*NURSING > CASE STUDY > Clinical Case Study NUR256. GI Bleed/Hypovolemic Shock RAPID Reasoning (All)
Clinical Case Study NUR256. GI Bleed/Hypovolemic Shock RAPID Reasoning
Document Content and Description Below
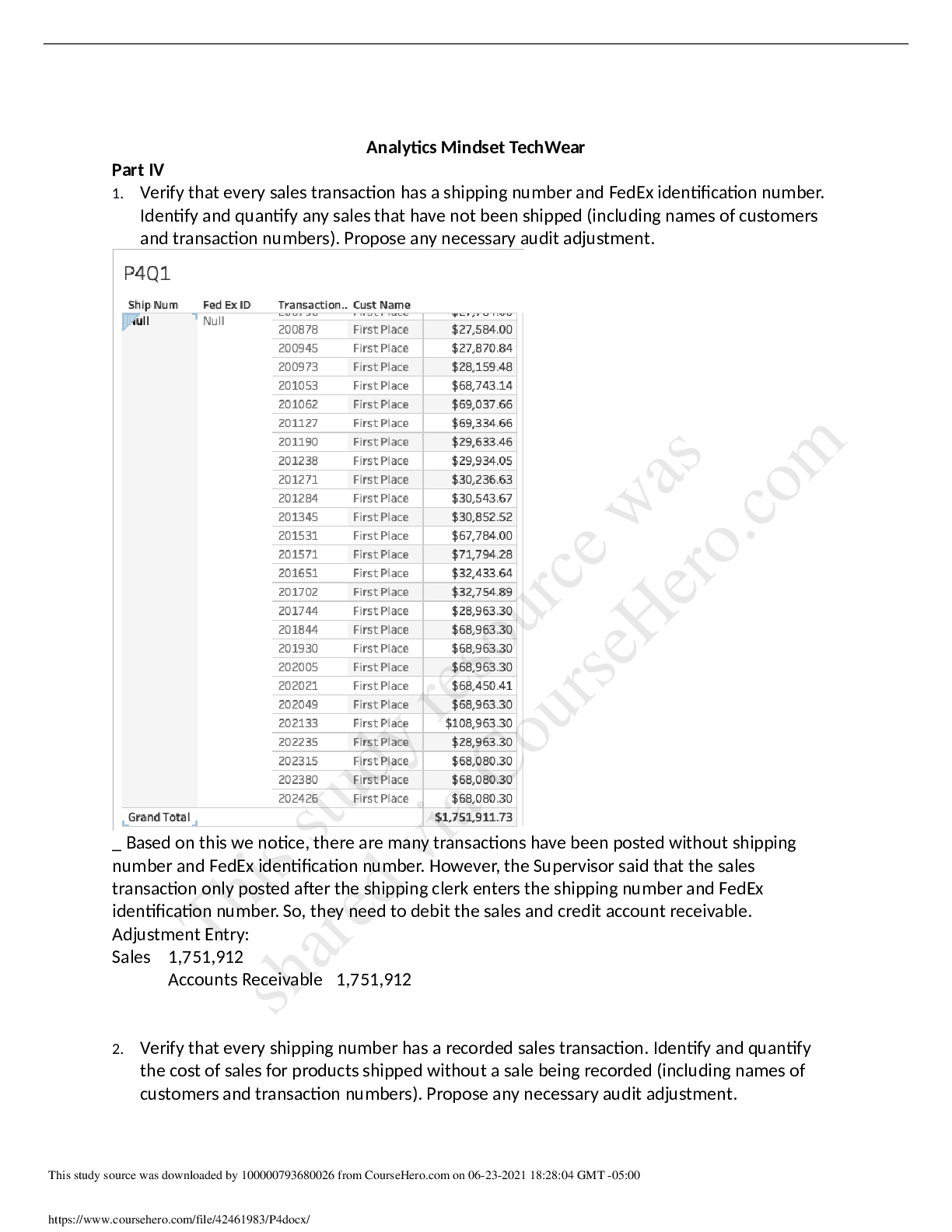
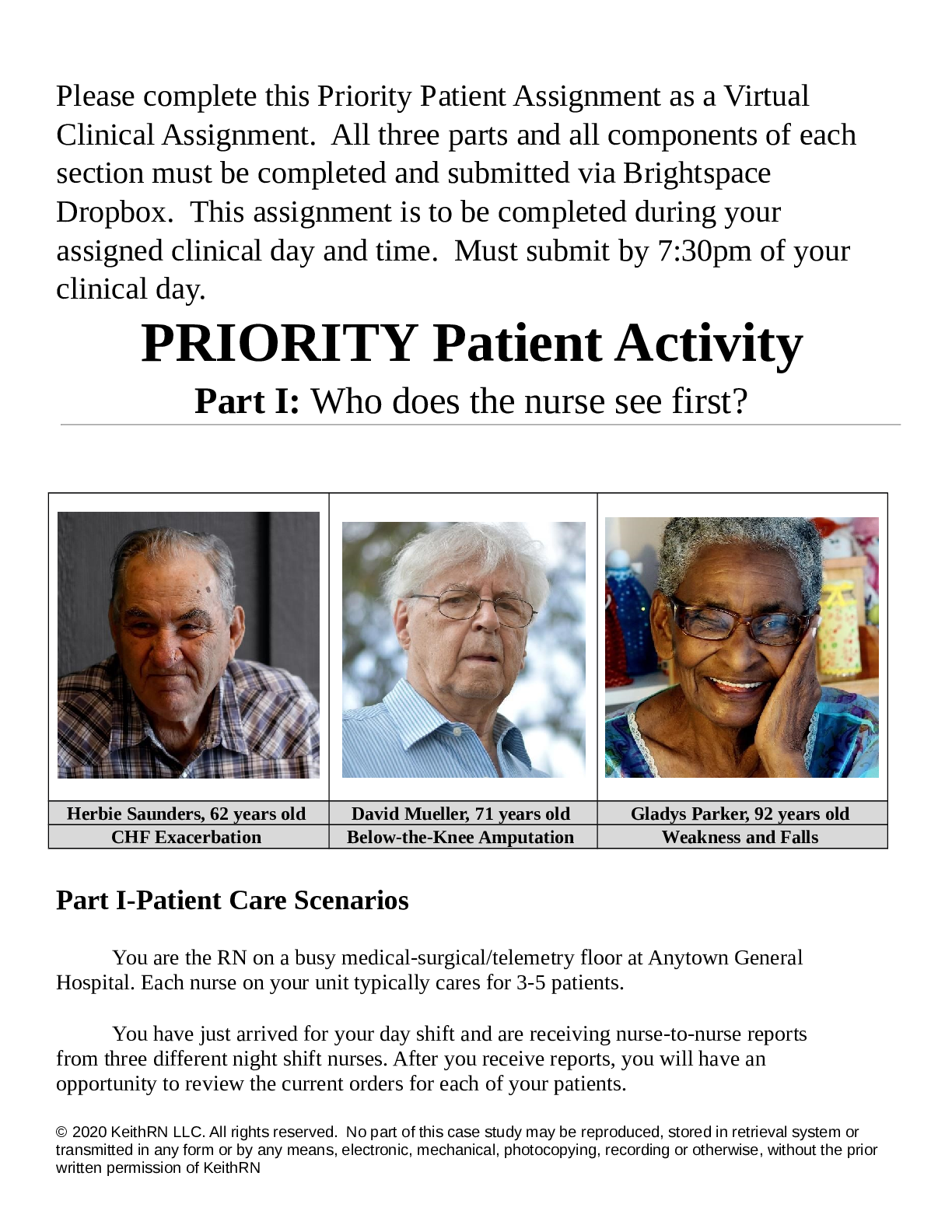
GI Bleed/Hypovolemic Shock RAPID Reasoning History of Present Problem: Jim Olson is a 45-year-old male with a history of cirrhosis and ETOH abuse who has not had any medical care the last ten ye... ars. He began vomiting large amounts of bright red blood when he woke up this morning. He was found on the floor of the bathroom by Sheila, his girlfriend, when he became lightheaded and fell on the floor and was too weak to get up. Sheila called 911. Paramedics report that there was a large dark red/black stool in the toilet. They were able to get an 18-gauge IV in the right antecubital vein, and Jim received 500 mL of 0.9% NS. His initial BP was 80/40 at the scene, and his most recent BP is 82/44 with a current heart rate of 128, sinus tachycardia. Personal/Social History: Jim recently lost his job as a construction laborer and was divorced six months ago. His ex-wife has full custody of his two children. Jim’s girlfriend states that he has been more depressed lately and has been drinking more heavily since his divorce. He takes ibuprofen daily for chronic back pain. What data from the history is important and RELEVANT; therefore, it has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: History of cirrhosis, ETOH abuse, hasn’t received medical care in 10 years, large dark red/black stool, vomiting red blood, recent BP: 82/44, sinus tachycardia According to Nursing Central, 21% of cases of liver cirrhosis are due to alcohol abuse. Jim has been dealing with alcohol abuse, so it is probably what led to his history of cirrhosis and since he has not received medical care in 10 years, his drinking could have been severely affecting his liver without the patient knowing. A sign of cirrhosis includes “bleeding from esophageal varices” (Sommers, 2019) which can be an indication as to why he was vomiting blood and why his stool is reddish black. Both the hypotension and tachycardia are due to the patient experiencing the sudden blood loss. Sommers, M. S. (2019). Davis's diseases and disorders: a nursing therapeutics manual(6th ed.). Philadelphia: F.A. Davis. RELEVANT Data from Social History: Clinical Significance: Lost his job, divorced, no custody of his kids, depression, drinking more heavily, taking ibuprofen for chronic back pain The patient’s depression due to his divorce and losing his job which led to him drinking more than his usually does could be what led to his present problem. The patient also taking ibuprofen daily while drinking could be dangerous because “high doses and long-term ibuprofen use make your stomach more likely to bleed” (2019). The signs and symptoms of gastrointestinal bleeding include both blood in a person’s vomit and stool, both symptoms the patient experienced which could indicate he is suffering from internal bleeding. Never Mix Ibuprofen and Alcohol: MD. (2019, March 6). Retrieved November 2, 2019, from https://www.ashleytreatment.org/ibuprofen-and-alcohol/. Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 98.2 F/36.8 C (oral) Provoking/Palliative: P: 138 (regular) Quality: Denies R: 28 (regular) Region/Radiation: BP: 74/30 MAP: 45 Severity: O2 sat: 95% RA Timing: What VS data is RELEVANT that must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: Pulse: 138, BP: 74/30, MAP: 45 The patient’s pulse has increased from 128 to 138 and his blood pressure has decreased from 82/44 to 74/30 which is an indication that his present problem is getting more severe. The patient’s MAP is 45 and according to Taber’s Medical Dictionary, the normal mean arterial pressure is 70-110 mmHg (Venes, 2017). In an article written by Daniel DeMers, he states “to perfuse vital organs requires the maintenance of a minimum MAP of 60 mmHg” (DeMers, 2019). If the MAP remains below the required number for too long, the patient can experience either ischemia or even infarction, so MAP must be regulated so the organs can continue to be sufficiently perfused. Venes, D. (2017). Taber’s cyclopedic medical dictionary(23rd ed.). Philadelphia: F.A. Davis Company. DeMers, D. (2019, February 24). Physiology, Mean Arterial Pressure. Retrieved November 2, 2019, from https://www.ncbi.nlm.nih.gov/books/NBK538226/. Current Assessment: GENERAL APPEARANCE: Lethargic, body tense, appears uncomfortable but denies pain RESP: Breath sounds clear with equal aeration bilaterally ant/post, non-labored respiratory effort CARDIAC: Pale, extremities cool, no edema, heart sounds regular with no abnormal beats, pulses weak, equal to palpation at radial/pedal/post-tibial landmarks, 1-2 second capillary refill NEURO: Alert & oriented to person, place, time, and situation (x4), whispers responses GI: Abdomen flat, soft/non-tender, bowel sounds audible per auscultation in all four quadrants, feels nauseated GU: No urine output present GI: Abdomen flat, soft/non-tender, bowel sounds audible per auscultation in all four quadrants, feels nauseated GU: No urine output present SKIN: Skin integrity intact, skin turgor elastic, no tenting present What assessment data is RELEVANT that must be recognized as clinically significant? Cardiac Telemetry Strip: Interpretation: Regular/Irregular: Regular P wave present? Yes PR: 0.16 QRS: 0.12 QT: 0.32 Interpretation: Patient is experiencing sinus tachycardia showing a heart rate of 140. Clinical Significance: Through the EKG strip, you can see that the P wave is present but the time between atrial depolarization and ventricular repolarization is short meaning the heart is contracting rapidly, leading to sinus tachycardia. Lab Results: Complete Blood Count (CBC) Current High/Low/WNL? WBC (4.5-11.0 mm3) 8.5 WNL Neutrophil % (42-72) 75 High Hgb (12-16 g/dL) 5.5 Low Platelets(150-450 x 103/µl) 68 Low What lab results are RELEVANT that must be recognized as clinically significant to the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: hemoglobin, platelets In the clinical handbook for medical-surgical nursing it states, “In hypovolemic shock resulting from hemorrhage, the hemoglobin… concentrations are lower than normal” (LeMone, Burke, Bauldoff & Guburd, 2016). Both the hemoglobin and platelets would be low because the patient has been losing blood both through stool and vomit which is why his levels are significantly