Pharmacology > EXAM > NR 508 Advanced Pharmacology Quiz 3 Spring 2019 – Chamberlain College of Nursing / NR508 Advanced (All)
NR 508 Advanced Pharmacology Quiz 3 Spring 2019 – Chamberlain College of Nursing / NR508 Advanced Pharmacology Quiz 3 Spring 2019
Document Content and Description Below
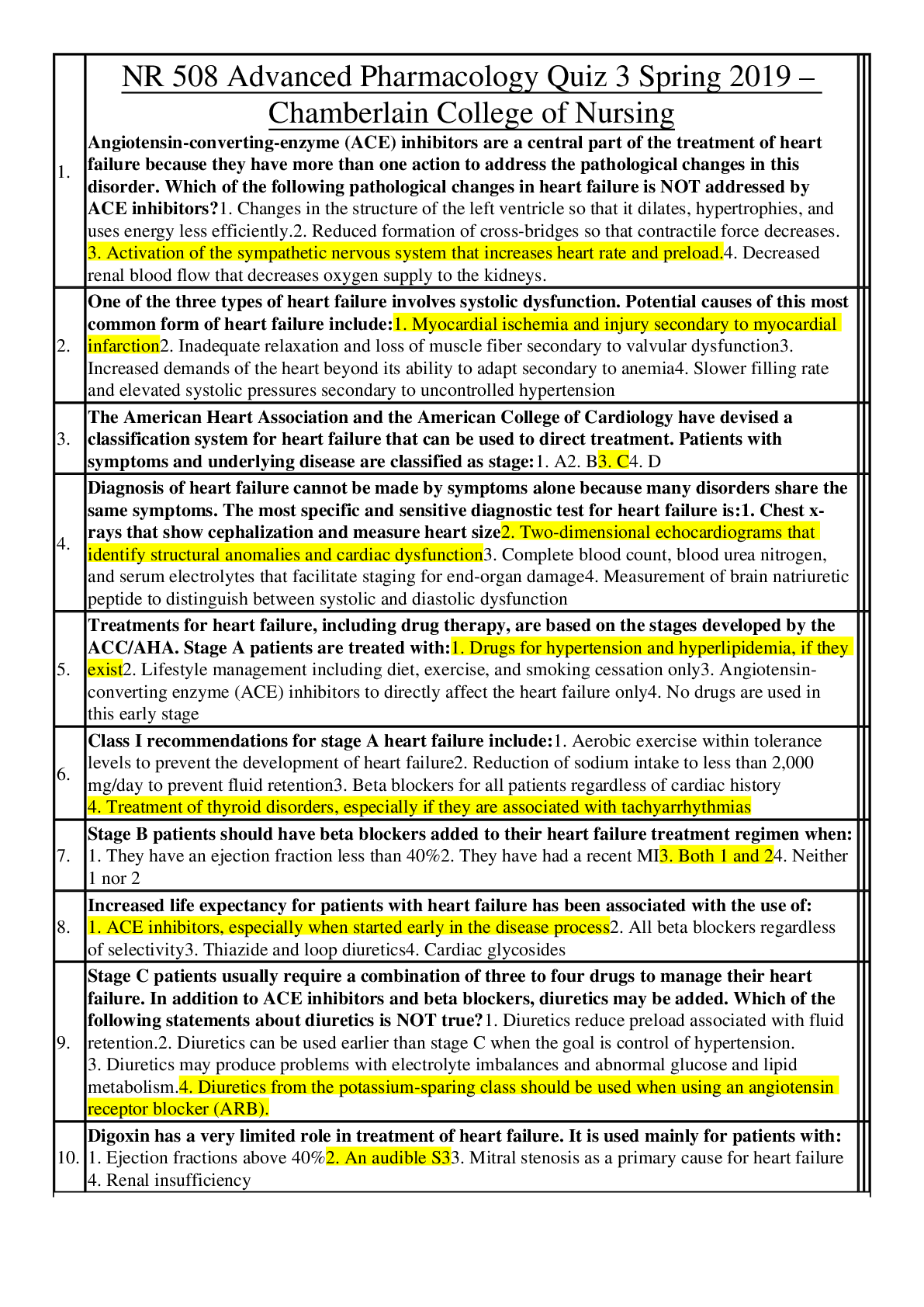
1. NR 508 Advanced Pharmacology Quiz 3 Spring 2019 – Chamberlain College of Nursing Angiotensin-converting-enzyme (ACE) inhibitors are a central part of the treatment of heart failure because they... have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors? 1. Changes in the structure of the left ventricle so that it dilates, hypertrophies, and uses energy less efficiently. 2. Reduced formation of cross-bridges so that contractile force decreases. 3. Activation of the sympathetic nervous system that increases heart rate and preload. 4. Decreased renal blood flow that decreases oxygen supply to the kidneys. 2. One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include: 1. Myocardial ischemia and injury secondary to myocardial infarction 2. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction 3. Increased demands of the heart beyond its ability to adapt secondary to anemia 4. Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension 3. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as stage: 1. A 2. B 3. C 4. D 4. Diagnosis of heart failure cannot be made by symptoms alone because many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is: 1. Chest x-rays that show cephalization and measure heart size 2. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction 3. Complete blood count, blood urea nitrogen, and serum electrolytes that facilitate staging for end-organ damage 4. Measurement of brain natriuretic peptide to distinguish between systolic and diastolic dysfunction 5. Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with: 1. Drugs for hypertension and hyperlipidemia, if they exist 2. Lifestyle management including diet, exercise, and smoking cessation only 3. Angiotensin-converting enzyme (ACE) inhibitors to directly affect the heart failure only 4. No drugs are used in this early stage 6. Class I recommendations for stage A heart failure include: 1. Aerobic exercise within tolerance levels to prevent the development of heart failure 2. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention 3. Beta blockers for all patients regardless of cardiac history 4. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias 7. Stage B patients should have beta blockers added to their heart failure treatment regimen when: 1. They have an ejection fraction less than 40% 2. They have had a recent MI 3. Both 1 and 2 4. Neither 1 nor 2 8. Increased life expectancy for patients with heart failure has been associated with the use of: 1. ACE inhibitors, especially when started early in the disease process 2. All beta blockers regardless of selectivity 3. Thiazide and loop diuretics 4. Cardiac glycosides 9. Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true? 1. Diuretics reduce preload associated with fluid retention. 2. Diuretics can be used earlier than stage C when the goal is control of hypertension. 3. Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism. 4. Diuretics from the potassium-sparing class should be used when using an angiotensin receptor blocker (ARB). 10. Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with: 1. Ejection fractions above 40% 2. An audible S3 3. Mitral stenosis as a primary cause for heart failure 4. Renal insufficiency 11. Which of the following classes of drugs is contraindicated in heart failure? 1. Nitrates 2. Long-acting dihydropyridines 3. Calcium channel blockers 4. Alpha-beta blockers 12. Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is: 1. Aldosterone antagonists 2. Eplerenone 3. ACE inhibitors 4. ARBs 13. ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes is considered to be safe, at least in the later parts of pregnancy? 1. Diuretics 2. ARBs 3. Beta blockers 4. Nitrates 14. Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: 1. Symptoms markedly worsen or the patient becomes hypotensive and has syncope 2. There is evidence of progressive renal insufficiency or failure 3. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic 4. Any of the above 15. ACE inhibitors are a foundational medication in HF. Which group of patients cannot take them safely? 1. Elderly patients with reduced renal clearance 2. Pregnant women 3. Women under age 30 4. 1 and 2 16. What assessment that can be done at home is the most reliable for making decisions to change HF medications? 