*NURSING > Study Notes > NUR 2790 Final Exam Content Guide_Rasmussen College: Download To Score An A (All)
NUR 2790 Final Exam Content Guide_Rasmussen College: Download To Score An A
Document Content and Description Below
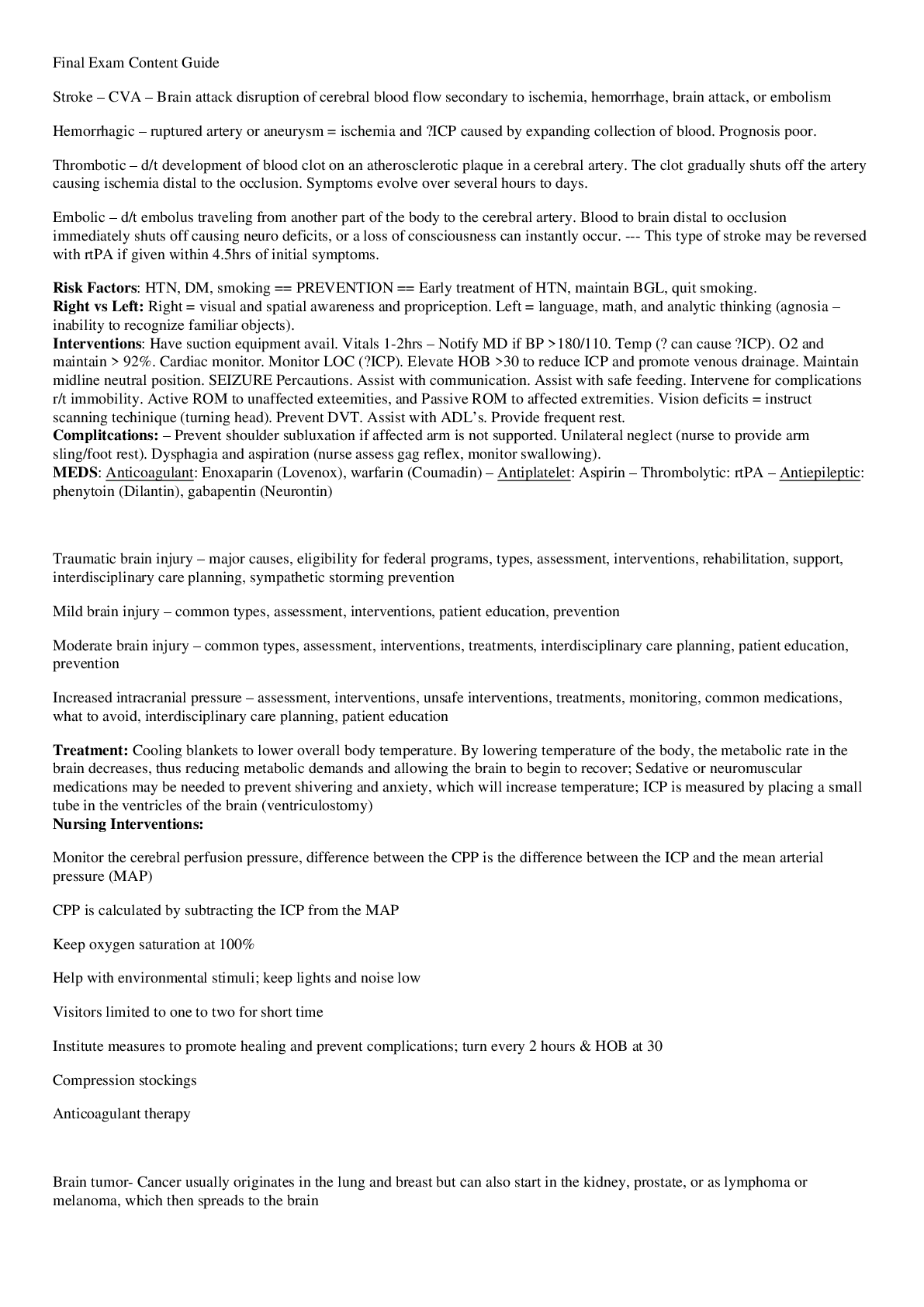
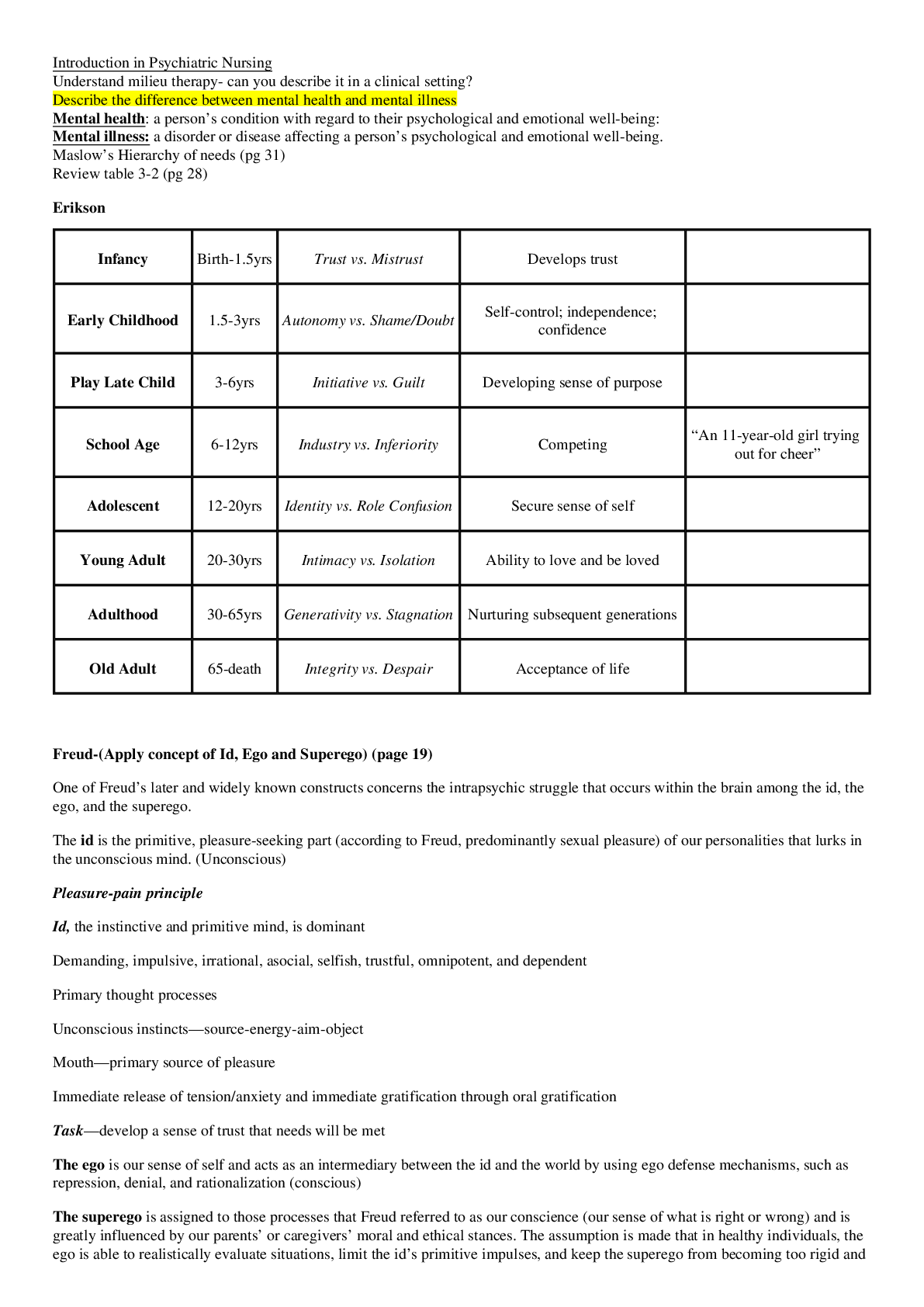
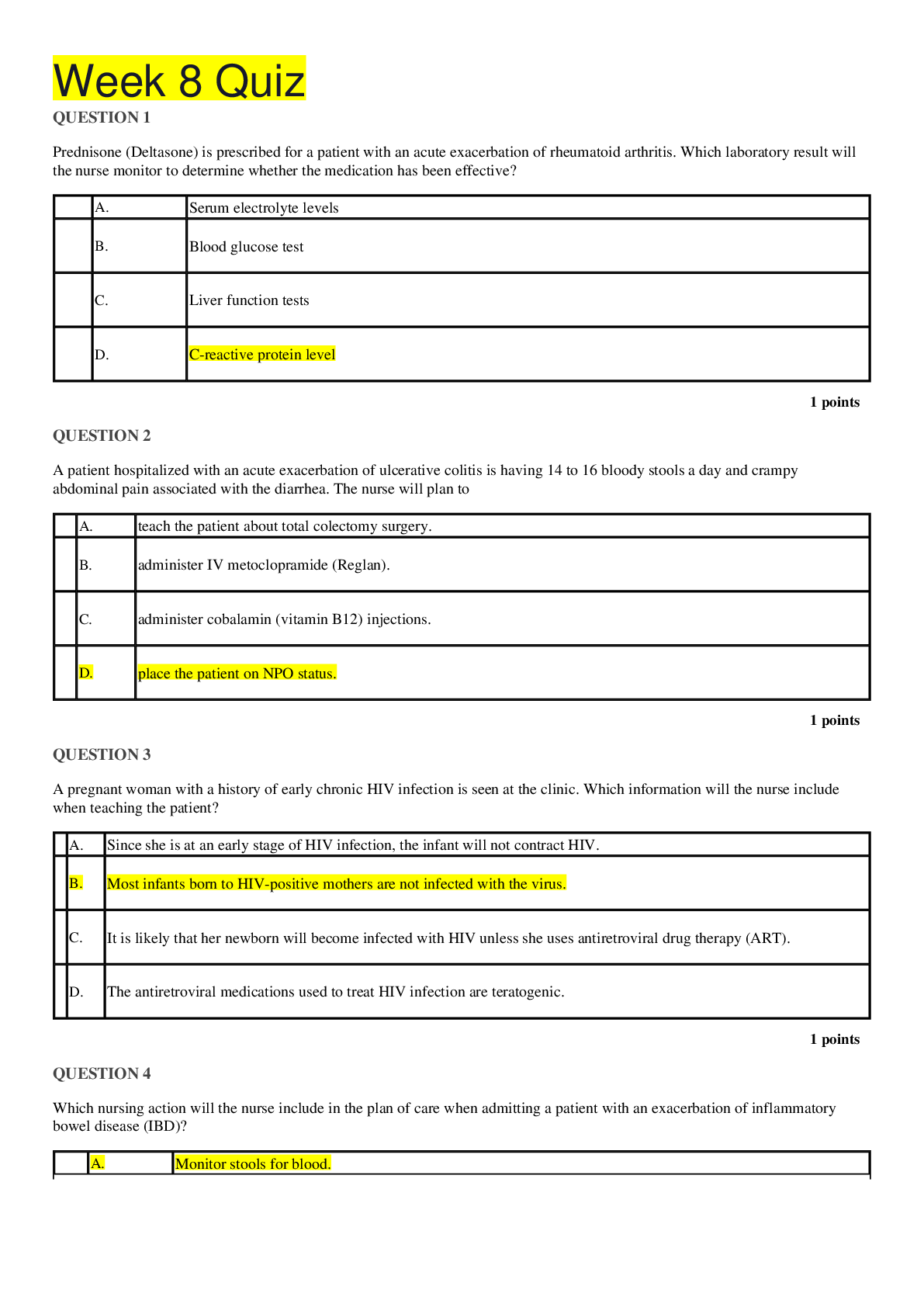
Final Exam Content Guide 1. Stroke – CVA – Brain attack disruption of cerebral blood flow secondary to ischemia, hemorrhage, brain attack, or embolism 1) Hemorrhagic – ruptured artery or aneu... rysm = ischemia and ↑ICP caused by expanding collection of blood. Prognosis poor. 2) Thrombotic – d/t development of blood clot on an atherosclerotic plaque in a cerebral artery. The clot gradually shuts off the artery causing ischemia distal to the occlusion. Symptoms evolve over several hours to days. 3) Embolic – d/t embolus traveling from another part of the body to the cerebral artery. Blood to brain distal to occlusion immediately shuts off causing neuro deficits, or a loss of consciousness can instantly occur. --- This type of stroke may be reversed with rtPA if given within 4.5hrs of initial symptoms. Risk Factors: HTN, DM, smoking == PREVENTION == Early treatment of HTN, maintain BGL, quit smoking. Right vs Left: Right = visual and spatial awareness and propriception. Left = language, math, and analytic thinking (agnosia – inability to recognize familiar objects). Interventions: Have suction equipment avail. Vitals 1-2hrs – Notify MD if BP >180/110. Temp (↑ can cause ↑ICP). O2 and maintain > 92%. Cardiac monitor. Monitor LOC (↑ICP). Elevate HOB >30 to reduce ICP and promote venous drainage. Maintain midline neutral position. SEIZURE Percautions. Assist with communication. Assist with safe feeding. Intervene for complications r/t immobility. Active ROM to unaffected exteemities, and Passive ROM to affected extremities. Vision deficits = instruct scanning techinique (turning head). Prevent DVT. Assist with ADL’s. Provide frequent rest. Complitcations: – Prevent shoulder subluxation if affected arm is not supported. Unilateral neglect (nurse to provide arm sling/foot rest). Dysphagia and aspiration (nurse assess gag reflex, monitor swallowing). MEDS: Anticoagulant: Enoxaparin (Lovenox), warfarin (Coumadin) – Antiplatelet: Aspirin – Thrombolytic: rtPA – Antiepileptic: phenytoin (Dilantin), gabapentin (Neurontin) 2. Traumatic brain injury – major causes, eligibility for federal programs, types, assessment, interventions, rehabilitation, support, interdisciplinary care planning, sympathetic storming prevention 3. Mild brain injury – common types, assessment, interventions, patient education, prevention 4. Moderate brain injury – common types, assessment, interventions, treatments, interdisciplinary care planning, patient education, prevention 5. Increased intracranial pressure – assessment, interventions, unsafe interventions, treatments, monitoring, common medications, what to avoid, interdisciplinary care planning, patient education Treatment: Cooling blankets to lower overall body temperature. By lowering temperature of the body, the metabolic rate in the brain decreases, thus reducing metabolic demands and allowing the brain to begin to recover; Sedative or neuromuscular medications may be needed to prevent shivering and anxiety, which will increase temperature; ICP is measured by placing a small tube in the ventricles of the brain (ventriculostomy) Nursing Interventions: • Monitor the cerebral perfusion pressure, difference between the CPP is the difference between the ICP and the mean arterial pressure (MAP) • CPP is calculated by subtracting the ICP from the MAP • Keep oxygen saturation at 100% • Help with environmental stimuli; keep lights and noise low • Visitors limited to one to two for short time • Institute measures to promote healing and prevent complications; turn every 2 hours & HOB at 30 • Compression stockings • Anticoagulant therapy 6. Brain tumor- Cancer usually originates in the lung and breast but can also start in the kidney, prostate, or as lymphoma or melanoma, which then spreads to the brain - Primary brain tumor means that the cancer