*NURSING > STUDY GUIDE > NR 566 (NR566Advanced Pharmacology) NR 566 final study guide / NR566 Week 5 Study Outline (latest sp (All)
NR 566 (NR566Advanced Pharmacology) NR 566 final study guide / NR566 Week 5 Study Outline (latest spring 2020)
Document Content and Description Below
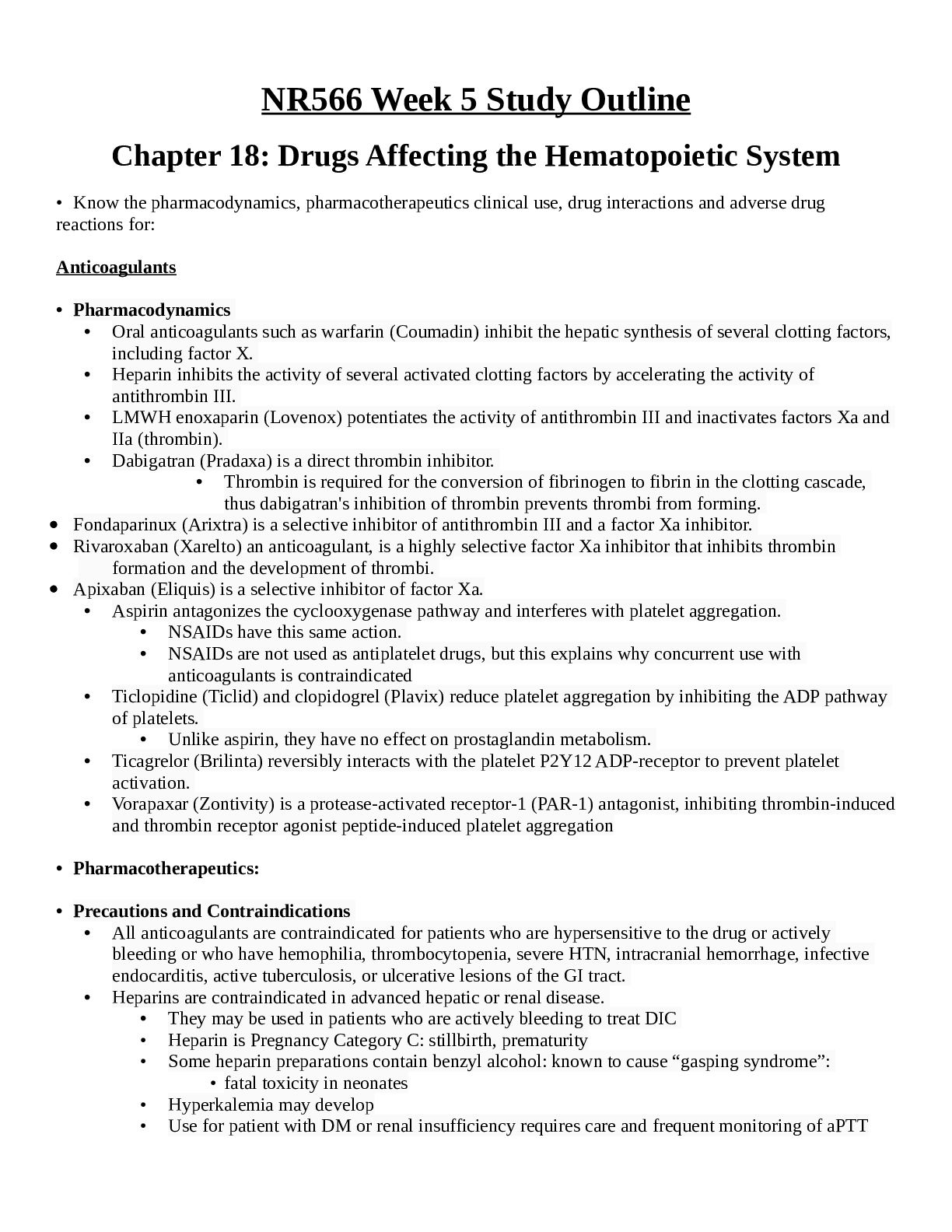
NR566 Week 5 Study Outline Chapter 18: Drugs Affecting the Hematopoietic System • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions for: Anti... coagulants • Pharmacodynamics • Oral anticoagulants such as warfarin (Coumadin) inhibit the hepatic synthesis of several clotting factors, including factor X. • Heparin inhibits the activity of several activated clotting factors by accelerating the activity of antithrombin III. • LMWH enoxaparin (Lovenox) potentiates the activity of antithrombin III and inactivates factors Xa and IIa (thrombin). • Dabigatran (Pradaxa) is a direct thrombin inhibitor. • Thrombin is required for the conversion of fibrinogen to fibrin in the clotting cascade, thus dabigatran's inhibition of thrombin prevents thrombi from forming. • Fondaparinux (Arixtra) is a selective inhibitor of antithrombin III and a factor Xa inhibitor. • Rivaroxaban (Xarelto) an anticoagulant, is a highly selective factor Xa inhibitor that inhibits thrombin formation and the development of thrombi. • Apixaban (Eliquis) is a selective inhibitor of factor Xa. • Aspirin antagonizes the cyclooxygenase pathway and interferes with platelet aggregation. • NSAIDs have this same action. • NSAIDs are not used as antiplatelet drugs, but this explains why concurrent use with anticoagulants is contraindicated • Ticlopidine (Ticlid) and clopidogrel (Plavix) reduce platelet aggregation by inhibiting the ADP pathway of platelets. • Unlike aspirin, they have no effect on prostaglandin metabolism. • Ticagrelor (Brilinta) reversibly interacts with the platelet P2Y12 ADP-receptor to prevent platelet activation. • Vorapaxar (Zontivity) is a protease-activated receptor-1 (PAR-1) antagonist, inhibiting thrombin-induced and thrombin receptor agonist peptide-induced platelet aggregation • Pharmacotherapeutics: • Precautions and Contraindications • All anticoagulants are contraindicated for patients who are hypersensitive to the drug or actively bleeding or who have hemophilia, thrombocytopenia, severe HTN, intracranial hemorrhage, infective endocarditis, active tuberculosis, or ulcerative lesions of the GI tract. • Heparins are contraindicated in advanced hepatic or renal disease. • They may be used in patients who are actively bleeding to treat DIC • Heparin is Pregnancy Category C: stillbirth, prematurity • Some heparin preparations contain benzyl alcohol: known to cause “gasping syndrome”: • fatal toxicity in neonates • Hyperkalemia may develop • Use for patient with DM or renal insufficiency requires care and frequent monitoring of aPTT • Has been associated with fatal medication errors r/t different strengths of preparations • JCo: anticoagulant therapy is a National patient Safety Goal: plan in place at each facility to reduce patient harm • LMWHs are contraindicated for patients with allergies to pork, sulfites, or benzyl alcohol; uncontrolled bleeding; and in patients who have antiplatelet antibodies • Renal impairment: cautious use • Body weight less than 50 kg associated with increased r/f bleeding: • enoxaparin dose adjustment • Cautious use: