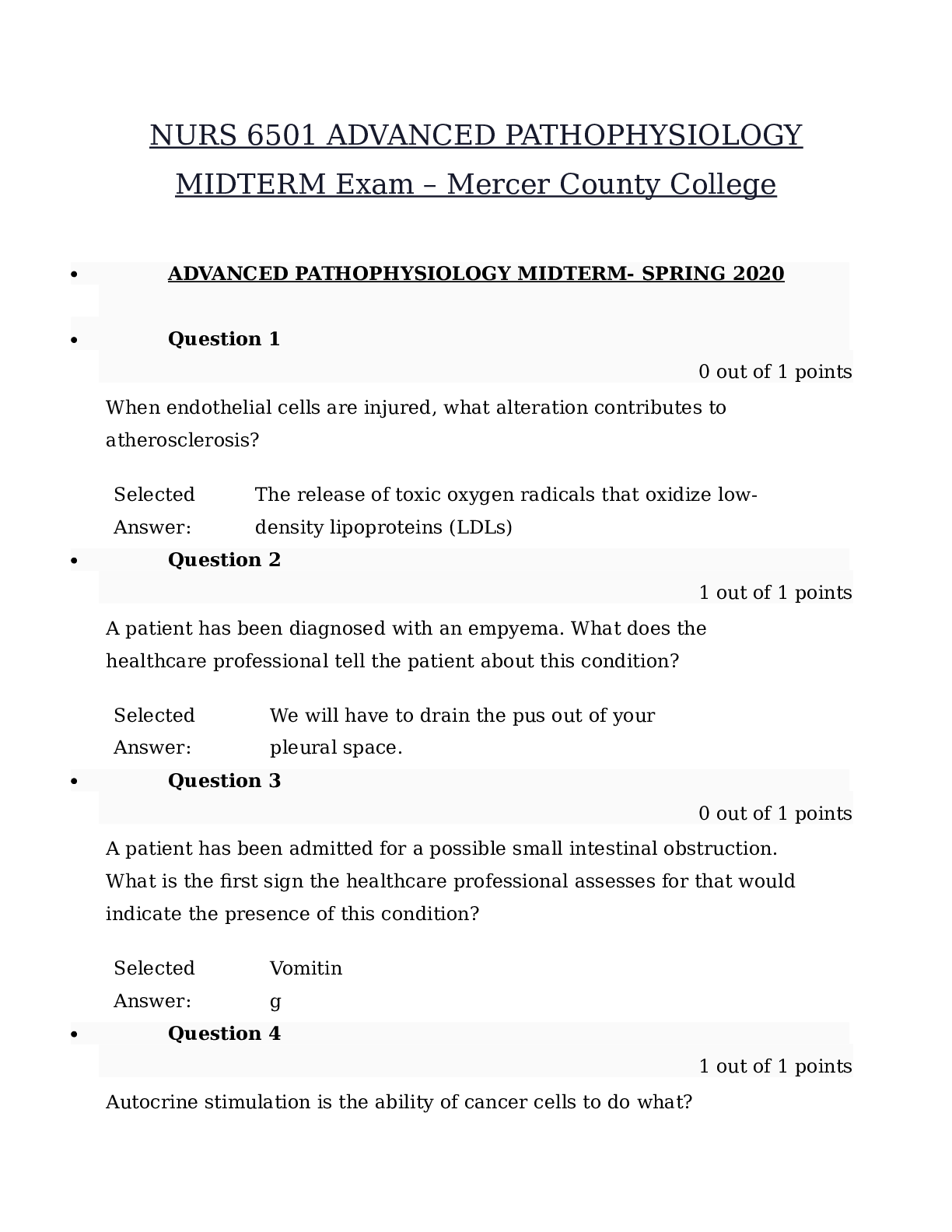
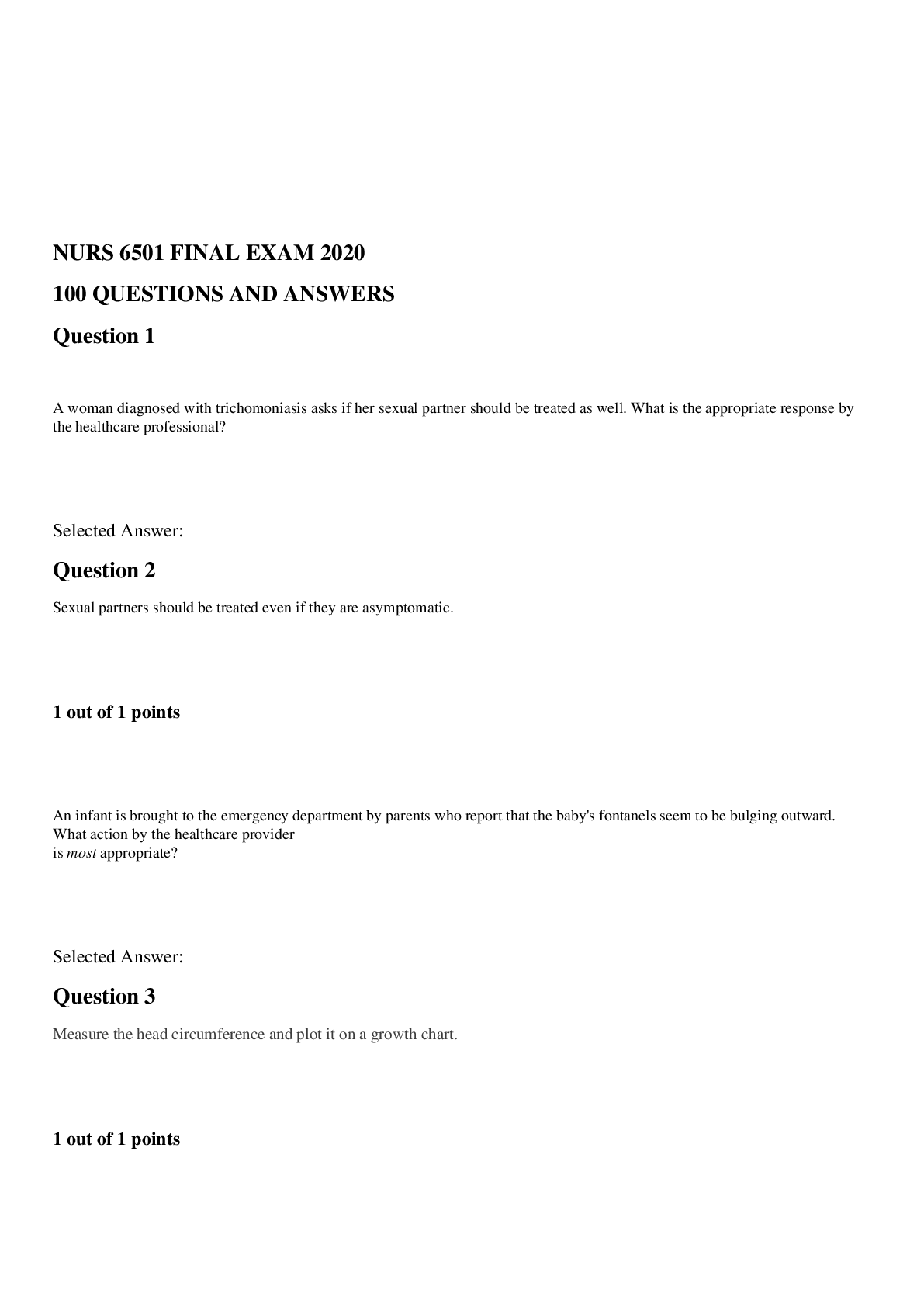
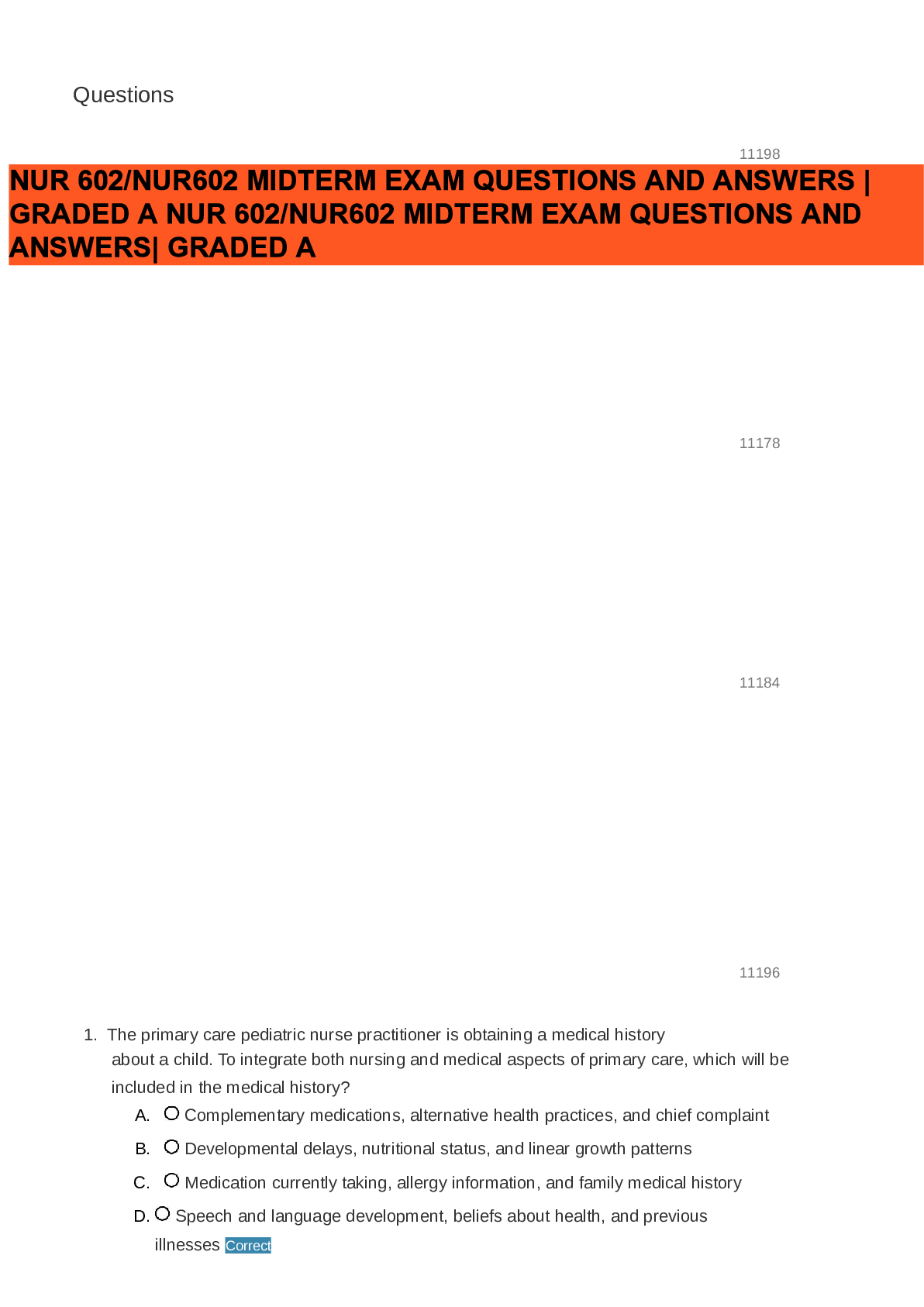
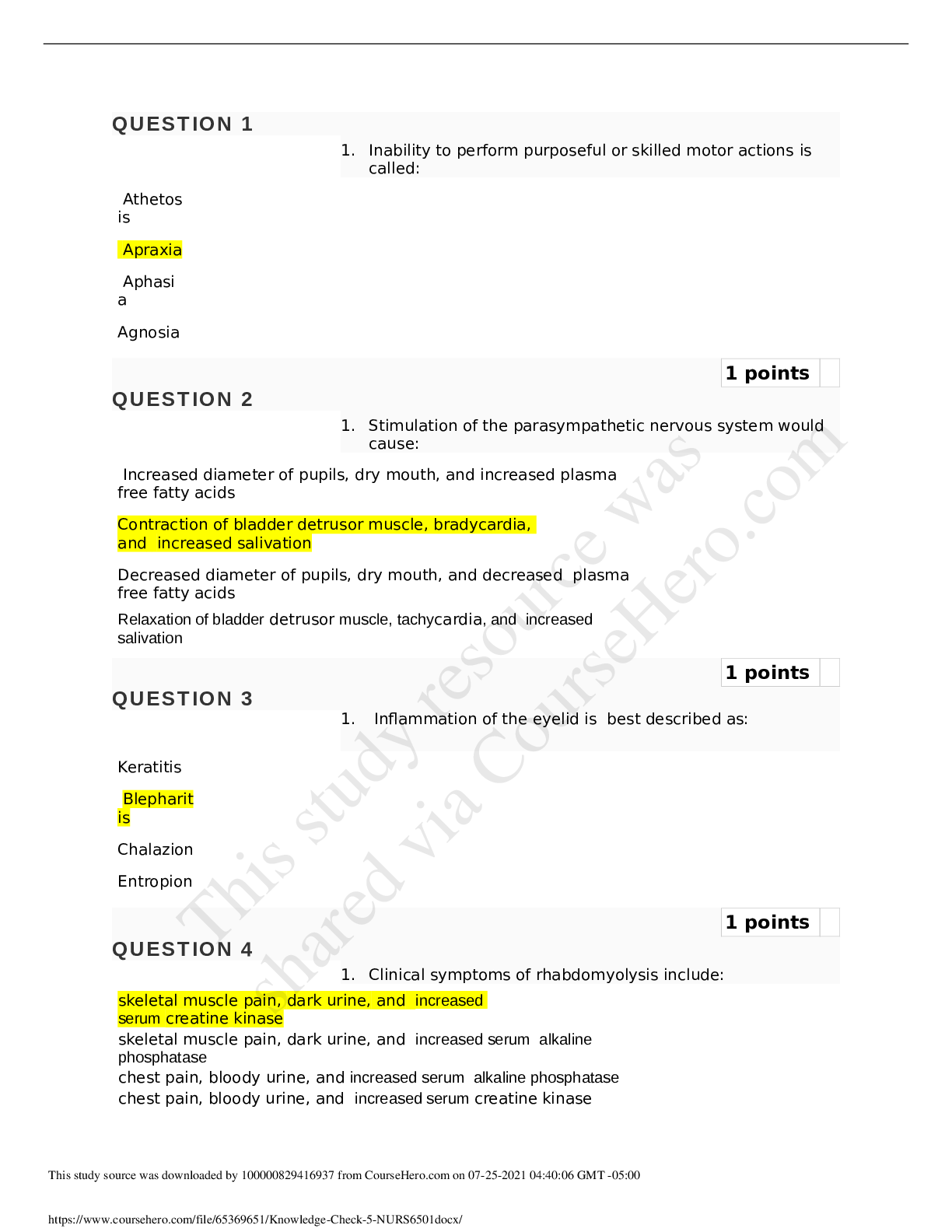
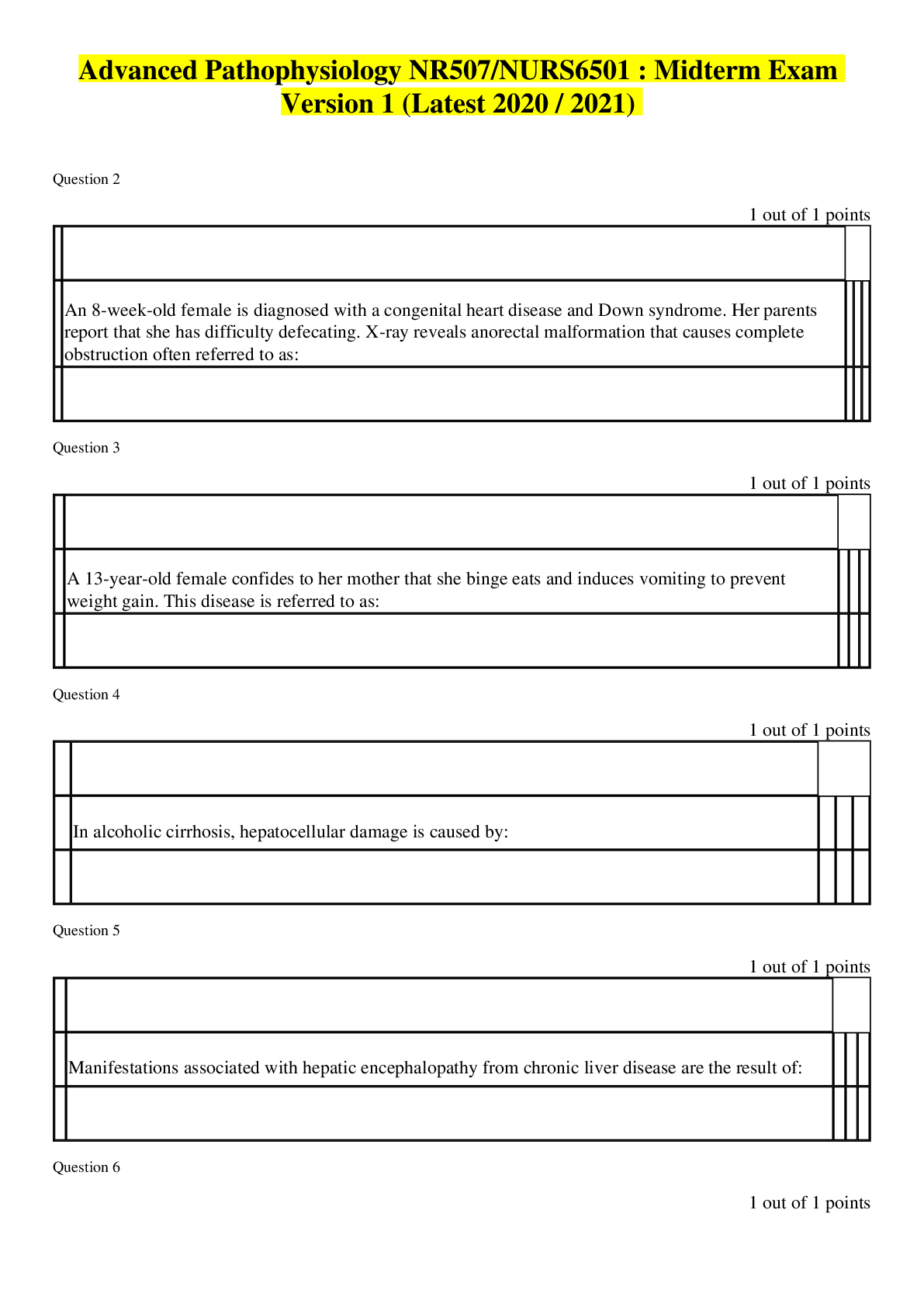
*NURSING > QUESTIONS & ANSWERS > Walden Universty NURS 6501 Advanced Pathophysiology Module 3 Knowledge Check: GI and Hepatobiliary D (All)
Walden Universty NURS 6501 Advanced Pathophysiology Module 3 Knowledge Check: GI and Hepatobiliary Disorders. (answered)
Document Content and Description Below
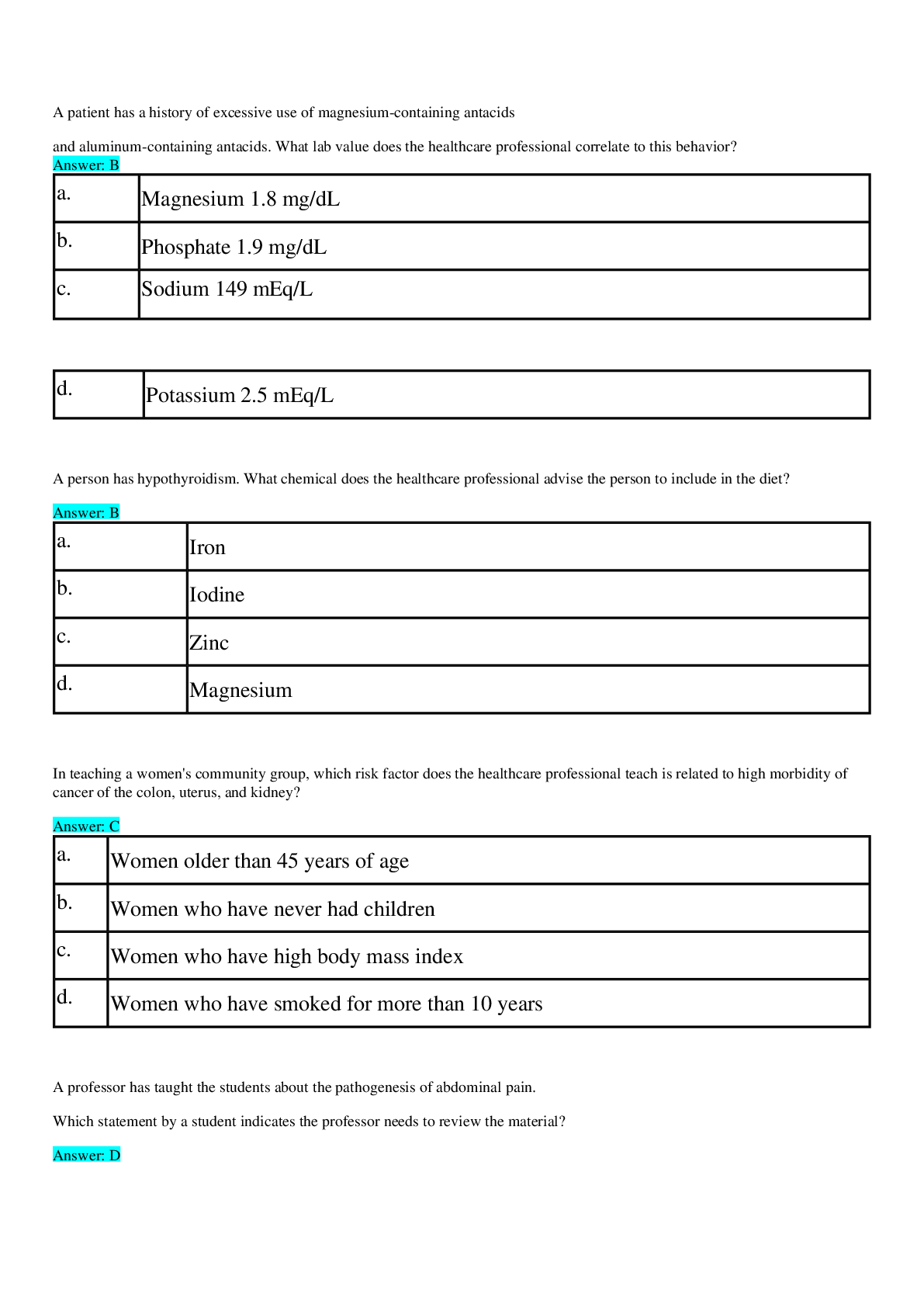
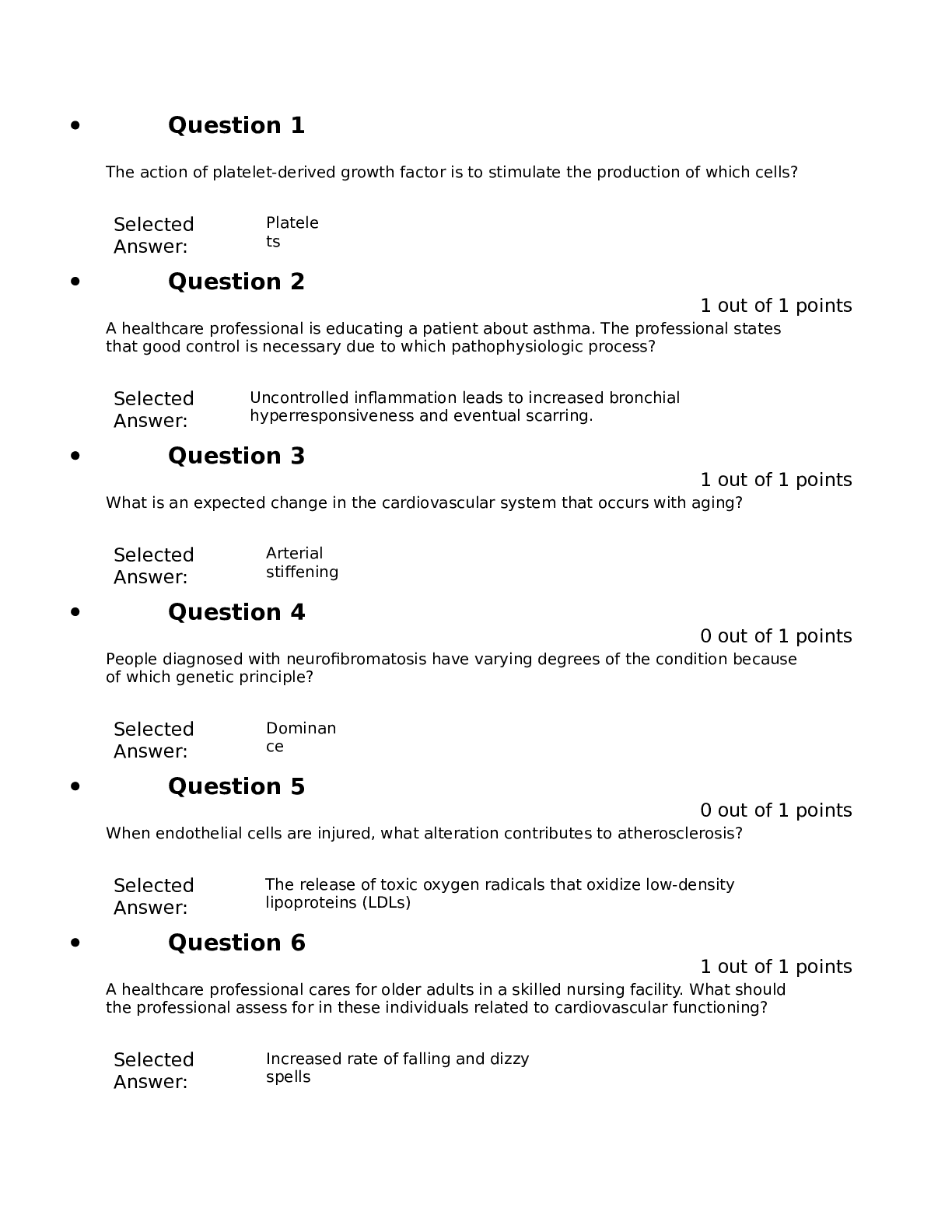
NURS 6501 Module 3 Knowledge Check: GI and Hepatobiliary Disorders: A 45-year-old male comes to the clinic with a chief complaint of epigastric abdominal pain that has persisted for 2 weeks. He de... scribes the pain as burning, non-radiating and is worse after meals. He denies nausea, vomiting, weight loss or obvious bleeding. He admits to bloating and frequent belching. PMH: osteoarthritis; seasonal allergies with frequent sinusitis infections Meds: Zyrtec 10mg daily year-round; Ibuprofen 400-600mg prn pain Family Hx: non-contributory Social hx: recently divorced and expressed concern at how expensive it is to support 2 homes. Works as a manager at a local tire and auto company. He has 25 pack/year hx of smoking; drinks 2-3 beers/day; and drinks 5-6 cups of coffee/day. He denies illicit drug use, vaping or unprotected sexual encounters Breath test in office revealed + urease The healthcare provider suspects the client has peptic ulcer disease. What factors may have contributed to the development of PUD? How do these