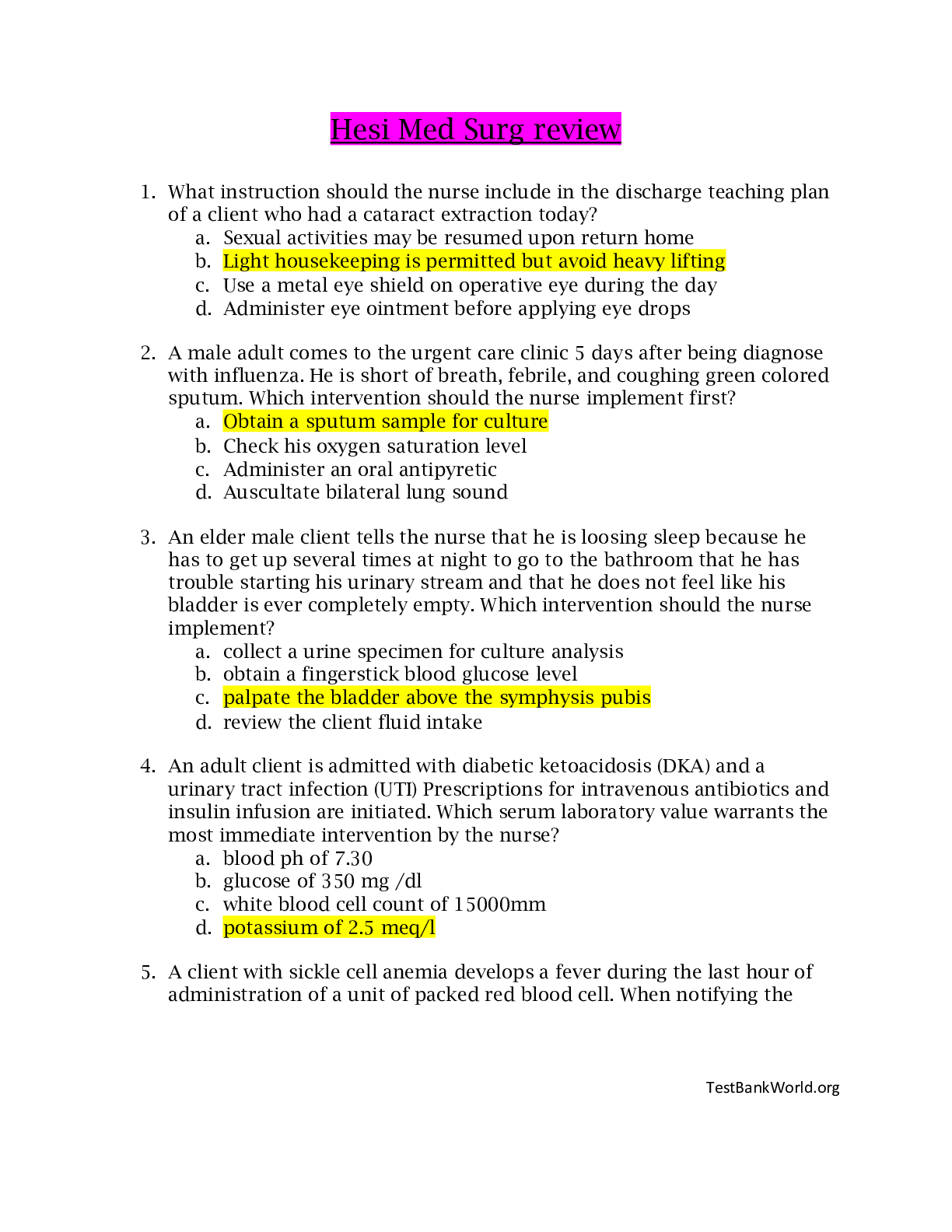
*NURSING > MED-SURG EXAM > Med-Surg-100 Question & Answers Review (test bank) (All)
Med-Surg-100 Question & Answers Review (test bank)
Document Content and Description Below
1 Which of the following is an important component of a teaching plan for the client recently diagnosed with peptic ulcer disease? Incorrect: Antacids should not be taken concurrently with other ulc... er drugs such as H2 blockers because they will decrease drug absorption by 10% to 20%.Correct: The GI complications of NSAID use are strongly linked to mucosal injury and the development of gastric ulcers.Incorrect: Although milk-based diets may provide symptom relief, research has shown they do not influence healing and in fact actually act to increase acid secretion. Diet plays no defined role in ulcer development and current management of ulcers. 2 A nurse admits a 42-year-old female with the following characteristics: excessive sleeping, fatigue, constipation, weight gain, and complaint of intolerance to cold. These signs and symptoms are most consistent with: Incorrect: Although some of the symptoms mentioned would be consistent with acute renal failure (i.e. fatigue, weight gain), there is no mention of the classic symptoms of acute renal failure. These would include signs and symptoms of fluid overload and electrolyte imbalance such as hypertension, neck vein distention, low urine output, confusion. acute renal failure. aplastic anemia. hypothyroidism. diabetes mellitus. 3 A client newly diagnosed with HIV says to the nurse, "I can't believe this is happening. There must be some new treatments that can help." The most appropriate nursing diagnosis for this client based on his comments would be: Incorrect: The defining characteristics of altered family processes include verbal hostility between family members and a general lack of communication and respect between family members. Although this may be a problem for the client with HIV, more data is needed to formulate this nursing diagnosis in this situation.Incorrect: The client has not expressed a feeling of aloneness or verbalized discomfort in social situations, which are characteristics of social isolation. Although clients with a diagnosis of HIV or AIDS may experience social isolation, there is insufficient data to validate this as a problem for this individual.Correct: The client's statement is most consistent with anticipatory grieving which is characterized by the normal grief response including anger, denial, disbelief, and guilt.Incorrect: The defining characteristics of ineffective individual coping include verbalization of the inability to cope, inability to problem-solve, altered social participation, inability to meet basic needs and role expectations and inappropriate use of defense mechanisms to mention a few. Although the client is expressing disbelief, there is insufficient data to support a nursing diagnosis of ineffective individual coping. altered family processes. social isolation. anticipatory grieving. ineffective individual coping. 4 T he nature of systemic lupus erythematosus (SLE) requires the nurse to teach the patient and family: Incorrect: Pregnancy is not necessarily contraindicated in clients with SLE. Although pregnancy does not induce SLE exacerbations, pregnancy should be planned with the client's primary care provider.Correct: Factors such as fatigue, sun exposure, stress, and infection can exacerbate systemic lupus erythematosus. Nursing interventions should include teaching the client and family measures to reduce stress and cope with the chronic disease.Incorrect: Neither discoid nor systemic lupus erythematosus is a contagious disease. Both are thought to be autoimmune disorders.Incorrect: The lesions of SLE are well demarcated and are relatively benign in nature. The rash is generally confined to the face, scalp, and neck. Although other parts of the body may be involved (i.e. mucous membranes), the rash does not actually spread like an allergic dermatitis (i.e. when an irritant or allergen is spread by the hands to another body part as in poison ivy). birth control measures to prevent pregnancy. strategies to prevent and cope with stress. measures to prevent spread of the disease. methods to diminish spread of skin lesions. 5 A Type I diabetic is prescribed to take Regular and NPH insulin before breakfast. The client administers his insulin at 6:00 a.m. prior to breakfast. The nurse should teach the client to: Incorrect: The onset of NPH insulin is approximately 1-2 hours with peak effect between 6-12 hours. Therefore a snack eaten between breakfast and lunch, when the NPH insulin is beginning to reach it's peak action would be important to prevent hypoglycemia before lunch. In addition, regular or quick acting insulin requires that a supplemental snack of 15 g of carbohydrate be given to match the peak action of the insulin. Since regular insulin is peaking at 2-4 hours post administration, a 10:00 a.m. snack would be recommended.Incorrect: Because the NPH insulin will still be peaking from approximately 12:00 p.m. to 6:00 p.m., delaying the evening meal (dinner) until after 6:00 p.m. would put the client at risk for hypoglycemia.Incorrect: Carbohydrate intake must be coordinated with the peak action of insulin. Therefore, the client should be taught to consistently eat carbohydrates at meals, ranging from 45-60% of the total caloric intake.Correct: The peak time of NPH insulin is 4-12 hours. If the client takes the NPH insulin at 6:00 a.m., the insulin will be peaking between 12:00 p.m. and 6:00 p.m. Therefore it is important that food be scheduled between this time period to prevent hypoglycemia. avoid any snacks between breakfast and lunch. delay dinner until after 6:00 p.m.. eat a low carbohydrate lunch at noon. schedule a snack at 3:00 p.m.. 6 A client with a fractured femur was recently admitted to the orthopedic unit in traction. In planning care to minimize the risk for fat embolism, the nurse should implement which intervention? Correct: Immobilization, surgery or trauma to the skeletal system, poor hydration and low tidal volume in the lung are predisposing factors to fat embolism syndrome. Nursing interventions to reduce the risk of fat embolism include good respiratory care, adequate hydration, and stable traction. Other measures include: the use of intermittent pneumatic compression, leg elevation, elastic stockings, and medications (anticoagulant, anti-platelet agents).Incorrect: Fat embolism is not related to diet. The use of supplementary oxygen may require an order, particularly to the client with chronic obstructive pulmonary disease. Range of motion is not recommended for the affected leg.Incorrect: A liquid diet is not necessary for the client in traction. Physical therapy is essential in the rehabilitative phase.Incorrect: Sedation and analgesia are not related to the prevention of fat emboli. The client is encouraged to move the unaffected extremities to reduce the risk of fat embolism syndrome, pressure-related skin injury, and muscle soreness. Provide a low-fat, high-carbohydrate diet, give oxygen, and encourage range of motion in the affected leg. Keep the client on a liquid diet, and have physical therapy start the client on an exercise program for upper body strengthening. Maintain sedation and administer intravenous fluids and medications for pain as needed. 7 T he nurse is caring for a client who has just developed ventricular tachycardia following a myocardial infarction. The nurse anticipates the client will immediately be given which of the following medications? Incorrect: Atropine sulfate is an anticholinergic drug used to increase the heart rate in symptomatic bradycardia (defined as 40 beats per minute).Incorrect: Epinephrine is an adrenergic agent that increases the heart rate. This drug would be contraindicated in fast-rate dysrhythmias. It is one of the first line drugs administered during CPR. By constricting peripheral blood vessels, epinephrine shunts blood to the central circulation and increases blood flow to the heart and brain. It is also given for asystole to stimulate electrical and mechanical activity to produce myocardial contraction.Correct: The first line drug for management of serious ventricular dysrhythmias is lidocaine, which decreases myocardial irritability (automaticity) in the ventricles.Incorrect: Nitroglycerin is used to dilate coronary arteries and improve blood flow. It has no antidysrhythmic effect. Atropine sulfate Epinephrine Lidocaine Nitroglycerin 8 D uring a home visit the nurse determines that the client is experiencing dumping syndrome following his recent total gastrectomy. Which dietary recommendation should the nurse convey to the client? Incorrect: Oral vitamins will have no effect on dumping syndrome. Further, they are of no benefit to the client following total gastrectomy due to loss of intrinsic factor normally secreted by the parietal cells of the stomach. Intrinsic factor is essential for the absorption of vitamin B12. Monthly injection of vitamin B12 will prevent the development of pernicious anemia.Incorrect: Malabsorption of fat may occur after gastrectomy from reduced acid secretion and availability of pancreatic enzymes required for fat absorption. Dumping syndrome occurs because of the rapid entry of hypertonic food into the upper small intestine without undergoing the usual breakdown and dilution in the stomach. This stimulates motility and diarrhea. Preventive measures include a moderate-fat, high-protein diet with limited carbohydrates.Correct: Fluids with meals are discouraged because they increase total volume and further promote diarrhea.Incorrect: Rest on the left side for 20-30 minutes after eating is thought to delay gastric emptying and may be helpful for some individuals. Begin taking a vitamin B complex supplement. Eat a high carbohydrate, low fat, low protein diet. Decrease fluid intake with meals. Go for a slow, short walk after eating. 9 A client with asthma goes into status asthmaticus. Which clinical signs, if present, would indicate that intubation and mechanical ventilation are needed? Incorrect: Both hyperresonance (air-trapping) and tachypnea are characteristic of an acute asthma attack.Incorrect: Severe inspiratory and expiratory wheezing is consistent with an acute asthma attack. Clients with status asthmaticus may be moving minimal amounts of air into and out of the lungs therefore audible wheezing may NOT be present.Correct: These blood gas values indicate respiratory acidosis and hypoxemia. This occurs as a result of a prolonged attack where respiratory muscle exhaustion causes hypoventilation. If respiratory acidosis and hypoxemia are present, intubation and ventilatory assistance may be required if oxygen and other treatment measures are ineffective.Incorrect: Tachycardia and an elevated blood pressure are expected findings during an acute asthma attack. However, clients with status asthmaticus may exhibit pulsus paradoxus. Pulsus paradoxus is an accentuation of the normal decrease in systolic arterial pressure with inspiration. This is a result of changes in intrapleural pressure during respiration that occurs in obstructive airway disease. Hyperresonance and tachypnea Severe inspiratory and expiratory wheezing pH 7.32, PCO2 55 mm Hg, PO2 74 mm Hg Pulse 110/minute, BP 150/88 10 Which nursing intervention is the priority for care of the client during the acute phase of a cerebrovascular accident (CVA)? Incorrect: Following a CVA clients are at risk for a variety of complications associated with immobility and subsequent disuse such as contractures and skin breakdown. While preventive nursing care measures are incorporated into the daily routine, during the acute phase of a stroke, the immediate priority is maintaining a patent airway and adequate oxygenation to support cerebral perfusion.Correct: During the acute phase of a cerebrovascular accident it is essential to assess respiratory function and maintain a patent airway to support oxygenation and cerebral perfusion. Because of motor of sensory deficits, the client with a CVA is at risk of aspiration of food, fluid, and secretions.Incorrect: The effects of a CVA are life altering. The emotional changes and physical limitations that commonly occur, challenge the coping abilities of the client and family. Although a nursing care plan would be incomplete without addressing the coping needs of the client and family, the immediate priority post CVA is respiratory and neurological assessment and promotion of oxygenation to the brain.Incorrect: Problems with urinary incontinence are common after stroke and the plan of care during hospitalization and rehabilitation will include measures to restore continence. However, the immediate care priority in the acute phase of stroke is airway, oxygenation, and cerebral perfusion. Decrease the complications of disuse. Monitor the status of respiratory function. Maintain effective coping by the family. Assess for bladder distention. 11 Of the following nursing diagnoses, which one would most effectively address primary prevention as it relates to drug management in the elderly population? Incorrect: The nursing diagnosis that most effectively guides primary prevention of drug reactions and interactions involves identifying the risk and taking measures to prevent adverse reactions, self-care deficit, and/or injuries. Although elderly clients taking multiple drugs are at greater risk for adverse reactions because of complex drug regimens and age-related physiological changes, a diagnosis of 'self-care deficit related to adverse reactions to prescribed drugs' addresses an actual problem with drug management.Incorrect: The prevention of drug mismanagement, adverse reactions and side effects is best addressed using a potential nursing diagnosis that identifies risk factors in the elderly population. The other answer options are nursing diagnosis that address 'actual' problems.Incorrect: Although elderly clients may be noncompliant with the drug regimen due to lack of sufficient knowledge regarding drug administration, this diagnosis does not focus on problem prevention.Correct: Because elders consume disproportionately more of all kinds of drugs than do middle-aged adults, 'risk for injury related to polypharmacy' is the nursing diagnosis that would focus on prevention of complications for this group of individuals. Self-care deficits related to adverse reactions to prescribed drugs Body image disturbance related to drug side effects Noncompliance related to knowledge deficit Risk for injury related to polypharmacy 12 The nurse is planning care for a 48-year-old female following a total hysterectomy. Which of the following interventions would be contraindicated? Incorrect: Frequent ambulation is encouraged as the most reliable means of stimulating peristalsis. In addition, ambulation supports oxygenation through natural deep breathing and assists in the elimination of residual anesthetic.Incorrect: The risk of thromboembolism is significant in the post-hysterectomy client because of venous pooling and pelvic congestion. Nursing interventions to prevent thromboembolism include compression stockings and leg/foot flexion and extension exercises.Incorrect: Pain relief should be promoted not only for comfort but to promote frequent turning, coughing and deep breathing, and early ambulation. Narcotic analgesics are the most effective in relieving pain during the immediate postoperative period and should be encouraged to prevent severe pain and enhance activity.Correct: Venous pooling and pelvic congestion are common complications after hysterectomy, especially if the lithotomy position was used. Efforts should be taken to avoid positioning the client with the knees bent since this promotes pelvic congestion. Early ambulation Compression stockings Narcotic analgesics Pillows under the knees 13 The nurse is teaching an asthmatic client how to treat episodes of acute bronchoconstriction. Of the following inhaled agents, if prescribed, the nurse should teach the client to immediately take the: Incorrect: The anticholinergic Atrovent is ineffective in acute bronchospasm when a rapid response is required. It is used in maintenance therapy in chronic, bronchoconstrictive conditions such as chronic bronchitis and emphysema.Correct: The 1st drug of choice in an acute asthma attack is a short-acting inhaled beta2-adrengergic agonist such as albuterol sulfate (Proventil) or metaproterenol sulfate (Alupent). These drugs cause smooth muscle relaxation and bronchodilation and start to act within 10 minutes.Incorrect: Inhaled steroids do not play a role in acute situations. Corticosteroids primarily work by suppressing inflammation in the airways, thereby decreasing mucus secretion and edema. Another important action is to increase the number and sensitivity of beta2-adrenergic receptors, which increases the effectiveness of beta2-adrengergic bronchodilators. In maintenance therapy, it should be noted that the inhaled beta2-agonist should be given first to open the airway; followed by the inhaled steroid, which will be more effective when inhaled deeper into the lung.Incorrect: Cromolyn (Intal) is used to prevent acute asthma attacks in clients with chronic asthma. The drugs in this category are used only for prophylaxis and are not effective in acute bronchospasm. Mast cell stabilizers prevent the release of bronchoconstrictive and inflammatory substances when mast cells are confronted with allergens. anticholinergic (Atrovent). beta2-adrenergic agonist (Albuterol). corticosteroid (Azmacort). mast cell stabilizer (Cromolyn). 