical cancer A. HPV 52. Kaposi sarcoma B. Human herpesvirus (HHV) 8 53. Liver cancer C. Hepatis B virus (HBV) 54. Stomach cancer D. Helicobacter pylori Chapter 13: Cancer Epidemiology 1. Which characteristic among women correlates with a high morbidity of cancer of the colon, uterus, and kidney? Ans: Women who have a high body mass index 2. Which substance has been shown to increase the risk of cancer when used in combination with tobacco smoking? Ans: Alcohol 3. Which cancers pose the highest risk for radiologists? Ans: Leukemia 4. Research has shown a link between cancer and which sexually transmitted disease? Ans: Human papillomavirus 5. Research has supported that alcohol consumption has a convincing impact on increasing the risk of which cancer? Ans: Pharynx 6. Research supports the premise that exercise has a probable impact on reducing the risk of which cancer? Ans: Colon 7. The World Health Organization (WHO) defines grade 1 (overweight) as a BMI of: Ans: 25 to 29.9 8. Tobacco smoking is associated with which cancers? Ans: Lung Bladder Kidney Pancreas 9. The significant risk factors associated with the development of basal cell carcinoma include: Ans: Light-colored hair Pale eyes Fair skin Freckles 10. Which environmental factors have been shown to have greatest significant effect on the frequency of genetic mutations in humans? Ans: Tobacco use Radiation exposure Obesity 11. Research data support the relationship between the exposure of ultraviolet light (UVL) and the development of: Ans: Basal cell carcinoma Squamous cell carcinoma 12. Alcohol consumption has been proven to be a consistent risk factor in the development of which major cancer? Ans: Colorectal Breast Esophageal 13. Nutritional counseling regarding cancer stem cell repopulation must stress the importance of including sufficient quantities of what in a daily diet? Ans: Vitamin A Vitamin D 14. Which personal lifestyle choices will likely have a positive impact on reducing an individual’s risk for developing cancer? Ans: Wearing a hat while golfing Staying indoors during smog alerts 15. Which individual is at risk for developing lung and respiratory tract cancers because of exposure to known cancer-inducing environmental factors? Ans: A patient whose partner smokes 1 1/2 packs of cigarettes a day A 10-year employee of an asbestos fiber manufacturer A farmer whose equipment is primarily driven by diesel engines A 10-year delivery employee for a paper manufacturing company 16. Which primary prevention strategy has a substantial likelihood of reducing the risk of developing cancer? Ans: Offering free smoking cessation classes to college students Providing a breast cancer screening at a senior center twice a year Supplying low sugar, low-fat snacks at an after-school tutoring program 17. When considering topics for a series of community discussions related to cancer prevention strategies, the nurse will include: Ans: Healthy eating Tobacco avoidance Impact of obesity on one’s health Age-appropriate exercise routines Chapter 21: Mechanisms of Hormonal Regulation 1. What imbalance lessens the rate of secretion of parathyroid hormone (PTH)? Ans: Increased serum calcium levels 2. Regulation of the release of catecholamines from the adrenal medulla is an example of which type of regulation? Ans: Neural 3. How does a faulty negative-feedback mechanism result in a hormonal imbalance? Ans: Excessive hormone production results from a failure to turn off the system. 4. Which substance is a water-soluble protein hormone? Ans: Insulin 5. Which of the following is a lipid-soluble hormone? Ans: Cortisol 6. Most protein hormones are transported in the bloodstream and are: Ans: Free in an unbound, water-soluble form 7. When insulin binds its receptors on muscle cells, an increase in glucose uptake by the muscle cells is the result. This is an example of what type of effect by a hormone? Ans: Direct 8. Thyroid-stimulating hormone (TSH) is released to stimulate thyroid hormone (TH) and is inhibited when plasma levels of TH are adequate. This is an example of: Ans: Negative feedback 9. Lipid-soluble hormone receptors are located: Ans: Inside the plasma membrane in the cytoplasm 10. Which second messenger is stimulated by epinephrine binding to a -adrenergic receptor? Ans: Cyclic adenosine monophosphate (cAMP) 11. Which hormone does the second messenger calcium (Ca++) bind to activate phospholipase C through a G protein? Ans: Angiotensin II 12. The control of calcium in cells is important because it: Ans: Acts as a second messenger. 13. The portion of the pituitary that secretes oxytocin is: Ans: Posterior 14. Antidiuretic hormone acts to cause vasoconstriction when: Ans: Vasopressin is pharmacologically administered. 15. What is the target tissue for prolactin-releasing factor? Ans: Anterior pituitary 16. Where is antidiuretic hormone (ADH) synthesized, and where does it act? Ans: Hypothalamus; renal tubular cells 17. Where is oxytocin synthesized? Ans: Posterior pituitary 18. The releasing hormones that are made in the hypothalamus travel to the anterior pituitary via the: Ans: Portal hypophyseal blood vessels 19. Which mineral is needed for thyroid-stimulating hormone (TSH) to stimulate the secretion of thyroid hormone (TH)? Ans: Iodide 20. Which hormone triggers uterine contractions? Ans: Oxytocin 21. What effect does hyperphosphatemia have on other electrolytes? Ans: Decreases serum calcium 22. Insulin transports which electrolyte in the cell? Ans: Potassium 23. A person who has experienced physiologic stresses will have increased levels of which hormone? Ans: Adrenocorticotropic hormone 24. What is the action of calcitonin? Ans: Decreases serum calcium. 25. Which hormone is involved in the regulation of serum calcium levels? Ans: Parathyroid hormone (PTH) 26. Which hormone inhibits the secretion of growth hormone (GH)? Ans: Thyroid-stimulating hormone 27. Target cells for parathyroid hormone are located in the: Ans: Tubules of nephrons 28. Which compound or hormone is secreted by the adrenal medulla? Ans: Epinephrine 29. The secretion of adrenocorticotropic-stimulating hormone (ACTH) will result in the increased level of which hormone? Ans: Cortisol. 30. Which human physiologic system is believed to be an integral factor in unhealthy aging? Ans: Endocrine 31. What are the effects of aging on pancreatic cells? Ans: Pancreatic cells are replaced by fat cells. 32. Aldosterone directly increases the reabsorption of: Ans: Sodium 33. Which is an expected hormonal change in an older patient? Ans: Thyroid-stimulating hormone secretion below normal 34. What are actions of glucocorticoids? Ans: Decreasing muscle cell reuptake of glucose Carbohydrate metabolism Liver gluconeogenesis Match the anatomic structure with its hormone. Names of structures may be used more than once. 35. Calcitonin - C. Thyroid 36. Cortisol - D. Adrenal cortex 37. Oxytocin - B. Posterior pituitary 38. Glycoproteins - A. Anterior pituitary 39. Epinephrine - E. Adrenal medulla Chapter 22: Alterations of Hormonal Regulation 1. The effects of the syndrome of inappropriate antidiuretic hormone (SIADH) secretion include solute: Ans: Dilution and water retention 2. The common cause of elevated levels of antidiuretic hormone (ADH) secretion is: Ans: Ectopically produced ADH 3. Which laboratory value would the nurse expect to find if a person is experiencing syndrome of inappropriate antidiuretic hormone (SIADH)? Ans: Serum sodium (Na+) level of 120 mEq/L and serum hypoosmolality 4. Diabetes insipidus is a result of: Ans: Antidiuretic hormone hyposecretion 5. A patient who is diagnosed with a closed head injury has a urine output of 6 to 8 L/day. Electrolytes are within normal limits, but his antidiuretic hormone (ADH) level is low. Although he has had no intake for 4 hours, no change in his polyuria level has occurred. These symptoms support a diagnosis of: Ans: Neurogenic diabetes insipidus 6. Diabetes insipidus, diabetes mellitus, and syndrome of inappropriate antidiuretic hormone all exhibit which symptom? Ans: Thirst 7. The cause of neurogenic diabetes insipidus (DI) is related to an organic lesion of the: Ans: Posterior pituitary 8. Which form of diabetic insipidus (DI) will result if the target cells for antidiuretic hormone (ADH) in the renal collecting tubules demonstrate insensitivity? Ans: Nephrogenic 9. Which laboratory value is consistently low in a patient with diabetes insipidus (DI)? Ans: Urine-specific gravity 10. Which form of diabetes insipidus (DI) is treatable with exogenous antidiuretic hormone (ADH)? Ans: Neurogenic 11. Which condition may result from pressure exerted by a pituitary tumor? Ans: Hypothyroidism 12. The term used to describe a person who experiences a lack of all hormones associated with the anterior pituitary is: Ans: Panhypopituitarism 13. Visual disturbances are a result of a pituitary adenoma because of the: Ans: Pressure of the tumor on the optic chiasm 14. Which disorder is considered a co-morbid condition of acromegaly? Ans: Diabetes 15. Which disorder is caused by hypersecretion of the growth hormone (GH) in adults? Ans: Acromegaly d. Myxedema 16. Giantism occurs only in children and adolescents because their: Ans: Epiphyseal plates have not yet closed. 