*NURSING > QUESTIONS & ANSWERS > Nursing > Care of Adults and Older Adults 2020 QUESTIONS (400 QUESTIONS, CORRECT ANSWERS, AND RATION (All)
Nursing > Care of Adults and Older Adults 2020 QUESTIONS (400 QUESTIONS, CORRECT ANSWERS, AND RATIONALE).
Document Content and Description Below
Care of Adults and Older Adults 1. The nursing unit manager on a medical teaching unit says that she would like a nurse to present a case study at interdisciplinary rounds on a patient who has co... mpartment syndrome from a leg injury. This is the first patient you have cared for with this complication, and you have difficulty presenting your ideas in front of a group. What would you do? A. Ask to attend the rounds to increase your understanding of the condition. B. Research the condition and present what you have learned as well as your assessment findings and care measures. C. Suggest that a more experienced nurse be selected to present this case study. D. Approach the unit manager, explain your difficulty presenting in front of interdisciplinary team members, and ask to be excused from presenting. 2. Which of the following situations would indicate a professional boundary violation? A. To empathize with a patient's situation, sharing a personal experience with a patient that is very similar to the situation the patient is experiencing. B. Reminding a patient who has dementia that certain sexual touch behaviours are not acceptable. C. Being concerned about a patient's welfare and seeking ways to protect the client's best interests. D. Having well-intentioned behaviours that detract from achievable health outcomes for patients. 3. An important component of professional practice is self-awareness. Why is self-awareness an important basis for nursing practice? A. It may prevent biases and assumptions from affecting relationships. B. It may allow the nurse to examine how biases and assumptions could interfere with therapeutic effectiveness. C. It may enable the nurse to treat people from different cultural backgrounds according to the dominant beliefs of their culture. D. It allows for mo re objectivity in facilitating the healing process. 4. Which of the following is a theoretical perspective that underlies group process and effectiveness? A. The personality style theory acknowledges that the nature of individuals in a group helps us understand group dynamics and sources of conflict in the group. B. When groups are formed to complete a task, the task functions need to be assigned to individuals to ensure effective group functioning. C. Considering the roles and functions or groups would explain the developmental theory of groups. D. For group effectiveness, a group needs to have homogeneity and common views and interests. 5. Which of the following group principles interfere with the effectiveness of a group? A. Groups get to know each other while focusing on accomplishing tasks. B. Groups set norms, cooperate, and monitor progress. C. Groups encourage similarity of viewpoints and minimize differing opinions. D. Groups deal with conflicts and allow members to express their differences. 6. Janna, age 27 years, a sing le mother, appreciates the help you have given her through the birth of her first child. When you conclude your last follow-up community visit, she expresses gratitude and suggests that you come back and visit her and the baby for regular outings. How would you respond? A. Acknowledge your appreciation of this experience, explain that her nursing needs have been met, and tell her you have to leave to care for other new mot hers. B. Thank her for the offer and tell her that you will have to give her a call to see whether you will be able to work in outings in your personal schedule. C. Tell her this would be unprofessional. D. Stale that you would really like to do this but you are too busy with your other commitments. . 7. How would you respond to Mr. Carlson? A. Remind him that he has signed the consent and that the surgery has been scheduled. B. Discuss his fear s regarding the surgery and reassure him that many patients want to change their minds as the surgery draws near. C. Explore reasons why he wishes to cancel the surgery, clarify his concerns, and reinforce that he can change his mind if he chooses. D. Tell him not to make up his mind until the doctor comes to talk to him again. 8. Mr. Carlson makes the decision to sign himself out of the hospital. What actions would you take? A. Ensure that he signs the release form and contact the doctor and the operating room staff. B. Convince him 10 slay because heart surgery is very important. C. Contact the nursing unit manager and document it in the chart. D. Realistically explain the wail list for surgery and what could happen to him. . 9. You are admitting Darlene, age 40 years, who has come in for regulation of her insulin dependent diabetes. When she is unpacking, you note that she has a bag with some of her used syringes with needles, which she places in the top drawer of her bedside table. What would you do? A. Rein force that she should keep the syringes in her suitcase so there are no injuries to staff members. B. Ask her why she is keeping the used syringes and ensure they are disposed of safely. C. Ask her to glove and dispose of the contaminated syringes in the needle receptacle. D. Report the incident to the diabetic care team so effective teaching can be done. 10. You are supervising a nursing student during a dressing change. When the student is removing the dressing from a leg ulcer, the patient begins to yell and swear at both of you. He threatens to throw the water pitcher if both of you don't leave his room immediately. What should you do? A. Leave the leg ulcer undressed and exit the room immediately. B. Report the incident to the doctor and have him or her explain that this behaviour will not be tolerated. C. Temporarily dress the wound, explain that verbal abuse is not tolerated, leave the room and return later to discuss alternate wound dressing strategies. D. Firmly explain that that behaviour will not be tolerated, remove the water pitcher, and continue applying the dressing 11. You have completed your initial assessment and charting on a patient with chronic obstructive pulmonary disease. When you go back into the room 1 hour later, you note that his Status has changed: He has become confused end does not know where he is; is taking short, rapid breaths at 34 breaths/min; has to sit up to breathe; and has a bluish tinge around his lips. His oxygen saturation levels have gone from 94% to 84%. What would you document for the assessment? A. Confused and disoriented X3, Dyspneic, Pallor of lips. Oxygen saturation dropped from 94% to 84%. B. Confused, Cheyne Stokes breathing at rate of 34/min. Positioned in Fowler's position. Blue lips. C. Disoriented, Tachypneic breathing at 34/min. Short of breath. Oxygen saturation at 84%. D. Disoriented to place, tachypneic, shallow breathing at 34/min, orthopneic with circumoral cyanosis. Oxygen saturation at 84%. 12. Laurana, age 24 years, is being discharged today after the birth of her first baby. She is concerned about how she will manage at home and wonders how she can get her questions answered. What sources of information would you suggest? A. Parents and friends. B. A retired nurse in her neighborhood and web sites. C. Community health clinics, telehealth, and hospital-based web site. D. Pamphlets, library books, husband, parents, and in-laws. 13. What is the most important responsibility when inserting a nasogastric (NG) tube? A. Accurate measurement and lubrication of the NG tube. B. Asking the patient to breathe deeply when the tube is inserted past the nasopharynx. C. Encouraging the patient to swallow sips of water to facilitate the insertion. D. Checking the placement of the tube by aspiration and testing the pH of the contents. Case Study: Mrs. April Hume, age 86 years, has been admitted with advanced liver metastasis after a mastectomy. She is very weak and is experiencing abdominal pain, has ascites, and is having difficulty breathing. She has requested that only supportive measures be given. Questions 14 and 15 14. Which would be priority nursing Interventions? A. Addressing concerns she might have regarding death and dying, encouraging family support, and promoting her independence in meeting her needs. B. Initiating oxygen therapy, Fowler's positioning, pain control, and addressing her Questions and concerns. C. Encouraging her to eat, mobilizing her every 2 hours, and having her perform deep breathing and coughing exercises every half hour. D. Ensuring that she under stands that she is on a palliative care unit and explaining that only comfort measures she requests will be followed. 15. Mrs. Hume is anxious and concerned about her breathing difficulties. She states that she feels that breathing is taking so much energy that she is hardly able to eat. She is having difficulty mobilizing because of the pain and spends most of her time in bed. She says that her family is concerned about her lack of progress. What would you do? A. Explore other ways to more effectively control her symptoms and advocate for her when approaching her family. B. Rein force the meaning of supportive care to her family and restrict their visits so Mrs. Hume has more rest time. C. Provide support for the family and encourage Mrs. Hume to become more actively involved in her care. D. Determine where the patient is regarding the stages of dying and discuss the findings with her family. 16. If a mass casualty occurs near your acute care unit what would be included in a disaster preparedness plan? A. An informal fan out to contact and inform all registered nurses about the disaster and elicit their help in assisting with the casualties. B. A formal written plan of action for coordinating the response of the hospital staff and to designate how different areas will be used. C. A designation of levels of casualty care and having nurses volunteer services at different levels. D. A formal plan to ensure that medical supplies and medications are available for the great number of casualties. 17. Mrs. Jones recently had a cystectomy for bladder cancer. She has an ileal conduit (urostomy). What teaching would you include? A. How to protect the skin, how to apply a dressing over the ostomy site, and the importance of reporting shreds of mucus in the urine as evidence of a urinary tract infection. B. Stoma care and application of an ostomy pouch and drainage bag, increasing intake of fluids, observing amount and the colour of the urine. C. Odour control, skin cleansing, and irrigation of the ostomy. D. Signs of infections or skin breakdown, intermittent application of the appliance, and the importance of dietary restrictions. , 18. Which of the following patients require increased sensory stimulation to prevent sensory deprivation? A. A 24-year-old patient who has been admitted with an anxiety disorder and appears very agitated. B. A 60-year-old patient, who is blind, reads books through use of Braille, listens to the radio, and regularly takes walks around the unit. C. A 65-year-old patient, who has employment-induced presbycusis and advanced glaucoma. D. An 84-year-old patient who has hemiparesis and ambulates with a walker. . 19. Mrs. Starface, age 62 years, a First Nations patient, has been admitted with a chronic cough and progressive weight loss. She has a positive Mantoux test result, and is placed in isolation for suspected tuberculosis. What isolation precautions should the nurse take? A. Have her wear a disposable mask when she is transported to the radiography department. B. Wear a gown and gloves while in her isolation room. C. Wear a disposable mask, gown, and gloves while giving care. D. Discourage visitors from spending time with the patient to reduce transmission. . 20. Mrs. Mames, age 27 years, gravida 1, para 0, is admitted in active labour. She states that her contractions are very intense and that she needs pain medication. What is the most important factor to assess before analgesic administration? A. Her respiratory rate and fetal heart rate during contractions. B. The frequency, duration, and intensity of her contractions. C. The effectiveness of the coaching from her husband. D. How well she manages through the next five contractions. 21. Mrs. Dravies, gravida 2, para 1, is admitted at 8 weeks gestation for a moderate amount of bleeding and abdominal cramps. A day later, the bleeding stops, and she is being discharged. What would you include in discharge teaching? A. Ask her how badly she wants this baby and what she would be willing to do to ensure carrying the baby to term. B. Ask her if she understands the reason for the cramping and bleeding and explain what precautions she could take to retain the pregnancy. C. Explain that nurse aborts the fetus if it is abnormal and that bleeding and cramps may indicate an abnormality. D. Ask her if she has been eating nutritious meals and restricting her activity during pregnancy. 22. Mr. Jones, age 64 years, had a transurethral resection of the prostate yesterday. How could you detect hypovolemic shock in this client? A. Slow, irregular heart rate and pulse deficit. B. Bounding pulse and hypotension. C. Pallor, cold extremities, and tachycardia. D. Dark red-tinged urine, shivering, and confusion. 23. Jennifer, age 16 years, is admitted to the postanesthesia recovery room after wiring of a fractured jaw. She is conscious. Her breathing has become noisy and shallow. Her oxygen saturation levels were at 98 and now are at 90. What actions would you take? A. Position her in Sims position with her head to the side, give oxygen as ordered, and suction if needed. B. Position her in Fowler’s position to assist her in breathing and give oxygen as ordered. C. Insert an airway, suction her, and position her in the supine position. D. Encourage her to breathe deeply, position her in the prone position, and give oxygen as ordered. 24. Daniel, age 16 years, had a cast applied after a fracture of the tibia. When teaching him before discharge about detecting signs of impaired circulation and nervous system functioning, which signs would indicate problems? A. Pallor, coolness, and numbness of the toes. B. Pain at the fracture site and a small amount of bleeding through the cast. C. Inability to move the leg at the fracture site. D. Slight edema of the foot and presence of pedal pulse. 25. Mr. Blair had a bowel resection 2 days ago and has had a nasogastric (NG) tube inserted. He is complaining of increased abdominal pain and nausea. What assessments or actions would be most appropriate? A. Check the patency and amount of drainage from the NG tube. B. Give him an analgesic and antiemetic as ordered. C. Irrigate the NG tube with water and give an analgesic as ordered. D. Explain that nausea is common because the NG tube irritates the gag reflex. 26. Mr. Evans has ascites secondary to cirrhosis of the liver. He is jaundiced and malnourished. Which of the following problems is not associated with cirrhosis of the liver? A. Eupnea related to esophageal varices. B. Potential for pressure ulcers related to malnourishment. C. Concentrated, dark urine related to kidney excretion of bile byproducts. D. Confusion and disorientation related to increase in circulating toxins. 27. Mrs. Chu had a cholecystectomy 2 days ago. Which signs would indicate a wound infection? A. Serosanguineous drainage, temperature of 38 degree C, and abdominal pain. B. Purulent drainage, pain in the mid incision, and temperature of 38.5 degree C. C. Serous drainage, temperature of 38 degree C, and redness of the incision line. D. Sanguinous drainage, temperature of 37.5 degree C, and bradycardia. 28. Dillon is 7 years old and weighs 30 kg. He has acute streptococcal pharyngitis. He is prescribed Keflex (cephalexin) 26.67 mg/kg q6h. How much would he receive in each dose? A. 150 mg. B. 200 mg. C. 400 mg. D. None of the above. 29. Jane, age 18 years, has an asthma attack when in the hospital. She is in respiratory distress. What initial action would you take? A. Position her in the supine position and administer oxygen and bronchodilators as ordered. B. Position her in the Sims position and gave bronchodilators as ordered. C. Position her in Fowler’s position, initiate oxygen, and give bronchodilators as ordered. D. Give bronchodilators and steroid medication as ordered. 30. Mrs. Jones, age 34 years, returns from the recovery room after bowel surgery. She is receiving morphine sulfate through a patient-controlled analgesia (PCA) pump. When you assess her pain levels, her pain intensity is 8 of 10. When you ask her if she has been using the button to relieve her pain, she states, “I’m afraid that I’ll become addicted if I use too much morphine.” Which would be the best response to her concern? A. “Morphine is not addicting in these circumstances.” B. “You need to take the morphine to help you rest and recuperate from the surgery; you can deal with the addiction later.” C. “When morphine is used to alleviate severe pain for 2 to 3 days, there is little likelihood of becoming addicted.” D. “Have you had problems with drug addiction before?” 31. Mr. Keaton, age 65 years, has a plastic anemia and is going to receive a transfusion of packed blood cells. In addition to taking vital signs and verifying that packed blood cells are matched to the patient, what other assessments would you make? A. Assess pain at the transfusion site and transfuse the packed blood cells over 5 hours to lessen reactions. B. Check the patient regarding chills, low back pain, dyspnea, and skin itching during the transfusion. C. Ask the patient about headaches, maintaining bed rest during the transfusion, and reducing intake of fluids to reduce the likelihood of fluid overload. D. Transfuse the blood quickly for the first 15 minutes and then check for abnormal breath sounds and other symptoms. . 32. Mrs. Kilts, age 84 years, has hypostatic pneumonia. When you complete your assessment, which of the following would indicate hypoxia? A. Tachypnea, orthopnea, tachycardia, and circumoral cyanosis. B. Hypotension, bradycardia, braypnea, and use of accessory muscles in the neck. C. Eupnea, hypertension, bradycardia, and cyanosis of the nail beds. D. Occasional productive cough, pursed-lip breathing, and nasal flaring. 33. When you enter the recreation room, you observe Sara Jones, age 20 years, pacing, speaking in a threatening manner, and appearing to defend herself. She has been diagnosed with paranoid schizophrenia. What approach would you take? A. Approach her directly and tell her you are going to get her some medication to help her calm down. B. Ignore her until she calms down and then approach her gently and ask what is wrong. C. Ask her if she is hallucinating and whether she has taken her medication today, D. Approach her calmly and find out what is causing her to be upset. 34. Mr. Pritchard, age 55 years, has been informed by his doctor that his pancreatic cancer is inoperable and that it has spread to his liver. When you enter the room, he states, “The doctor feels that things are hopeless. I hate this place. You're all so useless. Just leave me alone." What would be a therapeutic response? A. "This is devastating news for you. I'll let you have some time and will come back later." B. "You arc much too young to have inoperable cancer. How does your family fee l about this?" C. "You'll need to get over this. Your family needs you to get your affairs in order." D. "Why are you upset with us? You need some time to calm down.” 35. Mr. Corwin, age 74 years, has had an open reduction and internal fixation (ORIF) after a right hip fracture. What are important priorities on the first postoperative day? A. Supporting the leg to maintain adduction, ensuring adequate pain control, and maintaining bed rest. B. Assessing the neurovascular status in the right leg; providing pa in control; and encouraging deep breathing and coughing exercises, position changes, and early ambulation. C. Assessing for skin integrity, enhancing his nutritional status, and restricting his movement and activity in bed. D. Preventing confusion and disorientation, restricting analgesics, and encouraging pursed-lip breathing. 