*NURSING > HESI > Med SURG Practice Exam - Questions And Answers From Evolve HESI/ Complete Solution (All)
Med SURG Practice Exam - Questions And Answers From Evolve HESI/ Complete Solution
Document Content and Description Below
Med SURG Practice EXAM Questions The nurse is assessing a client's laboratory values following administration of chemotherapy. Which lab value leads the nurse to suspect that the client is ex... periencing tumor lysis syndrome (TLS)? A Serum PTT of 10 seconds. B Serum calcium of 5 mg/dl. Correct C Oxygen saturation of 90%. D Hemoglobin of 10 g/dl. TLS results in hyperkalemia, hypocalcemia, hyperuricemia, and hyperphosphatemia. A serum calcium level of 5 (B), which is low, is an indicator of possible tumor lysis syndrome. (A, C, and D) are not particularly related to TLS. Awarded 0.0 points out of 1.0 possible points. 2. ID: 6974889585 A client is admitted to the hospital with a diagnosis of severe acute diverticulitis. Which assessment finding should the nurse expect this client to exhibit? A Lower left quadrant pain and a low-grade fever. Correct B Severe pain at McBurney's point and nausea. C Abdominal pain and intermittent tenesmus. D Exacerbations of severe diarrhea. Left lower quadrant pain occurs with diverticulitis because the sigmoid colon is the most common area for diverticula, and the inflammation of diverticula causes a low-grade fever (A). (B) would be indicative of appendicitis. (C and D) are symptoms exhibited with ulcerative colitis. Awarded 0.0 points out of 1.0 possible points. 3. ID: 6974891763 During CPR, when attempting to ventilate a client's lungs, the nurse notes that the chest is not moving. What action should the nurse take first? A Use a laryngoscope to check for a foreign body lodged in the esophagus. B Reposition the head to validate that the head is in the proper position to open the airway. Correct C Turn the client to the side and administer three back blows. D Perform a finger sweep of the mouth to remove any vomitus. The most frequent cause of inadequate aeration of the client's lungs during CPR is improper positioning of the head resulting in occlusion of the airway (B). A foreign body can occlude the airway, but this is not common unless choking preceded the cardiac emergency, and (A, C and D) should not be the nurse's first action. Awarded 0.0 points out of 1.0 possible points. 4. ID: 6974891794 A client is admitted to the hospital with a medical diagnosis of pneumococcal pneumonia. The nurse knows that the prognosis for gram-negative pneumonias (such as E. coli, Klebsiella, Pseudomonas, and Proteus) is very poor because A they occur in the lower lobe alveoli which are more sensitive to infection. B gram-negative organisms are more resistant to antibiotic therapy. Correct C they occur in healthy young adults who have recently been debilitated by an upper respiratory infection. D gram-negative pneumonias usually affect infants and small children. The gram-negative organisms are resistant to drug therapy (B) which makes recovery very difficult. Gram-negative pneumonias affect all lobes of the lung (A). The mean age for contracting this type of pneumonia is 50 years (C and D), and it usually strikes debilitated persons such as alcoholics, diabetics, and those with chronic lung diseases. Awarded 0.0 points out of 1.0 possible points. 5. ID: 6974891705 A client is placed on a mechanical ventilator following a cerebral hemorrhage, and vecuronium bromide (Norcuron) 0.04 mg/kg q12 hours IV is prescribed. What is the priority nursing diagnosis for this client? A Impaired communication related to paralysis of skeletal muscles. Correct B High risk for infection related to increased intracranial pressure. C Potential for injury related to impaired lung expansion. D Social isolation related to inability to communicate. To increase the client's tolerance of endotracheal intubation and/or mechanical ventilation, a skeletal-muscle relaxant, such as vecuronium, is usually prescribed. Impaired communication (A) is a serious outcome because the client cannot communicate his/her needs due to intubation and diaphragmatic paralysis caused by the drug. Although this client might also experience (D), it is not a priority when compared to (A). Infection is not related to increased intracranial pressure (B). The mechanical venilator provides consistent lung expansion (C). Awarded 0.0 points out of 1.0 possible points. 6. ID: 6974890435 When preparing a client who has had a total laryngectomy for discharge, what instruction is most important for the nurse to include in the discharge teaching? A Recommend that the client carry suction equipment at all times. B Instruct the client to have writing materials with him at all times. C Tell the client to carry a medic alert card stating that he is a total neck breather. Correct D Tell the client not to travel alone. It is imperative that total neck breathers carry a medic alert notice (C) so that if they have a cardiac arrest, mouth-to-neck breathing can be done. Mouth-to-mouth resuscitation will not help them. They do not need to carry (A) nor refrain from (D). There are many alternative means of communication for clients who have had a laryngectomy; depending on (B) is probably the least effective. How do you know he can read and write? Awarded 0.0 points out of 1.0 possible points. 7. ID: 6974891729 The nurse would be correct in withholding a dose of digoxin in a client with congestive heart failure without specific instruction from the healthcare provider if the client's A serum digoxin level is 1.5. B blood pressure is 104/68. C serum potassium level is 3. Correct D apical pulse is 68/min. Hypokalemia (C) can precipitate digitalis toxicity in persons receiving digoxin which will increase the chance of dangerous dysrhythmias (normal potassium level is 3.5 to 5.5 mEq/L). The therapeutic range for digoxin is 0.8 to 2 ng/ml (toxic levels=>2 ng/ml); (A) is within this range. (B) would not warrant the nurse withholding the digoxin. The nurse should withhold the digoxin if the apical pulse is less than 60/min (D). Awarded 0.0 points out of 1.0 possible points. 8. ID: 6974890473 After the fourth dose of gentamicin sulfate (Garamycin) IV, the nurse plans to draw blood samples to determine peak and trough levels. When are the best times to draw these samples? A 15 minutes before and 15 minutes after the next dose. B One hour before and one hour after the next dose. C 5 minutes before and 30 minutes after the next dose. Correct D 30 minutes before and 30 minutes after the next dose. Peak drug serum levels are achieved 30 minutes after IV administration of aminoglycosides. The best time to draw a trough is the closest time to the next administration (C). (A, B, and D) are not as good a time to draw the trough as (C). (B and D) are not the best times to draw the peak of an aminoglycoside that has been administered IV. Awarded 0.0 points out of 1.0 possible points. 9. ID: 6974891711 A client has undergone insertion of a permanent pacemaker. When developing a discharge teaching plan, the nurse writes a goal of, "The client will verbalize symptoms of pacemaker failure." Which symptoms are most important to teach the client? A Facial flushing. B Fever. C Pounding headache. D Feelings of dizziness. Correct Feelings of dizziness (D) may occur as the result of a decreased heart rate, leading to decreased cardiac output. (A and C) will not occur as the result of pacemaker failure. (B) may be an indication of infection postoperatively, but is not an indication of pacemaker failure. Awarded 0.0 points out of 1.0 possible points. 10. ID: 6974890487 A client with heart disease is on a continuous telemetry monitor and has developed sinus bradycardia. In determining the possible cause of the bradycardia, the nurse assesses the client's medication record. Which medication is most likely the cause of the bradycardia? A Propanolol (Inderal). Correct B Captopril (Capoten). C Furosemide (Lasix). D Dobutamine (Dobutrex). Inderal (A) is a beta adrenergic blocking agent, which causes decreased heart rate and decreased contractility. Neither (B), an ACE inhibitor, nor (C), a loop diuretic, causes bradycardia. (D) is a sympathomimetic, direct acting cardiac stimulant, which would increase the heart rate. Awarded 0.0 points out of 1.0 possible points. 11. ID: 6974890493 In preparing a discharge plan for a 22-year-old male client diagnosed with Buerger's disease (thromboangiitis obliterans), which referral is most important? A Genetic counseling. B Twelve-step recovery program. C Clinical nutritionist. D Smoking cessation program. Correct Buerger's disease is strongly related to smoking. The most effective means of controlling symptoms and disease progression is through smoking cessation (D). The cause of Buerger's disease is unknown; a genetic predisposition is possible, but (A) will not be of value. The client with Buerger's disease does not need referral to a 12-step program any more than the general population (B). Diet is not a significant factor in the disease, and general healthy diet guidelines can be provided by the nurse (C). Awarded 0.0 points out of 1.0 possible points. 12. ID: 6974894214 Which symptoms should the nurse expect a client to exhibit who is diagnosed with a pheochromocytoma? A Numbness, tingling, and cramps in the extremities. B Headache, diaphoresis, and palpitations. Correct C Cyanosis, fever, and classic signs of shock. D Nausea, vomiting, and muscular weakness. Pheochromocytoma is a catecholamine secreting tumor of the adrenal medulla, and (B) is the typical triad of symptoms depending upon the relative proportions of epinephrine and norepinephrine secretion. (A) lists the signs of latent tetany, exhibited by clients diagnosed with hypoparathyroidism. (C) lists the signs of an Addisonian (adrenal) crisis. (D) lists the signs of hyperparathyroidism. Awarded 0.0 points out of 1.0 possible points. 13. ID: 6974890477 In assessing a client diagnosed with primary hyperaldosteronism, the nurse expects the laboratory test results to indicate a decreased serum level of which substance? A Sodium. B Antidiuretic hormone. C Potassium. Correct D Glucose. Clients with primary aldosteronism exhibit a profound decline in the serum levels of potassium (C) (hypokalemia)--hypertension is the most prominent and universal sign. (A) is normal or elevated, depending on the amount of water reabsorbed with the sodium. (B) is decreased with diabetes insipidus. (D) is not affected by primary aldosteronism. Awarded 0.0 points out of 1.0 possible points. 14. ID: 6974891771 A middle-aged male client with diabetes continues to eat an abundance of foods that are high in sugar and fat. According to the Health Belief Model, which event is most likely to increase the client's willingness to become compliant with the prescribed diet? A He visits his diabetic brother who just had surgery to amputate an infected foot. Correct B He is provided with the most current information about the dangers of untreated diabetes. C He comments on the community service announcements about preventing complications associated with diabetes. D His wife expresses a sincere willingness to prepare meals that are within his prescribed diet. The loss of a limb by a family member (A) will be the strongest event or "cue to action" and is most likely to increase the perceived seriousness of the disease. (B, C, and D) may influence his behavior but do not have the personal impact of (A). Awarded 0.0 points out of 1.0 possible points. 15. ID: 6974891774 The nurse is taking a history of a newly diagnosed Type 2 diabetic who is beginning treatment. Which subjective information is most important for the nurse to note? A A history of obesity. B An allergy to sulfa drugs. Correct C Cessation of smoking three years ago. D Numbness in the soles of the feet. An allergy to sulfa drugs may make the client unable to use some of the most common antihyperglycemic agents (sulfonylureas). The nurse needs to highlight this allergy for the healthcare provider. (A) is common and warrants counseling, but does not have the importance of (B). (C) does increase the risk for vascular disease, but it is not as important to the treatment regimen as (B). Diabetic neuropathy, as indicated by (D), is common with diabetics, but when the serum glucose is decreased, new onset numbness can possibly improve. Awarded 0.0 points out of 1.0 possible points. 16. ID: 6974890475 A client with cirrhosis develops increasing pedal edema and ascites. What dietary modification is most important for the nurse to teach this client? A Avoid high carbohydrate foods. B Decrease intake of fat soluble vitamins. C Decrease caloric intake. D Restrict salt and fluid intake. Correct Salt and fluid restrictions are the first dietary modifications for a client who is retaining fluid as manifested by edema and ascites (D). (A, B, and C) will not impact fluid retention. Awarded 0.0 points out of 1.0 possible points. 17. ID: 6974894204 A female client receiving IV vasopressin (Pitressin) for esophageal varice rupture reports to the nurse that she feels substernal tightness and pressure across her chest. Which PRN protocol should the nurse initiate? A Start an IV nitroglycerin infusion. Correct B Nasogastric lavage with cool saline. C Increase the vasopressin infusion. D Prepare for endotracheal intubation. Vasopressin is used to promote vasoconstriction, thereby reducing bleeding. Vasoconstriction of the coronary arteries can lead to angina and myocardial infarction, and should be counteracted by IV nitroglycerin per prescribed protocol (A). (B) will not resolve the cardiac problem. (C) will worsen the problem. Endotracheal intubation may be needed if respiratory distress occurs (D). Awarded 0.0 points out of 1.0 possible points. 18. ID: 6974890412 A client who is HIV positive asks the nurse, "How will I know when I have AIDS?" Which response is best for the nurse to provide? A "Diagnosis of AIDS is made when you have 2 positive ELISA test results." B "Diagnosis is made when both the ELISA and the Western Blot tests are positive." C "I can tell that you are afraid of being diagnosed with AIDS. Would you like for me to call your minister?" D "AIDS is diagnosed when a specific opportunistic infection is found in an otherwise healthy individual." Correct AIDS is diagnosed when one of several processes defined by the CDC is present in an individual who is not otherwise immunosuppressed (D) (PCP, candidacies, cryptococcus, cryptosporidiosis, Kaposi’s sarcoma, CNS lymphomas). (A and B) identify the presence of HIV, indicating a high probability that in time the individual will develop AIDS, but do not necessarily denote the presence of AIDS. (C) is telling the client how he/she feels (afraid) and is dismissing the situation to the minister. This client is asking a question and specific medical information needs to be provided. Awarded 0.0 points out of 1.0 possible points. 