17. Amenorrhea, galactorrhea, hirsutism, and osteoporosis are each caused by a: Ans: Prolactinoma 18. Graves’ disease develops from a(n): Ans: Thyroid-stimulating immunoglobulin that causes overproduction of thyroid hormones 19. The signs of thyrotoxic crisis include: Ans: Hyperthermia and tachycardia 20. Pathologic changes associated with Graves’ disease include: Ans: High levels of circulating thyroid-stimulating immunoglobulins 21. The level of thyroid-stimulating hormone (TSH) in individuals with Graves’ disease is usually: Ans: Low 22. Palpation of the neck of a person diagnosed with Graves disease would detect a thyroid that is: Ans: Diffusely enlarged 23. A deficiency of which chemical may result in hypothyroidism? Ans: Iodine 24. What are clinical manifestations of hypothyroidism? Ans: Constipation, decreased heat rate, and lethargy 25. Diagnosing a thyroid carcinoma is best performed with: Ans: Fine-needle aspiration biopsy 26. Renal failure is the most common cause of which type of hyperparathyroidism? Ans: Secondary 27. The most common cause of hypoparathyroidism is: Ans: Parathyroid gland damage 28. The most probable cause of low serum calcium after a thyroidectomy is: Ans: Hypoparathyroidism caused by surgical injury 29. A patient diagnosed with diabetic ketoacidosis (DKA) has the following laboratory values: arterial pH 7.20; serum glucose 500 mg/dl; positive urine glucose and ketones; serum potassium (K+) 2 mEq/L; serum sodium (Na+) 130 mEq/L. The patient reports that he has been sick with the “flu” for 1 week. What relationship do these values have to his insulin deficiency? Ans: Decreased glucose use causes fatty acid use, ketogenesis, metabolic acidosis, and osmotic diuresis. 30. Polyuria occurs with diabetes mellitus because of the: Ans: Elevation in serum glucose 31. Type 2 diabetes mellitus is best described as a(an): Ans: Resistance to insulin by insulin-sensitive tissues 32. A person diagnosed with type 1 diabetes experiences hunger, lightheadedness, tachycardia, pallor, headache, and confusion. The most probable cause of these symptoms is: Ans: Hypoglycemia caused by increased exercise 33. Which serum glucose level would indicate hypoglycemia in a newborn? Ans: 28 mg/dl 34. When comparing the clinical manifestations of both diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar nonketotic syndrome (HHNKS), which condition is associated with only DKA? Ans: Kussmaul respirations 35. Hypoglycemia, followed by rebound hyperglycemia, is observed in those with: Ans: The Somogyi effect 36. The first laboratory test that indicates type 1 diabetes is causing the development of diabetic nephropathy is: Ans: Protein on urinalysis 37. Which classification of oral hypoglycemic drugs decreases hepatic glucose production and increases insulin sensitivity and peripheral glucose uptake? Ans: Biguanide (metformin) 38. What causes the microvascular complications in patients with diabetes mellitus? Ans: The capillary basement membranes thicken, and cell hyperplasia develops. 39. Retinopathy develops in patients with diabetes mellitus because: Ans: Retinal ischemia and red blood cell aggregation occur. 40. A person has acne, easy bruising, thin extremities, and truncal obesity. These clinical manifestations are indicative of which endocrine disorder? Ans: Cushing disease 41. A person may experience which complications as a result of a reduction in parathyroid hormone (PTH)? Ans: Muscle spasms Tonic-clonic seizures Laryngeal spasms Asphyxiation 42. A chronic complication of diabetes mellitus is likely to result in microvascular complications in which areas? Ans: Eyes Renal system Nerves Match the phrases with the corresponding terms. _48_ A. Acromegaly _44_ B. Cushing disease _47_ C. Addison disease _43_ D. Graves’ disease _46_ E. Myxedema _45_ F. Pheochromocytoma 43. Hypersecretion of thyroid hormone (TH) 44. Hypersecretion of adrenocorticotropic hormone (ACTH) 45. Hypersecretion of adrenal medulla hormones 46. Hyposecretion of thyroid hormone (TH) 47. Hyposecretion of adrenal cortex hormones 48. Hypersecretion of growth hormone (GH) Chapter 23: Obesity and Disorders of Nutrition 1. If a patient with multiple sclerosis starts coughing frequently during meals and starts to eat significantly less food than normal, the patient may have Ans: dysphagia. 2. For a patient with dysphagia, the food that would be most difficult to swallow is Ans: chicken noodle soup. 3. If a patient has difficulty swallowing, the best position for eating is Ans: Sitting upright opposite a caregiver. 4. The most acute risk for patients with dysphagia is Ans: dehydration. 5. The most helpful recommendation for a client who often experiences heartburn at night would be to Ans: avoid eating within 4 hours of going to bed. 6. An example of a meal that is likely to relax the lower esophageal sphincter and allow gastroesophageal reflux is Ans: fried chicken and pasta salad. 7. Peptic ulcer disease (PUD) would be most like to occur in someone who uses medication to treat Ans: joint pain or arthritis. 8. Nutrition therapy for peptic ulcers should be individualized, depending on Ans: patient tolerance. 9. If a patient who has undergone gastric bypass surgery for treatment of extreme obesity experiences sudden sweating, nausea, and stomach cramps after meals, the patient may have Ans: dumping syndrome. 10. An appropriate meal for someone with dumping syndrome would be Ans: half a turkey sandwich. 11. If a patient has esophagitis and also has worn tooth enamel, he or she may have Ans: an eating disorder. 12. An example of a meal that may contain gluten is Ans: roast beef with mashed potatoes and gravy. 13. A patient with lactose intolerance would be most likely to experience symptoms if he or she ate a Ans: cup of pudding. 14. Milk may be made suitable for patients with lactose intolerance by treating it with tablets that contain Ans: lactase enzyme. 15. For patients with inflammatory bowel disease, nutrition therapy is Ans: an important adjunct to drugs and surgery. 16. Because patients with active Crohns disease have intestinal inflammation, they benefit from high intake of Ans: protein. 17. Patients with inflammatory bowel disease may benefit from a high-fiber diet during Ans: times of remission. 18. Fluid loss is most likely to be a problem for a patient with Ans: an ileostomy. 19. The most significant nutritional concern for a patient with an ileostomy is Ans: loss of fluid and electrolytes. 20. For patients with ostomies, a lower amount of output occurs Ans: if the ostomy is closer to the rectum. 21. If a patient has had a large portion of their small intestine removed because of cancer and is unable to maintain a stable weight, a feeding regimen that would be most appropriate is Ans: supplemental parenteral nutrition. 22. If a patient receiving chemotherapy is struggling with nausea and vomiting, helpful suggestions may include Ans: eating frequent small meals throughout the day. 23. The best way to prevent formation of diverticula in the colon is to Ans: eat plenty of fruits, vegetables, and whole grains. 24. Someone who may benefit from avoiding sugar-free chewing gum is a patient with Ans: irritable bowel syndrome. 25. In consuming a high-fiber diet, it is important to also consume adequate amounts of Ans: fluid. 