NUR 2488 Study Guide Exam 1_Rasmussen College: SATISFACTION GUARANTEED
Document Content and Description Below
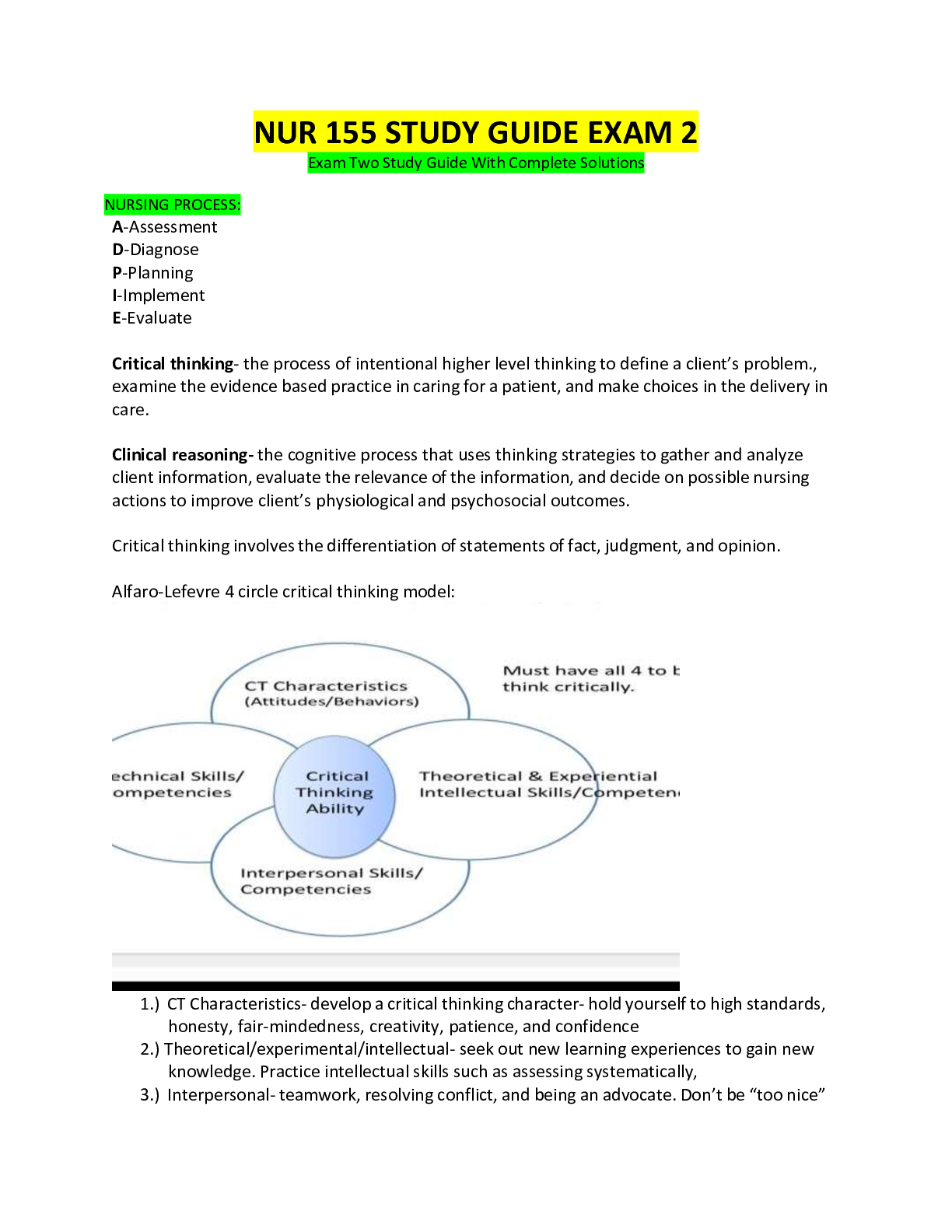
Theorists: Freud: “father of psychiatry” Believes psychological disturbances were related to events of early trauma or events not remembered or recognized. Formation of personality, conscious ... and unconscious influences, importance of individual talk sessions, attentive listening, transference, countertransference ● Id: primary thought process, instinctive, pleasure seeking part of the personality, lurks in the unconscious mind (EAT THE CAKE).basic pleasure seeking( devil on shoulder) Impulsive, I WANT NOW Food, sex, sleep Awareness (Pleasure principle, reflex action, primary process) ● Ego: ability to realistically evaluate situations (problem solver, reality tester). Sense of self (PRESENT EVERY DAY). Current self Mechanisms (Problem solver, reality tester) ● Super ego: primarily our conscience, moral component, influenced by family and friends (DONT EAT THE CAKE). Morality (Angel on shoulder) Moral compone HINT: think of the movie Kronk, the devil on his shoulder is the Id, Ego is himself, Superego is the angel on his other shoulder. Maslow’s Hierarchy of Needs: Needs are placed on a pyramid, most basic and important needs are on the lower level and have to be met before the needs at the top (self-actualization) can be made. Bottom to top: ● Physiological needs: the most basic needs, drives priority (food, water, oxygen, sleep, sex, constant body temp) Bottom of pyramid Food, water, oxygen, elimination, rest, and sex ● Safety needs: security, protection, freedom from fear/anxiety/chaos, law and order. (Fall risk) Security, protection, stability, structure, order, and limits ● Belongingness and Love Needs: need for an intimate relationship, love, affection and belonging, wills seek to overcome feelings of loneliness. (Having a family and home) Affilitation, affectionate relationships, and love ● Esteem Needs: the need to have a high self-regard and have it relayed to them from others, feel confident, valued and valuable. Self-esteem related to competency, achievement, and esteem from others ● Self-Actualization needs: the path that will result in inner peace/fulfillment. (What we strive to become as humans) (Top of pyramid) Becoming everything one is capable of ● Self-Transcendence needs: when an individual “seeks to further a cause beyond the self and to experience a communion beyond the boundaries of the self through peak experiences”. Self-transcendent experiences are those in which a person experiences a sense of identity that transcends or extends beyond the personal self. Erikson’s Stages of Development: ● Infancy: Trust vs Mistrust: birth to 1.5 years. Developing a basic sense of trust, leading to hope and physical comfort. ● Early Childhood: Autonomy vs Shame/Doubt: 1.5 to 3 years. Gaining self-control, independence with the environment. ● Preschooler: Initiative vs Guilt: 3 to 6 years. Achieve sense of purpose and mastery of skills. ● School Age: Industry vs Inferiority: 6-12 years. Gain sense of self-confidence and recognition thru learning, competing and performing. Competing in sports ● Adolescence: Identity vs Role Confusion: 12-20 years. Integrate all the tasks previously mastered into a secure self. ● Young Adulthood: Intimacy/Solidarity vs Isolation: 20-30 years. Forming intense relationships, committing to another person, cause and institution. ● Adulthood: Generativity vs Self-Absorption: 30-65 years. Achieve life goals, obtain certain awareness of future generations. ● Elderly: Integrity vs Despair: 65++. Obtaining self-worth, finding meaning in one’s whole life. Understand the role of neurotransmitters as related to disorders Dopamine, Serotonin, Norepinephrine, GABA • Dopamine: “Alertness” associated with feelings of euphoria, bliss, motivation, concentration • Serotonin: “Satisfaction” regulates mood, social behavior, appetite, digestion, sleep, memory, and sexual desire and function • Norepinephrine: “Balanced mood” stress hormone “fight or flight response” • GABA: promotes calm relaxation What disorders are impacted by the neurotransmitters? • Dopamine o Decrease: Parkinson disease and Depression o Increase: Schizophrenia, mania • Norepinephrine o Decrease: Depression o Increase: Anxiety states • Serotonin o Decrease: Depression o Increase: Anxiety states • Histamine o High levels associated with anxiety and depression What class of medications are impacted by neurotransmitters (IE: SSRI impacts Seratonin) • Antidepressant: serotonin • Antianxiety: GABA • Sedative hypnotic: histamine • Mood stabilizer: norepinephrine • Antipsychotic: dopamine • Anticholinesterase: aceylcholine Nurse-Client Relationship: Understand what occurs in the orientation, working, and termination phase Phases of Nurse-Client Relationships: ● Orientation: Introductory Phase: nurse and client get to know each other, this phase includes building an environment of trust/rapport, establishing relationship parameters, creating a formal or informal contract, acknowledging confidentiality, evaluating the client’s problems, and beginning a plan for the termination phase. Gather assessment data, formulate working diagnosis, develop realistic plan of action. **Three processes occur: opening the relationship, clarifying the problem, and structuring and formulation the contract for what will be accomplished during the relationship. ● Working: exploration of feelings or situations that are causing the problems. Re-experiencing of old conflicts can awaken high levels of anxiety, intense emotional states may surface, defense mechanisms, denying, manipulation, evaluation of problems and goals, promote alternative reactions/behaviors to situations. The nurse’s awareness of his or her own personal feelings and reactions to the patient are VITAL for effective interaction with the patient *transference occurs as the patient projects intense feelings onto the therapist. *countertransference occurs as the therapist projects feelings onto the patient ● Termination: final phase. Summarization of goals, review of what was achieved during communication, discussing new ways to implement new coping strategies, evokes strong feelings in both client and nurse. Maintaining contact on a personal level is acceptable. Understand the differences between a nurse-client and a social relationship Nurse-Client vs Social Relationships: ● Social Relationships: Can be defined as a relationship that is primarily initiated for friendship, enjoyment, or communal effort. Mutual needs are met during the time of a social relationship. Communication does not have to be therapeutic in a social relationship (advice giving). Includes friendship and socialization, mutual needs are met, may include giving advice, basic needs are met, content is superficial, roles may shift, little evaluation of interaction occurs ● Therapeutic Relationships: the nurse uses all of their communication skills, understanding of human behavior, and personal insight to enhance the client’s growth. This type of relationship is client-focused. Boundaries are kept clear, advice isn’t given, but the nurse aids the client in exploring their options. The relationship is professional and goal oriented. Nurse maximizes communication skills, understanding of human behaviors, and personal strengths to enhance patient’s growth. Patient needs are addressed, language is straightforward, focus is on the patient’s ideas Understand boundaries with clients ● Nurse-Client Boundaries: clear boundaries allow clients to feel safe enough to express themselves. The nurse’s needs should be separated from those of the client. Transference and countertransference can lead to loosened boundaries. No self-disclosure, no giving or receiving gifts, touching is allowed only if it provides a therapeutic effect, no romantic associations, no favoring, no secrets, no special attention or time. (Don’t lie to get info, that's what waterboarding is for… :) The role of the psych RN- what is considered within the scope of practice? ● Psych Nurse Scope of Practice: psychiatric nursing is a specialized area of nursing committed to promoting mental health through the assessment, diagnosis, and treatment of behavioral problems, psychiatric disorders, and comorbid conditions. Psychiatric nursing interventions are an art and a science employing a purposeful use of self and a wide range of nursing, psychosocial, and neurobiological research evidence to produce effective outcomes.