originated in the brain tissue; however, this type of tumor is rare - Secondary brain tumor is one that started in another location in the body and spread to the brain or CNS • Treatment: Main interventions are chemotherapy, radiation, & surgery • Potential Complications: Increased intracranial pressure 7. Hepatitis – is inflammation of the liver. Increased inflammation = necrosis interfereing with blood flow to liver. Symptoms – influenza like (Fatigue, joint pain, abd pain, ↓appetite with nausea). Dark urine. Clay stool. Jaundice. Fever. Vomiting. Labs – Elevated ALT/AST and total bilirubin NORMAL VALUES: ALT or SGPT: 10-25 units/L -- 200-400 can = hepatitis or liver damage from drugs/chemicals Jaundice caused by liver = >300 not caused by liver <300 AST or SGOT: 8-38 units/L Liver injury can ↑by 10X. Bilirubin: Total: 0.1-1.2 mg/dL adults Liver Biopsy – most definitive diagnostic approach. Need informed consent. Have Pt lie supine URQ exposed, take EXHALE breath and hold during needle insertion – resume breathing after needle withdrawn. After procedure lie in on Right side and maintain for several hours. a. Who is at risk for: i. Hepatitis A: Individuals living with infected people, sex partners of infected people, traveling to other countries - Fecal/oral route, contaminated food or water (PPE for incontinent PT’s) - Can take vaccine after exposure. ii. Hepatitis B: Health care workers or people exposed to blood and body fluids, inmates in prisons, drug users, multiple sex partners, hemodialysis patients, recipients of clotting factor concentrates - Blood, Body fluids (semen, saliva, vaginal), blood through skin and mucous membranes - Use PPE if exposure to blood. iii. Hepatitis C: IV drug users, recipients of blood products or tissue transplants before 1992, tattoos and piercings - Blood and plasma through skin and mucous membranes - Use PPE if exposure to blood. iv. Hepatitis D: coinfection with hep B b. Chronic Hepatits = B, C, or D. 8. Cirrhosis – Cirrhosis of the liver is a chronic, progressive condition characterized by destruction of the liver cells and subsequent formation of fibrotic tissue that reconfigures normal, healthy liver tissue. This lack of elasticity causes blood, bile, and lymphatic systems to become congested and obstructed, and further damage is incurred. Extensive scarring of the liver caused by necrotic injury or chronic reaction to inflammation over time. Signs and symptoms: Jaundice develops from liver’s inability to handle the flow of bile. Ascites. Petechiae, ecchymosis (large-yellow, purple-blue bruises), nosebleeds. Asterixis (liver flapping tremor – rapid flexion of wrists and fingers). Fetor hepaticus (liver breath – fruity or musty odor). o Causes: 3 major types of cirrhosis, which are differentiated by the underlying pathology. Laënnec’s cirrhosis - Alcoholic Cirrhosis Postnecrotic Cirrhosis: caused by viral hepatitis or certain meds or toxins. Biliary Cirrhosis: chronic biliary obstruction or autoimmune disease. Cardiac Cirrhosis: Occurs when blood flow out of the liver is restricted by severe right sided-sided failure. Tricuspid regurgitation can be associated with cardiac cirrhosis. A large amount of blood is delivered to the liver each minute. When that blood is not able to exit at a predictable rate, liver engorgement occurs and the pressure in the liver vasculature increases, causing venous congestion, anoxia or hypoxia, and hepatic cell necrosis and subsequent fibrosis. LAB: ALT/AST elevated initially due to inflammation, but then return to normal when liver is unable to produce an inflammatory response. - RBC, Hbg, hematocrit, platelet are all decreased. - Ammonia ↑ -- cirrhosis prevents conversion to urea DIAGNOSTIC: Ultrasound, Abd X-ray, CT, LIVER BIOPSY, EGD, ERCP ERCP: Endoscopic retrograde cholangiopancreatography -- used to view the biliary tract to assist in removing stones, to collect specimens for biopsy, and for placement of a stent. Interventions: Monitor Resp status – HOB 30. Skin integrity = Pruritus occurs with jaundice (use cold water and lotion to stop scratching). May need to restrict fluids (ascites, peripheral edema). Monitor