*NURSING > DISCUSSION POST > NR 601 Week 3 – Psychiatric Disorders and Screening Discussions - With Well Explained Answers ( Do (All)
NR 601 Week 3 – Psychiatric Disorders and Screening Discussions - With Well Explained Answers ( Download to Score an A)
Document Content and Description Below
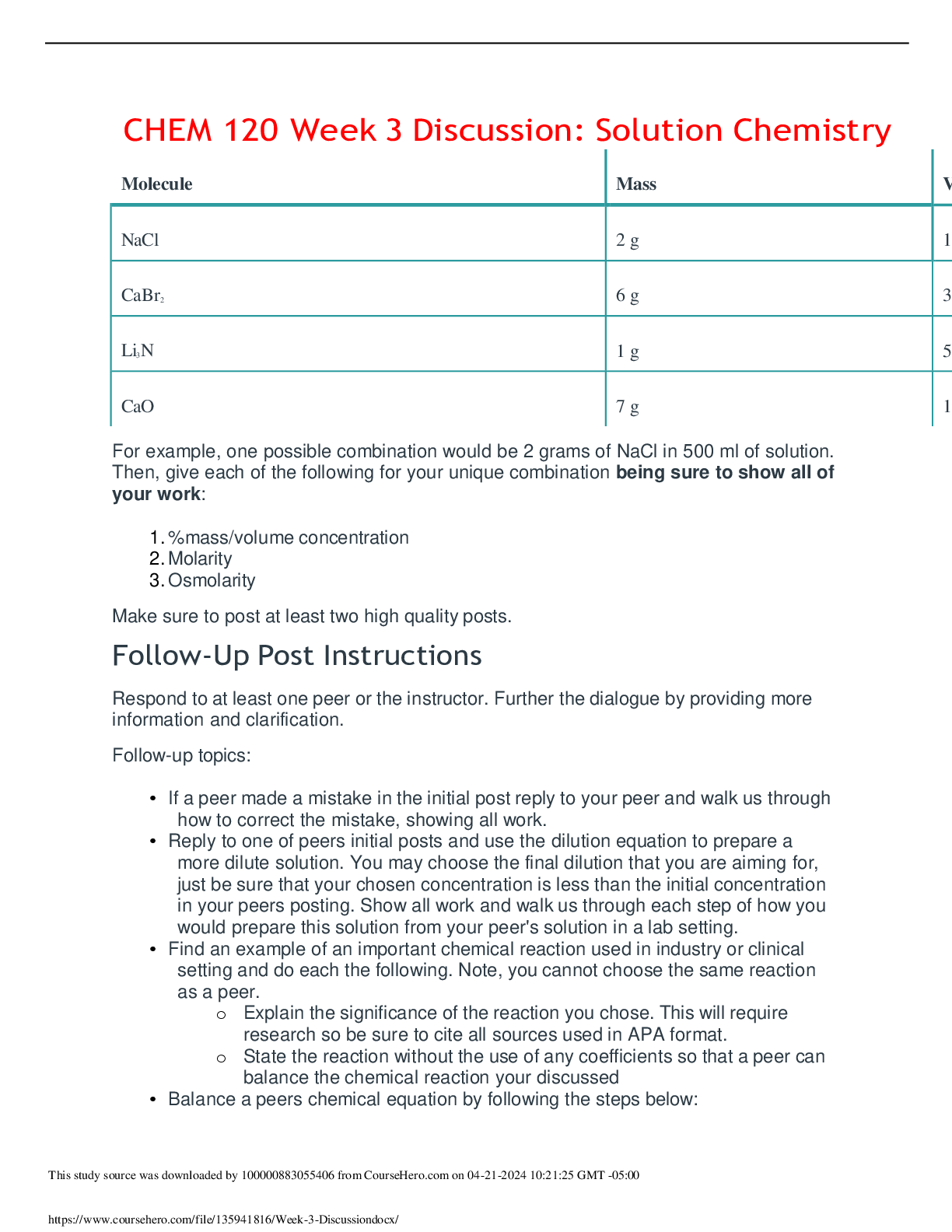
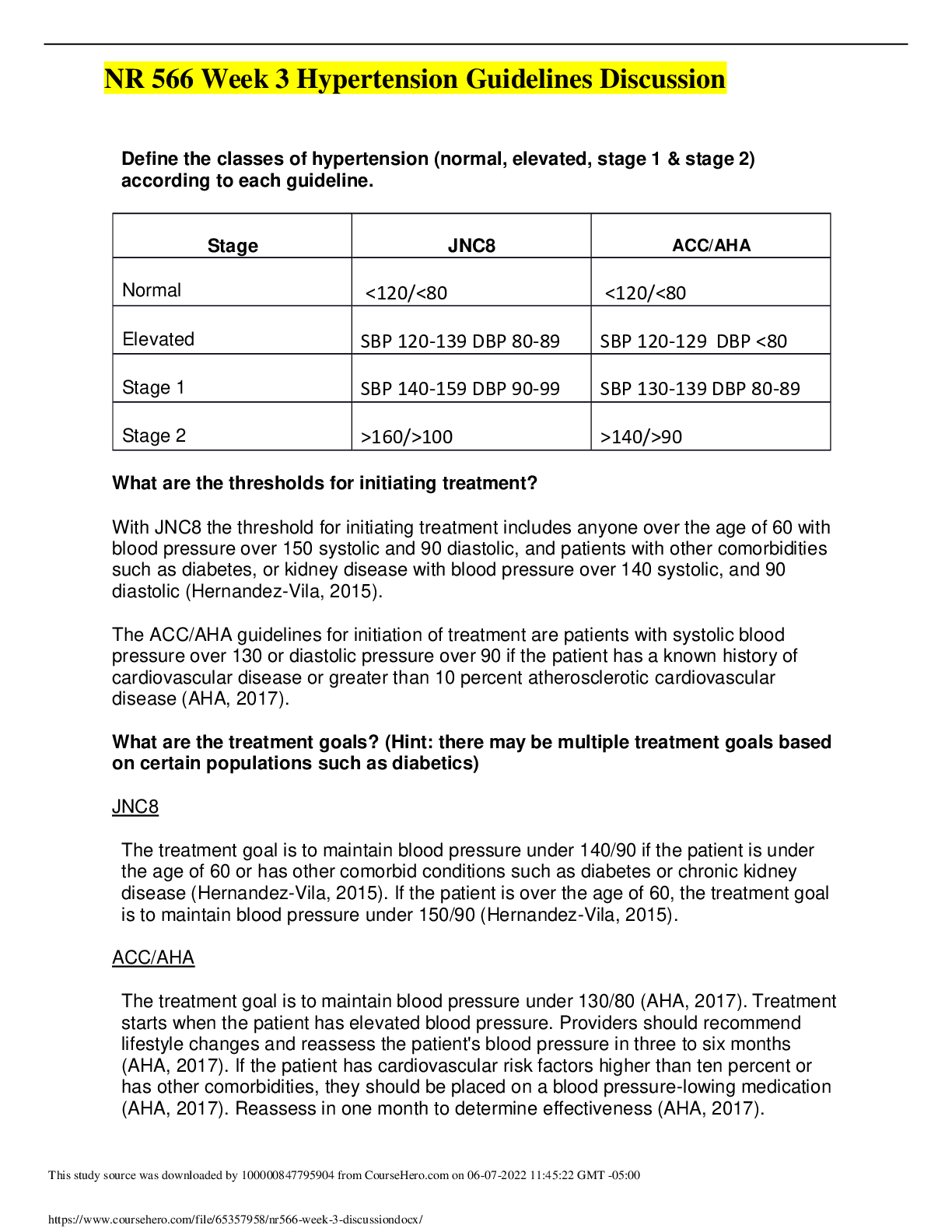
Research screening tools for depression and anxiety. • Choose one screening tool for depression and one screening tool for anxiety that you feel are appropriate to screen KB. • Explain why you c... hose that particular tool for KB. • Score KB based on the information provided (not all data may be provided). Include what questions could be scored, and your chosen score. Assume that any question topics not mentioned are not a concern at this time. The screening tool chosen for depression is the Patient Health Questionnaire-9 (PHQ-9). It is estimated that 14% of patients in the primary care setting have depression; and it is frequently not diagnosed because of the lack of utilization of standardized screening tools (Hirschtritt & Kroenke, 2017). According to Hirschtritt and Kroenke (2017), when standardized screening tools are not utilized, primary care providers only recognize depression in an estimated 47% of patients. The PHQ-9 is a self-report questionnaire based on symptoms experienced over the past 2 weeks that comprises of 9 items, which are then added together to result a score ranging from 0 through 27 (Hirschtritt & Kroenke, 2017). According to Hirschtritt & Kroenke (2017), a total score ≥10 has an estimated specificity of 85.3% for major depressive disorder. There are several benefits to the PHQ-9 screening tool which include: self-report format, quick scoring and interpretation, available in multiple languages, and can be administered remotely such as in cases where telehealth is utilized (Hirschtritt & Kroenke, 2017). I chose the PHQ-9 screening tool for depression because it is geared towards the general adult population, and is frequently utilized in the primary care setting. I find this screening tool very effective and have used it many times thus far in my clinical rotations, as well as in the emergency department where I currently work. PHQ-9: Over the last 2 weeks, how often have you been bothered by any of the following problems? (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day) 1. Little interest or pleasure in doing things = 3 2. Feeling down, depressed, or hopeless = 3 3. Trouble falling or staying asleep, or sleeping too much = 1 4. Feeling tired or having little energy = 3 5. Poor appetite or overeating = 3 6. Feeling bad about yourself or you are a failure or have let yourself or your family down = 2 7. Trouble concentrating on things, such as reading the newspaper or watching television = 2 8. Moving or speaking so slowly that other people could have noticed? Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual = Not Known 9. Thoughts that you would be better off dead or of hurting yourself in some way = Not Known Total score = 17 (Hirschtritt & Kroenke, 2017). The scoring ranges for symptoms are as followed: mild depressive symptoms (5-9), moderate (10-14), moderately severe (15-19), and severe depressive symptoms (≥20). Two items were excluded from the questionnaire because they were not of concern at this time. Based on the total score of 17, it can be determined that KB has moderately severe depressive symptoms (Hirschtritt & Kroenke, 2017). Patients who score a 10 or higher on the PHQ-9 screening tool should have a more thorough examination by either a primary care provider and/or a psychologist or psychiatrist before starting treatment (Hirschtritt & Kroenke, 2017). The screening tool selected for anxiety is the Primary Care PTSD Screen (PC-PTSD). The PC- PTSD is a commonly used, 4-item self-report questionnaire that uses a score of three as the screening threshold (Kearney & Simpson, 2015). A positive screening result does not mean that a patient has post-traumatic stress disorder (PTSD), but it does indicate that they are at risk (Kearney & Simpson, 2015; Friedman, 2018). This screening tool is reliable and practical for use in the primary care setting because it can assist primary care providers in identifying anxiety related to traumatic events (Kearney & Simpson, 2015; Friedman, 2018). The PC-PTSD Screen was chosen based on the subjective information provided by the patient. My initial interpretation and assessment of this patient was generalized anxiety disorder (GAD), therefore I was going to use the GAD-7. However, the more I examined the SOAP note, I came to the conclusion that the patient appears to be experiencing symptoms more related to PTSD. PC-PTSD Screen: Instructions: In your life, have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month, you: 1. Have had nightmares about it or thought about it when you did not want to? Not Known 2. Tried hard not to think about it or went out of your way to avoid situations that reminded you of it? YES 3. Were constantly on guard, watchful, or easily startled? Not Known 4. Felt numb or detached from others, activities, or your surroundings? YES (Friedman, 2018). Due to limited information provided in the SOAP note, two of the questions were excluded from the survey. However, KB’s screen was positive due to answering yes to the questions that were applicable. If a patient answers yes to any of the three out of four questions from the PC-PTSD Screen tool, then it is considered a positive screen. At this point, a positive screen should be further evaluated by a mental health professional (Friedman, 2018). Identify your next step for evaluation and treatment for KB. Include any necessary physical medicine evaluation. When screening is positive for possible depression, the diagnosis should be established by utilizing the Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-5), which provides diagnostic measures for major depressive disorder (MDD) (Maurer, Raymond, & Davis, 2018). All patients must be carefully assessed for underlying medical conditions by performing a history and physical examination, because many medical conditions and medications can cause symptoms of depression (Maurer et al., 2018). According to Maurer et al. (2018), obtaining basic laboratory studies, especially in older adult patients, is necessary in order to rule out any medical conditions that may be mimicking symptoms of depression. Ruling out a thyroid issue or anemia should be considered by obtaining a thyroid-stimulating hormone level and a complete blood count as these conditions can