( Educational teaching and therapeutic interventions) Nursing Process: Describe the nursing process when developing plan of care (Figure 7-1) ● How to Develop a Plan of Care: EBP should be used when developing plans of care. The plan of care should be client-focused and address their needs. Nurses work with other healthcare team members to develop plans of care. Assessments are essential to developing a care plan that suits the client. (Plan for outcomes first - Outcome identification) Nursing Process Assessment -Construct database -MSE (mental status exam), psychosocial, physical, history, Interviews, standardized rating scales -Verify data Nrsg DX -Identify problem -Construct nursing dx -Prioritize dx Outcome ID -ID attainable and culturally expected outcomes, document expected outcomes as measureable goals, include time estimate for expected outcomes. Planning -ID safe, pertinent, EB actions, Interventions that are culturally relevant and compatable with health beliefs and practice, document plan using recognized terminology Implementation -Basic and advanced interventions Practice interventions -Coordinate care, health promotion, milieu therapy, pharm, bio and integrative therapies, Advanced -Prescriptive authority and tx, psychotherapy, consultation. Evaluation -Document results If outcome not achieved -Additional data, reassess, revision of plan Developing a goal/outcome includes? SMART Goals? Specific Measurable Achievable Relevan Time-bound Understanding the difference between mental health and mental illness ● Mental Health: the successful performance of mental functions, resulting in the ability to engage in productive activities, enjoy fulfilling relationships, adapt to change, and cope with adversity. ● Mental Illness: medical conditions (dysfunctions of the brain and neurotransmitters) that affect a person’s thinking, feeling, mood, ability to relate to others, and daily functioning. The Interview: Describe the sections of the psychiatric assessment ● Psychiatric Assessment: establish rapport, obtain an understanding of the problem, review physical status/vitals, assess for risk factors, perform an MSE, assess psychosocial status, identify goals for treatment, formulate a plan of care , and document data. Describe the sections of the MSE ● Sections of the MSE: the MSE organizes OBJECTIVE data. Evaluates a client’s cognitive processes. ○ Personal Information gathered includes personal information (demographics), ○ Appearance (grooming, hygiene, facial expression, tattoos, dress), ○ Behavior (body movements, eye contact), speech (rate, volume, disturbances), affect (what we see) ○ Mood (flat, bland, animated: patient reports), (what they say…) ○ Thought (disorganized, coherent, flight of ideas, neologisms, delusions, suicidal), ○ Perceptual disturbances (hallucinations, illusions), and cognition (orientation (alert and oriented x3) memory, knowledge, attention span, abstraction, insight, judgement) Describe how to assess: attention, abstraction, insight, judgement -Attention: performance of serial events, digit span tests. (Serial 7’s) -Abstraction: performance on tests involving similarities, proverbs (People in glass houses shouldn’t throw stones) -Insight: ability to identify and understand present condition. (Why are you here? Subjective) -Judgement: ability to assess a practical dilemma. (Give pt situation “found envelope of money, what do you do?”) What considerations should be evaluated during an interview? Barriers to the Interview: Lighting, noise, distractions, eye level, environment (Physical barriers: HOH, poor vision) ** especially important with Elderly** Communication: Empathetic vs. sympathetic responses ○ Empathy is a concept that includes moral, cognitive, emotional, and behavioral components. Empathy is understanding the feeling of others. (“I understand how you feel.”) ○ Sympathy is when we feel the feelings of others, and thus lose objectivity. Sympathy is associated with feelings of pity and commiseration.(“I feel bad for you.” or “I’m so sorry”) ***ACKNOWLEDGE FEELINGS FIRST!!!!