*NURSING > CASE STUDY > (answered) Assessment & Reasoning GI System Peggy Scott, 48 years old (latest complete solution) (All)
(answered) Assessment & Reasoning GI System Peggy Scott, 48 years old (latest complete solution)
Document Content and Description Below
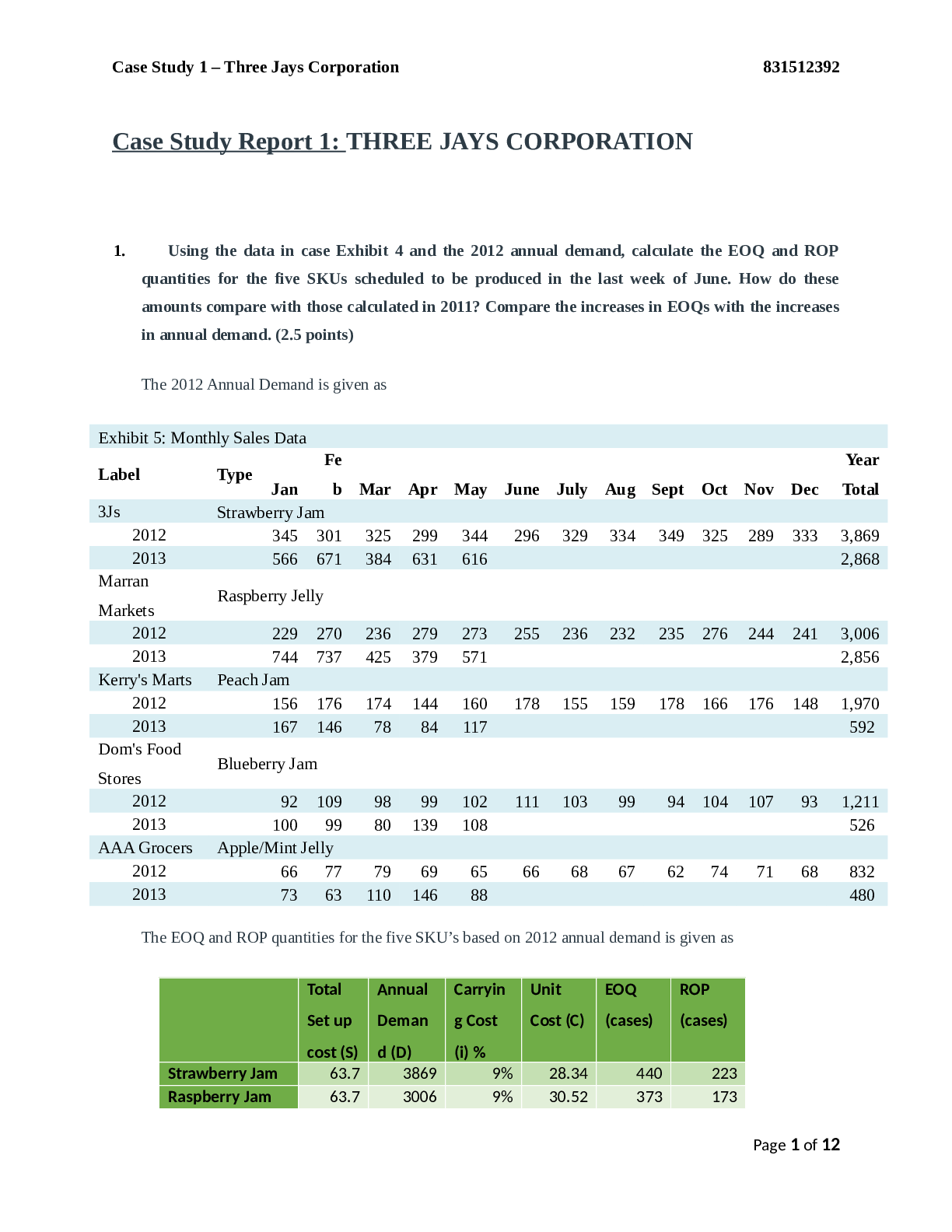
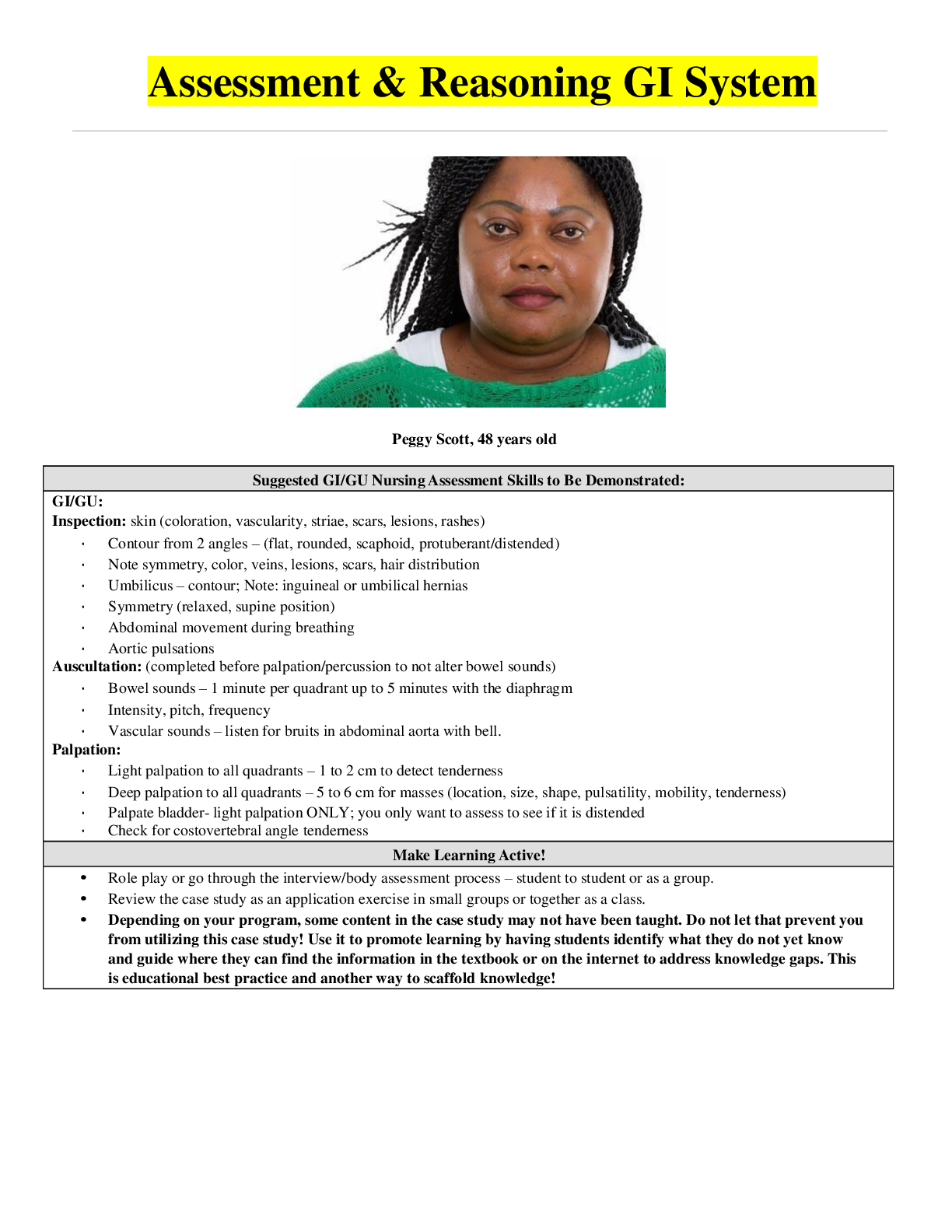
Peggy Scott, 48 years old Suggested GI/GU Nursing Assessment Skills to Be Demonstrated: GI/GU: Inspection: skin (coloration, vascularity, striae, scars, lesions, rashes) Contour from 2 angles ... – (flat, rounded, scaphoid, protuberant/distended) Note symmetry, color, veins, lesions, scars, hair distribution Umbilicus – contour; Note: inguineal or umbilical hernias Symmetry (relaxed, supine position) Abdominal movement during breathing Aortic pulsations Auscultation: (completed before palpation/percussion to not alter bowel sounds) Bowel sounds – 1 minute per quadrant up to 5 minutes with the diaphragm Intensity, pitch, frequency Vascular sounds – listen for bruits in abdominal aorta with bell. Palpation: Light palpation to all quadrants – 1 to 2 cm to detect tenderness Deep palpation to all quadrants – 5 to 6 cm for masses (location, size, shape, pulsatility, mobility, tenderness) Palpate bladder- light palpation ONLY; you only want to assess to see if it is distended Check for costovertebral angle tenderness Make Learning Active! Role play or go through the interview/body assessment process – student to student or as a group. Review the case study as an application exercise in small groups or together as a class. Depending on your program, some content in the case study may not have been taught. Do not let that prevent you from utilizing this case study! Use it to promote learning by having students identify what they do not yet know and guide where they can find the information in the textbook or on the internet to address knowledge gaps. This is educational best practice and another way to scaffold knowledge! Copyright © 2019 Keith Rischer, d/b/a KeithRN. All Rights reserved. Present Problem: Peggy Scott is a 48-year old African American woman who came to the emergency department because she is having severe abdominal pain radiating to the back that started 24 hours ago but has become progressively worse in the last couple of hours. She is now nauseated and states that she has “puked small amounts of green liquid” five times in the last four hours. She had two loose stools today that were dark brown or black in color. Peggy has struggled with ETOH use/abuse most of her