14 A client is admitted to the Intensive Care Unit following a femoral-popliteal bypass graft. Which intervention provides the most relevant data about graft patency? Incorrect: This activity evaluates neurological status and would not provide any significant data regarding graft patency, circulation, and perfusion.Incorrect: Monitoring ECG activity is a critical nursing intervention because clients with vascular disease commonly have problems with CAD or hypertension. However, palpating arterial pulses gives the most information about the patency of the graft and perfusion of blood to areas below the bypass.Incorrect: Because coronary artery disease and hypertension are common in clients with vascular disease, dysrhythmias or cardiac failure are potential complications of vascular surgery. Therefore, accurate documentation of I & O is also essential to quality nursing care to detect alterations in cardiac output and renal perfusion. However, palpating arterial pulses gives the most information about the patency of the graft and perfusion of blood to areas below the bypass.Correct: Graft patency is a priority concern in the postoperative client because the risk of reocclusion from thrombosis, restenosis, or debris is significant. The nurse should monitor the client's peripheral pulses and limb temperature, as well as the degree of pain, pallor, sensation, and movement. Check the equality of the client's hand grasps. Check the electrocardiogram every four hours. Record the client's intake and output. Palpate all arterial pulse sites as frequently as every hour. 15 A preoperative order is written for meperidine 50 mg IM. Which desired effects can the nurse anticipate following drug administration? Incorrect: Anticholinergic agents such as Robinul are often given preoperatively to inhibit salivation and excessive respiratory secretions.Correct: Meperidine (Demerol) is an opioid analgesic. Meperidine binds to opiate receptors in the central nervous system resulting in altered perception of and response to painful stimuli. As a secondary response, the client's blood pressure can be expected to decrease as pain diminishes. It should be noted that hypotension can be an adverse reaction.Incorrect: Meperidine is not known to have any antiemetic or GI stimulant effects. A drug expected to have these effects would be metoclopramide (Reglan). Recall that opioids can have a constipating effect.Incorrect: The therapeutic effects described are characteristic of Versed, a sedative/ hypnotic that induces short-term sedation and postoperative amnesia. Decreased salivation and mucous production Pain reduction and decreased blood pressure Reduced nausea and increased peristalsis Sedation and amnesia following the surgical procedure 21 When treating clients with chronic obstructive pulmonary disease (COPD) who are hypoxemic, the standard of care is to: Correct: Breathing very high concentrations of O2 for prolonged periods is associated with acute respiratory distress syndrome. A firm general principle is to use the lowest amount of O2 that will achieve an acceptable PO2.Incorrect: It is true that precautions must be taken when giving O2 to clients with COPD. These persons chronically retain carbon dioxide; low O2 levels produce the drive to breathe.Incorrect: This is a common misunderstanding by clients requiring O2 therapy. Studies have shown that clients receive the most benefit from O2 therapy if the oxygen is used continuously.Incorrect: Clients with COPD who are carbon dioxide retainers must receive supplemental O2 by controlled O2 delivery devices. When low-flow O2 is desired, oxygen is given by nasal cannula. The Venturi mask can also be used to deliver O2 at controlled levels. administer the least amount of O2 that achieves an acceptable PO2. maintain low-flow O2 under all circumstances. institute O2 therapy only when dyspnea occurs. use a nasal cannula rather than a facial mask. 22 A client is being treated for pulmonary edema secondary to congestive heart failure. Which signs/symptoms, if present, would suggest to the nurse the onset of acute respiratory failure? Incorrect: Although acute dyspnea will occur as a result of hypoxemia, alone it is not a criterion for diagnosing acute respiratory failure.Incorrect: An irregular apical pulse in this situation may be associated with the client's congestive heart failure, commonly associated with dysrhythmias such as atrial fibrillation. An irregular apical pulse is not a component of the physiological criteria used to diagnose acute respiratory failure.Incorrect: Jugular vein distention is a clinical manifestation of the client's congestive heart failure.Correct: Acute respiratory failure is defined as any rapid change in respiration resulting in hypoxemia, hypercarbia, or both. Physiological criteria for acute respiratory failure include sudden onset of PO2 50 mmHg or less, PCO2 50 mm Hg or more, and pH 7.35 or less. Acute dyspnea Irregular apical pulse Jugular vein distention PO2 < 50 mm Hg, PCO2 > 50 mm Hg 23 The primary care provider prescribes levodopa for a 68-year-old male diagnosed with Parkinson's disease. The nurse knows that this drug helps reduce rigidity by: Incorrect: A deficient amount of norepinephrine is thought to be a contributing factor in depression. Some of the antidepressants such as the monoamine oxidase inhibitors (MAO) act by facilitating release of norepinephrine in nerve terminals. Parkinson's disease does not involve this neurotransmitter.Incorrect: Parkinson's disease involves deficient amounts of dopamine. Insufficient dopamine allows large numbers of excitatory acetylcholine (ACh) secreting neurons to remain active, creating an imbalance between excitatory and inhibitory neuronal activity. This results in the characteristic excessive excitation of neurons that occurs in Parkinson's disease interfering with control or initiation of voluntary. Anticholinergic agents, such as Cogentin, are often prescribed to decrease the excitatory effects of ACh.Incorrect: A deficiency of norepinephrine and/or serotonin is thought to be a component of depression. Selective serotonin reuptake inhibitors (SSRI) are antidepressants that increase the amounts of these neurotransmitters in the CNS. Parkinson's disease does not involve this neurotransmitter.Correct: Parkinson's disease results from degeneration of the substantia nigra, leading to a decrease in the amount of dopamine, resulting in loss of the ability to refine voluntary movement. Levodopa is converted to dopamine in the central nervous system. enhancing the release of norepinephrine. increasing the action of acetylcholine. inhibiting the reuptake of serotonin. restoring deficient dopamine. 24 When evaluating serial electrocardiograms (ECGs) for a client with coronary artery disease, the nurse knows that this diagnostic tool is important because the ECG: Incorrect: Although ECG characteristics may lend support to the diagnosis of angina and/or infarction, it does not give definitive data that would help distinguish between stable and unstable angina. The client's history often distinguishes between types of angina (i.e. provocative factors, what relieves the pain, duration etc.).Incorrect: Blood studies are equally important but can take longer to analyze. Injured myocardial cells release several enzymes that are important indicators of acute myocardial infarction.Incorrect: Stress testing is an important diagnostic tool different from the 12- lead ECG. An exercise stress test demonstrates the significance of coronary artery blockages and can indicate areas of the myocardium that do not receive adequate perfusion at peak exercise.Correct: ST segment elevation is the hallmark of acute myocardial ischemia leading to infarction. Because ECG findings correlate to anatomical locations, it can indicate which type of infarction has occurred. Therefore, the ECG is an important diagnostic tool. can help distinguish between stable and unstable angina. is a more reliable diagnostic tool than blood studies. replaces the need for stress testing. wave abnormalities can signal injury and/or infarction. 25 Acute respiratory distress syndrome (ARDS) can be detected early in high-risk clients. Which of the following are early manifestations of ARDS? Incorrect: These are late signs of ARDS. As alveoli collapse and gas exchange is impaired, signs of hypoxia occur including cyanosis and tachycardia. The client becomes fatigued as the work of breathing increases as evidenced by intercostal retractions. Incorrect: Early in the course of ARDS chest auscultation is clear. As the leakage of fluid into the interstitial and intra-alveolar spaces increases, terminal airways become filled with fluid and adventitious breath sounds are auscultated. Grunting respirations and shallow breathing are also late signs as respiratory fatigue and hypoxia occur. Incorrect: Generally, blood-tinged or frothy sputum occur with pulmonary edema. This occurs as a result of increased pulmonary capillary pressures and RBCs entering the alveoli. Correct: Although clinical presentation will vary depending on the pathophysiology contributing to ARDS, early indicators include dyspnea, restlessness, hyperventilation, cough, and labored breathing. Late: Tachycardia, cyanosis, intercostal retractions Late: Adventitious breath sounds, grunting respirations, shallow breathing Pulm edema: A productive cough with bloody or frothy sputum Dyspnea, restlessness, and hyperventilation 26 A client is admitted to the emergency department with diabetes mellitus and a blood sugar of 620 mg/dl. Her skin is flushed and warm, mucous membranes are dry, respirations are rapid and deep, and she is irritable. Arterial blood gas (ABG) values reveal pH 7.18, PCO2 12 mmHg, HCO3 12 mEq/L. The ABG results confirm the client is in: Incorrect: Although the pH does indicate acidosis, the PCO2 does not indicate respiratory acidosis. Recall that CO2 when combined with H2O forms H2CO3 or carbonic acid. Therefore, if the PCO2 is low, then less carbonic acid is formed. Respiratory acidosis would be reflected in an elevated PCO2 when carbon dioxide is retained and more carbonic acid is formed.Incorrect: Although the low PCO2 is consistent with respiratory alkalosis, the pH indicates acidosis. Therefore, we can eliminate alkalosis as a correct choice.Correct: The imbalance is metabolic acidosis suggested immediately by the client's history and clinical manifestations. Diabetic ketoacidosis occurs most often in clients with type I IDDM who experience illness, infection, or trauma. The insulin deficiency prevents normal utilization of serum glucose by the cells. The body is forced to break down fat and protein stores for energy resulting in ketone bodies accumulating in the blood. Ketones cause the blood pH to drop. The pH is acidotic (< 7.35). The client's low PCO2 does not match with acidosis. In other words, the low PCO2 is not the cause of the acidosis but is decreased, indicating CO2 is being blown-off as a result of the client's rapid and deep respirations, referred to as Kussmaul's respirations. This is a compensatory response to the metabolic acidosis indicated by the low HCO3. The HCO3 is low in proportion to the increase in fixed acids in the blood (in this case ketones). The metabolic acidosis is only partially compensated as indicated by the abnormal pH.Incorrect: The pH is consistent with acidosis since it is less than 7.35. Therefore, we can immediately eliminate alkalosis as a correct interpretation. respiratory acidosis, partially compensated. respiratory alkalosis, uncompensated. metabolic acidosis, partially compensated. metabolic alkalosis, fully compensated. 27 The nurse is evaluating central venous pressure (CVP) measurements for a client with multi-system injuries who was recently admitted to the intensive care unit. The nurse determines the most recent CVP measurement to be very low. This reading indicates: Incorrect: The CVP does not give any direct information about pressure in the arterial system. However, it does provide information about fluid volume and therefore could indirectly suggest blood pressure changes. In the case of a low CVP reading, hypovolemia is the likely cause and blood pressure would be decreased.Correct: CVP is the measurement of systemic venous pressure at the level of the right atrium. Because 60% of the blood volume is in the venous system, the CVP is valuable in assessing fluid volume excess or deficit. Usually, decreased CVP is caused by hypovolemia.Incorrect: The CVP does not give any information about oxygenation. Arterial blood gas analysis can be obtained via an arterial catheter for assessment of oxygenation status.Incorrect: Aside from direct observation, the best tool for analyzing ventilation status is arterial blood gas analysis. The CVP does not provide information about ventilation. hypertension. hypovolemia. hypoxia. hyperventilation. 28 Which of the following individuals has the most risk factors for developing hypertensive disease? A/an: Incorrect: Based on the data, this client is at low risk since her weight is within ideal range for her height. Obesity is an important risk factor in the incidence of hypertension. She does not have any risk factors listed.Incorrect: This client's age represents a risk factor. However, persons of Hispanic culture have been noted to be at higher risk. Although elevated cholesterol and triglyceride levels are correlated with coronary artery disease and hypertension, this client's cholesterol level is at the upper edge of normal. This client has two risk factors.Correct: Age is the primary risk factor for hypertension. It is more common among men than women until after menopause, and is twice as prevalent and more severe among African Americans. Smoking and excess alcohol use are also risk factors. This client has five risk factors.Incorrect: Although this female is the oldest of the four choices, her culture does not place her at high risk. Heredity also plays a role in hypertensive disease. This client has two risk factors. 