36. Mr. Balm, age 70 years, comes into the emergency department with acute onset of severe chest pain, dyspnea, and anxiety. His respirations are 28 breaths/min, and he has circumoral cyanosis with an oxygen saturation of 84%. What would your immediate actions be? A. Gather information regarding the nature and intensity of the chest pain. B. Place him in Fowler's position, Initiate oxygen therapy, and gel an analgesic ordered. C. Keep him in the supine position, encourage deep breathing, and request an ECG. D. Get an order for an analgesic, position him in the side-lying position, and encourage pursed- lip breathing. 37. During a gymnastics practice, 18-year-old Tracey falls and fractures her right tibia. The doctor asks to be notified if anterior compartment syndrome presents in the right extremity. What signs and symptoms would indicate this syndrome? A. Edema of the right foot, loss of sensation in the right leg, and hypotension. B. Edema of the right foot, redness on the skin surface or the calf, and poor capillary refill in the toenails. C. Severe pain aggravated by plantarflexion, tense and tender muscles in the lateral right calf, and paresthesia. D. Painful contracture of the calf muscles, inability to extend the leg, and redness arid warmth in the calf region. 38. Mr. Harris, age 65 years, had a n abdominal perineal resection for cancer of the rectum. He is receiving morphine via a patient-control analgesia (PCA) pump. What would your priority assessment be regarding the analgesia? A. The rate and depth of respiration. B. The pulse rate and blood pres sure C. The effectiveness of pain control D. The accuracy of the programming on the pump. 39. You are caring for Shauna, an 18- year-old gymnast who has been admitted for investigation of seizures. She weighs 50 kg. For two meals, you observe that she eats a very small amount of salad and skim milk. What approach would you take? A. Tell her you will have a dietician come to assess her eating habits. B. Ask her about her usual eating patterns and reason for her low intake. C. In form the doctor regarding her poor intake and suggest an appetite stimulant. D. Inform her that it she isn't eating foods, a nasogastric feeding tube will have to be inserted. 40. When you complete the initial postoperative assessment for Mr. Violini, age 55 years, you note that his IV is in fusing at 200 cc/hr. You check the order, which reads: "IV of 1000 cc D5S to infuse over 8 hours." What actions would you lake? A. Continue infusing the IV at 200 cc/hr and observe his hydration status. B. Change the rate to 125 cc/hr and observe for fluid overload. C. Reduce the rate to 150 cc/hr and observe for fluid overload. D. Tell him that he should not adjust the flow clamp on the IV. 41. Dana Evans, age 19 years, has been admitted after an asthma attack. When you complete your assessment, you observe that she is anxious, has audible wheezing, and is using her neck muscles when breathing. What would you do? A. Position her in orthopneic position, encourage coughing exercises, and ask her to calm down. B. Position her in Fowler's position, administer oxygen, and give her the ordered pm lorazepam (Ativan) 2 mg. C. Encourage her to lie in a semi-prone position, perform diaphragmatic breathing, and give her the ordered pm beclomethasone dipropionate (Beclovent) inhaler. D. Position her in Fowler's position, administer oxygen as ordered, and give her the ordered pm med salbutamol (ventolin) by inhaler. 42. Mr. Lexus, age 33 years, comes into the emergency department with severe back pain radiating to the left lower groin region. The doctor suspects renal calculi and orders meperidine HCI (Demerol) 100 mg 1M q3-4h pm. One hour after Mr. Lexus receives the medication, he states that the pain is still at 8 of 10. What actions would you take? A. Explain that the medication takes longer than 1 hour to exert its effects. B. Tell him he will have to wait for 2 more hours before he can get his next injection. C. Contact the doctor, explain that the pain is still at 8 of 10, and request a higher dosage. D. Ask Mr. Lexus if he has routinely taken pain killers or street drugs. 43. Which of the following indicates that the nurse is using critical thinking skills? A. The nurse follows the routine of the unit and encourages others to do the same. B. The nurse asks another nurse to outline the steps in performing a wound packing. C. The nurse does not know the answer and checks to find the answer on the unit or in the library. D. The nurse asks the patient about the symptoms she is experiencing an d lists them on the care plan. 44. Which is the most important step in the nursing process? A. The assessment step because it involves collecting, organizing, and validating information that is used for the remaining steps. B. The nursing diagnosis step because it involves identifying the problems. C. The planning steps because it identifies ways to reduce, prevent and resolve problems. D. The implementation step because it ensures that interventions are effective. 45. When identifying the nursing diagnosis or patient problems, which statement is most accurate? A. The nursing diagnosis helps to clarify the medical diagnosis and the problems that result from this diagnosis. B. Critical thinking skills are used to interpret, analyze, and duster the assessment data to determine the problems. C. The nursing diagnosis focuses on ways to prevent, reduce, or resolve the identified problems. D. The identification of patient problems provides the means of measuring the degree to which the goals are met. 46. When performing a psychosocial assessment, which areas should be assessed? A. Breathing patterns, circulation patterns, and metabolic needs. B. Health ha bits, family, and social and sexual pattern). C. General survey, movement, eating habits, and activities of daily living. D. Rest and sleep patterns, activity and exercise patterns, and coping and stress tolerance. 47. What is the primary purpose of conducting a health history? A. Identify the risk factors and how to promote health for the client. B. Obtain information to identify the level of health of the client and his or her past illnesses. C. Examine the chief complaint of the client and related factors. D. Provide for health teaching opportunities. 48. When completing the physical assessment of the abdomen, which is the first skill used in the assessment? A. Palpation. B. Auscultation. C. Percussion. D. Inspection. 49. Which of the following statements heard during shift report identifies an important priority for action? A. A patient is reluctant to ambulate on the evening of surgery. B. A postoperative patient's pulse has been increasing, and his blood pressure is decreasing. C. A postoperative patient is drowsy and slow to respond when the analgesic is at its maximal effect. D. A postoperative patient has not voided for 5 hours alter surgery. 50. Upon completion of teaching related to Lanoxin (digoxin), a client is able to explain the effects of the medication and when not take it and can also identify the radial pulse site. What would this indicate? A. An accurate assessment of her teaching needs. B. An evaluation of psychomotor and cognitive learning. C. A high degree of motivation. D. An independent learner. 51. When teaching a group of middle-aged women, what would you include when discussing primary prevention? A. Prevention of anemia and type 1 diabetes. B. Prevention of ulcers and inflammatory bowel disease. C. Fall prevention and maintaining joint mobility. D. Prevention of osteoporosis and the importance of regular breast self-examinations and regular Pap smears. 52. A community health nurse is planning to address the needs of elderly adults living in their homes. What primary area s should be included in this discussion? A. Importance of exercise, balanced nutrition and hydration, and safety and fall prevention. B. Prevention of joint deterioration and mobility problems. C. Prevention of hearing and visual deficits. D. Importance of frequent doctor visits and access to health care resources. 53. Which of the following legal definitions is true? A. Good Samaritan laws are designed to protect victims in emergency situations. B. Negligence is intentional failure to act responsibly or deliberate omission of a professional act. C. Malpractice is failure to perform professional duties that result in patient injury. D. Scope of practice involves general guidelines that define nursing. 54. A nurse has delegated the taking of vital signs for an unregulated health care provider. When a client's blood pressure is reported as high, the registered nurse rechecks the blood, pressure and other vital signs for the patient. What would these actions be called? A. Obligation to the patient. B. Reversing of delegation. C. Empowerment of the patient. D. Accountability for care. 55. When suctioning a tracheotomy, which actions are correct? A. Insert the suction catheter as far as patient can tolerate and suction for 25 seconds. B. Oxygenate the patient and then suction for 10 to 15 seconds while withdrawing the catheter. C. Suction every 15minutes to prevent secretions, from accumulating. D. Commence suctioning upon insertion of the catheter and continue for 5 seconds while withdrawing the catheter. 56. A patient has been admitted to the emergency department after a car accident. He is sent to the hospital unit after emergency chest tube insertion. What would constitute an emergency situation with the chest tube? A. Bubbling of air in the underwater seal chamber. B. Improper suction setting on the wall suction. C. Disconnection of the connecting tubing from the chest tube. D. Drainage of bloody material into the drainage chamber. 57. A postoperative patient after bowel surgery has orders for DAT (diet as tolerated). What assessments would indicate return of peristalsis? A. Distended abdomen and tympany on percussion. B. Soft abdomen and absence of bowel sounds on auscultation. C. Intermittent cramping, abdominal pain and bowel sounds in all four quadrants. D. Nausea, vomiting, and pain on palpation. 58. A patient has a patient-controlled analgesia (PCA) pump with morphine after a bowel resection. What are the nursing responsibilities after the client has self-administered a bolus of medication? A. Have the client mobilize to reduce the harmful effects of morphine. B. Ensure that the client understands that a bolus may take up to 15 minute to alleviate the pain. C. Encourage deep breathing and coughing exercises to lessen respiratory depression. D. Reduce the amount of IV pain medication being administered on a regular basis. 59. Your assigned patient has been requesting a stronger pain medication. In response, the doctor has ordered morphine combined with a nonsteroidal anti-inflammatory drug (NSAID) for pain relief. How would you explain the effectiveness of these two medications? A. Combining these two drugs will increase pain relief without the increased side effects of increasing the morphine dose. B. The two drugs are antagonistic, so they will relieve the pain but will counteract the side effects. C. Combining the two drugs will lessen the incidence of addiction. D. The NSAID will relieve muscle pain; the morphine will act centrally on the central nervous system to relieve pain. 60. In addition to the pain medication, what other measures help promote comfort and alleviate pain? A. Encouraging ambulation and vigorous rubbing of the inflamed tissues. B. Gentle massage of the area, warm and cold applications, guided imagery, and TENS. C. Prolonged heat applications followed by prolonged cold application to the area D. Encouraging tensing of muscles and performing distraction exercises. 61. Which of the following would be indicators of severe hypoxia? A. Generalized pallor and eupnea. B. Circumoral cyanosis and Pa02 of 70 mm Hg. C. Low oxygen saturation levels of 95%. D. Increased anxiety and drowsiness. 62. What nursing measures are important when a Foley retention catheter has been inserted? A. The Foley catheter should be left unsecured to prevent urethral irritation. B. Urine samples should be obtained by disconnecting the catheter from the drainage bag. C. The patient should limit fluid intake to keep the catheter patent. D. Reflux of urine from the tubing to the bladder should be prevented. 63. You read through your assigned patient's chart. The history states: "Paroxysmal nocturnal dyspnea; reduced CSWM in left leg." What do these medical history terms and abbreviations indicate.'? A. The patient is experiencing intermittent shortness of breath, is unable to breathe unless in a supine position, and has impaired venous return in the left leg. B. The patient is experiencing painful breathing and shortness of breath with exertion and has impaired arterial flow to the left leg. C. The patient is experiencing periods of severe shortness of breath at night and impaired circulation and sensory and motor functioning in the left leg. D. The patient has reduced breathing capacity, loss of breathing reserve, and impaired motor movement of the left leg. 64. Which sexuality alterations might emerge after a myocardial infarction (MI)? A. The patient may be concerned that a heart attack may occur during orgasm. B. Emotional concerns may interfere with the phase of resolution. C. The arousal phase may he affected by personal concerns. D. Sexual dysfunction may present because of reduced ventricular contractions. 65. Which of the following signs and symptoms would indicate impaired arterial circulation in the lower extremities? A. Capillary refill in the toenails with in 2 seconds. B. Absence of dorsalis pedis pulse; coolness and decreased sensation in the feet. C. Edema and coolness in the ankles and feet. D. Redness, inflammation, and sharp pain with calf muscle con traction. 66. Which of the following isolation precautions would be relevant for the communicable illness identified? A. Airborne precautions are indicated for varicella (chickenpox) and involve wearing a mask when in the room. B. Gloves, a mask, and a gown are worn when changing a wound dressing infected with Staphylococcus spp. C. If a patient is infected with VRE (vancomycin-resistant Enterococcus), vital signs equipment is brought into the room every time it is needed. D. Specimens obtained from a contaminated wound would be transferred directly to the laboratory without special precautions. 67. You are developing a care plan for a patient with tuberculosis. What isolation precautions would you take? A. Use a special mask to prevent inhaling infected airborne droplets. B. Wear a mask, gown, and gloves when providing care. C. Wear c, gown and gloves when in contact with the patient. D. Prevent visitors from visiting to reduce the possibility of transmission. 68. You arc assessing a patient who has been in a car accident. He complains about sore ribs and painful breathing on the left side of his chest cage. What assessment findings would alert you to a pneumothorax? A. Pain on exhalation; fatigue. B. Dyspnea; decreased breath sounds on the affected side. C. Bradycardia and hypertension. D. Tachypnea and hyperventilation. 69. A patient has been diagnosed with deep vein thrombosis (DVT). Suddenly, the patient develops chest pain and severe dyspnea. He looks anxious and is very apprehensive. What actions would you take? A. Position him in Fowler's position, initiate oxygen, and call the physician. B. Auscultate for abnormal breath sounds and encourage deep breathing. C. Encourage pursed- lip breathing and coughing exercises. D. Ambulate the patient, encourage deep breaths, and take the apical pulse. 70. Your patient has a cerebrovascular accident (CVA). Which of the following neurologic deficits may present after a CVA? A. Visual field deficits such as homonymous hemianopsia. B. Emotional changes such as lack of emotional response and enhanced coping. C. Motor deficits such as paresthesia with numbness and tingling. D. Verbal deficits such as dysphagia and memory loss. 71. Which of the following assessment findings are associated with cholelithiasis? A. Associated risk factors include being male and athletic. B. Jaundice is seen if the calculus lodges in the common bile duct. C. Biliary colic attacks occur when there is stone formation in the gallbladder. D. Symptoms of pain include steady LUQ pain radiating to the left scapula. 72. Which of the following assessment findings are seen in patients with cancer of the head of the pancreas? A. Early onset of pain. B. Anorexia, nausea, and vomiting. C. Early onset of jaundice and pruritus. D. Presence of steatorrhea, melena stools, and dilute urine. 73. A client presents with cirrhosis of the liver secondary to alcohol abuse. What assessment findings would indicate portal hypertension? A. Ascites and hematemesis. B. Pulmonary edema. C. Absence of jugular vein distension. D. Cramps and watery diarrhea. 74. Alter a total hip arthroplasty, what are the most important precautions to prevent dislocation? A. Limit movement s resulting in internal rotation and adduction of the affected hip. B. Use a pillow under the knees to prevent hip flexion. C. Reduce extension and hyperextension of the affected hip. D. Use toile t seats to prevent circumduction of the hip joint. 75. Without hand washing between activities, a nurse makes an occupied bed and then assists another patient with meal preparation. Considering the chain of infection, which statement is true? A. The new portal of entry of microorganisms could be through the mouth. B. The mode of transmission is through direct contact. C. Microorganisms from the bed making would be spread by direct contact. D. An epidemic infect ion would occur if pathogens from the health care agency caused an illness. 76. What are characteristics of effective decision making strategies in a nurse? A. Reviewing the chart and duplicating the actions of previous nurses. B. Gathering assessment data and analyzing and identifying-priority problems. C. Independently developing a plan of care based on the nurse's workload. D. Willingness to follow the doctor's orders and directions without questioning his or her rationale. 77. What are important considerations when assessing and caring for a patient with pyrexia? A. The patient usually experiences a decrease in vital signs. B. The patient usually exhibits flushing of the skin and jaundice. C. The patient may experience dehydration and convulsions from a high temperature. D. The patient may experience increased urine output and dilute urine. 78. Which of the following statements is true regarding wound healing when an infection is present? A. The infected portion of the wound will likely heal by primary intention. B. The inflammatory phase of healing will be shortened. C. The proliferative or regeneration phase will be delayed and prolonged. D. There will be less for mat ion of granulation tissue because of the infection, 79. Which of the following assessment factors would indicate a need for oral pharyngeal suctioning? A. Thin sputum and a weak cough. B. Breathing rate of 36 breaths/min; noisy, gurgling respirations. C. Auscultation of fluid (rales and rhonchi) in the lower lobes of the lungs. D. Oxygen saturation levels of 95%; use of diaphragmatic breathing. 