26. If a client complains of excessive gas, a good question to ask is whether he or she Ans: chews gum. 27. An example of a daily change that may help decrease constipation is Ans: eating oatmeal and raisins instead of a bagel for breakfast. 28. An example of a high-fiber food item to include with lunch is Ans: black bean soup. 29. A possible cause of acute diarrhea is Ans: emotional stress. 30. Treatment of diarrhea generally begins with Ans: adequate fluids to hydrate the patient. Chapter 32: Structure and Function of the Cardiovascular and Lymphatic Systems 1. Which statement does not accurately describe the pericardium? Ans: It is made up of connective tissue and a surface layer of squamous cells. 2. Which cardiac chamber has the thinnest wall and why? Ans: The right and left atria; they are low-pressure chambers that serve as storage units and conduits for blood. 3. Which chamber of the heart endures the highest pressures? Ans: Left ventricle 4. What is the process that ensures mitral and tricuspid valve closure after the ventricles are filled with blood? Ans: Increased pressure in the ventricles pushes the valves to close. 5. Regarding the heart’s valves, what is a function of the papillary muscles? Ans: These muscles prevent backward expulsion of the atrioventricular valve. 6. During the cardiac cycle, why do the aortic and pulmonic valves close after the ventricles relax? Ans: Blood fills the cusps of the valves and causes the edges to merge, closing the valves. 7. Oxygenated blood flows through which vessel? Ans: Pulmonary veins 8. The significance of the atrial kick is that it affects the contraction of the: Ans: Left atria, which increases the blood volume into the ventricle. 9. Occlusion of the left anterior descending artery during a myocardial infarction would interrupt blood supply to which structures? Ans: Left and right ventricles and much of the interventricular septum 10. Occlusion of the circumflex artery during a myocardial infarction would interrupt blood supply to which area? Ans: Left atrium and the lateral wall of the left ventricle 11. The coronary ostia are located in the: Ans: Aorta 12. The coronary sinus empties into which cardiac structure? Ans: Right atrium 13. What is the ratio of coronary capillaries to cardiac muscle cells? Ans: 1:1 (one capillary per one muscle cell) 14. During the cardiac cycle, which structure directly delivers action potential to the ventricular myocardium? Ans: Purkinje fibers 15. What causes depolarization of a cardiac muscle cell to occur? Ans: Rapid movement of sodium into the cell 16. Which event occurs during phase 1 of the normal myocardial cell depolarization and repolarization? Ans: Early repolarization when calcium slowly enters the cells 17. Which phase of the normal myocardial cell depolarization and repolarization correlates with diastole? Ans: Phase 4 18. In the normal electrocardiogram, what does the PR interval represent? Ans: Atrial activation to onset of ventricular activity 19. The cardiac electrical impulse normally begins spontaneously in the sinoatrial (SA) node because it: Ans: Depolarizes more rapidly than other automatic cells of the heart. 20. What period follows depolarization of the myocardium and represents a period during which no new cardiac potential can be propagated? Ans: Refractory 21. Which complex (wave) represents the sum of all ventricular muscle cell depolarizations? Ans: QRS 22. What can shorten the conduction time of action potential through the atrioventricular (AV) node? Ans: Catecholamines 23. If the sinoatrial (SA) node fails, then at what rate (depolarizations per minute) can the atrioventricular (AV) node depolarize? Ans: 40 to 60 24. What is the effect of epinephrine on 3 receptors on the heart? Ans: Prevents overstimulation of the heart by the sympathetic nervous system. 25. Where in the heart are the receptors for neurotransmitters located? Ans: Myocardium and coronary vessels 26. What enables electrical impulses to travel in a continuous cell-to-cell fashion in myocardial cells? Ans: Intercalated disks 27. Within a physiologic range, what does an increase in left ventricular end-diastolic volume (preload) result in? Ans: Increase in force of contraction 28. As stated in the Frank-Starling law, a direct relationship exists between the of the blood in the heart at the end of diastole and the of contraction during the next systole. Ans: Volume; strength 29. Pressure in the left ventricle must exceed pressure in which structure before the left ventricle can eject blood? Ans: Aorta 30. Continuous increases in left ventricular filing pressures result in which disorder? Ans: Pulmonary edema 31. When the volume of blood in the ventricle at the end of diastole increases, the force of the myocardial contraction during the next systole will also increase, which is an example of which law or theory about the heart? Ans: Frank-Starling law 32. The resting heart rate in a healthy person is primarily under the control of which nervous system? Ans: Parasympathetic d. Spinal 33. The Bainbridge reflex is thought to be initiated by sensory neurons in which cardiac location? Ans: Atria 34. After the baroreceptor reflex is stimulated, the resulting impulse is transmitted from the carotid artery by which sequence of events? Ans: Glossopharyngeal cranial nerve through the vagus nerve to the medulla to increase parasympathetic activity and to decrease sympathetic activity 35. Reflex control of total cardiac output and total peripheral resistance is controlled by what mechanism? Ans: Sympathetic stimulation of the heart, arterioles, and veins 36. What is the most important negative inotropic agent? Ans: Acetylcholine 37. The right lymphatic duct drains into which structure? Ans: Right subclavian vein 38. Where is the major cardiovascular center in the central nervous system? Ans: Brainstem 39. What is an expected change in the cardiovascular system that occurs with aging? Ans: Arterial stiffening 40. What is the major determinant of the resistance that blood encounters as it flows through the systemic circulation? Ans: Muscle layer of the arterioles 41. Which function of the cardiovascular system is often affected by ischemia? Ans: Heart rate (HR) 42. What physical sign is the result of turbulent blood flow through a vessel? Ans: Murmur heard on auscultation 43. What is the major effect of a calcium channel blocker such as verapamil on cardiac contractions? Ans: Decreases the strength of cardiac contractions. 44. An early diastole peak caused by filling of the atrium from peripheral veins is identified by which intracardiac pressure? Ans: V wave 45. Which intracardiac pressure is generated by the atrial contraction? Ans: A wave 46. Which intracardiac pressure is produced because of the descent of the tricuspid valve ring and by the ejection of blood from both ventricles? Ans: X descent 47. Which statements are true concerning the method in which substances pass between capillaries and the interstitial fluid? Ans: Substances pass through junctions between endothelial cells. Substances pass through pores or oval windows (fenestrations). Substances pass between vesicles by active transport across the endothelial cell membrane. Substances pass through endothelial cell membranes by diffusion. Match the description with the corresponding terms. _48_ A. Relationship among blood flow, pressure, and resistance _52_ B. Increased heart rate from increased volume _51_ C. Relationship of wall tension, intraventricular pressure, internal radius, and wall thickness _49_ D. Cycles of attachment, movement, and dissociation of thin filaments during the attachments of actin to myosin _50_ E. Length-tension relationship of cardiac muscle 48. Poiseuille law 49. Cross-bridge theory 50. Frank-Starling law 51. Laplace’s law 52. Bainbridge reflex Chapter 33: Alterations of Cardiovascular Function 1. What is the initiating event that leads to the development of atherosclerosis? Ans: Injury to the endothelial cells that line the artery walls 2. What is the effect of oxidized low-density lipoproteins (LDLs) in atherosclerosis? Ans: LDLs cause smooth muscle proliferation. 3. Which inflammatory cytokines are released when endothelial cells are injured? Ans: Tumor necrosis factor–alpha ((TNF-?), interferon-gamma (IFN-), and interleukin 1 (IL-1) 4. When endothelia cells are injured, what alteration contributes to atherosclerosis? Ans: Cells are unable to make the normal amount of vasodilating cytokines. 