factors contribute to the formation of peptic ulcers? A 36-year-old morbidly obese female comes to the office with a chief complaint of “burning in my chest and a funny taste in my mouth.” The symptoms have been present for years but patient states she had been treating them with antacid tablets which helped until the last 4 or 5 weeks. She never saw a healthcare provider for that. She says the symptoms get worse at night when she is lying down and has had to sleep with 2 pillows. She says she has started coughing at night which has been interfering with her sleep. She denies palpitations, shortness of breath or nausea. PMH: HTN; venous stasis ulcers; IBS; OA of knees; morbid obesity Family hx: non-contributory Meds: Amlodipine 10mg QD; Dicyclomine 20mg QD; Motrin 600mg q6hrs prn Social: 15 pack/year hx of smoking; occasional alcohol use; denies vaping The healthcare provider diagnoses the patient with GERD. The client asks the APRN what causes GERD. What is the APRN’s best response? A 34-year-old construction worker presents to his PCP with a chief complaint of passing foul smelling dark, tarry stools. He stated the first episode occurred last week, but it was only a small amount after he had eaten a dinner of beets and beef. The episode today was accompanied by nausea, sweating, and weakness. He states he has had some mid epigastric pain for several weeks and has been taking OTC antacids. The most likely diagnosis is upper GI bleed which won’t be confirmed until further endoscopic procedures are performed. What factors can contribute to an upper GI bleed? A 64-year-old steel worker presents