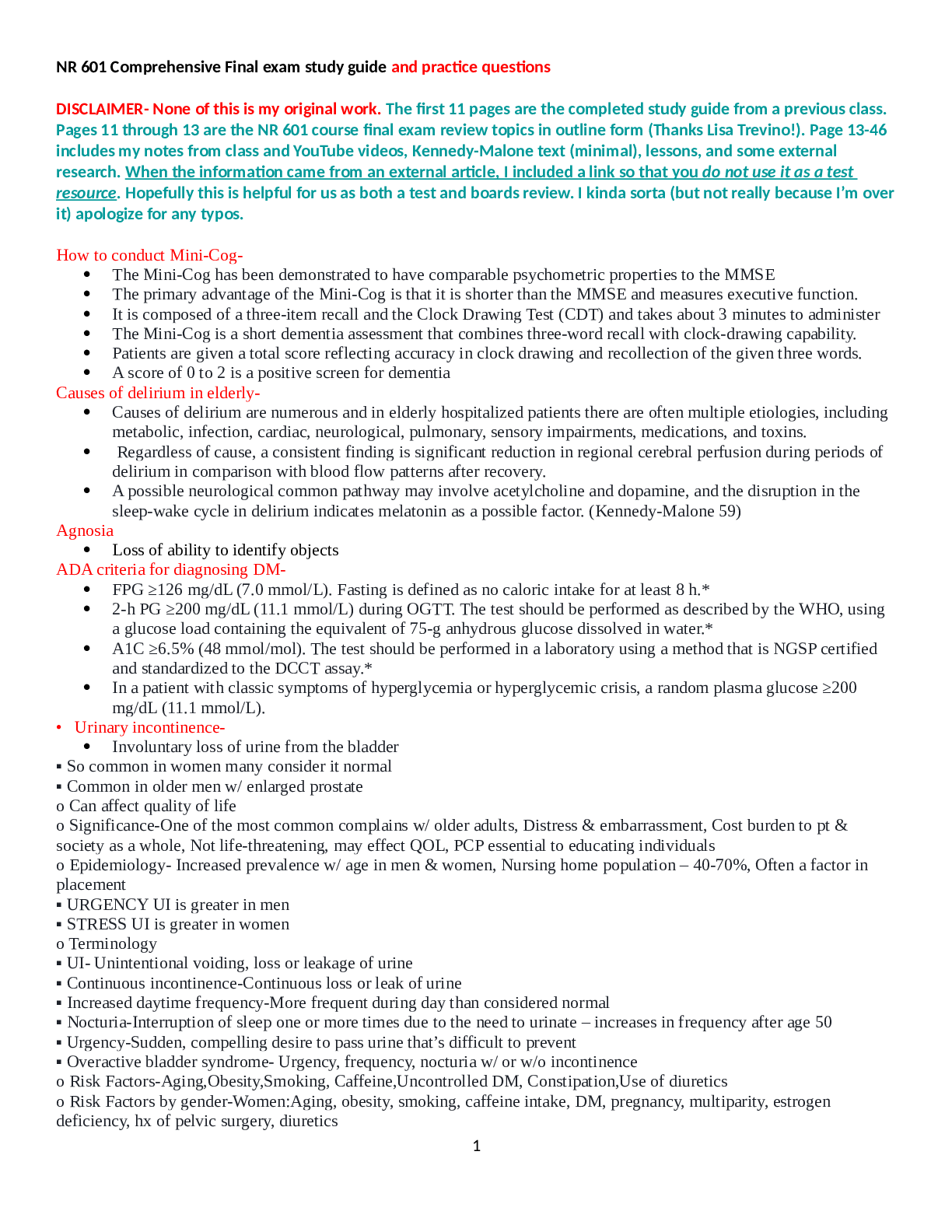
*NURSING > STUDY GUIDE > MED SURG 2 PRACTICE QUESTIONS WITH LATEST UPDATED ANSWERS GRADE A (RETAKE) (All)
MED SURG 2 PRACTICE QUESTIONS WITH LATEST UPDATED ANSWERS GRADE A (RETAKE)
Document Content and Description Below
Med-Surg 2 Practice Questions 1. An 83-year-old woman is being discharged from the hospital following stabilization of her international normalized ratio (INR) levels (used to assess the effective... ness of warfarin therapy). She has chronic atrial fibrillation and has been on warfarin (coumadin) for several years. Discharge instructions include returning to the clinic weekly for INR testing. Which statement by the patient indicates that she may be unable to have the testing done? a. "When I have the energy, I have to take a bus to get this test done." b. "I will need to ask my son to bring me into town every week for the test." c. "Should I just keep taking the same pill every day until I can get a ride into town." d. "It is very important to have this test every week. I have several church friends who can bring me." 2. What is an important nursing measure in the rehabilitation of an older adult to prevent loss of function from inactivity and immobility? a. Using assistive devices such as walkers and canes. b. Teaching good nutrition to prevent loss of muscle mass. c. Performance of active and passive range-of-motion (ROM) exercises. d. Performance of risk appraisals and assessments related to immobility. 3. An appropriate care choice for an older adult who lives with an employed daughter but requires help with activities of daily living is: a. adult day care b. long term care c. a retirement center d. an assisted living facility 4. What is most appropriate for the nurse to do when interviewing an older patient? a. ensure all assistive devices are in place. b. interview the patient and caregiver together. c. perform the interview before administering analgesics. d. move on to the next question if the patient does not respond quickly. 5. Which assessment findings would alert the nurse to possible elder mistreatment (select all that apply)? a. agitation b. depression c. weight gain d. weight loss e. hypernatremia 6. A 70-year-old man has just been diagnosed with chronic obstructive pulmonary disease (COPD). At what point should the nurse begin to include the patient's wife in the teaching around the management of the disease? a. as soon as possible b. when the patient requests assistance from his spouse and family c. when the patient becomes unable to manage his symptoms independently d. after the patient has had the opportunity to adjust to his treatment regimen 7. The long-term care nurse is performing assessments on several of the residents. Which are the normal age-related physiological change(s) the nurse expects to note? Select all that apply. A. Increased heart rate B. Decline in visual acuity C. Decreased respiratory rate D. Decline in long term memory E. Increased susceptibility to UTI’s F. Increased incidence of awakening after sleep onset 8. The home health nurse is visiting a client for the first time. While assessing the client’s medication history, it is noted that there are 19 prescriptions and several OTC medications that the client has been taking. Which intervention should the nurse take first? A. Check for medication interactions B. Determine whether there are medication duplications C. Call the prescribing HCP and report polypharmacy D. Determine whether a family member supervises medication administration 9. The nurse is providing medication instructions to an older client who is taking digoxin (Lanoxin) daily. The nurse notes that which age-related body change could place the client at risk for digoxin toxicity? A. Decreased muscle strength and loss of bone density B. Decreased cough efficiency and decreased vital capacity C. Decreased salivation and decreased gastrointestinal mobility D. Decreased lean body mass and decreased glomerular filtration rate CHAPTER 15 – CANCER 1. A patient who is scheduled for a breast biopsy asks the nurse the difference between a benign tumor and a malignant tumor. Which answer by the nurse is correct? a. "Benign tumors do not cause damage to other tissues." b. "Benign tumors are likely to recur in the same location." c. "Malignant tumors may spread to other tissues or organs." d. "Malignant cells reproduce more rapidly than normal cells." 2. The nurse is caring for a patient who smokes two packs/day. Which action by the nurse could help reduce the patient's risk of lung cancer? a. Teach the patient about the seven warning signs of cancer. b. Plan to monitor the patient's carcinoembryonic antigen (CEA) level. c. Teach the patient about annual chest x-rays for lung cancer screening. d. Discuss risks associated with cigarette smoking during each patient encounter. 3. The nurse should suggest which food choice when providing dietary teaching for a patient scheduled to receive external-beam radiation for abdominal cancer? a. Fruit salad b. Creamed broccoli c. Baked chicken d. Toasted wheat bread 4. During a routine health examination, a 40-yr-old patient tells the nurse about a family history of colon cancer. Which action should the nurse take next? a. Obtain more information about the family history. b. Schedule a sigmoidoscopy to provide baseline data. c. Teach the patient about the need for a colonoscopy at age 50. d. Teach the patient how to do home testing for fecal occult blood. 5. The nurse teaches a patient who is scheduled for a prostate needle biopsy about the procedure. Which statement, if made by the patient, indicates that teaching was effective? a. "The biopsy will remove the cancer in my prostate gland." b. "The biopsy will determine how much longer I have to live." c. "The biopsy will help decide the treatment for my enlarged prostate." d. "The biopsy will indicate whether the cancer has spread to other organs." 6. The nurse teaches a postmenopausal patient with stage III breast cancer about the expected outcomes of cancer treatment. Which patient statement indicates that the teaching has been effective? a. "After cancer has not recurred for 5 years, it is considered cured." b. "The cancer will be cured if the entire tumor is surgically removed." c. "I will need follow-up examinations for many years after treatment before I can be considered cured." d. "Cancer is never cured, but the tumor can be controlled with surgery, chemotherapy, and radiation." 7. External-beam radiation is planned for a patient with cervical cancer. What instructions should the nurse give to the patient to prevent complications from the effects of the radiation? a. Test all stools for the presence of blood. b. Maintain a high-residue, high-fiber diet. c. Clean the perineal area carefully after every bowel movement. d. Inspect the mouth and throat daily for the appearance of thrush. 8. The nurse is caring for a patient with colon cancer who is scheduled for external radiation therapy to the abdomen. Which information obtained by the nurse would indicate a need for patient teaching? a. The patient has a history of dental caries. b. The patient swims several days each week. c. The patient snacks frequently during the day. d. The patient showers each day with mild soap. 9. A patient undergoing external radiation has developed a dry desquamation of the skin in the treatment area. The nurse teaches the patient about the management of the skin reaction. Which statement, if made by the patient, indicates the teaching was effective a. "I can use ice packs to relieve itching." b. "I will scrub the area with warm water." c. "I can buy aloe vera gel to use on my skin." d. "I will expose my skin to a sun lamp each day." 10. A patient with metastatic cancer of the colon experiences severe vomiting after each administration of chemotherapy. Which action, if taken by the nurse, is appropriate? a. Have the patient eat large meals when nausea is not present. b. Offer dry crackers and carbonated fluids during chemotherapy. c. Administer prescribed antiemetics 1 hour before the treatments. d. Give the patient a glass of a citrus fruit beverage during treatments. 11. The nurse administers an IV vesicant chemotherapeutic agent to a patient. Which action is most important for the nurse to take? a. Infuse the medication over a short period of time. b. Stop the infusion if swelling is observed at the site. c. Administer the chemotherapy through a small-bore catheter. d. Hold the medication unless a central venous line is available. 12. A chemotherapy drug that causes alopecia is prescribed for a patient. Which action should the nurse take to support the patient's self-esteem? a. Encourage the patient to purchase a wig or hat to wear when hair loss begins. b. Suggest that the patient limit social contacts until regrowth of the hair occurs. c. Teach the patient to wash hair gently with mild shampoo to minimize hair loss. d. Inform the patient that hair usually grows back once chemotherapy is complete. 13. A patient receiving head and neck radiation for larynx cancer has ulcerations over the oral mucosa and tongue and thick, ropey saliva. Which instructions should the nurse give to this patient? a. Remove food debris from the teeth and oral mucosa with a stiff toothbrush. b. Use cotton-tipped applicators dipped in hydrogen peroxide to clean the teeth. c. Gargle and rinse the mouth several times a day with an antiseptic mouthwash. d. Rinse the mouth before and after each meal and at bedtime with a saline solution. 