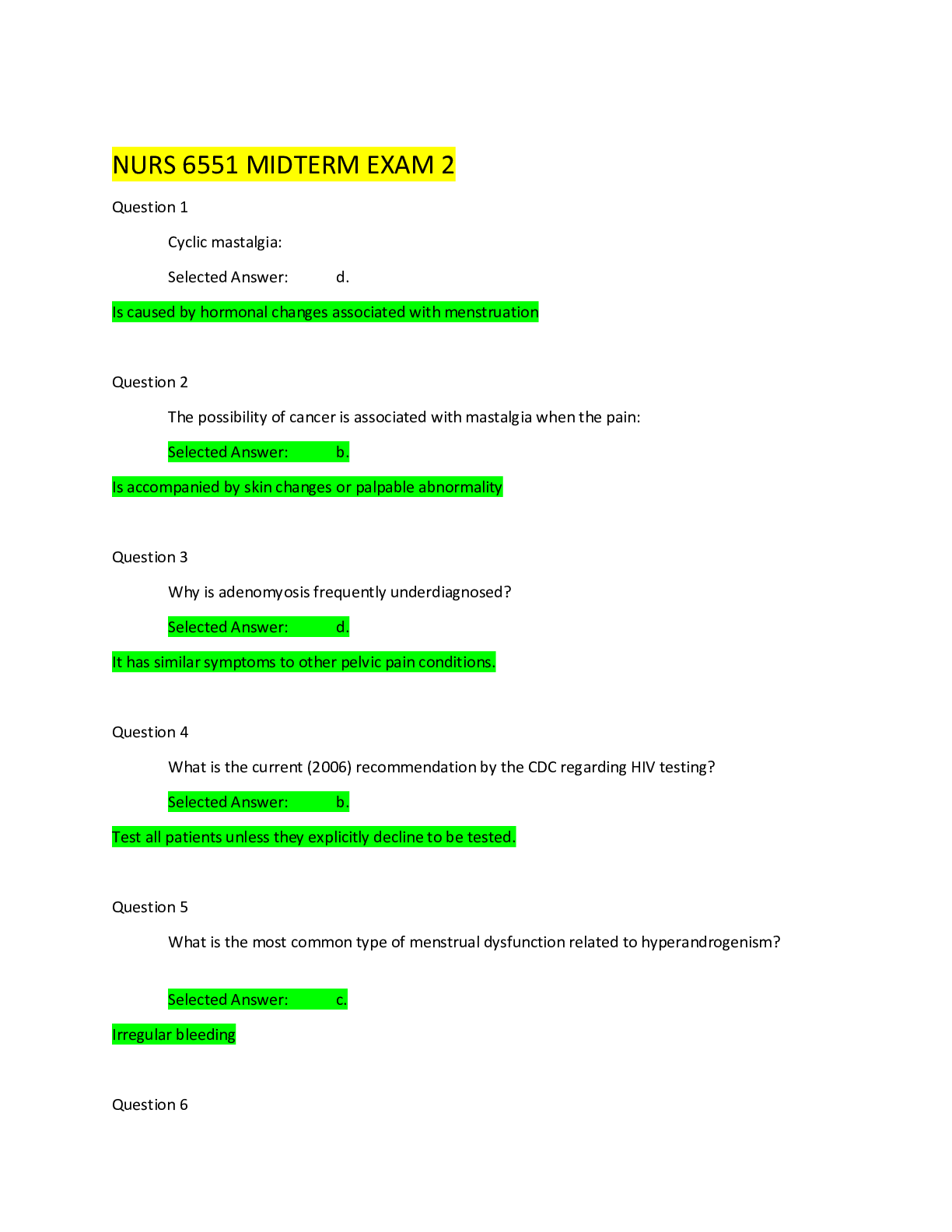
*NURSING > EXAM > NUR2633 Exam 2 Focused Review / MCH – Study Guide Test 2: Module 3 ,4 and 5 (Labor, Postpartum an (All)
NUR2633 Exam 2 Focused Review / MCH – Study Guide Test 2: Module 3 ,4 and 5 (Labor, Postpartum and Newborn care)
Document Content and Description Below
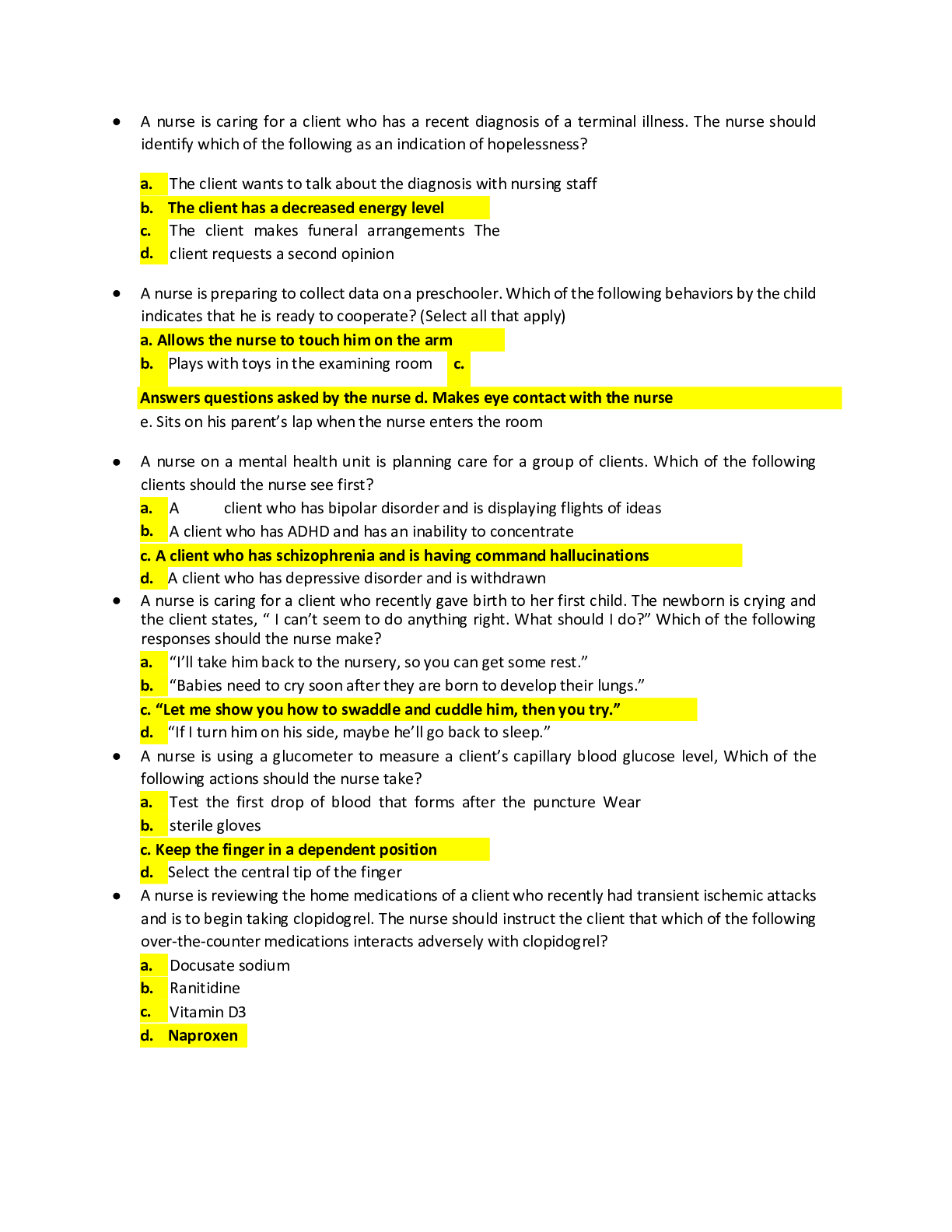
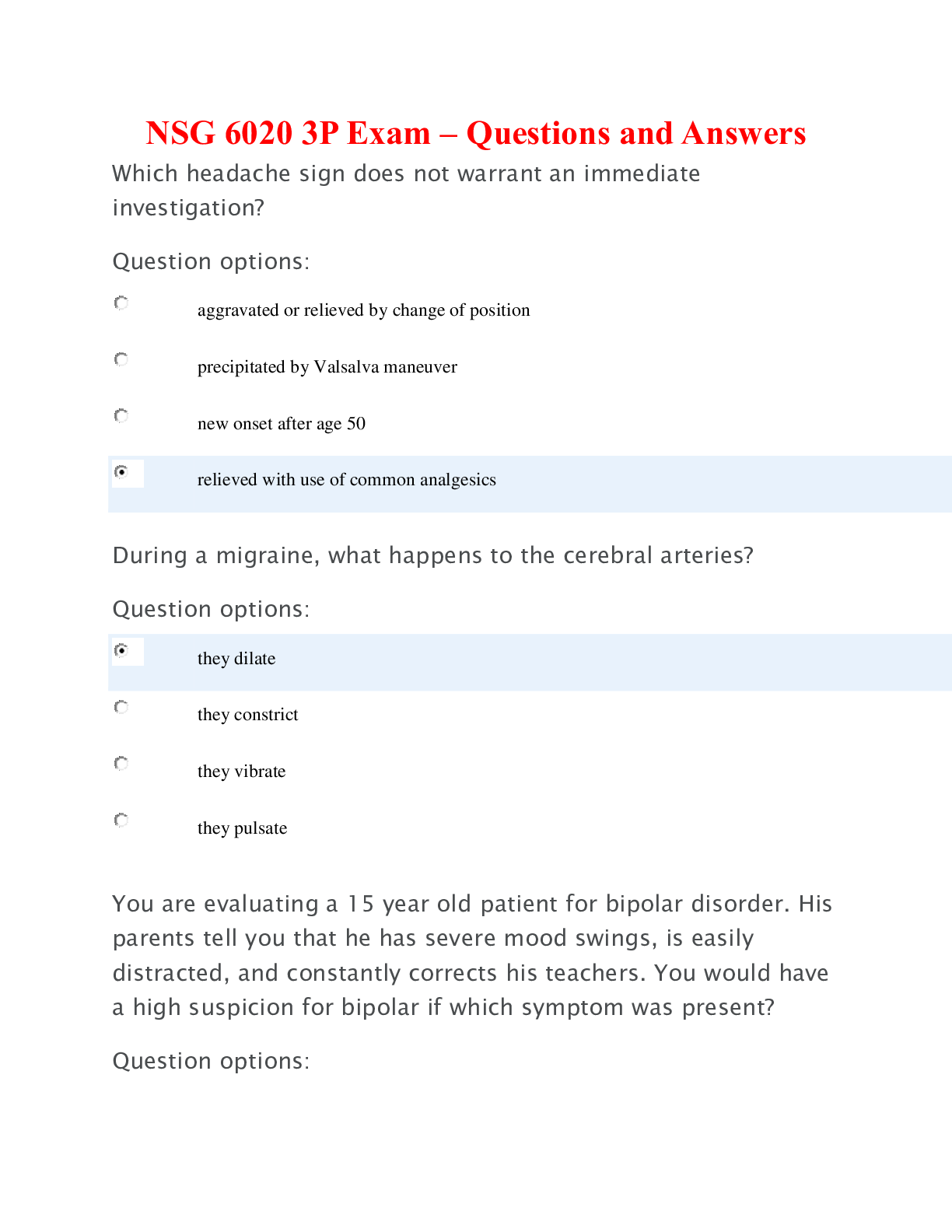
NUR2633 Exam 2 Focused Review NUR2633 – MCH – Study Guide Test 2: Module 3 ,4 and 5 (Labor, Postpartum and Newborn care) 1. Know the Stages and phases of labor including the physiological chang... es, the normal progression and the psychological impact to your patient. Know the labs that are essential to have for your patient prior to delivery of baby. Stages of labor First Stage- labor- variable Second stage- delivery of baby- up to 3 hours (2 without anesthesia) Pushing stage. Third Stage- delivery of placenta- 5-30 minutes Fourth Stage- Recovery 2 hours Within the first stage- we have 3 phases. 0-4cm- latent- most variable. Objective signs: cervical change, some effacement, communicative, contractions 8-10 min apart, mild contractions 4-8 cm- active- Intensity in contractions; bloody show- This is where we medicate mom.. 4-6 hours. Contractions are getting closer together and stronger. Membranes may rupture, contractions 2-5 min apart, more focused, less talking, risk to baby is greater, amount of perfusion to baby is less, baby can get hypoxic during long labor with progression 8-10 cm- transitional- rectal pressure- need to bear down and want to push- about 2 hours or less., may scream, writhe around in bed, will not feel any cervix around baby’s head Make sure mom is in a comfortable position and her surroundings are calm and inviting. Squatting or sitting is the best position. CBC, Hep, Rubella, HIV, Syphilis, Group B, Blood type, RH, drug screen, urine analysis 2. Know the reasons and the findings of each vaginal exam. Three pieces of information that we must get during a vaginal exam: Dilation (cervix is opening), station # of cm above the ischial spine is a negative number, below the ischial spine is a positive number, and effacement (from thick to thin)0%-100% You can also get the presentation of the baby and feel is the membranes are intact. Vaginal exams are done at admission for baseline, when membranes rupture, and when she asks for pain meds, and when patient says she is ready to push. 3. Know the medications of labor