80. Which of the following is an important consideration when performing oral-pharyngeal suctioning? A. Oxygen provided before suctioning limits the effectiveness of the suction. B. The nurse should only suction when the patient agrees to the procedure. C. Fluid intake should be limited to reduce the secretions produced. D. The duration of each suctioning episode should be IO to 15 seconds. 81. What important postoperative care measures related to care of chest tubes should be done the day after a lobectomy? A. Disconnect the tubing to empty and measure drainage at the end of each shift. B. Frequently check the dressing and chest tube for drainage. C. Ensure that all connections arc securely taped. D. Position the patient in the prone or supine position to permit optimal drainage. 82. Nutrients are important for wound healing. Which of the following is true regarding the role of specific nutrients in healing? A. Vitamin C is needed for building capillaries and fibroblasts in the inflammatory phase. B. Essential amino acids art' needed to ensure building blocks are present for building or proliferative phase. C. Nonessential fatty acids to provide a good supply of glucose for energy. D. Vitamin K is needed for the convalescent phase to help restore energy and nutrient needs. 83. Mr. John G. has a history of cramps and has been experiencing diarrhea for the past 2 days. His urine is concentrated. You would assess for: A. Dehydration by checking tissue turgor and checking mucous membranes. B. Impaction as a result of the surgery. C. Signs of kidney suppression because of the concentrated urine. D. Absence of bowel sounds in the abdomen. 84. What assessment findings would indicate circulatory overload from too rapid an IV in fusion? A. Decreased pulse, decreased blood pressure, and jugular vein distension. B. Increased pulse, increased respirations, and jugular vein distension. C. Headache, paleness, and hypertension. D. Increased temperature, peripheral edema, and decreased pulse rate. 85. Which is the priority system to assess when a patient has severe hypothyroidism? A. Respiratory system. B. Heart and circulation. C. Neuro logic system. D. Integumentary system. 86. A patient with diabetes is being tested for glvcosylated hemoglobin. How would you explain the reason for this diagnostic test? A. It determines the fasting blood glucose level. B. It determines the average blood glucose level in the previous; months. C. It determines the ratio of glucose to hemoglobin. D. It is used to identify a reduction in hemoglobin because of high glucose levels. Case Study: Mr. Evan Jenkins, age 65 years, has had type 2 diabetes for 20 years and has been admitted to the hospital with chronic renal failure. Questions 87 to 90 87. When completing the initial assessment, which signs would indicate circulatory overload? A. Increased blood pressure, apprehension, and shock. B. Weigh t gain, coughing of frothy sputum, and jugular vein distension. C. Cool, dry skin; gastric distension; and pleural edema. D. Apprehension, poor tissue turgor, and bradycardia. 88. Which of the following statements is true regarding end-stage renal failure? A. A common cause of renal failure is pyelonephritis. B. It results in an increase in erythropoietin, leading to chronic fatigue. C. It results in a decrease in creatinine and blood urea nitrogen. D. It is characterized by fluid volume excess, hypernatremia, and hyperkalemia. 89. What are important nursing care measures for a patient with chronic renal failure? A. Prepare the client for temporary peritoneal dialysis or hemodialvsis. B. Restrict sodium and potassium; restrict fluids as ordered. C. Provide a diet high in protein; restrict fluids as ordered. D. Monitor for hypotension and maintain accurate intake and output records. 90. Mr. Jenkins makes this comment just before his hemodialysis treatment: "What have I got to live for? I'd just like this to be over.” How would you interpret these comments? A. This indicates feelings of depression associated with a long –term, incurable disease. B. This response will be temporary, and he will feel much better after his hemodialysis is initiated. C. His family is no t providing the support he needs at this time. D. This is an unusual response and indicates that his cognitive abilities have become impaired by the disease. 91. A client has just been transferred to the postanesthesia recovery room. What are the most important initial assessments that need to be completed? A. Skin color, warmth of extremities, and mental status assessment. B. Temperature, metabolic rate, and presence of reflexes. C. Vital signs, level of consciousness, pain level and wound dressing. D. Emotional stat us, response to anaesthesia, and social support. 92. Which factors increase the risk of postoperative complications? A. Hypotension and athletic bradycardia. B. Hypertension and obesity, chronic lung condition. C. Poor gag reflex and optimal nutritional star D. High hemoglobin and negative midstream urine analysis. Case Study: Mrs. Jane Everly, age 65 years, had a left cerebrovascular accident (CVA) with right-sided hemiplegia. She is confused and disoriented and has a nasogastric (NG) feeding tube inserted. Questions 93 to 98 93. Which is the most import ant consideration before administering tube feedings through an NG tube? A. Ensure that the anchoring tape is intact. B. Determine placement of the tube by aspiration of gastric contents. C. Position the patient in the supine position to prevent aspiration. D. Flush out the tube with 50 cc of water before the feeding to prevent obstruction of the tube. 94. Mrs. Everly's family is upset that this CVA has happened to her at such a young age. They ask you what she should be doing differently and what they should do to prevent having a CVA. What risk factors are associated with the incidence of CVA? A. Genetics plays the most important role in its incidence. B. Lack of exercise and effective stress management. C. Smoking, high cholesterol levels, and hypertension. D. Low weight, dehydration, and aerobic exercise. 95. Mrs. Everly is prescribed warfarin sodium (Coumadin) 8.5 mg after her prothrombin time and INR (International Normalized Ratio) laboratory report were reviewed. She has warfarin tablets of the following strengths: 5 mg/tab, 3 mg/tab, and 2 mg/tab. Which of the following would you give? A. 1 tablet of 5 mg, 1 tablet of 3 mg, and ½ tablet of 2 mg. B. 1/2 tablet of 5 mg, 1 tablet of 3 mg, and 1 tablet of 2 mg. C. 1 tablet of 5 mg and 1/2 tablet of 5 mg. D. 1 tablet of 5 mg, I tablet of 2 mg, and ½ tablet of 3 mg. 96. Mrs. Everly undergoes intense rehabilitation and is discharged with residual hemiparesis. As the home care coordinator, what would be important for you to do before Mrs. Everly's return home? A. Reduce risk factors and implement measures to prevent a subsequent CVA. B. Identify complications of immobility and reinforce measures to prevent them. C. Reduce nutritional intake and fluid intake to promote weight loss. D. Assess the home and demonstrate effective use of assistive devices. 97. What are important factors to consider in helping her integrate back into the community? A. Financial resources, ability to afford home care nursing. B. Independence, adjustment to moving back home, sleeping patterns. C. Coping abilities, emotional lability, physical deficits, family supports. D. Redefining her community involvement, daily checks of blood pressure. 98. What community resources could help her and her family learn more about stroke and rehabilitation? A. Heart and Stroke Foundation and Canadian Stroke Network. B. Internet resources and products to help stroke patients. C. Community drop-in center for retired persons and community health center. D. Hospital outpatient department and mediclinic. Case Study: Jeffrey Brim, age 18 years, has been admitted unconscious to the neurosurgical unit after a car accident that resulted in a head injury. He was not wearing a seatbelt. Questions 99 to 103 99. When caring for an unconscious patient, which is the most important nursing measure? A. Maintaining a patent airway. B. Maintaining integrity of the skin and mucous membranes. C. Maintaining fluid and nutritional balance. D. Preventing urinary incontinence. 100. You are asked to complete a neurologic assessment. Which of the following would indicate an abnormal neurologic finding? A. The client is conscious and responds to verbal commands. B. Temperature, 37, pulse, 86 bpm and blood pressure, 120/80 mm Hg. C. The pupils are equal and sluggish in reaction to light. D. The patient has equal strength in hand grasps and foot pushes. 101. What change in vital signs would indicate increased intracranial pressure? A. Hypotension and tachycardia. B. Increase in temperature and tachypnea. C. Increasing systolic blood pressure. D. Widening pulse pressure and bradycardia. 102. The doctor has indicated a poor prognosis for recovery, and the client's family is very concerned. How would you support the family? A. Listen to them, explain what is happening, and encourage them to be involved in their family member's care. B. Encourage them to have realistic expectations of recovery and reinforce the poor prognosis. C. Identify the strongest family member and communicate with that person. D. Explain the parents never get over the horrors of such massive injuries. 103. Jeffrey's teachers have asked for a nurse to speak regarding prevention of injuries caused by car accidents. Considering the age group and injury risks, what would you address? A. Allow open discussion of what went wrong with this accident. B. Discuss the downfalls of inexperienced drivers and the omnipotence that young drivers feel. C. Discuss the purpose of seatbelts, the effects of drinking and driving, and the effects of speed. D. Explain how accidents can be prevented and discuss the high cost of injuries in this age group, 104. Mrs. Ava J., age 58 years, has had a bone density test indicating osteoporosis. What risk factors would predispose a person to osteoporosis? A. Excessive sunlight exposure and increased calcium intake. B. Increased weight -bearing activities. C. Heavy smoking, sedentary lifestyle, and diet low in calcium. D. Diet deficient in vegetables and fruits; increased alcohol intake. 105. Persons in a retirement residence a re asking for assistance in preventing falls and reducing injuries. What would you omit from the discussion? A. Explanation of the importance of a health professional evaluating gait and assessing for motor deficits. B. Discussion of instability and effective use of ambulatory aids. C. Teaching about stabilizing by sitting for a few minutes before standing to lessen dizziness. D. Talk about decreasing activity and the regular use of restraints to prevent falls, 106. Which statement is true regarding informed consent before a surgical procedure? A. Consent must be signed after explanations of the benefits and risks of the procedure. B. The nurse is responsible for giving the explanations and providing information regarding the risks. C. The patient cannot decide not to have the surgery after the consent has been signed. D. Informed consents are documents of understanding, not legal documents. 107. A patient comes into the preoperative clinic and states that she has decreased her nutritional intake and has lost 15 kg in the past 2 months. Which of the following statements is true regarding wound healing when poor nutritional status is present? A. The wound is likely to become infected and will then heal by primary intention. B. The inflammatory phase of healing will be shortened. C. The proliferative or regeneration phase will be prolonged. D. There will be less formation of scar tissue because of the client's nutritional state. 108. John Smith has been diagnosed with lung cancer. He approaches you about his diagnosis and states, "I can hardly face my family. They have been after me to quit smoking for so long, but I never really believed this would happen to me.” What elements of family-centered care would be important? A. Assessing his guilt and identifying how each member is affected by his diagnosis. B. Assuring family members that this is not the time to be judging but to be supporting him in his recovery. C. Encouraging him to stop smoking and apologize to his family. D. Developing a sense of trust, discussing feelings, and identifying the family's strengths and coping strategies. 109. Mary Lane, age 72, is admitted to the hospital with a GI disorder. Which disorder would' contraindicate abdominal palpation? A. Aortic aneurysm B. Bowel obstruction C. Cirrhosis D. Umbilical hernia Case Study: As a nurse, you are taking care of Mr. Jackson, age 56 years, who has been admitted with a myocardial infarction. Questions 110 to 113 110. You observe that Mr. Jackson is very sad and dejected. He states, "Life will never be the same.” How would you respond to him? A. "This makes you really sad." B. “Why do you think life will never be the same?" C. "Could you be a little more hopeful of your recovery from this heart attack?" D. "You're concerned when you think about how this will change your life?" 111. What questions would you ask to determine his coping abilities? A. "What could you have done to prevent this illness? B. "How is this illness impacting you and your family?" C. "How ca n we take away your worries while you are in hospital?" D. "What a re the worst challenges that you have laced?" 112. Mr. Jackson has been taking a diuretic, furosemide (Lasix). His serum potassium level is 3.2 mmol/L. Which assessment findings would confirm hypokalemia? A. Muscle weakness and a weak, irregular pulse. B. Diarrhea and cramps. C. Tetany and tremors. D. Headaches and poor tissue turgor. 113. When Mr. Jackson goes home, he enters a community heart rehabilitation program. What lifestyle changes will be reviewed? A. Reduced Intake of unsaturated fats, anaerobic activity, increase fluids. B. Reduced intake of calcium, increased intake of sodium, rest periods. C. Reduced cholesterol levels, progressive activity levels, coping strategies. D. Increasing homocysteine levels, reducing weight, sedentary lifestyle. 114. Upon inspecting a client's abdomen, the nurse notes a, distinct rhythmic pulsation in the midline. Although this pulsation may be normal in a thin client, the nurse should: A. Call the physician immediately, as this finding usually indicates abdominal aneurysm. B. Palpate the area to determine the extent of the pulsation, then call the physician with this information. C. Auscultate the area to determine whether a bruit is present. D. Percuss the area to determine whether the bowel is displaced. 115. When practicing according to ethical principles, what is the principle of beneficence? A. It consists of the patient's having freedom to make decisions and take appropriate action. B. It uses the principle of loyalty to ethical beliefs as a guideline for behaviour. C. It means ensuring that nursing virtues serve as the basis of practice. D. It is to act in the best interests of others; to become a client advocate. Case Study: Mr. Jules Hilt, age 22 years, has been injured in a snowmobile occident. He suffered a neck injury when he was thrown from the snowmobile, Questions 716 to 118 116. When completing your assessment. What findings would indicate an incomplete spinal cord injury (SCI)? A. Immediate flaccid paralysis that persists for months. B. Evidence of voluntary motor and sensory function below the level of injury. C. Presence of spinal shock response with hypertension and tachycardia. D. Presence of paralytic ileus and urinary retention. 117. What emergency interventions would need to be implemented if the injury is at C4 level? A. Measures to reverse-hypertension. B. Mechanical ventilation. C. Measures to control hyperthermia. D. Use of a catheter to intervene in urinary retention. 118. Corticosteroids (methylprednisolone) are given IV within 8 hours of the injury. Why would methylprednisolone be administered? A. To reverse spinal shock. B. To reduce damage and improve functional recovery. C. To assist the body in maintaining the stress response. D. To reduce spinal cord edema. 119. Which of the following are important considerations when providing culturally competent care in a community clinic? A. Knowing about different cultural practices and generalizing when caring for clients from that culture. B. Asking about cultural beliefs related to health, illness, treatments, and dietary practices C. Making decisions for the client and in forming him or her about appropriate health interventions. D. Explaining that multiculturalism in Canada means all cultures melting to join the dominant culture. 120. When you enter a female client's room, you find her passionately kissing and embracing another woman. What action would you take? A. Quietly leave the room, come back later, and state that this behaviour is unacceptable in the hospital. B. Announce your presence by excusing yourself and proceed to conduct the health history. C. Do not disturb the couple, leave the room, and allow them privacy. D. Explain that intimate encounters are better facilitated in the privacy of their home. Case Study: You are a health nurse in an elderly seniors' residence. Your role is to individualize health teaching and assessment and focus on risk identification and injury prevention. Questions 121 to 125 121. What methods would you use to identify the clients' educational needs? A. Have the families meet together as a group to identify primary needs of each senior. B. Conduct focus group interviews and have the clients fill out a survey. C. Develop a list of the seniors' common interests and have them select their preferred choices. D. Discuss with attendants what the primary interests of the clients are. 122. Safe medication administration is an issue, what factors influence medication effectiveness for elderly adults? A. There is a lower risk of drug interactions. B. There is usually less need for medications. C. There is an increase in lipid solubility and distribution throughout the body. D. There is less efficient absorption, detoxification, and elimination. 123. Several clients are concerned that they are taking too many medications and arc unsure of the reasons for taking some of the medications. What would you do? A. Review all the medications and their actions and side effects with each client. B. Have a pharmacist discuss the medications and interactions and initiate physician referrals as needed. C. Give a general presentation on common groupings of medications and indications. D. Ask each client to research the medications prescribed an d identify the reasons they were prescribed. 124. A health assessment of visual alterations is scheduled. Which of the following is true regarding visual alterations or deficits in seniors? A. Cataracts are seen individuals older than age 65 years and occur when the cornea becomes opaque and impairs the visual field. B. Glaucoma is a painless blockage in the circulation of the vitreous humour in the eye, leading to increased intraocular pressure. C. Diabetic retinopathy is the leading cause of blindness an d occurs because of ischemic retinal blood vessel changes. D. Macular degeneration occurs when there is blurring and distortion of visual images caused by destruction of peripheral visual fields. 125. Some of the clients are not participating in activities and appear to be becoming more reserved and isolated, as reported by their families and other residents. What would be you r approach? A. Respect each client's choke of not participating in activities and leave the clients, alone. B. Encourage family members to visit as often as they are able to provide socialization. C. Assess for depression and signs of sensory deprivation; take action as needed. D. Explain to the clients that participation is mandatory and that it is for their health and benefit. 