*NURSING > ATI MEDICAL SURGICAL > ATI MED-SURG 1 TEST 2|questions,answers with their rationales (latest summer 2021) (All)
ATI MED-SURG 1 TEST 2|questions,answers with their rationales (latest summer 2021)
Document Content and Description Below
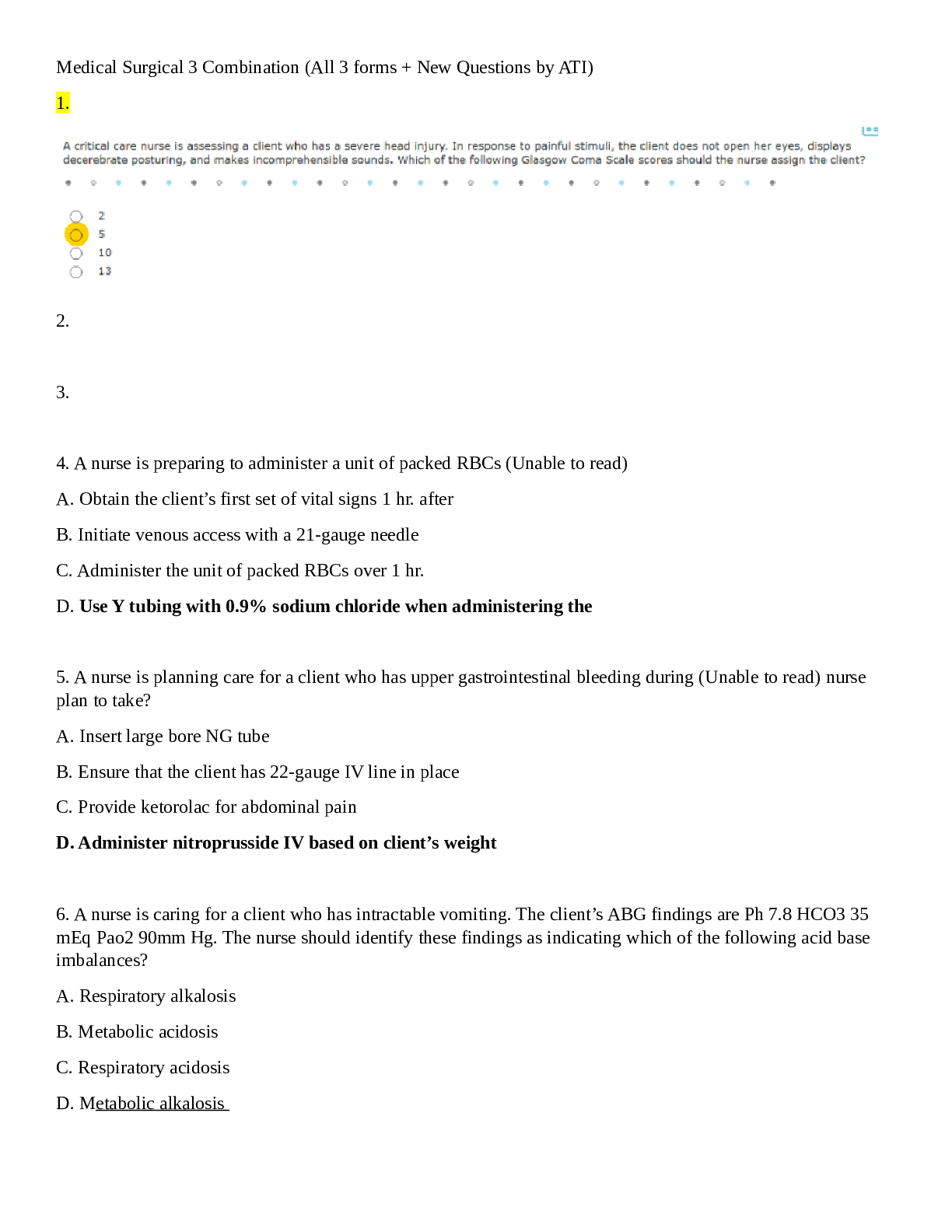
AIIH MED-SURG 1 TEST 2 1. The client undergoing preoperative assessment before an elective procedure tells the nurse that she has been taking 10 mg of prednisone daily for rheumatoid arthritis. Wha... t is the nurse’s best action? A. Notify the surgeon and anesthesiologist. B. Document the information as the only action. C. Reschedule the surgery in 2 weeks when the client has cleared the drug from her system. D. Suggest that the client switch to a nonsteroidal anti-inflammatory agent for pain relief. 2. How does palliative surgery differ from any other type of surgery? A. The main purpose is cosmetic in nature rather than functional repair or comfort. B. There are fewer risks associated with palliative surgery than with any other type of surgery. C. The outcomes of palliative surgery cannot be ensured to produce the desired effect or restoration of functional ability. D. Palliative surgery is performed to provide temporary relief of distressing symptoms rather than to cure a problem or condition. 3. While examining the 82-year-old client's preoperative laboratory blood tests, the nurse finds the client's serum sodium level to be 139 mEq/mL. What is the nurse’s best action? A. Increase the IV flow rate. B. Initiate oxygen therapy by mask. C. Document the finding as the only action. D. Notify the surgeon and anesthesiologist. 4. The client who is scheduled to have surgery cannot read or write. The surgeon obtaining the consent wants to have the client's spouse sign the consent instead. What is the nurse’s best action? A. Nothing; a signed informed consent statement does not need to be obtained from this client. B. Locate the spouse, because the informed consent statement must be signed by the client's closest relative. C. Inform the surgeon that the client may sign the informed consent statement with an X in front of two witnesses. D. Notify the administration because the court must appoint a legal guardian to represent the client's best interests and give consent for all surgical procedures. 5. When asked about allergies, the preoperative client tells the nurse she has allergies to all of the following substances. Which allergy alerts the nurse to potential problems in relation to the scheduled surgery? A. Pollens B. Bee stings C. Shellfish D. Peanuts 6. The client is NPO for surgery scheduled to occur in 4 hours. It is now 9 AM and the client's normal oral medications (consisting of digoxin, 0.125 mg, Colace, 300 mg, and Feostat, 325 mg) are due to be administered. The physician will not be available until the time of surgery. What is the nurse’s best action? A. Hold all medications. B. Administer all medications orally. C. Administer all medications parenterally. D. Administer digoxin with minimal water and hold the other drugs. 7. Twenty minutes after the client has received a preoperative injection of atropine and midazolam (Versed), the client tells the nurse that he must be allergic to the medication because his mouth is dry and his heart seems to be beating faster than normal. What is the nurse’s best first action? A. Document the findings as the only action. B. Check the client's pulse and blood pressure. C. Prepare to administer epinephrine and diphenhydramine (Benadryl). D. Explain to the client that these symptoms are normal responses to the medication. 8. The client scheduled to have surgery within the next 2 hours tells the nurse during the admission interview the following information. Which piece of information should the nurse be certain to communicate on the outside of the chart for the entire surgical team to know? A. The client is allergic to cats. B. The client is hard of hearing. C. The client had a glass of wine 12 hours ago. D. The client takes 2000 mg of vitamin C each day. 9. Which statement made by the client indicates a need for further teaching? A. “These exercises help prevent blood clots.” B. “Once I am up and walking around, I won't need to do these as often.” C. “Keeping my knees bent will prevent my arthritis from making me so stiff.” D. “If I feel pain in my calf when I bend my ankles up and down, I should tell my nurse.” 