cause fatigue, depression, or weight and appetite changes (Maurer et al., 2018). Lastly, serum electrolytes should be evaluated with a basic metabolic panel because an imbalance in sodium levels may lead to confusion and early delirium, which may also mimic depression (Maurer et al., 2018). The diagnostic criteria for PTSD provided by the DSM-5 include: avoidance of people, places, or things that are constant reminders of a traumatic event, experience with death of a close family member, occurrence of intrusive memories of the traumatic event, and negative changes in cognition and mood related to the traumatic event (Greene, Neria, & Gross, 2016). KB fits the criteria for diagnosis of PTSD; therefore, further evaluation and treatment is necessary to improve the outcome of this patient. According to Greene et al (2016), management of PTSD in the primary care setting can be coordinated by either the primary care provider or a primary care nurse through patient education, encouraging and/or enrolling a patient in a community PTSD group, providing prescription medications, and providing cognitive behavioral therapy. Psychoeducation and pharmacotherapy are first-line treatment options for the management of PTSD (Bernardy & Friedman, 2015). What medication, if any, would you recommend for treatment? Provide the rationale. This should include the medication class, mechanism of action of the medication and why this medication is appropriate for KB. Include initial prescribing information and education to include side effects and when KB should notice efficacy. Second-generation antidepressants are equally effective in treating depression (Kovich & DeJong, 2015). Therefore, the medication I recommend for treatment is sertraline (Zoloft). Sertraline is a selective serotonin reuptake inhibitor (SSRI), which works by increasing the amount of serotonin by blocking the presynaptic serotonin reuptake pump (Bernardy & Friedman, 2015). Guidelines recommend SSRIs as effective first-line options for the treatment of depression; and clinical trials have also shown adequate results in improving symptoms of PTSD (Kovich & DeJong, 2015; Bernardy & Friedman, 2015). As a result of clinical trials, sertraline received U.S. Food and Drug Administration (FDA) approval for PTSD. Sertraline is generally well tolerated and is recommended as first-line therapy in several treatment guidelines (Bernardy & Friedman, 2015). Another reason why sertraline is appropriate for KB is because second- generation antidepressants have similar efficacy for treating anxiety in patients who have both major depressive disorder and anxiety symptoms (Kovich & DeJong, 2015). Clinical guidelines recommend selecting among second-generation antidepressants based on cost, adverse effects, and patient preference; and for patients with accompanying anxiety, there is no definitive data supporting the use of one medication over another. (Kovich & DeJong, 2015). Rx: Sertraline 25 mg tablets Sig: Take one tablet by mouth once daily. Disp: #30 (Thirty) Refill: 0 Sertraline can be increased at 1-week intervals to a max of 200 mg/day in order to reach the desired therapeutic outcome (Hollier, 2018). SSRIs have a better side effect profile than other classes of antidepressants, and side effects associated with SSRIs are seen with the