*NURSING > STUDY GUIDE > NUR 206_ATI FUNDAMENTALS EXAM, Chapters 1 to 58, Complete Latest 2023 (All)
NUR 206_ATI FUNDAMENTALS EXAM, Chapters 1 to 58, Complete Latest 2023
Document Content and Description Below
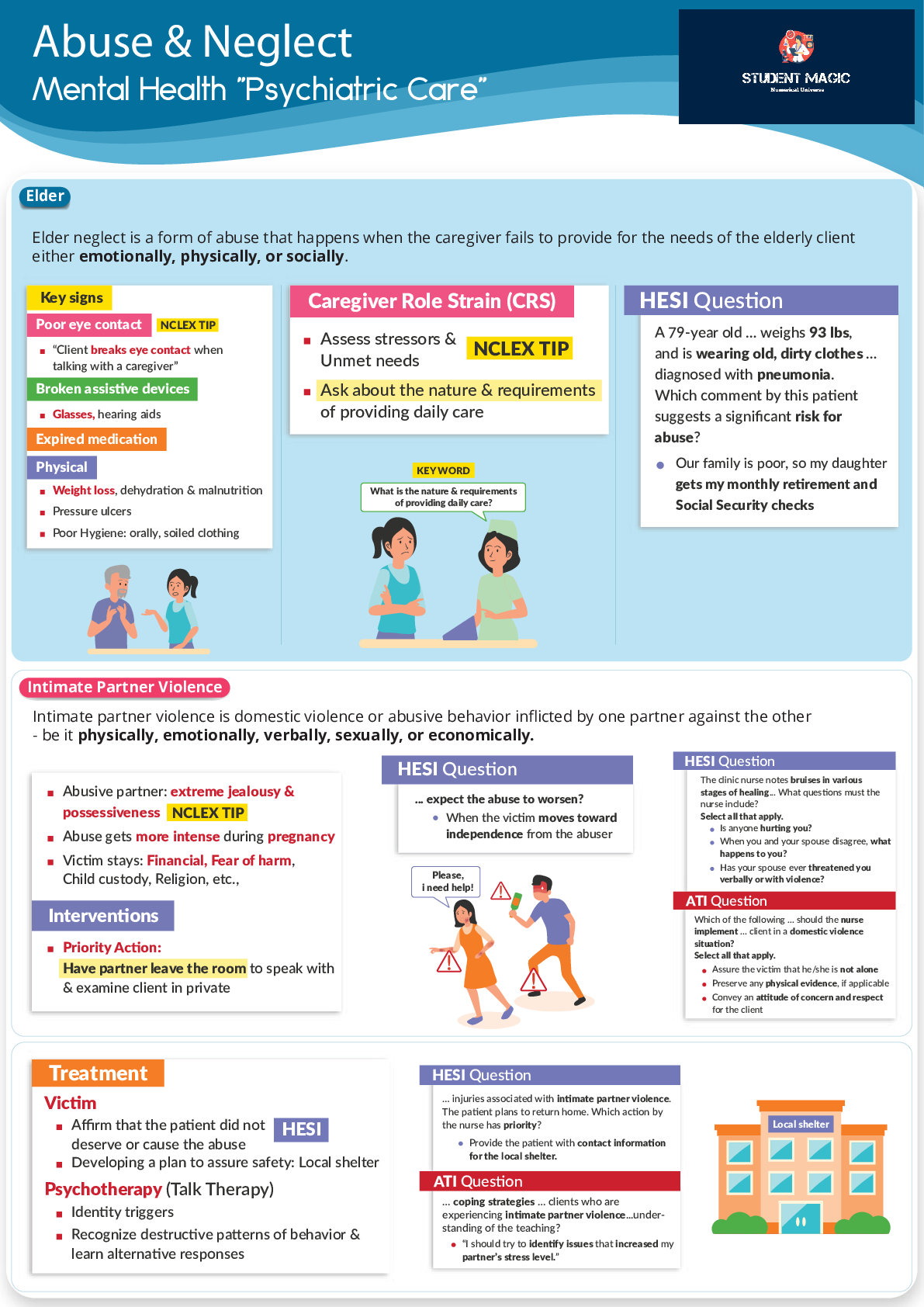
NUR 206_ATI FUNDAMENTALS EXAM, Chapters 1 to 58, Complete Latest 2023-ATI FUNDAMENTALS EXAM 1. CHAPTER 1: HEALTH CARE DELIVERY SYSTEMS A. Components of Health care systems a. Participants 1. Consumers... - clients 2. Providers a. Licensed providers: registered nurses, license practical (or vocational) nurses (LPN), advanced practice nurses (APN), medical doctors, pharmacists, dentists, dietitians, physical/respiratory/occupational therapists, etc b. Unlicensed providers: assistive personal b. Settings 1. Hospitals, homes, skilled nursing, assisted living, schools, etc c. Regulatory Agencies 1. US department of Health and Human Services 2. US Food and Drug Administration (FDA) 3. State and local public health agencies 4. State licensing boards a. Determines laws/regulations that govern nursing in their state b. ensure health care providers and agencies comply with state regulations c. Issue/revoke nursing license i. Nurses need a license in every state they practice in 5. Joint Commission (JCAHO) a. Set quality standards for accreditation of health care facilities 6. Professional Standards Review Organizations- monitor health care services provided d. Healthcare financing Mechanisms 1. Public federally funded programs a. Affordable Care Act (Obamacare) i. Increases access to healthcare for all individuals ii. Decreasing healthcare costs iii. Providing opportunities for uninsured to become insured at an affordable cost b. States Children’s Health Insurance i. Covers uninsured children up to 19 years old at a low cost to parents c. MEDICARE MEDICAID Eligibility: >65 years old OR on disability for more than 2 years OR have ALS OR on dialysis Part A: inpatient hospital, limited skilled nursing care, home health care (hospital insurance) Part B: outpatient care, diagnostic services, OT/PT (medical insurance) Part C: combination of parts A and B, optional private insurance (Medicare advantage plan) Part D: prescription drugs (medications) Eligibility: low socioeconomic status, no insurance Federally and state funded Individual states determine eligibility requirements e. Levels of Health Care Preventative Focuses on educating and equipping clients to reduce or control risk factors for disease Primary Emphasizes health promotion and includes prenatal, well-baby care, family planning, nutrition counseling, disease control Secondary Diagnosis and treatment of acute illness and injury Tertiary Provision of specialized and highly technical care Restorative Intermediate follow-up care for restoring health and promoting self-care Continuing Addresses long-term or chronic health care needs over a period of time 2. CHAPTER 2: THE INTERPROFESSIONAL TEAM A. Interprofessional Personnel (non-nursing) Spiritual Support Staff Provides spiritual care (pastors, rabbis, priests) Registered Dietitian Assess/plans for/educates regarding nutrition needs Laboratory technician Obtains specimens of body fluids, and performs diagnostic tests Occupational therapist Focuses on patient’s independence and regain activities of daily living (ADL) skills Pharmacist Provides and monitors meds Physical Therapist Focuses on increasing musculoskeletal function (especially lower extremities), to maintain mobility Provider Assess/diagnose/treat diseases or injury, includes doctors, APNs, physician’s assistant Radiologic technologist Positions client and performs x rays and other imaging procedures for providers to review for diagnosis of disorders of various body parts Respiratory therapist Evaluates respiratory status and provides respiratory treatments including oxygen including oxygen therapy, chest physiotherapy, inhalation therapy, and mechanical ventilation Social worker Works with clients and families by coordinating inpatient and community resources to meet psychosocial and environmental needs that are necessary for recovery and discharge Speech-language pathologist Evaluates and makes recommendations regarding the impact of disorders or injuries on speech, languages, and swallowing Ex: patient with dysphagia call speech pathologist for consult 3. CHAPTER 3: ETHICAL RESPONSIBILITIES A. Ethical Decision Making In Nursing a. Basic principles of ethics 1. Advocacy- support of client’s health, wellness, safety, privacy, and personal rights 2. Responsibility- willingness to respect obligations and follow through on promises 3. Accountability- ability to answer for one’s own actions 4. Confidentiality- protection of privacy without diminishing access to high-quality care b. Ethical Principles for client care Autonomy The right to make one’s own personal decisions, even when those decisions might not be in that person’s best interest (ex: Jehovah’s witness- blood transfusion) Beneficence Action that promotes good for others, without any self interest Fidelity Fulfillment of promises Justice Fairness in care delivery and use of resources Nonmaleficence A commitment to do no harm Veracity Commitment to tell the truth c. Ethical Dilemma 1. Problems that involve more than one choice and stem from differences in values and beliefs of the decision maker a. A problem is an ethical dilemma when: i. There is not enough scientific data to solve it ii. It conflicts between 2 moral imperatives iii. Answer will have a profound effect on the situation and the client 2. When making an ethical decision: a. Identify if the issue is an ethical dilemma, gather as much relevant info as possible, reflect on own values, list and analyze all possible options, select correct option, apply it to situation 4. LEGAL RESPONSIBILITIES A. Sources of Law a. Federal regulations 