5. Which factor is responsible for the hypertrophy of the myocardium associated with hypertension? Ans: Angiotensin II 6. What pathologic change occurs to the kidney’s glomeruli as a result of hypertension? Ans: Ischemia of the tubule 7. What effect does atherosclerosis have on the development of an aneurysm? Ans: Atherosclerosis erodes the vessel wall. 8. Regarding the endothelium, what is the difference between healthy vessel walls and those that promote clot formation? Ans: Inflammation and roughening of the endothelium of the artery are present. 9. What is the usual source of pulmonary emboli? Ans: Deep venous thrombosis c. Valvular disease 10. Which factor can trigger an immune response in the bloodstream that may result in an embolus? Ans: Amniotic fluid 11. Which statement best describes thromboangiitis obliterans (Buerger disease)? Ans: Inflammatory disorder of small- and medium-size arteries in the feet and sometimes in the hands 12. Which statement best describes Raynaud disease? Ans: Vasospastic disorder of the small arteries and arterioles of the fingers and, less commonly, of the toes 13. What change in a vein supports the development of varicose veins? Ans: Damage to the valves in veins 14. Superior vena cava syndrome is a result of a progressive increase of which process? Ans: Occlusion 15. What term is used to identify when a cell is temporarily deprived of blood supply? Ans: Ischemia 16. The risk of developing coronary artery disease is increased up to threefold by which factor? Ans: Hypertension 17. Which risk factor is associated with coronary artery disease (CAD) because of its relationship with the alteration of hepatic lipoprotein? Ans: Diabetes mellitus 18. Nicotine increases atherosclerosis by the release of which neurotransmitter? Ans: Epinephrine 19. Which substance is manufactured by the liver and primarily contains cholesterol and protein? Ans: Low-density lipoproteins (LDLs) 20. Which elevated value may be protective of the development of atherosclerosis? Ans: High-density lipoproteins (HDLs) 21. Which laboratory test is an indirect measure of atherosclerotic plaque? Ans: C-reactive protein (CRP) 22. Cardiac cells can withstand ischemic conditions and still return to a viable state for how many minutes? Ans: 20 23. Which form of angina occurs most often during sleep as a result of vasospasms of one or more coronary arteries? Ans: Prinzmetal 24. When is the scar tissue that is formed after a myocardial infarction (MI) most vulnerable to injury? Ans: Between 10 and 14 days 25. An individual who is demonstrating elevated levels of troponin, creatine kinase–isoenzyme MB (CK-MB), and lactic dehydrogenase (LDH) is exhibiting indicators associated with which condition? Ans: Myocardial infarction (MI) 26. What is the expected electrocardiogram (ECG) pattern when a thrombus in a coronary artery permanently lodges in the vessel and the infarction extends through the myocardium from the endocardium to the epicardium? Ans: ST elevation myocardial infarction (STEMI) 27. How does angiotensin II increase the workload of the heart after a myocardial infarction (MI)? Ans: By increasing the peripheral vasoconstriction 28. The pulsus paradoxus that occurs as a result of pericardial effusion is caused by a dysfunction in which mechanism? Ans: Diastolic filling pressures of the left ventricle and reduction of blood volume in all four heart chambers. 29. A patient reports sudden onset of severe chest pain that radiates to the back and worsens with respiratory movement and when lying down. These clinical manifestations describe: Ans: Acute pericarditis 30. Ventricular dilation and grossly impaired systolic function, leading to dilated heart failure, characterize which form of cardiomyopathy? Ans: Congestive 31. A disproportionate thickening of the interventricular septum is the hallmark of which form of cardiomyopathy? Ans: Hypertrophic 32. Amyloidosis, hemochromatosis, or glycogen storage disease usually causes which form of cardiomyopathy? Ans: Restrictive 33. Which condition is a cause of acquired aortic regurgitation? Ans: Rheumatic fever 34. Which predominantly female valvular disorder is thought to have an autosomal dominant inheritance pattern, as well as being associated with connective tissue disease? Ans: Mitral valve prolapse 35. Which disorder causes a transitory truncal rash that is nonpruritic and pink with erythematous macules that may fade in the center, making them appear as a ringworm? Ans: Rheumatic fever 36. What is the most common cause of infective endocarditis? Ans: Bacterium 37. What is the most common cardiac disorder associated with acquired immunodeficiency syndrome (AIDS) Ans: Left heart failure 38. A patient is diagnosed with pulmonary disease and elevated pulmonary vascular resistance. Which form of heart failure may result from pulmonary disease and elevated pulmonary vascular resistance? Ans: Right heart failure 39. What cardiac pathologic condition contributes to ventricular remodeling? Ans: Myocardial ischemia 40. In systolic heart failure, what effect does the renin-angiotensin-aldosterone system (RAAS) have on stroke volume? Ans: Increases preload and increases afterload. 41. What is the cause of the dyspnea resulting from a thoracic aneurysm? Ans: Pressure on surrounding organs 42. Which statement is true concerning the cells’ ability to synthesize cholesterol? Ans: Most body cells are capable of producing cholesterol. 43. What is the trigger for angina pectoris? Ans: Myocardial ischemia 44. Individuals being effectively managed for type 2 diabetes mellitus often experience a healthy decline in blood pressure as a result of what intervention? Ans: Insulin-sensitivity medication therapy 45. Which statements are true regarding fatty streaks? Ans: Fatty streaks progressively damage vessel walls. Fatty streaks are capable of producing toxic oxygen radials. When present, inflammatory changes occur to the vessel walls. Oxidized low-density lipoproteins (LDLs) are involved in their formation. 46. What factors contribute to the development of orthostatic hypotension? Ans: Altered body chemistry Drug action of certain antihypertensive agents Prolonged immobility Effects of aging on postural reflexes 47. Which assessment findings are clinical manifestations of aortic stenosis? Ans: Angina Syncope 48. Which risk factors are associated with infective endocarditis? Ans: Intravenous drug use Long-term indwelling catheterization Heart valve disease Match the descriptions with the corresponding terms. _51_ A. Impairs flow from left atrium to left ventricle _49_ B. Impairs flow from the left ventricle _53_ C. Backflow into left atrium _52_ D. Backflow into right atrium _50_ E. Backflow into left ventricle 49. Aortic stenosis 50. Aortic regurgitation 51. Mitral stenosis 52. Tricuspid regurgitation 53. Mitral regurgitation Chapter 35: Structure and Function of the Pulmonary System 1. What pulmonary defense mechanism propels a mucous blanket that entraps particles moving toward the oropharynx? Ans: Cilia 2. Which term is used to identify the movement of gas and air into and out of the lungs? Ans: Ventilation 3. When an individual aspirates food particles, where would the nurse expect to hear decreased or absent breath sounds? Ans: Right lung 4. Aspiration is most likely to occur in the right mainstem bronchus because it: Ans: Extends vertically from the trachea. 