to his PCP with a chief complaint of passing bright red blood when had a BM that morning. He stated the first episode occurred last week, but it was only a small amount after he had eaten a dinner of beets and beef. The episode today was accompanied by nausea, sweating and weakness. He states he has had some LLQ pain for several weeks but described it as “coming and going.” He says he has had a fever and abdominal cramps that have worsened this morning. The likely diagnosis is lower GI bleed secondary to diverticulitis. What can cause diverticulitis in the lower GI tract? A 48-year-old man presents to his GI MD for increasing abdominal girth and increasing jaundice. He has a long hx of alcoholic cirrhosis and has multiple admissions for encephalopathy and GI bleeding from esophageal varices. He has been diagnosed with portal HTN and tells the APRN that he was told he had chronic, non-curable cirrhosis. How does cirrhosis cause portal HTN? A 48-year-old man presents to his GI MD for increasing abdominal girth and increasing jaundice. He has a long hx of alcoholic cirrhosis and has multiple admissions for encephalopathy and GI bleeding from esophageal varices. He has been diagnosed with portal HTN. The increased abd girth has been progressive, and he says it is getting hard to breathe. The APRN reviews his last labs and notes that the total protein is 4.6 gm/dl and albumin is 2.9 g/dl. Upon exam, he has icteric sclera, jaundice, and abd spider angiomas. There is a significant fluid wave when percussed. The APRN tells the patient that he has ascites. Explain how ascites develops as a result