low. LeMone, P. M., Burke, K. M., Bauldoff, G. M., & Gubrud, P. M. (2016). Clinical handbook for medical-surgical nursing: clinical reasoning in patient care(7th ed.). Boston: Pearson. Misc. Labs Current High/Low/WNL? Magnesium (1.6-2.0 mEq/L) 1.3 Low Lactate (0.5-2.2 mmol/L) 3.4 High Coags: PT/INR (0.9-1.1 nmol/L) 8.5 High What lab results are RELEVANT that must be recognized as clinically significant to the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: Magnesium, Lactate, PT/INR His magnesium is low due to electrolyte imbalance from him vomiting blood and his bloody bowel movement, his lactate is high and is indicative of the severity of acidosis, and his PT/INR is elevated due to his body trying to clot faster as an attempt to stop the bleeding. Liver Function Test (LFT): Current High/Low/WNL? Albumin (3.5-5.5 g/dL) 2.1 Low Total Bilirubin (0.1-1.0 mg/dL) 3.5 High Alkaline Phosphatase Male: 38-126 U/I Female: 7-230 U/I 152 High ALT (8-20 U/L) 68 High AST (8-20 U/L) 75 High What lab results are RELEVANT that must be recognized as clinically significant to the nurse? RELEVANT Lab(s): Clinical Significance: Albumin, Total Bilirubin, Alkaline Phosphate, ALT, AST The liver enzymes, AST and ALT, are elevated because according to Nursing Central, “Liver cellular dysfunction leads to accumulation of enzymes” (Sommers, 2019). Albumin is decreased, total bilirubin is increased, evidenced by liver damage, and alkaline phosphate is increased, related to the release of alkaline phosphate from damaged liver cells, due to cirrhosis, which is significant because the patient has a history of cirrhosis, but has also recently been drinking heavily which has possibly increased his liver damage. Sommers, M. S. (2019). Davis's diseases and disorders: a nursing therapeutics manual(6th ed.). Philadelphia: F.A. Davis. Clinical Reasoning Begins…. 1. What is the primary problem your patient is most likely presenting? (Management of Care/Physiologic Adaptation) I believe that the primary problem my patient is experiencing is hypovolemic shock. According to Nursing Central, hypovolemic shock “results from a decreased effective circulating volume of water, plasma, or whole blood” (Sommers, 2019). A common cause of hemorrhagic shock is sudden external blood loss resulting from severe gastrointestinal bleeding, which evidenced by the red stool, may be what the patient is experiencing. 2. What is the underlying cause/pathophysiology of this primary problem? (Management of Care/Physiologic Adaptation) According to Nursing Central, “active bleeding or rupture of organs can quickly result in hypovolemia [or]…other sources of hypovolemia include decreases in fluid intake(dehydration) and increases in fluid output(vomiting…)” (Sommers, 2019). The patient could possibly be experiencing GI bleeding due to the red stool which could have caused the hypovolemia or because of his increased intake of alcohol which could lead to dehydration and him vomiting blood, hypovolemia could have occurred. With hypovolemic shock, when the fluid loss is greater than 30%, a decrease in venous return occurs which decreases cardiac output, which in turn decreases perfusion to vital organs resulting in the symptoms associated with shock. (Sommers, 