19. ID: 6974891751 Which description of symptoms is characteristic of a client diagnosed with trigeminal neuralgia (tic douloureux)? A Tinnitus, vertigo, and hearing difficulties. B Sudden, stabbing, severe pain over the lip and chin. Correct C Facial weakness and paralysis. D Difficulty in chewing, talking, and swallowing. Trigeminal neuralgia is characterized by paroxysms of pain, similar to an electric shock, in the area innervated by one or more branches of the trigeminal nerve (5th cranial) (B). (A) would be characteristic of M ni re's disease (8th cranial nerve). (C) would be characteristic of Bell's palsy (7th cranial nerve). (D) would be characteristic of disorders of the hypoglossal cranial nerve (12th). Awarded 0.0 points out of 1.0 possible points. 20. ID: 6974890459 Which intervention should the nurse plan to implement when caring for a client who has just undergone a right above-the-knee amputation? A Maintain the residual limb on three pillows at all times. B Place a large tourniquet at the client's bedside. Correct C Apply constant, direct pressure to the residual limb. D Do not allow the client to lie in the prone position. A large tourniquet should be placed in plain sight at the client's bedside (B). If severe bleeding occurs, the tourniquet should be readily available and applied to the residual limb to control hemorrhage. The residual limb should not be placed on a pillow (A) because a flexion contracture of the hip may result. (C) should be avoided because it may compromise wound healing. (D) should be encouraged to stretch the flexor muscles and to prevent flexion contracture of the hip. Awarded 0.0 points out of 1.0 possible points. 21. ID: 6974891796 The nurse is assessing a client who has a history of Parkinson's disease for the past 5 years. What symptoms would this client most likely exhibit? A Loss of short-term memory, facial tics and grimaces, and constant writhing movements. B Shuffling gait, masklike facial expression, and tremors of the head. Correct C Extreme muscular weakness, easy fatigability, and ptosis. D Numbness of the extremities, loss of balance, and visual disturbances. (B) are common clinical features of Parkinsonism. (A) are symptoms of chorea, (C) of myasthenia gravis, and (D) of multiple sclerosis. Awarded 0.0 points out of 1.0 possible points. 22. ID: 6974891790 The nurse is completing an admission interview and assessment on a client with a history of Parkinson's disease. Which question provides information relevant to the client's plan of care? A "Have you ever experienced any paralysis of your arms or legs?" B "Have you ever sustained a severe head injury?" C "Have you ever been 'frozen' in one spot, unable to move?" Correct D "Do you have headaches, especially ones with throbbing pain?" Clients with Parkinson's disease frequently experience difficulty in initiating, maintaining, and performing motor activities. They may even experience being rooted to the spot and unable to move (C). Parkinson's disease does not cause (A). Parkinson's disease is not usually associated with (B), nor does it typically cause (D). Awarded 0.0 points out of 1.0 possible points. 23. ID: 6974890479 The nurse is interviewing a male client with hypertension. Which additional medical diagnosis in the client's history presents the greatest risk for developing a cerebral vascular accident (CVA)? A Diabetes mellitus. Correct B Hypothyroidism. C Parkinson's disease. D Recurring pneumonia. A history of diabetes mellitus poses the greatest risk for developing a CVA (A). (B, C, and D) may place the client at some risk due to immobility, but do not present a risk as great as (A). Awarded 0.0 points out of 1.0 possible points. 24. ID: 6974890485 The nurse notes that the only ECG for a 55-year-old male client scheduled for surgery in two hours is dated two years ago. The client reports that he has a history of "heart trouble," but has no problems at present. Hospital protocol requires that those over 50 years of age have a recent ECG prior to surgery. What nursing action is best for the nurse to implement? A Ask the client what he means by "heart trouble." B Call for an ECG to be performed immediately. Correct C Notify surgery that the ECG is over two years old. D Notify the client's surgeon immediately. Clients over the age of 40 and/or with a history of cardiovascular disease, should receive ECG evaluation prior to surgery, generally 24 hours to two weeks before. (B) should be implemented to ensure that the client's current cardiovascular status is stable. Additional data might be valuable (A), but since time is limited, the priority is to obtain the needed ECG. Documentation of vital signs is important, but does not replace the need for the ECG (C). The surgeon only needs to be notified if the ECG cannot be completed, or if there is a significant problem (D). Awarded 0.0 points out of 1.0 possible points. 25. ID: 6974889581 The nurse is receiving report from surgery about a client with a penrose drain who is to be admitted to the postoperative unit. Before choosing a room for this client, which information is most important for the nurse to obtain? A If suctioning will be needed for drainage of the wound. B If the family would prefer a private or semi-private room. C null D If the client's wound is infected. Correct Penrose drains provide a sinus tract or opening and are often used to provide drainage of an abscess. The fact that the client has a penrose drain should alert the nurse to the possibility that the client is infected. To avoid contamination of another postoperative client, it is most important to place an infected client in a private room (D). A penrose drain does not require (A). Although (B) is information that should be considered, it does not have the priority of (D). (C) is used to drain fluid from a dead space and is not important in choosing a room. Awarded 0.0 points out of 1.0 possible points. 26. ID: 6974890481 What is the correct procedure for performing an ophthalmoscopic examination on a client's right retina? A Instruct the client to look at examiner's nose and not move his/her eyes during the exam. B Set ophthalmoscope on the plus 2 to 3 lens and hold it in front of the examiner's right eye. C From a distance of 8 to 12 inches and slightly to the side, shine the light into the client's pupil. Correct D For optimum visualization, keep the ophthalmoscope at least 3 inches from the client's eye. The client should focus on a distant object in order to promote pupil dilation. The ophthalmoscope should be set on the 0 lens to begin (creates no correction at the beginning of the exam), and should be held in front of the examiner's left eye when examining the client's right eye. For optimum visualization, the ophthalmoscope should be kept within one to three inch of the client's eye (D). (A and B) describe incorrect methods for conducting an ophthalmoscopic examination. (C) should illicit a red reflex as the light travels through the crystalline lens to the retina. Awarded 0.0 points out of 1.0 possible points. 27. ID: 6974891731 During lung assessment, the nurse places a stethoscope on a client's chest and instructs him/her to say "99" each time the chest is touched with the stethoscope. What would be the correct interpretation if the nurse hears the spoken words "99" very clearly through the stethoscope? A This is a normal auscultatory finding. B May indicate pneumothorax. C May indicate pneumonia. Correct D May indicate severe emphysema. This test (whispered pectoriloquy) demonstrates hyperresonance and helps determine the clarity with which spoken words are heard upon auscultation. Normally, the spoken word is not well transmitted through lung tissue, and is heard as a muffled or unclear transmission of the spoken word. Increased clarity of a spoken word is indicative of some sort of consolidation process (e. g., tumor, pneumonia) (C), and is not a normal finding (A). When lung tissue is filled with more air than normal, the voice sounds are absent or very diminished (e. g., pneumothorax, severe emphysema) (B and D). Awarded 0.0 points out of 1.0 possible points. 28. ID: 6974890425 A client has taken steroids for 12 years to help manage chronic obstructive pulmonary disease (COPD). When making a home visit, which nursing function is of greatest importance to this client? Assess the client's A pulse rate, both apically and radially. B blood pressure, both standing and sitting. C temperature. Correct D skin color and turgor. It is very important to check the client's temperature (C). Infection is the most common factor precipitating respiratory distress. Clients with COPD who are on maintenance doses of corticosteroids are particularly predisposed to infection. (A and B) are important data for baseline and ongoing assessment, but they are not as important as temperature measurement for this client who is taking steroids. Assessment of skin color and turgor is less important (D). Awarded 0.0 points out of 1.0 possible points. 29. ID: 6974890429 While working in the emergency room, the nurse is exposed to a client with active tuberculosis. When should the nurse plan to obtain a tuberculin skin test? A Immediately after the exposure. B Within one week of the exposure. C Four to six weeks after the exposure. Correct D Three months after the exposure. A tuberculin skin test is effective 4 to 6 weeks after an exposure (C), so the individual with a known exposure should wait 4 to 6 weeks before having a tuberculin skin test. Awarded 0.0 points out of 1.0 possible points. 30. ID: 6974889587 The nurse is planning to initiate a socialization group for older residents of a long-term facility. Which information would be most useful to the nurse when planning activities for the group? A The length of time each group member has resided at the nursing home. B A brief description of each resident's family life. C The age of each group member. D The usual activity patterns of each member of the group. Correct An older person's level of activity (D) is a determining factor in adjustment to aging as described by the Activity Theory of Aging. All information described in the options might be useful to the nurse, but the most useful information initially would be an assessment of each individual's adjustment to the aging process. Awarded 0.0 points out of 1.0 possible points. 31. ID: 6974890443 The nurse knows that lab values sometimes vary for the older client. Which data would the nurse expect to find when reviewing laboratory values of an 80-year-old male? A Increased WBC, decreased RBC. B Increased serum bilirubin, slightly increased liver enzymes. C Increased protein in the urine, slightly increased serum glucose levels. Correct D Decreased serum sodium, an increased urine specific gravity. In older adults, the protein found in urine slightly rises probably as a result of kidney changes or subclinical urinary tract infections. The serum glucose increases slightly due to changes in the kidney. The specific gravity declines by age 80 from 1.032 to 1.024. Awarded 0.0 points out of 1.0 possible points. 32. ID: 6974894202 A 77-year-old female client is admitted to the hospital. She is confused, has no appetite, is nauseated and vomiting, and is complaining of a headache. Her pulse rate is 43 beats per minute. Which question is a priority for the nurse to ask this client or her family on admission? "Does the client A have her own teeth or dentures?" B take aspirin and if so, how much?" C take nitroglycerin?" D take digitalis?" Correct Elderly persons are particularly susceptible to digitalis intoxication (D) which manifests itself in such symptoms as anorexia, nausea, vomiting, diarrhea, headache, and fatigue. Although it is important to obtain a complete medication history (B and C), the symptoms described are classic for digitalis toxicity, and assessment of this problem should be made promptly. (A) is irrelevant. Awarded 0.0 points out of 1.0 possible points. 33. ID: 6974889589 A 67-year-old woman who lives alone tripped on a rug in her home and fractured her hip. Which predisposing factor probably led to the fracture in the proximal end of her femur? A Failing eyesight resulting in an unsafe environment. B Renal osteodystrophy resulting from chronic renal failure. C Osteoporosis resulting from hormonal changes. Correct D Cardiovascular changes resulting in small strokes which impair mental acuity. The most common cause of a fractured hip in elderly women is osteoporosis, resulting from reduced calcium in the bones as a result of hormonal changes in later life (C). (A) may or may not have contributed to the accident, but it had nothing to do with the hip being involved. (B) is not a common condition of the elderly; it is common in chronic kidney disease (CKD). (D) may occur in some people, but does not affect the fragility of the bones as osteoporosis does. Awarded 0.0 points out of 1.0 possible points. 34. ID: 6974891733 During a health fair, a 72-year-old male client tells the nurse that he is experiencing shortness of breath. Auscultation reveals crackles and wheezing in both lungs. Suspecting that the client might have chronic bronchitis, which classic symptom would the nurse expect this client to have? A Racing pulse with exertion. B Clubbing of the fingers. C An increased chest diameter. D Productive cough with grayish-white sputum. Correct Chronic bronchitis, one of the diseases comprising the diagnosis of COPD, is characterized by a productive cough with grayish-white sputum (D), which usually occurs in the morning and is often ignored by smokers. (A) is not related to chronic bronchitis; however, it is indicative of other problems such as ventricular tachycardia and should be explored. (B and C) are symptoms of emphysema and are not consistent with the other symptoms. (C) is usually referred to as a "barrel chest." Awarded 0.0 points out of 1.0 possible points. 35. ID: 6974891747 An 81-year-old male client has emphysema. He lives at home with his cat and manages self-care with no difficulty. When making a home visit, the nurse notices that his tongue is somewhat cracked and his eyeballs are sunken into his head. What nursing intervention is indicated? A Help the client to determine ways to increase his fluid intake. Correct B Obtain an appointment for the client to see an ear, nose, and throat specialist. C Schedule an appointment with an allergist to determine if the client is allergic to the cat. D Encourage the client to slightly increase his use of oxygen at night and to always use humidified oxygen. The nurse should suggest creative methods to increase the intake of fluids (A), such as having disposable fruit juices readily available. Clients with COPD should have at least three liters of fluids a day. These clients often reduce fluid intake because of shortness of breath. (B) is not indicated. These symptoms are not indicative of an allergy (C). Many elderly depend on their pets for socialization and self-esteem. Humidified oxygen will not relieve these symptoms and increased oxygen levels will stifle the COPD client's trigger to breathe (D). Awarded 0.0 points out of 1.0 possible points. 