14. Interleukin-2 (IL-2) is used as adjuvant therapy for a patient with metastatic renal cell carcinoma. Which information should the nurse include when explaining the purpose of this therapy to the patient a. IL-2 enhances the body's immunologic response to tumor cells. b. IL-2 prevents bone marrow depression caused by chemotherapy. c. IL-2 protects normal cells from harmful effects of chemotherapy. d. IL-2 stimulates malignant cells in the resting phase to enter mitosis. 15. The nurse teaches a patient with cancer of the liver about high-protein, high-calorie diet choices. Which snack choice by the patient indicates that the teaching has been effective? a. Lime sherbet b. Fresh strawberries c. Blueberry/strawberry yogurt d. Cream cheese bagel 16. A hospitalized patient who has received chemotherapy for leukemia develops neutropenia. Which observation by the nurse would indicate a need for further teaching a. The patient ambulates around the room. b. The patient's visitors bring in fresh peaches. c. The patient cleans with a warm washcloth after having a stool. d. The patient uses soap and shampoo to shower every other day. 17. The nurse is caring for a patient diagnosed with stage I colon cancer. When assessing the need for psychologic support, which question by the nurse will provide the most information? a. "How long ago were you diagnosed with this cancer?" b. "Do you have any concerns about body image changes?" c. "Can you tell me what has been helpful to you in the past when coping with stressful events?" d. "Are you familiar with the stages of emotional adjustment to a diagnosis like cancer of the colon?" 18. A nurse plans a community education program related to prevention of the cancer with the highest death rates in both women and men. What should the nurse include in the teaching plan? a. Smoking cessation b. Screening with colonoscopy c. Regular examination of reproductive organs d. Use of sunscreen as protection from ultraviolet light 19. A 33-year-old patient has recently been diagnosed with stage II cervical cancer. What should the nurse understand about the patient's cancer? a. It is in situ. b. It has metastasized. c. It has spread locally. d. It has spread extensively. 20. The nurse is caring for a patient suffering from anorexia secondary to chemotherapy. Which strategy would be most appropriate for the nurse to use to increase the patient's nutritional intake? a. Increase intake of liquids at mealtime to stimulate the appetite. b. Serve three large meals per day plus snacks between each meal. c. Avoid the use of liquid protein supplements to encourage eating at mealtime. d. Add items such as skim milk powder, cheese, or peanut butter to selected foods. 21. Previous administrations of chemotherapy agents to a cancer patient have resulted in diarrhea. Which dietary modification should the nurse recommend? a. A bland, low-fiber diet b. A high-protein, high-calorie diet c. A diet high in fresh fruits and vegetables d. A diet emphasizing whole and organic foods 22. Which item would be most beneficial when providing oral care to a patient with metastatic cancer who is at risk for oral tissue injury secondary to chemotherapy? a. Firm-bristle toothbrush b. Hydrogen peroxide rinse c. Alcohol-based mouthwash d. 1 tsp salt in 1 L water mouth rinse 23. Which nursing diagnosis is most appropriate for a patient experiencing myelosuppression secondary to chemotherapy for cancer treatment? a. Acute pain b. Hypothermia c. Powerlessness d. Risk for infection 24. After 3 weeks of radiation therapy, a patient has lost 10 pounds and does not eat well because of mucositis. Which nursing diagnosis would be most appropriate? a. Risk for infection related to poor nutrition. b. Ineffective health management related to refusal to eat. c. Imbalanced nutrition: less than body requirements related to oral ulcerations d. Ineffective health maintenance related to lack of knowledge of nutritional requirements during radiation therapy. CHAPTER 30 – HEMATOLOGIC PROBLEM (THROMBOCYTOPENIA) 1. Which intervention will be included in the nursing care plan for a patient with immune thrombocytopenia purpura (ITP)? a. Assign the patient to a private room. b. Avoid intramuscular (IM) injection. c. Use rinses rather than a soft toothbrush for oral care. d. Restrict activity to passive and active range of motion. 2. Which laboratory results will the nurse expect to show a decrease value if a patient develops heparin-induced thrombocytopenia (HIT)? a. Prothrombin time (PT) b. Erythrocytes count c. Fibrinogen degradation products d. Activated partial thromboplastin time (aPTT) 3. Which action will the admitting nurse include in the care plan for a 30-year old woman who is neutropenia? a. Avoid any injections. b. Check temperature every 4 hours. c. Omit fruits or vegetables from the diet d. Pace a No Visitor sign on the door. 4. Which information obtained by ten nurse caring for a patient with thrombocytopenia should be immediately communicated to the health care provider? a. The platelet count is 52,000/L. b. The patient is difficult to arouse. c. There are purpura on the oral mucosa. d. There are large bruises on the patient’s back. 5. The nurse is planning to administer transfusion of packed red blood cells (PRBCs) to a patient with blood loss from gastrointestinal hemorrhage. Which action can the nurse delegate to an unlicensed assistive personnel (UAP)? a. Verify the patient identification (ID) according to hospital policy. b. Obtain the temperature, blood pressure, and pulse before the transfusion. c. Double-check the product numbers on the PRBCs with the patient ID band. d. Monitor the patient for shortness of breath or chest pain during the transfusion. 6. A 19-year-old woman with immunize thrombocytopenic purpura (ITP) has an order for a platelet transfusion. Which information indicates that the nurse should consult with the healthcare provider before obtaining and administering platelets? a. The platelet count is 42,000/mL. b. Petechiae are present on the chest. c. Blood pressure (BP) is 94/56 mmHg. d. Blood oozing from the venipuncture site. 7. Which sign would the nurse expect to assess in the client diagnosed with immune thrombocytopenic purpura (ITP)? a. Petechiae on the anterior chest, arms, and neck. b. Capillary refill of less than three (3) seconds. c. An enlarged spleen. d. Pulse oximeter reading of 95%. 8. A nurse is planning care for a client who has thrombocytopenia. Which of the following interventions should the nurse include in the plan? a. Apply pressure to needlestick sites for 10 min. b. Assess core temperatures using a rectal thermometer. c. Measure abdominal girth twice weekly. d. Monitor for the presence of WBCs in the urine. CHAPTER 33 – CAD & ACUTE CORONARY SYNDROME 1. When developing a teaching plan for a 61-year-old man with the following risk factors for coronary artery disease (CAD), the nurse should focus on the a. family history of coronary artery disease. b. Increased risk associated with the patient’s gender. c. Increased risk of cardiovascular disease as people age. d. Elevation of their patients low-density lipoprotein (LDL) level. 2. Which assessment data collected by the nurse who is admitting a patient with chest pain suggest that the pain is caused by an acute myocardial infarction (AMI)? a. The pain increases with deep breathing. b. The pain has lasted longer than 30 minutes. c. The pain is relieved after the patient takes nitroglycerin. d. The pain is reproducible when the patient raises the arms. 3. After the nurse has finished teaching a patient about the use of sublingual nitroglycerin (Nitrostat), which patient statement indicates that the teaching has been effective? a. "I can expect some nausea as a side effect of nitroglycerin." b. "I should only take the nitroglycerin if I start to have chest pain." c. "I will call an ambulance if I still have pain after taking 3 nitroglycerin 5 minutes apart." d. "Nitroglycerin helps prevent a clot from forming and blocking blood flow to my heart." 4. A patient who has had chest pain for several hours is admitted with a diagnosis of rule out acute myocardial infarction (AMI). Which laboratory test should the nurse monitor to help determine whether the patient has had an AMI? a. Myoglobin b. Homocysteine c. C-reactive protein d. Cardiac-specific troponin 5. The nurse will suspect that the patient with stable angina is experiencing a side effect of the prescribed metoprolol (Lopressor) if the a. patient is restless and agitated. b. blood pressure is 90/54 mm Hg. c. patient complains about feeling anxious. d. cardiac monitor shows a heart rate of 61 beats/minute. 6. Heparin is ordered for a patient with a non-ST-segment-elevation myocardial infarction (NSTEMI). What is the purpose of the heparin? a. Heparin enhances platelet aggregation. b. Heparin decreases coronary artery plaque size. c. Heparin prevents the development of new clots in the coronary arteries. d. Heparin dissolves clots that are blocking blood flow in the coronary arteries. 