126. Nurse Hanes has completed discharge teaching of a dressing change to a patient. The next day, Nurse Pane observes that the client seems confused about the dressing and reminds Nurse Hanes about a video on dressing technique. In demonstrating that she is open to feedback about her own practice, what would Nurse Hanes' response be? A. "He really didn't seem motivated to learn, so I'm not sure that would help.” B. “I actually don't think that videos are very useful for patient teaching." C. "My client did seem to have difficulty; maybe the video would help.” D. “I wonder if you would reteach him; you have so much more experience.” 127. Two registered nurses arc working nights with a senior student nurse and an unregulated health care worker (UHCW). While one RN is on break, a client requests his pain medication. The nurse knows he will have to waste 0.5 ml, of Demerol to administer the ordered dosage. Which of the following actions would be indicated? A. Draw up the medication and discard the wastage. The amount of wastage is toe small to need to be recorded. B. Draw up the medication; lock up the wastage in the medication cabinet until the other RN returns and can witness and cosign the wastage. C. Call the student nurse to witness the" wastage and cosign for Its proper disposal. D. Ask the UHCW to witness the wastage and confirm to the other RN that the medication was disposed of appropriately, 128. Sanchea Jones notices the smell of marijuana on a colleague upon return from lunch break. Shortly after, Sanchea notices that the colleague is having difficulty drawing up a dose of insulin; she appears uncoordinated and is unaware that she has contaminated the needle several times. What is the best action for Sanchea to take? A. Take the syringe and insulin vials from her and draw up the insulin for her. Instruct her to be very careful when she is giving the injection. B. Take the insulin vials and needle from her draw up the insulin and administer lt for her. Ask a colleague to help keep an eye on her for the rest of the shift. C. Reassign her responsibilities and inform her she will have to report her if it happens again. D. Stop her from drawing up the insulin. Call a Supervisor, inform him or her about the incident, and document the observations. Case Study: Tara Fisher, age 43 years, has had symptoms of systemic lupus erythematosus (SLE) for years, but she was just recently diagnosed with the condition. She has been taking corticosteroids for the past 1.5 years. Questions 129 to 133 129. What are some of the effects of corticosteroids when they have been administered for a long period of time? A. Hypoglycemia and cognitive changes. B. Skeletal muscle a trophy an d osteoporosis. C. Hyponatremia and hypokalemia, D. Edema and hyperpigmentation of the skin. 130. When teaching Tara regarding the long-term effects of corticosteroids, how would you explain the importance of not suddenly discontinuing this medication? A. Long-term use of these hormones has resulted in depression of your body's own production, and a crisis could occur if you suddenly stop taking them. B. Corticosteroids assist in the responding to stress by stimulating your stress hormones, epinephrine and norepinephrine. C. Corticosteroid administration causes Cushing's syndrome, and sudden stoppage results in more serious aggravation of this syndrome. D. The feedback mechanism results in extra stimulation of the pituitary gland to increase production of the corticosteroids. 131. Tara is very dejected that she needs to continue taking the corticosteroids to control her symptoms of SLE. When you come in to administer her medication, she refuses to take it, stating. "This is turning me into an old woman before my time.” How would you respond? A. Explain that the symptoms of the disease are chronic and progressive and are much worse than the side effects from the- drugs, B. Ask her about the medication side effects and explain why suddenly stopping the drug can cause problems. C. Encourage her to take the medication until she is able to consult with her doctor regarding the side effects. D. Document her refusal to lake the medication and notify the doctor. 132. Tara states that she is not sure how she can handle the long-term effects of this disease and that her multiple hospitalizations arc really affecting the family and her role in the family. How would you respond to her? A. "Have you discussed with your family ways they could take the burden off you at this time?" B. "Who in your family is the strongest an d could manage to take over your role in addition to theirs?" C. "This illness has really taken its toll on you and you r family. Which effects are most difficult to handle?” D. "Which roles arc you not able to handle? Maybe, we could consult with a social worker regarding these." 133. Tara tells you she feels -so alone with this illness" and asks you what resources may be available to assist her. What community resources might you suggest? A. Chronic illness support group or SLE support group. B. Internet resources and chat lines. C. Medical library to find out more about the illness. D. Nursing text s to help her better understand this condition. Case Study: Jeremy Brook, a 29-year-Old bisexual male, comes to the sexual health clinic. He has symptoms of night sweats, fatigue, and weight loss. His temperature is 39°C. He has a history of syphilis and hepatitis B and is being investigated for HIV infection. He has a chronic lung infection and is being investigated for digestive problems. Questions 134 to 138 134. Which of the following groups have an increased risk of contracting HIV? A. Having a recent blood transfusion; being a heterosexual monogamous woman or man. B. Participating in unprotected sex with multiple sexual partners; sharing IV needles. C. Health care workers working in emergency settings, bisexuals, and hemophiliacs. D. Individuals from dev eloping countries, oral drug abusers. and alcoholics with nutritional deficiencies. 135. What is the primary risk factor for health care workers contracting HIV when providing patient care for Jeremy? A. Needlestick injuries or contact with the client's blood. B. Contact with saliva or urine drainage. C. Droplet transmission from coughing and sneezing. D. Accidental injury. 136. When the results of the tests come back confirming Jeremy is HIV positive, he asks about the significance of this diagnosis. What opportunistic infections or cancers tend to develop with AIDS? A. Hepatitis B, chicken pox, measles, and leukemia. B. Pneumocystis carinii pneumonia. Kaposi's sarcoma, and herpes simplex. C. Uterine sarcoma, Melanoma, and S. coli infection. D. Prostate cancer, lung cancer, urinary tract infections, and prostatitis. 137. Jeremy is started on antiviral medications. In addition to teaching regarding medications, what should the nurse include to reinforce health and prevent illness for Jeremy? A. Prevention of transmission, isolation precautions. and avoidance of infection. B. Medications and side effects; nutritional supplementation. C. Prevention of transmission, optimal nutrition, and exercise. D. Safe sex practices, choices of medications, and hospice care. 138. Jeremy states: "why did this ever have to happen to me? I can't even bring myself to tell my family.” What would this indicate? A. Denial of the disease. B. Guilt and remorse regarding the disease. C. Realization of the seriousness of the disease. D. Anger over contracting the disease. 139. When students in a health class are discussing birth control and safer sex, which would indicate that teaching, was effective? A. A student indicates that safe sex means preventing pregnancy through use of birth control. B. A student states that the rhythm method means not having sex just before menstruation. C. A student indicates that responsible sex involves using condoms for protection and birth control. D. A student states that the intrauterine device is the most effective way to prevent pregnancy. 140. Three college students in the class have indicated that they have never gone to the doctor to have a Pap test done even though they have been sexually active for several years. You have read a research article regarding factors that increase cancer of the cervix. What would be important information to reinforce? A. Teens can he vulnerable to developing cancer of the cervix if they are exposed to certain strains of human papilloma virus (HPV). B. Uterine cancer is more common in sexually active teens. C. Breast cancer is more common in sexually active teens. D. Teens having unprotected sex are more vulnerable to ectopic pregnancies, which can be identified with a Pap test. 141. Some female college students discuss that they have encountered situations that almost culminated in date rape. When considering preventive precautions, which statement is false? A. Alcohol is usually involved in date rape. B. Date rape drugs, such as ketamine, are not detectable in a drink. C. If rape occurs; the victim should not douche or wash and should go to the police station. D. Date rape is usually a misinterpretation of responsive cues. 142. In another college health class, the topic of risk taking Behaviours, or “living dangerously," is being discussed. What topic would not be included? A. Effects of cigarette smoking. B. Responsible drinking patterns. C. Motor vehicle accidents. D. Aerobic exercise. Case Study: James Edwards, age 42 years, is admitted with steam bums to his face, neck, and chest region. Questions 743 to ' 48 143. During the initial assessment, it is important to include the rule of nines to estimate the ex tent of the burn and to assess its depth. In addition, what would be the most important assessment priority? A. Assessing tolerance of the pain. B. Checking for airway patency. C. Observing for facial swelling and disfiguration. D. Determining oxygen saturation levels. 144. James Is assessed and has fluid replacement ordered. What important assessment data will help ensure accurate replacement? A. Vital signs and presence of edema. B. Age, Weight, vital signs, and tissue turgor. C. Urine output, mucous membrane hydration, and orientation. D. Capillary refill, specific gravity of urine, and blood pressure readings. 145. Which replacement fluid is most likely to be used during the initial 24 hours after a burn? A. Ringer's lactate is used as long as the urine output is maintained at an adequate level. B. Packed blood cells are used to replace the red blood cells that have been lost. C. Dextrose with water arc used to dehydrate the patient. D. Albumin is used to restore plasma proteins. 146. Fluid therapy has been ordered at 1500 eel8 hr. The drip administration set is to gtt/ml. How fast will the IV run (drops/ minute)? A. 19 gtt/min. B. 31gtt /min. C. 26 gtt/min. D. 36 gtt/min. 147. When you assess the IV at the beginning of the shift it is 0.5 hour behind. Your assessment indicates that it is safe to catch up the IV to the ordered rate. and you decide to do this in the next 2 hours. What is the adjusted rate per hour for the next 2 hours? A. 150 cc/hr. B. 234 cc/hr. C. 281 cc/hr. D. 225 cc/hr. 148. The nurse notices that in the recuperation phase. James has become very quiet and withdrawn. What concerns should the nurse explore? A. Concerns regarding dependence and unwillingness to be discharged. B. Body image and self-esteem concerns. C. Concern s regarding coping abilities and family response. D. Financial concerns. Case Study: Dawn Mar, age 36 years, has been diagnosed with myasthenia gravis. Her history indicates progressive myopathy, dysphagia, diplopia, and dysarthria. Questions 149 to154 149. Assessments con firming Dawn's history would include: A. Atrophy of the muscles, difficulty chewing, Strabismus, and difficulty moving. B. Muscle inflammation, choking when eating, nearsightedness, and painful joints. C. Muscle weakness, difficulty swallowing, double vision, and difficult y speaking. D. Muscle pain, difficult y speaking, headaches, and arthritic changes. 150. Dawn asks you, "What is this disease? I have never even heard about it before." How would you respond? A. “It is a debilitating disease in which patches of nerves lose their myelin sheath, which Interferes with nerve transmission to the muscles." B. “It is a chronic disease in which there is a disturbance in nerve transmission to the muscle, resulting in fatigue and muscle weakness." C. “It is an inherited disorder in which there is progressive destruct ion of the basal ganglia in the cerebral cortex." D. "It is a progressive degenerative process involving spinal and lower motor neurons with spastic changes in cranial and spinal nerves ," 151. Diagnosis of myasthenia gravis is confirmed by evaluating the patient's response to an IV injection of the cholinesterase inhibitor edrophonium (Tensilon). If the patient responds positively, what would the nurse expect? A. Exaggeration of the symptoms. B. A rapid and dramatic increase in muscle strength. C. A slight increase in muscle strength followed by exaggerated muscle fatigue. D. Partial relief of muscle weakness. 152. What assessment findings would indicate an emergency myasthenic crisis? A. Airway obstruction, profound muscle weakness, and inability to move. B. Paralysis of the muscles and hyperventilation. C. Severe dyspnea, intensification of dysphagia, and dysarthria. D. Impairment of functioning of the autonomic and skeletal muscles. 153. What emergency procedures may be implemented during a myasthenic gravis crisis? A. Tracheotomy with mechanical ventilation. B. Insert ion of a nasogastric tube. C. Insertion of an endotracheal tube. D. Insertion of an oral airway. 154. Dawn is very concerned about the impact of her illness on her family, particularly her two daughters. What question would help in family assessment of her concerns? A. "Do your daughters know that they will have to fulfill your role until your disease is under control?" B. "Why is your condition having such a disruptive effect on your family?'" C. "How is your condition affecting your family members and their usual roles?" D. "How can we help your family adjust to this illness and give you the support you need to recover?" 155. What question would you ask to assess coping abilities of a family? A. "How has your family handled difficult situations before? What strengths emerged from these situations?" B. "Has your family been able to handle chronic illness management before?" C. "What is the best way your family resolves crisis situations?" D. "Does your family have the strength to deal with the changes and still support you through this difficult time?" 156. Which therapeutic interventions may be implemented for individuals with myasthenia gravis? A. Cholinergic medications, muscle relaxants, and nervous system antagonists. B. Anticholinergic medications, muscle stimulants, and nervous system stimulants. C. Cholinesterase inhibitors, thymectomy, and corticosteroids. D. Cholinergic inhibitors, immunosuppressants, and antibodies. 157. A patient who is overweight asks for information regarding diet counseling. What action should the nurse take? A. Suggest a diet with a very limited number of calories from fat and carbohydrates so that she will have reinforcement from quick initial weight loss. B. Assess the patient's eating and exercise patterns and together develop a weight control program that allows for gradual weight loss. C. Examine emotional eating issues and identify the foods that are most harmful and are contributing to the weight gain. D. Identify which diet would be most suited to her needs and body type and then 'have her follow through with the diet principles. 158. A client is receiving IV therapy with 5% dextrose in water (D5W). When assessing the IV site, you note that there is a red line and pain and edema at the insert ion site. What actions would you take? A. Slow the infusion rate and apply warm compresses to the site. B. Discontinue the infusion and apply a warm compress to the IV site. C. Reposition the IV access de vice to lessen the vein irritation. D. Apply antibacterial ointment to the IV site and slow the IV infusion. 159. A physician in a clinic asks you to perform an IV insertion. You have not don e an IV start for many years. What would you do? A. Quickly review the procedure and perform the IV insertion. B. Explain that you are unable to perform the IV start until you have completed an inservice and practice session on IV insertions. C. State that it is not within your scope of practice as a nurse working in a clinic. D. Explain that you do not have malpractice insurance to cover this skill. 160. You are working with a licensed practical nurse (LPN) and have delegated the taking of vital signs for a preoperative patient. When you are reviewing the chart as the patient is leaving for the operating room, you note that his temperature is 38.4 degree C and pulse is 110 bpm. What should you do? A. Have the LPN take the vital signs again, phone the operating room, and cancel the surgery. B. Take the vital signs yourself and do not dele gate this preoperative responsibility in the future. C. Notify the surgeon and await his or her decision; reinforce with the LPN the importance of reporting abnormal preoperative vital signs. D. Sign off the chart but flag that the vital signs are abnormal: allow the patient to go to the operating room. 161. You are on a surgical unit and have been assigned four patients. When you receive your report, you find out that you have a patient who had a transurethral resection of the prostate (TURP) today. A postoperative patient from yesterday is requesting pain medication. A patient with a postoperative infection needs to have an IV antibiotic given in 1/2 an hour. Another patient is to be discharged shortly when his family arrives. Which patient would be your first priority to complete an initial assessment? A. The patient who had the TURP. B. The patient requesting pain medication. C. The patient with the postoperative infection to get IV medication ready. D. The patient being discharged. 162. A 62-year-old mal e client had drainage of a pelvic abscess secondary to diverticulitis 6 days ago. While drinking water, he begins to cough violently. His daughter runs to the nurse's station, screaming that her father ha s "exploded." Upon entering the room, the nurse observes that the "Client ha s experienced dehiscence, and a small segment of bowel is protruding. What should be the nurse's priority action? A. Ask the client what ha s occurred, call the physician, haw the daughter stay with her father, and cover the area with the bed sheet soaking ill water. B. Have a nursing assistant hold the incision together while you obtain the vital signs, call the physician, and flex the client's knees. C. Obtain vital signs, call the physician, obtain emergency orders, and explain to the daughter exactly what has occurred. D. Have the nursing assistant call the physician while you remain with the client, flex the client's knees, and cover the incision with sterile gauze. 163. A patient is receiving external-beam radiation therapy to her thoracic and lumbar spine because of metastatic breast cancer. Which of the following people should be permitted to visit? A. Her pregnant granddaughter. B. Her husband, who is recovering from the flu. C. Her grandson and his family, including his wife and four children, who are between the ages of 4 and 8 years. D. Her elderly sister, who has a history of chronic obstructive pulmonary disease and frequent respiratory infect ions. 164. When monitoring a patient who is at risk for hemorrhage, which assessment data would be significant? A. Warm, dry skin; hypotension; and bounding pulse. B. Hypertension; bounding pulse; and cold, clammy skin. C. Weak, thready pulse: hypertension; and warm, dry skin. D. Hypotension; cold, clammy skin; and weak, thread y pulse. 