36. ID: 6974889599 An elderly male client comes to the geriatric screening clinic complaining of pain in his left calf. The nurse notices a reddened area on the calf of his right leg which is warm to the touch and suspects it might be thrombophlebitis. Which type of pain would further confirm this suspicion? A Pain in the calf awakening him from a sound sleep. B Calf pain on exertion which stops when standing in one place. C Pain in the calf upon exertion which is relieved by rest and elevating the extremity. Correct D Pain upon arising in the morning which is relieved after some stretching and exercise. Thrombophlebitis pain is relieved by rest and elevation of the extremity (C). It typically occurs with exercise at the site of the thrombus, and is aggravated by placing the extremity in a dependent position, such as standing in one place (B). (A and D) describe pain that is not common with thrombophlebitis. Awarded 0.0 points out of 1.0 possible points. 37. ID: 6974890423 An elderly client is admitted with a diagnosis of bacterial pneumonia. The nurse's assessment of the client will most likely reveal which sign/symptom? A Leukocytosis and febrile. B Polycythemia and crackles. C Pharyngitis and sputum production. D Confusion and tachycardia. Correct The onset of pneumonia in the elderly may be signaled by general deterioration, confusion, increased heart rate or increased respiratory rate (D). (A, B, and C) are often absent in the elderly with bacterial pneumonia. Awarded 0.0 points out of 1.0 possible points. 38. ID: 6974890453 A 58-year-old client, who has no health problems, asks the nurse about the Pneumovax vaccine. The nurse's response to the client should be based on which information? A The vaccine is given annually before the flu season to those over 50 years of age. B The immunization is administered once to older adults or persons with a history of chronic illness. Correct C The vaccine is for all ages and is given primarily to those persons traveling overseas to areas of infection. D The vaccine will prevent the occurrence of pneumococcal pneumonia for up to five years. It is usually recommended that persons over 65 years of age and those with a history of chronic illness receive the vaccine once in a lifetime (B). (Some resources recommend obtaining the vaccine at 50 years of age.) The influenza vaccine is given once a year, not the Pneumovax (A). Although the vaccine might be given to a person traveling overseas, that is not the main rationale for administering the vaccine (C). It is usually given once in a lifetime (D), but with immunosuppressed clients or clients with a history of pneumonia re-vaccination is sometimes required. Awarded 0.0 points out of 1.0 possible points. 39. ID: 6974890431 The nurse is assessing a client with bacterial meningitis. Which assessment finding indicates the client may have developed septic emboli? A Cyanosis of the fingertips. Correct B Bradycardia and bradypnea. C Presence of S3 and S4 heart sounds. D 3+ pitting edema of the lower extremities. Septic emboli secondary to meningitis commonly lodge in the small arterioles of the extremities, causing a decrease in circulation to the hands (A) which may lead to gangrene. (B, C, and D) are abnormal findings, but do not indicate the development of septic emboli. Awarded 0.0 points out of 1.0 possible points. 40. ID: 6974891761 A client with multiple sclerosis has experienced an exacerbation of symptoms, including paresthesias, diplopia, and nystagmus. Which instruction should the nurse provide? A Stay out of direct sunlight. B Restrict intake of high protein foods. C Schedule extra rest periods. Correct D Go to the emergency room immediately. Exacerbations of the symptoms of MS occur most commonly as the result of fatigue and stress. Extra rest periods should be scheduled (C) to reduce the symptoms. (A, B, and D) are not necessary. Awarded 0.0 points out of 1.0 possible points. 41. ID: 6974890497 A client has been taking oral corticosteroids for the past five days because of seasonal allergies. Which assessment finding is of most concern to the nurse? A White blood count of 10,000 mm3. B Serum glucose of 115 mg/dl. C Purulent sputum. Correct D Excessive hunger. Steroids cause immunosuppression, and a purulent sputum (C) is an indication of infection, so this symptom is of greatest concern. Oral steroids may increase (A) and often cause (D). (B) may remain normal, borderline, or increase while taking oral steroids. Awarded 0.0 points out of 1.0 possible points. 42. ID: 6974891741 The healthcare provider prescribes aluminum and magnesium hydroxide (Maalox), 1 tablet PO PRN, for a client with chronic kidney disease (CKD) who is complaining of indigestion. What intervention should the nurse implement? A Administer 30 minutes before eating. B Evaluate the effectiveness 1 hour after administration. C Instruct the client to swallow the tablet whole. D Question the healthcare provider's prescription. Correct Magnesium agents are not usually used for clients with CKD due to the risk of hypermagnesemia, so this prescription should be questioned by the nurse (D). (A, B, and C) are not recommended nursing actions for the administration of aluminum and magnesium hydroxide (Maalox). Awarded 0.0 points out of 1.0 possible points. 43. ID: 6974890451 A female client taking oral contraceptives reports to the nurse that she is experiencing calf pain. What action should the nurse implement? A Determine if the client has also experienced breast tenderness and weight gain. B Encourage the client to begin a regular, daily program of walking and exercise. C Advise the client to notify the healthcare provider for immediate medical attention. Correct D Tell the client to stop taking the medication for a week to see if symptoms subside. Calf pain is indicative of thrombophlebitis, a serious, life-threatening complication associated with the use of oral contraceptives which requires further assessment and possibly immediate medical intervention (C). (A) are symptoms of oral contraceptive use, but are of less immediacy than (C). (B) may cause an embolism if thrombophlebitis is present. By not seeking immediate attention, (D) is potentially dangerous to the client. Awarded 0.0 points out of 1.0 possible points. 44. ID: 6974891721 The nurse is preparing a teaching plan for a client who is newly diagnosed with Type 1 diabetes mellitus. Which signs and symptoms should the nurse describe when teaching the client about hypoglycemia? A Sweating, trembling, tachycardia. Correct B Polyuria, polydipsia, polyphagia. C Nausea, vomiting, anorexia. D Fruity breath, tachypnea, chest pain. Sweating, dizziness, and trembling are signs of hypoglycemic reactions related to the release of epinephrine as a compensatory response to the low blood sugar (A). (B, C, and D) do not describe common symptoms of hypoglycemia. Awarded 0.0 points out of 1.0 possible points. 45. ID: 6974891707 A client who is receiving chemotherapy asks the nurse, "Why is so much of my hair falling out each day?" Which response by the nurse best explains the reason for alopecia? A "Chemotherapy affects the cells of the body that grow rapidly, both normal and malignant." Correct B "Alopecia is a common side effect you will experience during long-term steroid therapy." C "Your hair will grow back completely after your course of chemotherapy is completed." D "The chemotherapy causes permanent alterations in your hair follicles that lead to hair loss." The common adverse effects of chemotherapy (nausea, vomiting, alopecia, bone marrow depression) are due to chemotherapy's effect on the rapidly reproducing cells, both normal and malignant (A). (B and D) do not provide correct information about chemotherapy-induced alopecia. Although (D) is a true statement, it does not effectively answer the client's question. Awarded 0.0 points out of 1.0 possible points. 46. ID: 6974890465 A client receiving cholestyramine (Questran) for hyperlipidemia should be evaluated for what vitamin deficiency? A K. Correct B B12. C B6. D C. Clients should be monitored for an increased prothrombin time and prolonged bleeding times which would alert the nurse to a vitamin K deficiency (A). These drugs reduce absorption of the fat soluble (lipid) vitamins A, D, E, and K. (B, C, and D) are not fat soluble vitamins. Awarded 0.0 points out of 1.0 possible points. 47. ID: 6974891743 A client experiencing uncontrolled atrial fibrillation is admitted to the telemetry unit. What initial medication should the nurse anticipate administering to the client? A Xylocaine (Lidocaine). B Procainamide (Pronestyl). C Phenytoin (Dilantin). D Digoxin (Lanoxin). Correct Digoxin (Lanoxin) (D) is administered for uncontrolled, symptomatic atrial fibrillation resulting in a decreased cardiac output. Digoxin slows the rate of conduction by prolonging the refractory period of the AV node, thus slowing the ventricular response, decreasing the heart rate, and effecting cardiac output. (A, B, and C) are not indicated in the initial treatment of uncontrolled atrial fibrillation. Awarded 0.0 points out of 1.0 possible points. 48. ID: 6974894206 A client taking a thiazide diuretic for the past six months has a serum potassium level of 3. The nurse anticipates which change in prescription for the client? A The dosage of the diuretic will be decreased. B The diuretic will be discontinued. C A potassium supplement will be prescribed. Correct D The dosage of the diuretic will be increased. This client's potassium level is too low (normal is 3.5 to 5). Taking a thiazide diuretic often results in a loss of potassium, so a potassium supplement needs to be prescribed to restore a normal serum potassium level (C). (A, B, and D) are not recommended actions for restoring a normal serum potassium level. Awarded 0.0 points out of 1.0 possible points. 49. ID: 6974891713 A client taking furosemide (Lasix), reports difficulty sleeping. What question is important for the nurse to ask the client? A "What dose of medication are you taking?" B "Are you eating foods rich in potassium?" C "Have you lost weight recently?" D "At what time do you take your medication?" Correct The nurse needs to first determine at what time of day the client takes the Lasix (D). Because of the diuretic effect of Lasix, clients should take the medication in the morning to prevent nocturia. The actual dose of medication (A) is of less importance than the time taken. (B) is not related to the insomnia. (C) is valuable information about the effect of the diuretic, but is not likely to be related to insomnia. Awarded 0.0 points out of 1.0 possible points. 50. ID: 6974890495 The nurse assesses a client with advanced cirrhosis of the liver for signs of hepatic encephalopathy. Which finding would the nurse consider an indication of progressive hepatic encephalopathy? A An increase in abdominal girth. B Hypertension and a bounding pulse. C Decreased bowel sounds. D Difficulty in handwriting. Correct A daily record in handwriting may provide evidence of progression or reversal of hepatic encephalopathy leading to coma (D). (A) is a sign of ascites. (B) are not seen with hepatic encephalopathy. (C) does not indicate an increase in serum ammonia level which is the primary cause of hepatic encephalopathy. Awarded 0.0 points out of 1.0 possible points. 51. ID: 6974891798 A client who was in a motor vehicle collision was admitted to the hospital and the right knee was placed in skeletal traction. The nurse has documented this nursing diagnosis in the client's medical record: "Potential for impairment of skin integrity related to immobility from traction." Which nursing intervention is indicated based on this diagnosis statement? A Release the traction q4h to provide skin care. B Turn the client for back care while suspending traction. C Provide back and skin care while maintaining the traction. Correct D Give back care after the client is released from traction. (C) indicates that back care is performed while traction is left intact, which is the correct intervention for maintaining skin integrity. Maintaining skin integrity and providing back care is difficult when a client is in traction, but it cannot be delayed until the client is removed from traction (D). The nurse should never release the traction (A and B). Awarded 0.0 points out of 1.0 possible points. 52. ID: 6974890471 A splint is prescribed for nighttime use by a client with rheumatoid arthritis. Which statement by the nurse provides the most accurate explanation for use of the splints? A Prevention of deformities. Correct B Avoidance of joint trauma. C Relief of joint inflammation. D Improvement in joint strength. Splints may be used at night by clients with rheumatoid arthritis to prevent deformities (A) caused by muscle spasms and contractures. Splints are not used for (B). (C) is usually treated with medications, particularly those classified as non-steroidal antiinflammatory drugs (NSAIDs). For (D), a prescribed exercise program is indicated. Awarded 0.0 points out of 1.0 possible points. 53. ID: 6974894210 The nurse is assessing a client who smokes cigarettes and has been diagnosed with emphysema. Which finding would the nurse expect this client to exhibit? A A decreased total lung capacity. B Normal arterial blood gases. C Normal skin coloring. Correct D An absence of sputum. The differentiation between the "pink puffer" and the "blue bloater" is a well-known method of differentiating clients exhibiting symptoms of emphysema (normal color but puffing respirations) from those exhibiting symptoms of chronic bronchitis (edematous, cyanotic, shallow respirations) (C). Total lung capacity is increased in emphysema since these clients have hyperinflated lungs (A). Arterial blood gases are typically abnormal (B). (D) is indicative of bronchitis, while clients with emphysema usually have copious amounts of thick, white sputum. Awarded 0.0 points out of 1.0 possible points. 54. ID: 6974890499 A client is admitted to the medical intensive care unit with a diagnosis of myocardial infarction. The client's history indicates the infarction occurred ten hours ago. Which laboratory test result would the nurse expect this client to exhibit? A Elevated LDH. B Elevated serum amylase. C Elevated CK-MB. Correct D Elevated hematocrit. The cardiac isoenzyme CK-MB (C) is the most sensitive and most reliable indicator of myocardial damage of all the cardiac enzymes. It peaks within 12 to 20 hours after myocardial infarction (MI). (A) is a cardiac enzyme that peaks around 48 hours after an MI. (B) is expected with acute pancreatitis. (D) would be expected in a client with a fluid volume deficit, which is not a typical finding in MI. Awarded 0.0 points out of 1.0 possible points. 