and when to administer them. Pitocin- Promotes uterine contractions. Used to begin labor, augment labor and postpartum. We use 2 milliunits per minute which is equal to 6 ml per hour and it is titrated. Lactated Ringers. Every 20-30 minutes we move it up depending on the patient. Frequency of contractions no more than 2-3 minutes apart. Magnesium Sulfate- Preterm labor and pre-eclampsia Nubain and Stadol- Administer for Pain. Methergine (IM and PO after-contraindicated for hypertension) and Hemabate- Prevents hemorrhaging Cytotec- Causes uterine contractions. 4. Know the risks of rupturing membranes and what is the nursing intervention if this occurs spontaneously vs artificially. Infection is the biggest risk. Decrease the amounts of vaginal exams. Check the color and odor of the fluid as well when they ruptured. Baby should be delivered within 24 hours of ruptured membranes. 18 hours into ruptured membranes we administer antibiotics. AROM- Artificial rupture of membranes- fetal heart rate prior to AROM and after to determine if baby is in trouble or not. 5. Pain management – recognizing the risks and nursing interventions of regional anesthesia (epidurals/ spinal) (biggest risk to mom is hypotension – which causes fetal decelerations, so how do we prevent this?) Nubain and Stadol are systemic analgesics that is given during the active phase (peak of the contraction because there is less perfusion happening at that time so baby gets less of the meds). You do not want to give it to early or too late because then it all goes to the baby. Have Narcan in the warmer in case the baby does not have good APGAR score. 6. Preparation for epidural anesthesia also has to be considered as a nursing responsibility. Epidural (regional anesthesia)- Need consent from mom first, CBC w/ platelets, sit still, and give her About 1 liter of fluids. We give fluids to prevent hypotension. Client is placed supine after epidural, so we need to use a wedge under the right hip to decrease the pressure on the vena cava. NO PREGGO CAN LAY SUPINE DUE TO HYPOTENSION BECAUSE IT WILL PUT PRESSURE ON THE VENA CAVA. Vital signs every 5 minutes watching out for hypotension. 