42-year-old white female, 5 feet, 9 inches, weight 145 lbs. 64-year-old Hispanic male, cholesterol 180 mg/dl. 76-year-old black male, 40 pack year history of smoking, alcoholic. 80-year-old Asian female whose mother had coronary artery disease. 29 A client in the rehabilitative phase of a burn injury is having difficulty with pain management. The nurse planning this client's care should consider which intervention for pain control? Incorrect: The client with burn injury experiences pain that requires analgesia, usually narcotics in the acute phase. Non-pharmacologic treatments, such as relaxation technique, distraction, music therapy, guided imagery and hypnosis, are also effective in the reduction of perceived pain. Sedation promotes drowsiness and does not relieve pain. Incorrect: The nurse may teach the client with chronic pain the use of various nonpharmacologic therapies for pain management. The techniques of guided imagery, distraction, progressive relaxation, music therapy, and hypnosis that are used as an adjunct to analgesia may be more effective than medication alone. Correct: Pain relief with analgesic agents, such as narcotics or non-steroidal antiinflammatory agents, may be obtained through the oral or intravenous routes. Intramuscular administration is contraindicated due to the erratic and diminished circulation to muscle tissue. Non-pharmacologic treatments, such as relaxation technique, distraction, music therapy, guided imagery and hypnosis, are also effective in the reduction of perceived pain.Incorrect: Methods to control pain, either analgesic or nonpharmacologic therapies, are most effective if used at or just below the pain threshold. A cascade of physiologic responses occurs that contribute to the increased difficulty in controlling the perception of pain. A more effective strategy for pain management is to intervene before it escalates. Request that the primary care provider prescribe sedative medication. Ask the primary care provider to order a patient-controlled analgesic pump. Encourage the use of analgesia and non-pharmacologic methods of pain control. Teach the client to minimize the use of analgesia to prevent a tolerance effect. 30 As part of the collaborative plan of care, which class of medications would the nurse expect the practitioner to prescribe for the client with newly diagnosed glaucoma? Correct: Recall that in glaucoma, intraocular pressure rises as a result of structural resistance (open-angle) or complete obstruction (closed-angle) to the outflow of aqueous humor through the chamber located between the iris and cornea. Pressure is placed on the optic nerve and blindness can result. Miotics (direct-acting cholinergics) such as pilocarpine hydrochloride are commonly used to treat glaucoma. These drugs constrict the pupil so that the ciliary muscle is contracted which allows better circulation of aqueous humor.Incorrect: Antibacterial agents such as tobramycin or gentamicin sulfate are prescribed as anti-infective agents and are not routinely given to clients with glaucoma unless surgical intervention is required.Incorrect: Systemic anticholinergics such as atropine would be contraindicated, especially in the client with closed or narrowangle glaucoma, because of the anticholinergic effects (mydriasis or pupillary dilation). Ophthalmic atropine solution is classified as a cycloplegic mydriatic causing pupillary dilation. These drugs are hazardous in glaucoma.Incorrect: Systemic corticosteroids can raise intraocular pressure and even cause glaucoma. Therefore, corticosteroids decrease the effects of all drugs used for glaucoma. However, an ocular steroid may be prescribed following laser surgery. Direct-acting miotic agent Ophthalmic antibacterial agent Systemic Anticholinergic Corticosteroid 31 The nurse is obtaining a health history from the client scheduled for a transurethral resection of the prostate (TURP) in the morning. Which question should the nurse ask that is essential to the safety of the client prior to surgery? Correct: Since bleeding can be a common postoperative problem the nurse must carefully assess the client's medication history. The use of over-the-counter medications that impair clotting, such as ASA and NSAIDs should be documented.Incorrect: Although important to the overall assessment of the client with prostatic dysfunction, determining degree of nocturia is not the most essential piece of preoperative information.Incorrect: This would be an essential question to ask the client immediately prior to surgery. Although assessing voiding patterns is important in the client with prostatic disease, the question regarding aspirin therapy is essential to the client's safety.Incorrect: Again, this would be an important question to ask the client the morning of surgery. Questions regarding over-the-counter drugs and prescribed anticoagulants are essential to the client's safety. "Do you take aspirin or any blood thinners?" "How often do you get up during the night to urinate?" "How much did you urinate last time you voided?" "When did you last take your medications?" 32 A client with Acquired Immunodeficiency Syndrome (AIDS) develops shingles on the trunk. Which is the most likely rationale for this client to develop herpes zoster infection? Incorrect: Shingles, caused by the herpes zoster virus, occurs after exposure to the varicella-zoster virus (chickenpox).Correct: Shingles, caused by the herpes zoster virus, is an infection of the dorsal nerve root ganglion. Increased incidence of herpes zoster occurs in clients with AIDS, lymphoma, and leukemia because of the impaired immunologic response.Incorrect: Herpes zoster, also known as shingles, is a viral infection not related to a vaccination for measles, mumps or rubella.Incorrect: Herpes zoster is a viral infection, known as shingles. The client never had chicken pox as a child. Shingles frequently occurs in the host with immunosuppression. Client received a recent measles, mumps, and rubella vaccination. Herpes zoster is an allergic reaction to medication. 33 A client has a chest tube following a chest injury. Continuous bubbling in the water-seal chamber of the closed drainage system would alert the nurse to which of the following? Incorrect: Absence of tidaling of fluid in the water-seal chamber could suggest that the tubing is obstructed by a kink or dependent fluid has filled a loop of tubing. It also may suggest lung re-expansion. In the presence of a pneumothorax, tidaling or fluctuation in the water-seal chamber will occur. The water level will rise on inspiration and fall on expiration.Incorrect: Continuous bubbling in the water-seal chamber is not an indication that the drainage system is properly functioning. As described below, excessive bubbling may indicate a leak in the system.Correct: Unexpected or continuous bubbling in the water-seal chamber indicates an air leak in the closed system. During forceful expiration or coughing, bubbling is expected because air in the chest is being expelled. Efforts must be made to identify the source of the leak.Incorrect: Tidaling of fluid in the tubing and/or water-seal chamber will occur as long as a pneumothorax is present to any degree. As described above, continuous bubbling suggests a leak in the system. The affected lung is now fully expanded. The water-seal drainage is properly functioning. An air leak may be present in the closed system. The pneumothorax is expanding. 34 To prevent vessel and/or tissue injury during intravenous infusion of a concentrated potassium solution to the client with severe hypokalemia the nurse should: Incorrect: Intravenous potassium is extremely irritating to blood vessels and subcutaneous tissue. Potassium should NEVER be given IV push. The potassium would be insufficiently diluted, and if infiltration occurred during administration, severe tissue injury could occur. In addition, without proper dilution severe cardiac dysrhythmias could result.Incorrect: Intravenous potassium should be diluted in large quantities of solution. The recommended dilution is a solution that contains no more than 60 mEq/L in clients with a K+ < 2.0 mEq/L and ECG abnormalities; and 30 mEq/L for clients with less severe hypokalemia (i.e. 2.5 mEq/L) and no ECG manifestations. In clients unable to tolerate large fluid volumes, more concentrated K+ solutions are used such as 10-20 mEq/100 mL.Incorrect: For the same reasons as discussed above, potassium should NEVER be given as a bolus.Correct: To minimize irritation of the peripheral vein, a concentrated KCl solution should be piggybacked into a running primary line to help dilute the solution. To avoid fluid overload, a small volume of sodium chloride (i.e. 100 - 250 ml) could be initiated as the primary line to facilitate the potassium infusion and then discontinued after drug therapy. NOTE: if the client is not on a fluid restriction, and the situation is not emergent, the best way to safely administer potassium IV is to dilute the potassium in large volumes (i.e. 40 mEq/liter). administer the infusion IV push slowly over 5 minutes. dilute the potassium preparation in at least 20 mL sodium chloride. give the potassium as a bolus preparation. piggyback the solution into a primary line. 35 An adult client has been vomiting persistently for 3 days. On admission he weighed 155 pounds. He states he weighed 167 pounds one week ago. Serum sodium is 155 mEq/L. Which signs/symptoms would the nurse expect to find on assessment? Incorrect: A bounding pulse is characteristic of hypervolemia when excess fluid is in the vascular space. Hand veins that are slow to empty, or remain engorged when elevated above the heart is also indication of fluid volume excess.Incorrect: A reduction in urine specific gravity and serum osmolality indicate dilution of the vascular space as would occur in fluid volume excess. Dehydration would cause the blood and urine to be concentration with a resultant increase in urine specific gravity and serum osmolality.Correct: The client is exhibiting clinical manifestations of dehydration due to severe diarrhea occurring with inadequate volume replacement or fluid replacement with hyperosmolar solution. Both a fluid volume deficit and hypernatremia are present. Fluid volume deficit is manifested by postural hypotension (a key sign), tachycardia, dry mucous membranes, elevated body temperature, weight loss, reduced urine output and increased specific gravity. As the serum sodium rises due to loss of water, symptoms include extreme thirst and dry, sticky mucous membranes, rough dry tongue, increased serum osmolality, and behavioral changes such as restlessness and agitation.Incorrect: A combination of cough, dyspnea, and peripheral edema suggest fluid volume excess with accumulation of fluid in the lungs. Bounding pulse and hand veins are slow to empty Decreased urine specific gravity and serum osmolality Postural hypotension and thirst Cough, dyspnea, and peripheral edema 36 The client experiencing an acute myocardial infarction can be given Morphine sulfate IV every 2-3 hours prn chest pain. The primary function of Morphine sulfate in this situation is to: Incorrect: Increases in oxygenation of myocardial tissue occur through the use of vasodilators such as the nitrates. In addition, the most effective immediate intervention to increase myocardial oxygen supply is via supplemental oxygen.Correct: Morphine sulfate has a vasodilating effect on peripheral vessels thereby causing venous pooling and decreasing venous return (preload). This helps to reduce the workload of the heart. The analgesic effect of morphine also helps reduce the client's anxiety as chest pain is reduced or eliminated. The primary function of morphine is to decrease pain and the associated deleterious effects of pain (i.e. increased myocardial oxygen demand).Incorrect: Coronary artery vasodilators work by increasing blood flow to the myocardium. Morphine is not a coronary artery vasodilator.Incorrect: Antiplatelet agents such as aspirin work by inhibiting platelet aggregation resulting in reduced clot formation. Morphine does not have any affect on platelet aggregation. increase oxygenation of myocardial tissue. decrease anxiety and reduce cardiac workload. increase blood flow to the myocardium. inhibit platelet aggregation. 37 A post-menopausal female diagnosed with cervical cancer is admitted for placement of a radioactive implant. More teaching is required if the client states: Incorrect: A foul-smelling vaginal discharge is expected from destruction and sloughing of cells.Incorrect: Radiation precautions for internal radiotherapy include the principles of time and distance. Visitors will be held to the same precautions as staff, including the limitation of time at the bedside.Correct: This statement indicates the need for more teaching since the client with a cervical implant should select a low-residue diet to prevent abdominal distention. During treatment with an intracavity implant, it is important that all untreated tissues remain in their normal position and not come in contact with the radioactive device. The bowel is cleansed before therapy and a lowresidue diet is maintained during treatment to prevent bowel distention.Incorrect: The client must be kept in bed and as flat as possible to prevent dislodgement of the radioactive substance. Turning from side to side is permitted for comfort. "I can expect a foul-smelling vaginal discharge." "I realize time for visitors will be restricted." "I will select high fiber foods throughout the treatment." "I will remain in bed while the implant is in place." 38 In planning nursing care for the client with a left hemisphere stroke, the nurse develops the following interventions. Which one addresses the problem of unilateral neglect? Incorrect: This nursing intervention is aimed at addressing the problem of fluent aphasia where the individual has difficulty comprehending speech but may be able to speak fluently.Incorrect: This nursing intervention is aimed at addressing the problem of hemianopsia (loss of vision in a portion of the visual field).Correct: Unilateral neglect involves a distortion in body image in which the individual ignores the affected side of the body. Teaching the client to monitor the position of the right side will help the person be aware of that side and promote safety.Incorrect: This intervention is aimed at addressing the problems of agnosia/apraxia. Agnosia is the inability to recognize familiar objects, and apraxia is the inability to properly use objects or carry out a learned sequence of movements. Face the client and speak slowly and distinctly. Place objects within the client's visual field. Teach the client to monitor position of the right side. Verbally cue the client about correct use of objects. 39 While caring for a postoperative client the nurse checks the most recent arterial blood gas (ABG) values which reveal a pH 7.37, PCO2 of 40 mmHg and HCO3 of 24 mEq/L. What conclusion can the nurse make? Incorrect: These ABG values are within normal range. If the kidneys were retaining fixed acids there would be evidence of metabolic acidosis with a lowered pH and HCO3.Correct: Normally, the body maintains a ratio of carbonic acid (CO2 plus H2O) and bicarbonate at 1:20. This ratio keeps the pH within normal limits. Since the client's PCO2 and HCO3 levels are within normal range one can infer that the carbonic acid/bicarbonate ratio is normal.Incorrect: Since the pH, PCO2 and HCO3 levels are all within normal range, there is neither acidosis nor alkalosis. If respiratory alkalosis were present, the pH would be elevated and the PCO2 would be below normal.Incorrect: If the client were hyperventilating the PCO2 would most likely be low since carbon dioxide would be blown off. Kidneys are retaining fixed acids. Carbonic acid/bicarbonate ratio is normal. Respiratory alkalosis is present. The client is hyperventilating. 