of portal HTN. A 45-year-old man with known alcoholic cirrhosis, portal HTN, and ascites is brought into the ED by his family due to increasing confusion. The family states that he had been stumbling for several days but had not fallen. The family also noted that he had been “flapping his hands” as well. Labs revealed: Hgb 9.4 Hct 28 ammonia 159. The APRN informs the family that the patient has developed hepatic encephalopathy. Explain how hepatic encephalopathy develops in patients with cirrhosis of the liver. A 65-year-old man with a hx of a-fib presents to his PCP’s office 2 months after suffering a MI. He declined anticoagulation due to fear he would bleed to death. He has had sudden onset, moderately severe diffuse abd pain that began 18 hours ago. He has been vomiting, and has had several episodes of diarrhea, the last of which was bloody. He has a fever of 100.9. CBC reveals WBC of 15,000. What is the most likely mechanism behind his current symptoms? A 46-year-old white female presents to her PCP’s office with a chief complaint of severe, intermittent RUQ pain for the last 3 days. The pain is described as sharp and has occurred after eating French fries and cheeseburgers and radiates to her right shoulder. She has had a few episodes of vomiting “green stuff.” States had fever and chills last night which precipitated her trip to the office. She aloso had some dark orange urine, but she thought she was dehydrated. Physical exam: slightly obese female with icteric sclera as well as generalized jaundice. Temp 101, pulse 108, resp 18. Abd exam revealed rounded abd with slightly hypoactive