7. A patient who is being admitted to the emergency department with intermittent chest pain gives the following list of medications to the nurse. Which medication has the most immediate implications for the patient's care? a. Sildenafil (Viagra) b. Furosemide (Lasix) c. Captopril (Capoten) d. Warfarin (Coumadin) 8. A patient who has chest pain is admitted to the emergency department (ED) and all of the following are ordered. Which one should the nurse arrange to be completed first? a. Chest x-ray b. Troponin level c. Electrocardiogram (ECG) d. Insertion of a peripheral IV 9. A patient in the emergency department complains of back pain and difficulty breathing 15 minutes after a transfusion of packed red blood cells is started. The nurse’s first action should be a. Administer oxygen therapy at a high flow rate. b. Obtain a urine specimen to sent to the laboratory. c. Notify the health care provider about the symptoms. d. Disconnect the transfusion and infuse normal saline. CHAPTER 34 – HEART FAILURE 1. A 54-year-old male patient who had bladder surgery 2 days ago develops acute decompensated heart failure (ADHF) with severe dyspnea. Which action by the nurse would be indicated first? a. Perform a bladder scan to assess for urinary retention. b. Restrict the patient’s oral fluid intake to 500 mL per day. c. Assist the patient to a sitting position with arms on the overbred table. d. Instruct the patient to use pursed-lip breathing unit or the dyspnea subside. - COPD 2. The home care nurse visits a 75-year-old Hispanic woman with chronic heart failure. Which clinical manifestation, if assessed by the nurse, would indicate acute decompensated heart failure (pulmonary edema)? a. Fatigue, orthopnea, and dependent edema. b. Severe dyspnea and blood-streaked, frothy sputum. c. Temperature is 100.4 F and pulse is 102 beats/minute. d. Respiration 26 breaths/minute despite oxygen by nasal cannula. 3. A patient with a recent diagnosis of heart failure has been prescribed furosemide (Lasix) in an effort to physiologically do what for the patient? a. Reduce preload b. Decrease afterload c. Increase contractility d. Promote vasodilation 4. A patient who has chronic heart failure tells the nurse, I was fine when I went to bed, but I woke up in the middle of the night feeling like I was suffocating. The nurse will document this assessment as: a. Orthopnea b. Pulsus alternans c. Paroxysmal nocturnal dyspnea d. Acute bilateral effusion 5. During a visit to a 78-year-old with chronic heart failure, the home care nurse finds that the patient has ankle edema, a 2-kg weight gain over the past 2 days, and complains of "feeling too tired to get out of bed." Based on these data, the best nursing diagnosis for the patient is a. activity intolerance related to fatigue. b. disturbed body image related to weight gain. c. impaired skin integrity related to ankle edema. d. impaired gas exchange related to dyspnea on exertion. 6. Which diagnostic test will be most useful to the nurse in determining whether a patient admitted with acute shortness of breath has heart failure? a. Serum troponin b. Arterial blood gases c. B-type natriuretic peptide – (BNP) d. 12-lead electrocardiogram 7. A patient with a history of chronic heart failure is admitted to the emergency department (ED) with severe dyspnea and a dry, hacking cough. Which action should the nurse do first? a. Auscultate the abdomen. b. Check the capillary refill. c. Auscultate the breath sounds. d. Assess the level of orientation. 8. After receiving change-of-shift report on a heart failure unit, which patient should the nurse assess first? a. A patient who is cool and clammy, with new-onset confusion and restlessness b. A patient who has crackles bilaterally in the lung bases and is receiving oxygen. c. A patient who had dizziness after receiving the first dose of captopril (Capoten) d. A patient who is receiving IV nesiritide (Natrecor) and has a blood pressure of 100/62 9. Which assessment finding in a patient admitted with acute decompensated heart failure (ADHF) requires the most immediate action by the nurse? a. Oxygen saturation of 88% b. Weight gain of 1 kg (2.2 lb) c. Heart rate of 106 beats/minute d. Urine output of 50 mL over 2 hours 10. A patient has recently started on digoxin (Lanoxin) in addition to furosemide (Lasix) and captopril (Capoten) for the management of heart failure. Which assessment finding by the home health nurse is a priority to communicate to the health care provider? a. Presence of 1 to 2+ edema in the feet and ankles b. Palpable liver edge 2 cm below the ribs on the right side c. Serum potassium level 3.0 mEq/L after 1 week of therapy d. Weight increase from 120 pounds to 122 pounds over 3 days 11. A patient with heart failure has a new order for captopril (Capoten) 12.5 mg PO. After administering the first dose and teaching the patient about the drug, which statement by the patient indicates that teaching has been effective? a. "I will be sure to take the medication with food." b. "I will need to eat more potassium-rich foods in my diet." c. "I will call for help when I need to get up to use the bathroom." d. "I will expect to feel more short of breath for the next few days." 12. A 70-year-old woman with chronic heart failure and atrial fibrillation asks the nurse why warfarin (Coumadin) has been prescribed to her to continue at home. Which response by the nurse is accurate? a. "The medication prevents blood clots from forming in your heart." b. "The medication dissolves clots that develop in your coronary arteries." c. "The medication reduces clotting by decreasing serum potassium levels." d. "The medication increases your heart rate so that clots do not form in your heart." 13. A stable patient with acute decompensated heart failure (ADHF) suddenly becomes dyspneic. Before positioning the patient on the bedside, what should the nurse assess first? a. Urine output b. Heart rhythm c. Breath sounds d. Blood pressure CHAPTER 35 – DYSRHYTHMIAS 1. To determine whether there is a delay in impulse conduction through the atria, the nurse will measure the duration of the patient's a. P wave. b. Q wave. c. P-R interval. d. QRS complex. 2. The nurse needs to quickly estimate the heart rate for a patient with a regular heart rhythm. Which method will be best to use? a. Count the number of large squares in the R-R interval and divide by 300. b. Print a 1-minute electrocardiogram (ECG) strip and count the number of QRS complexes. c. Calculate the number of small squares between one QRS complex and the next and divide into 1500. d. Use the 3-second markers to count the number of QRS complexes in 6 seconds and multiply by 10. 3. A patient has a normal cardiac rhythm and a heart rate of 72 beats/minute. The nurse determines that the P-R interval is 0.24 seconds. The most appropriate intervention by the nurse would be to a. notify the health care provider immediately. b. give atropine per agency dysrhythmia protocol. c. prepare the patient for temporary pacemaker insertion. d. document the finding and continue to monitor the patient. 4. A patient with dilated cardiomyopathy has new onset atrial fibrillation that has been unresponsive to drug therapy for several days. The priority teaching needed for this patient would include information about a. anticoagulant therapy. b. permanent pacemakers. c. electrical cardioversion. d. IV adenosine (Adenocard). 5. A 20-year-old has a mandatory electrocardiogram (ECG) before participating on a college soccer team and is found to have sinus bradycardia, rate 52. Blood pressure (BP) is 114/54, and the student denies any health problems. What action by the nurse is most appropriate? a. Allow the student to participate on the soccer team. b. Refer the student to a cardiologist for further diagnostic testing. c. Tell the student to stop playing immediately if any dyspnea occurs. d. Obtain more detailed information about the student's family health history. 6. A 19-year-old student comes to the student health center at the end of the semester complaining that, "My heart is skipping beats." An electrocardiogram (ECG) shows occasional premature ventricular contractions (PVCs). What action should the nurse take next? a. Start supplemental O2 at 2 to 3 L/min via nasal cannula. b. Ask the patient about current stress level and caffeine use. c. Ask the patient about any history of coronary artery disease. d. Have the patient taken to the hospital emergency department (ED). 7. A patient who is on the progressive care unit develops atrial flutter, rate 150, with associated dyspnea and chest pain. Which action that is included in the hospital dysrhythmia protocol should the nurse do first? a. Obtain a 12-lead electrocardiogram (ECG). b. Notify the health care provider of the change in rhythm. c. Give supplemental O2 at 2 to 3 L/min via nasal cannula. d. Assess the patient's vital signs including oxygen saturation. 8. A patient’s cardiac rhythm is sinus bradycardia with a heart rate of 34 beats/minute. If the bradycardia is symptomatic, the nurse would expect the patient to exhibit a. Palpitations. b. Hypertension. c. Warm, flushed skin. d. Shortness of breath. 9. Which nursing action can the registered nurse (RN) delegate to experienced unlicensed assistive personnel (UAP) working as a telemetry technician on the cardiac care unit? a. Decide whether a patient's heart rate of 116 requires urgent treatment. b. Monitor a patient's level of consciousness during synchronized cardioversion. c. Observe cardiac rhythms for multiple patients who have telemetry monitoring. d. Select the best lead for monitoring a patient admitted with acute coronary syndrome. 