*** Describe and give examples for Therapeutic Communication Techniques ● Silence: gives the client time to collect their thoughts ● Accepting: indicates the client has been understood ● Sequencing: puts events and actions in perspective ● Observations: brings attention to the client’s behaviors ● Restating: directs questions/feelings/ideas back to client (Your life has no meaning?) ● Summarizing: combines the important points to enhance understanding Describe and give examples for Non-Therapeutic Communication Techniques ● Advising: assumes the client cannot think for themselves ● Minimizing: indicates the nurse doesn’t understand the client’s emotions (PT- I wanna kill myself, RN - I know how you feel) ● Falsely Reassuring: underrated the client’s concerns. ( “Everything is going to be fine”) ● Value Judgements: prevents problem solving ● Why: implies criticism; raises defensiveness (Refer to Table 8-2, Table 8-3 handout) Cultural Considerations: Define ethnicity: give examples ● Ethnicity: refers to a social group that shares a common and distinctive culture, religion, language (Latino, Asian, African American, and Native American) Define culture: give examples ● Culture: the arts, beliefs, and customs, of a group, place or time. (Lesbian, Christian, Anarchist, Vegan, Japanese, Military) Apply the impact of culture to patient care Cultural Considerations: Negotiating Barriers Four areas that may prove problematic for the nurse when interpreting specific verbal and nonverbal messages of the patient include the following: 1. Communication styles 2. Use of eye contact 3. Perception of touch 4. Cultural filters Understand both verbal and nonverbal communication styles of diverse populations Be aware of the cultural meanings of verbal and nonverbal communications to form positive therapeutic alliances Attitudes and beliefs regarding diverse populations affect relationships with patients Ethics: method of inquiry about morality of human behavior, practices or beliefs of groups such as nurses and physicians (nursing or medical ethics), or expected standards of moral behavior defined in a group’s code of professional ethics. Define and give examples for (pg. 62): ● Negligence: an act or omission to act that breaches the duty of due care (failure to complete tasks, failure to warn) ● Autonomy: respecting that others have the right to make decisions (Independence)(ie: what they want to take their meds with ) ● Justice: the duty to distribute resources equally, regardless of person, FAIR AND EQUAL. (Fairness, what I do for one, I do for all) ● Beneficence: the duty to act to the benefit of others. CHARITY (to the good of the patient) Ethics cont.: ● Veracity: one’s duty to truthfulness (honesty) - conformity to facts; accuracy. ● Fidelity: maintaining loyalty and commitment to the client. FAITHFUL (following through with what you say you are going to do) Examples of how these are used in patient care What rights do all patients have? Patient Rights: ● People with mental health illnesses are given the same rights as anyone else. ● Included is the right to receive human care and treatment. The medical, dental, and psychiatric needs of the patient must be met in accordance with the prevailing standards. It also includes the right to religious freedoms, social interactions, exercise, and recreation. What rights are limited to involuntarily admitted clients? ● People who are involuntarily committed also have the right to challenge their commitment through the writ of habeas corpus. (Lost the right to leave, right to privacy, right to belongings) Describe Duty to Warn and how it is used in psychiatric nursing Duty to Warn: Psychotherapists have a duty to warn a client’s potential victim(s) (Follow chain of command) Describe HIPPA and how it is used in psychiatric nursing HIPPA: the psychiatric client’s right to receive treatment and to have confidential medical records is legally protected by HIPPA. Information cannot be given to anyone who isn’t directly involved in the patient’s care, except in situations relating to duty to warn Describe when it is appropriate to use restraints/seclusion ● Guidelines: may only be used by people who have training to use them, those who are trained in the use of non-physical intervention skills, those who can recognize the symptoms of patient distress, and those who are CPR certified. An order must be obtained to place someone in restraints (except in extreme