untreated HTN, retinopathy (HTN or DM caused), severe liver disease, recent Hx of ulcer, or malignancy • Not used for thromboprophylaxis in patients with mechanical heart values: especially pregnant (r/f heart value thrombosis) • Enoxaparin: Preg Cat B, tinzaparin: teratogenicity and fetal death, fondaparinux: Preg B • First line drug for women who require antithrombotic therapy during pregnancy: LMWH • Pharmacokinetics of LMWH is altered during pregnancy • Warfarin • Hepatic dysfunction potentiates response through impaired synthesis of coagulation factors • Use with caution: Hypermetabolic states produced by fever or hyperthyroidism increase responsiveness to warfarin: • r/t increased catabolism of vit K dependent coagulation factors • Increased r/f bleeding in older adults • Caution use based on balance between potential for decreased r/f thromboembolism and the risk for bleeding especially in those with dementia or severe cognitive impairment: Hx of three falls in the previous year or recurrent injurious falls, uncontrolled HTN, or non-adherent or unreliable • Warfarin is Pregnancy Category X: Crosses placenta and can cause hemorrhagic disorders in the fetus and serious birth defects • Safe during lactation • Rivaroxaban (Xarelto): Black-Box Warning: premature discontinuation of anticoagulants including rivaroxaban may lead to thrombotic events. • An increased risk of stroke is seen in patients with atrial fibrillation when transitioning to warfarin • Rivaroxaban is Pregnancy Category C and is not recommended for use in pregnant women. • Apixaban (Eliquis): Black Box warning premature discontinuation leading to thrombotic events • Although there are no well-controlled studies: Pregnancy Category B • Hypersensitivity to aspirin and cross-sensitivity with NSAIDs may occur, contraindicating the drug • Aspirin hypersensitivity is more prevalent in patients with asthma, nasal polyps, or chronic urticaria. • Reye syndrome has been associated with its use in children and teenagers who have influenza or chickenpox. • Reversible hepatotoxicity has occurred • Use with caution in liver damage, preexisting hypoprothrombinemia, or vit K deficiency • Preg Cat C and Cat D in third trimester • Avoid during lactation • Clopidogrel and ticlopidine: severe hepatic disease (r/f bleeding d/o), do not use in these patients • Not recommended for patients with GI d/o • Preg Category B • Ticlopidine: clearance increased with age, older adults increased sensitivity to this drug (closely monitor or ADRs) • Older adults: increased levels of clopidogrel: no dosage adjustments • In older adults clopidogrel is a safer drug • Ticlopidine: elevations in cholesterol and TC within 1 month of therapy: factor in HLD • Ticagrelor: Black-Box Warning to not use in a patient with active pathological bleeding or history of intracranial hemorrhage. • Ticagrelor should be discontinued 5 days prior to any surgery. • Dabigatran: Black-Box Warning concerning discontinuation increasing risk of thrombotic events. • There is no reversal agent available for dabigatran • Vorapaxar: Black-Box Warning to not use in patients with a history of stroke, TIA, intracranial hemorrhage, or active pathological bleeding. • Vorapaxar is Pregnancy Category B, with no congenital malformations found in animal studies • ADRs • All anticoagulants: excessive bleeding • Risk is higher early in therapy, with wide