adult life but has been sober the past six months. She begins to cry and tells the nurse that this week was the one-year anniversary of her only son’s death in an automobile accident. She reports that she has been drinking one liter of vodka daily the past week. What data from the present problem are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: Severe abdominal pain radiating to the back. Began 24 hours ago and is worsening. Nauseous Puked green liquid 5x. 2 loose stool dark brown/black Crying about sons death - Constant pain in your upper belly that radiates to your back. This is a symptom of pancreatitis. -Nausea from alcohol intake which increases the production of stomach acids and delays the stomach from emptying. Also signs of pancreatitis. -Green/yellow vomit could indicate bile produced by the gallbladder. -Brown stool is normal but black would indicate bleeding in the GI tract iron/ something she ate What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect.) PMH: Home Meds: Pharm. Class: Mechanism of Action (own words): Depression Low back pain Pancreatitis (no current meds) ETOH abuse (no current meds) Ibuprofen 600 mg PO three times daily PRN Citalopram 40 mg PO daily NSAID nonsteroidal anti-inflammatory drugs SSRI serotoninreuptake inhibitors IBUPROFEN- reduces pain and inflammation in the body. Citalopram- used for depression Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment: T: 100.6 F/38.1 C (oral) Provoking/Palliative: Movement provokes, nothing relieves pain P: 98 (regular) Quality: Sharp R: 20 (regular) Region/Radiation: Epigastric area/LUQ BP: 146/94 Severity: 10/10 O2 sat: 95% room air Timing: Continuous since onset 24 hours ago What vital signs are abnormal? What is the reason (pathophysiology) for these findings? (Reduction of Risk Potential/Health Promotion and Maintenance) Abnormal VS: Clinical Significance: T: 100.6 oral temp P: 98 R: 20 BP: 146/94 -High fever likely caused due to pancreatitis -Although this is within normal limits it is borderline to tachycardia likely caused by pain level hypovolemia -Although this is technically normal it is borderline Tachypnea likely caused by current sitation, pain level -High bp could be a result of pain level and alcohol intake Current Assessment: GENERAL SURVEY: Alert, oriented, pleasant, in no acute distress, Is unkept in appearance with soiled clothing, body tense, grimacing NEUROLOGICAL: Alert & oriented to person, place, time, and situation (x4) HEENT: Head normocephalic with symmetry of all facial features. PERRLA, sclera