neuro status for hepatic encephalopathy. DIET: high carb, fat, and protein – low sodium. If ascites – measure abd girth daily. MEDS: General meds admin’d sparingly. Give diuretics. Lactulose may be needed to rid body of ammonia thru stool. Beta Blockers if PT has varices. Procedures: Paracentesis, Surgical bypass/shunt, liver transplant, 9. Liver damage – Associated lab values, types, common treatments, assessments, interventions, support, interdisciplinary care planning, patient education 10. Liver transplant – Reasons for in children and adults, common medications associated with, lab values, monitoring, interdisciplinary care planning 11. Hemochromatosis – Assessment, diagnostic tests, lab values, interventions, treatments, interdisciplinary care planning, patient education, symptoms, support, long term effects 12. Liver disease – Common symptoms, cause of, risk factors, assessment of, interventions, diagnostic tests, lab values (abnormal), patient education, common medications, what to avoid, interdisciplinary care planning, Kernicterus, Icterus Liver Enzyme Assessments: o Include albumin, total and direct bilirubin, alkaline phosphatase, aspartate transaminase (also known as AST /[SGOT]), and alanine transaminase ALT/[SGPT]). o Further testing could include prothrombin time (PT) after receiving vitamin K, gamma glutamyl transpeptidase (GGT), ammonia (NH3), amylase, viral studies for hepatitis antigens, isocitrate dehydrogenase (ICD), copper, and iron. o Liver enzymes can be elevated with conditions such as diabetes, obesity, autoimmune disorders, some viral infections (especially hepatitis), and some genetic diseases. o Prothrombin and hemoglobin prior to liver biopsy 13. Portal Hypertension -Assessment of, symptoms of, common diagnostic tests, lab values associated with, common medications, interdisciplinary care planning PH - Is the constant pressure of the blood, bile, and lymphatics within the liver. TREATMENT • Shunts to relieve the pressure in the portal vein • Shunts diverted blood from the portal vein to the inferior vena cava, thus bypassing the fibrotic blockage that caused congestion in the liver. distal splenorenal shunt (DSRS) • Transjugular intrahepatic portosystemic shunt (TIPS) 14. Macrovesicular fatty liver – Assessment of, common causes of, risk factors, treatment, diagnostic tests, lab values, patient education, interdisciplinary care planning 15. Musculoskeletal injuries – common types, assessment of, treatment for, common symptoms, activity and work related injuries, patient education, common medication 16. Casting – What risks are associated with applying a cast for a fracture? a. For unstable fractures casts may not be adequate in maintaining bone alignment. Complications of not maintaining proper alignment include nonunion, delayed union, or displacement of the fracture segments. Casts also immobilize the muscles and joints next to the fracture site, and may cause neurovascular compromise, malunion, skin breakdown, and compartment syndrome 17. Meniscal injury – Assessment, symptoms, interventions, diagnostic testing, medications, patient education 18. RICE – What does it mean, when is it used, what does it treat, patient education When educating a patient with a sprain, what exactly should be taught about RICE therapy? a. The immediate goal of treatment are to prevent swelling and to maintain ROM, immediate interventions include Rest, Ice, Compression and Elevation RICE 19. Stress Fractures – Prevention, causes, assessment, treatment, patient education 20. Hip Replacement – Reasons for, types, complications of, monitoring, signs of infection, signs of issues with the replacement, common pain management medications, interdisciplinary care planning 21. Decompensated congestive heart failure – signs and symptoms of, assessment of, common medications, interdisciplinary care planning, patient education, diagnostic tests, lab values 22. Adventitious lung sounds – Assessment, causes of, treatment 23. IV fluids – different types, why they are used and when are each type contraindicated, what to monitor for. 24. Serum sodium concentration – Normal and abnormal values, what to