5. Air passage among alveoli is collateral and evenly distributed because of the function of which structures? Ans: Pores of Kohn 6. Where in the lung does gas exchange occur? Ans: Alveolocapillary membrane 7. Surfactant produced by type II alveolar cells facilitates alveolar distention and ventilation by which mechanism? Ans: Decreasing surface tension in the alveoli 8. Which part of the brainstem provides basic automatic rhythm of respiration by sending efferent impulses to the diaphragm and intercostal muscles? Ans: Dorsal respiratory group (DRG) 9. Which structures secrete surfactant? Ans: Type II alveolar cells 10. Which structure is not associated with any lymphatic vessels? Ans: Acinus 11. Which describes the pressure in the pleural space? Ans: Below atmospheric 12. The adequacy of a person’s alveolar ventilation is assessed best by monitoring which mechanism? Ans: Arterial blood gas 13. Which normal physiologic change occurs in the aging pulmonary system? Ans: Stiffening of the chest wall 14. How is most of the oxygen in the blood transported? Ans: Bound to hemoglobin 15. Stretch receptors and peripheral chemoreceptors send afferent impulses regarding ventilation to which location in the brain? Ans: Dorsal respiratory group (DRG) in the medulla oblongata 16. Which substances cause airway epithelium to constrict? Ans: Histamine and prostaglandin 17. If a patient develops acidosis, the nurse would expect the oxyhemoglobin dissociation curve to react in which manner? Ans: Shift to the right, causing more oxygen (O2) to be released to the cells 18. How is most carbon dioxide (CO2) in the blood transported? Ans: In the form of bicarbonate 19. The sternocleidomastoid and scalene muscles are referred to as which group? Ans: Diaphragmatic muscles 20. An increase in surface tension caused by decreased surfactant production results in which alteration? Ans: Increase in alveoli fluid collection 21. Decreased lung compliance means that the lungs are demonstrating which characteristic? Ans: Stiffness 22. The lung is innervated by the parasympathetic nervous system via which nerve? Ans: Vagus 23. What event is characteristic of the function in Zone 1 of the lung? Ans: The capillary bed collapses, and normal blood flow ceases. 24. Hypoventilation that results in the retention of carbon dioxide will stimulate which receptors in an attempt to maintain a normal homeostatic state? Ans: Central chemoreceptors 25. What is the most important cause of pulmonary artery constriction? Ans: Low alveolar partial pressure of arterial oxygen (PaO2) 26. Where does the tracheal bifurcation occur? Ans: Carina 27. How low must the partial pressure of arterial oxygen (PaO2) drop before the peripheral chemoreceptors influence ventilation? Ans: Below 70 mm Hg 28. Which receptors are located in the smooth muscles of airways? Ans: Stretch receptors 29. Which receptors are located near the respiratory center? Ans: Central chemoreceptors 30. Which receptors are located in the aortic bodies, aortic arch, and carotid bodies? Ans: Peripheral chemoreceptors 31. What is the purpose of the spirometry measurement? Ans: To measure the volume and flow rate during forced expiration 32. Which structures belong to the upper conduction airway? Ans: Oropharynx Nasopharynx 33. Regarding the respiratory process referred to as remodeling, which statements are true? Ans: Remodeling involves the vascular walls. Scarring and thickening occurs during this respiratory process. Remodeling results in a permanent change. Remodeling increases blood flow resistance. 34. What are the effects of aging on the pulmonary system? Ans: Decreased chest wall compliance Decreased lung recoil Reduced ventilatory reserve Decreased partial pressure of arterial oxygen (PaO2) Match the receptor with its function. _37_ A. Irritant receptors _39_ B. Stretch receptors _35_ C. J-receptors _36_ D. Peripheral chemoreceptors _38_ E. Central chemoreceptors 35. Initiates rapid, shallow breathing 36. Monitors pH, partial pressure of carbon dioxide (PaCO2), and partial pressure of oxygen (PaO2) in arterial blood 37. Initiates cough reflex 38. Senses pH of cerebrospinal fluid 39. Hering-Breuer expiratory reflex Chapter 36: Alterations of Pulmonary Function 1. Besides dyspnea, what is the most common characteristic associated with pulmonary disease? Ans: Cough 2. Sitting up in a forward-leaning position generally relieves which breathing disorder? Ans: Orthopnea 3. Kussmaul respirations as a respiratory pattern may be associated with which characteristic(s)? Ans: Slightly increased ventilatory rate, large tidal volumes, and no expiratory pause 4. Respirations that are characterized by alternating periods of deep and shallow breathing are a result of which respiratory mechanism? Ans: Decreased blood flow to the medulla oblongata 5. With a total hemoglobin of 9 g/dl, how many grams per deciliter of hemoglobin must become desaturated for cyanosis to occur? Ans: 5 6. Which statement is true regarding ventilation? Ans: Hyperventilation causes hypocapnia. 7. What term is used to describe the selective bulbous enlargement of the distal segment of a digit that is commonly associated with diseases that interfere with oxygenation of the blood? Ans: Clubbing 8. Pulmonary edema and pulmonary fibrosis cause hypoxemia by which mechanism? Ans: Impairing alveolocapillary membrane diffusion 9. High altitudes may produce hypoxemia through which mechanism? Ans: Decreased inspired oxygen 10. Which condition is capable of producing alveolar dead space? Ans: Pulmonary emboli 11. What is the most common cause of pulmonary edema? Ans: Left-sided heart failure 12. Pulmonary edema usually begins to develop at a pulmonary capillary wedge pressure or left atrial pressure of how many millimeters of mercury (mm Hg)? Ans: 20 13. The collapse of lung tissue caused by the lack of collateral ventilation through the pores of Kohn is referred to as what type of atelectasis? Ans: Absorption 14. In what form of bronchiectasis do both constrictions and dilations deform the bronchi? Ans: Varicose 15. Which pleural abnormality involves a site of pleural rupture that acts as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing during expiration? Ans: Tension pneumothorax 16. In which type of pleural effusion does the fluid become watery and diffuse out of the capillaries as a result of increased blood pressure or decreased capillary oncotic pressure? Ans: Transudative 17. Which condition involves an abnormally enlarged gas-exchange system and the destruction of the lung’s alveolar walls? Ans: Emphysema 18. Which term is used to identify a circumscribed area of suppuration and destruction of lung parenchyma? Ans: Abscess 19. Which condition is not a cause of chest wall restriction? Ans: Pneumothorax 20. What causes pneumoconiosis? Ans: Inhalation of inorganic dust particles 21. Which condition is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury? Ans: Acute respiratory distress syndrome (ARDS) 22. Which structure(s) in acute respiratory distress syndrome (ARDS) release inflammatory mediators such as proteolytic enzymes, oxygen-free radicals, prostaglandins, leukotrienes, and platelet- activating factor? Ans: Neutrophils 23. Pulmonary edema in acute respiratory distress syndrome (ARDS) is the result of an increase in: Ans: Capillary permeability 24. In acute respiratory distress syndrome (ARDS), alveoli and respiratory bronchioles fill with fluid as a result of which mechanism? Ans: Inactivation of surfactant and the impairment of type II alveolar cells 25. Which type of pulmonary disease requires more force to expire a volume of air? Ans: Obstructive 26. Which immunoglobulin (Ig) may contribute to the pathophysiologic characteristics of asthma? Ans: IgE 27. Which statement about the late asthmatic response is true? Ans: The release of toxic neuropeptides contributes to increased bronchial hyperresponsiveness. 28. Clinical manifestations of inspiratory and expiratory wheezing, dyspnea, nonproductive cough, and tachypnea are indicative of which condition? Ans: Asthma 29. The most successful treatment for chronic asthma begins with which action? Ans: Avoidance of the causative agent 30. Which factor contributes to the production of mucus associated with chronic bronchitis? Ans: Increased Goblet cell size 31. Clinical manifestations of decreased exercise tolerance, wheezing, shortness of breath, and productive cough are indicative of which respiratory disorder? Ans: Chronic bronchitis 32. Clinical manifestations that include unexplained weight loss, dyspnea on exertion, use of accessory muscles, and tachypnea with prolonged expiration are indicative of which respiratory disorder? Ans: Emphysema 33. Which of the following is the most common route of lower respiratory tract infection? Ans: Aspiration of oropharyngeal secretions 34. What is the initial step in the management of emphysema? Ans: Cessation of smoking 35. In tuberculosis, the body walls off the bacilli in a tubercle by stimulating which action? Ans: Apoptotic infected macrophages that activate cytotoxic T cells 36. The progression of chronic bronchitis is best halted by which intervention? Ans: Smoking cessation 37. Clinical manifestations of inspiratory crackles, increased tactile fremitus, egophony, and whispered pectoriloquy are indicative of which respiratory condition? Ans: Pneumonia 38. Pulmonary artery hypertension (PAH) results from which alteration? Ans: Narrowed pulmonary capillaries 39. Squamous cell carcinoma of the lung is best described as a tumor that causes which alterations? Ans: Airway obstruction and atelectasis 40. What medical term is used to identify the accumulation of air in the pleural space? Ans: Pneumothorax 41. What medical term is used to identify the presence of pus in the pleural space? Ans: Empyema 42. Fluid in the pleural space characterizes which condition? Ans: Pleural effusion 43. Which statement is true regarding hypoxemia? Ans: Respiratory alterations cause hypoxemia. 