white bilaterally, conjunctival sac pink bilaterally. Lips, tongue, and oral mucosa pink and tacky dry in appearance. RESPIRATORY: Breath sounds clear with equal aeration on inspiration and expiration in all lobes anteriorly, posteriorly, and laterally, nonlabored respiratory effort on room air. CARDIAC: Pink, warm & dry, no edema, heart sounds regular, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refill. Heart tones audible and regular, S1 and S2, noted over A-P-T-M cardiac landmarks with no abnormal beats or murmurs. No JVD noted at 30-45 degrees. ABDOMEN: Abdomen round, soft, and tender in epigastric area and LUQ to gentle palpation. Nauseated with small light bile green emesis, BS + in all four quadrants GU: Voiding without difficulty, urine dark amber INTEGUMENTARY: Skin warm, dry, intact, normal color for ethnicity. No clubbing of nails, cap refill <3 seconds, Hair soft-distribution normal for age and gender. Skin integrity intact, skin turgor elastic, no tenting present. What assessment findings are abnormal? What is the reason (pathophysiology) for these findings? (Reduction of Risk Potential/Health Promotion & Maintenance) RELEVANT Assessment Data: Clinical Significance: General survey HEENT Abdomen Soiled clothing is seen with depression and or pain for face/intoxicated Dry mouth is a side effect of depression medication. Tenderness due to pancreatitis likely due to inflammation. Radiology Reports: What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) CT: Abdomen Results: Clinical Significance: Gallbladder normal in size and appearance with no stones present in the gallbladder or common bile duct. Pancreas is moderately enlarged. Alcohol is a common cause of pancreatitis. Normal gallbladder size and appearance so this can be ruled out. Lab Results: Complete Blood Count (CBC) WBC HGB PLTs % Neuts Bands Current: 14.8 10.2 98 88 0 RELEVANT Lab(s): Clinical Significance: WBC count is high (5-10) HBG is low (F-12-16) PLT 98 (100-400) %Neuts 88 (40-60) Bands normal Indicating infection Indicates blood loss- anemia which is found with pancreatitis. Indicates thrombocytopenia which is found in pts with alcoholic pancreatitis. Indicates neutropenia caused by Basic Metabolic Panel (BMP) Na K Gluc. Creat. Current: 139 3.4 195 1.1 RELEVANT Lab(s): Clinical Significance: -Sodium normal (135-145) -K low (3.5-5 normal) -Gluc high (normal 70-110) -Creatinine (normal 0.8-1.2) normal Low K+ due to vomiting and diarrhea Hyperglycemia caused by chronic drinking GI Labs: Amylase Lipase Albumin ALT AST Current: 288 