1. Health Insurance Portability and Accountability Act (HIPPA) 2. Americans with Disabilities Act (ADA) 3. Mental Health Parity Act (MHPA) 4. Patient Self-Determination Act (PSDA) b. Criminal and civil laws 1. Criminal law- relates to the relationship between an individual and the government 2. Civil law- protect individual rights (ex: tort law) c. State laws d. Licensure B. Types of Torts a. Unintentional torts 1. Negligence a. nurse fails to implements safety measured for a client at risk for falls (ex: bed alarm) b. 5 elements necessary to prove negligence i. Duty to provide care as defined by a standard ii. Breach of duty by failure to meet standard iii. Foreseeability of harm iv. Breach of duty has potential to cause harm v. Harm occurs 2. malpractice a. nurse admins a large dose of meds due to a calculation error and client gets hurt b. Intentional torts 1. Assault- threat 2. Battery- acting on the threat 3. False imprisonment a. A person is confined or restrained against his will; inappropriate use of restraints and sedatives C. Informed consent a. Legal process by which a client or the client legally appointed designee has given written permission for a procedure or treatment b. Provide should explain (needs to be in clients primary language- interpreter may be needed): 1. Reason the patient needs procedure or treatment 2. How the procedure/treatment will benefit the client 3. The risks involved if the client receives the procedure/treatment 4. Other options to treat the problem c. Nurses role: 1. Witness patient’s informed consent signature 2. Notify provider if they have more questions d. Individuals may grant consent for another person if they are: 1. Parent of a minor 2. legal guardian 3. court specified representative 4. individual has durable power of attorney authority for health care e. Refusal of treatment 1. Notify provider, patient signs a document indicating understanding of risks D. Advanced Directives a. Living will- legal document that expresses client’s wishes regarding medical treatment in the event the client becomes incapacitated and is facing end of life issues b. Durable power of attorney for health care- document in which clients designates health care proxy to make health care decisions for them if they are unable to do so c. Providers orders- unless there is DNR or AND in the clients medical record, the nurse will initiate CPR E. Mandatory reporting a. Abuse- nurses must report any suspicion of abuse (child, elderly, or domestic abuse) b. Communicable disease c. Impaired coworker (drinking, drugs) 1. Do not talk directly to them 2. Do not gather more information 3. Report the suspicion 5. INFORMATION TECHNOLOGY A. Documentation a. Elements of documentation 1. Subjective data- direct quotes or summarize information as the client’s statement 2. Objective data- what the nurse sees, hears, feels, and smells; NO OPINIONS b. Legal guidelines 1. Begin with date and time; write legibly, do not leave blank spaces; do not use correction fluid, erase, scratch out or blacken out errors, sign all documents with name and title B. Reporting formats a. Change of shift report b. Telephone reports 1. Try to have another RN there to listen in on phone call 2. Read back order to the provider 3. Provider signs order off within 24 hours c. Transfer (hand off) reports d. Incident reports 1. Document facts without judgement or opinion 2. Do not refer to an incident report in a client’s medical record C. Information security a. HIPPA (health insurance portability and accountability act of 1996 1. Only health care team members directly responsible for a client’s care may access that client’s record 2. Clients have a right to read and obtain a copy of their medical record 3. Staff must keep medical records in a secure area to prevent inappropriate access to the info 4. Electronic records are password-protected 5. Nurses must not disclose unauthorized individuals or family members 6. Nurses must not disclose client’s info to unauthorized individuals or family members a. Many hospitals use a code system 6. DELEGATION AND SUPERVISION A. Delegation a. RN cannot delegate 1. Patient education 2. task that needs nursing judgement 3. Nursing assessment RN to LPN RN to CNA Monitoring findings Reinforce patient teaching Tracheostomy care Suctioning Checking NG tube patency Administering enteral feedings Inserting a urinary catheter Administering medication Activities of Daily Living (ADLs) - Bathing, grooming, dressing, toileting, ambulating, feeding (without swallowing precautions), positioning Routine tasks - Bed making, specimen collection, intake and output, vital signs (for stable clients) b. 5 rights of delegation 1. Right task a. Right task is repetitive, requires little supervision, and is noninvasive for the client 2. Right circumstance a. Determine the health status and complexity of care the client requires 3. Right person a. Task is within the delegatee’s scope of practice 4. Right direction and communication a. Provide a method and timeline for reporting b. Communicate specific tasks and detail expected results. Timeline, and expectations for follow-up communication 5. Right supervision and evaluation a. Provide supervision and provide feedback 7. NURSING PROCESS A. Assessment/Data collection a. Subjective data (symptoms)- during nursing history 1. client’s feelings, perceptions, and descriptions of health status b. Objective data (signs)- during physical examination 1. Feel, see, hear, and smell objective data through observation or physical assessment of the client c. Sources of data collection 1. Primary sources a. Subjective: what the client tells the nurse b. Objective: data the nurse obtains through observation and examination 2. Secondary sources a. Subjective: what others tell the nurse (family, friends) b. Objective: data the nurse collects