2019). The patient seems to be experiencing stage III hypovolemic shock with some manifestations of stage IV, which is accompanied by tachycardia, weak pulses, significant hypotension, cold skin, and anuria (Sommers, 2019). Collaborative Care: Medical Management (Pharmacologic and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: • Establish two large bore IVs • 0.9% NS 1000 mL bolus • Ondansetron 4 mg IV push • Octreotide 50 mcg IV push Octreotide 50 mcg/hour IV gtt • Phytonadione (vitamin K) 2 mg in 50 mL D5W IVPB • Fresh frozen plasma (FFP) 4 units IV • Packed red blood cells (PRBC) 2 units Type O Neg • Type and cross match. Have four units PRBC available • Fluid resuscitation is most efficient through a large bore IV • To provide adequate cardiac output to perfuse the tissues • Prevention and treatment of nausea and vomiting • Increases absorption of fluid and electrolytes from the GI tract and increases transit time • Prevention and treatment of hypoprothrombinemia • To replace missing coagulation factors • Needed to restore the oxygen- carrying capacity of the blood of the patient • In case the two units of PRBC is not enough to restore the patient’s • The organs are perfused more rapidly • The organs are sufficiently perfused increasing the blood pressure and decreasing the heart rate • Decreased incidence and severity of nausea and vomiting • Control of severe flushing and diarrhea • Prevention of bleeding due to hypoprothrombinemia • Improvement in PT/INR • An increase in hemoglobin of 1g/dL • An increase in hemoglobin red blood cell loss Collaborative Care: Nursing 3. Review the following skills and essential knowledge that the nurse will use in this scenario to save Jim’s life: (Management of Care) Skill: What Does the Nurse Need to KNOW to be Safe in Practice: IV Insertion The nurse must choose the appropriate gauge IV catheter, must use aseptic technique, must cleanse the site circularly, must insert the needle bevel side up, must maintain sterility of the needle and hub, if unsuccessful, must obtain new devices Administration of fresh frozen plasma (FFP) Must be thawed in a 37-degree Celsius water bath for approximately 30 minutes, should be ABO compatible, there is a risk of transmitting bloodborne pathogens Administration of PRBC’s Red cells require compatibility testing, risk of transmitting bloodborne pathogens, should be warmed to prevent hypothermia, contains little or no clotting factors 4. What nursing priority(ies) will guide your plan of care? (if more than one – list in order of PRIORITY) (Management of Care) The most important nursing priority for a patient in shock is “maintaining cardiovascular and respiratory function to maintain oxygenation and perfusion”(LeMone, Burke, Bauldoff & Guburd, 2016). 