10. Sinus Bradycardia 10. Sinus Tachycardia 11. Artifact 12. A-Fib 13. Premature Atrial Contraction 14. Normal Sinus Rhythm 15. Atrial Flutter CHAPTER 28 – OBSTRUCTIVE PULMONARY DISEASES 1. Which information will the nurse include in the asthma teaching plan for a patient being discharged? a. Use the inhaled corticosteroid when shortness of breath occurs. b. Inhale slowly and deeply when using the dry power inhaler (DPI). c. Hold your breath for 5 seconds after using the bronchodilator inhaler. d. Tremors are an expected side effect of rapidly acting bronchodilators. 2. The emergency department nurse is evaluating the effectiveness of therapy for a patient who has received treatment during an asthma attack. Which assessment finishing is the best indicator that the therapy has been effective? a. No wheezes are audible. b. Oxygen saturation >90%. c. Accessory muscle use has decreased. d. Respiratory rate is 16 breaths/minute. 3. A patient with chronic obstructive pulmonary disease (COPD) has a nursing diagnosis of impaired breathing pattern related to anxiety. Which nursing action is most appropriate to include in the plan of care? a. Titrate oxygen to keep saturation at least 90%. b. Discuss a high-protein, high-calorie diet with the patient. c. Suggest the use of over-the-counter sedative medications. d. Teach the patient how to effectively use pursed lip breathing. 4. The nurse develops a teaching plan to help increase activity tolerance at home for an older adult with severe chronic obstructive pulmonary disease (COPD). Which instructions would be most appropriate for the nurse to include in the plan of care? a. Stop exercising when short of breath. b. Walk until pulse rate exceeds 130 beats/minute. c. Limit exercise to activities of daily living (ADLs). d. Walk 15 to 20 minutes daily at least 3 times/week. 5. Which instruction should the nurse include in an exercise teaching plan for a patient with chronic obstructive pulmonary disease (COPD)? a. "Stop exercising if you start to feel short of breath." b. "Use the bronchodilator before you start to exercise." c. "Breathe in and out through the mouth while you exercise." d. "Upper body exercise should be avoided to prevent dyspnea." 5. Which nursing action for a patient with chronic obstructive pulmonary disease (COPD) could the nurse delegate to experienced unlicensed assistive personnel (UAP)? a. Obtain oxygen saturation using pulse oximetry. b. Monitor for increased oxygen need with exercise. c. Teach the patient about safe use of oxygen at home. d. Adjust oxygen to keep saturation in prescribed parameters. 6. The nurse reviews the medication administration record (MAR) for a patient having an acute asthma attack. Which medication should the nurse administer first? a. Albuterol (Ventolin) 2.5 mg per nebulizer b. Methylprednisolone (Solu-Medrol) 60 mg IV c. Salmeterol (Serevent) 50 mcg per dry-powder inhaler (DPI) d. Triamcinolone (Azmacort) 2 puffs per metered-dose inhaler (MDI) 7. A patient with chronic obstructive pulmonary disease (COPD) has poor gas exchange. Which action by the nurse would be most appropriate? a. Have the patient rest in bed with the head elevated to 15 to 20 degrees. b. Ask the patient to rest in bed in a high-Fowler's position with the knees flexed. c. Encourage the patient to sit up at the bedside in a chair and lean slightly forward. d. Place the patient in the Trendelenburg position with several pillows behind the head. 8. The nurse takes an admission history on a patient with possible asthma who has new-onset wheezing and shortness of breath. Which information may indicate a need for a change in therapy? a. The patient has chronic inflammatory bowel disease. b. The patient has a history of pneumonia 6 months ago. c. The patient takes propranolol (Inderal) for hypertension. d. The patient uses acetaminophen (Tylenol) for headaches. 9. A patient newly diagnosed with mild asthma is being discharged. The nurse anticipates including which topic in the discharge teaching? a. Use of long-acting b-adrenergic medications b. Side effects of sustained-release theophylline c. Self-administration of inhaled corticosteroids d. Complications associated with oxygen therapy 10. A patient who is experiencing an acute asthma attack is admitted to the emergency department. Which assessment should the nurse complete first? a. Listen to the patient's breath sounds. b. Ask about inhaled corticosteroid use. c. Determine when the dyspnea started. d. Obtain the forced expiratory volume (FEV) flow rate. 11. In evaluating an asthmatic patient’s knowledge of self-care, the nurse recognizes that additional instruction is needed when the patient says: a. “I use my corticosteroid inhaler when I feel short of breath” b. “I get a flu shot every year and see my HCP if I have an upper respiratory tract infection c. “I use my inhaler before I visit my aunt who has a cat, but I only visit for a few minutes because of my allergies” d. “I walk 30 minute every day but sometimes I have to use my bronchodilator inhaler before walking to prevent me from getting short of breath”. 12. The nurse is caring for a client hospitalized with acute exacerbation of COPD. Which finding would the nurse expect to note on assessment of this client? Select all that apply: a. Hypocapnia b. A hyperinflated chest noted on the chest x-ray c. Decreased oxygen saturation with mild exercise d. Pulmonary function tests that demonstrate increased vital capacity 13. The nurse instructs a client to use the pursed-lip method of breathing and the client asks the nurse about the purpose of this type of breathing. The nurse responds, knowing that the primary purpose of pursed-lip breathing is to promote which outcome? a. Promote oxygen intake b. Strengthen the diaphragm c. Strengthen the intercostal muscles d. Promote carbon dioxide elimination 14. The nurse receives a change-of-shift report on the following patients with chronic obstructive pulmonary disease (COPD). Which patient should the nurse assess first? a. A patient with loud expiratory wheezes b. A patient with a respiratory rate of 38/minute c. A patient who has a cough productive of thick, green mucus d. A patient with jugular venous distention and peripheral edema 15. Which medication should the nurse anticipate being used first in the emergency department for relief of severe respiratory distress related to asthma? a. Prednisone orally b. Tiotropium inhaler c. Fluticasone inhaler d. Albuterol nebulizer 17. When teaching the patient about going from a metered-dose inhaler (MDI) to a dry powder inhaler (DPI), which statement by the patient shows the nurse that the patient needs more teaching? a. "I do not need to use the spacer like I used to." b. "I will hold my breath for 10 seconds or longer if I can." c. "I will not shake this inhaler like I did with my old inhaler." d. "I will store it in the bathroom so I will be able to clean it when I need to." 18. A patient is being discharged with plans for home O2 therapy provided by an O2 concentrator with a portable O2 -concentrator unit. In preparing the patient to use the equipment, what should the nurse teach the patient? a. The portable unit will last about 6 to 8 hours. b. The unit is strictly for portable and emergency use. c. The unit concentrates O2 from the air, providing a continuous O2 supply. d. Weekly delivery of one large cylinder of O2 will be necessary for a 7- to 10-day supply of O2 CHAPTER 58 – CHRONIC NEUROLOGICAL PROBLEMS 1.A 38-year-old woman has newly diagnosed multiple sclerosis (MS) and asks the nurse what is going to happen to her. What is the best response by the nurse? a. “You will have either periods of attacks and remissions or progression of nerve damage over time.” b. “You need to plan for a continuous loss of movement, sensory functions, and mental capabilities.” c. “You will most likely have a steady course of chronic progressive nerve damage that will change your personality.” d. “It is common for those with MS to have an acute attack of weakness and then not to have any other symptoms for years.” 2. During assessment of a patient admitted to the hospital with an acute exacerbation of MS, what should the nurse expect to find? a. Tremors, dysphasia, and ptosis b. Bowel and bladder incontinence and loss of memory c. Motor impairment, visual disturbances, and paresthesias d. Excessive involuntary movements, hearing loss, and ataxia 3. The nurse is teaching a female client with MS. When teaching the client how to reduce fatigue, the nurse should tell the client to: a. take a hot bath. b. rest in an air-conditioned room. c. increase the dose of muscle relaxants. d. avoid naps during the day. 4. The nurse explains to a patient newly diagnosed with MS that the diagnosis is made primarily by a. spinal x-ray findings. b. T-cell analysis of the blood. c. analysis of cerebrospinal fluid. d. history and clinical manifestations. 