from their sources B. Analysis/Data collection a. Requires nurses to look at the data and 1. Recognize patterns or trends 2. Compare the data with expected standards or reference ranges C. Planning a. Prioritize outcomes of care they can readily measure and evaluate D. Implementation a. Nurses base the care they provide on assessment data, analyses and then E. Evaluation a. Nurses evaluate the client’s responses to nursing interventions and form a clinical judgement about the extent to which clients have met the goals and outcomes 8. CRITICAL THINKING A. Don’t know specifics and know how to use critical thinking skills 9. ADMISSIONS, TRANSFERS, AND DISCHARGE A. Admission process a. Document client’s advance directive status (DNR, full code, etc), Base line data (vital signs, height, weight, allergies), Health history, swallowing problems (get evaluation from speech pathologist), spiritual health/quality of life concerns, safety assessments (risk for falls) b. Discharge planning starts at admission c. Inventory personal items 1. Assistive items: glasses, hearing aids, dentures 2. Medications 3. Discourage keeping valuables at the bedside B. Transfer a. Best thing to use: 1. Situation 2. Background 3. Assessment 4. Recommendation C. Discharge Education a. Review symptoms of potential complications and when to contact provider b. Provide names and numbers of community resources c. Step by step instructions for continuing treatments (dressing changes, etc) d. Dietary restrictions and guidelines e. Directions how to take medications f. Follow up appointments 10. MEDICAL AND SURGICAL ASEPSIS A. Hand Hygiene a. Hand wash with antimicrobial or alcohol-based products 1. Antimicrobial: wash for 15 seconds, dry hands with clean paper towel before turning off faucet a. Use antimicrobial soap over alcohol based when: i. Hands are visibly soiled ii. Before eating a meal iii. After using the bathroom iv. After contact with any bodily fluids 2. Alcohol based: use 3-5 mL, continue to rub until both hands are completely dry B. Physical environment a. Cover mouth and nose when coughing or sneezing, using and disposing of facial tissues 1. Ensure 3 spatial separation of 3 ft from a cough b. Keep nails short, clean, and no artificial nails; remove jewelry from hands and wrists c. Do not put items on flood, do not shake linens C. Sterile Field a. Do not cough, sneeze, talk over the sterile field b. Outer 1 inch wrapping of package is not sterile c. Objects below waist/above chest contaminated d. Do not reach across/above sterile field, turn back on sterile field 1. To add item drop form 6 inches above the field e. Any sterile, nonwaterproofed wrapper that encounters moisture becomes nonsterile 11. INFECTION CONTROL A. Immune Defenses a. Nonspecific innate- barriers respond immediately to all antigens 1. Ex: skin, mucus membrane, stomach acid b. Specific adaptive immunity – allows the body to make antibodies in response to a foreign organism (antigen) 1. Involves B ant T lymphocytes; takes more time c. Types of immunity 1. Active natural immunity- body produces antibodies in response to exposure to a live pathogen 2. Active artificial immunity- body produces antibodies in response to a vaccine 3. Passive natural immunity- antibodies passed down form a mom to a baby through breastmilk or the placenta 4. Passive artificial immunity- patient’s immunoglobins administered to them after exposure to pathogen B. Infection Processes a. Chain of infection 1. Causative agent (bacteria, virus, fungus, prion, parasites) 2. Reservoir- where it lives (human, animal, food, organic matter on inanimate surfaces, water, soil, insects) 3. Portal of exit- where it leaves the host (respiratory tract, gastrointestinal trac, etc) 4. Mode of transmission a. Contact- direct physical contact (person to person) b. Droplet- sneezing, coughing, and talking c. Airborne- sneezing and coughing 5. Portal of entry- how it enters the host (may be the same as the portal of exit) 6. Susceptible host- compromised defense mechanisms (immunocompromised, breaks in skin) leave the host more susceptible to infections b. Stages of infection 1. Incubation- pathogen enters the body to first symptom 2. Prodromal stage- onset of general symptoms to more distinct symptoms 3. Illness stage- specific symptoms to infection occur 4. Convalescence- acute symptoms disappear to total recovery c. Virulence- ability of pathogen to produce disease C. Assessment/Data collection a. Risk factors: 1. Inadequate hand hygiene, compromised health/defense, chronic or acute disease, poor personal hygiene, crowded environment, use of IV drugs, unprotected sex, poor sanitation b. Inflammation 1. Body’s local response to injury or infection 2. First stage: redness, edema, pain 3. Second stage: fluid containing dead tissue cells and WBCs accumulates and exudate appears at the site a. Types of exudate i. Serious (clear), sanguineous (blood), serosanguineous (pinkish tint), Purulent (leukocytes and bacteria) 4. Third stage: scar tissue D. Laboratory tests a. Leukocytosis- WBC level greater than 10,000/uL indicates infection 1. Normal range: 5,000-10,000/uL 2. Left shift: increase in neutrophils b. Elevated erythrocyte sedimentation rate (ESR)- over 20 mm/hr indicates infection c. Presence of micro-organisms on culture of the specific fluid/area d. Diagnostic procedures 1. Gallium scan, radioactive gallium citrate 2. X rays, CT scan, MRI E. Isolation Guidelines a. Standard precautions- for everyone 1. Hand hygiene- use alcohol based waterless product when hands are not visibly soiled 2. Masks, eye protection, face shields when splashing or spraying of bodily fluids may occur 3. Clean gloves b. Airborne precautions 1. Used for measles, varicella, pulmonary, or laryngeal tuberculosis 2. Private room 3. N95 masks for visitors and caregivers 4. Negative