40 In planning the care of an adult client with acute renal failure (ARF) caused by a drug overdose, the nurse is aware that the recovery phase of the nephrons occurs when: Correct: During the recovery phase of acute renal failure, the BUN and creatinine levels stabilize.Incorrect: A reduction of the glomerular filtration rate occurs in the oliguric phase when the kidney is unable to excrete metabolic wastes. This is manifested by increased serum urea nitrogen (BUN) and creatinine levels.Incorrect: During the recovery phase of ARF the client's energy levels generally improve but may continue to decrease. Fatigue may last from 3-12 months.Incorrect: A marked increase in urine output occurs in the diuretic phase of acute renal failure due to a decline in the concentrating ability of the renal tubules and the osmotic diuretic effect of a high BUN. BUN and creatinine levels stabilize. glomerular filtration rate decreases. the client's energy level returns. urine output increases by 3 to 5 liters per day. 41 Which clinical manifestation is the most reliable indicator for a fluid imbalance? Incorrect: Blood pressure changes often do occur with fluid and electrolyte disturbances, however many other factors raise or lower blood pressure (i.e. coronary artery disease, stress).Correct: Daily weight, at the same time, in similar clothing is the most reliable means of estimating fluid gains/losses.Incorrect: Urine output only measures the integrity of the urinary system. Intake AND output should be assessed to determine fluid gains/losses. However, I & O is not considered the most reliable indicator of fluid gains or losses because accuracy is hampered by many factors such as failure to (a) explain I & O to the client and family, (b) consider that parenteral fluid bottles are overfilled, (c) estimate fluid lost as perspiration, 'uncaught' emesis or wound exudate, (d) record intake or output.Incorrect: Skin turgor is not considered a reliable indicator of hydration especially in the elderly because of changes in skin elasticity. In addition, skin color changes do not typically occur in fluid or electrolyte imbalances. Blood pressure Daily weight Hourly urinary output Skin turgor and color 42 A client is admitted to the emergency department with a diagnosis of diabetic ketoacidosis. Which presenting sign/symptom would the nurse expect the physician to give highest priority? Incorrect: Although the serum potassium level is low, it is not the highest priority. IV potassium will be replaced once rehydration is achieved and renal output is established.Correct: A priority intervention in treating the client with diabetic ketoacidosis (DKA) is rehydration. Recall that hyperglycemia causes an osmotic diuresis resulting in dehydration. Priorities in management of DKA center on rehydration and IV insulin to control gluconeogensis and ketogenesis.Incorrect: Although the arterial pH indicates mild acidemia, treatment with sodium bicarbonate is not indicated unless pH is < 7.0 and client is exhibiting shock or dysrhythmia. The pH is low because in the presence of insulin deficiency the liver will produce excessive ketones that are acidic. This can lead to metabolic acidosis because ketones are acidic and they are retained in the presence of dehydration and decreased urine output. However, this client's arterial pH does not indicate severe acidosis. The priority focus should be on rehydration.Incorrect: Although it is important to determine if the client with DKA is septic, the client's WBC is only slightly elevated and may represent leukocytosis commonly seen in DKA. Serum potassium 3.2 mEq/L Dehydration Arterial pH 7.34 WBC 11,000/mm3 43 A young male client had a positive ELISA and Western blot test for HIV three years ago. He has been admitted to the medical unit with a diagnosis of Pneumocystis carinii pneumonia. This client would be categorized as having/being: Correct: In the past, clinicians used an informal staging system categorizing clients who have experienced an opportunistic infection as having AIDS. Pneumocystis carinii pneumonia is the most common opportunistic infection associated with HIV infection.Incorrect: In this informal staging system, those clients classified as having AIDS-related complex exhibited constitutional symptoms including persistent generalized lymphadenopathy, persistent fevers, involuntary weight loss or diarrhea.Incorrect: In this staging system, HIV positive referred to those clients who were completely asymptomatic but HIV positive.Incorrect: Although the end result may be similar, immunosuppression is different from immunodeficiency. AIDS is a syndrome involving immunodeficiency from depletion of T4 helper cells resulting in a dramatic loss of the protective immune response. On the other hand, immunosuppression involves an inhibition of the formation of antibodies to antigens that may be present. AIDS. AIDS-related complex. HIV positive. immunosuppression. 44 Which is an appropriate nursing care goal for the client with Cushing syndrome? Incorrect: Fluid volume excess is the primary concern in clients with Cushing's syndrome. Recall that this syndrome involves an excess of cortisol that has mineralocorticoid activity resulting in excessive retention of sodium and water.Correct: Clients with Cushing's syndrome are at increased risk for infection because cortisol excess results in decreased lymphocytes and cell-mediated immunity, and altered antibody activity. These changes make persons vulnerable to viral and fungal infections.Incorrect: Clients with cortisol excess are usually overweight as a result of changes in fat metabolism. The nurse should assist the client in restricting calories.Incorrect: Although rest and careful management of energy levels is important, the goal is to maintain the client's current activity level and gradually increase activity tolerance. Control fluid volume deficit Prevent infection Promote weight gain Restrict activity 45 A client with COPD is prescribed to take ipratropium (Atrovent) via a metered-dose inhaler with spacer. The client asks the nurse why the spacer is necessary. The most accurate response by the nurse is that the spacer: Incorrect: The correct use of an inhaler with a spacer entails positioning the nebulizer in the mouth WITHOUT sealing the lips around it.Correct: Because large droplets of the aerosol fall on the walls of the spacer, and finer droplets disperse more fully within the spacer and can be delivered deeper into the airways, each dose is used more efficiently.Incorrect: Although it is not necessary to coordinate breathing as carefully as it is with the standard inhaler, a deep breath should be taken while releasing a puff of medication into the spacer.Incorrect: The metered dose inhaler delivers a prescribed dose into the spacer. The spacer itself does not determine the dose to be given. helps clients form a tight seal with the mouth. ensures each dose is used more efficiently. eliminates the need to coordinate breathing with the inhaler. delivers medication at a prescribed dosage. 46 A client is on ventilatory assistance in the intensive care unit. Which of the following measures should the nurse implement to prevent pneumonia in the intubated client? Incorrect: Aspiration pneumonia can be prevented by inflating the endotracheal or tracheostomy cuff before feeding.Incorrect: Family visitation is important to every client, especially those individuals in the intensive care unit. Visitation is often limited in this environment to promote rest for the acutely ill client; however, family visitation should not be restricted to once per shift for the purposes of preventing pneumonia. Rather, visitors should be screened for colds/flu that may be transmitted to the client and staff.Correct: Individuals requiring mechanical ventilation for 48 hours or more have a 10% to 20% chance of developing pneumonia. One method to diminish the risk is to drain condensation in the ventilator equipment into the designated reservoir, NOT back into the liquid reservoir, and by changing respiratory equipment every 24 hours.Incorrect: In the hospital environment, all tracheostomy and endotracheal airways should be managed using sterile technique. Maintain cuff deflation at all times. Restrict family visitation to once per shift. Drain tube condensation into the external reservoir. Use clean technique when suctioning. 47 Data related to which of the following assessments would be essential prior to administration of an aminoglycoside, such as Gentamicin? Correct: Because aminoglycosides are nephrotoxic and ototoxic, laboratory reports of renal function and hearing are essential baseline data. The most serious adverse reaction is nephrotoxicity. Risks of kidney damage can be minimized by detecting early signs of renal impairment, using cautiously in clients with impaired renal functionincluding the elderly-and keeping clients well hydrated.Incorrect: There are not serious pulmonary side effects to this category of drugs.Incorrect: The aminoglycosides are not known to cause cardiac or coagulation problems.Incorrect: Serum electrolytes and acidbase balance may be altered in the client who receives an aminoglycoside and experiences nephrotoxicity. However, the essential baseline data should be direct tests of renal function such as BUN and creatinine. Audiometry, BUN/creatinine Chest x-ray, pulmonary function tests Electrocardiogram, coagulation studies Serum electrolytes, arterial blood gases 48 For the client with chronic renal failure, one of the goals of diet therapy is to: Incorrect: Because potassium retention occurs in chronic renal failure due to reduction in the nephrons excretory ability, a diet low in potassium is recommended. This includes reducing intake of foods high in potassium such as citrus fruits, green leafy vegetables, and salt substitutes.Incorrect: Ample calories are required for growth and repair and should be obtained from carbohydrates and fats because they do not require renal excretion of metabolic by-products.Incorrect: Although sufficient calories are required for growth and repair of the kidney, too many calories can place an increased excretory demand on the kidney.Correct: A key goal of the diet for clients with chronic renal failure is reducing the quantity of metabolic waste that requires excretion by the kidney (i.e. protein). Therefore, protein intake is restricted to 1-1.5 g/kg of ideal body weight. This is sufficient to promote healing but also limits excretory demands on the kidney. increase the intake of foods high in potassium to promote electrolyte balance. limit carbohydrates and fats to reduce excretory demands. maximize caloric intake to promote healing. restrict protein intake to decrease metabolic waste. 49 A client is scheduled to have a thoracentesis to remove excessive pleural fluid. The nurse helps prepare the client for this procedure by explaining that: Incorrect: During a thoracentesis it is important to emphasize to the client the importance of NOT moving during the procedure to avoid damage to the pleura and lung. Therefore, sedation is not administered since the cooperation of the client is essential.Correct: Coughing is also avoided during the procedure to avoid damage to the pleura of the lung.Incorrect: Supplemental oxygen should NOT be discontinued during the procedure especially in the client who is having difficulty breathing.Incorrect: The best position to facilitate removal of pleural fluid is to have the client lean over the bedside table with the head and crossed arms resting on several pillows, and the feet supported by a footstool. a sedative will be given prior to the exam. coughing should be avoided during the procedure. oxygen is temporarily discontinued. positioning will involve lying on the affected side. 50 During a health assessment of a post-menopausal female, the nurse documents the client's complaint that she "frequently loses urine." The nurse suspects stress incontinence. Which additional information should the nurse gather? Incorrect: Alcohol generally acts as a diuretic and increases urine output. The exact nature of alcohol consumption is not relevant to the incidence of stress incontinence.Incorrect: Medications, such as hypnotics, tranquilizers, sedatives, and diuretics, are contributing factors to “urge” incontinence.Incorrect: Stress incontinence is seen primarily in women who have relaxed pelvic muscles. Diet has not been implicated in the etiology of incontinence.Correct: Stress incontinence involves a loss of 50 ml or less of urine following an activity that increases intraabdominal pressure on the bladder such as lifting, coughing, sneezing, or laughing. Alcohol consumption Current medications Diet history Precipitating factors 51 An emergency room nurse is asked to develop a plan of care for clients who experience eye trauma. Which intervention should be included in those plans? Incorrect: Irrigation with copious amounts of a nontoxic solution such as water or saline would be appropriate if the visible foreign object was a loose substance such as dirt or an insect, or if the client sustained a chemical burn to the eye. In the case of an embedded or penetrating object, it is essential that an ophthalmologist evaluate the client's eye before any treatment is initiated. Blindness could occur if the injury is mistreated.Incorrect: Penetrating objects should not be removed. The eye should be protected with a shield such as a paper cup, the uninjured eye should be covered to prevent excess movement of the injured eye, and medical assistance obtained.Incorrect: To avoid further trauma, both eyes are patched. A pressure dressing is avoided to prevent further trauma.Correct: It is important to establish a baseline and evaluate vision before initiating treatment (as well as after). The exception is chemical burns to the eye, in which case flushing with saline irrigations is begun immediately. Immediately irrigate all injuries with a saline solution. Gently remove any penetrating objects. Cover the injured eye immediately with a pressure dressing. Briefly assess visual acuity prior to treatment. 52 As part of the treatment plan for the client with gastroesophageal reflux disease (GERD), the physician has prescribed omeprazole (Prilosec). This drug acts primarily by: Incorrect: The prokinetic agents such as cisapride (Propulsid) act by enhancing GI motility.Incorrect: The prokinetic agents (i.e. Propulsid) increase strength of esophageal peristalsis and increase lower esophageal sphincter pressure to prevent reflux.Incorrect: Antacids are given to neutralize gastric acids or buffer it's effects.Correct: Omeprazole (Prilosec) is classified as a proton pump inhibitor and acts by inhibiting gastric parietal cells and suppressing gastric acid secretion by more than 90%. The histamine (H2) receptor antagonists such as cimetidine (Tagamet) and ranitidine (Zantac) also reduce gastric acid secretion. enhancing GI motility. increasing lower esophageal sphincter pressure. neutralizing gastric acid. suppressing gastric acid secretion. 