7. Know the reasons, risks and nursing interventions of the need for a C/section. This includes post-operative care. Also discuss the option for a VBAC and the criterion needed to start the discussion: incision is the priority. Pre-op Prep for a C-Section: Labs, foley, consent and awake to participate. Ambulate, give Pitocin if client is not progressing. Pitocin needs to be titrated, so we do not end up with a titanic contraction. Fetal hypoxia and uterine fatigue. We allow contractions to get 2-3 or 2-4 minutes apart. When do we do a C-section? Breech, transverse, placenta previa or abruption, prior C-section, baby is too big, cord prolapse, failure to descend, failure to dilate, non-reassuring fetal tracing, infection, herpetic lesion. Post Op for C-section: Vital signs, bleeding, LOC, locate fundus, urine output, No ambulating initially (SCD’s are on), pain management, peri care, listen to lungs/abdomen/ heart. VBAC- Low transverse incision, vertex presentation, why did she have the first C-section, availability of anesthesia and physician. Risks: Uterine rupture Will do VBAC if: Vertex presentation, a low transverse incision, baby fits through the pelvis, doctor and anesthesia must be immediately available in case we have a ruptured uterus. 8. Non-pharmacological pain management for the laboring patient Walking, position change, massage, music, distraction, counterpressure, effleurage, hydrotherapy 9. Review the abnormalities of labor (dysfunction labor) and the obstetrical emergencies Cord prolapse (Breech, IUGR, Transverse, Small babies, Polyhydramnios. Variable decelerations or prolonged decelerations which will have us do a vaginal exam and feel the pulsation. Push on the presenting part, not on the cord. Position mom on her hands and knees. And do a C-section. Amniotic fluid embolism (Everyone is at risk. SOB, dyspnea, Pulmonary Embolism symptoms, chest pain, feeling of doom. Needs C-section. Mom usually does not survive.) Shoulder dystocia (Diabetic mothers- babies are macrosomia- we put pressure just anterior to the pelvic bone. Risk to baby is Erb’s Palsey). Second stage of labor- Pushing stage is very slow and when the baby comes out it retracts (the turtle sign). Ruptured Uterus (Infection, multiple babies, prior C-section, large babies. Recognize it with bleeding, pain and visible baby parts. Needs C-section.) 10. Review once again the issues of pre-eclampsia and knowing that delivery of the baby and placenta is the only cure – what if this patient is premature? Subjective: Headaches, blurry vision, swelling, epigastric pain. Objective: BP, Edema and protein. Administer Mag- 4 grams initially and them 2 grams maintenance dose. NOI: Left side, bedrest, dim lights, FHR, monitor fluids, Risks: Respiratory depression Preterm: Fetal monitor, vital signs, fluids, check for fetal fibronectin, vaginal exam. Call provider- advise and ask if we can administer Terbutaline, Mag Sulfate 11. Fetal monitoring – understand the parameters of normal fetal monitoring vs abnormal. a. Baseline ; Variability; Accelerations; Decelerations Late; Variable; Early; Prolonged b. Maternal Uterine Activity – what are the expectations? FHR 110-160 Variability- Minimal, moderate or absent. CNS is responding to the environment. Minimal- A baby would have minimal variability due to sleep cycle, mom got pain meds, mom is dehydrated. Give fluids; Caused by Hypertension, pain meds, dehydration. Moderate- Give fluids; As contractions get closer together, we will see some decelerations. Early decelerations are due to head compression. Variable decelerations due to cord compression. Late decelerations are due to placental insufficiency and it shows up late in the pattern. Stop Pitocin, change position, give o2, administer fluids. TELL PROVIDER. Accelerations are going above the baseline. Good during laboring process. Late decelerations: placental insufficiency, smoker, drug user, >40 weeks gestation (placenta wears out) Variable decelerations: cord compression early decelerations: head compression Contractions-count from beginning of one to to beginning of next contraction, don’t want it to be less than 2 minutes apart. 12. If the fetal monitoring is non-reassuring what is the nursing interventions to provide intra uterine resuscitation. Position change- increase LR- Give oxygen (8-10L by non-rebreather mask)- Stop Pitocin 13. Know obstetrical emergencies. Know the risk factors, treatment plan and any nursing interventions. (Identify risks, identify signs, interventions, and outcomes) Uterine rupture, cord prolapse, shoulder dystocia and Amniotic fluid embolism Discussed above. 14. Post dates: definition, risks to mother, risks to fetus, how do you recognize risks and manage those risks, and nursing interventions before and after the birth. Meconium aspiration- becomes Meconium aspiration pneumonia, aging placenta, Babies get too big, decelerations due to aging placenta, still birth (Do BPP at 40 weeks) Past dates after 42 weeks. 