BS. + rebound tenderness on palpation of RUQ. No tenderness or rebound in epigastrium or other quadrants. Labs show elevated WBC, elevated serum ALT and AST. Serum bili 2.5. Abd US demonstrated enlarged GB, dilated common bile duct and multiple stones in the bile duct. The APRN diagnoses the patient with acute cholecystitis and refers her to the ED for further treatment. Describe how gallstones are formed and why they caused the symptoms that the patient presented. Explain how the patient became jaundiced. Ruth is a 49-year-old office worker who presents to the clinic with a chief complaint of abd pain x 2 days. The pain has significantly increased over the past 6 hours and is now accompanied by N/V. the pain is described as “sharp and boring” in mid epigastrum radiating to the back. Ruth admits to a long hx of alcohol abuse, and often drinks up to a 1/5 of vodka daily. Physical Exam: Temp 102.2 BP 90/60, Resp 22. Pulse ox 92% RA General: thin, pale white female in obvious pain and leaning forward. Moving around on exam table and unable to sit quietly. CV: tachycardic. RRR without gallops, rubs, clicks or murmurs Resp: decreased BS in both bases with poor inspiratory effort ABD: epigastric guarding with tenderness. No rebound tenderness. Negative Cullen’s and + Turner’s signs observed. Hypoactive BS x 2 upper quads and no bowel sounds in both lower quads. The APRN makes a tentative dx of acute pancreatitis based on hx and physical exam and has the patient transferred to the ER where lab and xrays reveal acute pancreatitis. Explain how pancreatitis develops and the role alcohol played in this