53 The nurse is conducting a stop smoking clinic and includes a discussion of laryngeal cancer. Participants should be informed that a classic, early symptom of laryngeal cancer is: Incorrect: Signs of metastases of laryngeal cancer to other parts of the larynx include pain in the Adam's apple that radiates to the ear.Correct: Chronic hoarseness, especially in an individual who smokes is the most common presenting symptoms of laryngeal cancer. This is often associated with dysphagia. If treatment is initiated when hoarseness first appears a cure is usually possible.Incorrect: Enlarged cervical lymph nodes are considered late manifestations of laryngeal cancer as a result of metastases.Incorrect: Airway obstruction is a sign of advanced laryngeal cancer. pain in the ear. chronic hoarseness. enlarged cervical nodes. airway obstruction. 54 The nurse who provides health care maintenance care to a group of elderly women in a low-income apartment setting recognizes which assessment sign is related to the presence of osteoporosis in this population? Incorrect: The loss of appetite and muscle tissue wasting can occur in many disease states or use of various types of medications. Osteoporosis is a condition in which bone demineralization causes a reduction in bone density and mass.Correct: Osteoporosis is a common age-related metabolic bone disease in which there is reduced skeletal bone mass. The risk of fracture is caused by the bone fragility, especially in the hip, wrist and vertebrae. The clinical expression of post-menopausal osteoporosis may be the “dowager hump” and reduced height.Incorrect: A limitation in range of motion of the elbow and knee joints is most likely related to the pain associated with arthritic changes.Incorrect: An unstable gait and frequent falls signal neurological disease or stroke. Loss of appetite and wasting of muscle tissue Loss of height and a "humped" appearance to the upper back Inability to straighten the elbows and knees Unstable gait and frequent falls 55 In the client who is receiving a combination of furosemide and digoxin, the nurse should give high priority to assessing for digoxin toxicity when: Incorrect: These GI effects commonly occur with digoxin therapy. Although the presence of these symptoms raises suspicion of digitalis toxicity, many other conditions may cause anorexia and nausea. These symptoms may be side effects of other drugs such as diuretics. The priority assessment indicator is hypokalemia.Incorrect: Digoxin has a low therapeutic index. Concurrent treatment with other drugs affecting the heart, such as quinidine, verapamil, or nifedipine can contribute to digoxin toxicity. Opioids are not known to enhance digoxin toxicity.Incorrect: The desired effects of digoxin therapy are: a reduction in heart rate (negative chronotropic effect), and an increase in myocardial contractility (positive ionotropic effect). However, bradycardia may indicate digoxin toxicity.Correct: Electrolyte imbalances such as hypokalemia, hypomagnesemia, and hypercalcemia are known factors in promoting digoxin toxicity. The most common electrolyte disturbance is hypokalemia because potassium-losing diuretics are often given concurrently with digitalis preparations in the treatment of congestive heart failure. Hypokalemia increases cardiac excitability and increases the risk of digoxin toxicity. anorexia and nausea occur. given concurrently with opioids. pulse rate drops from 90 to 68 bpm. serum potassium falls. 56 Increased intracranial pressure (ICP) can occur due to a variety of diseases or injuries. Which physical assessment finding is an early sign of ICP in a client with a head injury? Correct: Increased intracranial pressure (ICP) is the pressure exerted in the cranium by the pressure of blood, edema, and impaired flow of cerebral spinal fluid (obstruction or infection.) The first and most sensitive indicators of ICP are the subtle changes in orientation and level of consciousness. Behavioral changes may include: restlessness, irritability, confusion, and decreased score on the Glasgow Coma Scale.Incorrect: The nurse may assess bradycardia and irregular respiratory pattern (Cheyenne Stokes) in the client in the later phases of increased intracranial pressure.Incorrect: The nurse may assess pupils that are fixed and dilated in the client experiencing the later phase of ICP. Sluggish papillary reactions or blurred vision occur in the earlier response to ICP.Incorrect: A sign that a client has developed ICP in an advanced phase is decreased motor activity or paralysis. Change in orientation and level of consciousness Bradycardia and tachypnea Fixed and dilated pupils Decreased motor activity or paralysis 57 Following a left, radical mastectomy the nurse assesses the wound and positions the left arm on pillows so that the hand is higher than the elbow and the elbow is higher than the shoulder. The primary reason this position is important is because it: Correct: This position prevents venous pooling in the hand and forearm by increasing venous return, promoting lymphatic flow, and prevent lymphedema. In the client who had a large number of lymph nodes dissected, lymphedema can occur and lead to infection. Clients must be taught how to prevent lymphedema through positioning and exercise.Incorrect: Elevating the arm would increase venous return - a desired goal in the management of lymphedema following radical mastectomy.Incorrect: Shoulder problems can occur if the client does not adhere to the prescribed exercise regimen. Performance of arm exercises helps restore full range of motion to the arm and shoulder, preventing a 'frozen shoulder' from lack of normal movement. However, the reason the arm is elevated is to promote lymphatic drainage.Incorrect: Although this position may enhance comfort, the primary reason for keeping the affected arm elevated is to promote lymphatic flow. enhances lymphatic drainage. decreases venous return. prevents shoulder subluxation. reduces pain. 58 In planning care for the client with renal calculi, the most appropriate outcome would be to expect the client to: Incorrect: Clients with renal stones typically are not febrile. However, the presence of renal calculi can lead to an increased risk for infection in susceptible individuals. Pain or renal colic is the primary symptom in an acute episode of renal calculi. Hematuria may be present if the stone has rough edges.Incorrect: An intake of 1000 mL daily is too low. Adequate hydration involves at least 2500 mL/day or more to help prevent urinary stasis that can lead to stone formation and UTI.Correct: Because stones can obstruct the ureters, the most important goal or outcome is to ensure urinary elimination by measuring I & O.Incorrect: The client may or may not need to acidify the urine based on the mineral composition of the stones. For example, phosphate calculi develop in alkaline urine, therefore prevention depends on keeping the urine acidic. On the other hand, uric acid stones tend to develop in acidic urine, therefore alkalinizing the urine is helpful. To facilitate treatment, a 24-hour urine collection is performed to determine urine pH and elements such as calcium, phosphorus, and uric acid levels. demonstrate a reduction in fever. consume at least 1000 mL of fluids/day. maintain urine output equal to intake. verbalize ways to acidify the urine. 59 The nurse teaches nursing assistants to recognize and notify the nurse when traction is interrupted for clients in Russell's traction. Which finding indicates a need to notify the client's nurse? Incorrect: As long as traction is maintained, the head of the bed may be elevated.Incorrect: The elevation of the foot of the bed may be used at times for counter traction.Correct: Russell's traction is a modification of Buck's traction. This type of traction adds a vertical pull by placing a sling under the leg above the knee. For effective use of traction, it is essential that the weights are hanging freely.Incorrect: The client is encouraged to move the unaffected extremities to reduce the risk of fat embolism syndrome, pressure-related skin injury, and muscle soreness. Head of the bed is elevated Foot of the bed is elevated Weights are not hanging freely Client is moving the unaffected leg 60 While a client is receiving a blood transfusion, the nurse continually assesses for the most common symptoms of a nonhemolytic transfusion reaction. These symptoms include: Correct: The characteristic symptoms of a febrile, nonhemolytic transfusion reaction are sudden chills and fever, headache, flushing and anxiety. This type of reaction occurs when the recipient becomes sensitized to the donor's WBC, platelets, or plasma.Incorrect: Urticaria, wheezing, and hypotension, chest tightness, and signs of shock are clinical manifestations of an anaphylactic reaction to blood components.Incorrect: Flushing, itching, and urticaria are typically symptoms of a mild allergic reaction to transfusion therapy caused by sensitivity of the recipient to foreign plasma proteins.Incorrect: Dyspnea, jugular vein distention, and hypertension are some of the signs/symptoms of circulatory overload that may occur if blood is given to rapidly or in the client with congestive heart or renal failure. sudden onset of chills and fever. urticaria, wheezing and hypotension. flushing, itching, and urticaria. dyspnea, jugular vein distention, and hypertension. 61 Immediately following the application of a cast to a client's fractured forearm, the nurse needs to closely monitor the: Incorrect. Although management of the airway and breathing are always the priority for care, no information is presented in the stem to suggest that the airway or breathing has been compromised at the time of the cast application.Incorrect. Nutritional status is not a priority for nursing care at the time of cast application, but will require attention later. The assessment of the color, movement of distal fingers and toes, swelling, pulses distal to cast, and sensation indicates adequacy of the neurovascular status of the extremity.Incorrect. The psychosocial response to injury is not a priority for the care of a client with a newly applied cast. The assessment of the color, movement of distal fingers and toes, swelling, pulses distal to cast, and sensation indicates adequacy of the neurovascular status of the extremity.Correct. A cast is a temporary device used for: 1) immobilization, 2) prevention or correction of a deformity, 3) bone realignment, or 4) promotion of healing, which allows for weight bearing and ambulation. Thorough assessment and prompt intervention are essential to prevent cast-related complications. The assessment of the color, movement of distal fingers and toes, swelling, pulses distal to cast, and sensation indicates adequacy of the neurovascular status of the extremity. client's airway and breathing. nutritional status of the client. client's psychosocial response to injury. neurovascular status of the injured arm. 62 A client arrives in the emergency department with an acute head injury suspected to be an intracranial hemorrhage. The nurse includes which intervention as a priority in the plan for care? Correct: The neurologic assessment (Glasgow Coma Scale) provides more data regarding the status of the client with acute head injury. The components of the scale includes: eye, motor and verbal response. The cranial nerve exam is performed in the assessment of the components: papillary response, extra-ocular movements, tracking, blink and gag reflexes, facial muscles, speech patterns, and any other pertinent neurologic findings.Incorrect: Measurement of the intake and output volumes is not priority care measures in the care of the client with a suspected intracranial hemorrhage. The neurologic assessment (Glasgow Coma Scale) provides more data regarding the status of the client with acute head injury.Incorrect: The vital sign assessment may change (bradycardia, abnormal respiratory pattern, increased systolic blood pressure and widened pulse pressure), however, subtle changes in level of consciousness usually precedes alterations in cardiorespiratory status.Incorrect: There may not be any external signs of bleeding with an acute head injury. Make frequent neurological assessments. Measure the client's intake and output. Monitor the client's vital signs frequently. Observe for signs of bleeding form the ears. 63 An adult client with cirrhosis of the liver has developed ascites. The serum sodium is 145 mEq/L and potassium is 3.2 mEq/L. Which of the following primary care provider orders should the nurse question? Incorrect: Although sodium restriction is often based on a 24-hour urine collection to determine sodium loss, sodium is generally restricted to 1 g (1000 mg) daily for clients with ascites.Correct: An intravenous infusion of 0.9% sodium chloride would be contraindicated in the client who is retaining sodium and water. This order should be questioned by the nurse.Incorrect: Fluids are restricted if hyponatremia is caused by fluid retention. A restriction of 1500 ml/24 hours is reasonable for the dilutional effect. A severe fluid restriction, coupled with diuretic therapy could lead to decreased output and renal failure.Incorrect: If bedrest and sodium restriction do not improve ascites, diuretics may be used. Spironolactone (aldactone) is often the first diuretic chosen because it promotes potassium retention. Note the client's K+ level is low, a common finding in clients with cirrhosis because aldosterone metabolism is impaired. Although thiazide diuretics may be used, they may worsen hypokalemia. 1000 mg of sodium per day. 0.9% NaCl to infuse IV at 50 cc/hr 1500 mL/24 hour fluid restriction Spironolactone 25 mg bid 64 While conducting an assessment for a client following a craniotomy, the nurse observes yellowish drainage on the dressing. The nurse should: Incorrect: Yellowish drainage should be immediately reported to the surgeon because it may indicate a cerebrospinal fluid (CSF) leak. After notifying the surgeon, the nurse should mark the drainage area with a pen in order to determine additional drainage at a later assessment.Incorrect: It would be inappropriate to delay reporting this finding to the surgeon since the yellow drainage may indicate leakage of CSF. Dressing reinforcement is generally appropriate when excessive drainage is expected and the original dressing is not to be removed. In this case, it would be important to evaluate the extent of drainage over time by marking the area on the original dressing and continue to observe.Incorrect: Surgeons generally have individual preferences regarding changing head dressings. Assessing the incision would not provide a further data regarding the yellow drainage. The presence of yellow drainage on a head dressing signals a possible CSF leak and should be immediately reported.Correct: Surgeons generally have individual preferences regarding changing head dressings. Assessing the incision would not provide a further data regarding the yellow drainage. Yellow drainage could signal a CSF leak and should be immediately reported. outline the drainage area and reassess in one hour. reinforce the dressing, document, and continue to observe. remove the dressing and assess the incision. report this finding immediately to the surgeon. 