15. Postpartum initial care and the immediate risks – what are the nursing interventions Pressure- gush of blood- cord gets longer- and the uterus gets firm (globular)- complain of feeling of fullness- Check the placenta- two arteries and one vein. Check that the membranes look clean. If there is an odor it will be sent for cultures. Check that all cotyledons are present. If the placenta does not deliver on its own than you must manually remove it. Give mom antibiotics. Adherent Placenta takes place when all or part of the placenta is stuck to the wall of the woman's womb. Non-adherent Placenta: Typically, the placenta detaches from the uterine wall after childbirth. With placenta accreta, part or all the placenta remains attached. This can cause severe blood loss after delivery. It's also possible for the placenta to invade the muscles of the uterus (placenta increta) or grow through the uterine wall (placenta percreta). Placenta accreta is considered a high-risk pregnancy complication. If the condition is diagnosed during pregnancy, you'll likely need an early C-section delivery followed by the surgical removal of your uterus (hysterectomy). Assessment of postpartum patient in recovery. Vital signs every 15 min for an hour- every 30 for the second hour Check lochia Pain- after birth pains NSAIDs. Check for location of fundus (@ umbilicus and it should be midline and hard) Put ice pack on parineal area Ambulate (We want the epi to have work off) Check IV patency- pitocin is running fast. 16. Postpartum hemorrhage is the most serious and most common complication. What are some of the causes and what are our INITIAL intervention and other nursing interventions. Massage the fundus FIRST! Administer Pitocin If bleeding persists, five Methergine (methylergonovine) Hemabate is last to use for hemorrhaging Send a type and cross to the bank just in case you need to transfuse. Who is at risk for hemorrhage- someone who delivered rapidly, infected uterus, distended uterus, prior hemorrhage. 17. Pain management of the postpartum patient, which patient will report more uterine pain? What about pain management of the newborn? Do they feel pain? How do we know? NSAIDs 18. Medications used for postpartum care. See meds above. 19. If an episiotomy is performed how do you assess and care for this? Tears Intervention: First degree: ice for about 24 hours; analgesics Second degree: add sitz bath Third degree (to the rectum): add a stool softener Fourth degree (through the rectum): add antibiotics and suggest C-section for subsequent deliveries. Medial lateral- vagina towards your buttocks Midline-cut towards the rectum 20. Know lactation and non-lactating