patient’s case. A 23-year-old bisexual man with a hx of IV drug abuse presents to the clinic with a chief complaint of fever, fatigue, loss of appetite, N/V, abd pain, and dark urine. He says the symptoms started about a month ago and have gotten steadily worse. He admits to reusing needles and had unprotected sexual relations with a man “a couple of months ago.” PMH: noncontributory Social/family hx: works occasionally as a night clerk in a hotel. Parents without illnesses. Admits to bisexual sexual relations and IV heroin use. He has refused drug rehab. 3 year/pack hx of tobacco but denies vaping Physical exam: unremarkable except for palpable liver edge 2 fingerbreadths below costal margin. No ascites or jaundice appreciated. The APRN suspects the patient has Hepatitis B given the strong hx of risk factors. She orders a hepatitis panel which was positive for acute Hepatitis B. What are the important hepatitis markers that indicated the patient had acute hepatitis B? Hannah is a 19-year-old college sophomore who came to Student Health with a chief complaint of lower abdominal pain. She says the pain has been present for 2 months and she has had multiple episodes of diarrhea alternating with constipation and anorexia. She says she has lost about 10 pounds in last 2 months without dieting. The abd pain has gotten worse in the last 2 hours, but she thought she had the “GI bug,” like other students at her synagogue had. Physical exam: noncontributory except for the abd which was lightly distended with no visible masses. Normoactive BS x 4. Diffuse tenderness throughout but increased pain on