10. The client’s surgery has been delayed because of hyperkalemia. The client doesn’t understand why. What is the nurse’s best response? A. “Potassium affects how the heart works and you could have a heart attack if this is not corrected.” B. “Your kidneys could quit working during surgery and the surgery would have to be cancelled.” C. “We want you to have the best recovery after surgery. Sometimes, if this problem is not corrected before surgery, you may be too sleepy after surgery to talk to your family.” D. “By making sure your potassium is normal before surgery, it will keep your heart functioning at its best during your surgery.” 11. Which nursing action or statement is most likely to reduce anxiety in a client being brought to the surgical suite? A. Asking the client if he or she has talked with the hospital chaplain B. Asking the client what specific surgery he or she is having done today C. Asking the client if he or she wants family members to be with them in the holding area D. Explaining to the client that the surgical area is the most technologically advanced in the city 12. Which task or function during a surgical procedure is designated as being within the scope of practice for the scrub nurse? A. Closing the surgical wound B. Setting up the sterile field C. Administering blood products D. Monitoring the client's cardiopulmonary function 13. Which is the best technique to use when rinsing hands and forearms after a surgical scrub? A. Rinsing is not performed after a surgical scrub because it will reduce the antimicrobial activity of the cleansing solution. B. Rinsing should start at the hand, with water running up the forearm. C. Rinsing should start at the elbow, with water running down to the hand. D. Rinsing should start with the hand positioned so that water runs off the extremity rather than up or down. ANS: D The object of a surgical scrub and rinse is to remove as many microorganisms and as much skin debris as possible. Rinsing so that water runs off rather than up or down the extremity limits the chance for loose debris and contaminants to move onto scrubbed surfaces. 14. In the operating room, the client tells the circulating nurse that he is going to have the cataract in his left eye removed. The nurse notes that the consent form indicates that surgery is to be performed on the right eye. What is the nurse’s best first action? A. Assume that the client is a little confused because he is older and has received midazolam intramuscularly. B. Check to see if the client has received any preoperative medications. C. Notify the surgeon and anesthesiologist. D. Ask the client his name. 15. The client is to undergo a gynecologic surgical procedure that requires the client to be in the lithotomy position. At what point should the circulating nurse place the client in the lithotomy position? A. Before anesthesia is administered to allow the client to move her legs herself and tell the nurse if any discomfort is being felt B. During stage 1 of general anesthesia to take advantage of the client's relaxed state C. During stage 2 of general anesthesia to ensure that the client will not be embarrassed by the position D. During stage 3 of general anesthesia to avoid overstimulating the client or disrupting the attainment of a patent airway 16. What is the priority nursing diagnosis for the client under general anesthesia during surgery? A. Acute Pain related to surgical procedure B. Risk for Infection related to surgical wound C. Risk for Impaired Skin Integrity related to prolonged static position D. Disturbed Body Image related to presence of surgical wound or scar 17. During which of the following types of anesthesia should the nurse expect the client to maintain a gag reflex during surgery? A. Inhalation of general anesthesia B. Intravenous general anesthesia C. Balanced anesthesia D. Regional anesthesia 18. Which nursing intervention by the circulating nurse is most important for clients having surgery under regional