5. A patient with newly diagnosed MS has been hospitalized for evaluation and initial treatment of the disease. Following discharge teaching, the nurse realizes that additional instruction is needed when the patient says what? a. “It is important for me to avoid exposure to people with upper respiratory infections.” b. “When I begin to feel better, I should stop taking the prednisone to prevent side effects.” c. “I plan to use vitamin supplements and a high-protein diet to help manage my condition.” d. “I must plan with my family how we are going to manage my care if I become more incapacitated.” 6. A patient with MS has a nursing diagnosis of self-care deficit related to muscle spasticity and neuromuscular deficits. In providing care for the patient, what is most important for the nurse to do? a. Teach the family members how to care adequately for the patient’s needs. b. Encourage the patient to maintain social interactions to prevent social isolation. c. Promote the use of assistive devices so the patient can participate in self-care activities. d. Perform all activities of daily living (ADLs) for the patient to conserve the patient’s energy. 7. You see a patient diagnosed several years ago with Parkinson’s disease at your outpatient clinic with a cough and fever. It is obvious that his Parkinson’s disease has advanced. During your assessment of him, you would expect to find a. slurred speech, visual disturbances, and ataxia. b. muscle atrophy, spasticity, and speech difficulties. c. muscle weakness, double vision, and reports of fatigue. d. drooling, stooped posture, tremors, and a propulsive gait. 9. An appropriate nursing diagnosis for a patient with advanced Parkinson’s disease is a. risk for injury related to limited vision. b. risk for aspiration related to impaired swallowing. c. urge incontinence related to effects of drug therapy. d. ineffective breathing pattern related to diaphragm fatigue. 9. The classic triad of manifestation associated with Parkinson’s disease are tremors, rigidity, and bradykinesia. What is a consequence r/t rigidity? a. Shuffling gait b. Impaired handwriting c. Lack of postural stability d. Muscle soreness and pain 10. A female client has experienced an episode of myasthenic crisis. The nurse would assess whether the client has precipitating factors such as: a. Getting too little exercise b. Taking excess prescribed medicatioN c. Omitting doses of medication d. Increasing intake of fatty foods 11. The nurse is teaching the female client with myasthenia gravis about the prevention of myasthenic and cholinergic crises. The nurse tells the client that this is most effectively done by: a. Eating large, well-balanced meals b. Doing muscle-strengthening exercises c. Doing all chores early in the day while less fatigued d. Taking medications on time to maintain therapeutic blood levels 12. During care of a patient in myasthenic crisis, maintenance of what is the nurse’s first priority for the patient? a. Mobility b. Nutrition c. Respiratory function d. Verbal communication 13. A female client with amyotrophic lateral sclerosis (ALS) tells the nurse, “Sometimes I feel so frustrated. I can’t do anything without help!” This comment best supports which nursing diagnosis? a. Anxiety b. Powerlessness c. Ineffective denial d. Risk for disuse syndrome 14. When providing care for a patient with ALS, the nurse recognizes what as one of the most distressing problems experienced by the patient? a. Painful spasticity of the face and extremities b. Retention of cognitive function with total degeneration of motor function c. Uncontrollable writhing and twisting movements of the face, limbs, and body d. Knowledge that there is a 50% chance the disease has been passed to any offspring 15. Female client is admitted to the hospital with a diagnosis of Guillain-Barre syndrome. The nurse inquires during the nursing admission interview if the client has history of: a. Seizures or trauma to the brain b. Meningitis during the last 5 years c. Back injury or trauma to the spinal cord d. Respiratory or gastrointestinal infection during the previous month. 16. A patient is admitted to the hospital with Guillain-Barre syndrome. She had weakness in her feet and ankles that has progressed to weakness with numbness and tingling in both legs. During the acute phase of the illness, what should the nurse know about Guillain-Barre syndrome? a. The most important aspect of care is to monitor the patient’s respiratory rate and depth and vital capacity. b. Early treatment with corticosteroids can suppress the immune response and prevent ascending nerve damage. c. The most serious complication of this condition is ascending demyelination of the peripheral nerves and the cranial nerves. d. Although voluntary motor neurons are damaged by the inflammatory response, the autonomic nervous system is unaffected by the disease. 17. A patient with Guillain-Barre syndrome asks whether he is going to die as the paralysis spreads toward his chest. In responding to the patient, what should the nurse know to be able to answer this question? a. Patients who require ventilatory support almost always die. b. Death occurs when nerve damage affects the brain and meninges. c. Most patients with Guillain-Barre syndrome make a complete recovery. d. If death can be prevented, residual paralysis and sensory impairment are usually permanent. 18. A male client with Bell’s palsy asks the nurse what has caused this problem. The nurse’s response is based on an understanding that the cause is: a. Unknown, but possibly includes ischemia, viral infection, or an autoimmune problem b. Unknown, but possibly includes long-term tissue malnutrition and cellular hypoxia c. Primary genetic in origin, triggered by exposure to meningitis d. Primarily genetic in origin, triggered by exposure to neurotoxins 19. The nurse has given the male client with Bell’s palsy instructions on preserving muscle tone in the face and preventing denervation. The nurse determines that the client needs additional information if the client states that he or she will: a. Increase exposure to cold and drafts b. Massage the face with a gentle upward motion c. Perform facial exercises d. Wrinkle the forehead, blow out the cheeks, and whistle 20. In providing care for patients with chronic, progressive neurologic disease, what is the major goal of treatment that the nurse works toward? a. Meet the patient’s personal care needs. b. Return the patient to normal neurologic function. c. Maximize neurologic functioning for as long as possible. d. Prevent the development of additional chronic diseases. 21. When obtaining a health history and physical assessment for a 36-year-old female patient with possible multiple sclerosis (MS), the nurse should a. assess for the presence of chest pain. b. inquire about urinary tract problems. c. inspect the skin for rashes or discoloration. d. ask the patient about any increase in libido. 22. A 31-year-old woman who has multiple sclerosis (MS) asks the nurse about risks associated with pregnancy. Which response by the nurse is accurate? a. "MS symptoms may be worse after the pregnancy." b. "Women with MS frequently have premature labor." c. "MS is associated with an increased risk for congenital defects." d. "Symptoms of MS are likely to become worse during pregnancy." 23. A 73-year-old patient with Parkinson's disease has a nursing diagnosis of impaired physical mobility related to bradykinesia. Which action will the nurse include in the plan of care? a. Instruct the patient in activities that can be done while lying or sitting. b. Suggest that the patient rock from side to side to initiate leg movement. c. Have the patient take small steps in a straight line directly in front of the feet. d. Teach the patient to keep the feet in contact with the floor and slide them forward. 24. The nurse advises a patient with myasthenia gravis (MG) to a. perform physically demanding activities early in the day. b. anticipate the need for weekly plasmapheresis treatments. c. do frequent weight-bearing exercise to prevent muscle atrophy. d. protect the extremities from injury due to poor sensory perception. 25. A 76-year-old patient is being treated with carbidopa/levodopa (Sinemet) for Parkinson's disease. Which information is most important for the nurse to report to the health care provider? a. Shuffling gait b. Tremor at rest c. Cogwheel rigidity of limbs d. Uncontrolled head movement CHAPTER 41 – UPPER GI BLEED 1. The nurse teaches a patient with a history of upper gi bleeding how to check for bloody stools. Which statement by the nurse is appropriate? a. “if vomiting of bright red blood occurs, stools will not be black and sticky.” b. “blood is never obvious in stools and must be detected by a lab test.” c. “acute bleeding in your stomach will cause bright red blood in your stools.” d. “stools that are black and tarry occur with slow bleeding from the stomach.” 2. The teaching plan for the patient being discharged after an acute episode of upper gi bleeding includes information concerning the importance of (select all that apply): a. Limiting etoh to one serving per day b. Only taking aspirin with milk or bread products c. Avoiding taking aspirin and drugs containing aspirin d. Only taking drugs prescribed by the health care provider e. Taking all drugs 1 hour before mealtime to prevent further bleeding 3. A patient with recurring heartburn receives a new prescription for esomeprazole (Nexium). In teaching the patient about this medication, the nurse explains that this drug a.neutralizes stomach acid and provides relief of symptoms in a few minutes. b.reduces the reflux of gastric acid by increasing the rate of gastric emptying. c. coats and protects the lining of the stomach and esophagus from gastric acid. d.treats gastroesophageal reflux disease by decreasing stomach acid production. 