circumstances, when one may be retroactively obtained). A renewal of restraints can only be made in increments of 4 hours, up to 24 hrs total. The patient must be observed every 15-20 min. ○ Last resort ○ Risk of harm to self/others ○ Require Dr. orders ● Usage: restraints and seclusion can only be used to ensure the immediate safety of the patient,staff, and others. They should only be used after all other means have failed to control/contain the crisis situation The purpose behind seclusion? Patient Safety Psychopharmacology: Identify the classes of medications used to treat psychiatric disorders- know generics Antidepressants: SSRIs: first line of defense for OCD, anxiety, depression, and NMS, serotonin syndrome. -Do not give to patient who has severe renal or hepatic impairment -Monitor CBC, platelets, and bleeding times -Side effects: anticholinergic effects with N/V, insomnia, sexual dysfunction, and GI upset -Client teaching: do not stop taking suddenly, may take with food -Drugs: fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil), citalopram Tricyclics: block monoamine uptake, increase norepinephrine and serotonin. -Increases mood, activity, and alertness, improves appetite and regulates sleep patterns. -Decreases clients preoccupation with morbidity -Takes 1-3 weeks for therapeutic effects to occur, max effects 6-8 weeks -Side Effects: anticholinergic effects, sedation, weight gain, dizziness, constipation, dry mouth, orthostatic hypotension, sedation, cardiac toxicity -Client teaching: takes 4-6 weeks to work, highly fatal, do not take with MAOIs -2nd line of defense, HIGHLY FATAL IN OVERDOSE -Prescribed only a week at a time (highly addictive) -Drugs: amitriptyline (Elavil), imipramine (Tofranil), nortriptyline (Pamelor) MAOIs: increases serotonin and dopamine ● Last line of defense for depression, potentially fatal food and drug interactions - ● Taken with SSRIs can cause serotonin syndrome ● Side Effects: dry mouth, nausea, drowsiness, muscle spasms and cramps, orthostatic hypotension, edema, wt gain, sexual dysfunction ● Client Teaching: avoid TYRAMINE rich foods (cheese, cured meats, avocados, and beer) take on empty stomach, has a wash out period, don’t stop suddenly. ● Tyramine foods can cause HYPERTENSIVE CRISIS ● Drugs: phenelzine (Nardil), tranylcypromine (Parnate) Anxiolytics Benzodiazepines: fast acting, short term treatment ONLY, prescriptions are PRN, high risk for dependency -Side Effects: sedation, hypnotic effects -Client Teaching: do not stop suddenly, notify MD of pregnancy -Drugs: Anxiety: diazepam (Valium), clonazepam (Klonopin), alprazolam (Xanax), lorazepam (Ativan) -Insomnia: flurazepam (Dalmane), temazepam (Restoril) Antipsychotics Typical Antipsychotics: targets positive symptoms of schizophrenia, blocks dopamine -Effects are seen in 1-2 days, but takes 2-4 weeks to be stabilized -Side Effects: EPS, NMS, parkinsonism, anticholinergic effects, gynecomastia, galactorrhea, amenorrhea, wt gain, sedation, orthostatic hypotension -Client Teaching: stop slowly, sunscreen, change positions slowly, routine follow ups, oral hygiene, take with food/milk/full glass of water to decrease GI upset, have CBC and liver enzymes checked. -Drugs: chlorpromazine (Thorazine), fluphenazine (Prolixin), haloperidol (Haldol) Atypical Antipsychotics: mainly used because of sedation effects, blocks dopamine and serotonin -Targets positive and negative symptoms of schizophrenia -Side Effects: NMS, less risk for EPS, CBC (agranulocytosis), drooling, wt gain, seizures -Client Teaching: have routine blood work, smoking lowers levels of meds, change positions slowly, oral hygiene, increase fluids -Drugs: clozapine (Clozaril), risperidone (Risperdal), quetiapine (Seroquel), aripiprazole (Abilify), olanzapine (Zyprexa) EPS (Extrapyramidal Side Effects) -Dystonia: muscle stiffness -Akathisia: restlessness -Tardive dyskinesia: involuntary muscle movements -Drug induced Parkinsonism: thorazine shuffle -NMS: sudden fever, rigidity, tachycardia, HTN, LOC -Orthostatic hypotension [Show More]
Last updated: 1 year ago
Preview 1 out of 15 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 14, 2020
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
May 14, 2020
Downloads
0
Views
42



 (1).png)