1. Weight 2. BP 3. Heart rate 4. Serum Glucose 17. Evidence is strong that the timing of HF interventions are best initiated when: 1. The person enters stage C 2. The person has functional disabilities 3. At the earliest indication 4. When stage IV is determined 18. HF patients frequently take more than one drug. When are anticoagulants typically used? 1. When the patient enters stage III 2. Only in cases of diastolic failure 3. When there is concurrent A Fib 4. In all cases 19. What can chest x-rays contribute to the diagnosis and management of HF? 1. They have no role. 2. They can give very precise pictures of pulmonary fluid status. 3. They provide an idea of general cardiac size and pulmonary great vessel distribution. 4. They can confirm the diagnosis. 20. The overall goal of treating hyperlipidemia is: 1. Maintain an LDL level of less than 160 mg/dL 2. To reduce atherogenesis 3. Lowering apo B, one of the apoliproteins 4. All of the above 21. When considering which cholesterol-lowering drug to prescribe, which factor determines the type and intensity of treatment? 1. Total LDL 2. Fasting HDL 3. Coronary artery disease risk level 4. Fasting total cholesterol 22. First-line therapy for hyperlipidemia is: 1. Statins 2. Niacin 3. Lifestyle changes 4. Bile acid-binding resins 23. James is a 45-year-old patient with an LDL level of 120 and normal triglycerides. Appropriate first-line therapy for James may include diet counseling, increased physical activity, and: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative 24. Joanne is a 60-year-old patient with an LDL of 132 and a family history of coronary artery disease. She has already tried diet changes (increased fiber and plant sterols) to lower her LDL and after 6 months her LDL is slightly higher. The next step in her treatment would be: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative 25. Sharlene is a 65-year-old patient who has been on a lipid-lowering diet and using plant sterol margarine daily for the past 3 months. Her LDL is 135 mg/dL. An appropriate treatment for her would be: 1. A statin 2. Niacin 3. A fibric acid derivative 4. Determined by her risk factors 26. Phil is a 54-year-old male with multiple risk factors who has been on a high-dose statin for 3 months to treat his high LDL level. His LDL is 135 mg/dL and his triglycerides are elevated. A reasonable change in therapy would be to: 1. Discontinue the statin and change to a fibric acid derivative. 2. Discontinue the statin and change to ezetimibe. 3. Continue the statin and add in ezetimibe. 4. Refer him to a specialist in managing patients with recalcitrant hyperlipidemia. 27. Jamie is a 34-year-old pregnant woman with familial hyperlipidemia and elevated LDL levels. What is the appropriate treatment for a pregnant woman? 1. A statin 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resins 28. Han is a 48-year-old diabetic with hyperlipidemia and high triglycerides. His LDL is 112 mg/dL and he has not tolerated statins. He warrants a trial of a: 1. Sterol 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resin 29. Jose is a 12-year-old overweight child with a total cholesterol of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____________ with a reevaluation in 6 months. 1. Statins 2. Niacin 3. Sterols 4. Bile acid-binding resins 30. Monitoring of a patient who is on a lipid-lowering drug includes: 1. Fasting total cholesterol every 6 months 2. Lipid profile with attention to serum LDL 6 to 8 weeks after starting therapy, then again in 6 weeks 3. Complete blood count, C-reactive protein, and erythrocyte sedimentation rate after 6 weeks of therapy 4. All of the above 31. Before starting therapy with a statin, the following baseline laboratory values should be evaluated: 1. Complete blood count 2. Liver function (ALT/AST) and creatine kinase 3. C-reactive protein 4. All of the above 32. When starting a patient on a statin, education would include: 1. If they stop the medication their lipid levels will return to pretreatment levels. 2. Medication is a supplement to diet therapy and exercise. 3. If they have any muscle aches or pain, they should contact their provider. 4. All of the above 33. Omega 3 fatty acids are best used to help treat: 1. High HDL 2. Low LDL 3. High triglycerides 4. Any high lipid value 34. When are statins traditionally ordered to be taken? 1. At bedtime 2. At noon 3. At breakfast 4. With the evening meal 35. Which the following persons should not have a statin medication ordered? 1. Someone with 3 first- or second-degree family members with history of muscle issues when started on statins 2. Someone with high lipids, but low BMI 3. Premenopausal woman with recent history of hysterectomy 4. Prediabetic male with known metabolic syndrome 36. Fiber supplements are great options for elderly patients who have the concurrent problem of: 1. End-stage renal failure on fluid restriction 2. Recurrent episodes of diarrhea several times a day 3. Long-term issues of constipation 4. Needing to take multiple medications around the clock every 2 hours 37. What is considered the order of statin strength from lowest effect to highest? 