55. ID: 6974891715 An adult client is admitted to the hospital burn unit with partial-thickness and full-thickness burns over 40% of the body surface area. In assessing the potential for skin regeneration, what should the nurse remember about full-thickness burns? A Regenerative function of the skin is absent because the dermal layer has been destroyed. Correct B Tissue regeneration will begin several days following return of normal circulation. C Debridement of eschar will delay the body's ability to regenerate normal tissue. D Normal tissue formation will be preceded by scar formation for the first year. Full-thickness burns destroy the entire dermal layer. Included in this destruction is the regenerative tissue. For this reason, tissue regeneration does not occur, and skin grafting is necessary (A). (B, C, and D) are incorrect. Awarded 0.0 points out of 1.0 possible points. 56. ID: 6974891788 In assessing cancer risk, the nurse identifies which woman as being at greatest risk of developing breast cancer? A A 35-year-old multipara who never breastfed. B A 50-year-old whose mother had unilateral breast cancer. Correct C A 55-year-old whose mother-in-law had bilateral breast cancer. D A 20-year-old whose menarche occurred at age 9. The most predictive risk factors for development of breast cancer are over 40 years of age and a positive family history (occurrence in the immediate family, i.e., mother or sister). Other risk factors include nulliparity, no history of breastfeeding, early menarche and late menopause. Although all of the women described have one of the risk factors for developing breast cancer, (B) has the greater risk over (A, C, and D). Awarded 0.0 points out of 1.0 possible points. 57. ID: 6974889593 A 51-year-old truck driver who smokes two packs of cigarettes a day and is 30 pounds overweight is diagnosed with having a gastric ulcer. What content is most important for the nurse to include in the discharge teaching for this client? A Information about smoking cessation. Correct B Diet instructions for a low-residue diet. C Instructions on a weight-loss program. D The importance of increasing milk in the diet. Smoking has been associated with ulcer formation, and stopping or decreasing the number of cigarettes smoked per day is an important aspect of ulcer management (A). Diet management includes a reduction in high-fiber/high-roughage foods as well as spicy foods. (B) would be indicated for inflammatory bowel disease. Sodium and caloric intake are not the key elements in an ulcer diet. Although this client does need (C), the management of his ulcer is the key factor at this point. (D) would actually increase gastric acid production. Awarded 0.0 points out of 1.0 possible points. 58. ID: 6974891753 Healthcare workers must protect themselves against becoming infected with HIV. The Center for Disease Control has issued guidelines for healthcare workers in relation to protection from HIV. These guidelines include which recommendation? A Place HIV positive clients in strict isolation and limit visitors. B Wear gloves when coming in contact with the blood or body fluids of any client. Correct C Conduct mandatory HIV testing of those who work with AIDS clients. D Freeze HIV blood specimens at -70 F to kill the virus. The CDC guidelines recommend that healthcare workers use gloves when coming in contact with blood or body fluids from ANY client (B) since HIV is infectious before the client becomes aware of symptoms. (A) is not recommended, nor is it necessary. (C) is very controversial, difficult to enforce, and is not recommended by CDC. (D) does not guarantee to kill the virus. Additionally, the purpose of the blood specimen will determine how it is stored and handled. Awarded 0.0 points out of 1.0 possible points. 59. ID: 6974891782 Two days postoperative, a male client reports aching pain in his left leg. The nurse assesses redness and warmth on the lower left calf. What intervention would be most helpful to this client? A Apply sequential compression devices (SCDs) bilaterally. B Assess for a positive Homan's sign in each leg. C Pad all bony prominences on the affected leg. D Advise the client to remain in bed with the leg elevated. Correct The client is exhibiting symptoms of deep vein thrombosis (DVT), a complication of immobility. The initial care includes bedrest and elevation of the extremity (D). SCDs are used to prevent thrombophlebitis, not for treatment, when a clot might be dislodged (A). Once a client has thrombophlebitis, (B) is contraindicated because of the possibility of dislodging a clot. (C) is indicated to prevent pressure ulcers, but is not a therapeutic action for thrombophlebitis. Awarded 0.0 points out of 1.0 possible points. 60. ID: 6974890410 A 46-year-old female client is admitted for acute renal failure secondary to diabetes and hypertension. Which test is the best indicator of adequate glomerular filtration? A Serum creatinine. Correct B Blood Urea Nitrogen (BUN). C Sedimentation rate. D Urine specific gravity. Creatinine (A) is a product of muscle metabolism that is filtered by the glomerulus, and blood levels of this substance are not affected by dietary or fluid intake. An elevated creatinine strongly indicates nephron loss, reducing filtration. (B) is also an indicator of renal activity, but it can be affected by non-renal factors such as hypovolemia and increased protein intake. (C) is a nonspecific test for acute or chronic inflammatory processes. (D) is useful in assessing hydration status, but not as useful in assessing glomerular function. Awarded 0.0 points out of 1.0 possible points. 61. ID: 6974891735 What types of medications should the nurse expect to administer to a client during an acute respiratory distress episode? A Vasodilators and hormones. B Analgesics and sedatives. C Anticoagulants and expectorants. D Bronchodilators and steroids. Correct Besides supplemental oxygen, this client with ARDS needs medications to widen air passages, increase air space, and reduce alveolar membrane inflammation, such as bronchodilators and steroids (D). (A) is ineffective for the client's respiratory distress. (B) further depresses and compromise the client's ability to breathe. Anticoagulants are not indicated since coagulation is not yet a problem, and expectorants are not appropriate for this critically ill client (C). Awarded 0.0 points out of 1.0 possible points. 62. ID: 6974889577 Despite several eye surgeries, a 78-year-old client who lives alone has persistent vision problems. The visiting nurse is discussing home safety hazards with the client. The nurse suggests that the edges of the steps be painted which color? A Black. B White. C Light green. D Medium yellow. Correct Yellow is the easiest for a person with failing vision to see (D). (A) will be almost impossible to see at night because the shadows of the steps will be too difficult to determine, and would pose a safety hazard. (B) is very hard to see with a glare from the sun and it could hurt the eyes in the daytime to look at them. (C) is a pastel color and is difficult for elderly clients to see. Awarded 0.0 points out of 1.0 possible points. 63. ID: 6974891737 Which intervention should the nurse implement for a female client diagnosed with pelvic relaxation disorder? A Describe proper administration of vaginal suppositories and cream. B Encourage the client to perform Kegel exercises 10 times daily. Correct C Explain the importance of using condoms when having sexual intercourse. D Discuss the importance of keeping a diary of daily temperature and menstrual cycle events. Pelvic relaxation disorders are structural disorders resulting from weakening support tissues of the pelvis. (B) helps strengthen the surrounding muscles. Medication will not help correct a cystocele, rectocele, or uterine prolapse (A). (C) will help prevent sexually transmitted diseases. (D) is used to identify fertile times during the woman's menstrual cycle. Awarded 0.0 points out of 1.0 possible points. 64. ID: 6974889597 The nurse working in a postoperative surgical clinic is assessing a woman who had a left radical mastectomy for breast cancer. Which factor puts this client at greatest risk for developing lymphedema? A She sustained an insect bite to her left arm yesterday. Correct B She has lost twenty pounds since the surgery. C Her healthcare provider now prescribes a calcium channel blocker for hypertension. D Her hobby is playing classical music on the piano. A radical mastectomy interrupts lymph flow, and the increased lymph flow that occurs in response to the insect bite increases the risk for the occurrence of lymphedema (A). (B) is not a factor. Lymphedema is not significantly related to vascular circulation (C). Only overuse of the arm, such as weight-lifting, would cause lymphedema--(D) would not. Awarded 0.0 points out of 1.0 possible points. 65. ID: 6974891749 In preparing to administer intravenous albumin to a client following surgery, what is the priority nursing intervention? (Select all that apply.) A Set the infusion pump to infuse the albumin within four hours. Correct B Compare the client's blood type with the label on the albumin. C Assign a UAP to monitor blood pressure q15 minutes. D Administer through a large gauge catheter. Correct E Monitor hemoglobin and hematocrit levels. Correct F Assess for increased bleeding after administration. Correct (A, D, E, and F) are the correct selections. Albumin should be infused within four hours because it does not contain any preservatives. Any fluid remaining after four hours should be discarded (A). Albumin administration does not require blood typing (B). Vital signs should be monitored periodically to assess for fluid volume overload, but every 15 minutes is not necessary (C). This frequency is often used during the first hour of a blood transfusion. A large gauge catheter (D) allows for fast infusion rate, which may be necessary. Hemodilution may decrease hemoglobin and hematocrit levels (E), while increased blood volume and blood pressure may cause bleeding (F). Awarded 0.0 points out of 1.0 possible points. 66. ID: 6974890406 The nurse working on a telemetry unit finds a client unconscious and in pulseless ventricular tachycardia (VT). The client has an implanted automatic defibrillator. What action should the nurse implement? A Prepare the client for transcutaneous pacemaker. B Shock the client with 200 joules per hospital policy. Correct C Use a magnet to deactivate the implanted pacemaker. D Observe the monitor until the onset of ventricular fibrillation. The client must be externally shocked (B) to restore an effective cardiac rhythm. The automatic defibrillator is obviously malfunctioning. (A) will not be effective during ventricular tachycardia, since it is used for asystole. Since the defibrillator is not functioning, (C) is not warranted. The client should be treated immediately to restore cardiac output (D). Awarded 0.0 points out of 1.0 possible points. 67. ID: 6974890401 A 57-year-old male client is scheduled to have a stress-thallium test the following morning and is NPO after midnight. At 0130, he is agitated because he cannot eat and is demanding food. Which response is best for the nurse to provide to this client? A "I'm sorry sir, you have a prescription for nothing by mouth from midnight tonight." B "I will let you have one cracker, but that is all you can have for the rest of tonight." C "What did the healthcare provider tell you about the test you are having tomorrow?" D "The test you are having tomorrow requires that you have nothing by mouth tonight." Correct (D) is the most therapeutic statement because the nurse is responding to the client's question. (A) is not an explanation and the nurse should teach the client why eating is prohibited after midnight, rather than enforcing this requirement without an explanation for it. (B) may result in an inaccurate test result, or may cause the test to be cancelled, which could also delay diagnosis and treatment. (C) defers the responsibility for answering the client's question to the healthcare provider, when the nurse could address the situation through client teaching. Awarded 0.0 points out of 1.0 possible points. 68. ID: 6974891769 How should the nurse position the electrodes for modified chest lead one (MCL I) telemetry monitoring? A Positive polarity right shoulder, negative polarity left shoulder, ground left chest nipple line. B Positive polarity left shoulder, negative polarity right chest nipple line, ground left chest nipple line. C Positive polarity right chest nipple line, negative polarity left chest nipple line, ground left shoulder. D Negative polarity left shoulder, positive polarity right chest nipple line, ground left chest nipple line. Correct In MCL I monitoring, the positive electrode is placed on the client's mid-chest to the right of the sternum, and the negative electrode is placed on the upper left part of the chest (D). The ground may be placed anywhere, but is usually placed on the lower left portion of the chest. (A, B, and C) describe incorrect placement of electrodes for telemetry monitoring. Awarded 0.0 points out of 1.0 possible points. 69. ID: 6974890414 A client is admitted for further testing to confirm sarcoidosis. Which diagnostic test provides definitive information that the nurse should report to the healthcare provider? A Lung tissue biopsy. Correct B Positive blood cultures. C Magnetic resonance imaging (MRI). D Computerized tomography (CT) of the thorax. Sarcoidosis is an inflammatory condition that is characterized by the formation of widespread granulomatous lesions involving a pulmonary primary site. Although chest radiography identifies sarcoidosis, lung tissue biopsy (A)obtained by bronchoscopy or bronchoalveolar lavage provides definitive confirmation. (B) does not provide results for sarcoidosis. Although MRI and CT identify pulmonary lesions, the (C and D) are not necessary and do not provide definitive confirmation. Awarded 0.0 points out of 1.0 possible points. 70. ID: 6974891745 During suctioning, a client with an uncuffed tracheostomy tube begins to cough violently and dislodges the tracheostomy tube. Which action should the nurse implement first? A Notify the healthcare provider for reinsertion. B Attempt to reinsert the tracheostomy tube. Correct C Position the client in a lateral position with the neck extended. D Ventilate client's tracheostomy stoma with a manual bag-mask. The nurse should attempt to reinsert the tracheostomy tube (B) by using a hemostat to open the tracheostomy or by grasping the retention sutures (if present) to spread the opening in insert a replacement tube (with its obturator) into the stoma. Once in place, the obturator should immediately be removed. (A, C, and D) place the client at risk of airway obstruction. Awarded 0.0 points out of 1.0 possible points. 