monitor for, symptoms associated with abnormal values, treatment, patient education 25. Potassium – Normal and abnormal values, what to monitor for, symptoms associated with abnormal values, treatment, patient education 26. Acid-base imbalance – Assessment of, causes of, different types, lab values associated with, diagnostic tests, treatment, risks associated with, patient education 27. COPD – Assessment, symptoms, causes, treatment, common medication, risks associated with, common lab values 28. Colon Cancer – Risk factors, assessment, treatment, symptoms of, common treatment, patient education, diagnostic tests 29. Chemotherapy – Common side effects, patient education 30. Bone Marrow Transplant – Monitor, patient education, common medications, risks associated with, types of 31. Lung Cancer – surgical treatments, what to monitor, patient education 32. Sinoatrial node – Function, complications of, symptoms of malfunctions of Pacemaker of heart. 60-100bpm (located – junction superior vena cava and Rt Atrium) 33. Serum electrolytes –complications associated with abnormal values, symptoms of abnormalities, patient education Magnesium Mg (1.8-3) Phosphorus P (2.5–4.5 mg/dL) -- Ca relationship Potassium K (3.5–5 mEq/L) -- Never give IV push, Highest IV rate 10meq/hr (may burn) Calcium Ca (8.5–10.5 mg/dL) -- Inverse relationship with phosphorus – ex: Low P when Ca is elevated Sodium Na (135–145 mEq/L) Carbon dioxide CO2 (22-26 mEq/L) Bicarbonate (venous) 23-29 mEq/L Chloride (cl) – (98-107 mEq/L) -- Bromides can cause false elevation of chloride levels - repeat lab draws 34. Hemoglobin –symptoms of abnormal values, complications of abnormal values, patient education HBG – 12-17 g/dl (Males: 13.5-18 grams/dL; females: 12-16 grams/dL) -Normally, Hgb and Hct levels parallel each other; Hct is usually 3 times higher than Hgb level 35. Anticoagulant therapy - PT and INR: NORM: 9.6-11.8 seconds --- Females slightly under (9.5-11.3) - Coumadin= 1.5 to 2.0 times the control in seconds - INR is similar to PT but standardizes normal values across all lab systems; it measures effectiveness of oral anticoagulation 5. Normal reference ranges are 2.0–3.0 for standard warfarin therapy and 3.0–4.5 for high-dose therapy - An INR >4 may result in ↑risk for bleeding - aPTT: NORM: aPTT value is 20 to 35 seconds, Heparin = 1.5 to 2.0 times the control in seconds - LOW= ineffective therapy HIGH=Risk for bleeding or hemorrhage - Clotting time: normal 8-15minutes 36. Platelets- Normal and abnormal values, risks associated with abnormal values, causes of abnormal values, interventions, medication management, patient education 150,000-450,000 -- Low: Chemo/bone marrow suppression, some infections - When microtrauma occurs and damages blood vessels, platelets aggregate and adhere to altered surface to form hemostatic plug to initiate clot formation 37. Complementary Therapies – Different types, why and when are they used, benefits of, patient education 38. End of life – Stages of grieving, support, patient education 39. Emergency Prioritizing Triaging – Classifications used in ED vs mass casualty Primary survey focuses on airway, breathing, circulation, and neurological disability/deficits (ABCD) a. Clear and open the airway b. Assess for respiratory distress c. Assess quality of ventilation (rate, color, auscultate lungs) d. Check pulses for quality and rate e. Assess for external bleeding f. Take blood pressure g. Assess level of consciousness and pupillary response, weakness or paralysis of extremities Treatment for anthrax RED: Priority I or emergent care is needed for victims who need immediate treatment, such as those with cardiac or respiratory distress, trauma and bleeding, or neurological deficits YELLOW: Priority II or urgent care is needed for victims who need treatment within 2 hours, such as clients with simple fractures, lacerations, or fevers; these victims should be reevaluated every 30 to 60 minutes GREEN: Priority III or non-urgent care is needed for victims who need treatment that can wait for hours; those with sprains, rashes, and minor pain should be reevaluated every 1-2 hrs. ORANGE tag indicates a client