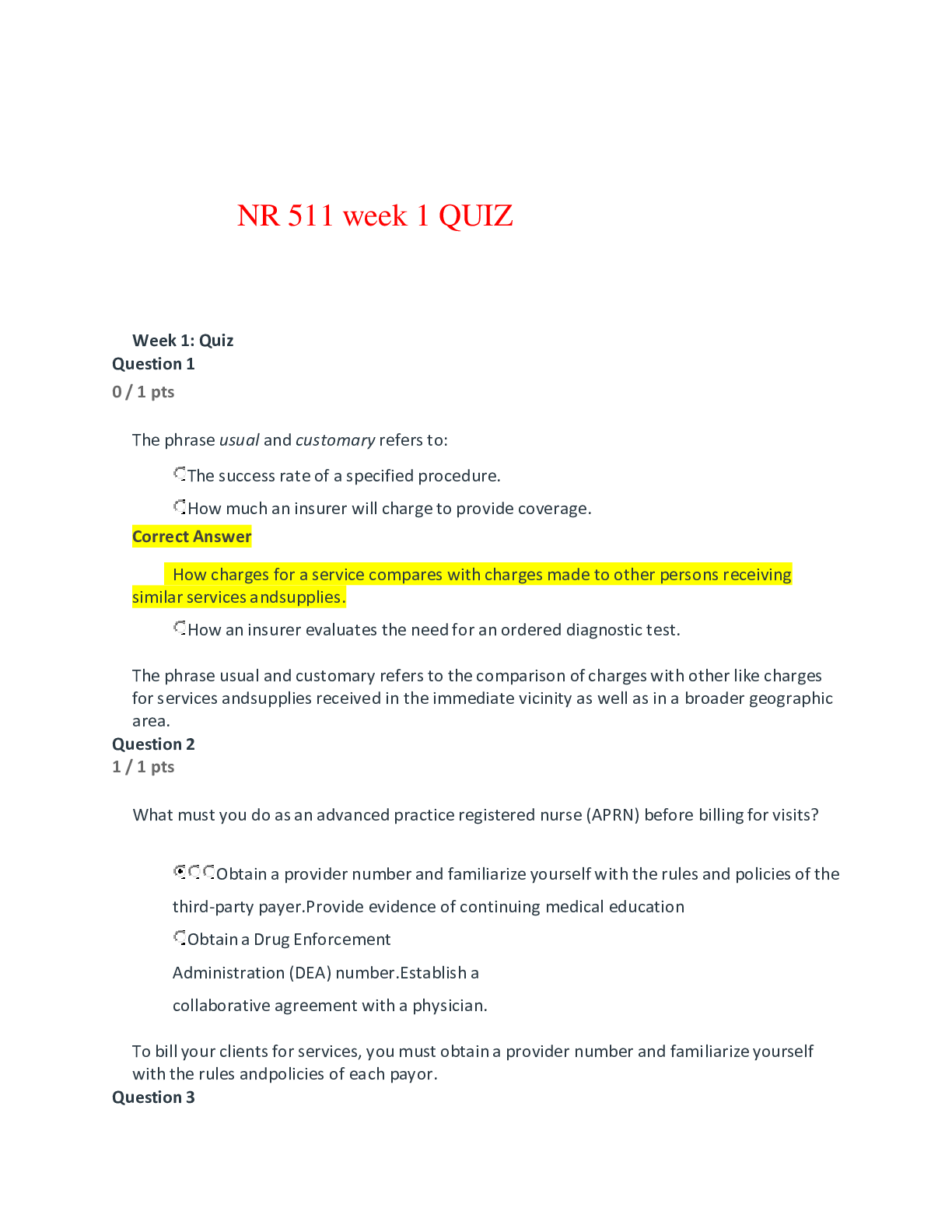
*NURSING > QUESTIONS & ANSWERS > nr 511-week-1-quiz (All)
nr 511-week-1-quiz
Document Content and Description Below
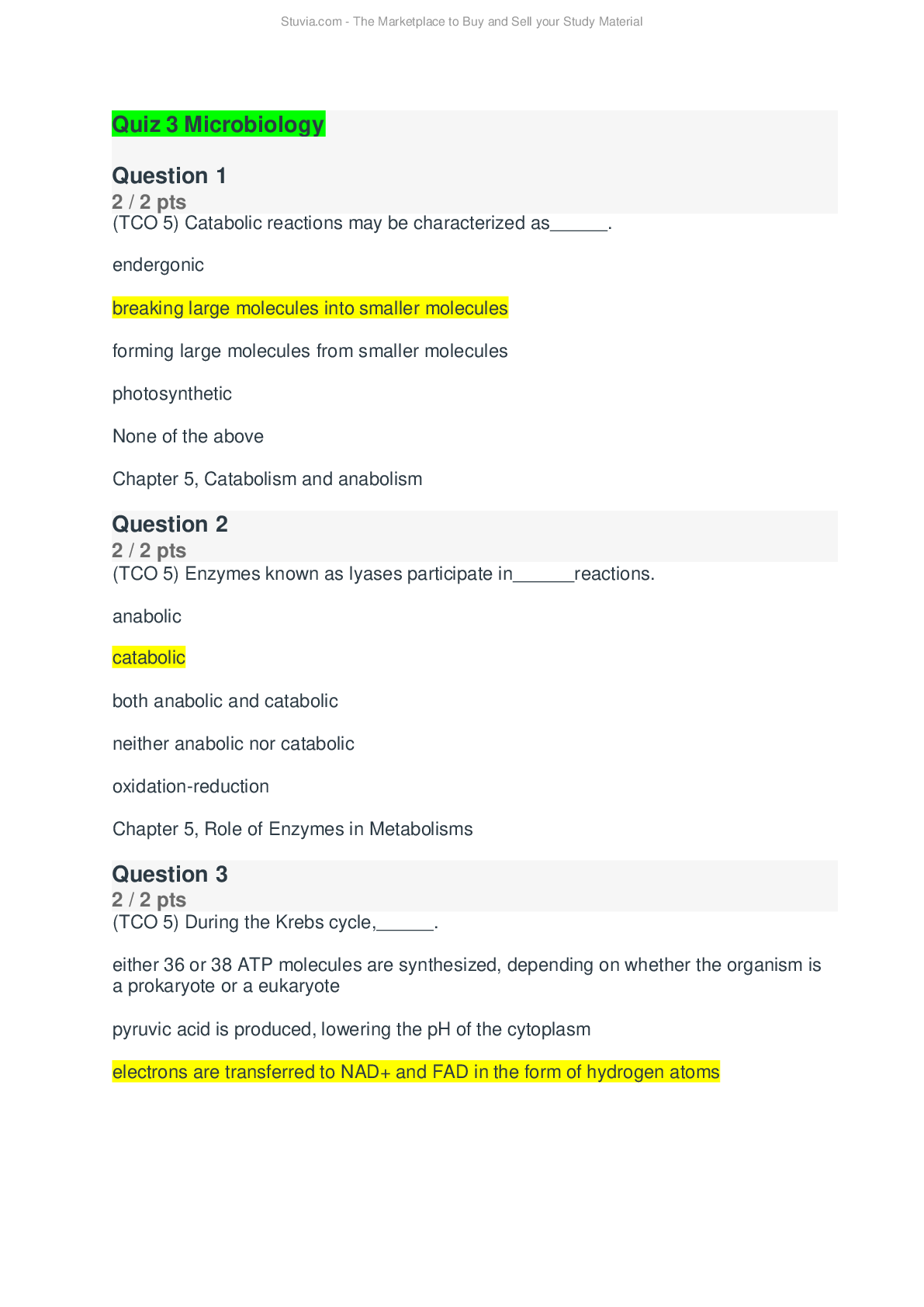
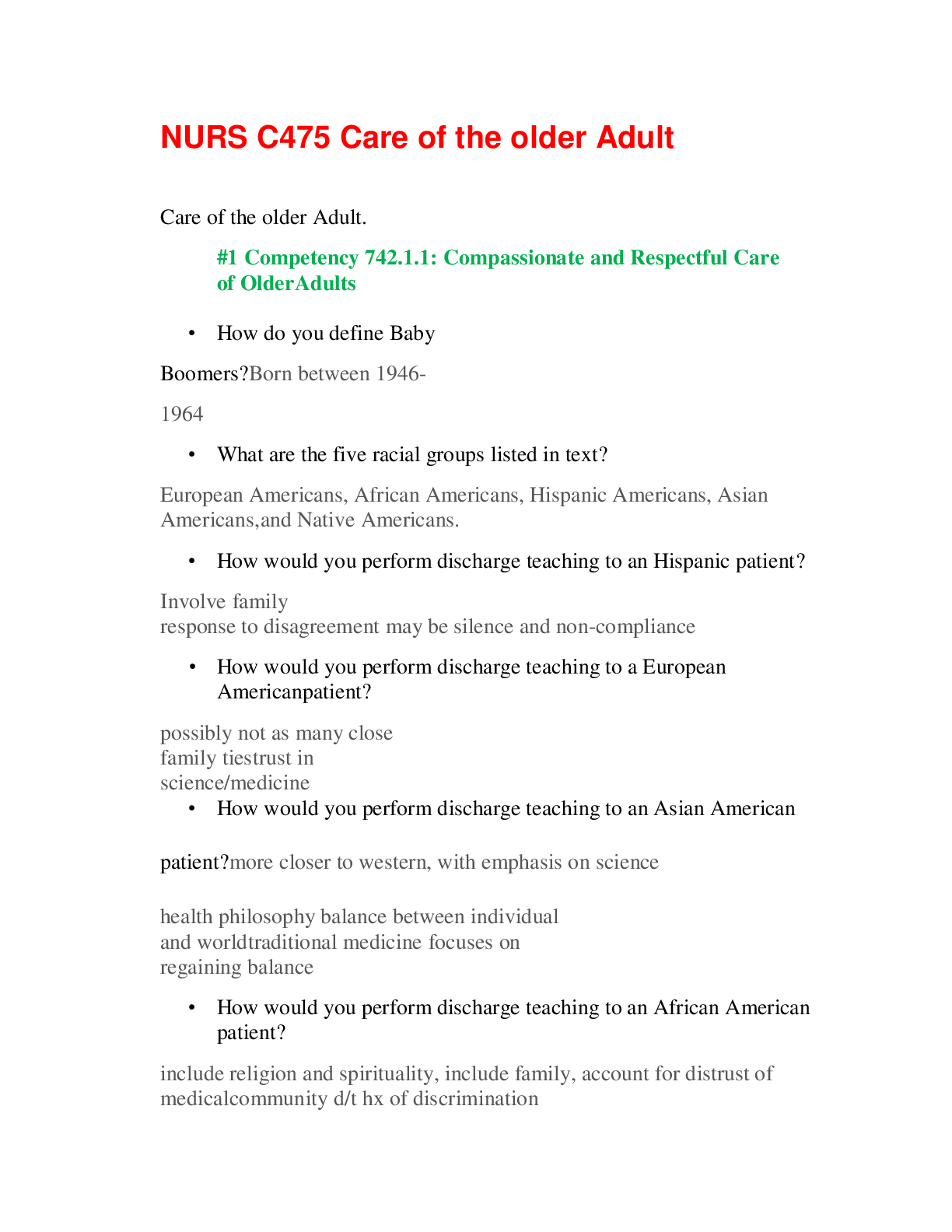
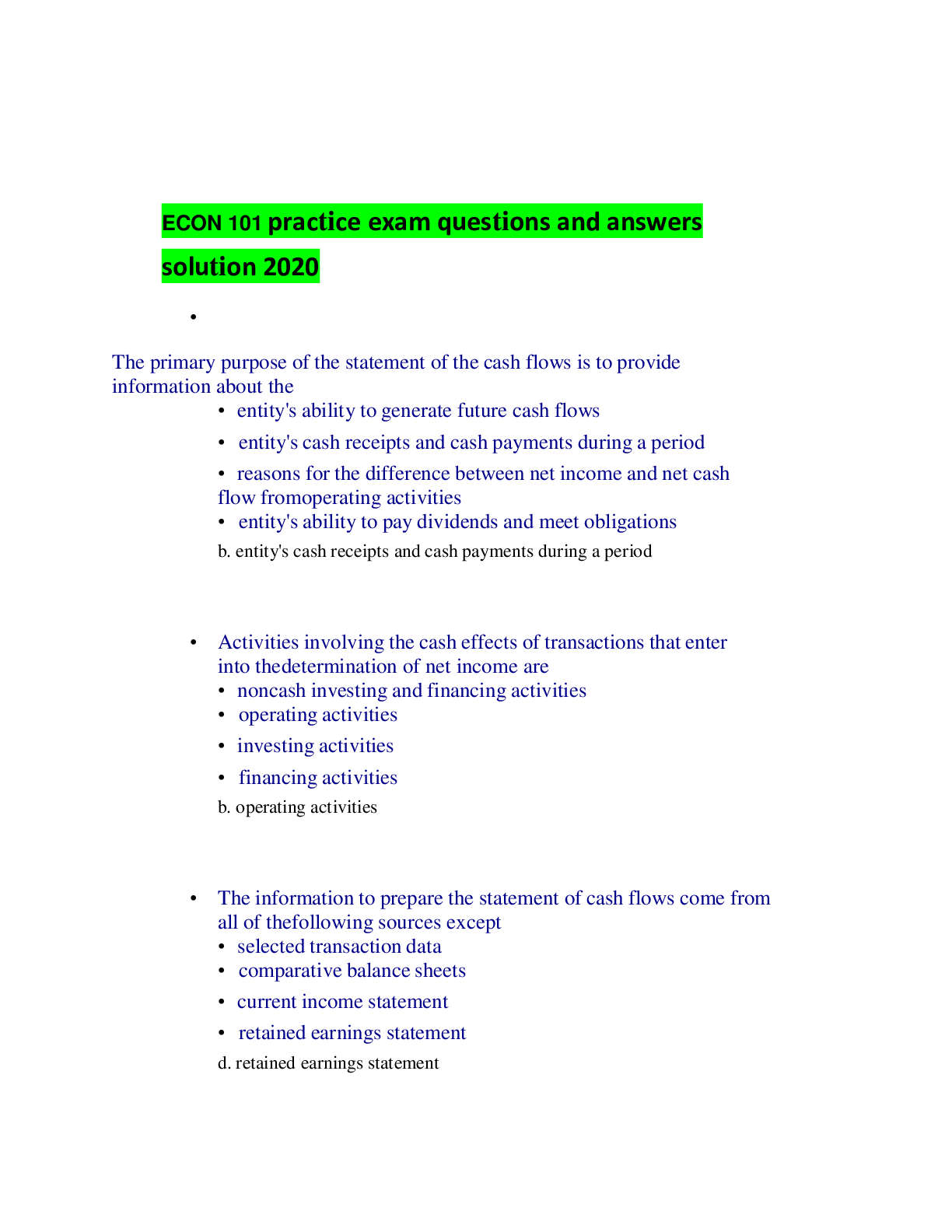
Which one of the following is true regarding the importance of documentation? It allows you to communicate your findings to other providers and serves as a record for the visit. It is only import... ant in order to bill the patient for your service. It is only important for defending yourself in the event of a law suit. It allows you to communicate your findings with the general public. The purposes of documentation are to record the patient's report of symptoms, PMH, lifestyle and family factors, positive and