*NURSING > EXAM REVIEW > Chamberlain College of Nursing NR 224 Exam 2 Review (All)
Chamberlain College of Nursing NR 224 Exam 2 Review
Document Content and Description Below
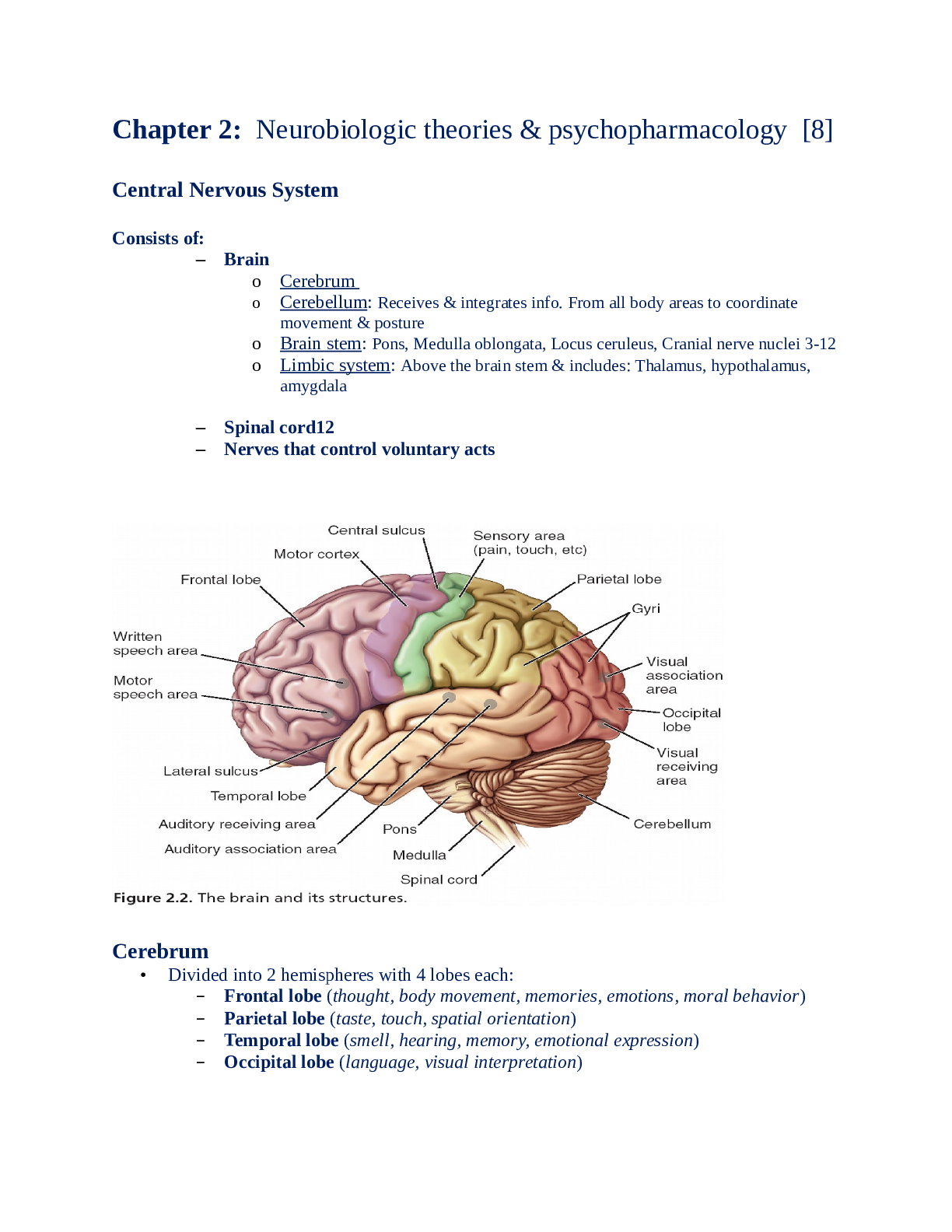
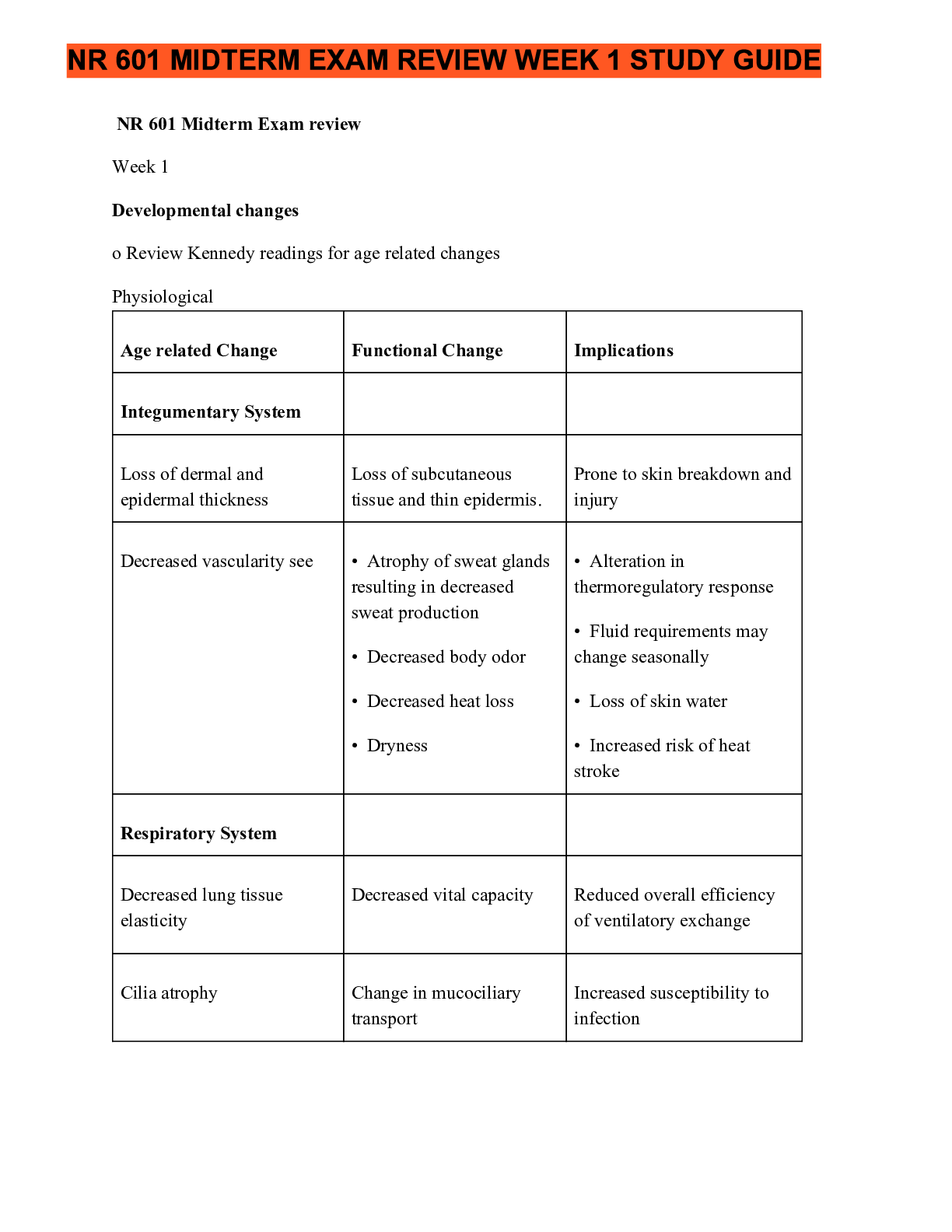
Chapter 48 Skin Integrity and Wound Care Skin: Two layers-epidermis and dermis -Separated by membrane, referred to as dermal epidermal junction -Epidermis: top layer, several layers -Dermis: inner... layer of skin, provides tensile strength, mechanical support, and protection to the underlying muscles, bones, and organs. (Contains mostly connective tissue and few skin cells) Collagen: tough, fibrous protein Pressure Ulcers -Pressure sore, decubitus ulcer, and bedsore -Localized injury to the skin and other underlying tissue, usually over a bony prominence -Result of pressure or pressure in combination with shear and/or friction -Decreased mobility, decreased sensory perception, fecal or urinary incontinence, and/or poor nutrition are at risk for PU development. Cause of PU -Tissue receive oxygen/nutrients and eliminate metabolic wastes via the blood. -Interference of blood flow disrupts cellular metabolism and function/life of cells. -Prolonged pressure affects cellular metabolism by decreasing or obliterating blood flow, results in tissue ischemia and ultimately tissue death. Pathogenesis of Pressure Ulcers -Three pressure-related factors contribute to PU development -Pressure intensity: pressure applied over a capillary exceeds the normal capillary pressure, vessel is occluded for prolonged period of time, tissue ischemia can occur. Leads to tissue death if patient cannot respond to discomfort. -Pressure duration: Low pressure over prolong period and high-intensity pressure over short period of time are two concerns related to duration of pressure. Check affected areas for blanching. -Tissue intolerance: ability of tissue to endure pressure depends on integrity of tissue and supporting structures. Shear, friction, and moisture affect ability of skin to tolerate pressure. Greater the degree to which factors shear, friction, and moisture, more susceptible skin will be to damage. -Underlying skin structures (blood vessels, collagen) assist in redistributing pressure. Systemic factors such as poor nutrition, increased aging, hydration status, and low blood pressure affect tolerance of the tissue to externally applied pressure. Blanching: occurs when normal red tones of the light-skinned patient