71. ID: 6974890469 When teaching diaphragmatic breathing to a client with chronic obstructive pulmonary disease (COPD), which information should the nurse provide? A Place a small book or magazine on the abdomen and make it rise while inhaling deeply. Correct B Purse the lips while inhaling as deeply as possible and then exhale through the nose. C Wrap a towel around the abdomen and push against the towel while forcefully exhaling. D Place one hand on the chest, one hand the abdomen and make both hands move outward. Diaphragmatic or abdominal breathing uses the diaphragm instead of accessory muscles to achieve maximum inhalation and to slow the respiratory rate. The client should protrude the abdomen on inhalation and contract it with exhalation, so (A) helps the client visualize the rise and fall of the abdomen. The client should purse the lips while exhaling, not (B). (C and D) are ineffective. Awarded 0.0 points out of 1.0 possible points. 72. ID: 6974890455 The nurse is planning care to prevent complication for a client with multiple myeloma. Which intervention is most important for the nurse to include? A Safety precautions during activity. B Assess for changes in size of lymph nodes. C Maintain a fluid intake of 3 to 4 L per day. Correct D Administer narcotic analgesic around the clock. Multiple myeloma is a malignancy of plasma cells that infiltrate bone causing demineralization and hypercalcemia, so maintaining a urinary output of 1.5 to 2 L per day requires an intake of 3 to 4 L (C) to promote excretion of serum calcium. Although the client is at risk for pathologic fractures due to diffuse osteoporosis, mobilization and weight bearing (A) should be encouraged to promote bone reabsorption of circulating calcium, which can cause renal complications. (B) is a component of ongoing assessment. Chronic pain management (D) should be included in the plan of care, but prevention of complications related to hypercalcemia is most important. Awarded 0.0 points out of 1.0 possible points. 73. ID: 6974889591 The nurse is caring for a client with a continuous feeding through a percutaneous endoscopic gastrostomy (PEG) tube. Which intervention should the nurse include in the plan of care? A Flush the tube with 50 ml of water q 8 hours. B Check for tube placement and residual volume q4 hours. Correct C Obtain a daily x- ray to verify tube placement. D Position on left side with head of bed elevated 45 degrees. Tube placement and residual volume should be checked before each feeding (B). Tube placement is checked by aspiration of stomach contents and measurement of pH. It is important to check for residual volume because gastric emptying is often delayed during illness. There is an increased risk for aspiration of the feeding with increased residual volume. (A, C, and D) are not correct procedures to follow. Awarded 0.0 points out of 1.0 possible points. 74. ID: 6974890447 A client with a 16-year history of diabetes mellitus is having renal function tests because of recent fatigue, weakness, elevated blood urea nitrogen, and serum creatinine levels. Which finding should the nurse conclude as an early symptom of renal insufficiency? A Dyspnea. B Nocturia. Correct C Confusion. D Stomatitis. As the glomerular filtration rate decreases in early renal insufficiency, metabolic waste products, including urea, creatinine, and other substances, such phenols, hormones, electrolytes, accumulate in the blood. In the early stage of renal insufficiency, polyuria results from the inability of the kidneys to concentrate urine and contribute to nocturia (B). (A, C, and D) are more common in the later stages of renal failure. Awarded 0.0 points out of 1.0 possible points. 75. ID: 6974890457 A client with diabetes mellitus is experiencing polyphagia. Which outcome statement is the priority for this client? A Fluid and electrolyte balance. B Prevention of water toxicity. C Reduced glucose in the urine. D Adequate cellular nourishment. Correct Diabetes mellitus Type 1 is characterized by hyperglycemia that precipitates glucosuria and polyuria (frequent urination), polydipsia (excessive thirst), and polyphagia (excessive hunger). Polyphagia is a consequence of cellular malnourishment when insulin deficiency prevents utilization of glucose for energy, so the outcome statement should include stabilization of adequate cellular nutrition (D). (A, B, and C) relate to subsequent osmolar fluid shifts related to glucosuria, polyuria, and polydipsia. Awarded 0.0 points out of 1.0 possible points. 76. ID: 6974891765 A client with a completed ischemic stroke has a blood pressure of 180/90 mm Hg. Which action should the nurse implement? A Position the head of the bed (HOB) flat. B Withhold intravenous fluids. C Administer a bolus of IV fluids. D Give an antihypertensive medication. Correct Most ischemic strokes occur during sleep when baseline blood pressure declines or blood viscosity increases due to minimal fluid intake. Completed strokes usually produce neurologic deficits within an hour, and the client’s current elevated blood pressure requires antihypertensive medication (D). Positioning the HOB flat (A) decreases venous drainage and contributes to cerebral edema post stroke. Increased blood viscosity during sleep may be related to reduced fluids, so (B) is not indicated. Increasing the vascular fluid volume increases the blood pressure, so (C) is not indicated. Awarded 0.0 points out of 1.0 possible points. 77. ID: 6974890441 The nurse is caring for a client with a stroke resulting in right-sided paresis and aphasia. The client attempts to use the left hand for feeding and other self-care activities. The spouse becomes frustrated and insists on doing everything for the client. Based on this data, which nursing diagnosis should the nurse document for this client? A Situational low self-esteem related to functional impairment and change in role function. B Disabled family coping related to dissonant coping style of significant person. Correct C Interrupted family processes related to shift in health status of family member. D Risk for ineffective therapeutic regimen management related to complexity of care. A stroke affects the whole family and in this case the spouse probably thinks that she is helping and needs to feel that she is contributing to the client's care. Her help is noted as being incongruent with attempts of self-care by the client thereby disabling family coping (B). The scenario does not discuss the client's self-esteem (A), interrupted family processes (C) or the risk for ineffective therapeutic regimen (D). Awarded 0.0 points out of 1.0 possible points. 78. ID: 6974894208 The nurse formulates the nursing diagnosis of, "Urinary retention related to sensorimotor deficit" for a client with multiple sclerosis. Which nursing intervention should the nurse implement? A Teach the client techniques of intermittent self-catheterization. Correct B Decrease fluid intake to prevent over distention of the bladder. C Use incontinence briefs to maintain hygiene with urinary dribbling. D Explain that anticholinergic drugs will decrease muscle spasticity. Bladder control is a common problem for clients with multiple sclerosis. A client with urinary retention should receive instructions about self-catheterization (A) to prevent bladder distention. Adequate hydration, not (B), is important to reduce the risk of urinary tract infections by promoting elimination which reduces the time microorganisms spend in the bladder and by diluting the number of microorganisms in the bladder. Self-catheterization helps prevent dribbling, so (C) is unnecessary. Cholinergic drugs improve bladder muscle tone and help with bladder emptying, not (D). Awarded 0.0 points out of 1.0 possible points. 79. ID: 6974891723 A 58-year-old client who has been post-menopausal for five years is concerned about the risk for osteoporosis because her mother has the condition. Which information should the nurse offer? A Osteoporosis is a progressive genetic disease with no effective treatment. B Calcium loss from bones can be slowed by increasing calcium intake and exercise. Correct C Estrogen replacement therapy should be started to prevent the progression osteoporosis. D Low-dose corticosteroid treatment effectively halts the course of osteoporosis. Post-menopausal females are at risk for osteoporosis due to the cessation of estrogen secretion, but a regimen including calcium, vitamin D, and weight-bearing exercise can prevent further bone loss (B). Osteoporosis can be managed with conservative therapy, such as bone metabolism regulators and estrogen replacement therapy (ERT) to improve bone density, but it is not a genetic disease (A). Although ERT is effective in managing osteoporosis, an increased risk for cancer and heart disease should be considered for individual clients. Corticosteroid therapy promotes bone resorption and is counterproductive in maintaining or increasing bone density (D). Awarded 0.0 points out of 1.0 possible points. 80. ID: 6974891755 The nurse is working with a 71-year-old obese client with bilateral osteoarthritis (OA) of the hips. What recommendation should the nurse make that is most beneficial in protecting the client's joints? A Increase the amount of calcium intake in the diet. B Apply alternating heat and cold therapies. C Initiate a weight-reduction diet to achieve a healthy body weight. Correct D Use a walker for ambulation to lessen weight-bearing on the hips. Achieving a healthy weight (C) is critical to protect the joints of clients with OA. Increasing the amount of calcium in the client's diet (A) will not protect hip joints from the effects of OA. Thermal therapies may lessen pain and stiffness from OA but are not protective of the joints (B). Assistive devices such as a walker may be beneficial to help avoid falls and assist in ambulation but are not protective against OA's effects (D). Awarded 0.0 points out of 1.0 possible points. 81. ID: 6974890433 A 20-year-old female client calls the nurse to report a lump she found in her breast. Which response is the best for the nurse to provide? A "Check it again in one month, and if it is still there schedule an appointment." B "Most lumps are benign, but it is always best to come in for an examination." Correct C "Try not to worry too much about it, because usually, most lumps are benign." D "If you are in your menstrual period it is not a good time to check for lumps." (B) provides the best response because it addresses the client's anxiety most effectively and encourages prompt and immediate action for a potential problem. (A) postpones treatment if the lump is malignant, and does not relieve the client's anxiety. (C and D) provide false reassurance and do not help relieve anxiety. Awarded 0.0 points out of 1.0 possible points. 82. ID: 6974890439 A 32-year-old female client complains of severe abdominal pain each month before her menstrual period, painful intercourse, and painful defecation. Which additional history should the nurse obtain that is consistent with the client's complaints? A Frequent urinary tract infections. B Inability to get pregnant. Correct C Premenstrual syndrome. D Chronic use of laxatives. Dysmenorrhea, dyspareunia, and difficulty or painful defecation are common symptoms of endometriosis, which is the abnormal displacement of endometrial tissue in the dependent areas of the pelvic peritoneum. A history of infertility (B) is another common finding associated with endometriosis. Although (A, C, and D) are common, nonspecific gynecological complaints, the most common complaints of the client with endometriosis are pain and infertility. Awarded 0.0 points out of 1.0 possible points. 83. ID: 6974890491 A female client requests information about using the calendar method of contraception. Which assessment is most important for the nurse to obtain? A Amount of weight gain or weight loss during the previous year. B An accurate menstrual cycle diary for the past 6 to 12 months. Correct C Skin pigmentation and hair texture for evidence of hormonal changes. D Previous birth-control methods and beliefs about the calendar method. The fertile period, which occurs 2 weeks prior to the onset of menses, is determined using an accurate record of the number of days of the menstrual cycles for the past 6 months, so it is most important to emphasize to the client that accuracy and compliancy of a menstrual diary (B) is the basis of the calendar method. (A and C) may be partially related to hormonal fluctuations but are not indicators for using the calendar method. (D) may demonstrate client understanding and compliancy but is not the most important aspect. Awarded 0.0 points out of 1.0 possible points. 84. ID: 6974890421 A client who is sexual active with several partners requests an intrauterine device (IUD) as a contraceptive method. Which information should the nurse provide? A Using an IUD offers no protection against sexually transmitted diseases (STD), which increase the risk for pelvic inflammatory disease (PID). Correct B Getting pregnant while using an IUD is common and is not the best contraceptive choice. C Relying on an IUD may be a safer choice for monogamous partners, but a barrier method provides a better option in preventing STD transmission. D Selecting a contraceptive device should consider choosing a successful method used in the past. The use of an IUD provides the client with no protection from STDs (A). While pregnancy rates with the use of an IUD are somewhat higher, (B) is not therapeutic, but judgmental. (C) is judgmental and does not provide the client any information about use of an IUD. While talking about contraceptives may include (D), it is does not provide the best information to maintain the client's health. Awarded 0.0 points out of 1.0 possible points. 85. ID: 6974890408 The nurse is teaching a female client who uses a contraceptive diaphragm about reducing the risk for toxic shock syndrome (TSS). Which information should the nurse include? (Select all that apply.) A Remove the diaphragm immediately after intercourse. B Wash the diaphragm with an alcohol solution. C Use the diaphragm to prevent conception during the menstrual cycle. D Do not leave the diaphragm in place longer than 8 hours after intercourse. Correct E Replace the old diaphragm every 3 months. Correct Correct selections are (D and E). The diaphragm needs to remain against the cervix for 6 to 8 hours to prevent pregnancy but should not remain for longer than 8 hours (D) to avoid the risk of TSS; the diaphragm should be replaced every 3 months (E). (A) increases the risk of pregnancy, and (B) can reduce the integrity of the barrier contraceptive but neither prevents the risk of TSS. The diaphragm should not be used during menses (C) because it obstructs the menstrual flow and is not indicated because conception does not occur during this time. Awarded 0.0 points out of 1.0 possible points. 