165. A patient who has had multiple hospital admissions for congestive heart failure is returned to the hospital by her daughter. The patient is admitted to the coronary care unit for observation. She states, “I know I'm sick, but I understand what is needed to take care of myself at home." The nurse recognizes that the patient is attempting to: A. Deny her illness. B. Suppress her fears. C. Reassure her daughter. D. Maintain her independence. 166. When teaching a patient newly diagnosed with inflammatory bowel disease, the nurse must first consider the influence of the: A. Patient's personal resources. B. Type of onset of the disease. C. Total stress of tilt' situation. D. Patient's past experiences. 167. A nurse is caring for a patient admitted to the hospital for treatment of infect ion secondary to AIDS. The patient is experiencing night fevers and as a result is perspiring profusely. Which of the following is the least helpful in managing this symptom? A. Keep a change of bed linen nearby and change as required. B. Administer an antipyretic agent after the patient spikes a fever. C. Ensure that the patient's pillow has a plastic pillowcase. D. Keep liquids for hydration available at the bedside. 168. An elderly client is apprehensive about being hospitalized. The nurse realizes that one of the stresses of hospitalization is the strangeness of the environment and activity. This stress can be reduced by: A. Listening to what the client has to say. B. Using the client's first name. C. Visiting the client frequently. D. Explaining procedures and unit routines to the client. 169. A client who has recently had a fractured hip repaired must be transferred from his bed to a wheelchair. While assisting with this, the nurse should remember that: A. During a weight-bearing transfer, the client’s knees should be slightly bent. B. Transfers to and from a wheelchair will be easier if the bed is higher than the wheelchair. C. The transfer can be accomplished by instructing the patient to pivot while placing his weight on both upper extremities rather than on his legs. D. The appropriate proximity and visual relationship of the wheelchair to the bed must be maintained. 170. When teaching a client about diabetes and self-administration of insulin, what should the nurse's first action be? A. Begin the teaching program at the client's level of understanding. B. Determine what the client knows about the health problem. C. Set specific short and long-term goals. D. Collect equipment needed to demonstrate giving an injection. 171. An elderly client with primary degenerative dementia has difficulty following simple directions and selecting clothes to be worn for the day. The nurse recognizes that these problems are the result of: A. Clouding of consciousness. B. Impaired judgment. C. Loss of abstract thinking ability. D. Decreased attention span. 172. During the day, a nurse puts one side rail up on the bed of a 73 -year-old client admitted to the unit after a hip fracture. What is the reason for putting up the side rail? A. Because all clients over 65 years of age should use side rails. B. Because elderly people are often disoriented for several days after anaesthesia. C. To be used as handholds and to facilitate the client's mobility in bed. D. As a safety measure because of the client's age. 173. Mr. Unter's family physician uses an electronic medical record. The primary objective of an electronic medical record is to support health care providers with: A. Reminders, alerts, support systems, and links to medical knowledge. B. Referrals, clinical decision support systems, and hospital records. C. Laboratory results, alerts, and medical knowledge. D. All of the above. 174. Nursing informatics includes: A. Use of decision-making systems to support the use of the nursing process. B. Research related to the information nurses use when making patient care decisions. C. Nursing use of a hospital information system. D. All of the above. Case Study: Mrs. Kennedy, age 78 years, .is admitted to a rehabilitation unit after a cerebrovascular accident (CVA). She is bedridden and aphasic. The next morning, the physician orders an indwelling catheter because Mrs. Kennedy has been incontinent during the night. Questions 775 to 178 175. Mrs. Kennedy's niece expresses that her aunt had not been incontinent while at home. She insists that the nurse failed to communicate the need for catheterization with her aunt or get consent. This is an example of: A. Treatment with out consent of the patient, which is an invasion of rights. B. Treatment for the patient's benefit. C. Inability to obtain consent for treatment because the patient was aphasic. D. Treatment that does not need special consent. 176. Mrs. Kennedy's emotional responses to her illness would be most influenced by: A. Her past experiences and coping abilities. B. The fact that she is incontinent. C. Her relation ship with the health care staff. D. Her ability to understand her illness. 177. In aiding Mrs. Kennedy to develop independence, her nurse should: A. Demonstrate ways she can regain independence in activities. B. Reinforce success in tasks accomplished. C. Establish long-term goals for the patient. D. Point out her errors in performance. 178, Because of symptoms experienced after her CVA, the nurse discovers that Mrs. Kennedy needs assistance using utensils while eating. What would the nurse do to support this? A. Encourage Mrs. Kennedy to participate in the feeding process to the best of her abilities. B. Feed another patient and wait in the dining room until Mrs. Kennedy feeds herself. C. Request that Mrs. Kennedy's food be pureed by dietary staff working at the facility, D. Have Mrs. Kennedy's niece feed her at every meal to reduce staffing limitations. 179. As a nurse, you are facilitating a cancer screening inservice for colorectal cancer, which of the following clients presents the fewest risk factors for colon cancer? A. A 45-year-old woman with a 25 -year history or ulcerative colitis. B. A 50• year-old man whose father died of colon cancer. C. A 60-year-old man who follows a die t low in fat and high in fibre. D. A 72-year-old woman with a history of breast cancer. 180. A 52-year-old woman has a blood pressure of 146/96 mm Hg. Upon hearing the reading, she exclaims, "Wow! My pressure seems high. Will I need to take medication?" Which of the following is the best response by the nurse? A. "Yes, Hypertension is now more prevalent among: women. It's fortunate we caught this during your routine examination." B. "We will need to reevaluate your blood pres sure because your age places you at a high risk for hypertension." C. “A single elevate d blood pressure does not confirm hypertension. You will need to have your blood pressure reassessed several times before a diagnosis can be made. " D. "You have no need to worry. You r blood pressure is probably elevated because you're in the doctor's office." 181. A client with a positive Mantoux test result is taking isoniazid as prescribed. Which of the following should the nurse assess for during the client's next clinic visit? A. Yellowing of the skin or eyes. B. Peripheral edema. C. Shortness of breath. D. Pruritus. 182. A client comes to the clinic because of low-grade afternoon levers, night sweats, and a productive cough. The physician suspects pulmonary tuberculosis, especially after the client remarks that his wife was recently diagnosed with the disease. A positive add-fast bacillus sputum culture confirms the diagnosis of tuberculosis. During the initial nursing history, you observe that the client refers to his diagnosis by using the impersonal pronoun it." What would your best response be? A. "Let's not talk about it. How long have you been having night sweats?" B. “Tell me how you feel about the diagnosis of tuberculosis." C. "It will not kill you if you take your medications." D. "You should not be embarrassed that you have tuberculosis." 183. To promote early and efficient ambulation after an above-the-knee amputation, the client should be encouraged to keep the hip: A. In a flexed position. B. Extended and abducted. C. In functional alignment. D. Slightly raised when moving the slump. 184. The nurse should be aware that a client with rheumatoid arthritis would most often have pain and limited movement of the joints: A. When the latex fixation test result is positive. B. When the room is cool. C. In the morning up on awakening. D. After assistive exercise. 185. To prepare a client with a long leg cast for walking with crutches, the nurse should encourage the client to: A. Sit up straight in a chair to develop the back muscles. B. Keep the affected limb in extension and abduction. C. Do exercises in bed to strengthen the upper extremities. D. Use a trapeze to strengthen the biceps muscles. 186. Which of the following nursing measures would be inappropriate to include when planning care for a client receiving chemotherapy via an IV access de vice? A. Clean the insertion site and change the dressing within 24 to 72 hours. B. Periodically flush [he catheter with heparin. C. Monitor for redness, drainage, and swelling at the insertion site. D. Rotate the insertion site every 72 hours. 187. A client taking lithium carbonate is going home for a 3-d ay pass. The nurse should advise the client to: A. Adjust the lithium dosage if mood changes arc noted. B. Have a snack with milk before going to bed. C. Avoid participation in controversial discussions. D. Continue to maintain normal sodium intake while at home. 188. A female client with a diagnosis of alcohol abuse appears untidy and disorganized. The plan that would best gain the client's involvement in personal care would include: A. Giving her a schedule and requiring her to bathe and dress herself every morning. B. Drawing up a schedule with her and making certain that she adheres to it. C. Bathing and dressing her each morning until she is willing to perform self-care independently. D. Assisting her in bathing and dressing by giving her clear, simple directions. Case Study: A nurse is developing a plan of care for Betty, who is experiencing anxiety after the recent loss of her job. Betty is verbalizing her concerns regarding her ability to meet her role expectations and financial obligations. Questions 189 and 190 189. Which nursing diagnosis would Betty be most a risk for? A. Altered family process. B. Altered thought process. C. Potential for anxiety, D. Ineffective individual coping. 190. Betty is now in a crisis slate. When developing a care plan for Betty, what should the nurse consider? A. Presenting symptoms in a crisis situation are similar for all individuals experiencing a crisis. B. A crisis state indicates that the individual has an emotional illness. C. A crisis state indicates that the individual has a mental illness. D. Presenting symptoms of a crisis are unique and vary from one person to another. 191. Pressure ulcers most often occur in clients who: A. Are immobilized. B. Have psychiatric diagnoses. C. Experience respiratory distress. D. Need close supervision for safety. Case Study: Brian, a 60-year-old retired plumber, falls and is unable to get up. His wife calls an ambulance, and he is brought to the emergency room where it is found that he has a fracture of the neck the left femur. Brian is admitted to the orthopaedic unit, put in Buck's traction, and prepared for surge the next day. Questions 192 and 193 192. On examination of Brian, what would the nurse expect? A. Lengthening of the affected extremity with internal rotation. B. Shortening of the affected extremity with external rotation. C. Abduction with external rotation. D. Abduction with internal rotation. 193. Part of the nursing care for Brian is assessment of the peripheral pulses. What characteristics are important to note when assessing the peripheral pulses? A. Contractility and rate. B. Color of the skin and rhythm. C. Amplitude and symmetry. D. Local temperature and visible pulsations. 194. To prevent pulmonary complications alter surgery, patients should be instructed to perform: A. Incisional splinting. B. Progressive ambulation. C. Diaphragmatic breathing. D. Range of motion exercises Case Study: Mrs. Doreen, age 69 years, was involved in a serious fall at her home. She has a fractured right hip and left tibia. She is scheduled for a right hip replacement and cast application to the left leg. She is currently in Buck's traction on the right side. She lives alone, and her daughter lives in the same community. Questions 195 to 201 195. Mrs. Doreen fears surgery. This fear may depend on past experiences with surgery or pre conceptions of surgery. To alleviate Mrs. Doreen's fears and misconceptions about surgery, what should the nurse do first? A. Provide an explanation about procedures involved in the planned surgery. B. Explain all nursing care and possible discomfort that may result. C. Tell her that pre operative fear is normal. D. Ask her to discuss her understanding of the planned surgery. 196. Identifying a patient upon admittance to the surgical suite is one of the circulating nurse's responsibilities. Which of the following would be the most appropriate verification of Mrs. Doreen's identification upon admittance to the surgical suite? A. Call the client by name before administering the anaesthetic. B. Check her name on the surgical list and suite assignment. C. Compare her arm bracelet with the information in the chart. D. Question the orderly who brought down the client and ask him to identify her. 197. Mrs. Doreen ha s just returned from the operating room with a Foley catheter, an IV line, and an oral airway and is unresponsive. Which of the following is the priority nursing assessment? A. Check the surgical dressing to ensure that it is intact. B. Confirm the placement of the oral airway, C. Examine the IV site for infiltration, D. Observe the Foley catheter for drainage, 198. Mrs. Doreen is on prolonged bed rest. The nurse caring for her should plan nursing care to avoid which common hazard associated with immobility? A. Increased heart rate, B. Shearing forces. C. Increased bone density. D. Hypertension. 199. The nurse encourages Mrs. Doreen to turn frequently in bed to prevent every thing except: A. Pneumonia. B. Urinary stasis, C. Abdominal pain, D. Deep vein thrombosis. 200. When turning Mrs. Doreen, the nurse notices a reddened are a on the coccyx. Which of the following is a priority nursing action? A. Test for blanching. B. Rub the reddened area. C. Check for perspiration. D. Use powder to minimize shear forces, 201. Mrs. Doreen is being discharged from the hospital. Which of the following is the most appropriate intervention for fall prevention? A. Eliminating home safely hazards. B. Encouraging an exercise regimen C. Maintaining medication ad ministration. D. Ensuring adequate nutrition. Case Study: Donna, age 20 years, is scheduled for a cholecystectomy, Questions 202 and 203 202. After the nurse completes the preoperative teaching, Donna states, "If I lie still and avoid turning, I will avoid pain. Do you think this is a good idea?" What is the nurse's best response? A. "It is always a good idea to rest quietly after surgery," B. "You need to turn from side to side every 2 hours." C. "The doctor will probably order you to lie flat for 24 hours." D. "Why don't you decide about activity after you return from the recovery room?" 203. Donna has returned from the operating room. When assessing her respiratory status as she recovers from general anaesthesia, it is of primary importance for the nurse to evaluate the patient's ability to: A. Inhale voluntarily. B. Breathe deeply. C. Swallow. D. Speak. 204. Through the prevention of postoperative complications, the nurse promotes rapid convalescence. Which of the following would be most indicative of a potential postoperative complication requiring further observation? A. Urinary output of 20 mL/hr. B. Temperature of 37.6°C. C. Serous drainage on the surgical dressing. D. Blood pressure of 100/70 mm Hg. 205. After a resection of a lower lobe of the lung, a client has a large amount of respiratory secretions. Nursing care should include: A. Turning and positioning. B. Administration of an expectorant. C. Intermittent positive-pressure breathing. D. Postural drainage. 206. When determining the method of oxygen administration to be used for a specific client, the major concern is: A. Facial anatomy. B. Pathologic condition. C. Age and mental capacity. D. Level of activity. 207. What preventive measure should be taken by the nurse regarding the untoward effects of oxygen therapy? A. Padding elastic bands of the face mask. B. Humidifying the gas before delivery. C. Taking the apical pulse before starting therapy. D. Placing (he client in the orthopneic position. 208. Clients are encouraged to perform deep breathing exercise after surgery. Deep breathing exercises help to: A. Counteract respiratory acidosis. B. Expand the residual volume. C. Increase the blood volume. D. Decrease the partial pressure of oxygen. 209. When oxygen therapy via nasal cannula is ordered for a patient, what is the priority nursing action? A. Post an "Oxygen in use" sign. B. Adjust the oxygen level before applying the cannula. C. Explain fire safety and oxygen use. D. Lubricate the nares with water-soluble gel. 210. What is the most therapeutic position for a patient diagnosed with cardiopulmonary disease? A. Supine position. B. Prone position. C. High Fowler's position. D. 45-degree semi-Fowler's position. 211. A patient is diagnosed with thrombophelbitis. What is the appropriate level of activity for this patient? A. Bed rest with the affected extremity in the dependent position B. Bed rest with bathroom privileges. C. Bed rest, keeping the affected extremity flat. D. Bed rest with elevation of the affected extremity. 212. Which patient assessment made by the nurse would require immediate intervention? A. Ten respirations per minute by a sleeping patient. B. Ranting sound in the pharynx of an unconscious patient C. Coughing and expectorating large amounts of thick mucus. D. Slight shortness of breath after returning from the bathroom. Case Study: Mr. Kenn, age39 years, arrives at the hospital to undergo a total laryngectomy and radical neck dissection. Questions213 to218 . 213. Mr. Kenn enters the operating room and appears relaxed. Then he begins talking rapidly, commenting, "I'm really nervous and scared about the operation." What is the client experiencing, and what action should the nurse take next? A. The client is experiencing anxiety; the nurse should listen attentively and provide realistic verbal reassurance. B. The client is experiencing an adverse effect of meperidine; the nurse should report it to the physician. C. The client is typically anxious; the nurse should proceed with the assessment and preparation for surgery. D. The client needs additional sedation; the nurse should request an order from the anaesthestologist. 214. It is Mr. Kenn's first postoperative day. What is a priority goal? A. Communicate by use of esophageal speech. B. Improve body image and self-esteem. C. Prevent aspiration. D. Maintain a patent airway. 215. When preparing to suction Mr. Kenn's tracheostomy, the nurse should be aware that the maximum recommended time frame for intermittent suction is: A. 1 to 5 seconds. B. 5 to 10 seconds. C. 10 to 15 seconds. D. 16 to 20 seconds. 216. Which of the following must you consider regarding positioning Mr. Kenn for suctioning? A. When performing suctioning on Mr. Kenn, who has a gag reflex, position him in the semi-Fowler's position. B. When performing oral and oropharyngeal suctioning on Mr. Kenn, ensure that his head is turned to one side. C. When performing nasal and nasopharyngeal suctioning on Mr. Kenn, ensure that his neck is hyperextended. D. All of the above. 