who has a non-emergent psychiatric condition BLACK: Victims who are deceased should be labeled with a black tag and transported to designated temporary morgue 40. Burns – Phases, different types, phases, monitoring and treatment associated with each type and phase, interventions, interdisciplinary care planning, patient education, medication management 41. Chest trauma – assessment, clinical manifestations, medication management, diagnostic tests, interventions, lab values 42. Mechanical ventilation – How to communicate with a client who is, complications of, what to monitor, patient education, why and when is it used 43. Sinus bradycardia – Assessment, symptoms, causes, interventions, treatment, common medication management, patient education 44. ECG tracings 45. Shock – The shock syndrome, or acute circulatory failure, can be classified according to etiology into three basic categories: hypovolemic, cardiogenic, and distributive. Sub-categories of distributive shock include neurogenic, anaphylactic, and septic. Causes of the different types: Progression from one stage to the other is dependent on the patient’s health status, duration of the insult, response to therapy, and the correction of the underlying cause. The end result is always the same; tissues fail to receive oxygen and nutrients, and are unable to eliminate waste products -Hypovolemic shock: an insufficient intravascular volume and low cardiac output. == Blood loss due to internal or external bleeding, fluid loss, injury or vomiting, diarrhea, severe dehydration, burns, surgery, ascites, or peritonitis. MANIFESTATIONS OF HYPOVOLEMIC SHOCK Tachycardia is a compensatory helps remove accumulating lactic acid (>5 will probably die). May result in cardiac arrhythmias/chest pain (poor filling of the cardiac arteries during diastole). D/t lack of tissue perfusion, the patient’s LOC is altered. Pulse pressure narrows = diastolic↑. Tachypnea and ↑ in depth of respirations (may gasp for breath). ↓urine output. Skin pale, cool, delayed capillary refill. Jugular veins appear flat. ↓cerebral perfusion and a change in LOC. Disoriented, confused, restless, anxious. Nursing Interventions: Minimize fluid loss. Large diameter catheter – Give Fluids (monitor FV overload), Oxygen, Meds. Observe for changes in Respirations, heart sounds, assess lung sounds, chest pain. (Risk of Secondary shock if given blood products = anaphylactic shock) Monitor lab results, I&O. Give pain meds. Position, the patient with legs elevated, trunk flat, and head and shoulders above the chest (modified Trendelenburg position). Monitor s/s infection (IV). -Cardiogenic Shock: a diminished cardiac output is due to loss of left ventricular pump function. It results in tissue hypoxia even when fluid volume is adequate. MANIFESTATIONS OF CARDIOGENIC SHOCK Hypotension SBP < 90 mm Hg. Heart rate > 100 beats per minute. Weak thready pulse, Diminished heart sounds. Change in level of consciousness (LOC). Cool, pale, moist skin Urine output less than 30 mL/hour Chest pain. Dysrhythmias. Tachypnea. Crackle breath sounds. ↓cardiac output. Nursing Interventions: Fluids, Oxygen, Meds. Observe for changes in Respirations, heart sounds, assess lung sounds, chest pain. Monitor lab results, I&O. Give pain meds to diminish myocardial O2 consumption). Calm environment, education to reduce anxiety. Limit activities to preserve O2. Give pain meds -Distributive shock: 3 types • Anaphylactic shock: due to hypersensitivity to a foreign substance (antigen/antibody reaction). • Neurogenic shock: due to disruption of outflow of sympathetic nervous system response—often due to tissue damage in the spinal cord pathway. (Above T6/T1) • Septic shock: result of overwhelming infection. Phases of shock: Initial - -Decreased CO, impaired tissue perfusion, elevated lactic acid. No clinical s/sx - Position pt. to maximize o2 return to the brain (admin O2), monitor pulse & resp rates, keep normothermic. Compensatory - - Body is trying to bring us back to homeostasis maintain BP and tissue perfusion. -Neural changes: SNS activated (epi/norepi activated) -Hormonal changes: (ACTH is released, kidneys affected, K+/Na+ affected) -Chemical compensation (leads to respiratory alkalosis!) - Monitor heart rate and pulse, blood pressure, central venous pressure (CVP), respiratory rate, core, and peripheral temperature, and urinary output. Pulse oximetry may also be performed. Arterial gases are monitored for accurate assessment. Blood sampling for urea and electrolyte levels, full blood count, and glucose levels may also be performed. Elevated glucose levels are present with release of stress hormones such as cortisol. Progressive - Multi organ dysfunction syndrome (MODS). Organ hypoperfusion Compensating mechanisms begin to fail. Symptoms are evident of inadequate organ perfusion. A full assessment should be done to identify any signs of blood or fluid loss, fluid shift as in ascites, infection, vomiting, or inadequate fluid intake. Refractory - - Death is inevitable. Failure of compensating mechanisms. No response to treatment. Risk of cardiac arrest. A rising serum lactate is an indicator of inadequate tissue perfusion due to metabolic acidosis. Low arterial oxygen content, chest pain, cardiac dysrhythmias, altered LOC, ↓urinary output. MAPB cannot be maintained without assistance. ASSESSMENT AND CARE OF SHOCK SYNDROME Clinical findings correlated with organs compromised by inadequate oxygen. Regardless of the type of shock, it leads to a SBP of less than 90 mm Hg and the narrowing of pulse pressure that is inadequate to meet the tissue needs. (SBP may be elevated initially.) Myocardial infarction – Coronary artery blood flow is blocked by atherosclerotic narrowing, thrombus formation, or (less frequently) persistent vasospasm; myocardium supplied by arteries is deprived of O2; persistent ischemia may rapidly lead to tissue death" Main cause is coronary artery disease (CAD), buildup of atherosclerotic plaque in coronary arteries that restricts blood flow to heart a. Nonmodifiable risk factors include age, gender, family history, and ethnic background b. Modifiable risk factors include smoking, obesity, stress, elevated cholesterol, diabetes mellitus, and hypertension ECG (12-lead): ST elevation, accompanied by T-wave inversion in leads that monitor affected area of heart; these changes resolve as treatment progresses Lab findings: elevated troponins (early or late diagnosis); elevated CK-MB isoenzymes over 5% (early diagnosis); or elevated LDH with “flipped” isoenzymes (late diagnosis)" Signs and Symptoms: N/V or just nausea, Diaphoresis and dizziness, chest pain lasting more than 15min (squeezing or pressure) and may extend to shoulder, left arm, back or jaw, anxiety and feelings of doom Women: fatigue, sleep disturbance, shortness of breath, back pain, upper abdominal pain, epigastric pain, and nausea with or without vomiting are the most commonly identified atypical symptoms seen in women suffering from an AMI. INTERVENTIONS: 1. Assess pain freq; pain is usually first presenting sign of new or extended MI 2. Hemodynamic status: BP,HR, LOC, skin color, temp. (Q5min during pain, Q15min post pain, and every 1-2hrs post MI for 24hrs) 3. ER treatment = MONA = Morphine (Relieve chest pain), oxygen (↑Oxygenation), nitrates (vasodilate coronary blood vessels and ↑ blood supply), and aspirin (antiplatelet agent to interfere with thrombus formation in affected artery). 4. Monitor continuous ECG to detect dysrhythmias (PVC’s and tachy common) With new pain or changes in level or character of pain 12-lead ECG immediately. 5. Monitor resp, breath sounds, admin O2 (2-4L/min) to ↑O2 to heart. 6. Provide rest to ↓O2 demand to heart 46. Angina: Angina is defined as acute cardiac pain caused by inadequate oxygen reaching the myocardium. Chest pain resulting from this restricted blood flow; (Women, diabetics, and elderly patients may not present with typical angina pain) a. Stable - a predictable response to increased activity. Ischemic episodes are precipitated by factors that increase oxygen demand (exercise) or reduce oxygen supply (anemia). Chest pain occurs predictably with the same onset, duration, and intensity and is relieved when the precipitating factor is removed or with nitroglycerin administration. b. Unstable - with unpredictability (at rest) and increasing severity – Often precursor to MI. Combo of unstable and MI = acute coronary syndrome (ACS). This syndrome is the result of rupture of an unstable or vulnerable plaque. Rupture of the plaque results in platelet aggregation and thrombus. c. Prinzmetal- caused by arterial spasm often awaking client from sleep. Underlying coronary artery stenosis may be absent. Ischemia occurs because of transient focal decreased oxygen supply unrelated to oxygen demand. Five assessment components (PQRST): factors that precipitate the symptoms, quality, radiating, severity/location, Time/duration, and factors that relieve the symptoms. Angina pain quality is typically described as pressure, heavy, squeezing, constrictive, suffocating, vise-like, or “like an elephant sitting on my chest.” Angina is rarely described as pain. Episodes may vary from mild to severe. Several symptoms may accompany angina pain including nausea, diaphoresis, SOB, fatigue, dizziness, weakness, and anxiety. Anginal pain is not stabbing or sharp and does not change with respirations, position change, or pressure applied to the chest wall. To demonstrate anginal pain, the patient may place a clenched fist over the sternum. This is referred to as the Levine’s sign, the universal sign for angina. 47. Vasopressin (DDAVP) – What it is used for, when is it ordered, what to monitor, patient education 48. Kidney failures – Different types, risk factors, assessment, treatment, monitoring, patient education 49. Compartment syndrome –Swelling in the soft tissues and muscles = compromised circulation to that area 50. Pathological fractures – Diseases associated with, monitoring of, patient education 51. Fractured pelvis – complications of, monitoring, patient education 52. Blood Gas Values – Normal and abnormal lab values, signs and symptoms associated with abnormal values causes of abnormalities, treatment of, complications of abnormal values. Normal Arterial Blood Gases: Serum Ph.: 7.35-7.45 PaCO2 – Carbon Dioxide: 35-45 HCO3 – Bicarbonate: 22-26 PaO2 – Oxygen: 80-100 53. Define: a. Ascites: The accumulation of fluid in the peritoneal cavity. b. Cholangitis: Inflammation of the bile duct c. Cholecystitis: Inflammation of the gallbladder. d. Cholelithiasis: Gallstones. e. Cholestasis: Any condition that impedes bile flowing freely through the bile ducts. f. Gluconeogenesis: The process of the liver converting predominant amino acids to glucose in the fasting state g. Glycogen hydrolysis: Conversion of stored glycogen into usable glucose to meet the immediate energy needs of the body. h. Glycogen synthesis: Conversion of glucose to glycogen that can be stored in preparation of times of fasting i. Gynecomastia: Breast enlargement in men j. Hepatomegaly: Enlarged liver, palpated below the level of the ribs. k. Icterus: Yellow coloration in the sclera of the eye l. Jaundice: Yellow pigmentation of the skin and sclera. m. Laparoscopic cholecystectomy: A surgical procedure using a laparoscope to remove the gallbladder n. Liver lobule: The functional unit of the liver o. Refractory ascites: Ascites that cannot be effectively managed with normal therapies. p. Steatorrhea: Pale-yellow, greasy, fatty stool, or chronic watery diarrhea Musculoskeletal Trauma Define: o Ankle sprain: When the ankle is displaced or a sudden force is applied, the ligaments are stretched beyond their normal stretching capacity and a sprain of the ligament occurs. o Arthroscopy: A diagnostic test performed in the knee joint; an arthroscopy is an endoscopic procedure used to diagnose and repair meniscal, patellar, extrasynovial, and synovial diseases o Closed reduction: External manipulation of a fracture, which forces it into alignment. o Compartment syndrome: Swelling in the soft tissues and muscles that in turn cause compromised circulation to that area o Cryotherapy: The use of ice or cold water over an injury site to decrease inflammation. o Fascia: An inelastic connective tissue that covers and separates muscles, tendons, and ligaments o Fasciotomy: Incision through a fibrous layer that separates muscles o Fracture: A break in a