1. Lovastatin, Simvastatin, Rosuvastatin 2. Rosuvastatin, Lovastatin, Atorvastatin 3. Atorvastatin, Rosuvastatin, Simvastatin 4. Simvastatin, Atorvastatin, Lovastatin 38. Gastroesophageal reflux disease may be aggravated by the following medication that affects lower esophageal sphincter (LES) tone: 1. Calcium carbonate 2. Estrogen 3. Furosemide 4. Metoclopramide 39. Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Food or drink that may aggravate GERD include: 1. Eggs 2. Caffeine 3. Chocolate 4. Soda pop 40. Metoclopramide improves gastroesophageal reflux disease symptoms by: 1. Reducing acid secretion 2. Increasing gastric pH 3. Increasing lower esophageal tone 4. Decreasing lower esophageal tone 41. Antacids treat gastroesophageal reflux disease by: 1. Increasing lower esophageal tone 2. Increasing gastric pH 3. Inhibiting gastric acid secretion 4. Increasing serum calcium level 42. When treating patients using the "Step-Down" approach the patient with gastroesophageal reflux disease is started on _______ first. 1. Antacids 2. Histamine2 receptor antagonists 3. Prokinetics 4. Proton pump inhibitors 43. If a patient with symptoms of gastroesophageal reflux disease states that he has been self-treating at home with OTC ranitidine daily, the appropriate treatment would be: 1. Prokinetic (metoclopramide) for 4 to 8 weeks 2. Proton pump inhibitor (omeprazole) for 12 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 2 weeks 44. If a patient with gastroesophageal reflux disease who is taking a proton pump inhibitor daily is not improving, the plan of care would be: 1. Prokinetic (metoclopramide) for 8 to 12 weeks 2. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 4 to 8 weeks 45. The next step in treatment when a patient has been on proton pump inhibitors twice daily for 12 weeks and not improving is: 1. Add a prokinetic (metoclopramide) 2. Referral for endoscopy 3. Switch to another proton pump inhibitor 4. Add a cytoprotective drug 46. Infants with reflux are initially treated with: 1. Histamine2 receptor antagonist (ranitidine) 2. Proton pump inhibitor (omeprazole) 3. Anti-reflux maneuvers (elevate head of bed) 4. Prokinetic (metoclopramide) 47. Long-term use of proton pump inhibitors may lead to: 1. Hip fractures in at-risk persons 2. Vitamin B6 deficiency 3. Liver cancer 4. All of the above 48. An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is: 1. Histamine2 receptor antagonists for 4 to 8 weeks 2. Proton pump inhibitor bid for 12 weeks until healing is complete 3. Proton pump inhibitor bid plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor bid and levofloxacin for 14 days 49. Treatment failure in patients with peptic ulcer disease associated with H. pylori may be because of: 1. Antimicrobial resistance 2. An ineffective antacid 3. Overuse of proton pump inhibitors 4. All of the above 50. If a patient with H. pylori-positive peptic ulcer disease fails first-line therapy, the second-line treatment is: 1. Proton pump inhibitor bid plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days 2. Test H. pylori for resistance to common treatment regimens 3. Proton pump inhibitor plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor and levofloxacin for 14 days 51. After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is: 1. Testing for H. pylori eradication with a serum ELISA test 2. Endoscopy by a specialist 3. A proton pump inhibitor for 8 to 12 weeks until healing is complete 4. All of the above 52. Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing it with their provider or a pharmacist first? 1. Patients with kidney stones 2. Pregnant patients 3. Patients with heartburn 4. Postmenopausal women 53. Patients taking antacids should be educated regarding these drugs, including letting them know that: 1. They may cause constipation or diarrhea 2. Many are high in sodium 3. They should separate antacids from other medications by 1 hour 4. All of the above 54. Kelly has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide: 1. Can be given to patients of all ages, including infants and children, for viral gastroenteritis 2. Slows gastric motility and reduces fluid and electrolyte loss from diarrhea 3. Is the treatment of choice for the diarrhea associated with E. coli 0157 4. May be used in pregnancy and by lactating women 55. Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate: 1. May lead to toxicity if taken with aspirin 2. Is contraindicated in children with flu-like illness 3. Has antimicrobial effects against bacterial and viral enteropathogens 4. All of the above 56. Hannah will be traveling to Mexico with her church group over spring break to build houses. She is concerned she may develop traveler's diarrhea. Advice includes following normal food and water precautions as well as taking: 1. Loperamide four times a day throughout the trip 2. Bismuth subsalicylate with each meal and at bedtime 3. A prescription for diphenoxylate with atropine to use if she gets diarrhea 4. None of the above 57. Josie is a 5-year-old patient who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie? 1. Prochlorperazine (Compazine) 2. Meclizine (Antivert) 3. Promethazine (Phenergan) 4. Ondansetron (Zofran) 58. Jim presents with complaints of "heartburn" that is minimally relieved with Tums (calcium carbonate) and is diagnosed with gastroesophageal reflux disease (GERD). An appropriate first-step therapy would be: 1. Omeprazole (Prilosec) twice a day 2. Ranitidine (Zantac) twice a day 3. Famotidine (Pepcid) once a day 4. Metoclopramide (Reglan) four times a day 59. Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for: 1. Iron deficiency anemia, vitamin B12 and calcium deficiency 2. Folate and magnesium deficiency 3. Elevated uric acid levels leading to gout 4. Hypokalemia and hypocalcemia 60. Sadie is a 72-year-old patient who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: 1. Megaloblastic anemia 2. Osteoporosis 3. Hypertension 4. Strokes 61. Patrick is a 10-year-old patient who presents with uncomfortable constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10-year-old child would be: 1. PEG 3350 (Miralax) 2. Bisacodyl (Dulcolax) suppository 3. Docusate (Colace) suppository 4. Polyethylene glycol electrolyte solution 62. Methylnaltrexone is used to treat constipation in: 1. Patients with functional constipation 2. Patients with irritable bowel syndrome-associated constipation 3. Children with encopresis 4. Opioid-associated constipation 63. An elderly person has been prescribed lactulose for treatment of chronic constipation. Monitoring with long-term treatment would include: 1. Electrolytes, including potassium and chloride 2. Bone mineral density for osteoporosis 3. Magnesium level 4. Liver function 64. Angina is produced by an imbalance between myocardial oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS? 1. Calcium channel blockers 2. Beta blockers 3. Angiotensin-converting-enzyme (ACE) inhibitors 4. Aspirin 65. Not all chest pain is caused by myocardial ischemia. Noncardiac causes of chest pain include: 1. Pulmonary embolism 2. Pneumonia 3. Gastroesophageal reflux 4. All of the above 66. The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is class: 1. I 2. II 3. III 4. IV 67. Patients at high risk for developing significant coronary heart disease are those with: 1. LDL values between 100 and 130 2. Systolic blood pressure between 120 and 130 3. Class III angina 4. Obesity 68. To reduce mortality, all patients with angina, regardless of class, should be on: 1. Aspirin 81 to 325 mg/d 2. Nitroglycerin sublingually for chest pain 3. ACE inhibitors or angiotensin receptor blockers 4. Digoxin 69. Patients who have angina, regardless of class, who are also diabetic, should be on: 1. Nitrates 2. Beta blockers 3. ACE inhibitors 4. Calcium channel blockers 70. Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct. 1. Lose at least 10 pounds of body weight. Excessive weight increases cardiac workload. 2. Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload. 3. Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of potassium to improve contractility and oxygen supply. 4. Intake a moderate amount of alcohol. Moderate intake has been shown by research to improve cardiac function. 71. Nitrates are especially helpful for patients with angina who also have: 1. Heart failure 2. Hypertension 3. Both 1 and 2 4. Neither 1 nor 2 72. Beta blockers are especially helpful for patients with exertional angina who also have: 1. Arrhythmias 2. Hypothyroidism 3. Hyperlipidemia 4. Atherosclerosis 73. Isosorbide dinitrate is a long-acting nitrate given twice daily. The schedule for administration is 7 a.m. and 2 p.m. because: 1. Long-acting forms have a higher risk for toxicity. 2. Orthostatic hypotension is a common adverse effect. 3. It must be taken with milk or food. 4. Nitrate tolerance can develop. 74. Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use? 1. These drugs are useful for immediate symptom relief when the patient is certain it is angina. 2. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away. 3. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than two doses. If chest pain is still not relieved, call 911. 4. All of the above 75. Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because: 1. Nitrates increase MOS and beta blockers increase MOD. 2. Their additive effects permit lower doses of both drugs and their adverse reactions cancel each other out. 3. They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease. 4. All of the above 76. Drug choices to treat angina in older adults differ from those of younger adults only in: 1. Consideration of risk factors for diseases associated with and increased in aging 2. The placement of drug therapy as a treatment choice before lifestyle changes are tried 3. The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult 4. Those with higher risk for silent myocardial infarction 77. Which of the following drugs has been associated with increased risk for myocardial infarction in women? 1. Aspirin 2. Beta blockers 3. Estrogen replacement 4. Lipid-lowering agents 78. Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT: 1. Patients often require multiple drugs 2. A large number of angina patients are older adults on fixed incomes 3. Generic formulations may be cheaper but are rarely bioequivalent 4. Lack of drug selectivity may result in increased adverse reactions 79. Situations that suggest referral to a specialist is appropriate include: 1. When chronic stable angina becomes unpredictable in its characteristics and precipitating factors 2. When a post-myocardial infarction patient develops new-onset angina 3. When standard therapy is not successful in improving exercise tolerance or reducing the incidence of angina 4. All of the above 80. The rationale for prescribing calcium blockers for angina can be based on the need for: 1. Increased inotropic effect in the heart 2. Increasing peripheral perfusion 3. Keeping heart rates high enough to ensure perfusion of coronary arteries 4. Help with rate control 81. Medications are typically started for angina patients when: 1. The first permanent EKG changes occur 2. The start of class I or II symptoms 3. The events trigger a trip to the emergency department 4. When troponin levels become altered 82. The most common cause of angina is: 1. Vasospasm of the coronary arteries 2. Atherosclerosis 3. Platelet aggregation 4. Low systemic oxygen 83. Ranolazine is used in angina patients to: 1. Dilate plaque-filled arteries 2. Inhibit platelet aggregation 3. Restrict late sodium flow in the myocytes 4. Induce vasoconstriction in the periphery to open coronary vessels 84. When is aspirin (ASA) used in angina patients? 1. All angina patients should be taking ASA unless it is contraindicated for allergy or other medical reasons. 2. ASA should only be used in men. 3. ASA has no role in angina, but is useful in MI prevention. 4. The impact of ASA is best at the time of an angina attack. 85. Because primary hypertension has no identifiable cause, treatment is based on interfering with the physiological mechanisms that regulate blood pressure. Thiazide diuretics treat hypertension because they: 1. Increase renin secretion 2. Decrease the production of aldosterone 3. Deplete body sodium and reduce fluid volume 4. Decrease blood viscosity 86. Because of its action on various body systems, the patient taking a thiazide or loop diuretic may also need to receive the following supplement: 1. Potassium 2. Calcium 3. Magnesium 4. Phosphates 87. All patients with hypertension benefit from diuretic therapy, but those who benefit the most are: 1. Those with orthostatic hypertension 2. African Americans 3. Those with stable angina 4. Diabetics 88. Beta blockers treat hypertension because they: 1. Reduce peripheral resistance 2. Vasoconstrict coronary arteries 3. Reduce norepinephrine 4. Reduce angiotensin II production 89. Which of the following disease processes could be made worse by taking a nonselective beta blocker? 1. Asthma 2. Diabetes 3. Both might worsen 4. Beta blockade does not affect these disorders 90. Disease states in addition to hypertension in which beta blockade is a compelling indication for the use of beta blockers include: 1. Heart failure 2. Angina 3. Myocardial infarction 4. Dyslipidemia 91. Angiotensin-converting enzyme (ACE) inhibitors treat hypertension because they: 1. Reduce sodium and water retention 2. Decrease vasoconstriction 3. Increase vasodilation 4. All of the above 92. Compelling indications for an ACE inhibitor as treatment for hypertension based on clinical trials includes: 1. Pregnancy 2. Renal parenchymal disease 3. Stable angina 4. Dyslipidemia 93. An ACE inhibitor and what other class of drug may reduce proteinuria in patients with diabetes better than either drug alone? 1. Beta blockers 2. Diuretics 3. Nondihydropyridine calcium channel blockers 4. Angiotensin II receptor blockers 94. If not chosen as the first drug in hypertension treatment, which drug class should be added as a second step because it will enhance the effects of most other agents? 1. ACE inhibitors 2. Beta blockers 3. Calcium channel blockers 4. Diuretics 95. Treatment costs are important for patients with hypertension. Which of the following statements about cost is NOT true? 1. Hypertension is a chronic disease where patients may be taking drugs for a long time. 2. Most patients will require more than one drug to treat the hypertension. 