anesthesia? A. Monitoring respiratory rate and depth B. Positioning for safety and comfort C. Minimizing external noise and stimuli D. Planning for nonpharmacologic pain interventions 19. Which of the following method is the best for correctly identifying the client prior to surgery? A. Ask the client his or her date of birth and confirm it with the chart. B. Ask the client his or her name and social security number. C. Check the client’s armband and ask his or her name. D. Check the client’s medical record number and surgical consent form. 20. Which function or assessment finding in a client being admitted to the postanesthesia care unit after surgery is the best indication that the client's respiratory status does not require immediate attention? A. The client is able to talk. B. The client is alert and oriented. C. The client's oxygen saturation is 90%. D. The client's chest rises and falls rhythmically during respiration. 21. Which assessment finding in a postoperative client indicates to the nurse that the interventions to prevent hypovolemia need to be re-evaluated? A. The blood pressure changes from 136/80 to 122/80 mm Hg. B. The urine output decreases from 40 to 10 mL/hour. C. The client cannot count backward from 100 by threes. D. The client's temperature has changed from 100.2° to 100.4° F. 22. The client is admitted to the postanesthesia care unit (PACU) after surgery that took place with the client in the lithotomy position. Which change in assessment findings alerts the nurse to a possible complication of this surgical position? A. The electrocardiogram (ECG) shows tall, peaked T waves and wide QRS complexes. B. The client only arouses in response to light shaking. C. The pulse pressure has increased from 28 to 40 mm Hg. D. The dorsalis pedis pulses are not palpable bilaterally. 23. In checking the neurologic status of the client just admitted to the PACU, the nurse notes that the right eye pupil is dilated more than the left pupil. What is the nurse’s best first action? A. Check the client's chart to compare these findings to the client's baseline neurologic assessment. B. Raise the head of the bed up to a 30-degree angle and administer oxygen. C. Test the client's deep tendon reflexes on all four extremities. D. Notify the physician and document the finding. 24. Which client is at greatest risk for respiratory complications after surgery under general anesthesia? A. 65-year-old woman taking a calcium channel blocker for hypertension B. 55-year-old man with chronic allergic rhinitis C. 45-year-old woman with diabetes mellitus type 1 D. 35-year-old man who smokes two packs of cigarettes daily 25. One hour after admission to the PACU, the postoperative client has become very restless. What is the nurse’s best first action? A. Ask the client if he or she is having pain. B. Check the client's oxygen saturation level. C. Document the finding as the only action. D. Explain to the client that he or she is in the “recovery room” after surgery. 26. The postoperative client's arterial blood gas values are pH 7.22, HCO – 21 mEq/L, PCO 65 mm Hg, and PO2 58 mm Hg. What is the nurse’s best first action? A. Notify the physician. B. Assess the client's airway. C. Increase the oxygen flow rate. D. Document the finding as the only action. 27. Two hours after abdominal surgery, the nurse auscultates the client's abdomen. No bowel sounds are present. What is the nurse’s best first action? A. Position the client on the right side with the bed flat. B. Check the dressing and apply an abdominal binder. C. Palpate the bladder and measure abdominal girth. D. Document the finding as the only action. 28.The client who is 24 hours postoperative from abdominal surgery has light brown fluid with small particles that look like coffee grounds in the NG tube drainage. What is the nurse’s best action? A. Notify the physician. B. Irrigate the tube with normal saline. C. Clamp the tube and advance it 1 to 2 inches. D. Document the finding as the only action. 