deep palpation LUQ and LLQ. Slight guarding but no rebound tenderness or rigidity. Rectal: tight anal sphincter and patient grimacing in pain during exam. Slightly + guaiac stool. Based on her hx and current symptoms, the APRN arranges for a consult with a GI who diagnoses Hannah with ulcerative colitis. How does ulcerative colitis develop in a susceptible person? A 64 year old woman with long standing CAD presents to the clinic with lower extremity swelling, abd distention, and SOB. Patient states she had a 30 lb weight gain in 6 weeks and is now requiring 3 pillows to sleep. Physical: well developed, well nourished female exhibiting signs of resp distress with use of accessory muscles. BP 150/80 HR 105 R 28 and labored Weight 89 kg HEENT was unremarkable. Cardiac: S1, S2 and S3 without S4 or murmur. Respiratory: + for bilateral rales ½ up both lung fields. Abdomen: enlarged with a positive fluid wave. Lower extremities: remarkable for 3+ pitting edema Labs: K increased from 3.4 to 6.1 in 2 weeks; BUN increased from 18 to 104; crea increased from 0.8 to 6.9 CXR: revealed CHF The APRN calls the cardiologist on call who admits the patient to the hospital and orders a nephrology consult. She was dx with exacerbation of CHF and AKI. What type of AKI does the patient have and what factors contributed to this dx? The APRN is giving a pathophysiology lecture to APRN students on renal blood flow, related hormones, and glomerular filtration rate. What would be the most important concept of glomerular filtration rate that the APRN should address? The APRN is giving a pathophysiology lecture to APRN