concerns. How do nurses manage engorgement vs. mastitis? Know the signs and symptoms of each and the differing interventions Engorgement- massage breast, cabbage leaves, warm showers, feed on demand. Non-lactating- Use ice and a tight-fitting bra and analgesics. Mastitis is unilateral. Tender, hot to the touch, feverish, engorged lymph’s under the arms and neck. Administer antibiotics. Unclog the milk duct. Keep breasts empty. Baby can still nurse since they will not get the infection. 21. Newborn care – initial assessments, and the normal parameters you would expect to see for the newborn, need for thermoregulation and how do we manage Initial assessment: AIRWAY- second breath is more important. RR of a newborn- 30-60 breathes per minute- Not regular- seconds of apnea/gasping HR between 100-160 Thermoregulation- Dry him off and warm him up Temp is taken auxiliary only (36.2-36.5) HR- check the base of the cord or with the stethoscope Shape of head- molding, caput, 2 fontanels, eyes Apical pulse for a full minute 22. Be able to speak to a full newborn assessment and know the vital sign parameters. Fontanels should be flat. Heads should be round. Ears should be symmetrical; a little bit above the eyes. Should have recoil; Not a lot of discharge Nose patent Eyes clear Palate should be intact Good sucking reflex Mucus membranes intact and moist Neck- ROM Tongue should be mobile Breast buds (may not have if baby is premature) Flexed posture Baby should have full bowel sounds after they start eating Cord should be clamped off and not show any signs of infection Check spine for bulges, dimples and openings Moro/Startle reflex shoes they are intact. Know they have primitive reflexes that only respond to activity. 23. Know APGAR'S Look at APGAR- Appearance/Color, pulse/HR >100, Grimace, Activity/muscle tone and RR. Most common score that we see is 8-9 Acrocyanotic- hands and feet are blue. They lose points for color. Respiratory distress sign is retractions, nasal flaring and grunting. APGAR score of 1-3 you should be resuscitating They are done at 1 minute and 5 minutes. 24. Risks to the newborn – birth injury due to Macrosomia, hypoglycemia, respiratory issues due to meconium, or prematurity, or DM, NAS: Irritable, uncontrollable, high pitched cries, constantly sucking, they throw up when you feed them. 25. Jaundice – a common occurrence what is the risk, how do we manage, and what are the risks of management. How can you prevent jaundice? Phototherapy and increase fluids/feedings. Expose the skin to the lights, cover eyes and genitals. Expect a lot more stooling- No lotion Change position every couple hours May need a heat source 26. Know cold stress and the effects to the newborn. Cover baby- thermoregulation takes about 24 hours. 