217. Mr. Keno is receiving mechanical ventilation. What nursing action is appropriate in relation to cuff care for h is tracheostomy? A. Inflate the cuff during suctioning. B. Allow the cuff to be deflated for 10 minutes every hour. C. Assess cuff pressure for a minimal air leak. D. Ensure the cuff pressure allows for a gradual decrease in tidal volume. 218. When performing deep trachea l suctioning for Mr. Kenn, the nurse should: A. Be sure the cuff of the tracheotomy is initiated during suctioning. B. Instil acetylcysteine (Mucomyst) into the tracheotomy before suctioning. C. Apply negative pressure as the catheter is being inserted. D. Hyperoxygenate the client before suctioning. Case Study: Mr. Ray, age 83 years, presents at the emergency department after falling on the ice out-side his senior citizens' housing facility. The admitting diagnosis is right hip fracture, and surgical repair is planned. Questions 219 to 221 219. What is the most important initial assessment finding by the nurse? A. Leg shortening on the affected side. B. Complaints of pa in. C. Neurovascular compromise. D. Internal or external rotation of the hip. 220. A progressive ambulation schedule is to be instituted for Mr. Ray after surgery. Mr. Ray has been receiving antihypertensive medication as well as morphine sulfate for pain. When getting the client out of bed, the nurse should first have him sit on the edge of the bed with his feet dangling. This anion is taken because the nurse is anticipating: A. Postural or orthostatic hypotension. B. Respiratory distress. C. Initial hypertension. D. Hip pain. 221. When assisting Mr. Ray to ambulate after rep air of his fractured right hip, where should the nurse stand? A. In front of the client. B. Behind the client. C. On the client's left side. D. On the client's right side. Case Study: Mr. Schultz is skiing. During his last ski run, he falls awkwardly and breaks his left leg. Questions 222 and 223 222. Mr. Shultz's leg is set in a long leg cast. The nurse should observe for signs indicative of compromised circulation, such as: A. Foul odour of the affected leg. B. Increased swelling of the toes. C. Increased body temperature. D. Purulent drainage on the cast. 223. During afternoon rounds, the nurse finds Mr. Schultz using a pencil to scratch inside his cast. Mr. Schultz is complaining of severe itching in the ankle area. Which action should the nurse take? A. Encourage him to scratch more gently with a pencil. B. Give him a sterile metal object to use for scratching. C. Administer diphenhydramine as ordered for the relief of severe itching. D. Obtain an order for a sedative, such as diazepam (Valium), to pre vent him from scratching. Case Study: Mr. Chorn is a patient with kidney failure. Questions 22 4 and 225 relate to this scenario. 224. Mr. Chorn is placed on fluid restriction of 1000 mL of fluid over a z-t-hour period. The nurse should: A. Eliminate the liquids between meal times. B. Divide the fluids equally among the three nursing shifts. C. Indicate just dear liquids in the restriction plan. D. Proportion mo re fluids in the day than during the night. 225. Mr. Chorn has an IV started. At what rate should the IV be set to infuse 3000 mL of D5W in a 24-hour period (drop factor, 10)? A. 125 mL/hr; 21 gtt/min. B. 100 mL/hr; 17 gtt/min. C. 150 mL/hr; 2l gtt/min. D. 200 mL/hr: 34 gtt/min. 226. In relation to extracellular body fluids, normal saline is: A. Hypertonic. B. Hypotonic. C. lsotonic. D. Acidotic. Case Study: Hannah York has Addison's disease. She is admitted to the hospital because of complications. Questions 22 7 and 228 227. Which assessment finding would most probably warrant a nursing diagnosis of fluid volume deficit? A. Leathery, pliable skin. B. Pretibial pitting edema. C. Pedal pulses of 4 +. D. Dry skin with poor turgor. 228. Hannah is drinking 3OOO ml, of fluid a day. When assessing her urine, the nurse can expect the urine to be: A. Dark and straw coloured. B. Straw coloured. C. Light amber. D. Dark amber. 229. Mrs. Anderson is receiving furosemide (Lasix) and digoxin. Nursing care should include observation for symptoms of electrolyte depletion caused by: A. Sodium restriction. B. Inadequate oral intake. C. Continuous dyspnea. D. Diuretic therapy. 230. Martin Fechner enters the hospital with diarrhea. anorexia. weight loss. and abdominal cramps. A tenta tive diag nos is of colitis has been made. He is scheduled for a sigmoidoscopy and barium enema. Symptoms of fluid and electrolyte imbalance the nurse should report immediately are: A. Extreme muscle weakness and tachycardia. B. Development of tetany with muscle spasms. C. Nausea, vomiting, and leg and stomach cramps. D. Skin rash, diarrhea, and diplopia. 231. Total parental nutrition (TPN) solution contains all of the following nutrients except: A. Dextrose. B. Amino adds. C. Electrolytes. D. Fat emulsions. 232. What is an appropriate nursing action to detect early signs of metabolic complications of total parental nutrition (TPN)? A. Assess lung sounds. B. Weigh the patient daily. C. Monitor urine output. D. Monitor vital signs. 233. The nurse should be aware that the patient’s serum blood glucose should be maintained below which level when receiving TPN? A. 3 mmol/L. B. 4.2 mmol/L. C. 5.5 mmol/L. D. 8.3 mmol/ L. 234. If symptoms of an air embolism occur. The patient should be placed in which of the following positions? A. On the back in semi-Fowler's position. B. On the left side in the deep Trendelenburg position. C. On the right side in the deep Trendelenburg position. D. On the left in semi-Fowler's position. 235. Symptoms of hyperglycemic hyperosmolar non-ketotic (HHNK) com a include all of the following except: A. Glycosuria. B. Seizures. C. Coma. D. Anuria. 236. After a laminectomy, a male client has a palpable bladder and complains of lower abdominal discomfort. He is voiding 60 to 80 ml. of urine every 4 hours. What is the best nursing Intervention? A. Observe for worsening discomfort. B. Administer the prescribed analgesic. C. Obtain an order for urinary catheterization. D. Reassure the client that this is a normal voiding pattern. 237. Which complication is a client who is receiving hemodialysis for chronic renal failure at risk of developing? A. Peritonitis. B. Renal calculi. C. Bladder infection. D. Serum hepatitis. 238. What is a major disadvantage of an ileal conduit? A. Stool continuously oozes from it. B. Absorption of nutrients is diminished. C. Peristalsis is greatly decreased. D. Urine drains from it continuously. Case Study: Mrs. Jules is a 77-year-old woman who has had problems with urinary urgency for the past 3 years. She is trying to deal with the problem herself by using on absorbent pad, but she is self-conscious and believes that "everyone notices it.” She states that the bulkiness and odour are embarrassing and now she does not like to go out. Questions 239 and 240 239. When caring for Mrs. Jules, who is now on a bladder-retraining program, the nurse should recognize that an intervention always implemented during a bladder-retraining program is toileting: A. Every 2 hours when awake. B. At 8 a.m., 2 p.m., 8 p.m., and 2 a.m. C. Every 4 hours and through the night. D. When the patient goes to bed at night. 240. What would be the most common reason why Mrs. Jules became incontinent of urine? A. Older adults lend to drink less fluid than younger patient s. B. Older adults' slow metabolism increases pressure from their intestines onto their bladder. C. Older adults use incontinence to manipulate and control others. D. The muscle s that control urination have weakened. 241. A physician orders daily stool examinations for a client with chronic bowel inflammation. These stool examinations are ordered to determine: A. Culture and sensitivity. B. Occult blood and organisms. C. Ova and parasites. D. Pat and undigested food. 242. A physician orders a low -residue diet for a client with an acute exacerbation of colitis. The nurse would know that the dietary teaching is understood when the client states, “I can eat:" A. "Cream soup and crackers, omelettes, mashed potatoes, peas, orange juice, and coffee.” B. "Stewed chicken, baked potatoes with butter, strained peas, white bread, plain cake, and milk." C. "Baked fish, macaroni with cheese, strained carrots, fruit gelatine, and milk.” D. "Lean roast bed, buttered white rice with egg slices, while bread with butter and jelly, and tea with sugar.” Case Study: Mrs. Hillster has a diagnosis of a bowel obstruction. She complains of nausea; is vomiting dark bite material; and has severe cramping, intermittent abdominal pain. This condition is caused by intussusceptions, and surgery is scheduled. Questions 243 to 245 243. Four days after surgery. Mrs. Hillster has not passed any flatus, and bowel sounds are not present. Even though her abdomen has become more distended, she feels little discomfort. Paralytic ileus is suspected. What causes this condition? A. Impaired blood supply to the bowel. B. Impaired neural functioning. C. Perforation of the bowel wall. D. Obstruction of the bowel wall. 244. Mrs. Hillster requires additional surgery, and an ileostomy is performed. What knowledge should guide the nurse when caring for Mrs. Hillster's ostomy? A. Expect the stoma to start draining 72 hours after surgery. B. Explain that the drainage can be controlled with daily irrigations. C. Anticipate that emotional stress can increase intestinal peristalsis. D. Be aware that bleeding from the stoma is a medical emergency. 245. Why is Mrs. Hillster at risk for the development of anemia? A. The hemopoietic factor is absorbed only in the terminal ileum. B. Folic acid is absorbed only in the terminal ileum. C. Iron absorption depends on simultaneous bile salt absorption in the terminal ileum. D. The trace elements required for hemoglobin synthesis occur only in the ileum. Case Study: Mr. Kerry is admitted to the hospital with extensive carcinoma of the descending portion of the colon with metastasis to the lymph nodes. He has undergone surgery and now has a colostomy. Questions 246 to 248 246. Which product should the nurse use to protect the skin surrounding the colostomy opening? A. Tincture of benzoin. B. Mineral oil. C. Stomahesive. D. Petroleum jelly. 247. What act ion should the nurse take if Mr. Kerry complains of abdominal cramps during his colostomy irrigation? A. Raise the irrigating container to quickly complete the irrigation. B. Reassure him and continue the irrigation. C. Pinch the tubing so that less fluid enters the colon. D. Clam p the tubing and allow the client to rest. 248. What should the nurse emphasize when discussing the regaining of bowel control with Mr. Kerry? A. An Irrigation routine. B. A soft, low-residue diet. C. Managing flu id Intake. D. A high-protein diet. 249. Mrs. Lyste is an immobile client. When a nurse repositions her, redness over a bony prominence is noticed. When this area is assessed, the red spot blanches wit h fingertip touch indicating: A. A local skin infection requiring antibiotics. B. Abnormal reactive hyperemia. C. Deep tissue damage. D. The reactive hyperemia is likely transient. Case Study: Sue Kong is a 38•year-vld woman. She had a panniculectomy (tummy tuck) and experienced wound dehiscence 3 days after surgery. Questions 250 to 252 250. Sue ha s yellowish discharge on her dressing every time the dressing is changed. The nurse notices that the amount of discharge is increasing. The nurse recognizes that the yellow drainage is from serum. Serous drainage from a wound is defined as: A. Fresh, red bleeding. B. Clear, watery plasma. C. Thick and yellow. D. Beige to brown and foul smelling. 251. Sue has a binder placed around her surgical incision. What is the purpose of applying a binder after panniculectomy surgery? A. Collection of wound drainage from the incision. B. Keeping her abdominal pain under control C. Reducing stress on the abdominal incision. D. Stimulation of peristalsis from direct pressure. 252. Sue is receiving hydrocolloid dressings for her abdomen. What is the purpose of this dressing? A. A dressing that is highly absorptive and prevents dehiscence of the wound. B. A dressing that is premoistened and promotes granulation of the wound. C. A dressing that contains a debriding enzyme that is used to remove necrotic tissue. D. A dressing that forms a paste that interacts with the surface of the wound. 253. Parenteral preparations of potassium must be administered slowly and cautiously to prevent: A. Acidosis. B. Cardiac arrest. C. Hypertension. D. Hyperglycemia. 254. When caring for a client within the first 24 hours after a cardiac catheterization, the nurse should: A. Keep the patient NPO for 2 to 4 hours after catheterization. B. Check the pulse distal to the catheter insertion site. C. Ensure that the patient is kept flat in bed f 8 hours after the procedure. D. Ensure that the doctor has order antiarrhythmic medications for the patient. Case Study: Mr. McKay, age 44 years, comes into the emergency department as he is passing a kid stone. Mr. McKay requires increased volume, and physician orders normal saline 125 mL/hr. You the nurse, and you need to start his IV line. Question 255 to 257 255. An air embolism may be avoided by: A. PICG insertion. B. Valsalva manoeuvre. C. Pneumocentesis. D. Fluoroscopy. 256. Mr. McKay's catheter has become occluded. What is the most common cause of catheter occlusion? A. Improper dressing. B. Catheter defects. C. Infection. D. Thrombosis. 257. Mr. McKay now complains of pain. Pain with infusion is a sign of which of the following? A. Catheter malposition. B. Pinch -off syndrome. C. Fibrin sheath occlusion. D. External compression. Case Study: As a result of an all-terrain vehicle mishap, Mr. Jool, age 60 years, has a punctured right lung. He is admitted to the hospital, and a chest tube is inserted. Questions 258 to 261 258. While turning Mr. Jool, his chest lube accidentally becomes disconnected. As a nurse, you should: A. Immediately tell him to breathe shallowly while you cover the wound. B. Immediately tell him to cough or exhale forcibly while you cover the wound. C. Calling for assistance and then cove r the wound with a sterile dressing. D. Call for assistance and cover the insertion site with clean gauze. 259. To prevent Mr. Joel's chest tube from disconnecting again, the tubing should be: A. Coiled flat on the bed and positioned loosely beside him. B. Coiled flat on the bed and secured without putting tension on the tube. C. Coiled flat and secured to his bedrail. D. Coiled flat and secured in dependent loops along the side of the bed. 260. Mr. Jool ha s his chest tube attached to a Pleurevac system, when ca ring for Mr. Joel, the nurse should: A. Change the dressing daily using aseptic technique. B. Palpate the surrounding area for crepitus. C. Empty the drainage chamber at the end of the shift. D. Clamp the chest tubes when suctioning the client. 261. When scheduling postural drainage treatments for Mr. Jool, when would be the most appropriate time of day for him to receive this treatment? A. Immediately upon awakening. B. One hour before a meal. C. Before bedtime. D. One hour after a meal. 262. The purpose of the water in the closed chest drainage chamber is to: A. Facilitate emptying bloody drainage from the chest. B. Foster removal of chest secretions by capillarity. C. Prevent entrance of air into the pleural cavity, D. Decrease the danger of sudden change in pressure in the lube. 263. A doctor orders a nurse to monitor the amount of chest tube drainage. The normal amount of drainage in 24 hours is approximately: A. 300 mL. B. 750 mL. C. 1200 mL. D. 1500 mL. 264. While delivering a tube feeding by gravity, the observation that indicates that the client is unable to tolerate a continuation of the feeding is: A. A passage of flat us. B. Rapid flow of the feeding. C. Epigastric tenderness. D. A rise of formula in the tube. 265. After a modified radical mastectomy, a client has two Jackson-Pratt portable wound drainage systems in place. When caring for these drains, the nurse should: A. Leave them open to the air to ensure maximum drainage. B. Ensure that the drainage receptacles are kept compressed to maintain suction. C. Attach the tubes to straight drainage to monitor the output. D. Irrigate the drains with normal saline to ensure patency. 266. A semi-Fowler's position is used to: A. Minimize flexion contractures of the hip. B. Relieve pressure on the ischial tuberosities. C. Prevent aspiration during nasogastric tube feeding. D. Reduce the development of pressure (decubitus) ulcers. Case Study: A physician has ordered insertion of a nasogastric (NC) tube for Mr. Brucks. Questions 267 and 268 267. During the insertion of the NG tube, the nurse would report that Mr. Brucks was experiencing difficulty if he demonstrates: A. Choking. B. Cyanosis. C. Flushing. D. Gagging. 268. To ensure that Mr. Brucks' NG tube is positioned correctly, the nurse should insert the tube a distance: A. That is equal to the distance from the patient's ear lobe to his (lose plus the distance from his nose to the lip of his xiphoid process. B. That is equal to the distance from the tip of his nose to the tip of the ear lobe down to the xiphoid process of the sternum. C. To the second or third black marking on the NG tube. D. From the lip of his ear to the tip of his xiphoid process. 269. Which of the following is true concerning the height of the IV solution bag? A. It should be placed 90 cm above the injection sue. B. It should be placed 30 cm allow the injection site. C. The greater the height, the lower the force. D. The lower the height, the greater the force. 270. The term “vasovagal reaction" refers to an autonomic nervous system response to: A. Stress. B. Fluid resuscitation. C. Sudden hydration. D. Circulatory overload. Case Study: Mrs. Better is a 59-year-old widow who was diagnosed 25 years ago with type 2 diabetes mellitus. She has recently been diagnosed with thyroid cancer. Mrs. Bezler is currently receiving total parenteral nutrition (TPN) therapy. Questions 271 and 272 271. The doctor has ordered a central venous pressure (CVP) catheter for Mrs. Bezler. In assessing Mrs. Bezler's CVP reading, a nurse should place the client: A. In a horizontal position. B. In a low Fowler's position. C. Side -tying on the affected side. D. Side -lying opposite to the manometer. 272. Which of the following statements concerning Mrs. Bezler's CVP catheter patency is correct? A. Patency includes the ability to infuse through and aspirate blood from the catheter. B. The risk for occlusion in creases with dehydration and atrial fibrillation. C. Occlusions can lead to superior vena cava syndrome. D. All of the above, 273. Which of the following veins has the least risk for catheter-related bloodstream infections? A. Brachycephalic. B. Femoral. C. Internal jugular. D. Subclavian. 274. The most important aspect of hand washing is: A. Water. B. Soap. C. Friction. D. Time. 275. When performing tracheotomy care, the nurse must: A. Monitor the client's temperature after the procedure. B. Use sterile gloves during the procedure. C. Use Betadine to clean the inner cannula when it is removed. D. Place the client in the semi-Fowler's position. 276. When transferring an immobilized client, the nurse should remember to use which principle of body mechanics'? A. Bending at the waist to provide the power ' for lifting. B. Keeping the body straight when lifting to reduce pressure on the abdomen. C. Placing the feet apart to increase the stability of the body. D. Relaxing the abdominal muscles and using the extremities to prevent strain. 