4. The family member of a patient who has suffered massive abdominal trauma in an automobile accident asks the nurse why the patient is receiving famotidine (Pepcid). The nurse will explain that the medication will a. prevent aspiration of gastric contents. b. inhibit the development of stress ulcers. c. lower the chance for H. pylori infection. d. decrease the risk for nausea and vomiting. 5. A patient who has gastroesophageal reflux disease (GERD) is experiencing increasing discomfort. Which patient statement to the nurse indicates that additional teaching about GERD is needed? a. "I take antacids between meals and at bedtime each night." b. "I sleep with the head of the bed elevated on 4-inch blocks." c. "I eat small meals during the day and have a bedtime snack." d. "I quit smoking several years ago, but I still chew a lot of gum." 6. A 68-yr-old male patient with a stroke is unconscious and unresponsive to stimuli. After learning that the patient has a history of gastroesophageal reflux disease (GERD), the nurse will plan to do frequent assessments of the patient's a. apical pulse. b. bowel sounds. c. breath sounds. d. abdominal girth. 7. A patient vomiting blood-streaked fluid is admitted to the hospital with acute gastritis. To determine possible risk factors for gastritis, the nurse will ask the patient about a. the amount of saturated fat in the diet. b. a family history of gastric or colon cancer. c. a history of a large recent weight gain or loss. d. use of nonsteroidal antiinflammatory drugs (NSAIDs). 8. The nurse will anticipate preparing an older patient who is vomiting "coffee-ground" emesis for a. endoscopy. b. angiography. c. barium studies. d. gastric analysis. 9. The nurse is assessing a patient who had a total gastrectomy 8 hours ago. What information is most important to report to the health care provider? a. Hemoglobin (Hgb) 10.8 g/dL b. Temperature 102.1°F (38.9°C) c. Absent bowel sounds in all quadrants d. Scant nasogastric (NG) tube drainage 10. Which prescribed action will the nurse implement first for a patient who has vomited 1100 mL of blood? a. Give an IV H2 receptor antagonist. b. Draw blood for typing and crossmatching. c. Administer 1 L of lactated Ringer's solution. d. Insert a nasogastric (NG) tube and connect to suction. CHAPTER 43 – GALLBLADDER DISEASE 1. The surgical treatment of choice for the patient with symptomatic gallbladder disease is a a. cholecystotomy. b. choledocholithotomy. c. Cholecystoduodenostomy d. laparoscopic cholecystectomy. 2. Postoperatively, a patient with an incisional cholecystectomy has a nursing diagnosis of ineffective breathing pattern related to splinted respirations secondary to a high abdominal incision. Which action should the nurse take first? a. Assess heart and lung sounds. b. Administer the prescribed analgesic. c. Position the patient on the operative side. d. Instruct the patient to cough and deep breathe. 3. Which clinical manifestation would the nurse expect a client diagnosed with acute cholecystitis to exhibit? a. Melena, weakness, tachycardia b. Acute right lower quadrant (RLQ) pain, diarrhea, and dehydration c. Ecchymosis petechiae, and coffee-ground emesis d. Nausea, vomiting, and diaphoresis 4. Marie, a 51-year-old woman, is diagnosed with cholecystitis. Which diet, when selected by the client, indicates that the nurse’s teaching has been successful? a. 4-6 small meals of low-fat foods daily b. High-fat, high-carbohydrate meals c. Low-fat, high-carbohydrate meals d. High-fat, low protein meals 5. The nurse recognizes that teaching a 44-year-old woman following a laparoscopic cholecystectomy has been effective when the patient states which of the following? a. I can expect yellow-green drainage from the incision for a few days. b. I can remove the bandages on my incision tomorrow and take a shower. c. I should plan to limit my activities and not return to work for 4 to 6 weeks. d. I will always need to maintain a low-fat diet since I no longer have a gallbladder. 6. A 51-year-old woman had an incisional cholecystectomy 6 hours ago. The nurse will place the highest priority on assisting the patient to a. choose low-fat foods from the menu. b. perform leg exercises hourly while awake. c. ambulate the evening of the operative day. d. turn, cough, and deep breathe every 2 hours. 7. The nurse is planning care for a 48-year-old woman with acute severe pancreatitis. The highest priority patient outcome is a. maintaining normal respiratory function. b. expressing satisfaction with pain control. c. developing no ongoing pancreatic disease. d. having adequate fluid and electrolyte balance. 8. Which action should the nurse in the emergency department take first for a new patient who is vomiting blood? a. Insert a large-gauge IV catheter. b. Draw blood for coagulation studies. c. Check blood pressure (BP), heart rate, and respirations. d. Place the patient in the supine position. 9. Which assessment finding is of most concern for a 46-year-old woman with acute pancreatitis? a. Absent bowel sounds b. Abdominal tenderness c. Left upper quadrant pain d. Palpable abdominal mass CHAPTER 64 – RHEUMATOID ARTHRITIS (RA) & OSTEOARTHRITIS (OA) 1. The nurse determines that teaching about management of osteoarthritis of the feet and hands has been effective when the patient says a. “I will be careful to avoid crowds and people with infections.” b. “I can use heat to relieve the stiffness when I wake up in the morning.” c. “I should exercise my hands every day, especially if they are painful and inflamed.” d. “I should avoid the use of glucosamine as it has been shown to have no therapeutic value.” 2. The nurse is working with a 73-year-old patient with osteoarthritis (OA). In assessing the patient's understanding of this disorder, the nurse concludes teaching has been effective when the patient describes the condition as which of the following? a. Joint destruction caused by an autoimmune process b. Degeneration of articular cartilage in synovial joints c. Overproduction of synovial fluid resulting in joint destruction d. Breakdown of tissue in non-weight-bearing joints by enzymes 3. The nurse is assessing the recent health history of a 63-year-old patient with osteoarthritis (OA). The nurse determines that the patient is trying to manage the condition appropriately when the patient describes which of the following activity patterns? a. Bed rest with bathroom privileges b. Daily high-impact aerobic exercise c. A regular exercise program of walking d. Frequent rest periods with minimal exercise 4. The nurse is admitting a patient who is scheduled for knee arthroscopy related to osteoarthritis (OA). Which of the following findings would the nurse expect to be present on examination of the patient's knees? a. Ulnar drift b. Pain with joint movement c. Reddened, swollen affected joints d. Stiffness that increases with movement 5. The basic pathophysiologic process of rheumatoid arthritis (RA) is a. destruction of joint cartilage and bones by an autoimmune process b. initiated by a viral infection that destroys the synovial membranes of joints c. the presence of HLA-DR4 antigen that causes inflammatory responses throughout the body d. an immune response that activates complement and produces inflammation of joints and other organ systems 6. During the physical assessment of the patient with moderate RA, the nurse would expect to find a. hepatomegaly b. Heberden's nodes c. spindle-shaped fingers d. crepitus on joint movement 7. A 70-year old patient is being evaluated for symptoms of RA. The nurse recognizes that a major problem in the management of RA in the older adult is that a. RA is usually more severe in older adults b. older patients are not as likely to comply with treatment regimens c. drug interactions and toxicity are more likely to occur with multidrug therapy d. laboratory and other diagnostic tests are not effective in identifying RA in older adults 8. After teaching a patient with RA about the prescribed therapeutic regimen, the nurse determines that further instruction is needed when the patient says, a. it is important for me to perform my prescribed exercises every day b. I should perform most of my daily chores in the morning when my energy level is highest c. an ice pack to a joint for 10 minutes may help relieve pain and inflammation when I have an acute flare d. I can use assistive devices such as padded utensils, electric can openers, and elevated toilet seats to protect my joints 9. Which finding will the nurse expect when assessing a 58-year-old patient who has osteoarthritis (OA) of the knee? a. Discomfort with joint movement b. Heberden's and Bouchard's nodes c. Redness and swelling of the knee joint d. Stiffness that increases with movement 10. After the nurse has finished teaching a 68-year-old patient with osteoarthritis (OA) of the right hip about how to manage the OA, which patient statement indicates a need for more teaching? a. "I can take glucosamine to help decrease my knee pain." b. "I will take 1 g of acetaminophen (Tylenol) every 4 hours." c. "I will take a shower in the morning to help relieve stiffness." d. "I can use a cane to decrease the pressure and pain in my hip." 11. The nurse will anticipate the need to teach a 57-year-old patient who has osteoarthritia (OA) about which medication? a. Adalimumab (Humira) b. Prednisone (Deltasone) c. Capsaicin cream (Zostrix) d. Sulfasalazine (Azulfidine) 12. A patient with rheumatoid arthritis (RA) complains to the clinic nurse about having chronically dry eyes. Which action by the nurse is most appropriate? a. Teach the patient about adverse effects of the RA medications. b. Suggest that the patient use over-the-counter (OTC) artificial tears. c. Reassure the patient that dry eyes are a common problem with RA. d. Ask the health care provider about discontinuing methotrexate (Rheumatrex) . 