negative findings on physical exam and the provider's plan. Documentation is important for billing purposes, communication with other providers and in the case litigation. https://www.coursehero.com/file/63618854/Quiz-1docx/ Question 4 0 / 1 pts Which of the following statements does not belong in the past medical history portion of your chart note? Correct Answer Your patient had lab work done at their last appointment; CBC was normal. Your patient’s father passed away from lung cancer. Your patient had a cholecystectomy 3 years prior. Your patient has an allergy to penicillin. Allergies, family history and surgical history all belong in the history portion of your note. Test results are objective findings and should be in the diagnostic tests (objective) section of the note. Question 5 1 / 1 pts In relation to writing a patient encounter note, the acronym SOAP stands for which of the following? Subjective, objective, assessment, plan. Symptoms, observations, assessment, plan. Symptoms, objective findings, assessment, plan. Subjective, outward findings, assessment, plan. The acronym SOAP stands for subjective, objective, assessment and plan. Question 6 0 / 1 pts Most health maintenance organizations (HMOs) use a reimbursement mechanism called capitation. What does this mean? The HMO reimburses the provider on a fee-for-service basis. The HMO is not responsible for provider reimbursement. The HMO reimburses the provider only if the patient has paid their deductible. Correct Answer The HMO reimburses the provider a predetermined fee per client per month based on the client’s age and sex. The reimbursement mechanism called capitation that some HMOs use is one in which the HMO reimburses the provider a set fee per client per month based on the client's age and sex. HMOs are prepaid, comprehensive systems of health benefits that combine both financing and delivery of services to subscribers. They may pay providers on a capitated or fee-for-service basis. https://www.coursehero.com/file/63618854/Quiz-1docx/ Question 7 1 / 1 pts individuals who did not have breast cancer. What is the specificity of the screening test? 40%. 60%. 20%. 80%. [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 08, 2021
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Apr 08, 2021
Downloads
0
Views
71


.png)
.png)


.png)
.png)
.png)
.png)

.png)

.png)
.png)