fluctuations in aPTT or INR, and older adults (especially women over 60) • Heparins: cause thrombocytopenia and anemia • More likely with bovine than with porcine • Early thrombocytopenia 2 to 3 days after starting therapy and delayed forms 7 to 12 days • Platelet below 100,000: d/c heparin • Enoxaparin antidote: protamine sulfate 1 mg for each mg of enoxaparin dalteparin and tinzaparin: 1 mg for each 100 anti-Xa IUs of dalteparin • Slow IV injection • Fondaparinux: no known antidote • Heparin has a short half-life: Tx is usually d/c of the drug • Protamine sulfate antidote for heparin OD • Warfarin: toxicity and OD Tx withholding one or more doses • Or 1 to 10 mg of vitamin K is the antidote for minor bleeding • 5 to 50 may be used for frank bleeding • Hemorrhagic skin necrosis in women and cyanotic toes in men have been reported • r/t transient inhibition in proteins S and C • Allergic reactions: symmetrical, maculopapular, erythematous lesions • Some are isolated and some confluent: face, neck, and torso • May not appear until 8 to 10 days • Ribaroxaban: bleeding is major ADR • No reversal agent • Back pain, upper ABD pain, osteoarthritis, dyspepsia, and fatigue • Apixaban: bleeding • No reversal agent • ASA: gastric erosions: increased r/f serious upper GI bleeding • More likely when used in combo with other anticoags such as warfarin • Salicylism (tinnitus) : serum levels above 200 mcg/mL • Toxicity: tinnitus, HA, hyperventilation, agitation, confusion, lethargy, diarrhea, and sweating • Ticagrelor: bleeding • Dyspnea: sometimes improves with use or must be d/c • HA, cough, dizziness, and nausea • Ticlopidine: reversible neutropenia at 3 weeks to 3 months after initiation of therapy • Severe neutropenia (<450) or thrombocytopenia (<80,000) d/c drug • Clopidogrel: ADRs similar to ASA, safe and effective • Dabigatran: bleeding • GI ADRs: dyspepsia and gastritis-like symptoms • Angioedema and thrombocytopenia • Vorapaxar: bleeding • Anemia, depression, and rashes or eruptions • Drug Interactions • Cephalosporins and PCNs given parenterally associated with coagulopathies, increased r/f bleeding when given with Heparin • Second and third gen cephalosporins and high doses of PCNs: increased r/f bleeding with Warfarin • Drugs that affect platelet functioning or cause hypoprothrombinemia (ASA, NSAIDS, dipyridamole, quinidine, and valproic acid: increased r/f bleeding • Heparin and LMWHs: similar drug interactions: also interact with antiplatelets including NSAIDS and dextran • Foods can effect anticoags • Warfarin: many drug interactions and increased INR monitoring within 4 to 7 days when other drugs are started or stopped even ABX • Vit K: antagonistic interaction with warfarin: decreases effectiveness • Inhibitors of CYP 1A2, CYP 2C9, or CYP 3A4 increase effect of warfarin • Inhibitors decrease the effectiveness of warfarin • Interacts with any other drug that increased bleeding: anticoags, antiplatelets, NSAIDS and SSRIs • ABX and antifungals may affect INR • Herbal Productions may increase bleeding: ginkgo biloba and garlic • Decrease effectiveness: St John’s wort, ginseng, and coenzyme Q10 • May influence metabolism of warfarin: St John’s wort, echinacea, ginkgo, goldenseal, AND GRAPEFRUIT JUICE • Dabigatran: rifampin (decreased levels of dabigatran) • Dronedarone increased dabigatran levels by 70 to 150% • CCB verapamil: increases dabigatran • Amiodarone increases dabigatran • Clopidogrel increases dabigatran • Ticagrelor: metabolized by CYP 3A4: avoid strong inhibitors ketoconazole, itraconazole, voriconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, atazanavir, and telithromycin • Avoid inducers: rifampin, dexamethasone, phenytoin carbamazepine, and phenobarbital • Vorapaxar: avoid with CYP3A inhibitors • Avoid use of inducers (rifampin, carbamazepine, St John’s Wort, and phenytoin • Clinical Use and Dosing Prevention and Treatment of Thromboembolism • Warfarin: drug of choice for prevention of venous thrombosis, systemic thrombosis, and pulmonary embolism o For prevention: give dose sufficient for INR between 2 and 3 o Beginning dose is 10 mg daily for the first 2 days with a recheck of INR in two to three doses o ICSI guidelines: recommend starting warfarin at 5 mg/day with a range of 2.5 mg to 7.5 mg/day o Further dosing is based on INR o Lower initiation doses for: Older than 75 Multiple comorbid conditions Poor nutrition (low albumin) Elevated INR when off warfarin Elevated LFTS Changing thyroid status o If INR is greater than 2 after the first 3 doses, consider decreased the dose by one half o If INR raises rapidly: search for reasons: drug interactions, poor nutrition, infection, or systemic disease process • Acute PE, DVT, or acute systemic embolization: admit to hospital for IV anticoagulation o Heparin, LMWH, or SC fondaparinux and then placed on oral anticoags o Treat while waiting on Dx tests o Acute PE: heparin, LMWH, or fondaparinux for at least 5 days until INR is greater than or equal to 2 for 24 hrs o ACCP recommends staring warfarin on the first day of Tx in conjunction with heparin, LMWH, or fondaparinux or SX heparin o PE due to transient (reversible) risk factor is warfarin for 3 months • Superficial Vein Thrombosis: 45 days of prophylaxis with fondaparinux or LMWH o Lower limb of at least 5 cm in length o ACCP recommends fondaparinux 2.5 mg/day over prophylactic LMWH • Deep Vein Thrombosis: Divided the Tx of acute DVT into acute treatment of DVT of the leg and Tx of the upper extremity DVT o Leg or UE: short term Tx with SC LMWHs, SC fondaparinux, or IV or SC heparin for at least 5 days and until the INR is 2 for 24 hr o LMWH and SC fondaparinux: preferred over heparin o Warfarin: initiated on the first Tx day (like PE) • Idiopathic DVT: maintained on warfarin with target of 2.5 (range 2.0 to 3.0) for 3 months • Indwelling Cline: at r/f DVT o Tx is the same as for leg DVT o After Cath removed: 3 months of anticoags (Warfarin) • All other patients requiring anticoags therapy can be started on Warfarin as OPs o 10 mg/day or 5 mg/day, o Unless patient wt. is less than 110 lbs., over 75, or at ARF bleeding Start these patients on 2.5 mg/day o Steady state is achieved in 5 to 7 days: dosage adjustments are made ATT based on INR • Goal of therapy is an INR of 2 to 3 for all Tx durations • For patients with DVT or PE and CA: LMWH for 3 to 6 months o Referral for management • Air travel time longer than 8 hrs: increases r/f thrombus formation o Wear loose clothing, avoid tight clothing around the waist or lower extremities, good hydration, and frequent calf muscle exercises o At high risk for DVT: wear compression stockings 15 to 30 mm Hg during air travel • Immobility (bedrest): ambulation as tolerated o Use of compression stocking with 30 to 40 mm Hg for 2 years