13. The nurse suggests that a patient recently diagnosed with rheumatoid arthritis (RA) plan to start each day with a. a warm bath followed by a short rest. b. a short routine of isometric exercises. c. active range-of-motion (ROM) exercises. d. stretching exercises to relieve joint stiffness. 14. Which assessment information obtained by the nurse indicates that a patient with an exacerbation of rheumatoid arthritis (RA) is experiencing a side effect of prednisone (Deltasone)? a. The patient has joint pain and stiffness. b. The patient's blood glucose is 165 mg/dL. c. The patient has experienced a recent 5-pound weight loss. d. The patient's erythrocyte sedimentation rate (ESR) has increased. 15. Which laboratory data is important to communicate to the health care provider for a patient who is taking methotrexate (Rheumatrex) to treat rheumatoid arthritis? a. The blood glucose is 90 mg/dL. b. The rheumatoid factor is positive. c. The white blood cell (WBC) count is 1500/µL. d. The erythrocyte sedimentation rate is elevated. 16. A patient with OA uses NSAIDs to decrease pain and inflammation. The nurse teaches the patient that common side effects of these drugs include a. allergic reactions, fever, and oral lesions b. fluid retention, hypertension, and bruising c. skin rashes, gastric irritation, and headache d. prolonged bleeding time, blood dyscrasias, and hepatic damage CHAPTER 49 – ENDOCRINE PROBLEMS 1. Which statement accurately describes Graves’ disease? a. Exophthalmos occurs in Graves’ disease b. It is an uncommon form of hyperthyroidism c. Manifestations of hyperthyroidism occur from tissue desensitization to the sympathetic nervous system d. Diagnostic testing in the patient with Graves’ disease will reveal an increased thyroid stimulating hormone (TSH) level 2. A patient with Graves’ disease asks the nurse what caused the disorder. What is the best response by the nurse? a. “The cause of Graves’ disease is not known, but it is thought to be genetic” b. “It is usually associated with a goiter formation from an iodine deficiency over a long period of time” c. “Antibodies develop against thyroid tissue and destroy it, causing a deficiency of thyroid hormones” d. “In genetically susceptible persons, antibodies are formed that cause excessive thyroid hormone excretion” 3. The nurse is caring for a patient who just returned to the surgical unit following a thyroidectomy. The nurse is most concerned if which is observed? a. The patient complains of increased thirst. b. The patient reports a sore throat when swallowing. c. The patient supports her head when moving in bed. d. The patient makes harsh, vibratory sounds when breathing. 4. What is a cause of primary hypothyroidism in adults? a. Malignant or benign thyroid nodules b. Surgical removal or failure of the pituitary gland c. Surgical removal or failure of the thyroid gland d. Autoimmune-induced atrophy of the thyroid gland 5. What characteristic is related to hashimoto’s thyroiditis? a. Enlarged thyroid gland b. Viral-induced hyperthyroidism c. Bacterial or fungal infection of the thyroid gland d. Chronic autoimmune thyroiditis with antibody destruction of thyroid tissue 6. The nurse administers corticosteroids to a patient with acute adrenal insufficiency. The nurse determines that treatment is effective if what is observed? a. The patient is alert and oriented. b. The patient’s lung sounds are clear. c. The patient’s urinary output decreases. d. The patient’s potassium level is 5.7 mEq/L. 7. An IV hydrocortisone infusion is started before a patient is taken to surgery for a bilateral adrenalectomy. Which explanation, if given by the nurse, is most appropriate? a. “The medication prevents sodium and water retention after surgery.” b. “The drug prevent clots from forming in the legs during your recovery from surgery.” c. “This medicine is given to help your body respond to stress after removal of the adrenal glands.” d. “This drug stimulates your immune system and promotes wound healing.” 8. Which information will the nurse teach a 48-year-old patient who has been newly diagnosed with Graves' disease? a. Exercise is contraindicated to avoid increasing metabolic rate. b. Restriction of iodine intake is needed to reduce thyroid activity. c. Antithyroid medications may take several months for full effect. d. Surgery will eventually be required to remove the thyroid gland. 9. A patient who had a subtotal thyroidectomy earlier today develops laryngeal stridor and a cramp in the right hand upon returning to the surgical nursing unit. Which collaborative action will the nurse anticipate next? a. Suction the patient's airway. b. Administer IV calcium gluconate. c. Plan for emergency tracheostomy. d. Prepare for endotracheal intubation. 10. Which nursing action will be included in the plan of care for a 55-year-old patient with Graves' disease who has exophthalmos? a. Place cold packs on the eyes to relieve pain and swelling. b. Elevate the head of the patient's bed to reduce periorbital fluid. c. Apply alternating eye patches to protect the corneas from irritation. d. Teach the patient to blink every few seconds to lubricate the corneas. 11. A 62-year-old patient with hyperthyroidism is to be treated with radioactive iodine (RAI). The nurse instructs the patient a. about radioactive precautions to take with all body secretions. b. that symptoms of hyperthyroidism should be relieved in about a week. c. that symptoms of hypothyroidism may occur as the RAI therapy takes effect. d. to discontinue the antithyroid medications taken before the radioactive therapy. 12. Which nursing assessment of a 69-year-old patient is most important to make during initiation of thyroid replacement with levothyroxine (Synthroid)? a. Fluid balance b. Apical pulse rate c. Nutritional intake d. Orientation and alertness 13. An 82-year-old patient in a long-term care facility has several medications prescribed. After the patient is newly diagnosed with hypothyroidism, the nurse will need to consult with the health care provider before administering a. docusate (Colace). b. ibuprofen (Motrin). c. diazepam (Valium). d. cefoxitin (Mefoxin). 14. A patient who was admitted with myxedema coma and diagnosed with hypothyroidism is improving and expected to be discharged in 2 days. Which teaching strategy will be best for the nurse to use? a. Provide written reminders of self-care information. b. Offer multiple options for management of therapies. c. Ensure privacy for teaching by asking visitors to leave. d. Delay teaching until patient discharge date is confirmed. 15. Which finding for a patient who has hypothyroidism and hypertension indicates that the nurse should contact the health care provider before administering levothyroxine (Synthroid)? a. Increased thyroxine (T4) level b. Blood pressure 112/62 mm Hg c. Distant and difficult to hear heart sounds d. Elevated thyroid stimulating hormone level 16. A 37-year-old patient is being admitted with a diagnosis of Cushing syndrome. Which findings will the nurse expect during the assessment? a. Chronically low blood pressure b. Bronzed appearance of the skin c. Purplish streaks on the abdomen d. Decreased axillary and pubic hair 17. A 44-year-old female patient with Cushing syndrome is admitted for adrenalectomy. Which intervention by the nurse will be most helpful for a nursing diagnosis of disturbed body image related to changes in appearance? a. Reassure the patient that the physical changes are very common in patients with Cushing syndrome. b. Discuss the use of diet and exercise in controlling the weight gain associated with Cushing syndrome. c. Teach the patient that the metabolic impact of Cushing syndrome is of more importance than appearance. d. Remind the patient that most of the physical changes caused by Cushing syndrome will resolve after surgery. 18. Which finding indicates to the nurse that the current therapies are effective for a patient with acute adrenal insufficiency? a. Increasing serum sodium levels b. Decreasing blood glucose levels c. Decreasing serum chloride levels d. Increasing serum potassium levels 19. A 38-year-old male patient is admitted to the hospital in Addisonian crisis. Which patient statement supports a nursing diagnosis of ineffective self-health management related to lack of knowledge about management of Addison's disease? a. "I frequently eat at restaurants, and my food has a lot of added salt." b. "I had the stomach flu earlier this week, so I couldn't take the hydrocortisone." c. "I always double my dose of hydrocortisone on the days that I go for a long run." d. "I take twice as much hydrocortisone in the morning dose as I do in the afternoon." 