277. The most important aspect in reducing the risk of bloodborne infections for nurses working in the operating room is: A. The avoidance of percutaneous injury. B. The awareness of emerging infectious diseases. C. The avoidance of doing invasive procedures. D. The awareness of potential risks. 278. Mr. Lee comes to the hospital for open heart surgery. After 3 days, he is diagnosed with an antibiotic-resistant organism. Which precautions should be used with Mr. Lee? A. Droplet. B. Airborne. C. Contact. D. Isolation. 279. Mr. Tames, age 55 years, has a history of hypertension and has just been prescribed a new anti hypertension medication. He complains of feeling dizzy at times. Which of the following is the best way to assess his blood pressure related to his complaints? A. Assess his blood pressure in the supine, sitting, and standing positions. B. Have him walk around the room and then assess his blood pressure. C. Assess his blood pressure at the beginning and the end of the examination. D. Take his blood pressure on the left arm and again in 5 minutes on the right arm. Case Study: Mr. Metivier, age 46 years, has presented to the emergency department for treatment of chest pain. After the pain subsides, he is admitted to a medical-surgical unit with telemetry because no cardiac unit beds are available. Questions 280 to 284 280. Mr. Metivier is scheduled for an EEG. Which of the following is the client permitted to ingest 24 hours before the test? A. Solid foods. B. Stimulants. C. Coffee and tea. D. Tranquilizers. 281. While in the hospital, Mr. Metivier has a myocardial infarction. The medical team is concerned about reducing the workload of his heart. Mr. Kerry's orders include strict bed rest and a clear liquid diet. The nurse should explain that the primary reason for this diet is to reduce: A. Gastric acidity of the stomach. B. The metabolic workload of digestion. C. Mr. Metivier's current weight. D. The amount of fecal elimination. 282. Two days after the myocardial infarction, Mr. Metivier's temperature is elevated. From his cardiac episode, which of the following would he most likely related to his infarction? A. Possible infect ion. B. Tissue necrosis. C. Pulmonary infarction. D. Pneumonia. 283. When creating a therapeutic environment for Mr. Metivier, the nurse should encourage: A. Daily papers in the morning. B. Telephone communication. C. Short family visits. D. Television for short periods. 84. Mr. Metivier, who is receiving multiple medications for a myocardial infarction, complains of severe nausea. Assessments reveal that his heartbeat is irregular and slow. The nurse should recognize these symptoms as toxic effects of which medication? A. Lanoxin (Digoxin). B. Aminosalicylic acid. C. Morphine sulfate (morphine). D. Meperidine hydrochloride (Demerol). 285. A 92-year-old patient has suffered a cerebrovascular accident (CVA). The right side of his face has visible ptosis. Knowing this, you may also suspect which of the following? A. Agenesis. B. Epistaxis. C. Dysphagia. D. Xerostomia. 286. An l 8-year-old young man ha s suffered a C5 spinal cord contusion that has resulted in quadriplegia. His mother is crying in the waiting room 2 days after the surgery has occurred. The mother asks you whether her son will eve r play football again. Which of the following would be the most therapeutic approach when working with this mother? A. Reassure her that given lime and motivation, he will return to his functional ability before the injury. B. Advise her that it is not in his best interest for her to be so upset and explain the importance of moral support. C. Reflect on how she is feeling and encourage her to express other fears that she has about his injury. D. Leave the waiting room, call the son's physician, and ask that the physician speak to his mother right away. 287. A 72-year-old client has been admitted to the medical-surgery unit from the emergency department with a diagnosis of left-sided vascular accident. In transferring him from the stretcher to his bed, the nurse notices that the client's respirations have a snoring quality. Which of the following is the priority nursing action? A. Plan: the client in a Fowler's position with the head of the bed at a 45-degree angle. B. Assess the client's ability to communicate his needs to the health care team. C. Position the client on his side with the head of the bed slightly elevated. D. Place all items that the client may need to the left side of the bed. 288. A client has been admitted and has been diagnosed with having a cerebrovascular accident. Twenty-four hours after admission, the client has right-sided hemiplegia. Which of the following neurologic deficits is closely associated with this type of hemiplegia? A. Difficulty speaking and understanding. B. Loss of consciousness. C. Inability to see to the left. D. Poor judgement and impulsive behaviour. 289. An 18-year-old young man has fractured his spine in a diving accident. Upon initial admission to hospital, what is the best position for the client? A. Prone with his head to the side. B. Side-lying with his head midline. C. High Fowler's position with his head to the side. D. Supine position with his head midline. 290. A patient has an impairment of cranial nerve II. Knowing the function of this nerve, a nurse must do which of the following to ensure the patient's safety? A. Clear any obstacles in a path for walking. B. Test the water temperature of the shower. C. Speak loudly to the patient. D. Check the temperature of hot tea the client is going to drink. 291. A nurse assesses a client who is in cardiogenic shock. The nurse understands that this type of shock is: A. A failure of peripheral circulation. B. An irreversible phenomenon. C. Generally caused by decreased blood volume. D. Usually a fleeting reaction to tissue injury. 292. A client has sustained a head injury and is to receive mannitol (Osmitrol) by IV push. In evaluating the effectiveness of the drug, the nurse should expect to find which of the following? A. Increased lung expansion. B. Decreased cerebral edema. C. Decreased cardiac workload. D. Increased cerebral circulation 293. A 64-year-old woman is found on the floor of her apartment. She had apparently fallen and hit her head on the bathtub. On admission to the neurology unit, she has a decreased level of consciousness. The physician's orders for positioning are as follows: "Elevate the head of the bed; keep the head in neutral alignment with no neck flexion or head rotation; avoid sharp hip flexion.” Which of the following is the best rationale for this positioning? A. To decrease cerebral arterial pressure. B. To avoid impeding venous outflow. C. To prevent flexion contractures. D. To prevent aspiration of stomach contents. 294. The first-line treatment of cardiogenic shock involves all the following except: A. Supplying supplemental oxygen B. Controlling chest pain. C. Hemodynamic monitoring. D. Enhancing safety and comfort. 295. A traumatic tension pneumothorax can be caused by: A. A penetrating injury resulting in air moving into the thoracic cavity without being able to exit. B. A blunt or penetrating injury resulting in air moving into the pleural space without being able to exit. C. A blunt injury in which air enters and exits the pleural cavity through the pressure deficit created by injury. D. A penetrating injury that causes air to be sucked Into the lungs during both inhalation and exhalation. 296. Which of the following are considered normal respiratory parameters? A. Respiratory rate of 10 to 20 breaths/min, Sp02 of 98%, and retraction and bulging of the Interspaces on inspiration. B. Respiratory rate of 10 to 20 breaths/min, Sp02 of 97% to 98%, and even breathing with occasional sighs. C. Accessory muscles are used to enhance respiration, restlessness, and pale lips and nail beds. D. None of the above. 297. A client with heart failure develops pink frothy sputum, coarse crackles, and restlessness. Of the following, which is the priority nursing action? A. Check the client's blood pressure. B. Place the client in high Fowler's position. C. Calculate the client's fluid balance. D. Notify the physician. 298. What position would be contraindicated for a client who has dyspnea? A. Supine. B. Contour. C. Fowler's position. D. Orthopneic. 299. From the following, which assessment findings would most likely indicate that a client is having difficulty breathing? A. 16 breaths/min and deep in character. B. 18 breaths/min and inhaled through the mouth. C. 20 breaths/min and shallow in character. D. 28 breaths/min and noisy. 300. A 57-year-old client is admitted to the hospital for exacerbation of chronic obstructive pulmonary disease (COPD). Which of the following would the nurse expect to find during a nursing assessment? A. Dyspnea, cough, and bradycardia. B. Wheezing, tachycardia, and restlessness. C. Barrel chest, tachycardia, and hypertension. D. Hypotension, confusion, and weight gain. 301. A client's arterial blood gas analysis reveals an excess of carbon dioxide. The nurse should recognize that this is consistent with which of the following? A. Metabolic acidosis. B. Metabolic alkalosis. C. Respiratory acidosis. D. Respiratory alkalosis. 302. Mrs. Schneider; age 82 years, is admitted with congestive heart failure and pulmonary edema. To help alleviate Mrs. Schneidar's distress, the nurse should: A. Elevate her lower extremities. B. Place her in an orthopneic position. C. Encourage frequent coughing. D. Prepare for modified postural drainage. 303. A 65-year-old man comes to the emergency department with severe chest pain and shortness of breath. He is diaphoretic, pale, and weak. Suddenly, he collapses and becomes unresponsive. What should the nurse do first when assessing this client? A. Check for a carotid pulse. B. Check for spontaneous respirations. C. Maintain an open airway. D. Gently shake him and shout. "Are you OK?" 304. A 48-year-old foreman at a local electric company comes to the emergency department complaining of severe substernal chest pain that radiates down his left arm. He is admitted to the coronary care unit with a diagnosis of myocardial infarction (MI). Which of the following should the nurse do first when the patient is admitted to the coronary care unit? A. Begin EGG monitoring. B. Obtain a family health history. C. Auscultate the lung fields bilaterally, D. Determine the quality of the client's pain. 305. When performing external cardiac compression, the nurse should exert downward vertical pressure on the lower sternum by placing: A. The heels of each hand side by side, extending the fingers over the chest. B. The heel of one hand on the sternum and the heel of the other on top of it with the fingers interlocking. C. The fingers of one hand on the sternum and the fingers of the other hand on top of them. D. The heel of one hand on the sternum and the fleshy pan of a clenched fist on the lower sternum. 306. A client's cardiac monitor is indicative of ventricular fibrillation. The nurse from the coronary care unit should prepare for: A. An IM injection or digoxin (Lanoxin). B. An I V line for emergency medications. C. Immediate defibrillation. D. Elective cardioversion. Case Study: Mr. and Mrs. Donald Reitz have been married almost 7 years when a physical examination confirms that Mrs. Reitz is 8 to 10 weeks pregnant. Mr. and Mrs. Reitz are overjoyed. About 10 days after her visit to the physician. at the time of her normal menstrual period, Mrs. Reitz starts to spot but denies pain. Her physician tells her to remain on complete bed rest for at least 72 hours. Questions 307 to 309 307. What is the most appropriate diagnosis for Mrs. Reitz? A. Threatened abortion. B. Inevitable abortion. C. Ectopic pregnancy. D. Missed abortion. 308. After a few hours. Mrs. Reitz begins to experience bearing-down sensations and suddenly expels tissue. A priority nursing action at this time would be to: A. Take her immediately to the delivery room. B. Check the fundus for firmness. C. Give her the sedation ordered. D. Immediately notify the physician. 309. When the nurse returns to the room, she notices that both Mrs. Reitz and her husband are visibly upset. Mr. Reitz has tears in his eyes, and Mrs. Reitz has he r face: turned to the wall, sobbing quietly. The best approach for the nurse to take is to go over to Mrs. Reitz and say: A. “I know how you feel, but you should not be so ups et now. It will make it more difficult for you to get better. B. “I can understand that you are upset, but be glad it happened early in your pregnancy and not after you carried the baby to full term." C. “I know that you are upset now. But hopefully you will become pregnant again very soon.” D. “I see that both of you are very upset. I will be here if you want to talk.” 310. Diabetic coma results from an excess accumulation of which substance in the blood? A. Ketones from rapid fat breakdown-causing acidosis. B. Glucose from rapid carbohydrate metabolism, causing drowsiness. C. Sodium bicarbonate, causing alkalosis. D. Nitrogen from protein catabolism, causing ammonia intoxication. 311. A client with diabetes mellitus has had declining renal function over the past several years. He is placed on hemodialysis because of persistently elevated creatinine levels. Which diet regimen would be best for the client on days between dialysis? A. High-protein with a prescribed amount of water. B. Low-protein diet with a prescribed amount of water. C. Low-protein diet with an unlimited amount of water. D. No protein in the diet and use of a salt substitute. 312. A 28-year-old woman has had type I diabetes for 10 years. She is doing home blood glucose monitoring and urinary dipsticks for acetone. She asks the nurse why she has to dipstick her urine, too. Upon which of the following rationales would the nurse base he r answer? A. A positive test reaction indicates too much glucose. B. A positive test reaction indicates too much insulin. C. A positive test reaction indicates ketoacidosis D. The test measures protein in the urine. 313. When working with a diabetic patient, the nurse must know that the difference between diabetic coma and hyperglycemic hyperosmolar nonketotic coma is that clients in diabetic coma experience; A. Fluid loss. B. Glycosuria. C. Increased blood glucose. D. Kussmaul respirations. Case Study: Mr. Hanif Mulji, age 28 years, is found in a coma in his hospital room. There was a strong odour of acetone on his breath. He is married, climbs mountains, and is a triathlete. Previous health records do not reveal that Mr. Mulji had diabetes mellitus. Emergency measures are instituted immediately. Questions 314 and 315 314. A nursing intervention that should be included in the plan of care for Mr. Mulji is: A. Withholding glucose in any from until the ketoacidosis is corrected. B. Observing for signs of hypoglycemia as a result of treatment. C. Giving fruit juices, broth, and milk as soon as he is able to take fluids orally. D. Regulating insulin dosage according to the amount of ketones found in the urine. 315. Important to both Mr. Mulji and his wife. Salima, is an undemanding that a diabetic diet: A. Is based on nutritional requirements that are the same for all clients. B. Can be planned around a wide variety of commonly available foods. C. Should be rigidly controlled to avoid similar diabetic emergencies. D. Must not include processed foods because they have too many variable seasonings. Case Study: Melanie, a 22-year-ofd college student, is admitted to the hospital for diabetic acidosis. Questions 316 to 318 316. After blood work end observation of urinary volume, the physician orders 20 mEq of potassium chloride to be added to the IV solution. The primary purpose for administering this drug to Melanie is: A. Replacement of potassium deficit. B. Treatment of hypercapnia. C. Prevention of flaccid paralysis. D. Treatment of cardiac dysrhythmias. 317. The nurse should recognize that Melanie needs fun he r teaching when, after reviewing the dietary exchange system. Melanie she states that: A. 1 scoop ice milk = I slice bread. B. 1 oz cheese = I cup milk. C. 1 egg = 1 oz meat. D. 1 slice bacon = 2 Tbsp cream. 318. Melanie's nursing care plan indicates that before discharge, she will know how to self-administer insulin, adjust the dosage, understand her diet, and perform glucose monitoring. She progresses well and is discharged 10 days after admission. Legally: A. The physician was responsible, and the nurse should have cleared the care with him or her. B. The nurse was properly functioning as a health teacher. C. The visiting nurse should do health teaching in the home. D. A family member should have also been taught to administer the insulin. 319. Early indications of lithium toxicity include: A. Torticollis. B. Tinnitus. C. Akathisia. D. Diarrhea. 320. Why is important for nurses to assess blood pressure in patients receiving antipsychotic drugs? A. Orthostatic hypotension is a common side effect. B. Most antipsychotic drugs cause elevated blood pressure. C. This provides additional support for the patient. D. It will indicate the need to institute antiparkinsonian drugs. 321, Alcohol withdrawal delirium is a medical emergency. Which of the following symptoms would alert the nurse to the potential for delirium tremors? A. Fever, hypertension, changes in level of, consciousness, and hallucinations. B. Hypertension, stupor, agitation, headache, and auditory hallucinations. C. Vomiting, ataxia, muscular rigidity, and tactile hallucinations. D. Coarse hand tremor, agitation, hallucinations, and hypertension. Case Study: Jane Bryant age 29 years, is involved in an automobile accident. She is brought to the emergency department with head trauma, bur she is awoke and able to speak. Questions 322 and 323 322. Which of the following questions would best assess her cerebral function? A. Can you tell me your address? B. How would you describe your eyesight? C. Have you noticed a change in you r coordination? D. Have you noticed a change in your muscle strength? 323. As the nurse, you assess the following change in Jane's status: Initially her pupils were equal; now the right pupil is fully dilated and nonreactive, and the left pupil is 4 mm and reacts to light. What would this suggest? A. Increased intracranial pres sure. B. Decreased intracranial pres sure. C. The test was not performed accurately. D. Normal response after a head injury. 324. The parents of a critically ill infant are practicing Roman Catholics. The nurse is aware that baptism is an important religious ritual. Which of the following is the best action for the nurse to take? A. Ask the hospital chaplain to baptize the baby. B. Ask the doctor to baptize the baby. C. Ask the parents what their wishes are regarding baptism. D. Do nothing because discussing baptism will make the parents mo re anxious. 325. A patient recovering from surgery in the hospital requests spiritual support from a parish nurse. A parish nurse is: A. A registered nurse who works in a community with religious organizations. B. Only concerned with how spirituality interacts with physical health. C. Someone who is called to the ministry to promote health. D. A nurse who believes faith and health are separate. 326. A 78-year-old woman has been discharged recently from the hospital after experiencing heart failure relating to long-standing hypertension and coronary artery disease. A community health nurse is evaluating her compliance with medication therapy. Which of the following factors best indicates that the client is complying with digoxin (Lanoxin) therapy? A. Her ability to correctly count her radial pulse. B. Her weight gain of 2 Ib in less than a week. C. An apical heart rate of 101 bpm. D. Absence of a pericardial friction rub. 327. The nurse is teaching a female client with osteoporosis about her prescribed diet. Which of the following foods is the best source of calcium? A. 1cup of low-fat yogurt. B. 1cu p of skim milk. C. 1 oz of cheddar cheese. D. 1 cup of ice cream. 