3. The cost includes the price of any routine or special laboratory tests that a specific drug may require. 4. Few antihypertensive drugs come in generic formulations. 96. Caffeine, exercise, and smoking should be avoided for at least how many minutes before blood pressure measurement? 1. 15 2. 30 3. 60 4. 90 97. Blood pressure checks in children: 1. Should occur with their annual physical examinations after 6 years of age 2. Require a blood pressure cuff that is one-third the diameter of the child's arm 3. Should be done during every health-care visit after 3 years of age 4. Require additional laboratory tests such as serum creatinine 98. Lack of adherence to blood pressure management is very common. Reasons for this lack of adherence include: 1. Lifestyle changes are difficult to achieve and maintain. 2. Adverse drug reactions are common and often fall into the categories more associated with nonadherence. 3. Costs of drugs and monitoring with laboratory tests can be expensive. 4. All of the above 99. Lifestyle modifications for patients with prehypertension or hypertension include: 1. Diet and increase exercise to achieve a BMI greater than 25. 2. Drink 4 ounces of red wine at least once per week. 3. Adopt the dietary approaches to stop hypertension (DASH) diet. 4. Increase potassium intake. 100. Which diuretic agents typically do not need potassium supplementation? 1. The loop diuretics 2. The thiazide diuretics 3. The aldosterone inhibitors 4. They all need supplementation 101. Aldactone family medications are frequently used when the hypertensive patient also has: 1. Hyperkalemia 2. Advancing liver dysfunction 3. The need for birth control 4. Rheumatoid arthritis 102. Hypertensive African Americans are typically listed as not being as responsive to which drug groups? 1. ACE inhibitors 2. Calcium channel blockers 3. Diuretics 4. Bidil (hydralazine family of medications) 103. What educational points concerning fluid intake must be covered with diuretic prescriptions? 1. Fluid should be restricted when on them. 2. Fluids should contain at least one salty item daily. 3. Fluid intake should remain near normal for optimal performance. 4. Avoidance of potassium-rich fluids is encouraged. 104. What is a common side effect concern with hypertensive medications and all individuals, but especially the elderly? 1. Risk of falls 2. Triggering of a hypertensive crisis 3. Erectile priapism 4. Risk for bladder cancer development 105. Ray has been diagnosed with hypertension and an angiotensin-converting enzyme inhibitor is determined to be needed. Prior to prescribing this drug, the NP should assess for: 1. Hypokalemia 2. Impotence 3. Decreased renal function 4. Inability to concentrate 106. Angiotensin-converting enzyme inhibitors are the drug of choice in treating hypertension in diabetic patients because they: 1. Improve insulin sensitivity 2. Improve renal hemodynamics 3. Reduce the production of angiotensin II 4. All of the above 107. A potentially life-threatening adverse response to angiotensin-converting enzyme inhibitors is angioedema. Which of the following statements is true about this adverse response? 1. Swelling of the tongue or hoarseness are the most common symptoms. 2. It appears to be related to the decrease in aldosterone production. 3. Presence of a dry, hacky cough indicates a high risk for this adverse response. 4. Because it takes time to build up a blood level, it occurs after being on the drug for about 1 week. 108. Angiotensin-converting enzyme inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use? 1. Stable angina because it decreases the thickening of vascular walls due to decreased modified release. 2. Heart failure because it reduces remodeling of injured myocardial tissues. 3. Both 1 and 2 are true and the reasons are correct. 4. Both 1 and 2 are true but the reasons are wrong. 5. Neither 1 nor 2 are true. 109. Despite good blood pressure control, an NP might change a patient's drug from an angiotensin-converting enzyme (ACE) inhibitor to an angiotensin II receptor blocker (ARB) because the ARB: 1. Is stronger than the ACE inhibitor 2. Does not produce a dry, hacky cough 3. Has no effect on the renal system 4. Reduces sodium and water retention 110. While taking an angiotensin II receptor blocker (ARB), patients need to avoid certain over-the-counter drugs without first consulting the provider because: 1. Cimetidine is metabolized by the CYP 3A4 isoenzymes 2. Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels 3. Both 1 and 2 4. Neither 1 nor 2 111. Laboratory monitoring for patients on angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers should include: 1. White blood cell counts with the drug dosage increased for elevations above 10,000 feet 2. Liver function tests with the drug dosage stopped for alanine aminotransferase values twice that of normal 3. Serum creatinine levels with the drug dosage reduced for values greater than 2.5 mg/dL 4. Serum glucose levels with the drug dosage increased for levels greater than 120 mg/dL 112. Jacob has hypertension, for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it: 1. Decreases the amount of calcium inside the cell 2. Reduces stroke volume 3. Increases the activity of the Na+/K+/ATPase pump indirectly 4. Decreases heart rate 113. Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker? 1. Bradycardia 2. Hepatic impairment 3. Increased contractility 4. Edema of the hands and feet 114. Patient teaching related to amlodipine includes: 1. Increase calcium intake to prevent osteoporosis from a calcium blockade. 2. Do not crush the tablet; it must be given in liquid form if the patient has trouble swallowing it. 3. Avoid grapefruit juice as it affects the metabolism of this drug. 4. Rise slowly from a supine position to reduce orthostatic hypotension. 115. Vera, age 70, has isolated systolic hypertension. Calcium channel blocker dosages for her should be: 1. Started at about half the usual dosage 2. Not increased over the usual dosage for an adult 3. Given once daily because of memory issues in the older adult 4. Withheld if she experiences gastroesophageal reflux 116. Larry has heart failure, which is being treated with digoxin because it exhibits: 1. Negative inotropism 2. Positive chronotropism 3. Both 1 and 2 4. Neither 1 nor 2 117. Furosemide is added to a treatment regimen for heart failure that includes digoxin. Monitoring for this combination includes: 1. Hemoglobin 2. Serum potassium 3. Blood urea nitrogen 4. Serum glucose 118. Which of the following create a higher risk for digoxin toxicity? Both the cause and the reason for it must be correct. 1. Older adults because of reduced renal function 2. Administration of aldosterone antagonist diuretics because of decreased potassium levels 3. Taking an antacid for gastroesophageal reflux disease because it increases the absorption of digoxin 4. Doses between 0.25 and 0.5 mg/day 119. Serum digoxin levels are monitored for potential toxicity. Monitoring should occur: 1. Within 6 hours of the last dose 2. Because a reference point is needed in adjusting a dose 3. After three half-lives from the starting of the drug 4. When a patient has stable renal function 120. Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: 1. Widening of the area of infarction 2. Onset of congestive heart failure 3. An electrolyte imbalance involving potassium 4. Renal dysfunction 121. Which of the following is true about procainamide and its dosing schedule? 1. It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. 2. Gastrointestinal adverse effects are common so the drug should be taken with food. 3. Adherence can be improved by using a sustained release formulation that can be given once daily. 4. Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. 122. Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT: 1. Notify your health-care provider immediately if you have visual change. 2. Monitor your own blood pressure and pulse daily. 3. Take a hot shower or bath if you feel dizzy. 4. Use a sunscreen on exposed body surfaces. 123. The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response? 1. Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism. 2. Amiodarone damages the thyroid gland and can result in inflammation of that gland, causing hyperthyroidism. 3. Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given. 4. Amiodarone can cause corneal deposits in up to 25% of patients. 124. Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 a.m. and 2 p.m. because: 1. It is a long-acting drug with potential for toxicity. 2. Nitrate tolerance can develop. 3. Orthostatic hypotension is a common adverse effect. 4. It must be taken with milk or food. 125. Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: 1. This is a parasympathetic response to the vasodilating effects of the drug. 2. Headaches are common side effects with these drugs. How severe are they? 3. This is associated with your smoking. Let's work on having you stop smoking. 4. This is not related to your medication. Are you under a lot of stress? 126. In teaching about the use of sublingual nitroglycerine, the patient should be instructed: 1. To swallow the tablet with a full glass of water 2. To place one tablet under the tongue if chest pain occurs and allow it to dissolve 3. To take one tablet every 5 minutes until the chest pain goes away 4. That it should "burn" when placed under the tongue or it is no longer effective 127. Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: 1. Become a vegetarian because this disorder is associated with eating red meat. 2. Stop taking the drug if abdominal cramps and diarrhea develop. 3. Report muscle weakness or tenderness and dark urine to his provider immediately. 4. Expect "hot flash" sensations during the first 2 weeks of therapy. 128. Which of the following diagnostic studies would NOT indicate a problem related to a reductase inhibitor? 1. Elevated serum transaminase 2. Increased serum creatinine 3. Elevated creatinine kinase 4. Increased white blood cell counts 129. Because of the pattern of cholesterol synthesis, reductase inhibitors are given: 1. In the evening in a single daily dose 2. Twice daily in the morning and the evening 3. With each meal and at bedtime 4. In the morning before eating 130. Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following laboratory results should be monitored? 1. Serum alanine aminotransferase 2. Serum amylase 3. Serum creatinine 4. Phenylketonuria 131. Niaspan is less likely to cause which side effect that is common to niacin? 1. Gastrointestinal irritation 2. Cutaneous flushing 3. Dehydration 4. Headaches 132. Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? 1. Reactive airway disease/asthma 2. Inflammatory bowel disease 3. Allergy to aspirin 4. Gallbladder disease 133. Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct. 1. Reductase inhibitors, due to an increased risk for rhabdomyolysis 2. Bile-acid sequestering resins, due to interference with folic acid absorption 3. Grapefruit juice, due to interference with metabolism 4. Niacin, due to decreased gemfibrozil activity 134. Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug: 1. Blocks synthesis of cholesterol in the liver 2. Exchanges chloride ions for negatively charged acids in the bowel 3. Increases HDL levels the most among the classes 4. Blocks the lipoprotein lipase pathway 135. Because of their site of action, bile acid sequestering resins: 1. Should be administered separately from other drugs by at least 4 hours 2. May increase the risk for bleeding 3. Both 1 and 2 4. Neither 1 nor 2 136. Colestipol comes in a powdered form. The patient is taught to: 1. Take the powder dry and follow it with at least 8 ounces of water 2. Take it with a meal to enhance its action on fatty food 3. Mix the powder with 4 to 6 ounces of milk or fruit juice 4. Take after the evening meal to coincide with cholesterol synthesis 137. The choice of diuretic to use in treating hypertension is based on: 1. Presence of diabetes with loop diuretics being used for these patients 2. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40mL/min range 3. Ethnicity with aldosterone antagonists best for African Americans and older adults 4. Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL 138. Direct renin inhibitors have the following properties. They: 1. Are primarily generic drugs 2. Are a renin-angiotensin-aldosterone system (RAAS) medication that is safe during pregnancy 3. Can be used with an angiotensin-converting enzyme and angiotensin II receptor blocker medications for stronger impact 4. "Shut down" the entire RAAS cycle 139. When comparing angiotensin-converting enzyme (ACE) and angiotensin II receptor blocker (ARB) medications, which of the following holds true? 1. Both have major issues with a dry, irritating cough 2. Both contribute to some retention of potassium 3. ARBs have a stronger impact on hypertension control than ACE medications 4. ARBs have stronger diabetes mellitus renal protection properties than ACE medications 140. What does the provider understand about the issue of "Diabetic Renal Protection" with angiotensin-converting enzyme (ACE) medications? Diabetes mellitus patients: 1. Have a reduced rate of renal progression, but still need to be discontinued when advanced renal issues present 2. Who start these medications never progress to renal nephropathy 3. With early renal dysfunction will see it reverse when on ACE medications 4. Without renal issues are the only ones who benefit from ACE protection 141. What dermatological issue is linked to Amiodarone use? 1. Increased risk of basal cell carcinoma 2. Flare up of any prior psoriasis problems 3. Development of plantar warts 4. Progressive change of skin tone toward a blue spectrum 142. Commercials on TV for erectile dysfunction (ED) medications warn about mixing them with nitrates. Why? 1. Increased risk of priapism 2. Profound hypotension 3. Development of blue discoloration to the visual field 4. Inactivation of the ED medication effect [Show More]
Last updated: 1 year ago
Preview 1 out of 35 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 03, 2020
Number of pages
35
Written in
Additional information
This document has been written for:
Uploaded
Jun 03, 2020
Downloads
0
Views
35


 – CHAMBERLAIN COLLEGE OF NURSING.png)