224 2.8 204 166 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: -Amylase high 288 (30-125) -Lipase high 224 (10-150) -Albumin low 2.8 (4-6) -ALT high 204 (10-30) AST high 166 (below 50) -Caused due to pancreatitis or even alcohol. (enzyme) -Due to pancreatitis. Lipase and amylase levels are drawn to diagnose pancreatitis. -Low albumin can be seen in inflammation, malnutrition etc. alcohol also impairs albumin levels. - could indicate liver damage due to alcohol abuse. -also indicates liver damage caused by alcohol abuse. High AST can also indicate pancreatitis which the patient has already been diagnosed with. Put it All Together and Think Like a Nurse! 1. Interpreting relevant clinical data, what is the primary problem? What body system(s) will you assess most thoroughly based on the primary/priority concern? What’s the Problem? What’s Causing the Problem? (explain pathophysiology in OWN words) PRIORITY Body System to Assess: pancreatitis All pt symptoms align with pancreatitis which is irritated due to alcohol use. Pt PMH shows diagnosis of pancreatitis and ETOH abuse. Digestive system and Endocrine system. 2. State the rationale and expected outcomes for the medical plan of care. Medical Management: Rationale: Expected Outcome: Establish peripheral IV 0.9% NS 1000 mL IV bolus Hydromorphone 1 mg IV every 2 hours PRN pain Ondansetron 4 mg IV every 6 hours PRN pain NPO Establishing a peripheral IV gives access to peripheral circulation to administer medications, fluids as well as blood labs NS IV is a solution administered to treat dehydration Hydromorphone is a narcotic and is used to treat pain. Ondansetron is administered to treat her nausea and vomiting. Nothing by mouth due to nausea. Used to administered medications via peripheral intravenous. Within a few hours or less we want the pt nausea to decrease and go away entirely. We will reassess pt and expect pain level to go down within 120 minutes. NPO to decrease vomiting. 3. Which specific nursing assessments for this body system are most important? Validate successful completion of each nursing assessment on a manikin (if available) identified with peer or faculty initials. PRIORITY Nursing Assessments: Rationale: Validate Student Performance: Digestive system and Endocrine system. Most importantly we need to focus on Ms.Scott’s abdominal and back pain due to her pancreatitis flare up. N/a 4. What is the current nursing priority and plan of care? Nursing PRIORITY: Acute pain PRIORITY Nursing Interventions: Rationale: Expected Outcome: During assessment