65 During a follow-up assessment after discharge from the hospital, a client diagnosed with epilepsy verbalizes to the nurse, "I'm constantly worried that I'll have a seizure and lose control. I'm afraid to go back to work or see my friends anymore." Which is the most appropriate nursing diagnosis for this client? Incorrect: The nursing diagnosis 'ineffective management of the therapeutic regimen” relates to the medication schedule and therapeutic drug levels and not the client's self-concept or adaptation to the illness.Incorrect: The nursing diagnosis “impaired verbal communication” relates to the expressive or receptive aspects of language. The client with epilepsy does not experience impairment to the language center except during the seizure event.Incorrect: The nursing diagnosis “risk for injury due to seizures” relates to the physical risk of injury during a seizure event. This situation pertains to the client's response to the condition and perceived self-concept as a result.Correct: The nursing diagnosis “self esteem disturbance related to the diagnosis of epilepsy” relates to the client's feelings and perceptions of self that has occurred as a result of the change in health status. Many clients who are diagnosed with epilepsy fear the onset of a seizure in a public setting. Ineffective management of therapeutic regimen Impaired verbal communication Risk for injury due to seizures Self-concept disturbance related to diagnosis of epilepsy 66 A client diagnosed with acute pancreatitis has a history of alcoholism and opioid abuse. Morphine 10-15 mg IV prn q 3-4 hours is ordered. Three hours after an initial dose the client is crying and asking for more morphine. Which intervention is indicated for the care of the client? Correct: The nurse should administer morphine. Nurses often fear giving prescribed analgesics will increase addiction and therefore under-medicate the client. Keeping the client in pain may actually contribute to a relapse of the addiction. In addition, it is common for the drug-addicted individual to require higher doses of analgesics than the average person.Incorrect: Placebos are unethical unless part of a research protocol where client consent has been obtained.Incorrect: Although nonpharmacological strategies are effective in diminishing the perception of pain; medication should not be withheld, especially when the request for the analgesic is within the prescribed time frame.Incorrect: Again, the client should not be penalized by withholding pain medication. The client should receive pain medication for only as long as s/he requires it. Administer morphine 15 mg as prescribed. Give a saline placebo. Substitute distraction techniques for opioid administration. Withhold the drug for another hour. 67 After administering a calcium channel blocker, which of the following desired outcomes does the nurse expect? Correct: Through coronary vasodilation, calcium channel blockers result in decreased frequency and severity of anginal attacks.Incorrect: Calcium channel blockers such as verapamil cause systemic vasodilation resulting in decreased blood pressure.Incorrect: The calcium channel blockers do not have any diuretic effect. It should be noted that these agents are contraindicated in clients with congestive heart failure since they may reduce contractility and cardiac output.Incorrect: Although calcium channel blockers have a vasodilating effect, they are not known to relieve the pain associated with arterial occlusion. Agents prescribed for intermittent claudication, such as pentoxifylline (Trental) improve blood flow by decreasing blood viscosity rather than by vasodilation. Decreased frequency and severity of angina Increased blood pressure Reduction in peripheral edema Relief of intermittent claudication 68 The nurse supervising care of clients with Alzheimer's disease in an adult day care identifies which of the following as the priority nursing diagnosis: Correct: The client's safety is always paramount to the plan of care. Because clients with Alzheimer's disease are prone to wandering, agitation, confusion, and seizures, risk for injury is high. Memory loss, impaired judgment, inability to make decisions, and decreased attention span all contribute to the risk for injury.Incorrect: The cognitive and biochemical changes in Alzheimer's disease affect personality and behavior. The client may begin to withdraw from friends and social events as memory impairments and personality changes become more apparent. While it is important for the nurse to minimize the impact of social isolation, the priority care concern is safety.Incorrect: In the early stages of Alzheimer's disease when memory and cognitive impairments are mild, clients may feel anxious and frustrated as they realize cognitive changes are occurring. As social interactions decrease, the client may feel alienated and powerless to do anything about it.Incorrect: Although this nursing diagnosis is extremely relevant to the care of clients with Alzheimer's disease, matters of safety take priority. One could argue that altered thought processes are the etiology of risk for injury, and that the diagnosis of altered thought processes is indeed a priority. However, the plan of care for the diagnosis of altered thought processes focuses primarily on promoting effective communication and reality orientation. safety due to memory loss and impaired judgment. social isolation due to diminishing social relationships. anxiety due to perceived powerlessness. altered thought processes due to dementia. 69 The biopsy report for the client after a colon resection indicates a grade 3, stage 3 adenocarcinoma. In planning care for this client, the nurse understands that the tumor: Correct: Grade 3 neoplasms are poorly differentiated (extensive structural changes from tissue of origin). Loss of differentiation means a higher degree of malignancy. Stage 3 lesions involve extensive local and regional spread.Incorrect: Well-differentiated neoplasms retain characteristics similar to the parent tissue and therefore are less invasive. This is characteristic of grade 1 lesions.Incorrect: Neoplasms that are localized without spread to adjacent tissue or other organs are classified as stage 2 lesions.Incorrect: Benign neoplasms are often encapsulated and therefore have limited growth potential. has metastasized to regional tissue. is similar to normal tissue and slow growing. was confined to the intestinal wall. was encapsulated and completely removed. 70 The nurse administers the MMR vaccine to a child in the health clinic. Which type of immunity will this child possess? Correct: Active artificial immunity is acquired through administration of antigens (vaccines or toxoids) to stimulate antibody production.Incorrect: Active natural immunity is acquired by the body's own efforts to form antibodies in the presence of active infection. An example is the individual who has had any of the childhood diseases such as chickenpox, measles, or the mumps.Incorrect: Passive artificial immunity is acquired by administering an antibody from an animal or another human. An example is administration of immune globulin to the person exposed to hepatitis B, or administration of tetanus immune globulin for prophylaxis against tetanus.Incorrect: Passive natural immunity is acquired when antibodies are transferred naturally from an immune mother to her baby through the placenta or in colostrum. Active artificial immunity Active natural immunity Passive artificial immunity Passive natural immunity 71 A 32-year-old female complains of having 10-12 diarrhea stools per day that contain bloody mucus and left-sided abdominal cramping prior to each stool. She states she has little desire to eat and has lost approximately 10 pounds in the last 2 weeks. Based on this data, which is the most likely cause of the client's symptoms? Incorrect: Cholecystitis is characterized by sudden onset of pain in the RUQ that often radiates to the right scapula or shoulder, and may be associated with eating a large or fatty meal. Bowel sounds may be decreased or absent and anorexia, nausea, and possibly vomiting may be present.Incorrect: Crohn's disease and ulcerative colitis are classified as inflammatory bowel disease. Although anorexia and weight loss often occur in both types of inflammatory bowel disease, symptoms of Crohn's disease differ from ulcerative colitis in that stools are large, semisolid, fewer in number (3-5/day), and rarely contain blood. Diffuse, colicky abdominal pain or localized pain in the right lower quadrant is characteristic of Crohn's disease. Symptoms may resemble those of appendicitis.Incorrect: The clinical manifestations of diverticulitis include crampy lower left quadrant pain, low-grade fever (a classic sign), feeling of bloating, nausea and vomiting.Correct: One of the distinguishing clinical manifestations between Crohn's disease and ulcerative colitis is bloody diarrhea. Clients with ulcerative colitis often experience profuse diarrhea (15-20 stools per day) containing a mixture of blood, mucus, and possibly pus. Left-sided abdominal cramping can be present prior to the bowel movement and is relieved by emptying the bowel. Significant losses of fluids and electrolytes can occur as well as weight loss. Cholecystitis Crohn's disease Diverticulitis Ulcerative colitis 72 A client inadvertently takes too many Coumadin tablets. The nurse anticipates the practitioner will order which of the following as an antidote? Incorrect: Acetyocysteine is the antidote for acetaminophen.Incorrect: Naloxone is the antidote for opioid analgesics.Incorrect: Protamine sulfate is the antidote for heparin.Correct: Vitamin K is the antidote for warfarin (Coumadin). Acetyocysteine Naloxone Protamine sulfate Vitamin K 73 The nurse is planning care for a client with hepatitis A. The nurse includes measures to prevent secondary transmission of the virus. Which intervention would most effectively achieve this goal? Correct: Hepatitis A virus is transmitted by the fecal-oral route, often through food contaminated by infected food handlers. Preventing spread of infection must include enteric precautions (wearing gloves when handling feces/urine).Incorrect: A private room is necessary only if the client cannot implement self-care measures for disposal of feces and urine (i.e. confusion, incontinence).Incorrect: Hepatitis B virus is transmitted through blood and body fluids.Incorrect: Contact precautions are used for clients known to have diseases easily transmitted by direct client contact. Contact precautions would be appropriate with hepatitis A in the client who is diapered or incontinent. Enteric precautions Private room Wearing gloves when handling blood Contact precautions 74 Which assessment data is essential to evaluate the effectiveness of oxygen therapy? Incorrect: Although the carbon dioxide level in arterial would be helpful information in evaluating the client's gas exchange and overall oxygenation status, it is not essential in evaluating O2 therapy. The PCO2 is a measurement of ventilation but is most essential in evaluating acid-base status since the PCO2 is the respiratory component in acid-base determinations.Incorrect: Although skin color is an important component in assessing tissue oxygenation, it is not a reliable indicator since pallor may be difficult to determine in clients with darker skin tones. The same is true in assessing cyanosis. Color changes must be assessed in a variety of places such as buccal mucosa, conjunctiva, lips, nail beds, and palate based on underlying skin tones.Correct: Either the PO2 or the oxygen saturation gives the most accurate information about arterial oxygenation. The PO2 is an indirect measure of O2 content of arterial blood. O2 saturation is an indication of the percentage of hemoglobin saturated with O2. Since the partial pressure of oxygen (PO2) is the driving force behind O2 saturation, both are useful in evaluating the effectiveness of O2 therapy. Pulse oximetry is a common method of measuring O2 saturation.Incorrect: Hemoglobin levels are essential to maximize the blood's oxygencarrying capacity since oxygen attaches to the hemoglobin molecule. However, the client's hemoglobin level does not provide data about the effectiveness of oxygen therapy. Arterial CO2 level Skin color Oxygen saturation Hemoglobin level 75 A client with a deep vein thrombosis has been receiving heparin therapy for two days. The morning APTT is 40 seconds. Which intervention should the nurse anticipate? Incorrect: The APTT value is at the low end of therapeutic range. In addition, the client has only been receiving heparin therapy for two days. A standard protocol calls for administration of a continuous infusion of heparin for at least 5 days.Correct: The normal control value for the activated partial thromboplastin time (APTT) is 25-35 seconds. During heparin therapy, the APTT should be maintained at about 1.5 to 2.5 times the control. Therefore, therapeutic values are 35-85 seconds. This client's APTT is at the low end of the therapeutic value. Thus, the most likely intervention would be to increase the heparin infusion rate.Incorrect: The normal control value for the activated partial thromboplastin time (APTT) is 25-35 seconds. During heparin therapy, the APTT should be maintained at about 1.5 to 2.5 times the control. Therefore, therapeutic values are 35- 85 seconds. The APTT value indicates the need for increasing the heparin rate to enhance therapeutic drug levels.Incorrect: Although the APTT is closely monitored throughout heparin therapy (i.e. approximately every 6 hours), there is no indication in this case for repeating the APTT before action can be taken. If the APTT value were extremely low or high a repeat value would be recommended. Discontinue drug therapy. Increase the heparin infusion rate. Maintain current heparin therapy. Repeat the APTT before any other action. 