air flow in the room c. Droplet Precautions 1. Used for pneumonia, influenza, rubella, mumps, sepsis 2. Private room or room with someone with the same thing 3. Masks for providers and visitors d. Contact Precautions 1. Used for respiratory syncytial virus (RSV), shigella, wound infections, scabies 2. Private room or room with other patient that has the same infection 3. Gloves and gowns worn by caregivers F. Herpes Zoster (shingles) a. Chickenpox shingles b. Risk factors 1. Concurrent illness, stress, compromise immune system, fatigue, poor nutritional status c. Symptoms: paresthesia, unilateral rash, low grade fever 1. Rash is erythematous, vesicular, pustular, or crusting d. Nursing care 1. Isolate the client until the vesicles have crusted 2. Avoid exposing to infants, pregnant women, and those who not had the chicken pox e. Medications: 1. analgesics- enhance client comfort 2. Antiviral agents- acyclovir f. Complications 1. Postherpetic neuralgia- pain more than 1 month after shingles is gone g. Prevention: Zoster vaccine and chicken pox vaccine 12. CLIENT SAFETY A. Preventing falls a. Patient with orthostatic hypotension should avoid getting up too quickly 1. Sit on side of bed for few seconds, stand up for a few seconds, then walk b. Provide regular toileting c. Place clients at risk for falls close to nurses’ station d. Provide hourly rounding e. Keep bed in low position and lock breaks f. Avoid using all side rails g. Provide nonskid footwear h. Use gait belts B. Seizures a. Sudden surge of electrical activity in the brain b. Do not restrain c. Lower them to the floor put them on their side don’t put anything in their mouth C. Fire Safety Fire Response R-rescue by moving people to a safer location A-alarm- activate facility’s alarm system C-contain- close doors/windows, turn off sources of oxygen E- extinguish the fire Fire Extinguishers P- pull the pin A-aim at base of fire S- squeeze the handle S- sweep the extinguisher side to side 13. HOME SAFETY A. Infants and Toddlers a. Do not feed the infant ad hard foods that could be choking hazard b. Always place infants on their back to rest c. Keep plastic bags to reach d. Make sure crib slats are no more than 2 3/8 inches apart e. Do not place anything in the crib with the infant f. Place toddlers in rear facing car seat in the back seat until 2 years old g. Use car seat with 5-point harness for infants and children h. Place pots on back burner and turn handle away from front of stove B. Preschool age children a. Place locked fences around pools and provide supervision around pools or water b. Use booster seats for children who are less than 4 feet 9 in tall and weigh less than 40 lbs c. If passenger seat has an air bag, place children under 12 years in the back seat d. Use of protective equipment in sports e. Keep firearms unloaded, locked up, and out of reach 1. Store bullets in different location f. Reduce setting on water heater to no higher than 120 degrees F C. Adolescents a. Educate on the hazards of smoking, alcohol, legal, and illegal drugs, and unprotected sex b. Educate on the hazards of driving while distracted c. Be alert ot signs of depression, anxiety, or other behavioral changes D. Older adults a. Remove items that could cause the client to trip, such as throw rugs and loose carpets b. Place electrical cords and extension cords against a wall behind furniture c. Place grab bars near the toilet and in the tub or shower, and install a stool riser d. Use nonskid mat in the tub or shower e. Place shower chair in the shower E. Fire Safety a. use and store oxygen equipment according to the manufacturer’s recommendation b. place a no smoking sign near front of the door c. ensure that electrical equipment is in a good repair and well grounded d. replace bedding that can generate static electricity (wool, nylon, synthetics) with items made from cotton. e. Keep flammable materials such as heating oil and nail polish remover away from the client when oxygen is in use F. Carbon Monoxide a. Very dangerous gas because it binds with hemoglobin and reduces the oxygen supplied to the tissues in the body b. Carbon monoxide cannot be seen, smelled, or tasted c. Symptoms: nausea, vomiting, headache, weakness, unconsciousness d. Gas burning furnaces, water heaters, and appliances should be inspected annually e. Carbon monoxide detectors should be installed and inspected regularly G. Food Poisoning a. Young, old, immunocompromised, and pregnant women are at risk complications b. Perform hand hygiene c. Ensure meet and fish are cooked at correct temperature d. Handling raw and fresh food separately to avoid cross contamination, refrigerated perishable items H. ABCDE principle a. Airway/cervical spine- need patent airway, stabilize cervical spine b. Breathing 1. Exception: COPD patients- O2 saturation is low 90s—expected a. NOT PRIORITY c. Circulation- assess BP, HR, capillary refill d. Disability- determine level of consciousness e. Exposure I. First Aid a. Bleeding 1. Direct pressure to wound site 2. Do not remove impaling objects- instead stabilize them b. Fractures 1. Apply a splint 2. Reassess neurovascular status below the injury c. Sprains 1. RICE a. Rest, ice, compression, elevate d. Frostbite 1. Warm the affected area to 37-42 degrees C (98.6-108 F) water bath 2. Admin tetanus vaccine e. Burns 1. Remove burning agent 2. Elevate clients extremity 3. Admin fluids and tetanus toxoid 14. ERGONOMIC PRINCIPLES A. Body Mechanics a. Spread feet apart to lower center of gravity and broaden base of support 1. Results in greater balance b. Use the major muscle groups to prevent back strain c. Distribute weight between the large muscles of arms and legs d. Hold object as close as possible e. Have a staff member help with positioning clients f. Use smooth movements g. Gurnee bed 1. Bed should be slightly lower 