44. Which medication classification is generally included in the treatment of silicosis? Ans: Corticosteroids 45. What medical term is used for a condition that results from pulmonary hypertension, creating chronic pressure overload in the right ventricle? Ans: Cor pulmonale 46. What are the causes of dyspnea? Ans: Decreased pH, increased partial pressure of arterial carbon dioxide (PaCO2) and decreased partial pressure of arterial oxygen (PaO2) Stimulation of stretch or J-receptors Presence of anxiety 47. Which inflammatory mediators are produced in asthma? Ans: Histamine Bradykinin Leukotrienes Prostaglandins 48. Which clinical manifestation is associated with pulmonary hypertension? Ans: Dyspnea on exertion Peripheral edema Jugular venous distention 49. Which statements are true regarding exudative effusion? Ans: Exudative effusion contains high concentrations of white blood cells. Exudative effusion may occur in response to an inflammatory process. The presence of a malignant cancer can trigger exudative effusion. Exudative effusion is a result of increased capillary permeability. 50. Which characteristics are symptomatic of a flail chest? Ans: Involves the fracture of several consecutive ribs. Involves multiple fractures to individual ribs. Can involve the fracture of the sternum. 51. Which statements regarding Mycobacterium tuberculosis are true regarding the bacilli’s ability to go into dormancy? Ans: Neutrophils and macrophages all play a role in its dormancy. The immune system is the controlling factor regarding its length of dormancy. The bacilli are sealed off in tubercles to allow for dormancy. Match the descriptions with the corresponding terms. _55_ A. Passage of fluid and solid particles into the lung _56_ B. Inflammatory obstruction of small airways _52_ C. Excessive amount of connective tissue in the lung _53_ D. Lung tissue collapse _54_ E. Abnormal dilation of the bronchi 52. Pulmonary fibrosis 53. Atelectasis 54. Bronchiectasis 55. Aspiration 56. Bronchiolitis Chapter 38: Structure and Function of the Renal and Urologic Systems 1. The area of the kidneys that contains the glomeruli and portions of the tubules is called the: Ans: Cortex 2. What is the functional unit of the kidney called? Ans: Nephron 3. Which cells have phagocytic properties similar to monocytes and contract like smooth muscles cells, thereby influencing the glomerular filtration rate? Ans: Mesangial cells 4. The only surface inside the nephron where cells are covered with microvilli to increase the reabsorptive surface area is called the: Ans: Proximal convoluted tubules 5. What part of the kidney controls renal blood flow, glomerular filtration, and renin secretion? Ans: Juxtaglomerular apparatus (JGA) 6. Kidney stones in the upper part of the ureter would produce pain referred to which anatomical area? Ans: Umbilicus 7. Innervation of the bladder and internal urethral sphincter is supplied by which nerves? Ans: Parasympathetic fibers 8. How much urine accumulates in the bladder before the mechanoreceptors sense bladder fullness? Ans: 250 to 300 ml 9. What is the trigone? Ans: A smooth triangular area between the openings of the two ureters and the urethra 10. The glomerular filtration rate is directly related to which factor? Ans: Perfusion pressure in the glomerular capillaries 11. On average, what percent of cardiac output do the kidneys receive? Ans: 20% to 25% 12. What effects do exercise and body position have on renal blood flow? Ans: They activate renal sympathetic neurons and cause mild vasoconstriction. 13. Blood vessels of the kidneys are innervated by the: Ans: Sympathetic nervous system 14. When renin is released, it is capable of which action? Ans: Formation of angiotensin I 15. What effect do natriuretic peptides have during heart failure when the heart dilates? Ans: Inhibits renin and aldosterone. 16. What is the direct action of atrial natriuretic hormone? Ans: Sodium excretion 17. What term is used to identify the movement of fluids and solutes from the tubular lumen to the peritubular capillary plasma? Ans: Tubular reabsorption 18. How high does the plasma glucose have to be before the threshold for glucose is achieved? Ans: 180 mg/dl 19. Which hormone is required for water to be reabsorbed in the distal tubule and collecting duct? Ans: Antidiuretic hormone 20. Which glycoprotein protects against urolithiasis and is a ligand for lymphokines? Ans: Uromodulin 21. What is the end-product of protein metabolism that is excreted in urine? Ans: Urea 22. What is the action of urodilatin? Ans: It inhibits salt and water reabsorption. 23. The concentration of the final urine is determined by antidiuretic hormone (ADH), which is secreted by which gland? Ans: Posterior pituitary 24. Which statement is true regarding urodilatin? Ans: Urodilatin is stimulated by a rise in blood pressure and an increase in extracellular volume. 25. What substance stimulates renal hydroxylation in the process of producing vitamin D? Ans: Parathyroid hormone 26. Which hormone is synthesized and secreted by the kidneys? Ans: Erythropoietin 27. What provides the best estimate of the functioning of renal tissue? Ans: Glomerular filtration rate 28. Which renal change is found in older adults? Ans: Decrease in the number of nephrons 29. Compared with a younger individual, how is the specific gravity of urine in older adults affected? Ans: Specific gravity of urine in older adults is considered low normal. 30. What process allows the kidney to respond to an increase in workload? Ans: Compensatory hypertrophy 31. Which process makes it possible for ureters to be transplanted successfully? Ans: Peristalsis 32. Which structures are parts of the nephron? Ans: Loop of Henle Renal corpuscle Proximal convoluted tubule Collecting duct 33. Which forces create passive transport of water in the proximal tubule? Ans: Peritubular capillary oncotic pressure Peritubular capillary osmotic pressure 34. Which hormones are produced by the kidney? Ans: Renin Erythropoietin 1,25-dihydroxyvitamin D3 35. Which statements are true regarding renal circulation? Ans: The interlobar arteries travel down into the renal columns. The arcuate arteries arch over the base of the pyramids. The interlobar arteries run between the pyramids. Match the descriptions with the corresponding terms. _39_ A. Good estimate of glomerular filtration rate _36_ B. Form in concentrated acidic or alkaline urine _37_ C. Cylindric with distinct borders _40_ D. Hematuria _38_ E. Pyuria 36. Crystals 37. Casts 38. Leukocytes 39. Creatinine clearance 40. Erythrocytes Chapter 39: Alterations of Renal and Urinary Tract Function 1. How does progressive nephrons injury affect angiotensin II activity? Ans: It is elevated. 2. Which mineral accounts for the most common type of renal stone? Ans: Calcium oxalate 3. Regarding the formation of renal calculi, what function does pyrophosphate, potassium citrate, and magnesium perform? Ans: They inhibit crystal growth. 4. Hypercalciuria is primarily attributable to which alteration? Ans: Intestinal hyperabsorption of dietary calcium 5. Detrusor hyperreflexia develops from neurologic disorders that originate where? Ans: Above the pontine micturition center 6. Considering the innervation of the circular muscles of the bladder neck, which classification of drug is used to treat bladder neck obstruction? Ans: ?