76 A nurse is observing a client who is being evaluated for possible appendicitis. During the diagnostic period, which intervention is appropriate? Incorrect: Enemas or laxatives may increase peristalsis and cause the appendix to rupture.Correct: To avoid masking critical changes in symptoms, pain medication is usually withheld until a definite diagnosis of appendicitis has been made.Incorrect: Heat should be avoided because the increased circulation to the appendix can lead to rupture.Incorrect: In preparation for possible surgery, the client is given nothing by mouth. Cleansing the GI tract with saline enemas in preparation for surgery Withholding analgesics until a diagnosis is established Applying heat to the right lower quadrant to promote comfort Restricting the client to clear liquids to reduce nausea 77 The home health nurse is working with a client who is in the convalescent phase after a cerebrovascular accident. Which statement by the client indicates to the nurse that further teaching regarding bowel training is needed? Correct: If a client indicates s/he frequently uses an enema more teaching is required. A bowel program of stool softeners, fiber laxatives, and suppositories is generally implemented to support bowel regularity. Enemas and harsh laxatives are avoided to prevent diarrhea and fluid and electrolytes imbalances.Incorrect: The client learned this concept well. Sufficient fluid intake, at least two liters daily, is necessary to maintain bowel patterns and promote proper stool consistency. Fiber without adequate fluid can aggravate bowel function.Incorrect: Incorporating the client's circadian rhythms into the bowel management program may be helpful in promoting defecation at a regular time.Incorrect: The client is adhering to an important aspect of bowel management. A well-balanced diet high in fiber stimulates peristalsis. "I find I need an enema almost every day." "I am drinking between six and eight glasses of fluid a day." "My care taker helps me use the toilet at 2 p.m. every day." "I have increased the fiber in my diet." 78 When planning an influenza immunization clinic, which of the following groups should be included because they are considered at high risk for flu and respiratory complications? Correct: The Advisory Committee for Immunization Practices (ACIP) recommends immunization against influenza for all persons at increased risk of adverse consequences from infection of the lower respiratory tract. This would include all persons older than 65 years of age, infants and children more than 6 months of age who are at increased risk for complications of influenza because of underlying medical conditions, and all health care workers.Incorrect: This age group is not considered in a high-risk category for serious consequences from infection of the lower respiratory tract.Incorrect: Children in general are not considered at high risk unless they have an underlying medical condition that places them at risk for adverse consequences from influenza.Incorrect: This age group is not considered by the ACIP as a high-risk group. Elderly residents of long term or chronic care facilities College students in athletic training season Children that spend 3 days a week or more in day care High school students who ride the bus to school 79 A client with a known history of alcoholism presents to the emergency department disoriented to time and place and vomiting dark emesis. The nurse realizes the first priority should be to: Correct: Esophageal varices can easily rupture causing excessive bleeding, hypovolemia, and shock. The client's disorientation and dark emesis suggest bleeding therefore assessment of vital signs is the first priority to evaluate hemostasis.Incorrect: Testing stool for blood is an appropriate assessment choice, however it would not be the first priority in the client exhibiting disorientation and dark emesis.Incorrect: Although esophageal tamponade may be required, other treatment measures are indicated especially if severe hemorrhage is not present. Gastric lavage and/or pharmacologic therapy using vasopressin may be tried initially.Incorrect: Checking prothrombin time would be important for monitoring the client's bleeding potential, which is often increased due to poor vitamin K absorption, impaired production of clotting factors, and thrombocytopenia. However, the priority intervention when bleeding is evident is to assess the client's hemodynamic status which includes pulse and blood pressure. assess pulse and blood pressure. obtain a stool specimen for guaiac. prepare the client for esophageal tamponade. perform phlebotomy to check prothrombin time. 80 A 55-year-old male suspected of having prostate cancer is admitted to the hospital. Which symptoms would be consistent with this diagnosis? Incorrect: These are clinical manifestations of testicular cancer. Signs/symptoms of testicular cancer are often subtle until the person notices a feeling of heaviness in the lower abdomen and groin. A painless lump or swelling may be present. Other nonspecific symptoms include weight loss, fatigue, and back pain.Correct: When the enlarged prostate gland impinges on the urethra, obstruction of urinary flow occurs. As a result, the bladder wall changes in contour creating pockets for urinary retention. Consequently the bladder has less capacity, muscle tone diminishes, and the bladder cannot empty completely at each voiding, and urinary stasis creates a fertile medium for bacterial growth and infection. Symptoms include urinary hesitancy, difficulty starting the stream, retention, nocturia, dysuria, urgency, and symptoms of UTI.Incorrect: A combination of hematuria, bilateral flank pain, fever, and pyuria is characteristic of adult polycystic kidney disease. Cysts are usually bilateral and diffusely scattered throughout the renal parenchyma causing pain, hematuria, and cyst infections.Incorrect: These are common clinical manifestations of epididymitis, a common inflammatory process most often caused by an ascending infection via the ejaculatory duct through the vas deferens into the epididymis. Back pain, painless testicular swelling, and weight loss Dysuria, frequency, urgency, hematuria, nocturia, and retention. Hematuria, bilateral flank pain, fever, and pyuria Scrotal pain and swelling, urethral discharge, and low-grade fever 81 Which symptom of Candida albicans, an opportunistic disease, is an early indication of human immunodeficiency virus (HIV) disease? Incorrect: Floaters, decreased vision and blindness are symptoms of Cytomegalovirus (CMV) retinitis. This is the most clinically significant type of infection in clients with HIV infection.Incorrect: Nodular lesions of the skin are likely to be Kaposis sarcoma. This common assessment finding is evident on the external skin surfaces.Incorrect: Fever, night sweats and chronic cough are symptoms of Pneumocystis carinii pneumonia. This respiratory complication is the most common life-threatening infection in clients with AIDS.Correct: Whitish-yellow patches in the mouth are characteristic of candidiasis. This secondary fungal infection, commonly caused by candida albicans, thrives in a warm, moist environment, such as the mucous membranes of the mouth, vaginal or intestinal tract. The opportunistic infection occurs frequently in the immunocompromised host, such as the client with AIDS. Floaters, decreased vision, and blindness Nodular lesions on the skin Fever, night sweats, and chronic cough Whitish-yellow patches in the mouth 82 Assessing a client with osteoarthritis, the nurse recognizes that the most common clinical manifestation of the disease is: Incorrect: Rheumatoid arthritis (RA) is a chronic, systemic, progressive, inflammatory connective tissue disorder. It affects primarily the small, peripheral joints with symmetrical distribution. This systemic disease affects all connective tissue, including the collagen of the heart, muscles, tendons, pleura or blood vessels. As the disease destroys the joints, the client experiences pain, stiffness, redness, warmth and swelling to the joints.Correct: Osteoarthritis is a non-inflammatory joint disease characterized by degeneration and loss of articular cartilage in synovial joints. This disease is not associated with chemical or metabolic degeneration as there is in rheumatoid arthritis. Pain upon movement of the involved joints accompanies osteoarthritis.Incorrect: Rheumatoid arthritis (RA) is a chronic, systemic, progressive, inflammatory connective tissue disorder. It affects primarily the small, peripheral joints with symmetrical distribution. This systemic disease affects all connective tissue, including the collagen of the heart, muscles, tendons, pleura or blood vessels. During the acute onset of rheumatoid arthritis, the client experiences fever and chills, pain and swelling of the joints. When RA develops insidiously, morning stiffness may occur as an early symptom.Incorrect: Rheumatoid arthritis is a chronic, systemic, progressive, inflammatory connective tissue disorder. It affects primarily the small, peripheral joints with symmetrical distribution. This systemic disease affects all connective tissue, including the collagen of the heart, muscles, tendons, pleura or blood vessels. The erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP) are usually elevated during the acute and chronic states of rheumatoid arthritis. reddened, swollen joints that are warm to the touch. pain upon movement of the involved joints. morning stiffness and fever. an elevated erythrocyte sedimentation rate (ESR). 83 A nurse has reviewed the cardiac enzyme studies of a client with unstable angina who was recently admitted to the cardiac care unit. The client's creatine kinase (CK) is elevated. The nurse can anticipate that further diagnostic studies to help clarify the client's cardiac injury will be: Incorrect: Serial blood pressure readings provide important information in the diagnosis of hypertension. Serial blood pressure readings are not used as a diagnostic tool to identify degree of myocardial injury and necrosis. Although the blood pressure is directly affected by myocardial damage if cardiac output is reduced, successively low or high pressures would not tell the physician any direct information about myocardial cell injury or death.Incorrect: Central venous pressure monitoring, although helpful in monitoring fluid status would not provide diagnostic information about the client's cardiac injury.Incorrect: A stress test is an important diagnostic tool in clients with stable angina. Client's experiencing unstable angina would be at increased risk for an acute MI if subjected to exercise stress testing.Correct: CK-MB is the isoenzyme specific to the myocardium and elevation begins within 4-8 hours after an acute MI. Cardiac troponin has a high specificity for myocardial injury and rises earlier than CK-MG. Both are important indicators of myocardial cell damage. serial blood pressure readings. central venous pressure monitoring. a treadmill stress test. isoenzyme and troponin I levels 84 When assessing a client for fluid and electrolyte imbalances, the nurse knows that a common cause of iso-osmolar fluid volume deficit (hypovolemia) is: Correct: Excess blood loss involves fluid and solute loss from the vascular space. These losses occur in proportion to one another, therefore the loss is isotonic in nature.Incorrect: A decrease in water intake results in an increase in the number of solutes in body fluid. The vascular space becomes hyperosmolar.Incorrect: Although vomiting and diarrhea usually result in fluid losses that are in proportion to electrolyte losses, severe vomiting and diarrhea cause a loss of body water greater than the loss of solutes such as electrolytes, resulting in hyperosmolar body fluid.Incorrect: Pure water losses, as occurs in diabetes insipidus, result in concentration of the solutes in the vascular space and hyperosmolarity. hemorrhage. inadequate fluid intake. severe vomiting and diarrhea. water losses with diabetes insipidus. 85 The nurse is caring for a male client who is using home peritoneal dialysis to manage chronic renal failure. The client informs the nurse that today the fluid returning after the instillation of the dialysate was cloudy. This is usually a sign of: Incorrect: Displacement would likely result in little to no return of the dialysate.Incorrect: Peritoneal dialysis works on the principle of osmosis to cause movement of extra fluid from the client into the dialysate. This process should not alter the appearance of the dialysate. A cloudy dialysate return should prompt the nurse to consult the physician since peritonitis may be present.Incorrect: The purpose of dialysis, whether peritoneal or hemodialysis is to remove waste and toxic material from the body. The presence of nitrogenous waste products in the dialysate will not alter the color or clarity of the solution. Any time the dialysate is cloudy in appearance, peritonitis should be suspected.Correct: Peritonitis is a major threat during peritoneal dialysis. Peritonitis is recognized by a fever, chills, abdominal tenderness or pain, vomiting, cloudy outflow of solution. displacement of the dialysis tube. fluid volume deficit. excess nitrogenous wastes. peritonitis. 86 When assessing a client with iron deficiency anemia, which of the following set of signs/ symptoms, if present, would coincide with this diagnosis? Incorrect: These clinical manifestations are characteristic of anemia secondary to acute blood loss.Correct: These are the classic symptoms of iron deficiency anemia often associated with chronic blood loss, inadequate iron intake or malabsorption. The hallmark of iron deficiency anemia is hypochromia, which is small red blood cells that are devoid of pigment. Clients with iron deficiency anemia often experience a generalized fatigue as related to diminished oxygen carrying capacity of the hemoglobin.Incorrect: These signs/ symptoms are indicative of hemolytic anemia often caused by drugs or an autoimmune response against the person's RBCs.Incorrect: These signs/symptoms correlate with disorders of coagulation such as hemophilia or thrombocytopenia, or may be found in clients with aplastic anemia along with the usual manifestations of anemia such as fatigue, exertional dyspnea and pallor. Hypotension, weakness, tachycardia Hypochromia, bright red tongue, fatigue Jaundice, pallor, splenomegaly Easy bruising, petechiae, infection 87 During a counseling session, the client scheduled for a radical prostatectomy asks the nurse how the surgery will affect sexual function. The nurse's response should be based on that fact that: Incorrect: Although clients are not able to ejaculate, the ability to have an erection and to experience orgasm will gradually return following radical prostatectomy.Incorrect: Aside from fertility, most aspects of sexual function will gradually return. However, clients may be impotent for several months even after a nerve-sparing prostatectomy. It would be inappropriate to assure the client that sexual function will be completely normal.Incorrect: The return of erectile capability may be delayed following total prostatectomy but the ability to have an erection will gradually return for most clients.Correct: Following any type of radical prostatectomy, the male will no longer be fertile, because the loss of the prostate gland interrupts the flow of semen and ejaculation will not occur. achieving orgasm will be impossible. all aspects of intercourse should return to normal. impotence is a permanent outcome. infertility will occur. 88 An adult client is admitted with dehydration caused by severe diarrhea. Blood pressure is 98/68, pulse 110/minute, respirations 20/minute. In the initial stages of fluid replacement, which intravenous solutions would be the best choice? Incorrect: Dextrose 5% in water is considered an isotonic solution in the container. However, the glucose is quickly metabolized in the body leaving free water, which is hypotonic. Hypotonic solutions cause water to move into the cell. Although considered a hydrating solution would not be the best FIRST choice in this situation because the client is hypotensive. The best solution to expand the vascular space is an isotonic solution such as 0.9% NaCl which is considered the isotonic standard (approximately equal to the sodium chloride concentration of the blood). It should also be noted that the free water in D5W could dilute the serum sodium level, which has been lowered by sodium and water losses from the severe diarrhea.Incorrect: A hypotonic solution such as .45% sodium chloride is useful for daily maintenance of body fluid but not for replacement therapy. Because it is hypotonic it is not the best choice for initial IV therapy in the client who is hypotensive.Correct: Because the client is hypotensive, the first objective is to raise the ECF volume. This is best achieved by using an isotonic solution such as .9% sodium chloride. Once the client's blood pressure is improved, other hydrating solutions such as Dextrose 5% in .45% sodium chloride would be given to hydrate the cell and provide calories and sodium which has been lost.Incorrect: An extremely hypertonic solution, such as 3% or 5% sodium chloride, is contraindicated in this situation. A hypertonic solution would draw water out of the cells causing further dehydration and could cause severe cerebral damage. Hypertonic saline is used when treating a client with severe hyponatremia. Dextrose 5% in water .45% sodium chloride .9% sodium chloride 3% sodium chloride 89 While setting up total parenteral nutrition (TPN) for a client, the nurse performs which intervention to prevent fluid and electrolyte imbalance? Incorrect: When infusing TPN the nurse should maintain a uniform infusion rate to prevent hypo or hyperglycemia or other fluid/electrolyte imbalances. The nurse closely monitors blood sugar throughout TPN therapy and the practitioner makes solution adjustments.Incorrect: The nurse's responsibility is to monitor for signs/symptoms of fluid and electrolyte imbalances and notify the physician who will make solution adjustments (i.e. reduce the potassium content if signs of hyperkalemia are present). Discontinuation of TPN is done gradually to prevent hypoglycemia.Incorrect: As described above, a uniform infusion rate should be maintained to prevent changes in blood glucose, which can occur rapidly if the infusion rate were to be increased or decreased.Correct: A safeguard against too rapid infusion of any IV solution is to use an infusion pump. In addition, it is equally important to continue to check the flow rate hourly and not assume that the pump is functioning properly. Adjust the flow rate based on finger stick glucose levels. Discontinue the infusion if signs of electrolyte imbalances occur. Reduce the flow rate if signs of overhydration develop. Set up an infusion pump and check the flow rate hourly. 