2. Patient’s arms crossed, chin tilted in 3. Put board against feet to prevent foot drop B. Client positions a. Semi-Fowlers- head of the bed elevated 15-45 degrees 1. Prevents regurgitation and aspiration 2. Promotes lung expansion and ventilation b. Fowlers- head of bed elevated 45-60 degrees 1. Useful during nasogastric tube insertion and suctioning 2. Promotes lung expansion and ventilation c. High Fowlers- head of bed elevated 60-90 degrees 1. Promotes lung expansion and ventilation 2. Relieves severe dyspnea 3. Prevents aspiration during meals d. Supine- client lies on back e. Prone- client lies on abdomen 1. Helps prevent hip flexion contractures after a lower extremity amputation f. Sims- client lays on left side and both legs in flexion 1. comfortable sleeping position for many clients 2. used for enema or rectal exams g. Orthopneic- sits at the side of bed with arms on bedside table 1. Promotes lung expansion and ventilation 2. Beneficial for COPD patients h. Trendelenburg- head of bed lower than the foot of the bed i. Reverse Trendelenburg- foot of the bed lower than the head of the bed 1. Promotes gastric emptying for GERD j. Modified Trendelenburg- flat with legs about the level of the heart 1. Prevent and treat hypovolemia or hypovolemic shock 15. SECURITY AND DISASTER PLANS A. Triage a. Class 1: Emergent category (red tag) 1. Highest priority- life threatening injuries b. Class 2: Urgent Category (Yellow tag) 1. Second highest priority- major injuries (ex: bone fracture) c. Class 3: Nonurgent Category (Green tag) 1. Minor injuries (ex: sprain, cut) d. Class 4: Expectant category (black tag) 1. Not expected to live and allowed to die naturally (ex: chest is crushed) B. Tornado a. Close drapes, lower bed to lowest position and move away from windows, place blanket over clients who are confined to bed C. Chemical Incident a. Undress the client b. Irrigate skin with running water 1. Except dry chemicals- then brush the agent off clothes and skin D. Hazardous material a. Identify hazardous material b. Use water E. Bomb threat a. Extend conversation for as long as possible b. Listen for distinguishing background noises to help police 16. HEALTH PROMOTION AND DISEASE PREVENTION A. Tests a. Colorectal screening 1. Every year beginning at age 50 for fecal occult blood testing 2. sigmoidoscopy every 5 years 3. colonoscopy ever 10 years b. Pap Smear (Papanicolaou test) 1. Every 3 years starting at age 21 c. Mammogram 1. Every year starting at age 40 d. Testicular Examination 1. Starting at age 20 e. Prostate exam 1. Starting at age 50 B. Prevention a. Primary Prevention 1. Helps prevent initial occurrence of disease a. Ex: immunization programs, client teaching b. Secondary Prevention 1. Early detection of illness, limiting severity a. Ex: screening c. Tertiary Prevention 1. Maximizing recovery after illness a. Ex: support groups, rehab 17. CLIENT EDUCATION A. Domains of Learning a. Cognitive Learning 1. Thinking, knowledge, comprehension b. Affective learning 1. Feelings, beliefs, values c. Psychomotor learning 1. mental and physical activity B. Assessment a. Assess learning needs b. identifying learning style (auditory, visual, kinesthetic) c. identify available resources C. Planning a. Identify mutually agreeable outcomes D. Implementation a. No medical jargon b. 6th grade level or lower E. Evaluation a. Observe demonstrations 18. SKIP 19. SKIP 20. SKIP 21. SKIP 22. SKIP 23. SKIP 24. SKIP 25. SKIP 26. DATA COLLECTION AND GENERAL SURVEY A. Therapeutic communication a. Don’t do one long assessment try to break it up b. Allow more time for responses for older adults c. Make sure client is comfortable d. Reduce environmental noises 1. Ex: tv, visitors B. Assessments a. Normal order: Inspection, palpation, percussion, auscultation 1. *Exception is abdomen: inspection, auscultation, percussion, palpation b. Inspection 1. Size, shape, color, symmetry, position c. Palpation 1. Size, consistency, texture, temperature, location, tenderness a. Palpate tender areas last 2. Dorsal surface: most sensitive to temperature 3. Palmar surface: sensitive to vibration d. Percussion 1. Size, location, tenderness, density e. Auscultation 1. Amplitude/intensity, pitch/frequency, duration, quality 2. Used for heart sounds, bowel sounds, lung sounds C. General Survey a. Physical Appearance 1. Age, gender race, level of consciousness, signs of distress, signs of substance abuse b. Body structure 1. Height and weight, Nutritional status, posture, abnormalities (amputation, skin lesions) c. Mobility 1. Gait, movements, range of motion d. Behavior 1. Mood, speech e. Vital signs 1. Temperature, pulse, respiration, blood pressure, oxygen saturation 27. VITAL SIGNS A. Temperature a. Ways to take temp 1. Oral: 36-38 C or 96.8 to 100.4 F 2. Rectal: 0.5 C or 0.9 F higher than oral a. 36.5-38.5 or 97.7- 101.1 F b. Patient in sim’s position, lubricate thermometer, place in about 1-1.5 in for adult 3. Axillary: 0.5 C or 0.9 F lower than oral a. 35.5-37.5 C or 95.9-99.3 F 4. Temporal: 0.5 C or 0.9 F higher than oral a. 36.5-38.5 or 97.7- 101.1 F b. Move gently from forehead over the temporal artery and then to skin behind earlobe 5. Tympanic a. Adult: pull ear up and back b. Child younger than 3: pull down and back b. Considerations 1. Newborns: 36.5-37.5 C or 97.7 and 99.5 F 2. Older adults: average temp: 36 C (96.8 F) 3. Hormonal Changes- temp rises with ovulation, menses, and menopause 4. Exercise, activity, and dehydration: development of hyperthermia 5. Recent food, drink, or smoking: wait 20-30 min to take temp c. Complications 1. Hyperthermia- greater than 39 C a. Obtain specimens b. Admin antibiotics c. Provide fluids d. Provide antipyretics e. Prevent shivering- offer blankets 2. Hypothermia- less than 35 C a. Provide warm environmental temperature i. Warming blanket, warmed IV fluids b. Keep head covered B. Pulse a. Rate 1. Normal adult: 60-100 bpm 2. Normal infant: 120-160 bpm b. Rhythm- regularity c. Strength (amplitude) 1. 