86. ID: 6974890404 A male client receives a local anesthetic during surgery. During the post-operative assessment, the nurse notices the client is slurring his speech. Which action should the nurse take? A Determine the client is anxious and allow him to sleep. B Evaluate his blood pressure, pulse, and respiratory status. Correct C Review the client's pre-operative history for alcohol abuse. D Continue to monitor the client for reactivity to anesthesia. Slurred speech in the post-operative client who received a local anesthetic is an atypical finding and may indicate neurological deficits that require further assessment, so obtaining the client's vital signs (B) will provide information about possible cardiovascular complications, such as stroke. The client's anxiety (A), a history of alcohol abuse (D), or local anesthesia (D) are unrelated to the client's sudden onset of slurred speech. Awarded 0.0 points out of 1.0 possible points. 87. ID: 6974894212 During an interview with a client planning elective surgery, the client asks the nurse, "What is the advantage of having a preferred provider organization insurance plan?" Which response is best for the nurse to provide? A Long-term relationships with healthcare providers are more likely. B There are fewer healthcare providers to choose from than in an HMO plan. C Insurance coverage of employees is less expensive to employers. Correct D An individual can become a member of a PPO without belonging to a group. The financial advantage of (C) is the feature of a PPO that is most relevant to the average consumer. The nurse must have knowledge about PPOs, which provide discounted rates to large employers who provide insurance coverage for their employees. In return, the insurance company receives a large pool of clients for their facilities. (A, B, and D) are not accurate representations of the PPO. Awarded 0.0 points out of 1.0 possible points. 88. ID: 6974891719 A client who is fully awake after a gastroscopy asks the nurse for something to drink. After confirming that liquids are allowed, which assessment action should the nurse consider a priority? A Listen to bilateral lung and bowel sounds. B Obtain the client's pulse and blood pressure. C Assist the client to the bathroom to void. D Check the client's gag and swallow reflexes. Correct Following gastroscopy, a client should remain nothing by mouth until the effects of local anesthesia have dissipated and the airway's protective reflexes, gag and swallow reflexes, have returned (D). (A, B, and C) are not the priority before reintroducing oral fluids after a gastroscopy. Awarded 0.0 points out of 1.0 possible points. 89. ID: 6974890445 After checking the urinary drainage system for kinks in the tubing, the nurse determines that a client who has returned from the post-anesthesia care has a dark, concentrated urinary output of 54 ml for the last 2 hours. What priority nursing action should be implemented? A Report the findings to the surgeon. Correct B Irrigate the indwelling urinary catheter. C Apply manual pressure to the bladder. D Increase the IV flow rate for 15 minutes. An adult who weighs 132 pounds (60 kg) should produce about 60 ml of urine hourly (1 ml/kg/hour). Dark, concentrated, and low volume of urine output should be reported to the surgeon. Although other actions (B, C, and D) may be indicated, the assessment findings should be reported to the healthcare provider. Awarded 0.0 points out of 1.0 possible points. 90. ID: 6974890419 The nurse is assisting a client out of bed for the first time after surgery. What action should the nurse do first? A Place a chair at a right angle to the bedside. B Encourage deep breathing prior to standing. C Help the client to sit and dangle legs on the side of the bed. D Allow the client to sit with the bed in a high Fowler's position. Correct The first step is to raise the head of the bed to a high Fowler's position (D), which allow venous return to compensate from lying flat and vasodilating effects of perioperative drugs. (A, B, and C) are implemented after (D). Awarded 0.0 points out of 1.0 possible points. 91. ID: 6974891757 A female client is brought to the clinic by her daughter for a flu shot. She has lost significant weight since the last visit. She has poor personal hygiene and inadequate clothing for the weather. The client states that she lives alone and denies problems or concerns. What action should the nurse implement? A Notify social services immediately of suspected elderly abuse. B Discuss the need for mental health counseling with the daughter. C Explain to the client that she needs to take better care of herself. D Collect further data to determine whether self-neglect is occurring. Correct Changes in weight and hygiene may be indicators of self-neglect or neglect by family members. Further assessment is needed (D) before notifying social services (A) or discussing a need for counseling (B). Until further information is obtained, explanations about the client's needs are premature (C). Awarded 0.0 points out of 1.0 possible points. 92. ID: 6974890467 A client with gastroesophageal reflux disease (GERD) has been experiencing severe reflux during sleep. Which recommendation by the nurse is most effective to assist the client? A Losing weight. B Decreasing caffeine intake. C Avoiding large meals. D Raising the head of the bed on blocks. Correct Raising the head of the bed on blocks (D) (reverse Trendelenburg position) to reduce reflux and subsequent aspiration is the most effective recommendation for a client experiencing severe gastroesophageal reflux during sleep. (A, B and C) may be effective recommendations but raising the head of the bed is more effective for relief during sleep. Awarded 0.0 points out of 1.0 possible points. 93. ID: 6974894200 When providing discharge teaching for a client with osteoporosis, the nurse should reinforce which home care activity? A A diet low in phosphates. B Skin inspection for bruising. C Exercise regimen, including swimming. D Elimination of hazards to home safety. Correct Discussion about fall prevention strategies is imperative for the discharged client with osteoporosis so that advice about safety measures can be given. A low phosphorus diet is not recommended in the treatment of osteoporosis (A). Bruising (B) is not a related symptom to osteoporosis. Weight-bearing exercise is most beneficial for clients with osteoporosis. Swimming (C) is not an a weight-bearing exercise. Awarded 0.0 points out of 1.0 possible points. 94. ID: 6974889595 The nurse is planning care for a client with newly diagnosed diabetes mellitus that requires insulin. Which assessment should the nurse identify before beginning the teaching session? A Present knowledge related to the skill of injection. B Intelligence and developmental level of the client. C Willingness of the client to learn the injection sites. Correct D Financial resources available for the equipment. If a client is incapable or does not want to learn, it is unlikely that learning will occur, so motivation is the first factor the nurse should assess before teaching (C). To determine learning needs, the nurse should assess (A), but this is not the most important factor for the nurse to assess. (B and D) are factors to consider, but not as vital as (C). Awarded 0.0 points out of 1.0 possible points. 95. ID: 6974890483 Which finding should the nurse identify as most significant for a client diagnosed with polycystic kidney disease (PKD)? A Hematuria. B 2 pounds weight gain. C 3+ bacteria in urine. Correct D Steady, dull flank pain. Urinary tract infections (UTI) for a client with PKD require prompt antibiotic therapy to prevent renal damage and scarring which may cause further progression of the disease, so bacteria in the urine (C) is the most significant finding at this time. (A) is an expected finding from the rupture of the cysts. (B) does not provide a time frame to determine if the weight gain is a significant fluid fluctuation, which is determined within a 24-hour time frame. Although kidney pain can also be abrupt, episodic, and colicky related to bleeding into the cysts, (D) is more likely an early symptom in PKD. Awarded 0.0 points out of 1.0 possible points. 96. ID: 6974890463 The nurse is assessing a client with chronic kidney disease (CKD). Which finding is most important for the nurse to respond to first? A Potassium 6.0 mEq. Correct B Daily urine output of 400 ml. C Peripheral neuropathy. D Uremic fetor. Hyperkalemia (normal serum level, 3.5 to 5.5 mEq) is a serious electrolyte disorder that can cause fatal arrhythmias, so (A) is the nursing priority. (B) is an expected finding associated with renal tubular destruction. In CKD, an increase in serum nitrogenous waste products, electrolyte imbalances, and demyelination of the nerve fibers contribute to the development of (C). (D) is a urinous odor of the breath related to the accumulation of blood urea nitrogen and is a common complication of CKD, but not as significant as hyperkalemia. Awarded 0.0 points out of 1.0 possible points. 97. ID: 6974889583 What discharge instruction is most important for a client after a kidney transplant? A Weigh weekly. B Report symptoms of secondary Candidiasis. C Use daily reminders to take immunosuppressants. Correct D Stop cigarette smoking. After renal transplantation, acute rejection is a risk for several months, so immunosuppressive therapy, such as corticosteroids and azathioprine (Imuran), is essential in preventing rejection, so the priority instruction includes measures, such as daily reminders (C), to ensure the client takes these medications regularly. Daily weights, not weekly (A), provides a better indicator of weight gain related to rejection. Although fungal infections related to the immunosuppression should be reported (B), it is more important to ensure medication compliance to prevent rejection. Although smoking (D) increases the risk of atherosclerotic vascular disease which is common in clients with an organ transplant, (C) remains the priority. Awarded 0.0 points out of 1.0 possible points. 98. ID: 6974889579 A postmenopausal client asks the nurse why she is experiencing discomfort during intercourse. What response is best for the nurse to provide? A Estrogen deficiency causes the vaginal tissues to become dry and thinner. Correct B Infrequent intercourse results in the vaginal tissues losing their elasticity. C Dehydration from inadequate fluid intake causes vulva tissue dryness. D Lack of adequate stimulation is the most common reason for dyspareunia. Estrogen deprivation decreases the moisture-secreting capacity of vaginal cells, so vaginal tissues tend to become thinner, drier (A), and the rugae become smoother which reduces vaginal stretching that contributes to dyspareunia. Dyspareunia is not related to (B or C). While (D) can contribute to discomfort during intercourse, the primary cause is hormone-related. Awarded 0.0 points out of 1.0 possible points. 99. ID: 6974891727 The nurse is teaching a female client about the best time to plan sexual intercourse in order to conceive. Which information should the nurse provide? A Two weeks before menstruation. Correct B Vaginal mucous discharge is thick. C Low basal temperature. D First thing in the morning. Ovulation typically occurs 14 days before menstruation begins (A), and sexual intercourse should occur within 24 hours of ovulation for conception to occur. High estrogen levels occur during ovulation and increase the vaginal mucous membrane characteristics, which become more "slippery" and stretchy, not (B). A rise in basal temperature, not (C), signals ovulation. The timing during the day is not as significant in determining conception as the day before and after ovulation (D). Awarded 0.0 points out of 1.0 possible points. 100. ID: 6974891739 A 49-year-old female client arrives at the clinic for an annual exam and asks the nurse why she becomes excessively diaphoretic and feels warm during nighttime. What is the nurse's best response? A Explain the effect of the follicle-stimulating and luteinizing hormones. B Discuss perimenopause and related comfort measures. Correct C Assess lung fields and for a cough productive of blood-tinged mucous. D Ask if a fever above 101º F has occurred in the last 24 hours. The perimenopausal period begins about 10 years before menopause with the cessation of menstruation at the average ages of 52 to 54. Lower estrogen levels causes FSH and LH secretion in bursts (surges), which triggers vasomotor instability, night sweats, and hot flashes, so discussions about the perimenopausal body's changes, comfort measures (B), and treatment options should be provided. In-depth pathophysiology of the symptoms (A) may only confuse the client. There is no indication that the client has tuberculosis and an infection, so (C and D) are not indicated. Awarded 0.0 points out of 1.0 possible points. 101. ID: 6974891701 Which information about mammograms is most important to provide a post-menopausal female client? A Breast self-examinations are not needed if annual mammograms are obtained. B Radiation exposure is minimized by shielding the abdomen with a lead-lined apron. C Yearly mammograms should be done regardless of previous normal x-rays. Correct D Women at high risk should have annual routine and ultrasound mammograms. The current breast screening recommendation is a yearly mammogram after age 40 (C). Breast self-exam (A) continues to be a priority recommendation for all women because a small lump (or tumor) is often first felt by a woman before a mammogram is obtained. The radiation exposure from a mammogram is low, so (B) is not normally provided. The frequency of using routine and ultrasound mammograms (D) in women with high-risk variables, such as a history of breast cancer, the presence of BRC1 and BRC2 genes, or 2 first-degree relatives with breast cancer, should be recommended and followed closely by the healthcare provider. Awarded 0.0 points out of 1.0 possible points. 102. ID: 6974890437 Which assessment finding by the nurse during a client's clinical breast examination requires follow-up? A Newly retracted nipple. Correct B A thickened area where the skin folds under the breast. C Whitish nipple discharge. D Tender lumpiness noted bilaterally throughout the breasts. A newly retracted nipple (A), compared to a life-long finding, may be an indication of breast cancer and requires additional follow-up. The inframammary ridge (B) is a normal anatomic finding. Up to 80% of women may experience an intermittent nipple discharge (C), especially related to recent stimulation, and in most cases, nipple discharge is not related to malignancy. (D) is a classic finding for fibrocystic breast disease, a benign condition. Awarded 0.0 points out of 1.0 possible points. 