after DVT episode Prevention of Embolic Stroke in AFib • Low risk for stroke: ASA 75 mg to 325 mg daily • Intermediate risk for stroke: oral anticoags o Anticoags or a combination of ASA and clopidogrel • High risk for stroke: oral anticoags o ACCP recommends: 150 mg of dabigatran BID rather than warfarin • For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 • For AFib and mitral stenosis: follow recommendation of those at high risk o If valve replacement: follow recommendations for those with heart valves regardless of AFib • Apixaban: to reduce risk of stroke and systemic embolism in non-valvular AFib o 5 mg BID o For those older than 80, less than 60 kg, or crt >1.5 dose at 2.5 mg BID Mitral Valve Disease • Rheumatic MVD but no AFib and left atrial diameter of less than 55 mm: no therapy • Rheumatic MVD with left atrial diameter of greater than 55 mm or left atrial thrombus or AFib or previous embolism: warfarin target INR of 2.5 • Therapy is continued indefinitely in all cases Antithrombotic Therapy for Ischemic Stroke • Acute ischemic stroke or TIA: early (within 48 hours) ASA therapy at 160 to 325 mg • ACCP has three options for long term therapy after noncardioembolic ischemic stroke or TIA • 75 to 100 mg ASA/day • Combo of ASA (25 mg) and ER dipyridamole or clopidogrel • Patients with Hx of ischemic stroke or TIA with AFib: 150 mg dabigatran BID over warfarin Recurrent Embolism or Prosthetic Heart Valves • Warfarin: drug of choice o Therapy initiated and maintained the same as for prevention of venous thrombosis o Except that the target INR is valve dependent • For patients with additional risk factors (AFib, MI, left atrial enlargement, endocardial damage, and low EF) o 75 to 100 mg/day of ASA should be added to Warfarin protocol o The same is true for patients with caged ball or caged disc valves • Bioprosthetic valves in SR: 75 to 100 mg/day of ASA o Therapy is continued indefinitely for mechanical heart valves • For systemic embolization that recurs after 6 months of therapy: therapy is continues for an additional 12 months • Pregnant patients with MHV: require anticoags o Use one of three treatment regiments LMWH BID SC heparin every 12 hours Or SX heparin or LMWH until the 13th week of pregnancy then warfarin until close to delivery with LMWH or heparin is resumed o Warfarin is a known teratogen: may cause fetal hemorrhage o Women with MHV at high risk of thromboembolism: ASA 75 to 100 mg/day added to anticoags regimen o Women on warfarin planning on pregnancy: frequent pregnancy tests and substitution of heparin or LMWH when pregnancy is achieved o Anticoagulation specialist and perinatologist Prevention of MI • Several protocols are effective in prevention of MI in patients with and w/o CAD o Over 50 w/o symptomatic CVD: ASA 75 to 100 mg/day o Established CAD (1 year post ACS, with prior revascularization, coronary stenoses greater than 50% by angiogram, and/or evidence for cardiac ischemia on Dx testing): ASA 75 to 100 mg/day or clopidogrel (75 mg/day) o Patients with ACS who have undergone PCI with or w/o stent placement: dual therapy: 90 mg ticagrelor BID plus ASA 75 to 100 mg/day ACCP: recommends use of ticagrelor over clopidogrel in PCI • Patient who have experienced an MI: anticlot therapy o STEMI: fibrinolytics then ongoing therapy after hospital d/c • Post-AMI TX: • Anterior AMI w/ r/f LV thrombus who do not get a stent: warfarin (INR target 2 to 3) and ASA 75-100 mg/day • Patients with an acute MI who have a bare metal stent: triple therapy o Warfarin (INR target 2-3), ASA low dose, and 75 mg daily clopidogrel for a month after stent placement o Then warfarin and one antiplatelet drug for months 2 and 3 o After 3 months: d/c warfarin and replaced with dual antiplatelet therapy (90 mg ticagrelor BID plus ASA 75 to 100 mg/day for up to 12 months • Patients with DM: ASA 75 to 162 mg/day • Vorapaxar: approved for reduction of thrombotic CV events in patients with Hx of MI or with PAD o Patient takes one 2.08 mg tablet daily in addition to ASA or clopidogrel Prevention of Post-Operative Thromboembolism • J Co requires that all hospital have a formal active strategy to prevent venous thrombosis • LMWH, low dose heparin, or fondaparinux o Moderate-risk major general surgery, higher risk patients who are having a major procedure for CA, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries • Length of Tx: determined by the type of surgery, ranging from a single dose to 10 days for most orthopedic procedures, to 28 days in high risk patients, patients undergoing major gynecological surgery, and patients having major surgery for CA • Hip or knee replacement: Apixaban 2.5 mg BID Perioperative Therapy of Patients on Warfarin or Antiplatelet Therapy • Stop Warfarin 5 days before surgery and resume 12 to 24 hours after surgery • For prevention of thromboembolism (MHV, AFib): may require parenteral anticoags perioperatively o Decision to bridge with heparin is determined by balancing r/f bleeding due to the surgical procedure and clotting risk due to the underlying d/o • Low bleeding risk: skin biopsies, cataract surgery, and most dental procedures can remain on warfarin o Dental procedures: tranexamic acid mouthwash can be used w/o interrupting anticoags therapy • Low risk thromboembolic risk (AFib w/o prior stroke or remote Hx of venous thrombosis): warfarin stopped 5 days prior to surgery and resumed that evening of surgery • High thromboembolic risk (PHV): bridging with LMWH or unfractionated heparin may be indicated • Antiplatelets: do not d/c before surgery • Rational Drug Selection • Cost can be significant • PO anticoags are preferred: no special equipment or skills to administer, less expensive • Brands are not interchangeable • Monitoring • Dosage adjustments of warfarin is by INR o Daily INRs initially to guard against excessive anticoagulation until therapeutic range for 2 days o Testing interval is then lengthened to 2 or 3 times weekly for 1 or 2 weeks o Self-testing is increasing in popularity: competency using the equipment o Computer assisted, validated, decision, support tools for warfarin dose regulation: more effective than traditional dosing at maintaining therapeutic INR values o Evidence based dosing tools, patient Edu, follow up, and optimal patient communication: best patient outcomes o CYP 2C9 or VKORC1 gene variants: may require 2 to 4 weeks longer to reach target INR • Monitoring heparin adjustments: aPTT blood tests o Goal of therapy is 1.5 to 2.5 times the control o Platelet and Hct every 2 or 3 days o Thrombocytopenis: tends to occur about 4th day and resolves despite continued heparin therapy o Day 8: thrombocytopenia severe enough to require d/c med o After this time period: periodic testing of platelet and Hct and occult blood in stool o Low