bone o Occult fracture: clinical symptoms of a fracture but no evidence on x-ray o Overuse syndrome: An injury to musculoskeletal tissues affecting the upper extremity or cervical spine, resulting from repeated movement, temperature extremes, overuse, incorrect posture, or sustained force or vibration. Also called repetitive motion injuries or cumulative trauma disorders. o Phantom limb sensation: When the patient has the perception of a limb that is no longer there. If the patient feels pain it is known as phantom limb pain. o Prosthesis: A replacement of a missing body part, such as an extremity. o Radiculopathy: A term used to specifically describe pain and other symptoms, like numbness, tingling, and weakness, in arms or legs that are caused by a problem with nerve roots o RICE: The acronym used for Rest, Ice, Compression, and Elevation when treating a sprain. o Rotator cuff tears: Refers to tears in one or more of the four muscles that form a single tendon in the shoulder. The rotator cuff is responsible for circumduction and internal and external rotation of the shoulder. o Sports medicine: The application of professional knowledge to the understanding, prevention, treatment, and rehabilitation of sports- and exercise-related problems. EXAM QUESTIONS 1) A client with a new burn injury asks the nurse why he is receiving intravenous cimetidine (Tagamet). What is the nurse’s best response? ---- “This will help prevent stomach ulcers, which are common after burns.” 2) The nurse is assigned a group of patients. Which patient would the nurse identify as being at increased risk for impaired gas exchange? ---- A patient with a hemoglobin of 8.5 g/dL 3) The nurse is assessing a patient for the adequacy of ventilation. What assessment findings would indicate the patient has good ventilation? (Select all that apply.) ---- 1. Oxygen saturation level is 98%. 2. Nail beds are pink with good capillary refill. 3. There is presence of quiet, effortless breath sounds at lung base bilaterally. 4) The nurse is assessing a patient's differential white blood cell count. What implications would this test have on evaluating the adequacy of a patient's gas exchange? -----Elevation of WC = generalized inflammation WRONG: A. White cell count will differentiate types of respiratory bacteria. 5) The nurse would identify which patient as having a problem of impaired gas exchange secondary to a perfusion problem? A patient with --- Peripheral artery disease of LE WRONG: severe anemia secondary to chemotherapy 6) A client is in the emergency department after being rescued from a house fire. After the initial assessment, the client develops a loud, brassy cough. What intervention by the nurse takes priority? ---- Apply oxygen and continuous pulse oximetry. 7) The nurse would identify which body systems as directly involved in the process of normal gas exchange? (Select all that apply.)----- Cardiovascular system, Pulmonary system, Neurologic. 8) The RN has assigned a client who has an open burn wound to the LPN. Which instruction is most important for the RN to provide the LPN? ------ Wash hands on entering the client’s room. 9) The acid-base status of a patient is dependent on normal gas exchange. Which patient would the nurse identify as having an increased risk for the development of respiratory acidosis? A patient with ---- Chronic lung disease with ↑CO2 retention WRONG: --- acute anxiety, hyperventilation, and decreased carbon dioxide retention 10) A client who weighs 90 kg and had a 50% burn injury at 10 AM arrives at the hospital at noon. Using the Parkland formula, calculate the rate that the nurse should use to deliver fluid when the IV is started at noon. ---- 4ml/Kg/%TBSA per 24 hours ---- 4 X 90 = 360 X 50 = 18,000 ---- Give half in first 8 hours 9,000/8 and second half in 16 hours 9,000/16. HOWEVER!!!! (Burn at 10am and its noon, so 6 hour infusion needed) 9,000 / 6 = 1,500mL/hr [Show More]
Last updated: 1 year ago
Preview 1 out of 16 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 13, 2020
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
May 13, 2020
Downloads
0
Views
47






.png)

.png)

.png)