0= absent 2. 1 = diminished 3. 2 = normal, expected 4. 3 = increased, strong 5. 4 = bounding d. Locate radial pulse 1. If pulse is regular: count rate for 30 sec and multiply by 2 2. If pulse is irregular: count for full min and compare to apical pulse e. Locate apical pulse 1. Fifth intercostal space, left midclavicular line f. Tachycardia- greater than 100 bpm g. Bradycardia- less than 60 bpm C. Respirations a. Physiological responses 1. Chemoreceptors in carotid arteries and the aorta monitor CO2 levels of the blood a. Rising CO2 levels trigger respiratory centers of the brain to increase respiratory rate b. Process of respiration 1. Ventilation- exchange of CO2 between environment and lungs 2. Diffusion- exchange of O2 and CO2 between alveoli and RBC 3. Perfusion- flow of RBC to and from pulmonary capillaries (tissues) c. Assessment 1. Rate a. Normal rate: i. adults= 12-20/min ii. infants= 35-40/min iii. school age kids= 20-30 2. Depth- deep or shallow 3. Rhythm d. Pulse Oximetry 1. Normal 95-100% 2. COPD normal: 91-100% e. Considerations 1. Increased respiratory rate a. Anxiety, smoking, illnesses, anemia, high altitude 2. Decreased respiratory rate a. Opioids, sedative meds, increasing old age D. Blood Pressure a. hypertension Systolic BP Diastolic BP normal <120 <80 Prehypertension 120-139 80-89 Stage 1 hypertension 140-159 90-99 Stage 2 hypertension >160 >100 b. Hypotension- Systolic is less than 90 mmHg c. Pulse pressure=systolic- diastolic 1. Increase pulse pressure can indicate cardiovascular disease d. Orthostatic hypertension- blood pressure that decreases when a client changes position from lying to sitting/standing 1. Take clients BP and HR while lying in supine 2. Then have them sit, wait 1-3 min, take BP again 3. The client has orthostatic hypotension if the Systolic decreases more than 20 mmHg and/or Diastolic decreases more than 10 mmHg with a 10-20% increase in HR e. Auscultatory method 1. Width of a cuff should be 40% of arm circumference 2. The inside of the cuff should surround 80% of the arm circumference a. Too large of cuff: falsely low readings b. Too small of cuff: falsely high readings f. Nursing implications 1. Don’t measure BP: a. in an arm with IV infusion in progress b. side where the client has had a mastectomy 28. HEAD AND NECK A. Cranial Nerves Number Name Function How to test 1 Olfactory Sensory: Smell 2 Optic Sensory: vision Snellen chart 3 Oculomotor Motor: pupil constriction, eye movements Follow the finger, penlight 4 Trochlear Motor: eye movements (up/down) 5 Trigeminal Sensory motor: face, chewing Close eyes- touch face- pt explains what they feel 6 Abducens Motor: eye movement laterally 7 Facial Sensory Motor: Facial muscles, taste (ant), parotid/lacrimal glands Smile/Frown 8 Vestibulocochlear Sensory: hearing and balance 9 Glossopharyngeal Sensory Motor: parotid gland, gag reflex, taste (posterior) Gag reflex 10 Vagus Sensory Motor: voice, pharyngeal/laryngeal muscles, thoracic/abdominal sense 11 Accessory Motor: sternocleidomastoid and trapezius muscle Shrug, turning head 12 Hypoglossal Motor: tongue B. Assess a. Thyroid glands 1. Take sip of water and feeling the thyroid gland as it moves up the trachea a. Sizes, masses, and smoothness b. Eyes 1. 20/30 vision means a client can read a line from 20 ft away that a person who has unimpaired vision can read from 30 ft away 2. Tests: a. Snellen chart- used to screen myopia (nearsightedness) b. Rosenbaum eye chart- used to screen for presbyopia (farsightedness) c. Ishihara Test- color vision d. Corneal light reflex e. Uncover/cover test- Strabismus (misalignment) f. 6 cardinal positions of gaze- wide H pattern 3. PERRLA a. P- pupils clear b. E- equal and between 3-7 mm c. R- round d. RL- reactive to light e. A- accommodation of pupils 4. 2 arteries for every 3 veins c. Ears 1. Check alignment 2. Pull auricle a. Adults: Up and back b. Young children: down and back 3. Insert otoscope 1-1.5 cm bur do not touch ear canal a. Expect to see: pearly gray and intact tympanic membranes i. Light reflex is visible ii. Normal amount of cerumen 4. Tests: a. Whisper test b. Rinne test c. Weber test i. Negative is normal C. Changes with aging a. Eyes: decreased visual acuity, glare/darkness, yellowing of the lens b. Ears: hearing loss, thickening of the tympanic membrane c. Mouth: decreased sense of taste, tooth loss, pale gums, gum disease, decreased salivation d. Voice: rise in pitch e. Nose: decreased sense of smell 29. THORAX, HEART, AND ABDOMEN A. Breasts a. Monthly self-exams after menstruation B. Lungs a. Percussion 1. Dullness: indicates pneumonia 2. Hyperresonance: pneumothorax, emphysema b. Auscultation 1. Expected: bronchial, bronchovesicular, vesicular 2. Unexpected: crackles (fluid), wheezes, rhonchi, pleural friction rub C. Heart a. S1 sound: mitral and tricuspid close b. S2 sound; aortic and pulmonic close c. Thrills: vibration murmurs d. Bruits: swishing sound obstructed blood flow e. Auscultatory sites: 1. Aortic, Pulmonic, Erbs’ point, Tricuspid, Apical D. Abdomen a. Bowel sounds 1. Expected: high pitched clicks and gurgles 2. Unexpected: loud, growling sounds b. Percussion 1. Expect to hear tympany 2. Expect dullness over liver a. Liver size: 6-12 cm c. Palpate tender areas last E. Expected Changes with Aging a. Breasts 1. Nipples can invert b. Lungs 1. AP diameter similar to transverse diameter (barrel chest) 2. Alveoli dwindle 3. Kyphosis becomes presen c. Cardiovascular 1. Systolic hypertension 2. Blood vessels thicken 3. Increase pulse pressure d. Abdomen 1. More adipose tissue 2. Decrease saliva, gastric secretions, pancreatic enzymes 3. Decrease motility 30. INTEGUMENTARY AND PERIPHERAL VASCULAR SYSTEMS