students on renal blood flow, related hormones, and glomerular filtration rate, autoregulation, and related hormone factors regulating renal blood flow. What would be the most important concept of autoregulation that the APRN should address? The APRN is giving a pathophysiology lecture to APRN students on renal blood flow, related hormones, and glomerular filtration rate, autoregulation, and related hormone factors regulating renal blood flow. What would be the most important concept of hormonal regulation that the APRN should address? A 28-year-old female comes to the clinic with chief complaint of right flank pain, urinary frequency, and foul-smelling urine. The symptoms have been present for 3 days, but this morning the patient states she had a fever of 101 and she thought she should get checked out. Physical: noncontributory with exception of right costovertebral angle tenderness upon percussion Urine dipstick + blood, + bacteria + WBC Renal US: right staghorn renal calculus Patient was dx with acute pyelonephritis. How does a renal calculi contribute to acute pyelonephritis? Mr. Kent is a 45-year-old AA male with a hx of T2DM, HTN and HLD. His renal function has slowly decreased over the past 4 years and his nephrologist has told him that his GFR has decreased to 15 cc and will soon need renal dialysis for chronic renal failure. How does chronic renal failure develop? [Show More]
Last updated: 10 months ago
Preview 1 out of 12 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 07, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Feb 07, 2021
Downloads
1
Views
109

.png)
.png)



.png)