NUR 2633 MCH – Study Guide Exam 2: Module 3,4 and 5,100% CORRECT
Document Content and Description Below
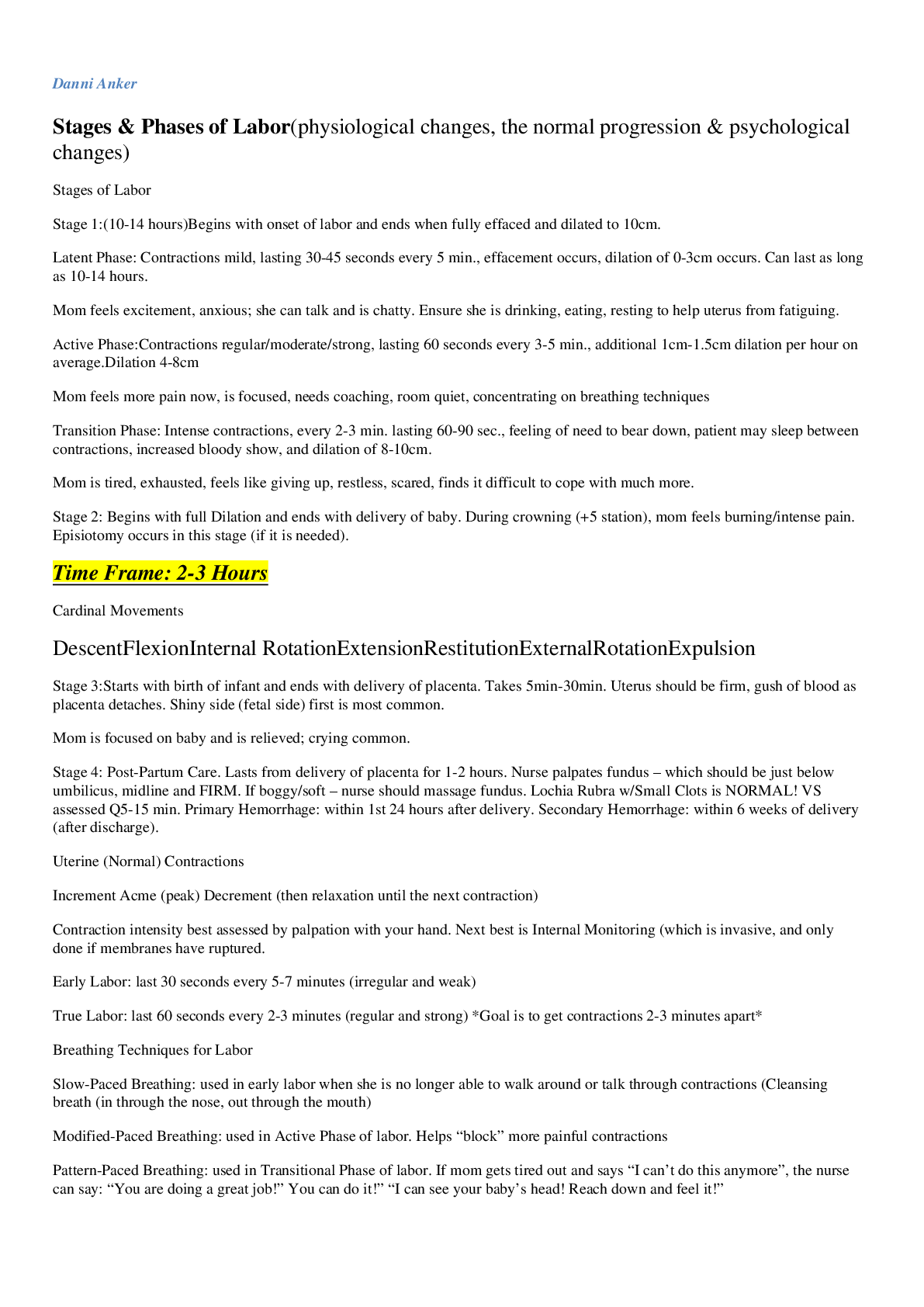
NUR 2633 MCH – Study Guide Exam 2: Module 3,4 and 5 Danni Anker Stages & Phases of Labor(physiological changes, the normal progression & psychological changes) 1. Stages of Labor a. Stage 1:(10... -14 hours)Begins with onset of labor and ends when fully effaced and dilated to 10cm. i. Latent Phase: Contractions mild, lasting 30-45 seconds every 5 min., effacement occurs, dilation of 0-3cm occurs. Can last as long as 10-14 hours. 1. Mom feels excitement, anxious; she can talk and is chatty. Ensure she is drinking, eating, resting to help uterus from fatiguing. ii. Active Phase:Contractions regular/moderate/strong, lasting 60 seconds every 3-5 min., additional 1cm-1.5cm dilation per hour on average.Dilation 4-8cm 1. Mom feels more pain now, is focused, needs coaching, room quiet, concentrating on breathing techniques iii. Transition Phase: Intense contractions, every 2-3 min. lasting 60-90 sec., feeling of need to bear down, patient may sleep between contractions, increased bloody show, and dilation of 8-10cm. 1. Mom is tired, exhausted, feels like giving up, restless, scared, finds it difficult to cope with much more. b. Stage 2: Begins with full Dilation and ends with delivery of baby. During crowning (+5 station), mom feels burning/intense pain. Episiotomy occurs in this stage (if it is needed). Time Frame: 2-3 Hours i. Cardinal Movements DescentFlexionInternal RotationExtensionRestitutionExternalRotationExpulsion c. Stage 3:Starts with birth of infant and ends with delivery of placenta. Takes 5min-30min. Uterus should be firm, gush of blood as placenta detaches. Shiny side (fetal side) first is most common. i. Mom is focused on baby and is relieved; crying common. d. Stage 4: Post-Partum Care. Lasts from delivery of placenta for 1-2 hours. Nurse palpates fundus – which should be just below umbilicus, midline and FIRM. If boggy/soft – nurse should massage fundus. Lochia Rubra w/Small Clots is NORMAL! VS assessed Q5-15 min. Primary Hemorrhage: within 1st 24 hours after delivery. Secondary Hemorrhage: within 6 weeks of delivery (after discharge). 2. Uterine (Normal) Contractions a. Increment Acme (peak) Decrement (then relaxation until the next contraction) b. Contraction intensity best assessed by palpation with your hand. Next best is Internal Monitoring (which is invasive, and only done if membranes have ruptured. i. Early Labor: last 30 seconds every 5-7 minutes (irregular and weak) ii. True Labor: last 60 seconds every 2-3 minutes (regular and strong) *Goal is to get contractions 2-3 minutes apart* 3. Breathing Techniques for Labor a. Slow-Paced Breathing: used in early labor when she is no longer able to walk around or talk through contractions (Cleansing breath (in through the nose, out through the mouth) b. Modified-Paced Breathing: used in Active Phase of labor. Helps “block” more painful contractions c. Pattern-Paced Breathing: used in Transitional Phase of labor. If mom gets tired out and says “I can’t do this anymore”, the nurse can say: “You are doing a great job!” You can do it!” “I can see your baby’s head! Reach down and feel it!” 4. Comfort During Labor a. Effleurage: massaging abdomen using light, circular motions. Helps distract mom from pain. b. Counterpressure: constant sacral pressure is applied. Helps with posterior occiput positioned baby c. Aromatherapy (lavender), Massage, Breathing Techniques, Music (releases endorphins and controls pain), Focal Therapy d. Hydrotherapy: use of water for relaxation. Intermittent or continuous FHR monitoring needed. Water temp should be between 96.8F - 100.4F. i. Do NOT use internal electrodes when patient is in tub/bath Know the rationale for when to and when NOT to do vaginal exams during labor • Do not do vaginal exam on a patient who has VAGINAL BLEEDING (especially those who have heavy bleeding). If you do a vaginal exam on a patient with vaginal bleeding, you may increase it (if patient has placenta previa) • Do Ultrasound, instead of Vaginal Exam. When do you do a vaginal check? 