document pt pain levels, location, when it occurs, etc. PQRST Pain management Determining location, pain intensity, characteristics etc are critical in determining proper treatment and underlying cause but in this case we already know that. Pain level will go down and within 1-2 weeks pancreatitis will heal. Evaluation: Thirty Minutes Later… Current VS: Most Recent: Current PQRST: T: 99.5 T: 100.6 F/38.1 C (oral) Provoking/Palliative: Movement provokes P: 88 P: 98 (regular) Quality: Sharp R: 15 R: 20 (regular) Region/Radiation: Epigastric area/LUQ BP: 130/90 BP: 146/94 Severity: 4/10 O2 sat:95% O2 sat: 95% room air Timing: Continuous since onset 24 hours ago, now decreased Evaluate the response to nursing and medical interventions. All orders have been implemented. What would be the EXPECTED response in clinical data collected if her pain is decreased and she is no longer nauseated? Current Assessment: GENERAL APPEARANCE: Alert, oriented, pleasant, in no acute distress, Is unkept in appearance with soiled clothing, body tense, grimacing RESP: Breath sounds clear with equal aeration on inspiration and expiration in all lobes anteriorly, posteriorly, and laterally, nonlabored respiratory effort on room air. CARDIAC: Pink, warm & dry, no edema, heart sounds regular, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refill. Heart tones audible and regular, S1 and S2, noted over A-P-T-M cardiac landmarks with no abnormal beats or murmurs. No JVD noted at 30-45 degrees. NEURO: Drowsiness as a side effect of pain medication. oriented to person, place, time, and situation (x4) GI: Abdomen round, soft, and tender in epigastric area and LUQ to gentle palpation. GU: Deceased urine output due to morphine. SKIN: Skin warm, dry, intact, normal color for ethnicity. No clubbing of nails, cap refill <3 seconds, Hair soft-distribution normal for age and gender. Skin integrity intact, skin turgor elastic, no tenting present. 1. What data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: TREND: Improve/Worsening/Stable: Temp: 99.5 BP: 130/90 Pt temp has decreased but still monitoring since this is still a low grade fever. Bp still high due to current situational stress, as well as pain level. Improving Improving. RELEVANT Assessment Data: Clinical Significance: TREND: Improve/Worse [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 18, 2023
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Jan 18, 2023
Downloads
0
Views
68

 Correct Study Guide, Download to Score A.png)

 Correct Study Guide, Download to Score A.png)