29. When changing the client's abdominal dressing on the second postoperative day, the nurse notes crusting on about half of the suture line and oozing of a small amount of serosanguineous drainage. What is the nurse’s best action? A. Clean the suture line gently and apply new dressings. B. Gently remove the crusts and culture the material beneath. C. Remove the sutures or staples in the area where crusts have formed. D. Apply a binder over the incision and notify the surgeon. 30. The client is 4 days postoperative from a bowel resection and has a large abdominal incision. When the nurse enters the client's room, he tells her that he felt the incision “pop” when he coughed just a moment ago. What is the nurse’s best response? A. “It is good that you are coughing and deep breathing to prevent lung complications.” B. “That is a normal feeling in the incision whenever you are moving.” C. “Be sure to splint the incision with a pillow or your hands when you cough.” D. “Lie down flat on the bed and let me examine your incision.” 31. When a nurse checks a postoperative client for pain relief 30 minutes after the client started patient-controlled analgesia (PCA) with morphine, the client is sleeping and has a respiratory rate of 8 breaths/minute. What is the nurse’s best first action? A. Attempt to arouse the client by calling his or her name and lightly shaking the client's arm. B. Administer oxygen by mask and apply an apnea monitor. C. Document the finding as the only action. D. Notify the physician immediately. 32. Which precaution or issue should the nurse reinforce to the postoperative client about correct use of the patient-controlled analgesia (PCA) device? A. “Push the button when you feel the pain beginning rather than waiting until the pain is at its worst.” B. “Push the button every 15 minutes whether you feel pain at that time or not.” C. “Instruct your family or visitors to press the button for you when you are sleeping.” D. “Try to go as long as you possibly can before you press the button.” 33. Which maneuver or technique should the nurse avoid to prevent pulmonary emboli in a postoperative client? A. Application of elastic wraps to the lower extremities B. Measuring calf circumference every shift C. Calf muscle massage D. Early ambulation 34. What dietary modifications should the nurse teach to the client who is going home with an extensive wound after surgery? A. “Drink at least 4 L of fluid every day.” B. “Eating dietary fiber can help prevent constipation.” C. “Be sure you are getting adequate amounts of vitamin C in your diet.” D. “Try to lose weight so that you don't put too much strain on the incision.” 35. A maintenance man falls from a ladder into the unit hall, striking his head on some equipment. The man is unconscious and not breathing; the Code Team has already been paged and is on its way. The nurse should: 1. wait for the team to start CPR. 2. open airway with a jaw thrust. 3. give two rescue breaths after extending the neck. 4. start chest compressions. 36. Standing in a fast food line, the person in front, while munching on a cookie, begins to cough heavily, with deep inspirations, and waves his arms around wildly. The nurse should immediately: 1. start rescue breathing as quickly as possible. 2. start chest compressions as quickly as possible. 3. perform the Heimlich maneuver. 4. do nothing at this point as long as there is air exchange. 37. One-person CPR principles, as taught and practiced by professional nurses, require that the initial intervention for an unconscious patient who is not breathing is to: 1. lift the jaw to clear the airway. 2. call for assistance. 3. start chest compressions. 4. make two rescue breaths. 38. The nurse assesses that the patient is in shock based on the findings of: 1. lack of urine output in the last hour, thready pulse, shallow respirations, decreased BP, and patient crying softly. 2. failure of the neurological system, thready pulse, decreased respirations, decreased BP, and decreased LOC. 3. failure of the renal system with bounding pulse, shallow respirations, decreased BP, 300 mL urine in the last hour, displaying unfounded anger. 4. unable to arouse patient, temperature 99.2º F, pulse 100, respiration 30, BP 120/78. 39. The nurse comes upon a traffic accident. One passenger is lying on the ground by an open door. The nurse stops and begins immediate nursing interventions by proceeding with assessing: 1. for uncontrolled bleeding. 