103. ID: 6974890489 What instruction should the nurse give a client who is diagnosed with fibrocystic changes of the breast? A Observe cyst size fluctuations as a sign of malignancy. B Use estrogen supplements to reduce breast discomfort. C Notify the healthcare provider if whitish nipple discharge occurs. D Perform a breast self-exam (BSE) procedure monthly. Correct Fibrocystic changes in the breast are related to excess fibrous tissue, proliferation of mammary ducts and cyst formation that cause edema and nerve irritation. These changes obscure typical diagnostic tests, such as mammography, due to an increased breast density. Women with fibrocystic breasts should be instructed to carefully perform monthly BSE (D) and consider changes in any previous "lumpiness." Fibrocystic disease does not increase the risk of breast cancer (A). Cyst size fluctuates with the menstrual cycle, and typically lessens after menopause, and responds with a heightened sensitivity to circulating estrogen (B), which is not indicated. Nipple discharge associated with fibrocystic breasts is often milky or watery-milky and is an expected finding (C). Awarded 0.0 points out of 1.0 possible points. 104. ID: 6974891792 A client has a staging procedure for cancer of the breast and ask the nurse which type of breast cancer has the poorest prognosis. Which information should the nurse offer the client? A Stage II. B Invasive infiltrating ductal carcinoma. C T1N0M0. D Inflammatory with peau d'orange. Correct Inflammatory breast cancer, which has a thickened appearance like an orange peel (peau d'orange), is the most aggressive form of breast malignancies (D). Staging classifies cancer by the extension or spread of the disease, and (A) indicates limited local spread. (B) indicates cancer cells have spread from the ducts into the surrounding breast tissue only. TNM classification is used to indicate the extent of the disease process according to tumor size, regional spread lymph nodes involvement, and metastasis, and (C) indicates early cancer with small in situ involvement, no lymph node involvement, and no distant metastases. Awarded 0.0 points out of 1.0 possible points. 105. ID: 6974891759 A client with early breast cancer receives the results of a breast biopsy and asks the nurse to explain the meaning of staging and the type of receptors found on the cancer cells. Which explanation should the nurse provide? A Lymph node involvement is not significant. B Small tumors are aggressive and indicate poor prognosis. C The tumor's estrogen receptor guides treatment options. Correct D Stage I indicates metastasis. Treatment decisions (C) and prediction of prognosis are related to the tumor's receptor status, such as estrogen and progesterone receptor status which commonly are well-differentiated, have a lower chance of recurrence, and are receptive to hormonal therapy. Tumor staging designates tumor size and spread of breast cancer cells into axillary lymph nodes, which is one of the most important prognostic factors in early-stage breast cancer, not (A). Larger tumors are more likely to indicate poor prognosis, not (B). Stage I indicates the cancer is localized and has not spread systemically (D). Awarded 0.0 points out of 1.0 possible points. 106. ID: 6974891725 Which postmenopausal client's complaint should the nurse refer to the healthcare provider? A Breasts feel lumpy when palpated. B History of white nipple discharge. C Episodes of vaginal bleeding. Correct D Excessive diaphoresis occurs at night. Postmenopausal vaginal bleeding (C) may be an indication of endometrial cancer, which should be reported to the healthcare provider. Compared to a new-onset of a single lump, breasts that feel lumpy (A) overall may be a normal variant or a finding consistent with nonmalignant fibrocystic disease. Up to 80% of women experience (B), depending on sexual stimulation or hormonal levels, and is no longer recommended as a reportable symptom when discovered during breast self-exam (BSE). The client may need further teaching concerning (D), a disturbing symptom, but it is not as important as (C). Awarded 0.0 points out of 1.0 possible points. 107. ID: 6974890427 A client who has heart failure is admitted with a serum potassium level of 2.9 mEq/L. Which action is most important for the nurse to implement? A Give 20 mEq of potassium chloride. B Initiate continuous cardiac monitoring. Correct C Arrange a consultation with the dietician. D Teach about the side effects of diuretics. Hypokalemia (normal 3.5 to 5 mEq/L) causes changes in myocardial irritability and ECG waveform, so it is most important for the nurse to initiate continuous cardiac monitoring (B) to identify ventricular ectopy or other life-threatening dysrhythmias. Potassium chloride (A) should be given after cardiac monitoring is initiated so that the effects of potassium replacement on the cardiac rhythm can be monitored. (C and D) should be implemented when the client is stable. Awarded 0.0 points out of 1.0 possible points. 108. ID: 6974891703 Which milestone indicates to the nurse successful achievement of young adulthood? A Demonstrates a conceptualization of death and dying. B Completes education and becomes self-supporting. Correct C Creates a new definition of self and roles with others. D Develops a strong need for parental support and approval. Transitioning through young adulthood is characterized by establishing independence as an adult, and includes developmental tasks such as completing education, beginning a career, and becoming self-supporting (B). (A and C) are characteristic of adolescence. Although strong bonds with parents are an expected finding for this age group, the need for support and approval (D) indicates dependency, which is a developmental delay. Awarded 0.0 points out of 1.0 possible points. 109. ID: 6974890449 Which client should the nurse recognize as most likely to experience sleep apnea? A Middle-aged female who takes a diuretic nightly. B Obese older male client with a short, thick neck. Correct C Adolescent female with a history of tonsillectomy. D School-aged male with a history of hyperactivity disorder. Sleep apnea is characterized by lack of respirations for 10 seconds or more during sleep and is due to the loss of pharyngeal tone which allows the pharynx to collapse during inspiration and obstructs air flow through the nose and mouth. With obstructive sleep apnea, the client is often obese or has a short, thick neck as in (B). (A, C, and D) are not typically prone to sleep apnea. Awarded 0.0 points out of 1.0 possible points. 110. ID: 6974891709 Small bowel obstruction is a condition characterized by which finding? A Severe fluid and electrolyte imbalances. Correct B Metabolic acidosis. C Ribbon-like stools. D Intermittent lower abdominal cramping. Among the findings characteristic of a small bowel obstruction is the presence of severe fluid and electrolyte imbalances (A). (B, C, and D) are findings associated with large bowel obstruction. Awarded 0.0 points out of 1.0 possible points. 111. ID: 6974890461 A client's susceptibility to ulcerative colitis is most likely due to which aspect in the client's history? A Jewish European ancestry. Correct B H. pylori bowel infection. C Family history of irritable bowel syndrome. D Age between 25 and 55 years. Ulcerative colitis is 4 to 5 times more common among individuals of Jewish European or Ashkenazi ancestry (A). H. pylori is associated with stomach inflammation and ulcer development (B). Irritable bowel syndrome (C) does not progress to inflammatory bowel disease. UC has a peak between the ages of 15 and 25 years, then a second peak between 55 and 65 years, not (D). Awarded 0.0 points out of 1.0 possible points. Practice EXAM 1. ID: 6974891751 Which description of symptoms is characteristic of a client diagnosed with trigeminal neuralgia (tic douloureux)? A Tinnitus, vertigo, and hearing difficulties. B Sudden, stabbing, severe pain over the lip and chin. Correct C Facial weakness and paralysis. D Difficulty in chewing, talking, and swallowing. Trigeminal neuralgia is characterized by paroxysms of pain, similar to an electric shock, in the area innervated by one or more branches of the trigeminal nerve (5th cranial) (B). (A) would be characteristic of M ni re's disease (8th cranial nerve). (C) would be characteristic of Bell's palsy (7th cranial nerve). (D) would be characteristic of disorders of the hypoglossal cranial nerve (12th). Awarded 0.0 points out of 4.44 possible points. 2. ID: 6974891769 How should the nurse position the electrodes for modified chest lead one (MCL I) telemetry monitoring? A Positive polarity right shoulder, negative polarity left shoulder, ground left chest nipple line. B Positive polarity left shoulder, negative polarity right chest nipple line, ground left chest nipple line. C Positive polarity right chest nipple line, negative polarity left chest nipple line, ground left shoulder. D Negative polarity left shoulder, positive polarity right chest nipple line, ground left chest nipple line. Correct In MCL I monitoring, the positive electrode is placed on the client's mid-chest to the right of the sternum, and the negative electrode is placed on the upper left part of the chest (D). The ground may be placed anywhere, but is usually placed on the lower left portion of the chest. (A, B, and C) describe incorrect placement of electrodes for telemetry monitoring. Awarded 0.0 points out of 4.44 possible points. 3. ID: 6974890453 A 58-year-old client, who has no health problems, asks the nurse about the Pneumovax vaccine. The nurse's response to the client should be based on which information? A The vaccine is given annually before the flu season to those over 50 years of age. B The immunization is administered once to older adults or persons with a history of chronic illness. Correct C The vaccine is for all ages and is given primarily to those persons traveling overseas to areas of infection. D The vaccine will prevent the occurrence of pneumococcal pneumonia for up to five years. It is usually recommended that persons over 65 years of age and those with a history of chronic illness receive the vaccine once in a lifetime (B). (Some resources recommend obtaining the vaccine at 50 years of age.) The influenza vaccine is given once a year, not the Pneumovax (A). Although the vaccine might be given to a person traveling overseas, that is not the main rationale for administering the vaccine (C). It is usually given once in a lifetime (D), but with immunosuppressed clients or clients with a history of pneumonia re-vaccination is sometimes required. Awarded 0.0 points out of 4.44 possible points. 4. ID: 6974891763 During CPR, when attempting to ventilate a client's lungs, the nurse notes that the chest is not moving. What action should the nurse take first? A Use a laryngoscope to check for a foreign body lodged in the esophagus. B Reposition the head to validate that the head is in the proper position to open the airway. Correct C Turn the client to the side and administer three back blows. D Perform a finger sweep of the mouth to remove any vomitus. The most frequent cause of inadequate aeration of the client's lungs during CPR is improper positioning of the head resulting in occlusion of the airway (B). A foreign body can occlude the airway, but this is not common unless choking preceded the cardiac emergency, and (A, C and D) should not be the nurse's first action. Awarded 0.0 points out of 4.44 possible points. 5. ID: 6974890479 The nurse is interviewing a male client with hypertension. Which additional medical diagnosis in the client's history presents the greatest risk for developing a cerebral vascular accident (CVA)? A Diabetes mellitus. Correct B Hypothyroidism. C Parkinson's disease. D Recurring pneumonia. A history of diabetes mellitus poses the greatest risk for developing a CVA (A). (B, C, and D) may place the client at some risk due to immobility, but do not present a risk as great as (A). Awarded 0.0 points out of 4.44 possible points. 6. ID: 6974890467 A client with gastroesophageal reflux disease (GERD) has been experiencing severe reflux during sleep. Which recommendation by the nurse is most effective to assist the client? A Losing weight. B Decreasing caffeine intake. C Avoiding large meals. D Raising the head of the bed on blocks. Correct Raising the head of the bed on blocks (D) (reverse Trendelenburg position) to reduce reflux and subsequent aspiration is the most effective recommendation for a client experiencing severe gastroesophageal reflux during sleep. (A, B and C) may be effective recommendations but raising the head of the bed is more effective for relief during sleep. Awarded 0.0 points out of 4.44 possible points. 7. ID: 6974890499 A client is admitted to the medical intensive care unit with a diagnosis of myocardial infarction. The client's history indicates the infarction occurred ten hours ago. Which laboratory test result would the nurse expect this client to exhibit? A Elevated LDH. B Elevated serum amylase. C Elevated CK-MB. Correct D Elevated hematocrit. The cardiac isoenzyme CK-MB (C) is the most sensitive and most reliable indicator of myocardial damage of all the cardiac enzymes. It peaks within 12 to 20 hours after myocardial infarction (MI). (A) is a cardiac enzyme that peaks around 48 hours after an MI. (B) is expected with acute pancreatitis. (D) would be expected in a client with a fluid volume deficit, which is not a typical finding in MI. Awarded 0.0 points out of 4.44 possible points. 8. ID: 6974890427 A client who has heart failure is admitted with a serum potassium level of 2.9 mEq/L. Which action is most important for the nurse to implement? A Give 20 mEq of potassium chloride. B Initiate continuous cardiac monitoring. Correct C Arrange a consultation with the dietician. D Teach about the side effects of diuretics. Hypokalemia (normal 3.5 to 5 mEq/L) causes changes in myocardial irritability and ECG waveform, so it is most important for the nurse to initiate continuous cardiac monitoring (B) to identify ventricular ectopy or other life-threatening dysrhythmias. Potassium chloride (A) should be given after cardiac monitoring is initiated so that the effects of potassium replacement on the cardiac rhythm can be monitored. (C and D) should be implemented when the client is stable. Awarded 0.0 points out of 4.44 possible points. 9. ID: 6974889581 The nurse is receiving report from surgery about a client with a penrose drain who is to be admitted to the postoperative unit. Before choosing a room for this client, which information is most important for the nurse to obtain? A If suctioning will be needed for drainage of the wound. B If the family would prefer a private or semi-private room. C null D If the client's wound is infected. Correct Penrose drains provide a sinus tract or opening and are often used to provide drainage of an abscess. The fact that the client has a penrose drain should alert the nurse to the possibility that the client is infected. To avoid contamination of another postoperative client, it is most important to place an infected client in a private room (D). A penrose drain does not require (A). Although (B) is information that should be considered, it does not have the priority of (D). (C) is used to drain fluid from a dead space and is not important in choosing a room. Awarded 0.0 points out of 4.44 possible points. 