-Adrenergic blocking medications 7. Renal cell carcinoma, classified as clear cell tumors, arises from epithelial cells in which structure? Ans: Proximal tubule 8. Bladder cancer is associated with the gene mutation of which gene? Ans: TP53 9. What is the most common cause of uncomplicated urinary tract infections? Ans: Escherichia coli 10. Which differentiating sign is required to make the diagnosis of pyelonephritis from that of cystitis? Ans: Urinalysis confirmation of white blood cell casts 11. Considering host defense mechanisms, which element in the urine is bacteriostatic? Ans: High urea 12. Which clinical manifestations of a urinary tract infection may be demonstrated in an 85-year-old individual? Ans: Confusion and poorly localized abdominal discomfort 13. Pyelonephritis is usually caused by which type of organism? Ans: Bacteria 14. Which abnormal laboratory value is found in glomerular disorders? Ans: Elevated creatinine concentration 15. Which glomerular lesion is characterized by thickening of the glomerular capillary wall with immune deposition of immunoglobulin G (IgG) and C3? Ans: Membranous 16. Goodpasture syndrome is an example of which of the following? Ans: Antiglomerular basement membrane disease 17. A patient exhibits symptoms including hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin as the major protein. These data suggest the presence of which disorder? Ans: Glomerulonephritis 18. Hypothyroidism, edema, hyperlipidemia, and lipiduria characterize which kidney disorder? Ans: Nephrotic syndrome 19. Which antibiotics are considered “major culprits” in causing nephrotoxic acute tubular necrosis (ATN)? Ans: Gentamicin and tobramycin 20. Which urine characteristics are indicative of acute tubular necrosis (ATN) caused by intrinsic (intrarenal) failure? Ans: Urine sodium >30 mEq/L 21. How are glucose and insulin used to treat hyperkalemia associated with acute renal failure? Ans: When insulin transports glucose into the cell, it also carries potassium with it. 22. Creatinine is primarily excreted by glomerular filtration after being constantly released from what type of tissue? Ans: Muscle 23. Which statement is false concerning the skeletal alterations caused by chronic renal failure when the glomerular filtration rate (GFR) declines to 25% of normal? Ans: The parathyroid gland is no longer able to secrete sufficient parathyroid hormone. 24. Anemia of chronic renal failure can be successfully treated with which element? Ans: Erythropoietin 25. When the right kidney is obstructed, how will the glomeruli and tubules in the left kidney compensate? Ans: Increase in size 26. What medical term is used to identify a functional urinary tract obstruction caused by an interruption of the nerve supply to the bladder? Ans: Neurogenic bladder 27. In glomerulonephritis, what damages the epithelial cells resulting in proteinuria? Ans: Activated complement Altered membrane permeability 28. Which statements are true concerning struvite stones? Ans: They are more common in women than in men. They grow large and branch into a staghorn configuration in renal pelvis and calyces. Struvite stones are closely associated with urinary tract infections caused by urease-producing bacteria, such as Pseudomonas. 29. Which statements are true regarding renal colic? Ans: Pain originates in the flank area. Renal colic indicates the presence of renal stones. Pain radiated to the groin. Renal colic indicates obstruction of the renal pelvis or proximal ureter. 30. Which conditions related to the bladder would result from the effects of lesions of the sacral segments below S1? Ans: Bladder distension Urinary retention 31. What are considered risk factors for developing bladder and kidney cancers Ans: Cigarette smoking Hypertension Exposure to aniline dyes 32. Which renal disorders are considered causes of intrarenal renal failure? Ans: Acute glomerulonephritis Allograft rejection Tumors Acute tubular necrosis (ATN) 33. Prerenal injury from poor perfusion can result from which condition? Ans: Renal vasoconstriction Renal artery thrombosis Hemorrhage Hypotension Match the predisposing factors causing pyelonephritis to the pathology mechanism. _37_ A. Kidney stones _38_ B. Vesicoureteral reflux _35_ C. Pregnancy _36_ D. Neurogenic bladder _34_ E. Female sexual trauma 34. Movement of organisms from the urethra into the bladder with infection and retrograde spread to the kidney 35. Dilation and relaxation of the ureter with hydroureter and hydronephrosis 36. Impairment to the bladder, interfering with normal bladder contraction and causing residual urine and ascending infection 37. Obstruction and stasis of urine, contributing to bacteremia and hydronephrosis; irritation of epithelial lining with entrapment of bacteria 38. Chronic reflux of urine up the ureter and into the kidney during micturition, contributing to bacterial infection Chapter 41: Structure and Function of the Digestive System 1. In the mouth and stomach, salivary ?-amylase initiates the digestion of which nutrients? Ans: Carbohydrates 2. Which elements in saliva protect against tooth decay? Ans: Exogenous fluoride and a pH of 7.4 ANS: D 3. Saliva contains which immunoglobulin (Ig)? Ans: IgA 4. What effect is a result of inhibiting the parasympathetic nervous system with a drug such as atropine? Ans: Salivation decreases. 5. Food enters the stomach via which sphincter? Ans: Cardiac 6. Which gastric cells secrete hydrochloric acid and intrinsic factor? Ans: Parietal 7. Which cells in the stomach secrete histamine? Ans: Enterochromaffin-like 8. The presence of chyme in the duodenum stimulates which hormones? Ans: Secretin and cholecystokinin 9. Which gastric hormone inhibits acid and pepsinogen secretion, as well as decrease the release of gastrin? Ans: Somatostatin 10. Which enzyme breaks down protein-forming polypeptides in the stomach? Ans: Pepsin 11. Exposure to which substance protects the mucosal barrier of the stomach? Ans: Prostaglandins 12. The ileum and jejunum are suspended by folds of the peritoneum that contain an extensive vascular and nervous network. What are these folds called? Ans: Mesentery 13. Where in the small intestines are lymphocytes, plasma cells, and macrophages produced? Ans: Lamina propria 14. Why are water and electrolytes transported in both directions through tight junctions and intercellular spaces rather than across cell membranes? Ans: The epithelial cell membranes are formed of lipids that are hydrophobic and therefore repel water. 15. Which statement best describes the gastrointestinal tract? Ans: The gastrointestinal tract is a hollow tube that extends from the mouth to the anus. 16. Glucose transport enhances the absorption of which electrolyte? Ans: Sodium 17. What process is capable of increasing both intrathoracic and intraabdominal pressure, thereby facilitating defecation? Ans: Valsalva maneuver 18. Which pancreatic enzyme is responsible for the breakdown of carbohydrates? Ans: Amylase d. Chymotrypsin 19. The formation of water-soluble molecules to facilitate the absorption of the by-products of lipid hydrolysis is accomplished by: Ans: Micelles 20. What is the primary source of physiologic iron? Ans: Heme from animal protein 21. Which statement is incorrect regarding the characteristics of vitamin B12? Ans: Vitamin B12 is necessary for platelet maturation. 22. Which water-soluble vitamin is absorbed by passive diffusion? Ans: Vitamin B6 23. Which vitamin facilitates the absorption of iron by the epithelial cells of the duodenum and jejunum? Ans: C 24. What is the role of the normal intestinal bacterial flora? Ans: Metabolizing bile salts, estrogens, and lipids 25. Kupffer cells are best described as: Ans: Bactericidal and therefore central to innate immunity 26. Bilirubin is a by-product of the destruction of which aged cells? Ans: Erythrocytes 27. The process of conjugation of bilirubin in the liver is best described as which transformation? Ans: Unconjugated (fat-soluble) bilirubin into conjugated (water-soluble) bilirubin 28. Which statement is incorrect regarding gallbladder function? Ans: Within 30 minutes of eating, the gallbladder forces bile into the stomach. 29. Which structure synthesizes clotting factors and the vitamin K necessary for hemostasis? Ans: Liver 30. How many days does it take for the entire epithelial population of the small intestines to be replaced? Ans: 4 to 7 31. Which statement is true regarding the state of the intestinal tract at birth? Ans: The intestinal tract is sterile. 