27. Know the benefits of breast feeding vs. bottle feeding. Bonding, antibodies, better nutrition, contracts the uterus, high in fat. 28. NAS – neonatal Abstinence syndrome – what is the manifestations that the baby will show and how do we manage this. NAS: Irritable, inconsolable, high pitched cries, constantly sucking, they throw up when you feed them, diarrhea, eyes constantly darting NAS can happen when mom is a drug user Morphine or methadone for baby if needed. Breastfeeding promotes bonding between mom/baby 29. Reasons for c/sections: know how to manage pre-operative, post-operative care. NOI: SCD’s, vital signs every 4 hours, pain management, foley (12-24hours), check incision, use incentive spirometer, bleeding, fundus, check skin, monitor I & O Ambulate is an order. 30. Postpartum blues, depression and psychosis – all very different with different symptoms and risks. Who is at risk, what do we do with the information, and how do we approach these patients. Psychosis needs to be in the hospital. Both mom and baby are at risk. 31. Circumcision – different types of equipment used, care during and after the procedure. What are the risks to the neonate and discharge information that should be provided Gomco- Post operative care petroleum gauze so that the penis does not Mogen- Same ^ Plastibell- it will fall off when it is healed. Risk is bleeding and unable to void. Check for voiding Profuse bleeding Cord care- alcohol wipes, soap and water 32. Manage newborn pain – how do we recognize signs and symptoms of pain, how we manage, what scale is used. Pharmacological: NSAID’s and Opioids- VERY SMALL DOSAGES (based on weight). Signs of pain: Grimacing, flaring legs, crying, crys scale- Non-pharmacological: Swaddle, sugar water on a piece of gauze, pacifier, skin to skin, rocking, distraction, Kangaroo care This is the vulnerable population we are discussing – laboring women and babies. Normal blood loss for vaginal deliveries is 500mL and 800 mL for C-sections. [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 09, 2021
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Mar 09, 2021
Downloads
0
Views
37

.png)