1. For Pain Meds 2. When water breaks 3. On Admission 4. When pt feels need to bear down Medications of labor and when to administer them (and in what order if using multiples…..example; if you are trying to stop labor which drug would you use 1st, 2nd, etc.) • Preterm Labor Meds o Magnesium Sulfate: Used to treat pre-term labor by relaxing the diaphragm and uterus (relaxes smooth muscle). Also treats Preeclampsia by depressing the CNS system, relaxing things and slowing things Antidote: Calcium Gluconate (should be next to the bed when patient is on Mag. Sulfate!) Adverse Reactions: Respiratory Depression, Hypotension, Bradycardia, hypothermia, drowsiness, arrhythmias How do you give it? 4-6g IV bolus over 15-30 minutes, then 1-3g IV maintenance dose Q hour. Onset & Duration: Immediately (IV) and lasts 30 minutes What can the patient expect to feel when med is given? • She may feel warm/flushed, N/V, visual blurring and H/A Nursing Interventions • Monitor BP, Pulse, Respirations & ECG. [Respirations should be over 16/min before each dose] • Medications of Labor Induction o BEST time to give is during the PEAK of the contraction (less Rx goes to baby) as the fetal blood vessels are contracted during this time and the Rx stays in mom’s blood system for several seconds before uterine blood vessels reopen. Induction of Labor • Pitocin (oxytocin) o Perform Bishop’s Score and use Pitocin if Cervix is favorable (if not you can use a cervical ripening agent) o Titrated via pump o CONSTANT fetal monitoring needed (FHR) • Cervical Ripening Agents o Misoprostol (Cytotec) • Medications for Pain During Labor Dilaudid Demerol • Used for pain mgt • Opioid Analgesic: used for chronig Sublimaze, Sufental Stadol (butorphanol) • Associated with Respiratory Depression in Mom & Baby • Can precipitate withdrawal symptoms in pt dependent on opioids Nubain (nalbuphine) • Can precipitate withdrawal symptoms in pt dependent on opioids • Takes 2-3 minutes to kick in & lasts 10 hours or so Combined Spinal Epidural • Spinal: used during the Latent Phase of labor for pain relief • Epidural: used when Active Labor begins Epidural Block • Used in Elective & Emergency C-Section • Vaginal Deliveries – ok, only if LOW block is used (not suitable for labor) Lumbar Epidural Block • First and Second stages of labor • HUGE BP drop here! Monitor maternal BP Local Perineal Infiltration/Pudendal Nerve Block • Used to repair episiotomy or right before birth for episiotomy • Used for pain mgt for forceps or vacuum extraction Pain management – recognize the risks and nursing interventions of regional anesthesia (epidurals/ spinal) (biggest risk to mom is hypotension – which causes fetal decelerations, so how do we manage this risk/prevent this? • Spinal Anesthesia o Administered through L3 or L4 lumbar interstitial space into the subarachnoid space. Vaginal Delivery • Low Spinal Anesthesia • Provides pain relief from hips to feet • Pt remains sitting for a few minutes after administration C-Section Delivery • Numb from nipples to feet • Patient immediately placed supine with L Lateral pelvic tilt after administration Postdural Puncture H/A: worse when sitting up. May include tinnitus and blurry vision/photophobia. Oral analgesics, bedrest in a dark room, caffeine and hydration help. If these fail to help, blood patch • Epidural Anesthesia o Administered into the epidural space (between L5 & S1) • Rupturing Membranes (Get baby out within 24 hours!) o AROM:(do NOT perform until engagement has occurred) Labor starts within 12 hours of rupture. If labor does not start, increased risk for infection, fetal injury and umbilical cord prolapse occur. Contractions are usually stronger with an anmniotomy. Temperature over 100.4F is indicative of infection. Temperature should be assessed Q2 hours at minimum. Sterile procedure. Get baby out within 24 hours! Rupture on side to avoid rush of fluid out (like a drain on a bathtub) o SROM (spontaneous):mother should be kept on immediate bedrestuntil fetal presenting part is engaged (keep the amniotic fluid from rushing out). Get baby out within 24 hours! • Nitrazine Strip o Beige = no fluid present o Blue, blue-green, grey = fluid IS present! • Fern Test o If the Nitrazine test is negative, then the Fern Test is performed via slide & microscope. A “ferning pattern” is seen on the slide and used most commonly when PROM is suspected. Epidural Placement (done by RN) 1. Wash/Dry Hands 2. Explain procedure to patient 3. Sitting position on the edge of the bed or operating table (“C” position with head bowed down and back arched) 4. Check IV for patency (IV bolus of LR 500ml-1000ml given to avoid Hypotension) 5. Assist patient to supine position & place pillow under head & Right Hip (wedge under R hip to offset uterus to prevent supine hypotension) 6. Monitor BP, Pulse, Respirations Q1-2 minutes for the first 10 min, then Q5-10min thereafter 7. Document in patient’s chart Interventions for Severe Maternal Hypotension/Decreased Placental Perfusion (pg. 418) 1. Place mom in Left Lateral position 2. Increase/Maintain IV fluids 3. O2 via facemask @ 10-12L/min 4. Alert MD 5. Administer IV vasopressor (Ex: Ephedrine 5-10mg) (if above measures are ineffective) 6. Remain calm, offer reassurance and monitor FHR & BP Q5min until stable Know the reasons, risks and nursing interventions for the C-Birth (Cesarean) patient. Understand non-pharmacological pain management for the laboring patient and types of non-pharmacological intervention the nurse can employ Review the abnormalities of labor (dysfunction labor )and the obstetrical emergencies Review once again the nursing considerations in the patient diagnosed with pre-eclampsia. Understand why pre-eclampsia often requires early delivery and the know the preparations necessary for the birth for pre-term infants. What will you do to give baby the best shot at post-birth stability? Understand that delivery of the baby and placenta is the only cure – and sometimes pre-eclampsia can occur AFTER birth. Fetal monitoring • Baseline: 110-160bpm • Variability: Fluctuations in FHR minute to minute. a. Marked: over 25bpm b. Moderate c. Minimal d. Absent • Accelerations: GOOD THING! FHR is going above baseline due to movement or increase in O2. Indicates good placental perfusion. • Decelerations a. Late b. Variable c. Early Know obstetrical emergencies. Know the risk factors, treatment plan and priority nursing interventions. Intrauterine Resuscitation(“Flip, Fluid, O2”) 1. Change mom’s position (side lying; LEFT side is best) 2. Increase the IV fluid (usually LR is used) 3. Add O2 (8-10L by mask) 4. Stop Pitocin (as it increases contractions, which are brief periods of time that baby isn’t getting O2) 5. Call MD! 6. Document what you did up to that minute Understand the initial care and the immediate risks for the newly delivered mother BUBBLE-HEEN: Post Partum Assessment Understand the care/management of Postpartum hemorrhage. What are causes for PPH and what interventions are likely to be ordered by the physician? Review standard medications used for postpartum care gas/bloating, pain, localized perineal pain, breast discomfort, important considerations for the postpartum/breast-feeding mom when medications are in use. If an episiotomy is performed how do you assess and care for this? Know the types of episiotomy, placement, and comfort cares following birth for the mother with an episiotomy. 