doses of SC heparin (5,000 U BID) do not require monitoring r/t does not prolong the aPTT • LMWH: same periodic monitoring of platelet and Hct: likelihood of thrombocytopenia is much less o Test for monitoring: anti factor Xa assay o aPTT may be prolonged: dopes not reliably reflect activity o Routine Xa not recommended: except in pregnant patients • ASA dose for antiplatelet therapy is low to moderate o Serum salicylate level is approximately 100 mcg/mL • Clopidogrel: safety profile similar to ASA, no routine monitoring • Ticlopidine: Severe neutropenia and thrombocytopenia have occurred o CBC, WBC with differential counts every 2 weeks, starting from the second week to the end of the third month of therapy o More frequent monitoring is necessary for patients whose absolute neutrophil counts consistently decline or are 30% lower than baseline o After the first 3 months: CBCs as needed for s/s of infection • Also know: Use of anticoagulants in pregnancy: • Enoxaparin is Pregnancy Category B. • Teratogenicity and fetal death have been reported as well for tinzaparin, although a clear cause-and-effect relationship was not established. • Fondaparinux is also listed as Pregnancy Category B but without adequate or well-controlled studies in pregnancy. • LMWHs do not cross the placenta and do not cause teratogenicity or fetal bleeding • The American College of Chest Physicians recommends LMWH as the first-line drug for women who require antithrombotic therapy during pregnancy: enoxaparin (Lovenox), dalteparin (Fragmin), and tinzaparin (Innohep) • The pharmacokinetics of LMWHs are altered during pregnancy. • LMWH passes in small amounts into breast milk but has low oral bioavailability and may be safely used during breastfeeding Thromboprophylaxis • Prevention and treatment of thromboembolism: o Warfarin is drug of choice for the prevention of venous thrombosis, systemic thrombosis, and pulmonary embolism • Prevention of embolic stroke in AFib: o Low risk for stroke: ASA 75 mg to 325 mg daily o Intermediate risk for stroke: oral anticoags Anticoags or a combination of ASA and clopidogrel o High risk for stroke: oral anticoags ACCP recommends: 150 mg of dabigatran BID rather than warfarin o For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 • Prevention of MI o Several protocols are effective in prevention of MI in patients with and w/o CAD Over 50 w/o symptomatic CVD: ASA 75 to 100 mg/day Established CAD (1 year post ACS, with prior revascularization, coronary stenoses greater than 50% by angiogram, and/or evidence for cardiac ischemia on Dx testing): ASA 75 to 100 mg/day or clopidogrel (75 mg/day) Patients with ACS who have undergone PCI with or w/o stent placement: dual therapy: 90 mg ticagrelor BID plus ASA 75 to 100 mg/day • ACCP: recommends use of ticagrelor over clopidogrel in PCI o Patient who have experienced an MI: anticlot therapy STEMI: fibrinolytics then ongoing therapy after hospital d/c o Post-AMI TX: o Anterior AMI w/ r/f LV thrombus who do not get a stent: warfarin (INR target 2 to 3) and ASA 75-100 mg/day o Patients with an acute MI who have a bare metal stent: triple therapy Warfarin (INR target 2-3), ASA low dose, and 75 mg daily clopidogrel for a month after stent placement Then warfarin and one antiplatelet drug for months 2 and 3 After 3 months: d/c warfarin and replaced with dual antiplatelet therapy (90 mg ticagrelor BID plus