20. A 29-year-old woman with systemic lupus erythematosus has been prescribed 2 weeks of high-dose prednisone therapy. Which information about the prednisone is most important for the nurse to include? a. "Weigh yourself daily to monitor for weight gain caused by increased appetite." b. "A weight-bearing exercise program will help minimize the risk for osteoporosis." c. "The prednisone dose should be decreased gradually rather than stopped suddenly." d. "Call the health care provider if you experience mood alterations with the prednisone." 21. A patient has just arrived on the unit after a thyroidectomy. Which action should the nurse take first? a. Observe the dressing for bleeding. b. Check the blood pressure and pulse. c. Assess the patient's respiratory effort. d. Support the patient's head with pillows. 22. The nurse is caring for a patient following an adrenalectomy. The highest priority in the immediate postoperative period is to a. protect the patient's skin. b. monitor for signs of infection. c. balance fluids and electrolytes. d. prevent emotional disturbances. 23. Which prescribed medication should the nurse administer first to a 60-year-old patient admitted to the emergency department in thyroid storm? a. Propranolol (Inderal) b. Propylthiouracil (PTU) c. Methimazole (Tapazole) d. Iodine (Lugol's solution) 24. Which assessment finding for a 33-year-old female patient admitted with Graves' disease requires the most rapid intervention by the nurse? a. Bilateral exophthalmos b. Heart rate 136 beats/minute c. Temperature 103.8° F (40.4° C) d. Blood pressure 166/100 mm Hg 25. A 37-year-old patient has just arrived in the postanesthesia recovery unit (PACU) after a thyroidectomy. Which information is most important to communicate to the surgeon? a. The patient reports 7/10 incisional pain. b. The patient has increasing neck swelling. c. The patient is sleepy and difficult to arouse. d. The patient's cardiac rate is 112 beats/minute. 26. Which assessment finding of a 42-year-old patient who had a bilateral adrenalectomy requires the most rapid action by the nurse? a. The blood glucose is 176 mg/dL. b. The lungs have bibasilar crackles. c. The blood pressure (BP) is 88/50 mm Hg. d. The patient reports 5/10 incisional pain. 27. After receiving change-of-shift report about the following four patients, which patient should the nurse assess first? a. A 31-year-old female with Cushing syndrome and a blood glucose level of 244 mg/dL b. A 70-year-old female taking levothyroxine (Synthroid) who has an irregular pulse of 134 c. A 53-year-old male who has Addison's disease and is due for a scheduled dose of hydrocortisone (Solu-Cortef). d. A 22-year-old male admitted with syndrome of inappropriate antidiuretic hormone (SIADH) who has a serum sodium level of 130 mEq/L 28. Which finding by the nurse when assessing a patient with Hashimoto's thyroiditis and a goiter will require the most immediate action? a. New-onset changes in the patient's voice b. Apical pulse rate at rest 112 beats/minute c. Elevation in the patient's T3 and T4 levels d. Bruit audible bilaterally over the thyroid gland 29. Which information obtained by the nurse in the endocrine clinic about a patient who has been taking prednisone (Deltasone) 40 mg daily for 3 weeks is most important to report to the health care provider? a. Patient's blood pressure is 148/94 mm Hg. b. Patient has bilateral 2+ pitting ankle edema. c. Patient stopped taking the medication 2 days ago. d. Patient has not been taking the prescribed vitamin D. CHAPTER 45 & 46 – RENAL & UROLOGIC PROBLEMS 1. The nurse plans care for the patient with acute post-streptococcal glomerulonephritis (APSG) based on what knowledge? a. Most patients with APSGN recover completely or rapidly improve with conservative management. b. Chronic glomerulonephritis leading to renal failure is a common sequela to acute glomerulonephritis. c. Pulmonary hemorrhage may occur as a result of antibodies also attacking the alveolar basement membrane. d. A large percentage of patients with apsgn develop rapidly progressive glomerulonephritis, resulting in kidney failure. 2. The nurse determines that instruction regarding prevention of future urinary tract infection (UTIs) has been effective for a 22-year-old female patient with cystitis when the patient states which of the following? a. "I can use vaginal sprays to reduce bacteria." b. "I will drink a quart of water or other fluids every day." c. "I will wash with soap and water before sexual intercourse." d. "I will empty my bladder every 3 to 4 hours during the day." 3. When admitting a patient with acute glomerulonephritis, it is most important that the nurse ask the patient about a. recent sore throat and fever. b. history of high blood pressure. c. frequency of bladder infections. d. family history of kidney stones. 4. Which finding by the nurse for a patient admitted with glomerulonephritis indicates that treatment has been effective? a. The patient denies pain with voiding. b. The urine dipstick is negative for nitrites. c. Peripheral and periorbital edema is resolved. d. The antistreptolysin-O (ASO) titer is decreased. 5. A patient's renal calculus is analyzed as being very high in uric acid. To prevent recurrence of stones, the nurse teaches the patient to avoid eating a. milk and dairy products. b. legumes and dried fruits. c. organ meats and sardines. d. spinach, chocolate, and tea. 6. To prevent the recurrence of renal calculi, the nurse teaches the patient to: a. use a filter to strain all urine. b. avoid dietary sources of calcium. c. drink diuretic fluids such as coffee. d. have 2000 to 3000 mL of fluid a day. 7. A 78-year-old who has been admitted to the hospital with dehydration is confused and incontinent of urine. Which nursing action will be best to include in the plan of care? a. Apply absorbent incontinent pads. b. Restrict fluids after the evening meal. c. Insert an indwelling catheter until the symptoms have resolved. d. Assist the patient to the bathroom every 2 hours during the day. 8. A patient with renal calculi is hospitalized with gross hematuria and severe colicky left flank pain. Which nursing action will be of highest priority at this time? a. Encourage oral fluid intake. b. Administer prescribed analgesics. c. Monitor temperature every 4 hours. d. Give antiemetics as needed for nausea. 9. The nurse observes nursing assistive personnel (NAP) taking the following actions when caring for a patient with a retention catheter. Which action requires that the nurse intervene? a. Taping the catheter to the skin on the patient's upper inner thigh b. Cleaning around the patient's urinary meatus with soap and water c. Using an alcohol-based hand cleaner before performing catheter care d. Disconnecting the catheter from the drainage tube to obtain a specimen 10. A patient undergoes a nephrectomy after having massive trauma to the kidney. Which assessment finding obtained postoperatively is most important to communicate to the surgeon? a. Blood pressure is 102/58. b. Incisional pain level is 8/10. c. Urine output is 20 mL/hr for 2 hours. d. Crackles are heard at both lung bases. 11. The nurse teaches a patient with chronic kidney disease about prevention of complications. What should the nurse include in the teaching plan? a. monitor for proteinuria daily with a urine dipstick. b. perform self-catheterization every 4 hours to measure urine. c. take calcium-based phosphate binders on an empty stomach. d. check weight daily and report a gain of greater than 4 pounds. 12. A patient undergoes peritoneal dialysis exchanges several times each day. What should the nurse plan to increase in the patient’s diet? a. Fat b. Protein c. Calories d. Carbohydrates CHAPTER 21 – VISUAL & AUDITORY PROBLEMS 1. Your patient has glaucoma. Which medication class should be questioned? a. Opioid pain meds b. Anticholinergics c. Benzodiazepines d. Beta-blockers 2. The nurse instructs a patient with primary open-angle glaucoma about the disorder. Which of the following statements, if made by the nurse, is most appropriate? a. “The retinal nerve is damaged by an abnormal increase in the production of aqueous humor.” b. Aqueous humor cannot drain from the eye, causing pressure damage to the optic nerve.” c. “As the lens enlarges with aging, it pushes the iris forward, covering the outflow channels of the eye.” d. “The lens blocks the pupillary opening, preventing the flow of aqueous humor into the anterior chamber. “ a. 3. How are cataracts diagnosed? Choose all that apply: a. Visual Acuity test b. Patient report of seeing “floaters” c. Slit Lamp d. Ophthalmoscope e. Recent viral infection 4. What is cataracts? a. loss of vision in one eye b. cloudiness of the lens c. loss of peripheral vision d. separation of the retina 5. What medications should the nurse expect to administer pre-operatively (choose all that apply)? a. General anesthesia b. Corticosteroids c. Pupillary Constricting drops d. Pupillary Dilation drugs [Show More]
Last updated: 1 year ago
Preview 1 out of 44 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 17, 2020
Number of pages
44
Written in
Additional information
This document has been written for:
Uploaded
Jul 17, 2020
Downloads
0
Views
54

 Rasmussen College.png)









.png)