90 During a home visit to an elderly client with glaucoma, the nurse evaluates the client's understanding of the use of eyedrops. Which statement, if made by the client, would indicate additional teaching is required? Incorrect: The client has described the proper technique for instilling ophthalmic drops or ointments.Incorrect: The client's wife understands the importance of safety. The use of miotic drugs causes pupil constriction and may adversely affect the client's night vision and adaptation to dark environments.Correct: This statement by the client indicates more teaching is required. There is no cure for glaucoma but it can be controlled. Blindness can be prevented by early detection, life-long treatment, close monitoring and follow-up care. Vision that has been lost to elevated intraocular pressure cannot be restored, but further loss can be prevented.Incorrect: The client understands the importance of avoiding increased pressure in the eye. Clients with glaucoma should avoid activities that increase intraocular such as bending from the waist, sneezing, vomiting, and straining to have a bowel movement. "I should pull my lower eyelid down and place the drop/s onto the lower lid." "My wife makes sure I do not drive after dark." "I'm glad I can stop taking this medicine when my vision improves." "I have been careful to avoid becoming constipated." 91 A client with a tracheostomy tube on mechanical ventilation suddenly becomes restless and anxious and attempts to cough. The high-pressure alarm sounds on the ventilator. The first action the nurse should take is: Incorrect: Although clients who are excessively anxious and fight the ventilator may be sedated or given a paralyzing agent, sources of the client's anxiety should be determined and addressed. In this case, behavior suggests the need for airway clearance.Incorrect: It is important to empty water from the ventilator tubing to prevent bacterial growth and pneumonia. However, the client's anxiety and attempts to cough in addition to the high-pressure alarm strongly suggest secretions in the airway. Suctioning should occur first. It would also be important to check the tubing for kinks or excessive water that could also sound the high-pressure alarm.Incorrect: An x-ray is not indicated in this situation. However, it may be appropriate to evaluate the position of an endotracheal tube; if displaced it could also cause the high-pressure alarm to sound.Correct: The highpressure alarm sounds when peak inspiratory pressure reaches the set alarm limit; indicating secretions in the airway or a mucous plug. Since the client is restless, anxious, and attempting to cough, the first nursing activity is to suction the tracheostomy tube. administer an antianxiety agent. empty water from the ventilator tubing. obtain a chest x-ray. suction the tracheostomy tube. 92 A 48-year-old male had a bronchoscopy with tissue biopsy 30 minutes ago. The client calls the nurse and reports the following symptoms. Which one should prompt the nurse to immediately notify the practitioner? Incorrect: Blood-streaked sputum may occur following a tissue biopsy. However, frank bleeding should be immediately reported.Incorrect: Because of the local anesthetic sprayed on the tongue and oropharynx, difficulty swallowing is expected until cough and gag reflexes return.Correct: Following a bronchoscopy it is essential that the nurse monitor for frank bleeding, laryngeal edema or laryngospasm (stridor) and increasing shortness of breath. These symptoms may indicate trauma to the larynx or vocal cords.Incorrect: A moderate amount of throat discomfort is expected following a bronchoscopy and should be managed with warm saline gargles once the client is able to effectively swallow. Blood-streaked sputum Difficulty swallowing Progressive dyspnea Throat discomfort 93 Which classification of medication is primary in the treatment of congestive heart failure because of its ability to increase the force and strength of the cardiac contraction and slow the heart rate? Incorrect: Although beta-adrenergic agonists such as isoproterenol (Isuprel) enhance myocardial contraction, they cause cardiac stimulation and increase the heart rate.Incorrect: Morphine sulfate is a narcotic analgesic used to decrease pain. It is also important in the treatment of pulmonary edema because it eases dyspnea and reduces preload (vasodilator effect).Incorrect: Diuretics are also primary drugs in the treatment of congestive heart failure but are given to increase excretion of sodium and water from the body.Correct: Digitalis preparations such as digoxin (Lanoxin) are classified as positive inotropic agents that work by increasing the force and strength of myocardial contraction. In addition, digitalis is a negative chronotropic drug (slows the cardiac rate). Beta-adrenergic agonists Narcotic analgesic Diuretics Digitalis preparations 94 A 68-year-old male client has a permanent tracheostomy tube following total laryngectomy. The most appropriate goal for the first postoperative day would be for the client to: Incorrect: Although early ambulation is advocated in most all post-operative clients to prevent atelectasis and paralytic ileus, it would be unrealistic and perhaps dangerous to expect the laryngectomy client to ambulate independently the first postoperative day.Correct: Some degree of airway obstruction is common in clients following laryngectomy related to edema from surgery or radiation prior to the surgery. A patent airway is a priority outcome immediately postop and it is reasonable to expect the client will assist in coughing and mobilizing secretions through the tracheostomy tube or laryngeal stoma.Incorrect: A nasogastric tube is used for food and fluids to minimize contamination of the pharyngeal and esophageal suture lines and to prevent fluid from leaking through the wound into the trachea before healing occurs.Incorrect: The laryngectomy patient, although very anxious following surgery, will be unable to verbalize because the larynx (vocal cords) have been removed. Communication can however be facilitated using other techniques. ambulate independently. help maintain a patent airway. consume oral fluids without aspirating. verbalize fear and anxiety. 95 Of the following individuals, who is at increased risk for developing acute renal failure (ARF) from a prerenal cause? The person who: Incorrect: Postrenal failure is caused by obstruction of urine flow between the kidney and urethral meatus as in such conditions as renal calculi, neoplasms, and prostatic hypertrophy.Incorrect: Intrarenal failure is caused by damage to the kidney tissues and structures and includes tubular necrosis, nephrotoxicity, and alteration in renal blood flow. Examples of intrarenal causes include glomerulonephritis, coagulopathies, malignant hypertension, nephrotoxic drugs such as gentamicin (an aminoglycoside), antiinflammatory agents, tetracyclines, and sulfonamides.Correct: Prerenal causes of ARF occur secondary to intravascular volume depletion. Examples of conditions leading to hypovolemia include hemorrhage, dehydration, diabetes insipidus, cirrhosis, excessive use of diuretics, burns; Conditions that lead to decreased cardiac output such as congestive heart failure and dysrhythmias are other prerenal causes of ARF.Incorrect: Nephrotoxic drugs such as the aminoglycosides are classified as intrarenal causes of acute renal failure. frequently develops kidney stones. has a coagulation disorder. hemorrhages during surgery. is receiving an aminoglycoside. The most common complication after a myocardial infarction (MI) is: Incorrect: Cardiogenic shock is caused by severe myocardial dysfunction and occurs in 5% to 10% of clients with acute myocardial infarction. Although serious and potentially fatal, the most common complication after an MI is dysrhythmias.Incorrect: Although ventricular aneurysms can develop following myocardial infarctions involving the entire myocardium, they are rare.Incorrect: Free wall rupture of a weakened area of the myocardium can occur but is very rare.Correct: Dysrhythmias often occur secondary to the ischemic processes of coronary artery disease and myocardial infarction. In addition to blocks along the conduction pathway, direct damage to the myocardial cell can cause electrolyte imbalances that alter the action potential, creating a variety of dysrhythmias. shock. ventricular aneurysms. rupture of the ventricular wall. dysrhythmias. 97 The nurse is caring for a client with Type 2 diabetes mellitus. The client's nutritional history indicates a diet high in carbohydrates and moderately sedentary lifestyle. The nurse notes the client is 5 feet, 4 inches and weighs 160 pounds. In planning nutritional management the nurse knows that: Incorrect: This client's height and weight indicate that she is overweight. A caloric increase would be inappropriate especially since this client's activity level is light.Incorrect: A common misconception in diabetes management is that carbohydrates (CHO) be restricted. Carbohydrates must be distributed on a consistent basis so that blood nutrients match insulin levels. Distribution of CHOs helps prevent increases in blood glucose following meals, and allows the blood glucose to return to pre-meal levels before the next meal. Clients who need to reduce weight are taught to maintain balanced intake of fat, CHO, and proteins but to reduce total calories.Correct: Weight is a major factor in monitoring diabetes control. Attaining and maintaining ideal body weight are major criteria in diabetes management. A large percentage (80-90%) of persons diagnosed with type 2 diabetes are overweight. The current nutritional management for diabetes is to maintain reasonable weight and control blood glucose without compromising health.Incorrect: Although obesity is a significant risk factor for type 2 diabetes, dietary management and weight loss is usually not sufficient to control blood glucose levels in the client diagnosed with type 2 diabetes. Many clients with type 2 diabetes require oral hypoglycemics to help decrease insulin resistance or augment insulin secretion. an increase in caloric intake is recommended. carbohydrates should be restricted. weight reduction is an important goal for care. diet alone is probably sufficient for glucose control. 98 An elderly client with a diagnosis of congestive heart failure complains of paroxysmal nocturnal dyspnea. Which nursing actions is most appropriate for the nurse to institute? Correct: Paroxysmal nocturnal dyspnea occurs 2-5 hours after the client lies down because chest expansion diminishes in the recumbent position resulting in decreased ventilation, and venous return to the right heart increases with elevation of the legs. The client awakes suddenly with severe shortness of breath that subsides only after sitting upright for 10-30 minutes. Clients experiencing orthopnea must sleep using several pillows or in a semi-Fowler's position.Incorrect: Increasing oxygen delivery will not eliminate the problem of orthopnea or nocturnal dyspnea that occurs when the legs are elevated to the level of the heart and venous return is increased causing increased fluid in the lungs. The most appropriate nursing measure is to elevate the head of the bed.Incorrect: Although bedrest decreases the workload of the failing heart, bedrest without elevation of the head of the bed will not diminish the problem of orthopnea or nocturnal dyspnea.Incorrect: Restricting fluids may or may not be indicated. If the client is currently receiving diuretics, a fluid restriction may be contraindicated to avoid fluid volume deficit. The increase of fluid returning to the lungs when lying in a supine position with the legs elevated can best be averted by elevating the head of the bed. Elevate the head of the bed. Increase O2 to 6 L per nasal cannula. Institute strict bedrest. Restrict fluids for the next 24 hours. 99 A client diagnosed with myasthenia gravis is brought to the emergency department with severe dyspnea, exaggerated muscle weakness, and dysphagia. To determine whether these symptoms are the result of cholinergic versus myasthenic crisis, the physician administers the Tensilon test. Of the following drug responses, which would indicate to the nurse that myasthenic crisis is present? Incorrect: Myasthenia gravis involves a decrease in the number and effectiveness of acetylcholine receptors at the neuromuscular junction resulting in progressive muscle weakness. Myasthenic crisis represents an exacerbation of the symptoms caused by undermedication with anticholinesterase drugs. In contrast, cholinergic crisis is an exacerbation of muscle weakness caused by overmedication. Tensilon (a short-acting anticholinsterase) produces a temporary improvement in myasthenic crisis but no improvement or worsening of symptoms in cholinergic crisis. Therefore, improved breathing would be expected if the client were in myasthenic crisis.Incorrect: In cholinergic crisis, muscle tone does not improve after administration of Tensilon. Instead, weakness increases and muscle twitching may be observed around the eyes and face.Correct: As explained above, clients who are experiencing myasthenic crisis respond positively to the Tensilon test with a temporary improvement in muscle tone.Incorrect: Improvement in the ability to swallow following Tensilon administration would be expected if the client were in myasthenic crisis. Breathing remains unchanged Facial twitching occurs Muscle strength briefly improves Dysphagia worsens 100 When differentiating between wound inflammation and wound infection, the nurse determines that a 2-day-old surgical incision is likely to be inflamed based on which physical assessment data? Correct: Tissue redness (erythema), slight swelling (edema) and increased warmth are signs of wound inflammation. Fever, purulent drainage, and tachycardia indicate infection.Incorrect: Pain and drainage may be normal at an incisional site and are not a sign of inflammation.Incorrect: Adhesions may form after wound healing has occurred. Purulent drainage is a sign of wound infection.Incorrect: Fever, tachycardia (increased heart rate) and tachypnea (increased respiratory rate) are signs of infection. Erythema, slight edema, and increase warmth Pain at the surgical site and drainage Adhesions and purulent drainage Fever, tachycardia, and tachypnea [Show More]
Last updated: 1 month ago
Preview 1 out of 44 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 21, 2020
Number of pages
44
Written in
Additional information
This document has been written for:
Uploaded
Dec 21, 2020
Downloads
1
Views
100