328. A client is being discharged after successful same -day cataract surgery. The nurse instructs the client about permitted activities and those to avoid. Which of the following activities is permitted? A. Cooking. B. Driving. C. Vacuuming. D. Showering. 329. A client with chronic obstructive pulmonary disease (COPD) is being discharged after treatment for an acute exacerbation. Which statement by the client indicates proper under standing of the discharge instructions? A. "I should take my bronchodilator at bedtime to prevent insomnia.” B. “I should do my most difficult activities when I first get up in the morning." C. “I should try to eat several small meals during the day.” D. “I should plan to do my exercises alter I eat.” 330. Which aging characteristic increases the risk of falls in elderly individuals? A. Forward- flexed posture. B. Decreased ability to ad apt. C. Inability to take responsibility. D. Increased reaction time. 331. Many falls in older adults are related to: A. Tripping. B. Wearing slippers. C. The urge to urinate. D. Barriers between the bed and bathroom. 332. A 63-year-old female client has a 10-yea r history of rheumatoid arthritis. Her 40-year-old daughter has recently noticed that she herself wakes up with stiff joints. The client shares her concerns regarding her daughter with you. What would be the most appropriate response? A. Explain that rheumatoid arthritis doe s not have a genetic basis, so there is nothing fur her to be concerned about. B. Tell her that the re is some evidence that a genetic basis for the disease may exist and suggest that the daughter be evaluated. C. Have her suggest that her daughter take aspirin for a few days to see if the stiffness is relieved. D. Reassure her that it is normal for a 40-year-old woman to have aches and pains and that her concern is probably unwarranted. 333. A plan of care for a client with osteoporosis includes active and passive exercises, calcium supplements, and daily vitamins. The de sired effect of therapy would be noted by the nurse if the client: A. Had fewer bruises than on admission. B. Developed an increase in her mobility. C. Developed fewer cardiac irregularities. D. Developed fewer muscular spasms. 334. A community health nurse visits an older adult client whose husband has recently passed away. The client says, "No one cares about me anymore.” All the people I loved are dead." Which of the following responses by the nurse conveys therapeutic communication? A. "That seems rather unlikely to me." B. "You must be feeling lonely at this time." C. "I don't believe that, and neither do you." D. "That's true. Why don't you just give up?" 335. Mrs. McDonald, an 84-yea r-old widow, has been diagnosed with metastatic melanoma and is admitted for hospice care, The nurse caring for Mrs. MacDonald knows that clients in the initial stage of accepting the diagnosis of terminal illness often: A. Ask for other medical opinions. B. Cry uncontrollably over the diagnosis. C. Criticize medical care received. D. Isolate themselves and refuse visitors. 336. A male client, age 78 years, has recently been diagnosed with hypothyroidism. He lives in his own apartment in a community facility designed for elderly people. He asks the nurse assigned to the complex for advice about his condition. What would be the best advice the nurse could give this client? A. "Stop taking your prescribed daily aspirin." B. "Stop attending your group activities." C. "Increase your daily caloric consumption." D. "Increase fibre and fluids in your diet." 337. Which clinical signs would indicate to a nurse caring for a terminally ill patient that death may be imminent? A. Cold, clammy skin and irregular, noisy breathing. B. Apnea and a body temperature of 37 °C. C. Swallowing reflex and bowel sounds present. D. Respirations regular at 18 breaths/min and pedal pulse present. 338. When a disaster occurs, the nurse may have to treat mass hysteria first. The person or persons to be cared for immediately would be those in which of the following states? A. Depressive, B. Euphoric. C. Panic. D. Comatose. 339. In any disaster concerning a number of people, the function that contributes most to saving lives is triage. When determining the priority of needs, the people who need immediate care are those with: A. A second-degree burn covering 10% of the body. B. Severe lacerations involving open fractures of major bones. C. Closed fracture s of major bones. D. Pain from whiplash and soft tissue injuries. 340. Then: has just been a z 25-vehicle collision in your community. You are the first on the scene. From the options below, who would require immediate care? A. Those with severe head injuries. B. Those with multiple fractures. C. Those with minor bleeding. D. Those with cont rolled severe bleeding. 341. A client is placed on home oxygen therapy using a nasal cannula at 2 L/min and an oxygen concentrator. The client expresses a fear of using oxygen at home, stating, "I just know it will blow up." What is the nurse's best response? A. "You have nothing to worry about. That never happens anymore.” B. "I would like to further discuss your concerns about this. What have you heard about using oxygen at home?" C. "I've brought information that I want you to read. After you go through it, you'll see that you don't have anything to worry about. " D. "Thousands of people use oxygen therapy safely in their homes every day." 342. A female client is discharged from the hospital after having an exacerbation of congestive heart failure. She is prescribed a daily oral doses furosemide (Lasix). Two days later, she tells her community health nurse that she feels weak and frequently feels her heart "flutter." What would be the nurse's priority action? A. Call the physician and tell the client to rest more often to decrease her symptoms. B. Tell the client to stop taking the digoxin, call the physician, and have the client stop all physical activity. C. Call the physician; report the symptoms: and upon the physician's order, send a blood sample to the laboratory to determine the client's potassium level. D. Give firm and clear instructions about avoiding foods that contain caffeine. 343. A nurse is teaching a client about the use of a respiratory inhaler. Which of the following would not be a component of the teaching plan? A. Remove the cap and shake the inhaler well before use. B. Press the canister down with your finger as you breathe in. C. Inhale the mist and quickly exhale. D. Wait I minute between puffs if more than I puff has been prescribed. 344. Mr. Tse has been recently diagnosed with kidney failure. A fluid restriction order of 1000 mL q24h is in effect. Knowing this, the nurse caring for Mr. Tse should: A. Eliminate all liquids between meal times. B. Divide fluids equally over three nursing shifts. C. Indicate just clear liquids in the restriction plan. D. Proportion more fluids during the day than during the night. 345. The nurse should provide a confused client with an environment that is: A. Challenging. B. Nonstimulating. C. Variable. D. Familiar. 346. Mr. Jones, age 78 years, has Parkinson's disease. He slept very poorly last night was nauseated when he got up this morning, and feels weak and tired . He ate a small portion of his breakfast. He is scheduled to go down to physiotherapy in 1 hour. What action should the nurse take? A. Give him an antiemetic to reduce the nausea and get him up and dressed to go to physiotherapy. B. Assess his nausea and sleep interferences; call physiotherapy to cancel or reschedule his appointment. C. Notify the dietician to change his diet to clear fluids; cancel physiotherapy until his strength resumes, D. Ask the dietician to visit with him regarding food preferences and recommend that the doctor order sleeping pills for him. Case Study: Jennifer Hall, age 43 years, has been admitted for a left mastectomy after confirmation of cancer from the biopsy report. She has a daughter who is 12 years old, Questions 347 to 351 347. Communication is very important when preparing Jennifer for the mastectomy. What are important issues to discuss with her? A. How body image changes will affect her sexual relationship. B. Concerns regarding the cancer and how the surgery will affect her, C. Impact of surgery on the family's coping abilities. D. History of breast cancer in the family. 348. Jennifer states that he r husband has been very supportive but says. "I've been a basket case just thinking of what implications this has for us as a family.” How would you respond? A. "Sounds like you are still in denial about the diagnosis.” B. “This is a very difficult adjustment period for you and your family. “ C. "You need to talk to someone who has gone through this same experience.” D. "Let's discuss this problem with your husband and daughter.” 349. What would you include in Jennifer's preoperative teaching before a mastectomy? A. Informing her regarding a Hemovac, pressure dressing, and deep breathing exercises. B. Explaining that a catheter will be inserted and removed on the first postoperative day. C. Informing her that she will not be allowed food or fluids for the first 2 day. D. Explaining that she will have minimal effects from the anaesthetic because the surgery is superficial and quick. 350. Jennifer's husband has arrived to be with her before her surgery. When she leaves for the operating room, what would you tell her husband? A. Encourage him to go to work and come back later in the evening when the anaesthetic effects are gone. B. Inform him that he can see her as soon as she comes out of the operating room. C. Inform him that she will be going to the recovery room after the operation; they will notify the unit when she is ready to come back, D. Take this opportunity to discuss the concerns she expressed regarding the implications this has for her family. 351. When Jennifer returns from the recovery room, which of the following is not included in the initial postoperative assessment? A. Assessing the vital signs and oxygen saturation levels. B. Checking the dressing, drain, and amount of drainage C. Checking the neurologic responses and level of pain D. Checking-for urinary retention and the need to void. 352. Mr. Gupta, age 44 years, is admitted to the hospital. His religious beliefs require that he meditate and pray several times every day. He tells the nurse he is uncomfortable praying in his semi-private room. How would the nurse respond? A. "It's unfortunate you feel uncomfortable. Could you pull the drapes around your bed for privacy?" B. "I'm sure this is difficult for you; I'll see when a private room may become available," C. "I can see you're concerned about this. I could arrange a private place for you to pray. " D. "I'm sorry for you r discomfort. Could I call the hospital chaplain to assist you?" 353. Mrs. Li is receiving chemotherapy through a central venous catheter into her right subclavian vein. The nurse observes that she is dyspneic and cyanotic; her blood pressure has dropped to 86/48 mm Hg and she has a weak, rapid pulse. Mrs. Li is complaining of pain in her chest and shoulder. What complication would the nurse suspect? A. Circulatory overload. B. Air embolism. C. Infection. D. Infiltration. 354. You are caring for a patient who has returned from the operating room after an exploratory laparotomy. He has an IV infusion at 150 cc/hr. He has not voided for 8 hours. Postoperative orders read: "Catheterize prn. Conservative measures to stimulate voiding have not been successful." What assessments and anions would you take? A. Palpate all four abdominal quadrants and assess his intake and output record. B. Inspect and palpate the lower abdomen; if it is distended and uncomfortable. Insert a straight catheter. C. Give him pain medication and catheterize him as soon as possible to lessen the possibility of a bladder and kidney infection. D. Wait until the patient experiences considerable discomfort in the bladder region and then catheterize. 355. Identify four criteria for evaluating nursing research information on the Internet. (4 points) Answer: • The publication source is trustworthy. • The author is reputable and has clinical credibility. • The research evidence has a methodology and references. • The publication has a clear layout. • It is easy to use and has a logical representation. • The information has purpose and suitability and is current. Rationale: All of the above are criteria that must be considered when evaluating nursing research posted on the Internet. 356. Define nursing informatics. (1 point) 357. Describe how a nurse could implement informatics into the work setting. (I point) 358. Identify two objectives for standardized interdisciplinary electronic documentation. (2 points) 359. As the nurse, you are conducting therapeutic range of motion exercises on your client. Identify the purposes of passive, active, and resistive range of motion exercises. (3 points) 360. A nurse is planning care for a client who is depressed and may be suicidal. Identify two signs that would indicate that a client is suicidal. (2 points) 361. A home care nurse visits a client. The client tells the nurse that the physician told him to take ibuprofen 0.4 g for mild pain. The medication bottle states ibuprofen is available in 200-mg tablets. In planning the pain medications for the client, how many tablets should the nurse tell the client to take? (I point) 362. Identify and briefly descry be three outcomes you would observe in a patient who has adapted to having an ostomy. (3 points) 363. If the patient's postoperative pain is not controlled, the risk for pressure ulcer development increases because pain will limit the patient's ability to change position frequently. What actions should the nurse take to reduce the risk for pressure ulcer development? (1 point) 364. A physician orders an IV solution of 1000 mL of D5W to be administered at 100 mL/hr. The drop factor of the IV administration set is 15 drops/hr. How many drops per minute should the patient receive? (1 point) 365. Identify three criteria for consent for surgery to be valid. (3 points) 366. Identify and briefly describe two reasons why repositioning a patient every 2 hours increases both circulation and respiration. (2 points) 367. Identify two reasons why body flu id losses may exceed fluid intake. (2 points) 368. Describe one characteristic of a healthy stoma. (1 point) Case Study: Mrs. Marge Evenrude, age 88 years, is admitted to the unit from the emergency department after having a cerebrovascular accident (CVA) affecting the right side of her body. She is aphasic and chokes when taking fluids. Her daughter was at her home and witnessed the CVA 2 hours ago. The doctor has ordered IV tissue plasminogen activator (TPA) to be given. Questions 369 to 370 369. Describe two measures you would take to enhance communication with Mrs. Evenrude. (2 points) 370. Identify two health team members and their role in the rehabilitation of Mrs. Evenrude. (2 points) 371. Describe one characteristic of a necrotic stoma. (1 point) 372. Identify three complications of endotracheal suctioning. (3 points) 373. Describe the purpose of antiembolism stockings. (1 point) 374. Joint mobility is limited by ligaments, muscles, and the nature of the joint. Describe three joint movements used in range of motion exercises. (3 points) 375. Identify two precautions taken to prevent dislodgement or disconnect ion of a central line. (2 points) 376. Describe the purpose of postural drainage. (1 point) 377. A stage II pressure ulcer is partial-thickness skin loss involving the epidermis or dermis. Describe two observations of a stage II pressure ulcer and identify the treatment objectives. (2 points) 378. Explain the three phases of wound healing. (3 points) 379. A tornado has just hit your community. Reports indicate that many people are dead and approximately 500 people are injured. As an RN, you are helping to provide round-the clock first aid services. What is your plan of action? (1 point) 380. Describe the difference between multi-trauma and multiple casualties. (2 points) 381. Provide two suggestions that can help a client regain control of urinary incontinence. (2 points) 382. Identify three vascular structures (veins) used for central venous access. (3 points) 383. Some medical conditions may create complications when inserting a venous device. Identify two such conditions. (2 points) 384. Describe two purposes of closed chest drainage. (2 points) 385. Describe three considerations a nurse must make before administering a nasogastric (NG) tube feeding. (3 points) 386. Identify three reasons a physician may order insertion of a tube. (3 points) 387. ldentify two priority nursing actions that must be taken before infusing blood products. (2 points) 388. What type of blood transfusion is Mr. Ramsay most likely to receive? (1 point) 389. Describe the causes, signs and symptoms, prevention, and treatment of hyperglycemia. (3 points) 390. Describe the causes, symptoms, and prevention. and treatment of hypoglycemia. (3 points) 391. Identify when central line catheters are more effective in the de livery of medications and solutions than peripherally placed catheters. (1 point) 392. Identify one bacterial respiratory infection spread by droplet and one viral infection spread by droplet transmission. (2 points) Case Study: Mr. Lechelt comes to the hospital for open heart surgery. After 3 days, he is diagnosed with an antibiotic-resistant organism. Questions 393 and 394 393. When caring for Mr. Lechelt, the nurse should adhere to good hand washing techniques. Hand washing is one example of universal standard precautions. Describe two other examples. (2 points) 394. Even though the nurse caring for Mr. Lechelt is wearing gloves, she washes her hands after removing the gloves. What is the reason she adheres to this routine? (1 point) 395. A nurse not ices that a patient's creatinine kinase (CK) levels are markedly elevated. What is a normal range for CK? (1 point) 396. How man y hours after a cardiac infarction occurs might creatinine kinase levels increase? (1 point) 397. Identify two contraindications for administration of thrombolytic therapy. (2 points) 398. Describe two key causes of hyponatremia. (2 points) 399. Identify two vasoactive medications used to treat patients in shock. (2 points) 400. Which two laboratory results would indicate respiratory acidosis? (2 point) 401. Identify and briefly describe three health promotion strategies nurses could implement to assist clients diagnosed with chronic illnesses. (1 points) 402. Describe one way a patient may exhibit that he or she is working through the grieving process. (1 point) [Show More]
Last updated: 1 year ago
Preview 1 out of 129 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 29, 2020
Number of pages
129
Written in
Additional information
This document has been written for:
Uploaded
Apr 29, 2020
Downloads
0
Views
58

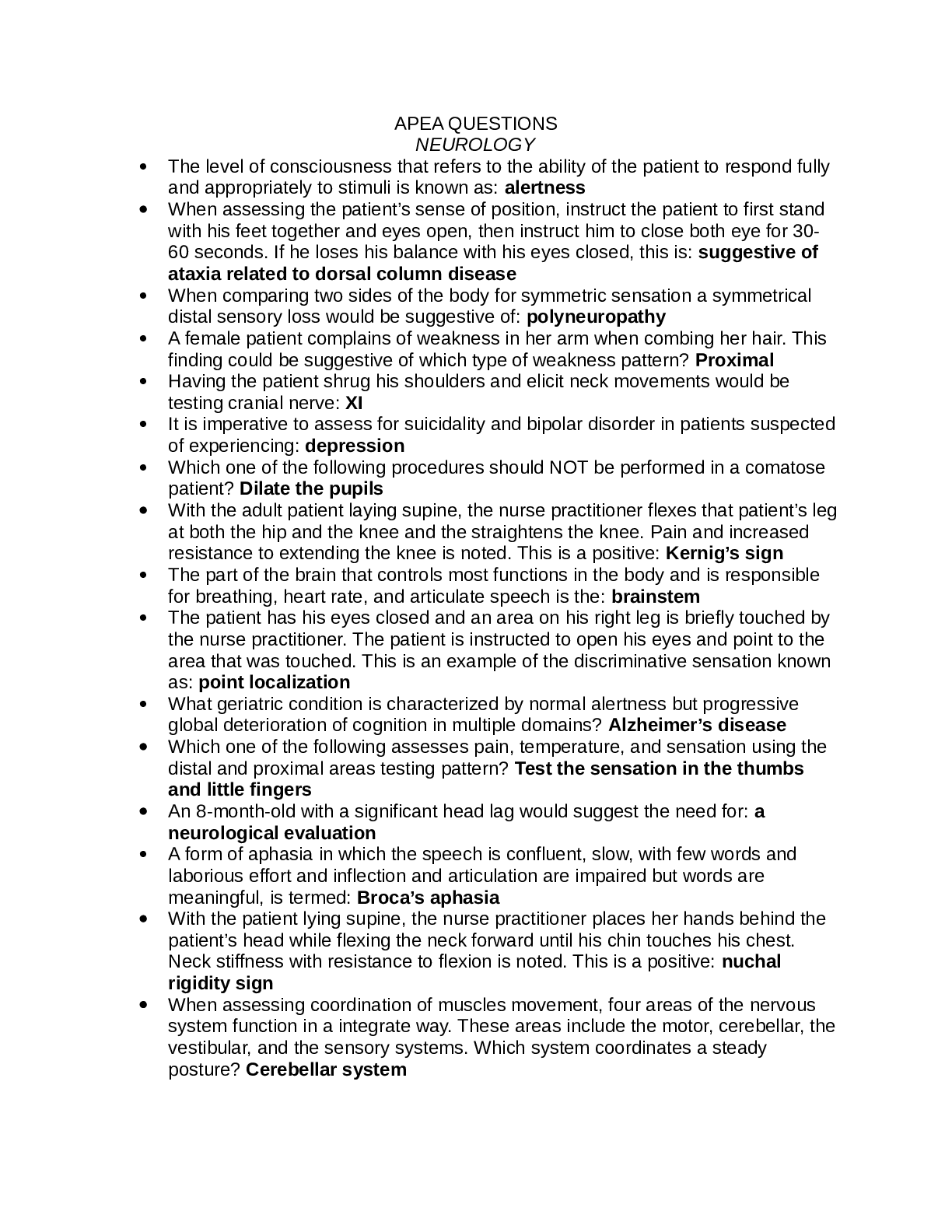
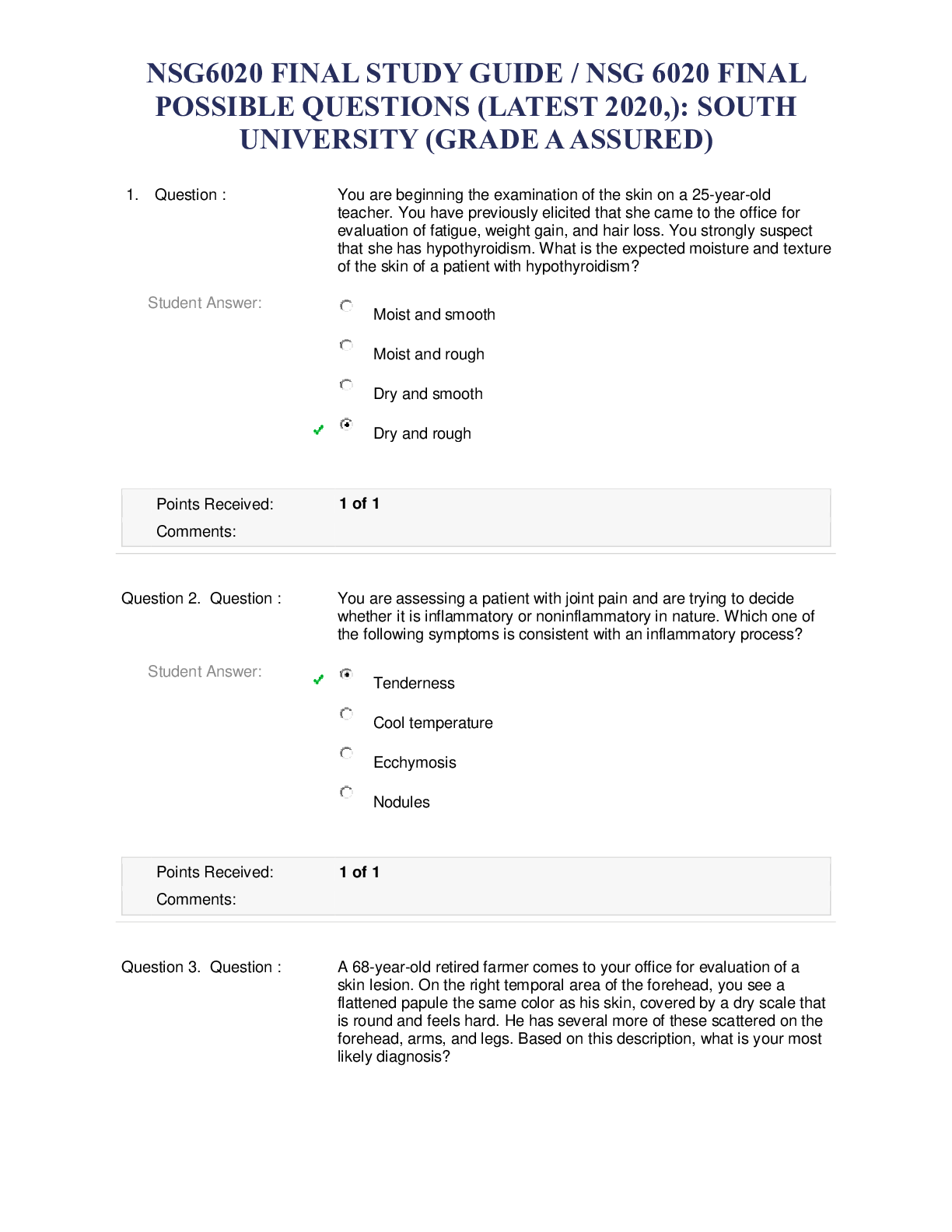
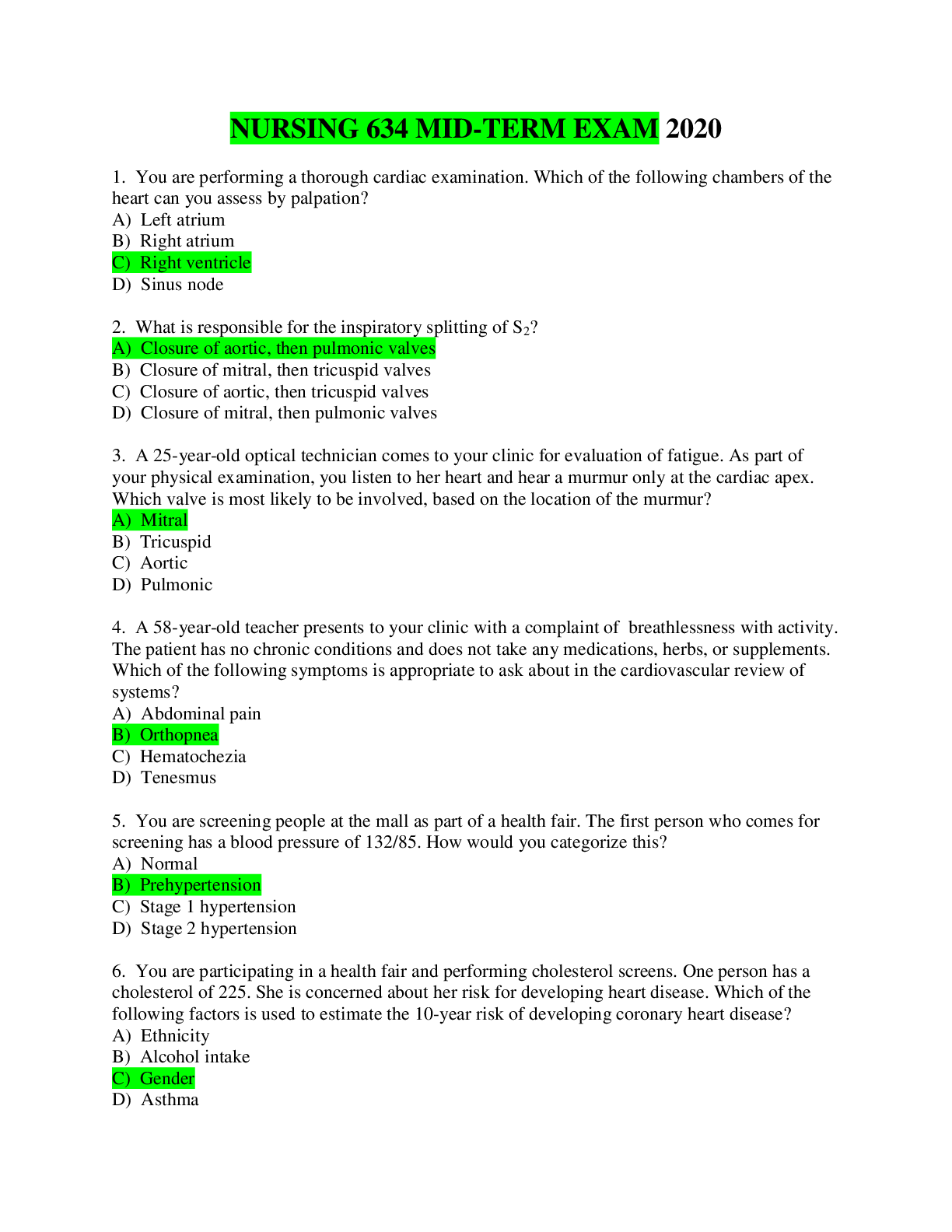
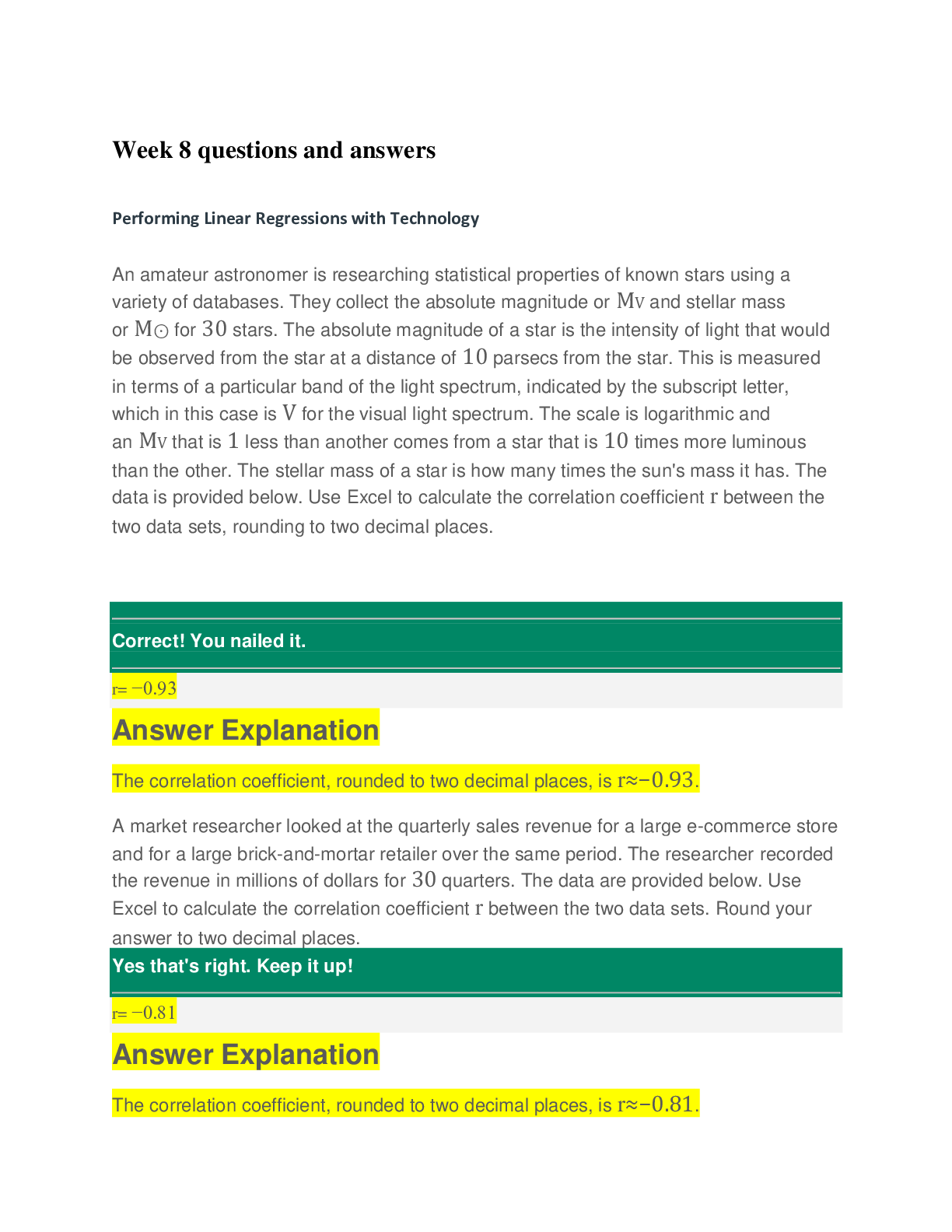
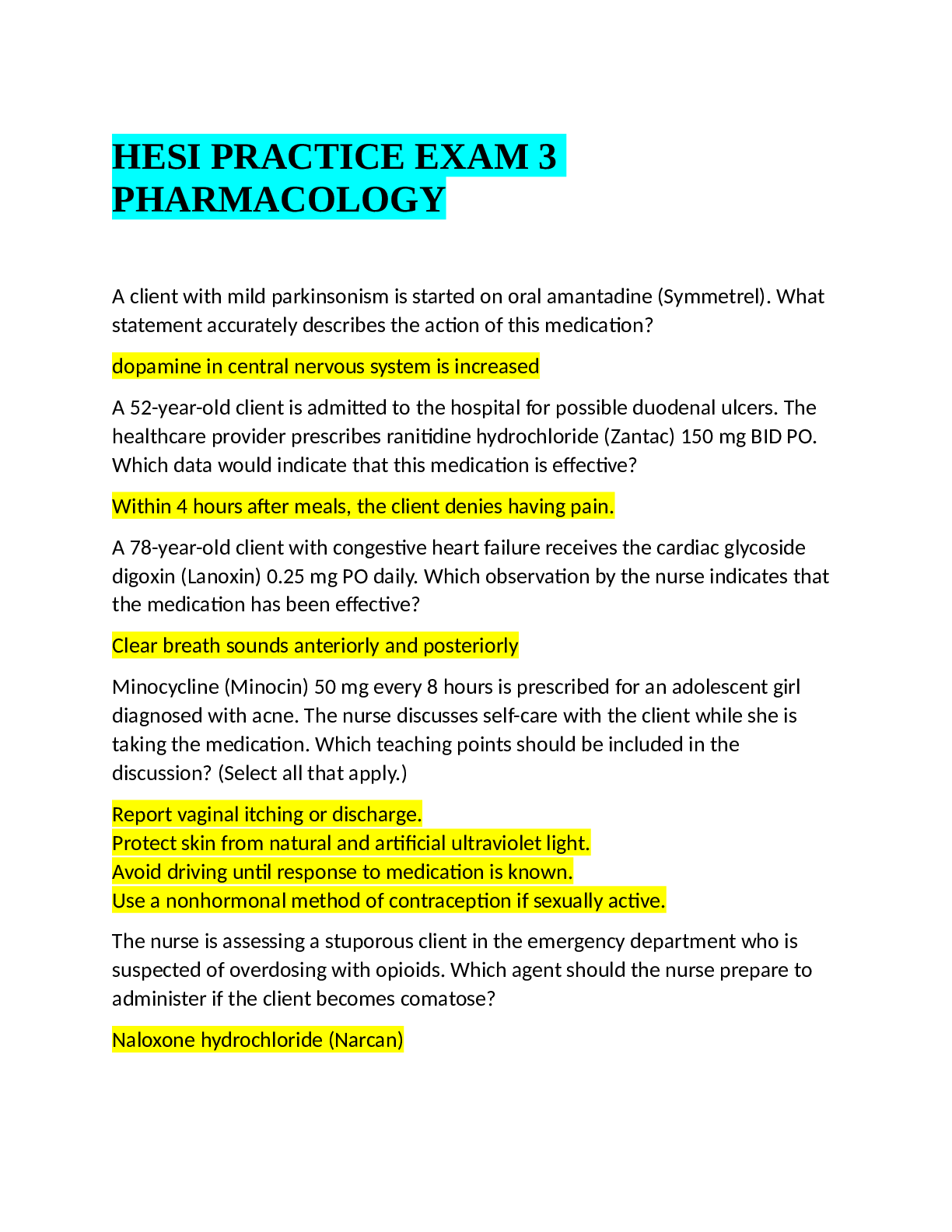


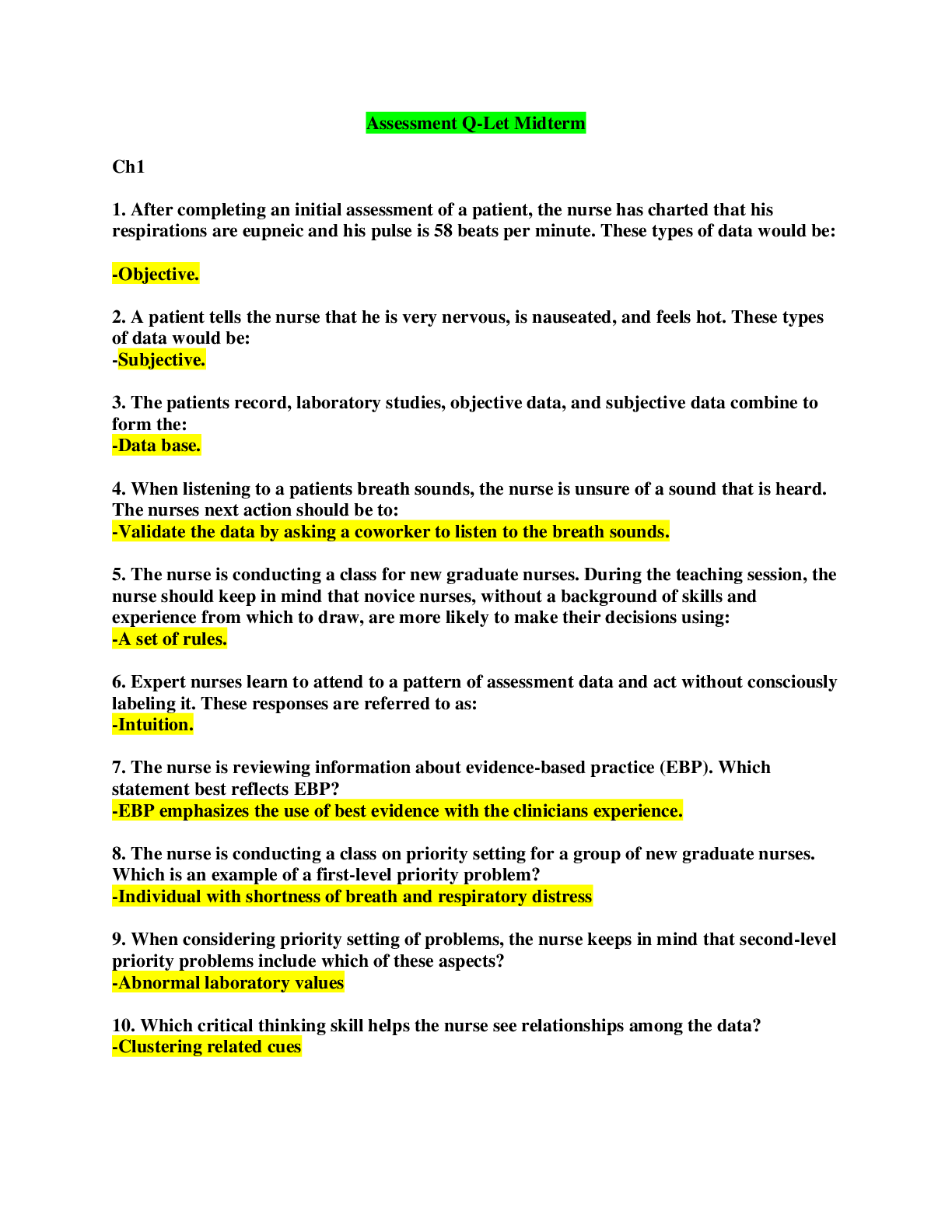
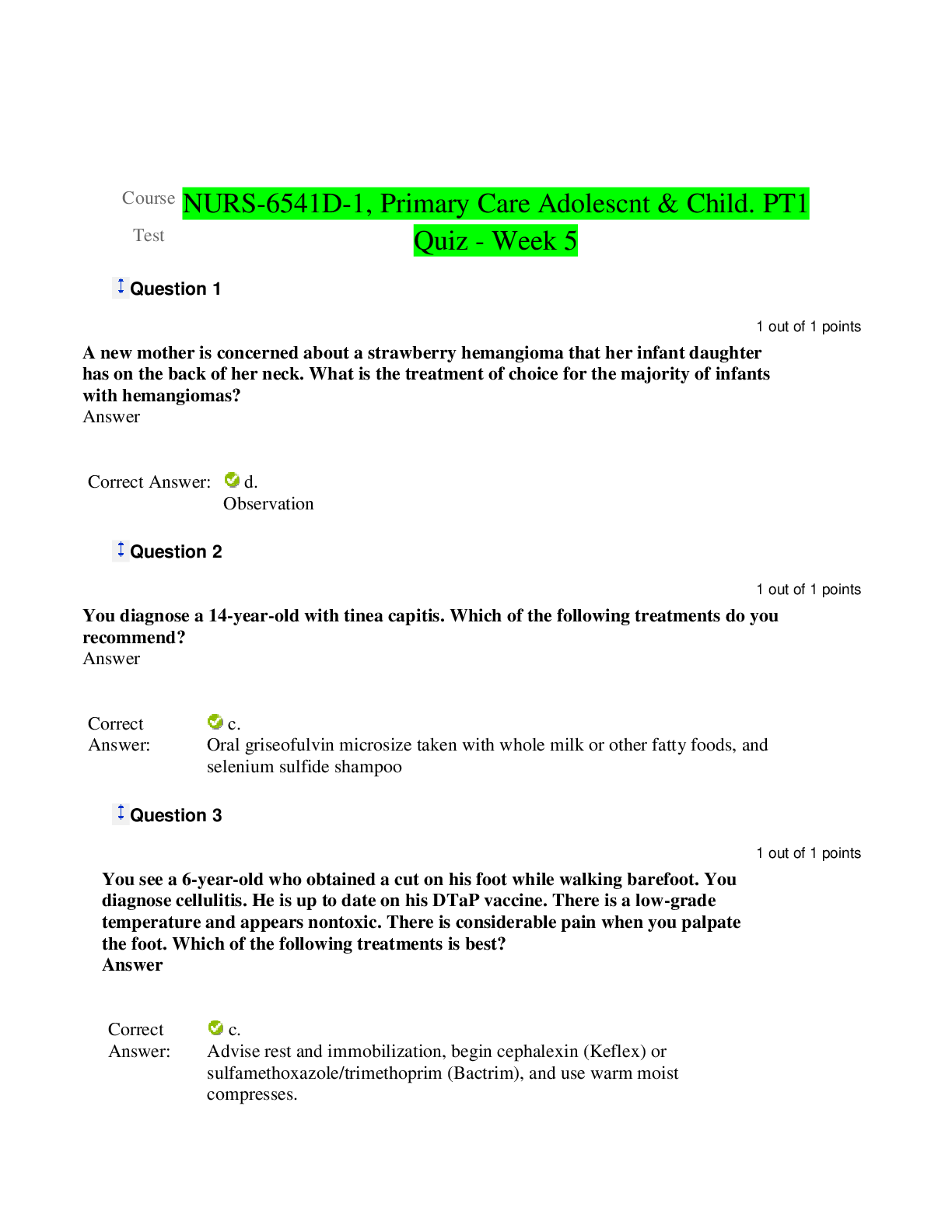
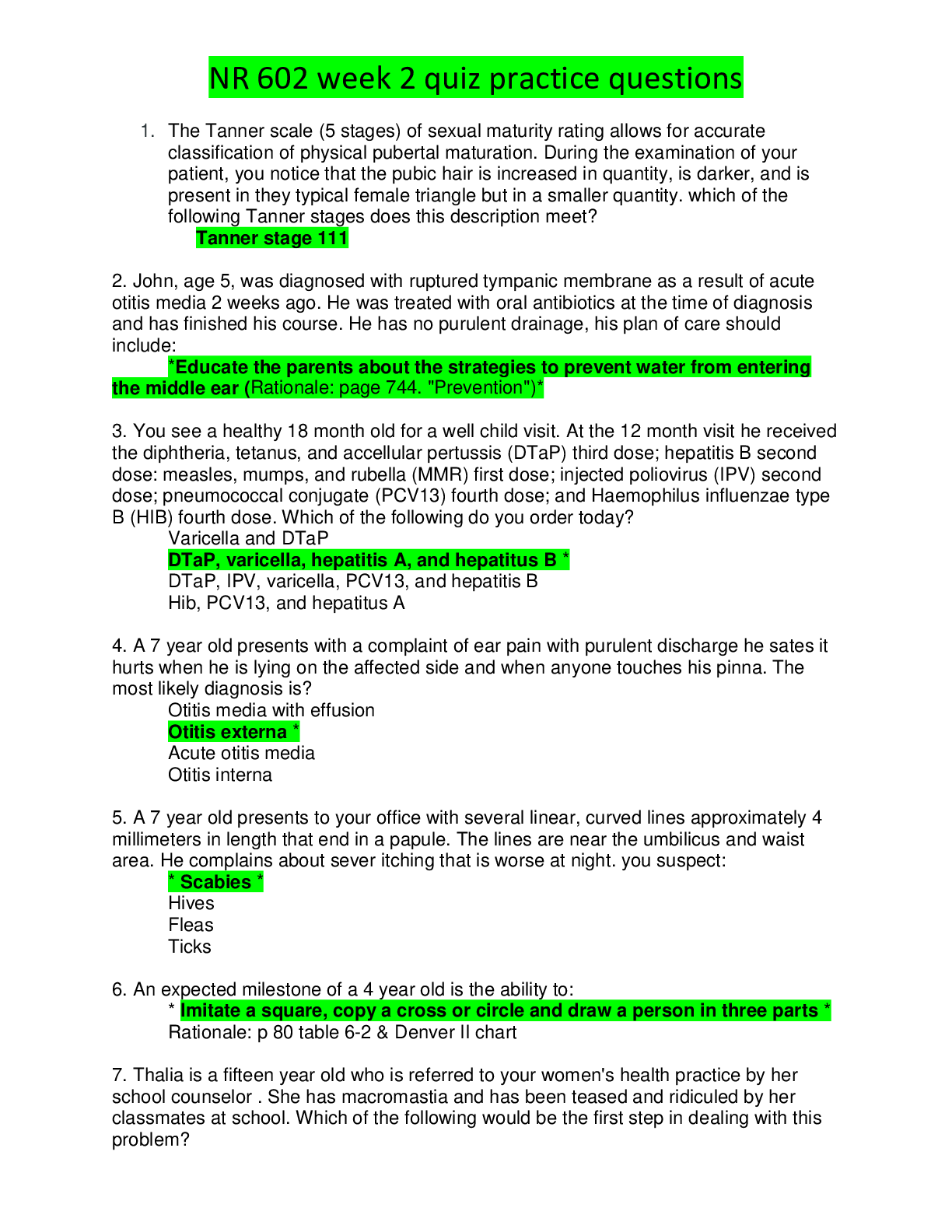
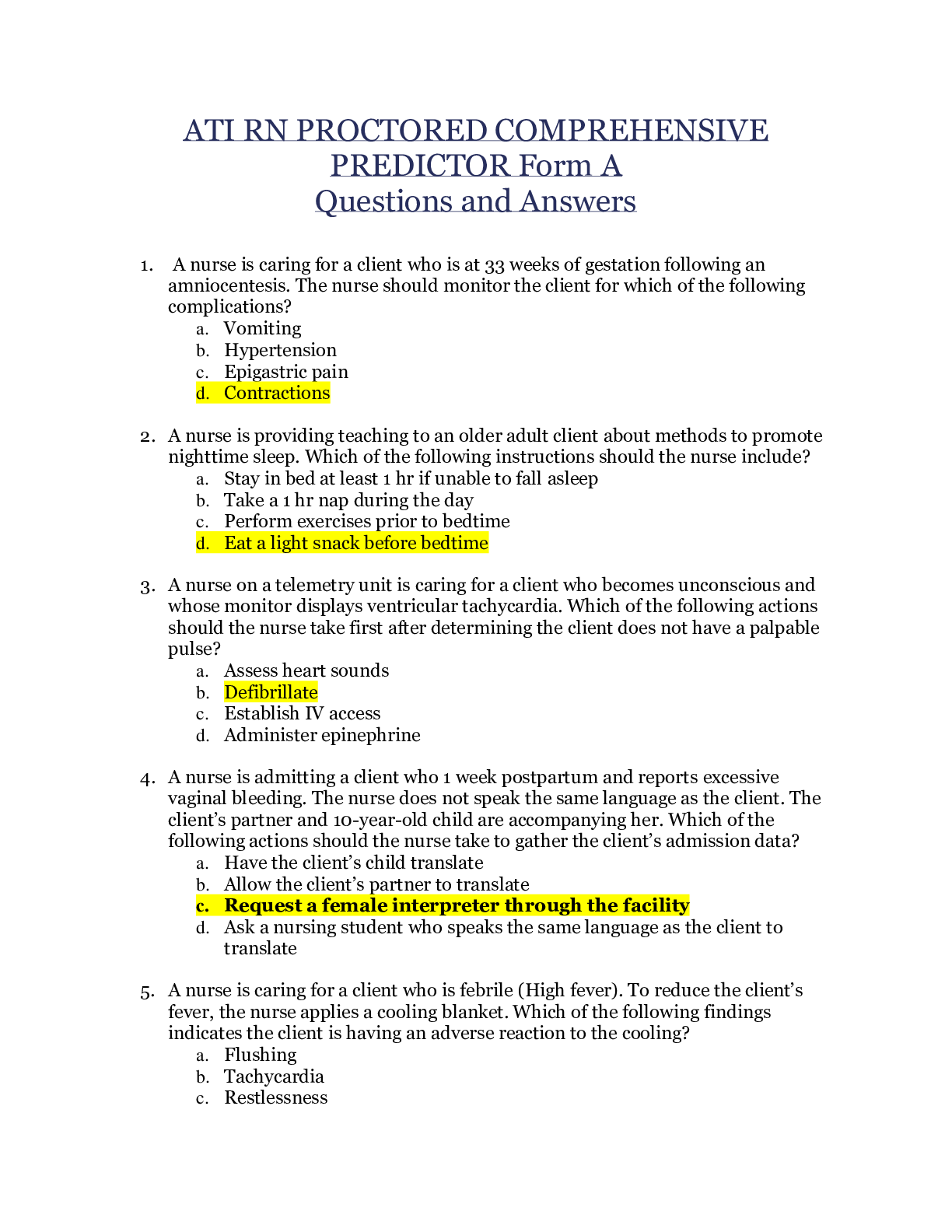
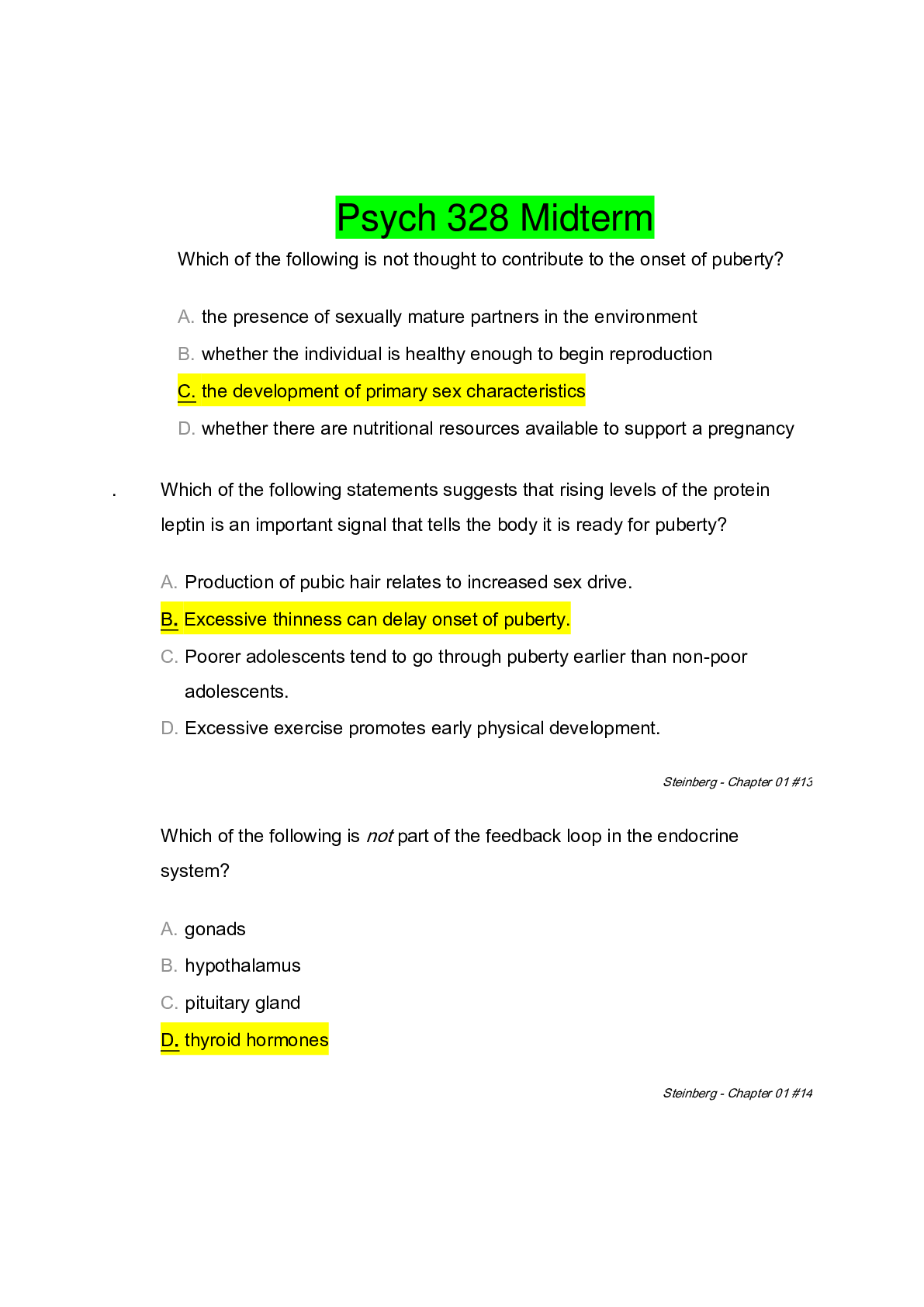
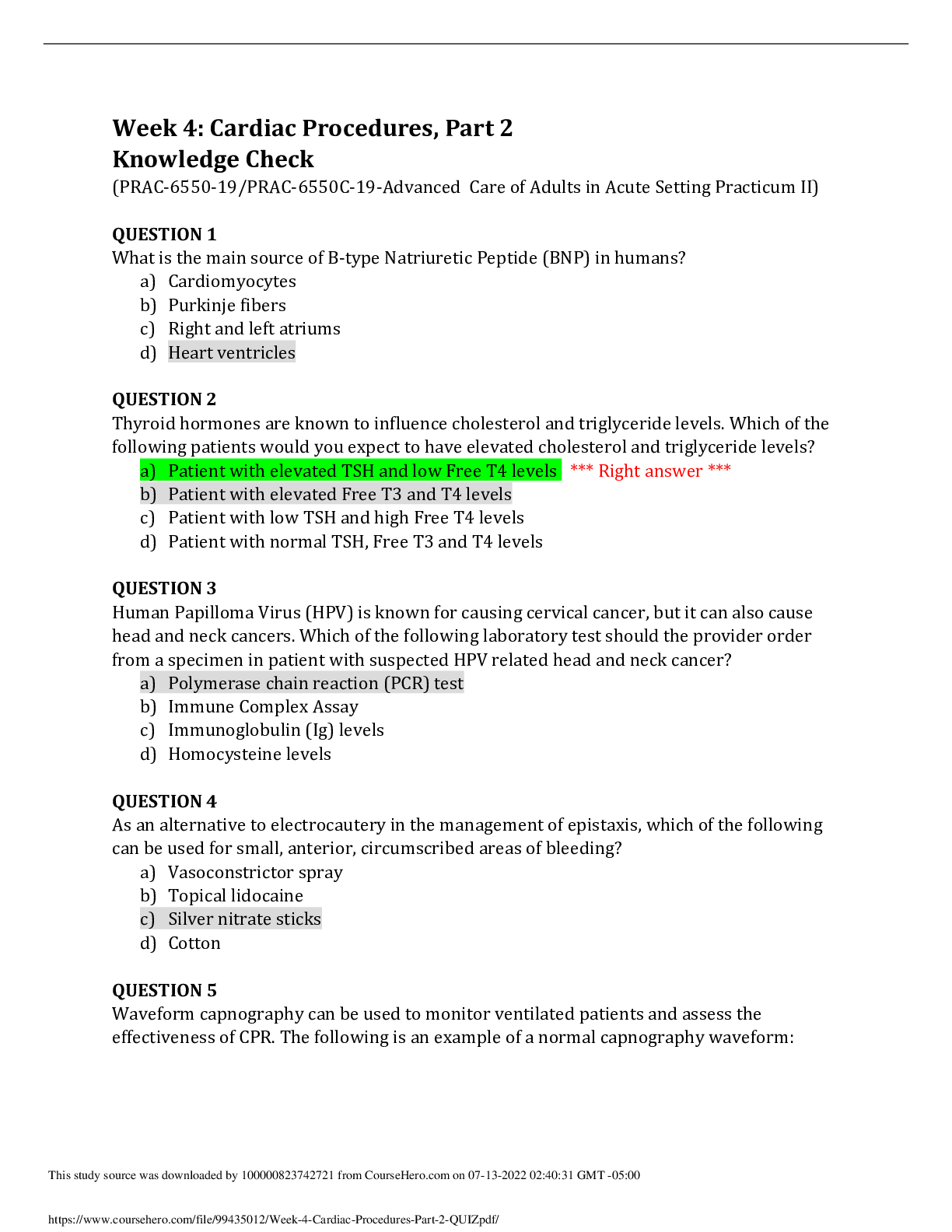
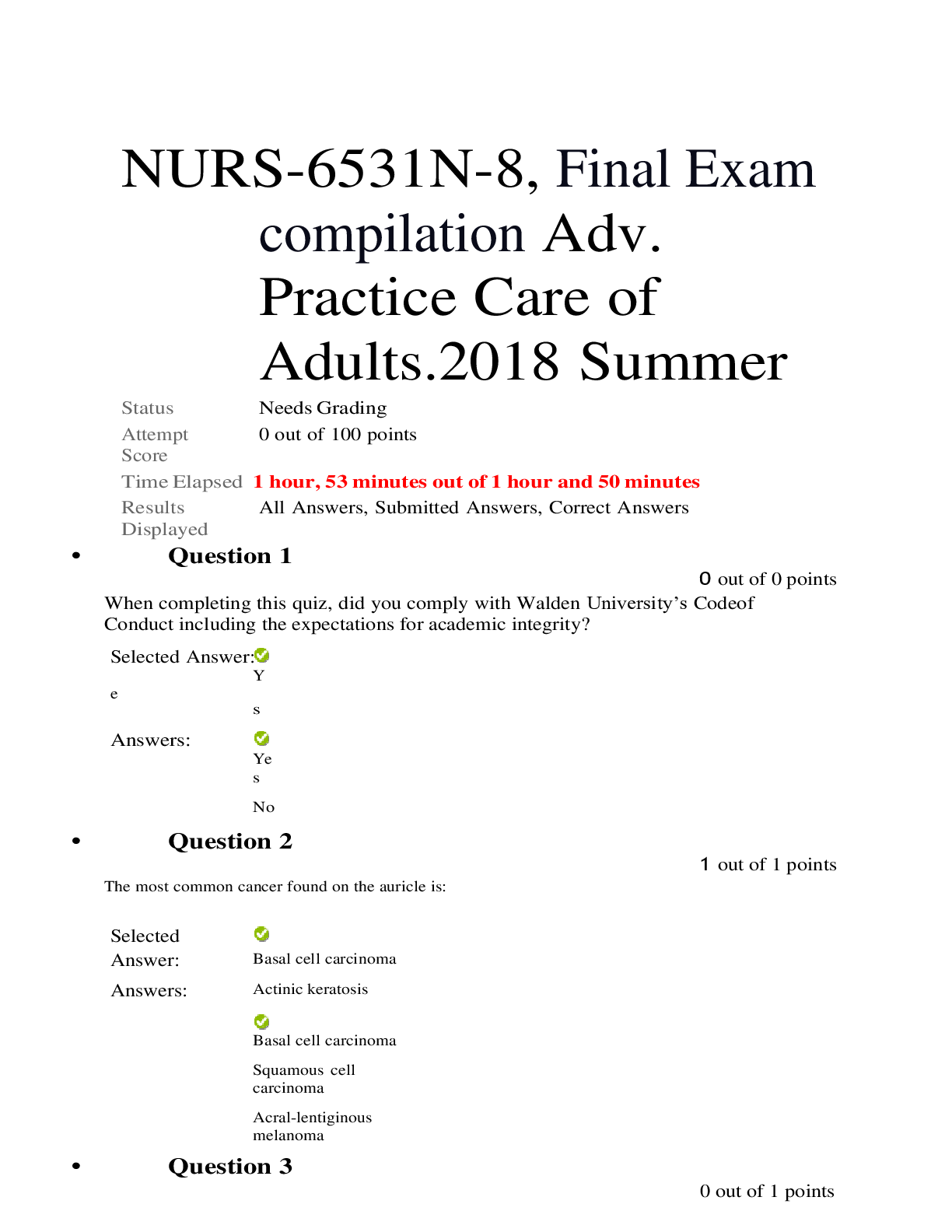
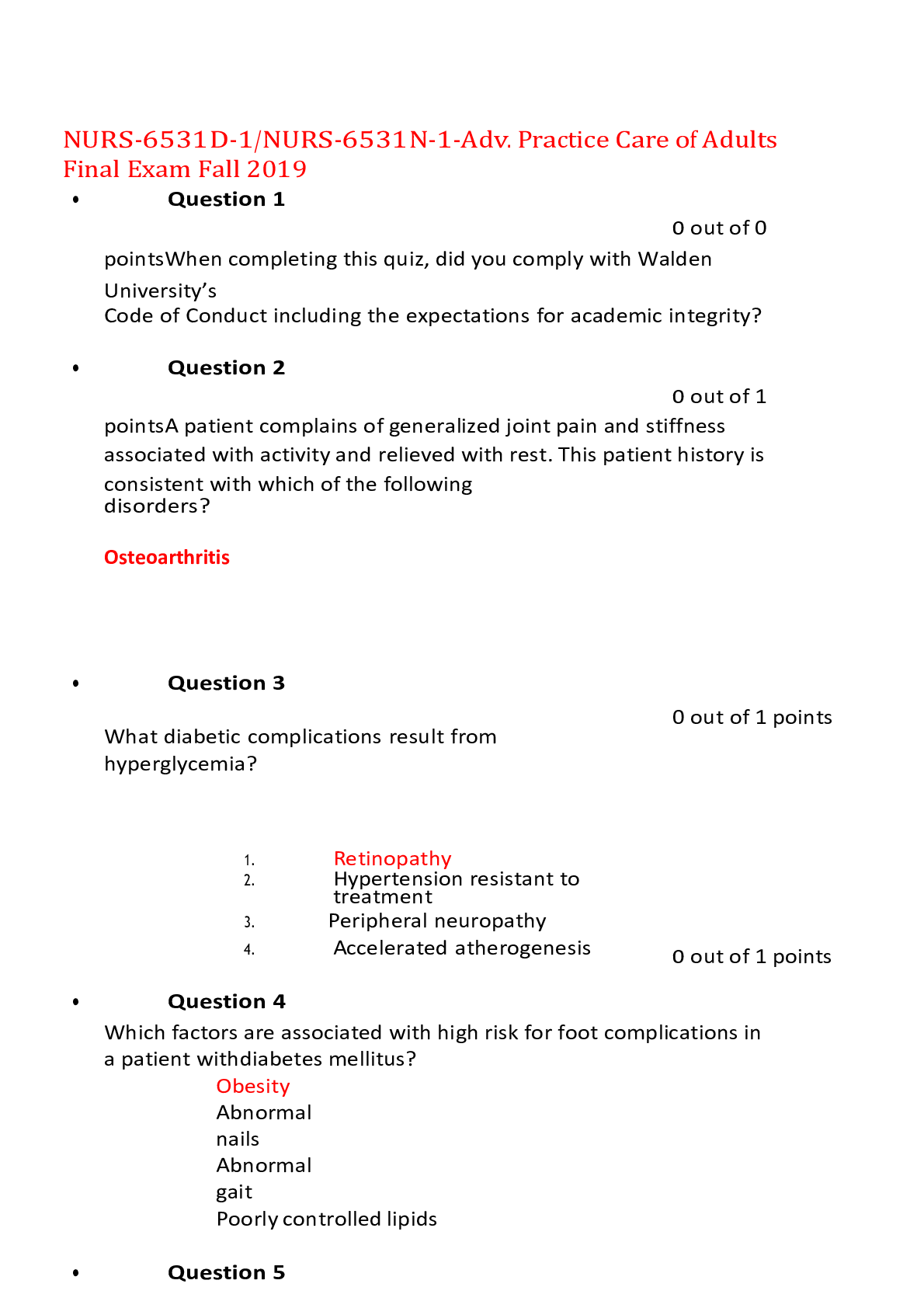
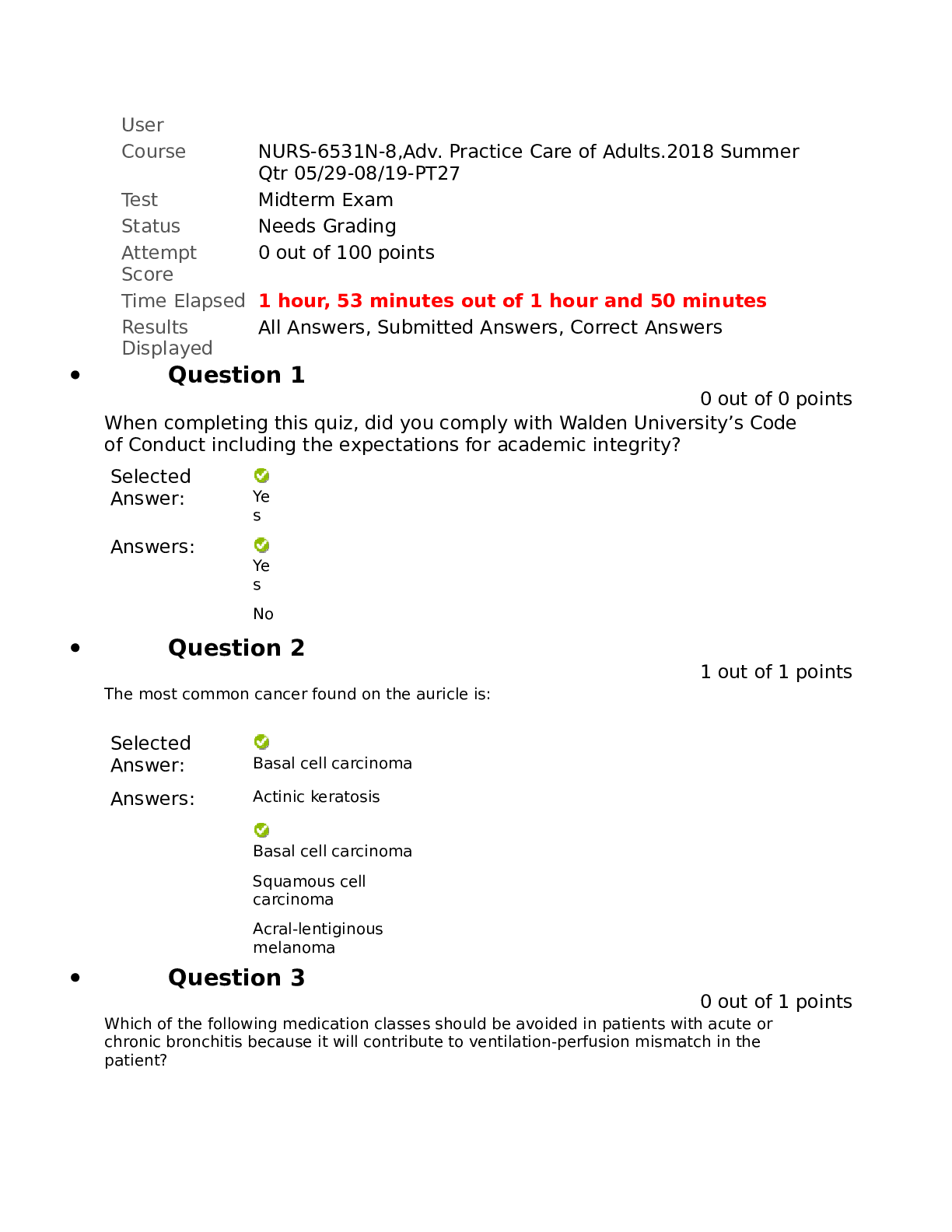
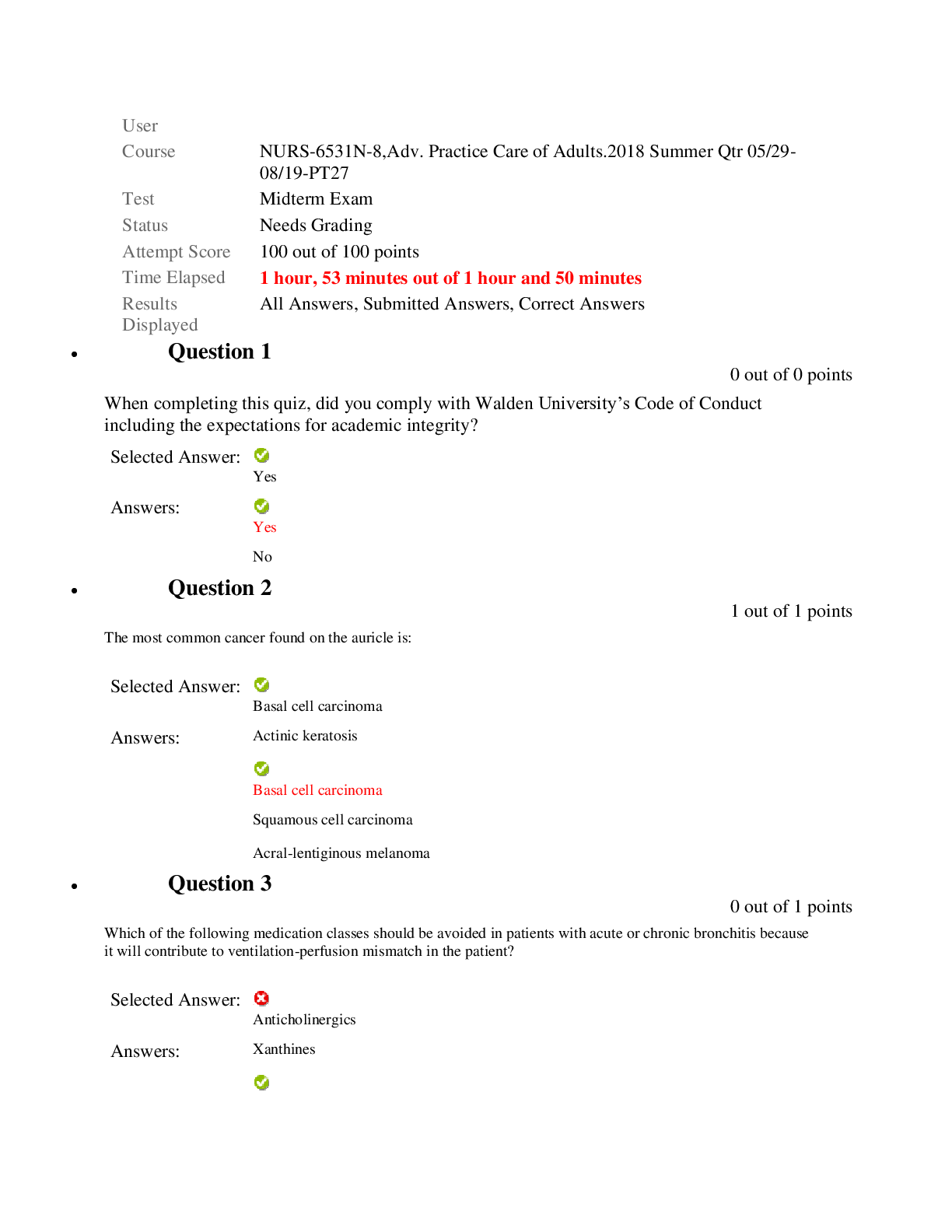
 Correct Study Guide, Download to Score A.png)
.png)



.png)
.png)