32. Gastric emptying is delayed by the presence of which substances? Ans: Solids Nonisotonic solutions Fats 33. Which statements are true regarding the ileogastric reflex? Ans: The purpose of ileogastric reflex is to inhibit gastric motility. Ileum distension triggers the ileogastric reflex. 34. Which hormones are involved in the relaxation of the stomach’s fundus during swallowing? Ans: Gastrin Cholecystokinin 35. Which hormones are involved in regulating gastric motility by making the threshold potential of muscle fibers more negative? Ans: Secretin Gastrin Motilin 36. What requirements are necessary for calcium to be absorbed through the ileum at concentrations of less than 5 mmol/L? Ans: Vitamin D3 A carrier protein 37. Which water-soluble vitamins are dependent on sodium for absorption? Ans: Vitamin C Folic acid 38. Which statement is correct regarding the functions of the pancreas? Ans: Cholecystokinin stimulates the release of pancreatic enzymes. Pancreatic polypeptide is released after eating. Acetylcholine (ACh) is liberated from the pancreatic branches of the vagus nerve. Match the hormone from the small intestine with its action. Hormones may be used more than once. _41_ A. Peptide YY _40_ B. Secretin _39_ C. Cholecystokinin _43_ D. Enteroglucagon _42_ E. Pancreatic polypeptide 39. Stimulates the gallbladder to eject bile and the pancreas to secrete alkaline fluid. 40. Stimulates the pancreas to secrete alkaline pancreatic juices. 41. Delays gastric and small bowel emptying. 42. Decreases pancreatic and enzyme secretions. 43. Enhances insulin release, lipolysis, and ketogenesis. Chapter 42: Alterations of Digestive Function 1. Where in the brain is the vomiting center located? Ans: Medulla oblongata 2. Antiemetic agents, such as domperidone and haloperidol, are antagonists for which receptors? Ans: Dopamine 3. What type of vomiting is caused by the direct stimulation of the vomiting center by neurologic lesions involving the brainstem? Ans: Projectile 4. Considering the normal frequency of bowel evacuation, how infrequently can evacuation occur and still be considered within normal range? Ans: Once a week 5. How many stools per day are considered the upper limits of normal? Ans: Three 6. The adult intestine processes approximately how many liters of luminal content per day? Ans: 9 7. A person who has cholera would be expected to have which type of diarrhea? Ans: Secretory 8. What type of diarrhea is a result of lactase deficiency? Ans: Osmotic 9. Which statement is false concerning how abdominal pain is produced? Ans: Low concentrations of anaerobes, such as Streptococci, Lactobacilli, Staphylococci, Enterobacteria, and Bacteroides, produce abdominal pain. 10. How can abdominal pain that is visceral in nature best be described? Ans: Abdominal pain that is visceral in nature is diffused, vague, poorly localized, and dull. 11. What is the cause of gastroesophageal reflux disease? Ans: Zone of low pressure of the lower esophageal sphincter 12. What term is used to identify frank bleeding of the rectum? Ans: Hematochezia 13. What is the cause of functional dysphagia? Ans: Neural or muscular disorders 14. What is the cause of reflux esophagitis? Ans: Delayed gastric emptying 15. By what mechanism does intussusception cause an intestinal obstruction? Ans: Telescoping of part of the intestine into another section of intestine, usually causing strangulation of the blood supply 16. What is the most immediate result of a small intestinal obstruction? Ans: Distention 17. An intestinal obstruction at the pylorus or high in the small intestine causes metabolic alkalosis by causing which outcome? Ans: Excessive loss of hydrogen ions normally absorbed from gastric juices 18. What are the cardinal symptoms of small intestinal obstruction? Ans: Colicky pain caused by distention, followed by vomiting 19. What is a cause of chronic antral gastritis? Ans: Helicobacter pylori bacteria 20. What is the primary cause of peptic ulcers? Ans: Helicobacter pylori 21. A peptic ulcer may occur in all of the following areas except the: Ans: Jejunum 22. Which statement is false regarding the contributing factors of duodenal ulcers? Ans: Gastric emptying is slowed, causing greater exposure of the mucosa to acid. 23. After a partial gastrectomy or pyloroplasty, clinical manifestations that include increased pulse, hypotension, weakness, pallor, sweating, and dizziness are the results of which mechanism? Ans: Rapid gastric emptying and the creation of a high osmotic gradient in the small intestine, causing a sudden shift of fluid from the blood vessels to the intestinal lumen 24. Which statement is consistent with dumping syndrome? Ans: Dumping syndrome usually responds well to dietary management. 25. What stimulates the desire to eat? Ans: Agouti-related protein (AgRP) 26. Which structure regulates eating behavior and energy metabolism? Ans: Hypothalamus 27. Which symptom is characteristic of bulimia nervosa? Ans: Recurrent episodes of binge eating with fears of not being able to stop eating. 28. The most common clinical manifestation of portal hypertension is what type of bleeding? Ans: Esophageal 29. What is the most common manifestation of portal hypertension–induced splenomegaly? Ans: Thrombocytopenia 30. Which statement is false concerning the accumulation of fluid in the peritoneal cavity? Ans: Circulating nitric oxide causes vasoconstriction, which forces fluid from the capillaries into the peritoneal cavity. 31. Which statement is false regarding the sources of increased ammonia that contribute to hepatic encephalopathy? Ans: Accumulation of short-chain fatty acids that is attached to ammonia is a source of increased ammonia. 32. Hepatic fat accumulation is observed in which form of cirrhosis? Ans: Alcoholic 33. Which statement is false concerning the pathophysiologic process of alcoholic cirrhosis? Ans: Inflammation and damage leading to cirrhosis begin in the bile canaliculi. 34. Which statement is false regarding the pathophysiologic process of acute pancreatitis? Ans: Acute pancreatitis is an autoimmune disease in which immunoglobulin G (IgG) coats the pancreatic acinar cells; consequently, the pancreatic enzymes destroy the cells. 35. The mutation of which gene is an early event associated with the pathogenetic origin of esophageal cancer? Ans: TP53 36. Obesity is defined as a body mass index (BMI) greater than what measurement? Ans: 30 37. Which statements are true regarding parietal pain? Ans: Parietal pain arises from the parietal peritoneum. It is generally more localized than visceral pain. Nerve fibers that travel to the spinal cord are involved in parietal pain. Parietal pain corresponds to dermatomes T6 and L1. 38. Which statements are true regarding chronic gastritis? Ans: Chronic gastritis tends to occur in older adults. Chronic gastritis results in chronic inflammation and mucosal atrophy. Mucosal atrophy is a common outcome of chronic gastritis. Epithelial metaplasia is often observed with chronic gastritis. 39. Which hormones are natural appetite suppressants? Ans: Insulin Calcitonin Serotonin 40. Which are the early (prodromal) clinical manifestations of hepatitis? Ans: Fatigue Vomiting Hyperalgia 41. Which clinical manifestations are consistent with cancer of the cecum and ascending colon? Ans: Mahogany-colored blood mixed with stool Anemia Pain Palpable mass in the lower right quadrant Match the descriptions with the corresponding terms. _43_ A. Ulcerative colitis _42_ B. Crohn disease 42. Alterations in immunoglobulin G (IgA) production have been found in individuals with this disorder. 43. Inflammation develops in crypts of Lieberkühn in the large intestine. [Show More]
Last updated: 1 year ago
Preview 1 out of 124 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 19, 2021
Number of pages
124
Written in
Additional information
This document has been written for:
Uploaded
Apr 19, 2021
Downloads
0
Views
37




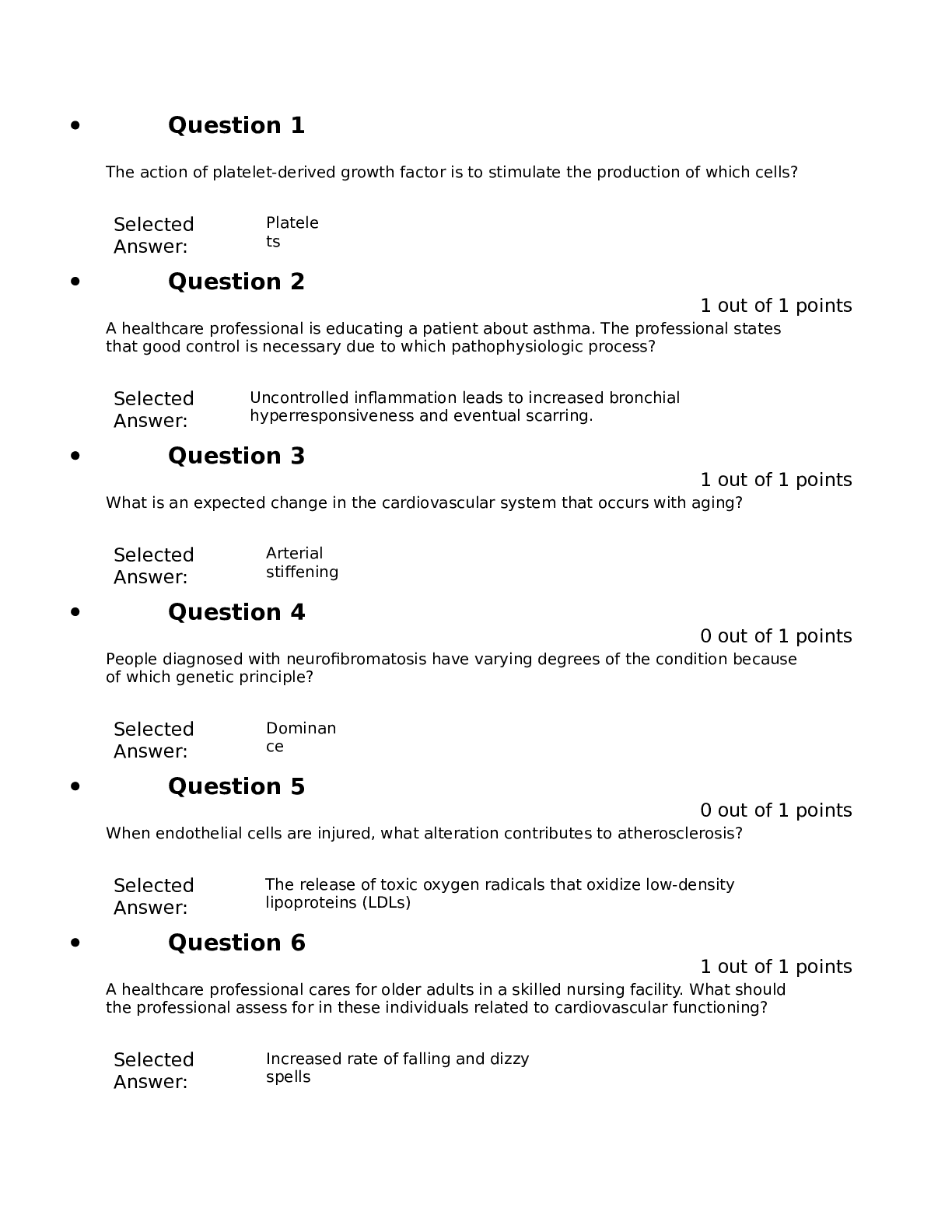
.png)
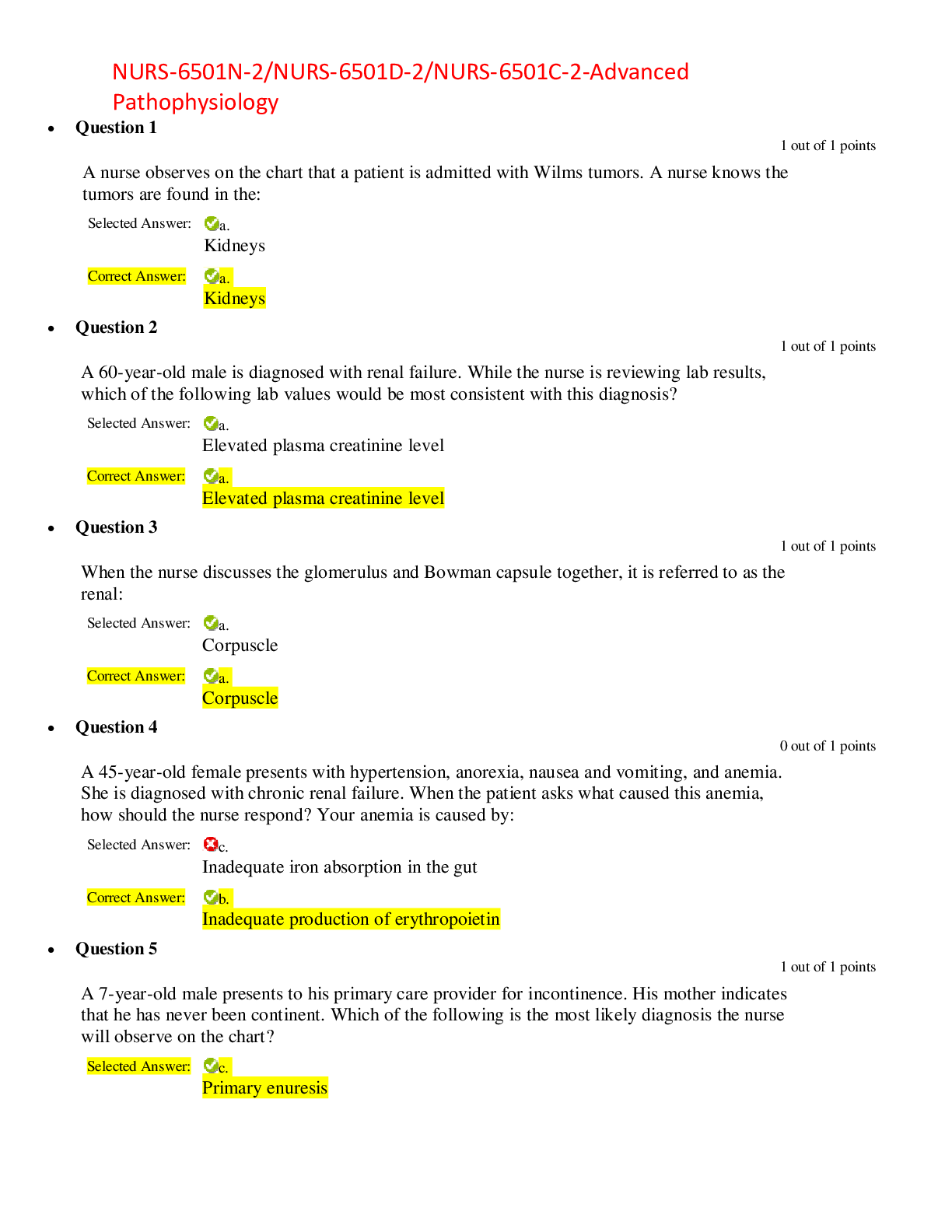
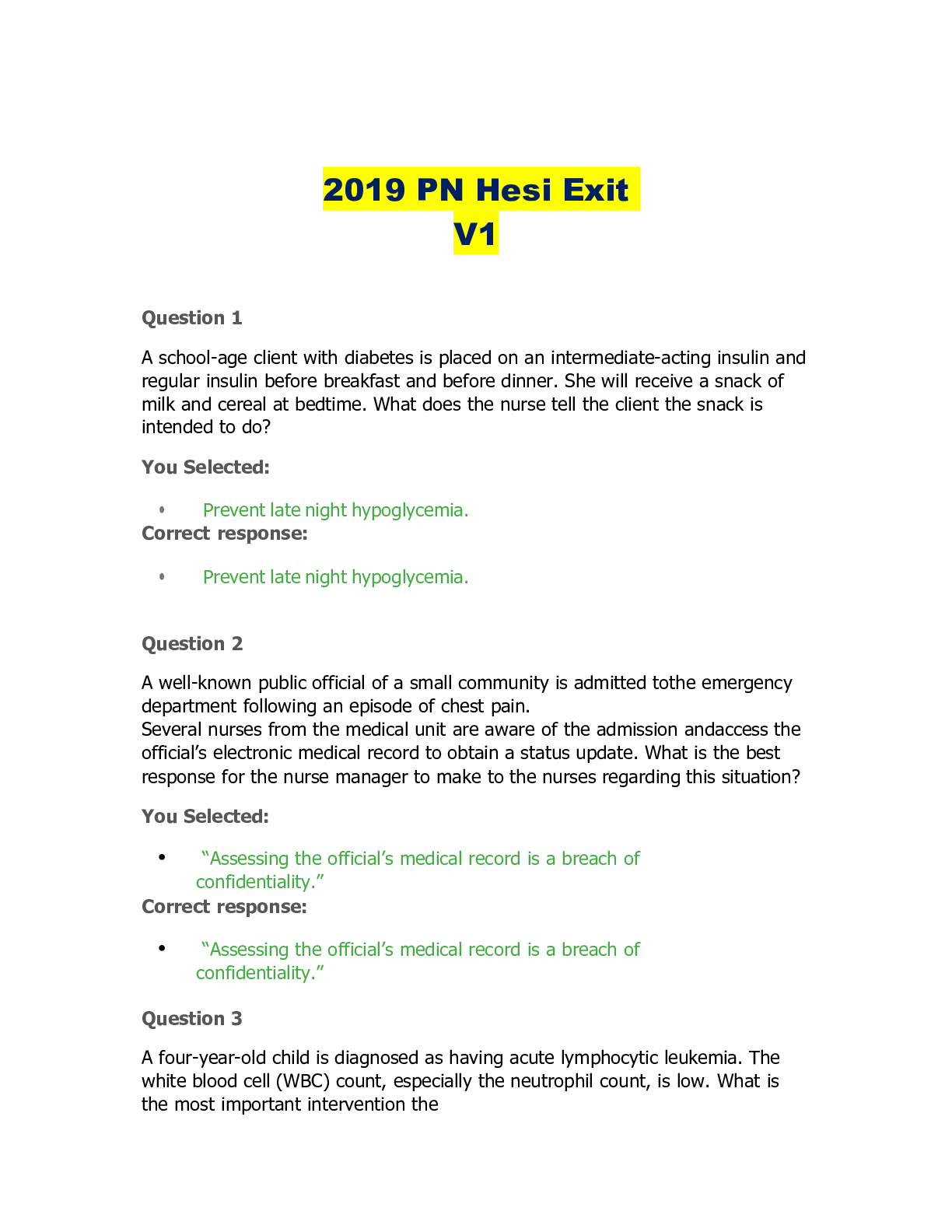

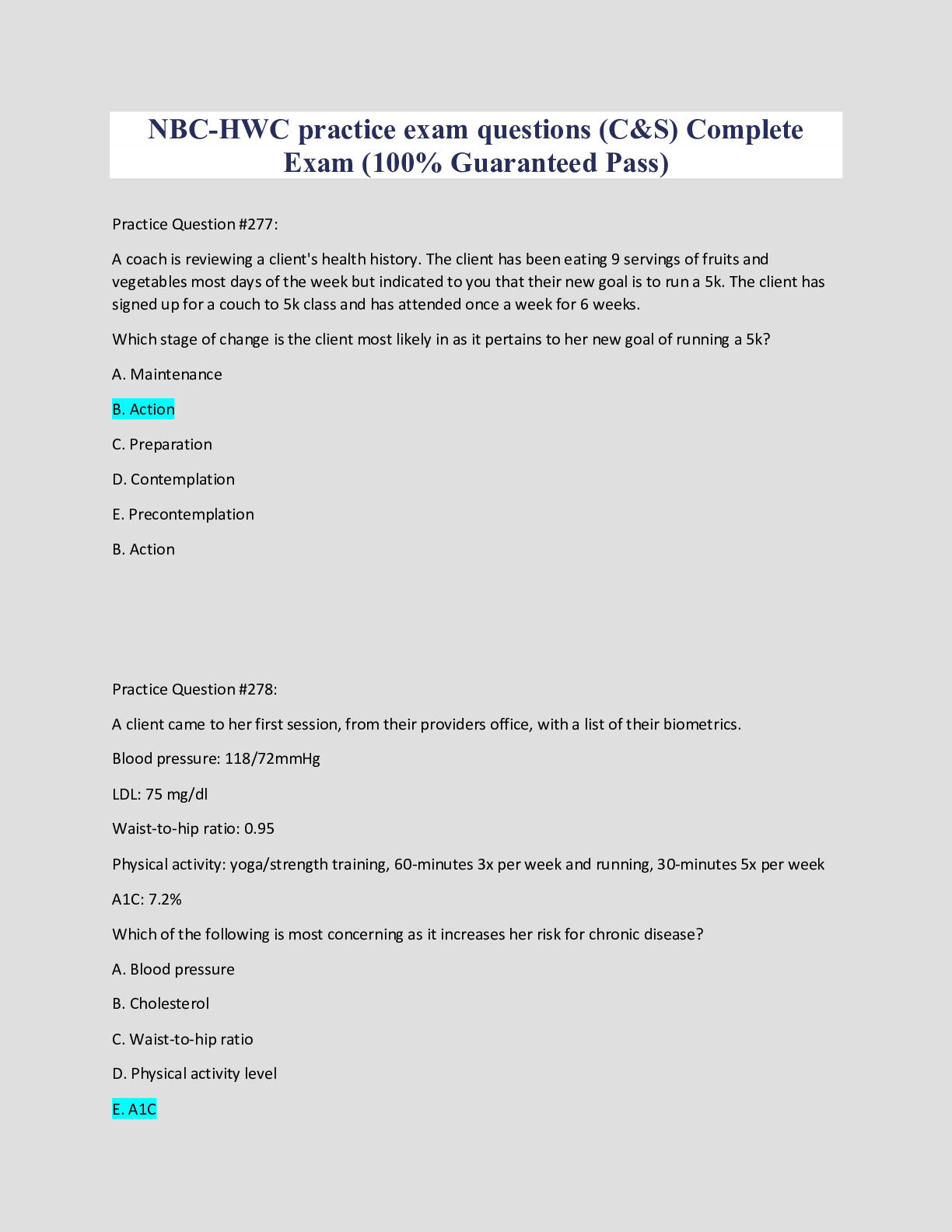
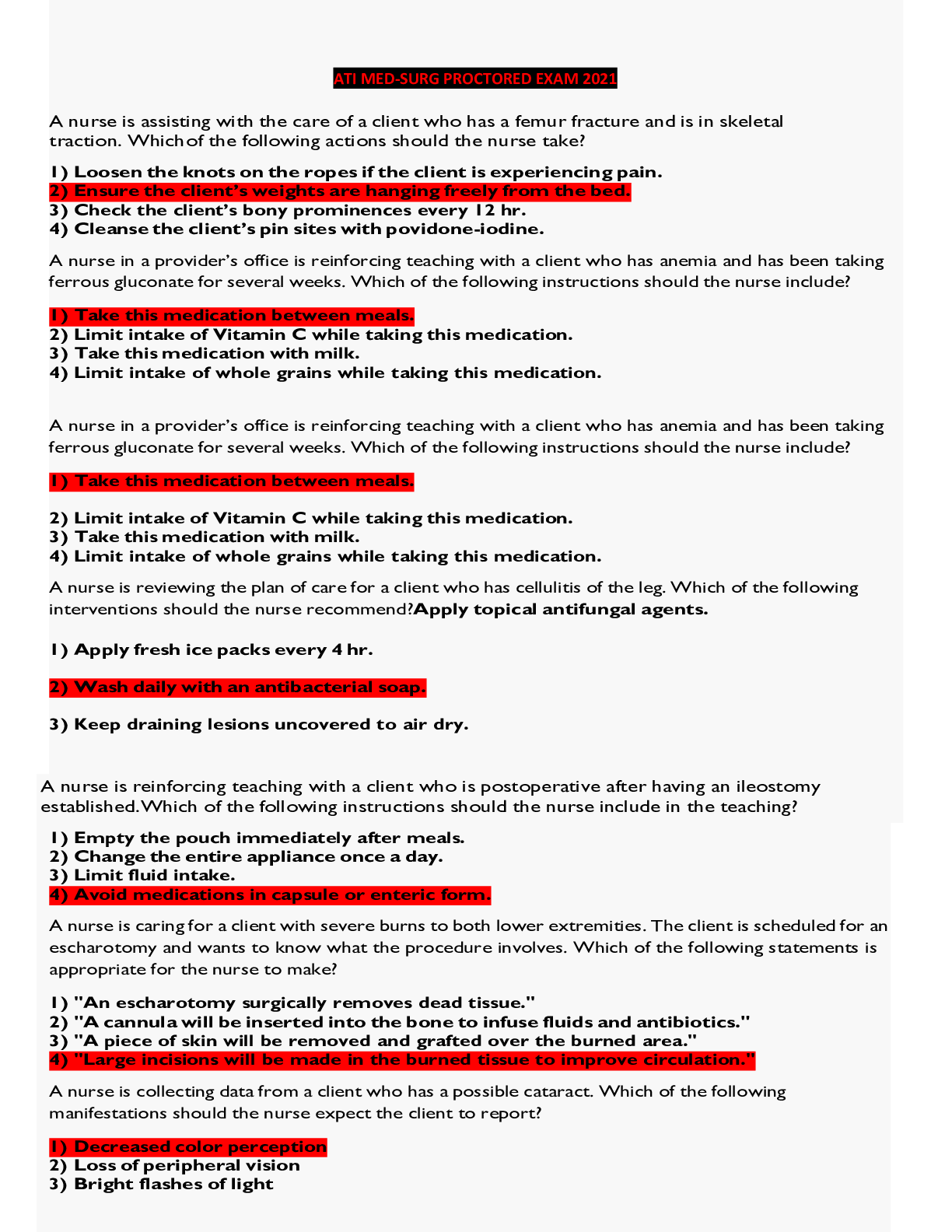
 – Chamberlain College of Nursing.png)