A. Skin a. Pallor- loss of color 1. Indicates: anemia, shock, or lack of blood flow b. Cyanosis- turning blue 1. Indicates: hypoxia c. Jaundice- yellow tint 1. Indicates: liver dysfunction, RBC destruction d. Erythema – redness 1. Indicates: inflammation, sun exposure, rash e. Brown pigmentation indicates venous insufficiency f. Skin turgor can indicate dehydration or aging B. Nails a. Capillary refill- normal return of color within 3 seconds C. Edema a. Evaluate pitting by compressing the skin for at least 5 seconds over a bony prominence 1. trace, 2 mm, rapid skin response 2. mild, 4 mm, 10-15 seconds skin response 3. moderate, 6 mm, prolonged, skin response 4. severe, 8 mm, prolonged skin response D. Lesions Primary Lesions Macule Flat, skin color change, < 1 cm Ex: freckle, petechiae Papule Solid elevation of skin, < 1 cm Ex: mole Nodule Deep, firm, 1-2 cm Ex: wart Vesicle Serous fluid- filled, < 1 cm Ex: blister, herpes, varicella Pustule Pus filled, varies in size Ex: acne Tumor Solid mass, deep, > 2 cm Ex: epithelioma, neoplasm Wheal Palpable, irregular borders, edematous Ex: insect bite Primary Lesions Erosion Loss of epidermis, moist, no bleeding Ex: popped blister, ruptured vesicle Crust Dried blood, serum, pus (elevated) Ex: scab Scale Flakes of skin Ex: dandruff, psoriasis, eczema Fissure Linear crack Ex: tinea pedis Ulcer Loss of epidermis and dermis, scarring Ex: pressure ulcer E. Expected changes with aging a. Dry, flaky skin b. Loss of elasticity c. Thinning of hair d. Less moisture and sweat e. Uneven pigmentation f. Slow wound healing g. Little subcutaneous tissue over bony prominences 31. MUSCULOSKELETAL AND NEUROSENSORY SYSTEMS A. Expected range of motion of joint movement Flexion Decreases the angle between 2 adjacent bones Extension Increases the angle between 2 adjacent bones Supination Ventral (front) surface faces up Pronation Ventral (front) surfaces faces down Abduction Moving extremity away from midline Adduction Moving extremity towards the midline Dorsiflexion Foot and toes upward Plantar flexion Foot and toes downward Eversion Turning body part away from midline Inversion Turning body part toward the midline External Rotation Rotating a joint outward Internal Rotation Rotating a joint inward B. Curvatures of the Spine a. Expected: concave cervical spine, convex thoracic spine, concave lumbar spine, convex sacral spine b. Unexpected: 1. Kyphosis- hunchback (in older adults) 2. Lordosis- exaggerated curvature of lumbar spine (toddler years and pregnancy) 3. Scoliosis- S shape C. Mental Status a. Alert 1. Client is responsive and can open eyes and respond spontaneously and appropriately b. Lethargic 1. Client can open eyes but falls asleep readily c. Obtunded 1. Responds to light shaking and can be confused and slow to respond d. Stuporous 1. Requires painful stimuli (rubbing the sternum) e. Comatose- no response 1. Decorticate rigidity- flexion and internal rotation of upper extremity joints and legs(arms-chin) 2. Decerebrate rigidity- neck and elbow extension, with wrists and fingers flexed (arms extended) a. Worse than decorticate D. Glasgow Coma Scale- baseline of level of consciousness a. Looks at eye, verbal, and motor 1. Highest value possible is 15 2. <8 indicates severe head injury 3. 8-12 indicates mild head injury E. Motor Function a. Assessing balance 1. Romberg’s Test a. Ask the client to stand with feet together, his arms at his sides and his eyes closed i. Expected findings: client stands with minimal swaying for at least 5 seconds 2. Heel-to-toe walk: heel to tow and walk in straight line F. Sensory Function a. Stereognosis- place familiar object in the client’s hand and ask them to identify it b. Graphesthesia- trace number on clients hand G. Grade DTR Response a. 4 very brisk with clonus b. 3 brisker than average c. 2 expected d. 1 diminished e. 0 no response H. Expected changes with aging a. Musculoskeletal system 1. Reduced muscle mass 2. Osteoporosis, loss of bone mass 3. Degenerative alterations in joints 4. Limited range of motion b. Neurological system 1. Short term memory decline 2. Diminished, slowed reflex 3. Altered hearing, vision, smell, and deep pain 32. THERAPEUTIC COMMUNICATION What to do: Do not - Use open ended questions (“tell me more”) -offer personal information but quickly return focus onto the patient -ask why -offer opinion -false reassurance -closed ended question(yes/no) -change subject -minimize patient’s feelings - say “I know how you feel” 33. COPING A. General Adaptation Syndrome a. Alarm Reaction- heightened response to stressors 1. Increased blood pressure and heart rate 2. Cortisol released b. Resistance Stage- body functions normalize while responding to the stressor 1. Body returns to homeostasis c. Exhaustion Stage- body functions are no longer able to maintain a response to the stressor 1. Can result in fatigue, depression 34. SELF CONCEPT AND SEXUALITY A. Impaired body image a. Due to amputation, mastectomy, hysterectomy b. loss of body function due to arthritis, spinal cord injury, or stroke 35. CULTURAL AND SPIRITUAL NURSING CARE A. Spirituality a. Christianity 1. may fast during lent b. Islam 1. Women must be cared for by female providers 2. May pray 5 times a day 3. Avoid alcohol and pork 4. Fast during Ramadan c. Jehovah’s Witness 1. Might night accept blood transfusions d. Judaism 1. Some practice a kosher diet a. No shellfish, pork, or meat with dairy e. Mormonism 1. Avoid alcohol, tobacco and caffeine B. Ethnocentrism a. Belief one’s own culture is superior to all other cultures 1. Nurses should avoid this C. Interpreter a. Use facility approved medical interpreter 1. Do not use family/ friends of patient or non-designated employee to interpret b. Only ask one question at a time c. Direct the questions to the client d. Use lay terminology 36. GRIEF, LOSS, AND PALLIATIVE