first few doses, but resolve in approximately 7 days (Kovich & DeJong, 2015). The most common side effects reported include: diarrhea, dizziness, dry mouth, fatigue, headache, sexual dysfunction, sweating, tremor, and weight gain; with nausea and vomiting being the most common reasons for stopping the medication (Kovich & DeJong, 2015). Sertraline has a higher incidence of diarrhea than most other second-generation antidepressants (Kovich & DeJong, 2015). SSRIs may increase the risk of suicidal thoughts and behaviors in patients with MDD, therefore, monitoring of the patient closely during the initial months of therapy is pertinent (Hollier, 2018). Many antidepressants can cause sedation; therefore, patients should be instructed to avoid activities that require alertness or coordination until they know how the medication will affect them (Hollier, 2018). Additionally, patients should be instructed to avoid alcohol and sedatives when taking antidepressants, notify the primary care provider of any adverse effects, and to not stop taking medication abruptly as this may cause a withdrawal syndrome (Hollier, 2018). It may take 3-6 weeks before benefits are seen (Hollier, 2018). In order to monitor patients closely for worsening depressive symptoms, suicidal thoughts, and unusual behaviors; patients should be seen by the primary care provider within 2 weeks of initiating or changing the dose of an antidepressant (Hollier, 2018). If the medication works as expected, when should KB expect to start feeling better? As stated previously, typically patients begin to benefit from an SSRI in 3-6 weeks, but full effect may be delayed for 4 weeks or longer (Hollier, 2018). Clinical guidelines recommend that treatment continue for 4-18 months with the first episode of major depression (Hollier, 2018). References Bernardy, N., & Friedman, M. (2015). Psychopharmacological strategies in the management of posttraumatic stress disorder (PTSD): What have we learned? Current Psychiatry Reports, 17(4), 1-10. doi:10.1007/s11920-015-0564-2 Friedman, M. J. (2018). Posttraumatic stress disorder in primary care practice. JAMA Internal Medicine, 178(11), 1445–1446. doi:10.1001/jamainternmed.2018.3108 Greene, T., Neria, Y., & Gross, R. (2016). Prevalence, detection and correlates of PTSD in the primary care setting: A systematic review. Journal of Clinical Psychology in Medical Settings, 23(2), 160–180. Hirschtritt, M. E., & Kroenke, K. (2017). Screening for depression. JAMA: Journal of the American Medical Association, 318(8), 745-746. Hollier, A. (2018). Clinical guidelines in primary care (3rd ed.). Advanced Practice Education Associates. Kearney, D. J., & Simpson, T. L. (2015). Broadening the approach to posttraumatic stress disorder and the consequences of trauma. Journal of the American Medical Association, 314(5), 453-455. Kovich, H., & DeJong, A. (2015). Common questions about the pharmacologic management of depression in adults. American Family Physician, 92(2), 94–100. Maurer, D. M., Raymond, T. J., & Davis, B. N. (2018). Depression: Screening and diagnosis. American Family Physician, 98(8), 508–515. [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 06, 2023
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Feb 06, 2023
Downloads
0
Views
68


 (1).png)
.png)
.png)
.png)

.png)
.png)