5. What interventions will you initiate based on this priority? (Management of care) Nursing Interventions: Rationale: Expected Outcome: 1. Assess and monitor cardiovascular function via blood pressure, heart rate and rhythm, pulse oximetry, peripheral pulses, and hemodynamic monitoring 2. Measure and record intake and output hourly 3. Monitor skin color, temperature, turgor, and moisture 4. Monitor body temperature 1. A baseline assessment is necessary to establish the stage of shock 2. Decrease in circulating blood volume can cause renal failure, urinary output of less than 30 mL per hour indicates reduced renal blood flow 3. Decreased tissue perfusion is evidenced when the skin becomes pale, cool, and moist 4. An increased body temperature increases metabolic demands and increases myocardial oxygen demand placing the patient at risk for hypoperfusion 1. With treatment, cardiovascular function will remain stable and within defined limits 2. Patient’s circulating blood volume and urinary output will remain at normal levels 3. To identify decreased hemoglobin concentration in order to prevent cyanosis 4. Decrease the temperature when necessary to decrease risk of hypoperfusion 6. What body system(s) will you most thoroughly assess based on the primary/priority concern and what specific assessments need to be performed by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) The circulatory system, respiratory system, integumentary system, and nervous system. The nurse will be monitoring fluid status such as daily weight, fluid intake by all routes, measuring fluid loss. The nurse will also be assessing fluid balance, hemodynamic values, and vital signs (LeMone, Burke, Bauldoff & Guburd, 2016). 7. What is the worst possible/most likely complication to anticipate? (Reduction of Risk Potential/Physiologic Adaptation) If hypovolemic shock is left uncorrected, “multiple organ failure and death” may occur (Sommers, 2019). 8. What nursing assessments will identify this complication EARLY if it develops? (Reduction of Risk Potential/Physiologic Adaptation) Hemodynamic monitoring, can be used to evaluate the patient’s response to therapy, vital signs, the worse the shock progresses, the worse the vital signs will become, monitoring arterial blood gases, insufficient oxygen perfusion will lead to metabolic acidosis, and fluid balance monitoring, urine output is an indicator of renal perfusion (LeMone, Burke, Bauldoff & Guburd, 2016). 9. What psychosocial needs will this patient and family likely have that will need to be addressed? (Psychosocial Integrity/Basic Care and Comfort) The patient and or the family may feel anxiety, fear, and powerlessness (LeMone, Burke, Bauldoff & Guburd, 2016). 10. How can the nurse address these psychosocial needs? (Psychosocial Integrity/Basic Care and Comfort) As a nurse, they can assess the cause of the anxiety and reduce the stimuli causing the anxiety to calm the patient down and facilitate rest, can administer pain medications and implement nonpharmacologic comfort measures, provide interventions such as maintaining a clean environment, eliminate all nonessential activities, using touch to provide support to increase comfort and reduce restlessness, and provide support for the patient and the family such as encouraging the expression of feelings and concerns, provide time, space, and privacy for family members, and proving information about the current setting to both the patient and family (LeMone, Burke, Bauldoff & Guburd, 2016). Caring & the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? (Psychosocial Integrity) The patient is most likely going to be frightened and feeling anxious. 