are absent Blanching Hyperemia: if an affected area blanches (turns light in color) and the erythema returns when you remove your finger, hyperemia is transient and is an attempt to overcome the ischemia episode. Risk Factors for PU developmentImpaired Sensory Perception: altered sensory perception for pain and pressure are more at risk for impaired skin integrity than those with normal sensation. Unable to feel when a portion of body undergoes increased, prolonged pressure/pain Impaired Mobility: Cannot change positions, at risk for PU Alteration in Level of Consciousness: Confused/disoriented/expressive aphasia/other inability to verbalize are unable to protect themselves from PU -May not understand how to relieve or communicate discomfort -Coma patients Friction: Force of two surfaces moving across one another (mechanical force exerted when skin is dragging across coarse surface) -Affect epidermis or top layer of skin. Skin appears red and painful “sheet burn” Moisture: reduces the resistance of skin to other physical factors such as pressure and/or shear force -Soften skin, susceptible to damage Shear Force: sliding movement of skin and subcutaneous tissue while the underlying muscle and bones are stationary -Shear force occurs when head of bed is elevated and sliding of the skeleton starts but the skin is fixed because of friction of bed. -Bed must be in limited 30 degree angle or less, use draw sheet or lift sheet to position patient Classification of Pressure Ulcers Stage I: Nonblanchable Redness of Intact Skin -Nonblanchable erythema localized area over bony prominence -Discoloration of skin, warmth, edema, hardness, pain. -Does not require dressing Stage II: Partial-thickness Skin Loss or Blister -Partial thickness loss of dermis -presents shallow open ulcer with red-pink wound bed -open/ruptured serum-filled or serosangineous filled blister -shiny or dry shallow ulcer without slough/bruising -Looks like open cradle with wound bed Stage III: Full-thickness Skin Loss (Fat Visible) -Full thickness tissue loss -subcutaneous fat may be visible, but bone tendon, or muscle is not exposed -some slough, may include undermining/tunneling -takes some time to heal -purulent drainage and odor, call doctor and perform SBAR (Situation, Background, Assessment, Recommendation) Stage IV: Full-thickness Tissue Loss (Muscle/Bone Visible) -Full thickness tissue loss (bone/muscle visible) -Slough or eschar may be present -often includes undermining and