2. ABC: airway, breathing, and circulation. 3. for abdominal deep wounds. 4. level of LOC and orientation. 40. The nurse finds a patient slumped to the floor and unconscious, with no pulse or respiration. The nurse should begin the protocol of: 1. basic life support. 2. advanced life support. 3. cardiopulmonary resuscitation. 4. first aid care. 41. As an immediate treatment for epistaxis, the nurse should give the following instructions: 1. “Stand still, lean your head backward so that the blood won’t get all over everything, and pinch your nose shut for at least 10 minutes.” 2. “Stand still, lean your head forward, and pinch your nose tightly for at least 10 minutes.” 3. “Sit down on a solid surface, lean your head forward to let the blood run out, and then pinch your nose closed for at least 30 minutes.” 4. “Sit down on a solid surface, lean your head forward so that you don’t choke on the blood, and pinch your nose shut for at least 10 minutes.” 42. Which condition complicates the assessment of an older adult patient with a suspected head injury? 1. Sensory deficits 2. Slowed metabolism 3. Preexisting cerebral dysfunction 4. Decreased pulmonary function 43. The nurse is called on to assist a neighbor who needs first aid. The nurse knows that legal responsibility for this action would be that the nurse: 1. is legally bound to help in any way possible. 2. is expected to demonstrate the same skill, knowledge, and care that would be provided by other nurses in the same community with the same credentials. 3. has no legal responsibilities outside the hospital setting and would be held accountable for nothing. 4. can legally perform any aid skill, even those not allowed the nurse in the hospital. 44. A nurse comes upon a traffic accident where there are injured, unconscious people lying on the highway. The nurse is aware that first aid interventions are sanctioned by the: 1. Good Samaritan Act. 2. Emergency Care Doctrine. 3. Fifth Amendment. 4. Liability Protection Against Malpractice Act. 45. The nurse giving discharge instructions to the patient who is severely allergic to insect stings would caution the patient to: 1. wear bright colors to repel insects. 2. apply perfume liberally as a protection. 3. dress in sleeveless, easily removable garments. 4. obtain an emergency treatment kit. 46. The patient is admitted to the emergency room after having been bitten on the hand by a black widow spider. The nursing intervention that is indicated is to: 1. monitor for respiratory distress. 2. wrap the hand in a warm compress. 3. seat the patient upright in a chair. 4. elevate the patient’s hand above his or her heart. 47. The nurse can cease CPR when there is: 1. spontaneous breathing and absence of dyspnea. 2. spontaneous breathing and absence of cyanosis. 3. heartbeat and spontaneous breathing. 4. heartbeat and return of consciousness. 48. When the accident victim presents to the emergency room with an open sucking chest wound, the nurse should apply to the wound: 1. occlusive dressing taped on four sides. 2. tight Ace bandage wrap. 3. no dressing of any sort. 4. flutter dressing taped on three sides. 49.A homeless person is brought to the ER after having been found asleep on a park bench under a layer of snow. He has a rectal temperature of 97 F. The nurse anticipates which of the following additional symptoms? 1. Diminished breath sounds, inadequate chest expansion 2. Shivering, decreased heart rate, and increased blood pressure 3. Confusion, increased hunger, hypertension 4. Decreased irregular heart and respiratory rates, decreased blood pressure 50.A mother brings in her 2-year-old who has drunk gasoline 1 hour ago. After initial assessment, the nurse will: 1. prepare to administer syrup of ipecac. 2. turn patient on the stomach to induce vomiting. 3. prepare to administer milk of magnesia. 4. prepare to administer bowel lavage and cathartics. [Show More]
Last updated: 1 year ago
Preview 1 out of 16 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 30, 2021
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
Apr 30, 2021
Downloads
0
Views
42

.png)

 – Chamberlain College of Nursing.png)