ASA 75 to 100 mg/day for up to 12 months o Patients with DM: ASA 75 to 162 mg/day o Vorapaxar: approved for reduction of thrombotic CV events in patients with Hx of MI or with PAD Patient takes one 2.08 mg tablet daily in addition to ASA or clopidogrel • Prevention of Post-Operative Thromboembolism o J Co requires that all hospital have a formal active strategy to prevent venous thrombosis o LMWH, low dose heparin, or fondaparinux Moderate-risk major general surgery, higher risk patients who are having a major procedure for CA, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries o Length of Tx: determined by the type of surgery, ranging from a single dose to 10 days for most orthopedic procedures, to 28 days in high risk patients, patients undergoing major gynecological surgery, and patients having major surgery for CA o Hip or knee replacement: Apixaban 2.5 mg BID • The ACCP recommends the use of LMWH, low-dose heparin, or fondaparinux as thromboprophylaxis in the following surgical procedures: moderate-risk major general surgery, higher-risk patients who are having a major procedure for cancer, major vascular surgery, major gynecological surgery, major urological procedures, bariatric surgery, thoracic surgery, and many orthopedic surgeries • LMWH should not be used for thromboprophylaxis in patients with mechanical prosthetic heart valves, especially pregnant women, as prosthetic heart valve thrombosis may occur. Population needed warfarin starting dose adjustment: Older than 75 years • Multiple comorbid conditions • Poor nutrition (low albumin) • Elevated INR when off warfarin • Elevated liver function tests • Changing thyroid status INR target goals o Prevention of DVT, PE, or systemic embolism: 2-3 o Prevention of embolic stoke in patient with AFib: 2-3 o Patients with St. Jude Medical bileaflet PHV: 2-3 o Patients with tilting disk valves and bileaflet PHV ion aortic position: 2.5-3.5 o Patients with CarboMedics bileaflet valve or Medtronic Hall tilting disk PHV: 2-3 o Patients with MHV and high risk (atrial thrombus, AFib, hypercoagulable state, and low EF): 2.5-3.5 o Patients with caged ball or caged disk PHV: 2.5 to 3.5 o Patients with bioprosthetic valve in mitral position: 2-3 o Patients with bioprosthetic vale in aortic position: 2-3 Anticoagulant preferred for patients at high risk for stroke with atrial fibrillation: • High risk for stroke: oral anticoags o ACCP recommends: 150 mg of dabigatran BID rather than warfarin • For patients with paroxysmal AFib at high risk for stroke: warfarin target INR between 2 to 3 o than 80, less than 60 kg, or crt >1.5 dose at 2.5 mg BID Drugs which decrease anticoagulant medication effectiveness: o Heparin: NTG decreases effect of heparin o Warfarin: oral contraceptives, barbiturates, carbamazepine, chlordiazepoxide, cholestyramine, dicloxacillin, griseofulvin, nafcillin, rifampin, flu vaccine, foods high in vitamin K, large amounts of avocado, soy milk, ginseng o Clopidogrel: phenytoin, tolbutamide, tamoxifen, torsemide, Fluvastatin, NSAIDS Chapter 19: Drugs Affecting the Immune System ...........CONTINUED (93 Pages) [Show More]
Last updated: 1 year ago
Preview 1 out of 54 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 10, 2021
Number of pages
54
Written in
Additional information
This document has been written for:
Uploaded
Mar 10, 2021
Downloads
0
Views
32




.png)








.png)
.png)