1st degree Laceration • Ice and NSAIDs 2nd degree Laceration • Ice, NSAIDs, and Sitz 3rd degree Laceration • 4th degree Laceration Know lactation basics and how to manage the initial postpartum breast comfort issues for the mother who chooses to nurse, as well as for the mother who chooses not to breastfeed. Engorgement vs. mastitis and how you might manage both conditions. Mastitis – continue breast feeding, unilateral pain, generally not feeling well, abx possibly, pump, get the milk out, red breast, painful to touch Engorgement – cabbage leaves, pump, warm showers, tight/supportive bra Newborn care – what are our initial assessments and the normal parameters for newborn vitals/condition? Understand thermoregulation in the newborn and how you would manage an infant experiencing unstable temperatures following birth. Be able to speak to a full newborn assessment and know the vital sign parameters. APGAR – What it is, how it is scored, when you would initiate resuscitation • Scored at 1 MINUTE after birth, and again at 5 MINUTES after birth • Nurse dries infant’s skin and wraps them in warm, dry blanket before placing on mom’s chest Understand risks to the newborn – Review birth injury due to Macrosomia (big babies), Hypoglycemia: @ risk is IGUR, LGA, and babies of diabetic mom’s, post term. Sx: jittery, not feeding well, tachycardia, apnea, high-pitched cry, irritable, seizures, temperature instability, diaphoresis, poor muscle tone Respiratory issues: Meconium aspiration/complications: can lead to pneumonia or hypoxia. Baby will have meconium stained skin, nails and umbilical cord. Respiratory distress and a barrel shaped chest from over inflated lungs. Rales and Rhonchi heard on auscultation. Confirmed via CXR. Tx: Percussion and O2, suction PRN Infant prematurity, or impact of the gestational diabetic mother on the infant risk. Review Jaundice. What is it? How do we manage it? How do we prevent it? What are risk factors? Understand physiologic vs. pathologic. Breast Feeding Contracts Uterus Bonding Immunity Colostrum Decreased risk of Ear Infections, UTI, pneumonia *Jaundice DO NOT BREASTFEED if…. Active TB or HIV Active Herpes lesions Taking Lithium Taking Methotrexate Bottle Feeding May keep baby fuller, longer Others can help feed baby Convenience Interfere with return to work Embarrassment Involvement of Father NAS – neonatal Abstinence syndrome – what is the manifestations that the baby will show and how do we manage this. Review postpartum blues vs. depression, postpartum psychosis, risks, treatments, and primary concerns. *Gynecoid pelvis is the ideal pelvis shape for vaginal deliveries. *ROA is ideal position for baby *Squatting is the best position and helps to open the pelvic outlet *Occiput posterior position is associated with back labor;Counterpressure on the sacral area is needed. *Hands & Knees position is best for those experiencing back labor from the Occiput Posterior position. It also helps the baby rotate into an anterior position. Nulligravida – never been pregnant Nullipara – previously pregnant, but no living children Primigravida – first pregnancy Multigravida – multiple pregnancies Primipara- first time parent Multipara – parent of previous children [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 17, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Feb 17, 2021
Downloads
0
Views
39