tunneling-Suspected deep-tissue injury, purple or maroon localized area of discolored intact skin or blood filled blister caused by damage of underlying soft tissue from pressure and/or shear Unstageable/Unclassified: Full-Thickness Skin or Tissue Loss-Depth Unknown -Base of wound cannot be visualized and tissue injury in which the depth of injury is unknown. -Full-thickness tissue loss which actual depth of ulcer is completely obscured by slough (yellow, tan, gray, green, or brown) and/or eschar (tan, brown, or black) in the wound bed -Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels serves as “the natural (biological) cover of the body” and should not be removed. Suspected Deep-Tissue Injury-Depth Unknown -Purple or maroon localized area of discolored intact skin or blood-filled blister caused by damage of underlying soft tissue from pressure/sheer -Tissue may be painful, firm, mushy, boggy, warmer, or cooler than adjacent tissue -For dark-skinned patients proper lighting is important to accurately assess the skin Risk for Skin Breakdown from Body Fluids Low Risk: Saliva, serosanguineous drainage Moderate Risk: bile, stool, urine, ascetic fluid, purulent exudate High Risk: gastric drainage, pancreatic drainage Bony Prominences -Elbow, heel, sole, ear, shoulder, thigh, lateral knee, lower leg, posterior knee, scapula, occipital bone, iliac crest, sacrum, ischium, achilies tendon. Factors Influencing Pressure Ulcer Formation and Wound Healing Nutrition: Physiological process of wound healing depend on the availability of protein, vitamins (A and C) and trace minerals zinc and cooper -At least 1500 calories per day Tissue Perfusion: oxygen fuels the cellular functions essential to the healing process, critical for wound healing -pumping of oxygen to wound site Infection: prolongs inflammatory phase -Delays collagen synthesis, prevents epithelialization, and increases the production of proinflammatory cytokines, leads to additional tissue destruction -Change in odor, purulent drainage, volume, character of wound drainage, redness of tissue, fever, or pain Age: increased age affects all phases of wound healing -Decrease macrophages leads to delayed inflammatory response, delayed collagen synthesis, slower epithelialization TABLE 48-1 Wound Classification [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 07, 2021
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Aug 07, 2021
Downloads
0
Views
46




.png)



.png)


 - Already Graded A.png)