CARE A. Types of Loss a. Maturational loss 1. Loss that is expected, it is associated with normal life transitions a. Ex: child leaving home for college b. Situational Loss 1. Unanticipated loss caused by an external event a. Ex: car accident B. Stages of Grief a. Denial- patient has difficulty believing a terminal diagnosis or loss b. Anger- client lashes out at other people or things c. Bargaining- client negotiates for more time or a cure d. Depression- client is overwhelmingly sad e. Acceptance- client moves forward C. Types of grief a. Anticipatory grief- grief before having a loss (ex: terminal illness) b. Complicated grief- prolonged, severe grief 1. No acceptance of the loss after 6 months D. Palliative Care vs hospice care a. Palliative care- symptom relief and cure b. Hospice care- includes palliative care but down not look for cure 1. Patients are not expected to live longer than 6 months] E. Manifestations of approaching death a. Decreased level of consciousness, labored breathing, mottling (cyanosis), slow/weak pulse, dropping blood pressure, decreased urine output b. Hearing is not diminished F. Preparing the body for viewing a. Remove all tubes and personal belongings and excess supplies b. Lay the body supine with pillow under the bed c. Apply fresh linens, put dentures in, dim the lights 37. HYGIENE A. Foot care a. Important for diabetic patients 1. May experience decreased sensations a. Variations in temperature b. Can’t tell if something is in shoe (Ex: nail in foot) 2. Inspect feet daily, cut nails straight across, check shoes for objects, wear cotton socks 3. Test water temperature for bath 4. Dry feet thoroughly- especially in between toes 5. Apply moisturizer on feet (not in between toes) 6. Do not use over the counter products- go to podiatrist 7. Do not use heating pad on feet B. Oral Care for unconscious patient a. Have suction apparatus ready- prevent aspiration b. Position client on his side with his head turned toward you to allow oral secretions to collect c. Denture care: 1. Top denture: pull down and out 2. Bottom denture: pull up and out 3. Store dentures in denture cup 38. REST AND SLEEP A. Sleep Cycle NREM Stage 1 NREM Stage 2 NREM Stage 3 NREM Stage 4 REM Very light sleep Only a few minutes long Vital signs and metabolism beginning to decrease -Deeper sleep -10-20 min long -Vital signs and metabolism beginning to decrease -initial stages of deep sleep -15-20 min long -difficult to awaken -deepest sleep -15-30 min long -vital signs low - very difficult to awaken - physiologic rest and restoration -sleep walking, sleep talking - vivid dreaming -longer with each sleep cycle -average length 20 min -varying vital signs -very difficult to awaken -cognitive restoration B. Sleep Apnea a. More than 5 breathing cessations lasting longer than 10 seconds per hour during sleep b. CPAP mask C. Factors that interfere with sleep a. Caffeine consumption, heavy meals before bedtime b. Exercise promotes sleep if at least 2 hours before bedtime 39. NUTRITION AND ORAL HYDRATION A. Basic Nutrients the body requires a. Carbohydrates 1. Provide most of the body’s energy 2. Each gram produces 4 kcal b. Fats 1. Provides energy and vitamins 2. No more than 35% of caloric intake should be from fat 3. Each gram produces 9 kcal c. Proteins 1. Repairs body tissues 2. Each gram produces 4 kcal 3. Important for wound healing d. Vitamins 1. Fat soluble vitamins A, D, E, K 2. Water soluble vitamins C and B complex B. Age a. Newborn 1. Breast milk and formula used during the first full year of life 2. Solid food starting at 4-6 months a. No cows milk or honey for the first year b. Older adults 1. Slower metabolic rate requires fewer calories 2. Thirst sensations diminish 3. Calcium is important for both men and women C. BMI a. Weight (kg) divided by height (m2) b. Scale: 1. <18= underweight 2. 18.5-24.9=healthy 3. 25-29.9= overweight 4. 30>= obese D. Diets a. Clear liquid- water, tea, coffee, broth, clear juices, gelatin, ginger ale b. Full liquid- milk, pudding, fruit, ice cream, juice c. Pureed- pureed meats, fruits, scrambled eggs 1. used if jaw is wired shut or after oral surgery d. Mechanical soft- diced or ground foods 1. Used if patient does not have teeth e. Low residue- low in fiver and easy to digest 1. Used for IBS or other GI disorders E. Dysphagia a. See Speech pathologist b. Semi fowlers position c. Thickened liquids d. Check for food pockets e. Tuck chin to chest when swallowing f. Monitor patient during meals g. Suction equipment ready h. Avoid straws 40. MOBILITY AND IMMOBILITY A. Respiratory a. Nursing interventions 1. Reposition every 1-2 hours 2. Instruct clients to turn, cough, and breathe deeply every 1-2 hours while awake 3. Instruct clients to use an incentive spirometer while awake 4. Instruct clients to consume at least 2000 mL fluid per day, unless intake is restricted B. Instructions a. Cane 1. maintain 2 points of support on the ground at all times 2. Keep the cane on the stronger side of the body 3. Support body weight on both legs move cane forward 6-10 in 4. Move weaker leg forward, then move stronger leg past the cane b. Crutches 1. Do not alter crutches after fitting a. 3 finger widths between axilla and the top of the crutch 2. Support body weight at the hand grips with elbows flexed (20-30 degrees) 3. Stairs- hold rail with one hand and crutches in the other C. DVT a. Symptoms: pain, edema, warmth, and erythema b. Nursing actions 1. Notify provider immediately 2. Position client with leg elevated, give anticoagulants c. Anti-embolic stockings [Show More]
Last updated: 7 months ago
Preview 1 out of 51 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 09, 2023
Number of pages
51
Written in
Additional information
This document has been written for:
Uploaded
Oct 09, 2023
Downloads
0
Views
134


.png)








.png)