2. What can I do to engage myself with this patient’s experience, and show that he/she matters to me as a person? (Psychosocial Integrity) As the nurse, I can make sure to explain to the patient all the procedures in order to provide reassurance, I can touch the patient’s hand or arm to provide reassurance as well, explain the treatment alternatives and keep the patient and family updated with the patient’s response to the therapies, explain and answer the patient’s questions about the risks involved with blood component therapy (Sommers, 2019). I can also acknowledge the beliefs, values, and expectations of the patient and family, remain with the patient during procedures, maintain a clean environment, speak slowly and calmly, allow family members access to the patient when feasible, and provide anticipatory guidance to prepare for recovery or death and to support realistic hope (LeMone, Burke, Bauldoff & Guburd, 2016). Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention at the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? I learned a lot from this scenario. I learned how to take the patient’s history in account when diagnosing their current problem, and how to assess the lab results in order to connect them to the patient’s diagnosis and once the diagnosis is found, which interventions are best to be used, and what the interventions mean and how they can positively affect the patient. I also realized how important it is to include the patient in the care and to make sure they understand why each procedure is being done, and to make sure as a nurse, we are there to support and care for the patient not only medically, but emotionally as well. Overall, I learned how important each intervention is to ensure patient recovery and prevent complications, while taking care of your patient’s needs. 2. How can I use what has been learned from this scenario to improve patient care in the future? I believe I can use what I learned to make sure I perform the correct nursing interventions for the patient, but I also care for the patient emotionally such as making sure they are comfortable by reducing their anxiety by being by their side through their entire stay, answering any questions they have regarding their care, physically maintaining their comfort such as integrating touch to provide reassurance or grouping nursing activities to increase rest periods, etc. This scenario has just opened my eyes to the many different ways I can address my patient’s needs through management of care and comfort. . References DeMers, D. (2019, February 24). Physiology, Mean Arterial Pressure. Retrieved November 2, 2019, from https://www.ncbi.nlm.nih.gov/books/NBK538226/. LeMone, P. M., Burke, K. M., Bauldoff, G. M., & Gubrud, P. M. (2016). Clinical handbook for medical-surgical nursing: clinical reasoning in patient care(7th ed.). Boston: Pearson. Never Mix Ibuprofen and Alcohol: MD. (2019, March 6). Retrieved November 2, 2019, from https://www.ashleytreatment.org/ibuprofen-and-alcohol/. Sommers, M. S. (2019). Davis's diseases and disorders: a nursing therapeutics manual (6th ed.). Philadelphia: F.A. Davis. Venes, D. (2017). Taber’s cyclopedic medical dictionary (23rd ed.). Philadelphia: F.A. Davis Company [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2021
Downloads
0
Views
57