10. ID: 6974891731 During lung assessment, the nurse places a stethoscope on a client's chest and instructs him/her to say "99" each time the chest is touched with the stethoscope. What would be the correct interpretation if the nurse hears the spoken words "99" very clearly through the stethoscope? A This is a normal auscultatory finding. B May indicate pneumothorax. C May indicate pneumonia. Correct D May indicate severe emphysema. This test (whispered pectoriloquy) demonstrates hyperresonance and helps determine the clarity with which spoken words are heard upon auscultation. Normally, the spoken word is not well transmitted through lung tissue, and is heard as a muffled or unclear transmission of the spoken word. Increased clarity of a spoken word is indicative of some sort of consolidation process (e. g., tumor, pneumonia) (C), and is not a normal finding (A). When lung tissue is filled with more air than normal, the voice sounds are absent or very diminished (e. g., pneumothorax, severe emphysema) (B and D). Awarded 0.0 points out of 4.44 possible points. 11. ID: 6974891749 In preparing to administer intravenous albumin to a client following surgery, what is the priority nursing intervention? (Select all that apply.) A Set the infusion pump to infuse the albumin within four hours. Correct B Compare the client's blood type with the label on the albumin. C Assign a UAP to monitor blood pressure q15 minutes. D Administer through a large gauge catheter. Correct E Monitor hemoglobin and hematocrit levels. Correct F Assess for increased bleeding after administration. Correct (A, D, E, and F) are the correct selections. Albumin should be infused within four hours because it does not contain any preservatives. Any fluid remaining after four hours should be discarded (A). Albumin administration does not require blood typing (B). Vital signs should be monitored periodically to assess for fluid volume overload, but every 15 minutes is not necessary (C). This frequency is often used during the first hour of a blood transfusion. A large gauge catheter (D) allows for fast infusion rate, which may be necessary. Hemodilution may decrease hemoglobin and hematocrit levels (E), while increased blood volume and blood pressure may cause bleeding (F). Awarded 0.0 points out of 4.44 possible points. 12. ID: 6974891761 A client with multiple sclerosis has experienced an exacerbation of symptoms, including paresthesias, diplopia, and nystagmus. Which instruction should the nurse provide? A Stay out of direct sunlight. B Restrict intake of high protein foods. C Schedule extra rest periods. Correct D Go to the emergency room immediately. Exacerbations of the symptoms of MS occur most commonly as the result of fatigue and stress. Extra rest periods should be scheduled (C) to reduce the symptoms. (A, B, and D) are not necessary. Awarded 0.0 points out of 4.44 possible points. 13. ID: 6974890443 The nurse knows that lab values sometimes vary for the older client. Which data would the nurse expect to find when reviewing laboratory values of an 80-year-old male? A Increased WBC, decreased RBC. B Increased serum bilirubin, slightly increased liver enzymes. C Increased protein in the urine, slightly increased serum glucose levels. Correct D Decreased serum sodium, an increased urine specific gravity. In older adults, the protein found in urine slightly rises probably as a result of kidney changes or subclinical urinary tract infections. The serum glucose increases slightly due to changes in the kidney. The specific gravity declines by age 80 from 1.032 to 1.024. Awarded 0.0 points out of 4.44 possible points. 14. ID: 6974891739 A 49-year-old female client arrives at the clinic for an annual exam and asks the nurse why she becomes excessively diaphoretic and feels warm during nighttime. What is the nurse's best response? A Explain the effect of the follicle-stimulating and luteinizing hormones. B Discuss perimenopause and related comfort measures. Correct C Assess lung fields and for a cough productive of blood-tinged mucous. D Ask if a fever above 101º F has occurred in the last 24 hours. The perimenopausal period begins about 10 years before menopause with the cessation of menstruation at the average ages of 52 to 54. Lower estrogen levels causes FSH and LH secretion in bursts (surges), which triggers vasomotor instability, night sweats, and hot flashes, so discussions about the perimenopausal body's changes, comfort measures (B), and treatment options should be provided. In-depth pathophysiology of the symptoms (A) may only confuse the client. There is no indication that the client has tuberculosis and an infection, so (C and D) are not indicated. Awarded 0.0 points out of 4.44 possible points. 15. ID: 6974890447 A client with a 16-year history of diabetes mellitus is having renal function tests because of recent fatigue, weakness, elevated blood urea nitrogen, and serum creatinine levels. Which finding should the nurse conclude as an early symptom of renal insufficiency? A Dyspnea. B Nocturia. Correct C Confusion. D Stomatitis. As the glomerular filtration rate decreases in early renal insufficiency, metabolic waste products, including urea, creatinine, and other substances, such phenols, hormones, electrolytes, accumulate in the blood. In the early stage of renal insufficiency, polyuria results from the inability of the kidneys to concentrate urine and contribute to nocturia (B). (A, C, and D) are more common in the later stages of renal failure. Awarded 0.0 points out of 4.44 possible points. 16. ID: 6974891788 In assessing cancer risk, the nurse identifies which woman as being at greatest risk of developing breast cancer? A A 35-year-old multipara who never breastfed. B A 50-year-old whose mother had unilateral breast cancer. Correct C A 55-year-old whose mother-in-law had bilateral breast cancer. D A 20-year-old whose menarche occurred at age 9. The most predictive risk factors for development of breast cancer are over 40 years of age and a positive family history (occurrence in the immediate family, i.e., mother or sister). Other risk factors include nulliparity, no history of breastfeeding, early menarche and late menopause. Although all of the women described have one of the risk factors for developing breast cancer, (B) has the greater risk over (A, C, and D). Awarded 0.0 points out of 4.44 possible points. 17. ID: 6974891790 The nurse is completing an admission interview and assessment on a client with a history of Parkinson's disease. Which question provides information relevant to the client's plan of care? A "Have you ever experienced any paralysis of your arms or legs?" B "Have you ever sustained a severe head injury?" C "Have you ever been 'frozen' in one spot, unable to move?" Correct D "Do you have headaches, especially ones with throbbing pain?" Clients with Parkinson's disease frequently experience difficulty in initiating, maintaining, and performing motor activities. They may even experience being rooted to the spot and unable to move (C). Parkinson's disease does not cause (A). Parkinson's disease is not usually associated with (B), nor does it typically cause (D). Awarded 0.0 points out of 4.44 possible points. 18. ID: 6974890429 While working in the emergency room, the nurse is exposed to a client with active tuberculosis. When should the nurse plan to obtain a tuberculin skin test? A Immediately after the exposure. B Within one week of the exposure. C Four to six weeks after the exposure. Correct D Three months after the exposure. A tuberculin skin test is effective 4 to 6 weeks after an exposure (C), so the individual with a known exposure should wait 4 to 6 weeks before having a tuberculin skin test. Awarded 0.0 points out of 4.44 possible points. 19. ID: 6974894200 When providing discharge teaching for a client with osteoporosis, the nurse should reinforce which home care activity? A A diet low in phosphates. B Skin inspection for bruising. C Exercise regimen, including swimming. D Elimination of hazards to home safety. Correct Discussion about fall prevention strategies is imperative for the discharged client with osteoporosis so that advice about safety measures can be given. A low phosphorus diet is not recommended in the treatment of osteoporosis (A). Bruising (B) is not a related symptom to osteoporosis. Weight-bearing exercise is most beneficial for clients with osteoporosis. Swimming (C) is not an a weight-bearing exercise. Awarded 0.0 points out of 4.44 possible points. 20. ID: 6974890481 What is the correct procedure for performing an ophthalmoscopic examination on a client's right retina? A Instruct the client to look at examiner's nose and not move his/her eyes during the exam. B Set ophthalmoscope on the plus 2 to 3 lens and hold it in front of the examiner's right eye. C From a distance of 8 to 12 inches and slightly to the side, shine the light into the client's pupil. Correct D For optimum visualization, keep the ophthalmoscope at least 3 inches from the client's eye. The client should focus on a distant object in order to promote pupil dilation. The ophthalmoscope should be set on the 0 lens to begin (creates no correction at the beginning of the exam), and should be held in front of the examiner's left eye when examining the client's right eye. For optimum visualization, the ophthalmoscope should be kept within one to three inch of the client's eye (D). (A and B) describe incorrect methods for conducting an ophthalmoscopic examination. (C) should illicit a red reflex as the light travels through the crystalline lens to the retina. Awarded 0.0 points out of 4.44 possible points. 21. ID: 6974891782 Two days postoperative, a male client reports aching pain in his left leg. The nurse assesses redness and warmth on the lower left calf. What intervention would be most helpful to this client? A Apply sequential compression devices (SCDs) bilaterally. B Assess for a positive Homan's sign in each leg. C Pad all bony prominences on the affected leg. D Advise the client to remain in bed with the leg elevated. Correct The client is exhibiting symptoms of deep vein thrombosis (DVT), a complication of immobility. The initial care includes bedrest and elevation of the extremity (D). SCDs are used to prevent thrombophlebitis, not for treatment, when a clot might be dislodged (A). Once a client has thrombophlebitis, (B) is contraindicated because of the possibility of dislodging a clot. (C) is indicated to prevent pressure ulcers, but is not a therapeutic action for thrombophlebitis. Awarded 0.0 points out of 4.44 possible points. 22. ID: 6974890455 The nurse is planning care to prevent complication for a client with multiple myeloma. Which intervention is most important for the nurse to include? A Safety precautions during activity. B Assess for changes in size of lymph nodes. C Maintain a fluid intake of 3 to 4 L per day. Correct D Administer narcotic analgesic around the clock. Multiple myeloma is a malignancy of plasma cells that infiltrate bone causing demineralization and hypercalcemia, so maintaining a urinary output of 1.5 to 2 L per day requires an intake of 3 to 4 L (C) to promote excretion of serum calcium. Although the client is at risk for pathologic fractures due to diffuse osteoporosis, mobilization and weight bearing (A) should be encouraged to promote bone reabsorption of circulating calcium, which can cause renal complications. (B) is a component of ongoing assessment. Chronic pain management (D) should be included in the plan of care, but prevention of complications related to hypercalcemia is most important. Awarded 0.0 points out of 4.44 possible points. 23. ID: 6974891715 An adult client is admitted to the hospital burn unit with partial-thickness and full-thickness burns over 40% of the body surface area. In assessing the potential for skin regeneration, what should the nurse remember about full-thickness burns? A Regenerative function of the skin is absent because the dermal layer has been destroyed. Correct B Tissue regeneration will begin several days following return of normal circulation. C Debridement of eschar will delay the body's ability to regenerate normal tissue. D Normal tissue formation will be preceded by scar formation for the first year. Full-thickness burns destroy the entire dermal layer. Included in this destruction is the regenerative tissue. For this reason, tissue regeneration does not occur, and skin grafting is necessary (A). (B, C, and D) are incorrect. Awarded 0.0 points out of 4.44 possible points. 24. ID: 6974889583 What discharge instruction is most important for a client after a kidney transplant? A Weigh weekly. B Report symptoms of secondary Candidiasis. C Use daily reminders to take immunosuppressants. Correct D Stop cigarette smoking. After renal transplantation, acute rejection is a risk for several months, so immunosuppressive therapy, such as corticosteroids and azathioprine (Imuran), is essential in preventing rejection, so the priority instruction includes measures, such as daily reminders (C), to ensure the client takes these medications regularly. Daily weights, not weekly (A), provides a better indicator of weight gain related to rejection. Although fungal infections related to the immunosuppression should be reported (B), it is more important to ensure medication compliance to prevent rejection. Although smoking (D) increases the risk of atherosclerotic vascular disease which is common in clients with an organ transplant, (C) remains the priority. Awarded 0.0 points out of 4.44 possible points. 25. ID: 6974891741 The healthcare provider prescribes aluminum and magnesium hydroxide (Maalox), 1 tablet PO PRN, for a client with chronic kidney disease (CKD) who is complaining of indigestion. What intervention should the nurse implement? A Administer 30 minutes before eating. B Evaluate the effectiveness 1 hour after administration. C Instruct the client to swallow the tablet whole. D Question the healthcare provider's prescription. Correct Magnesium agents are not usually used for clients with CKD due to the risk of hypermagnesemia, so this prescription should be questioned by the nurse (D). (A, B, and C) are not recommended nursing actions for the administration of aluminum and magnesium hydroxide (Maalox). Awarded 0.0 points out of 4.44 possible points. [Show More]
Last updated: 1 year ago
Preview 1 out of pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 26, 2021
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
Jan 26, 2021
Downloads
0
Views
5

.png)
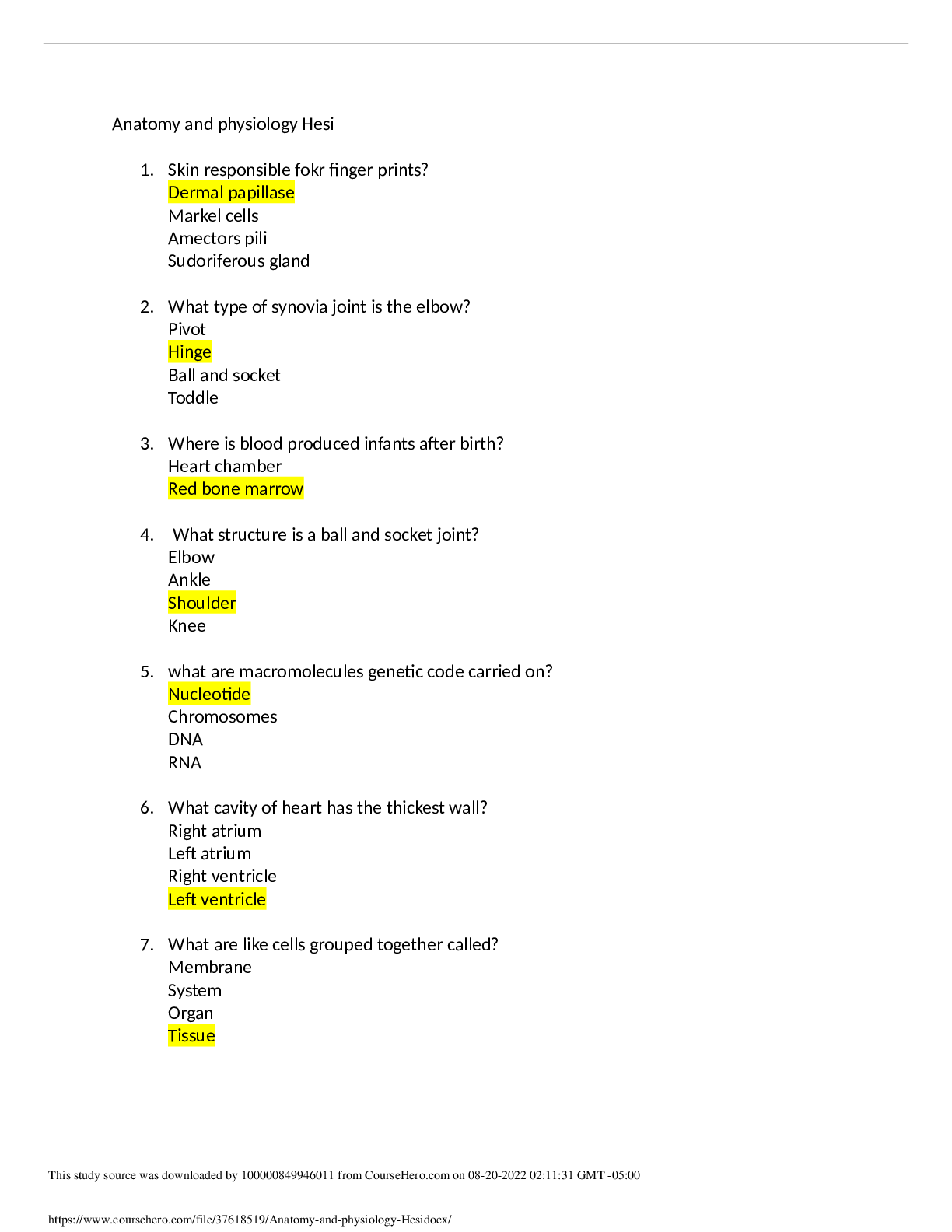
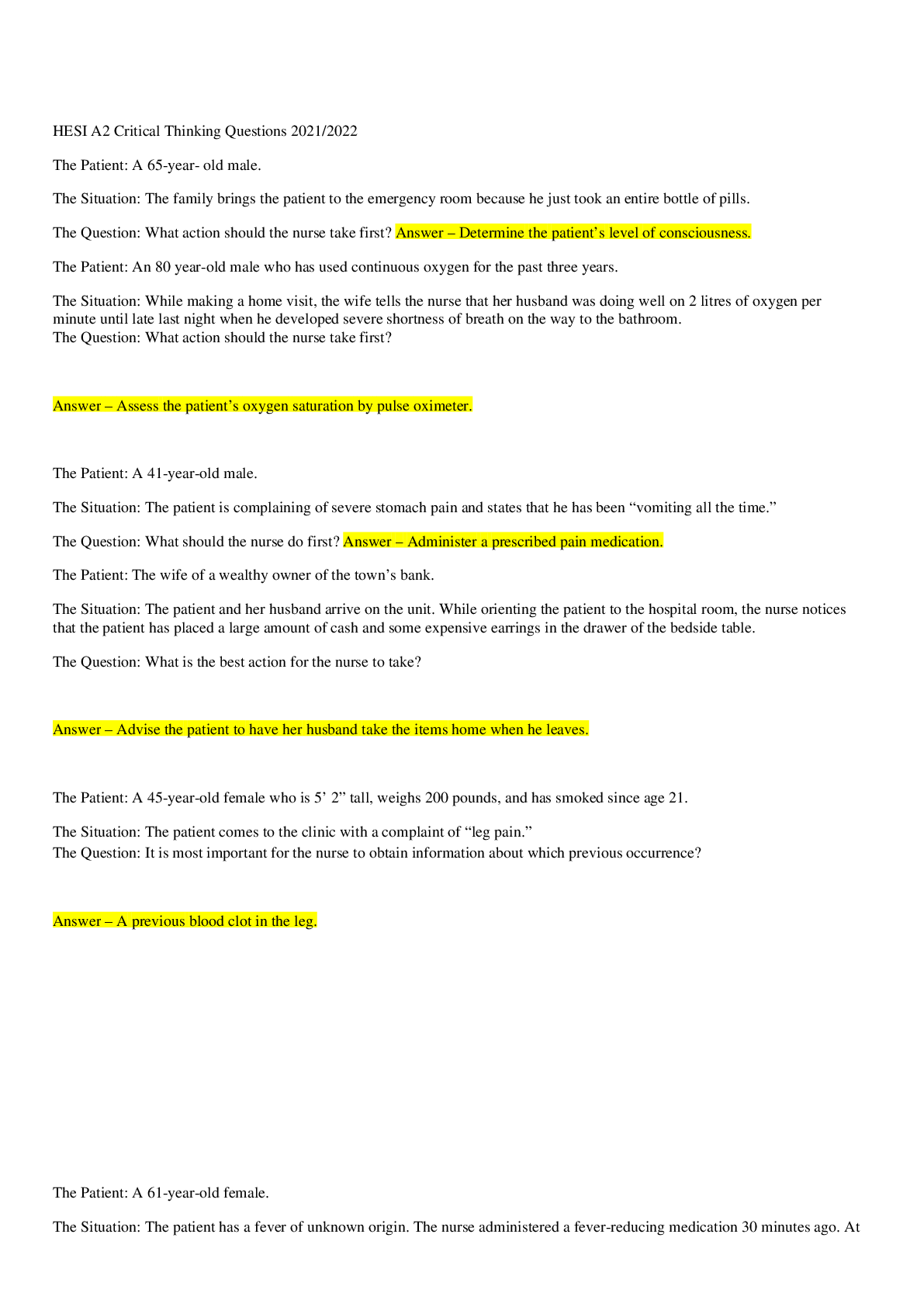
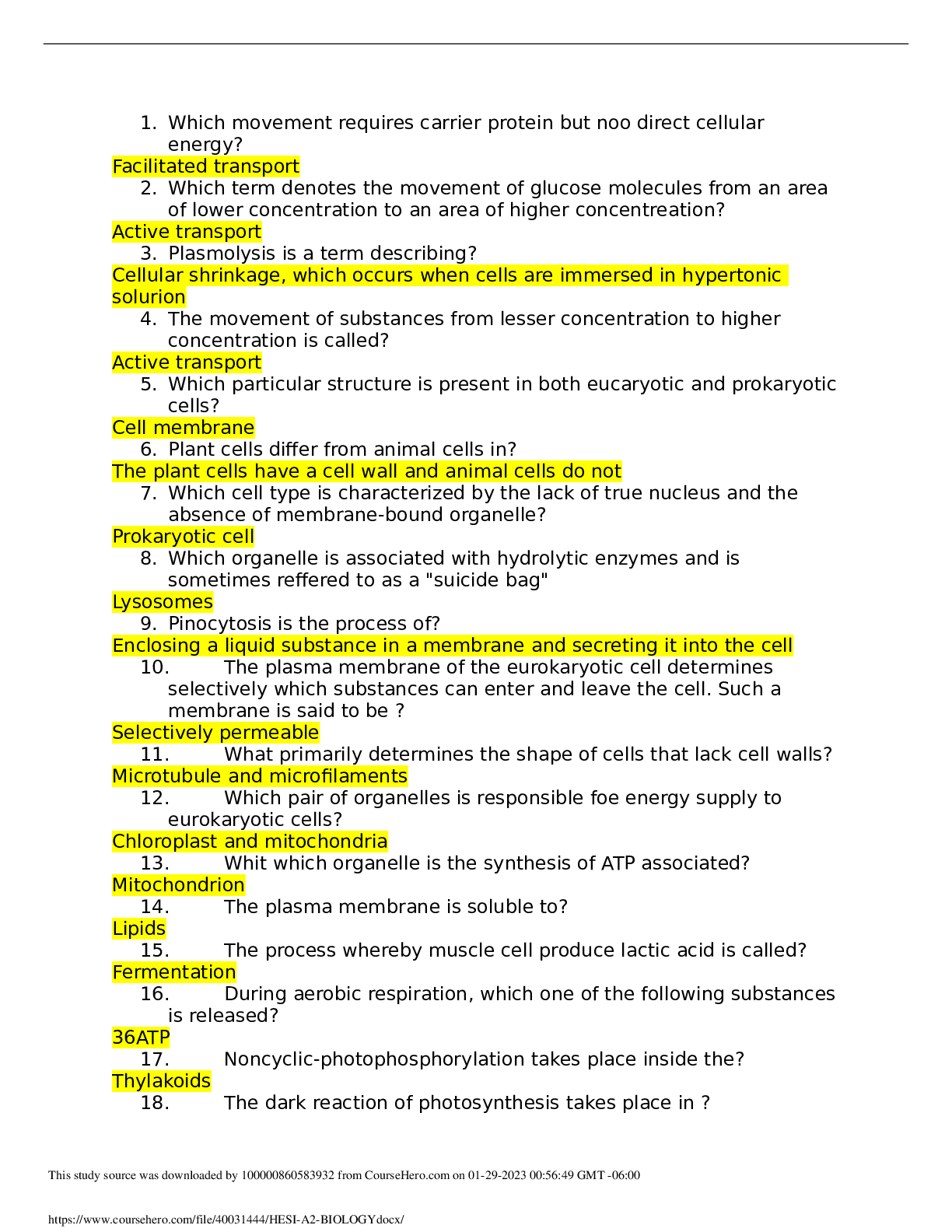
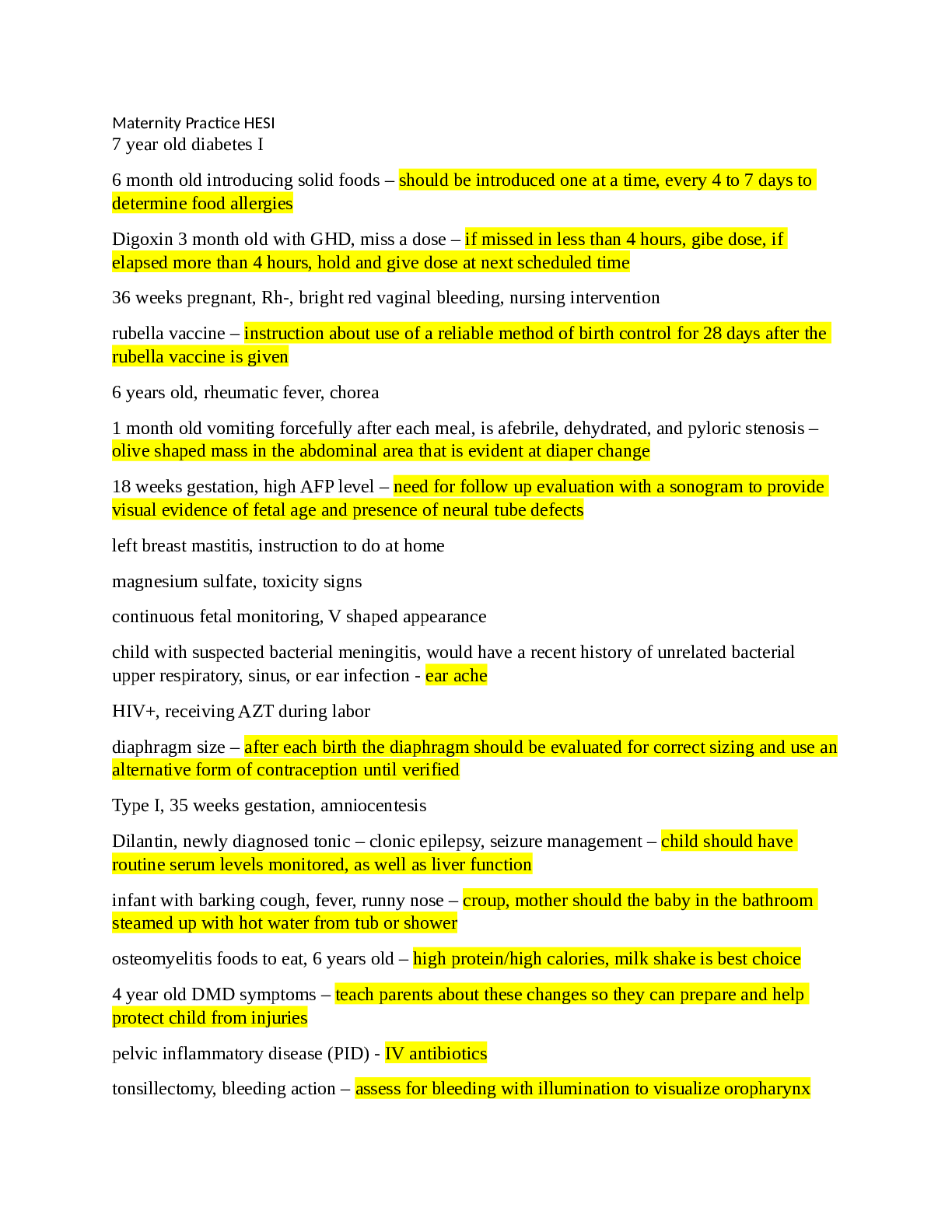

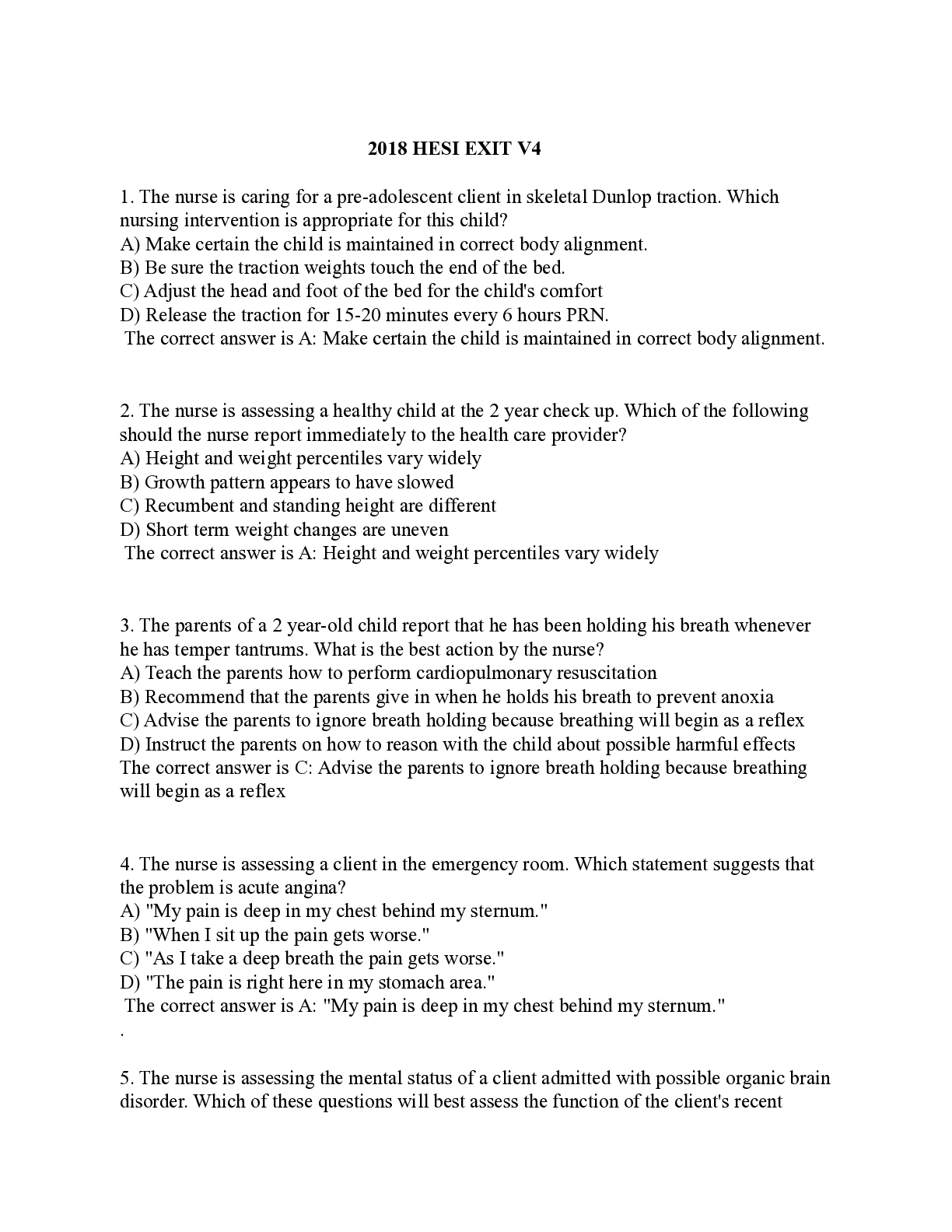
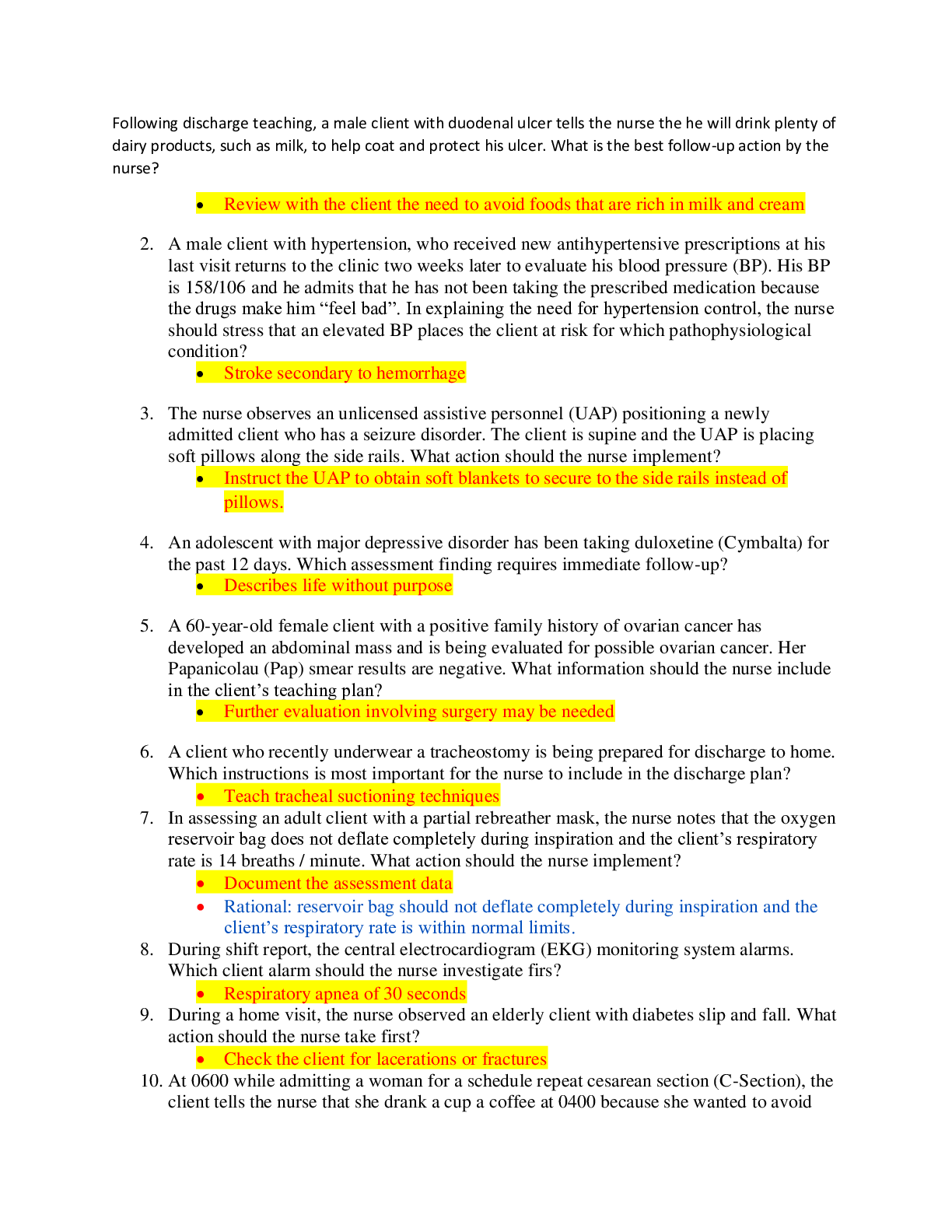
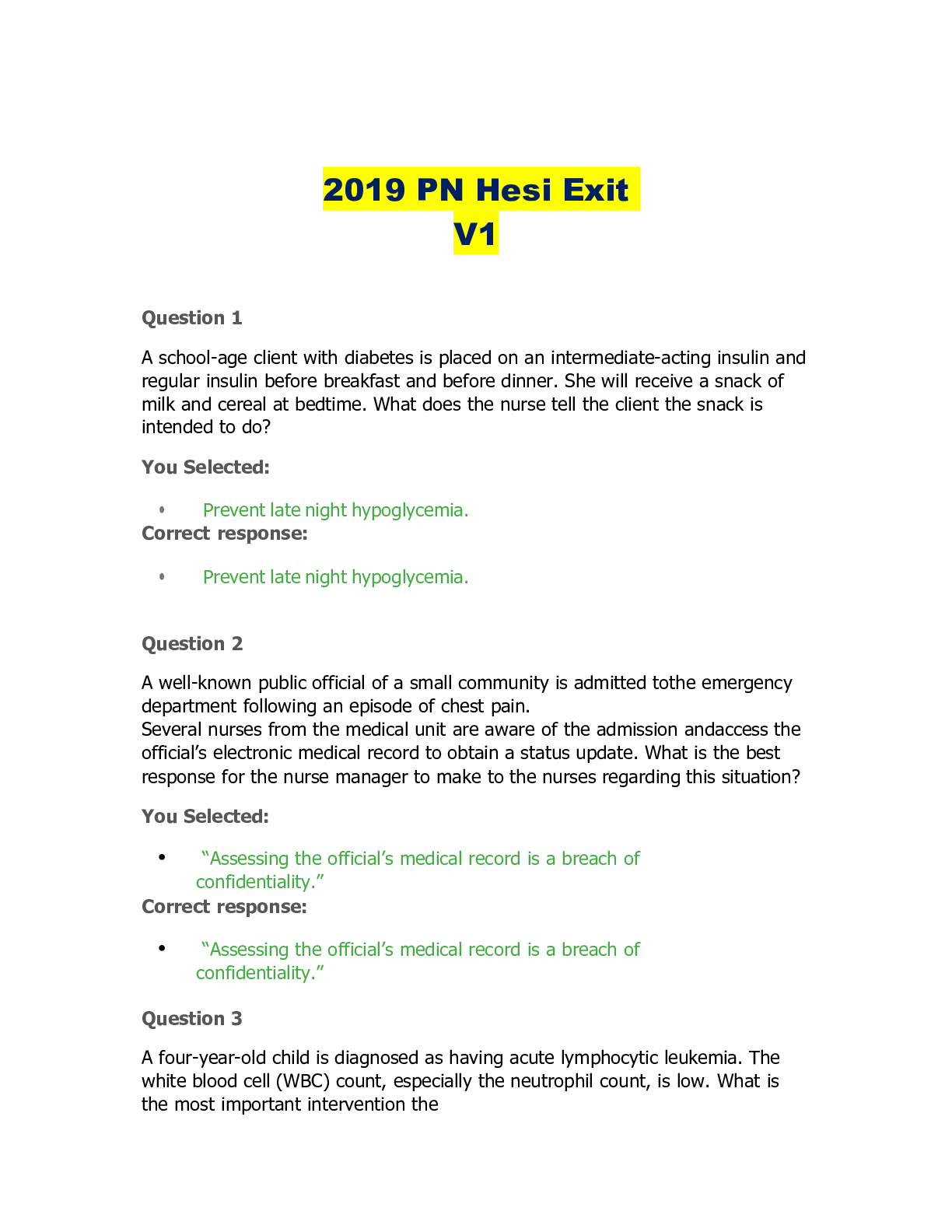
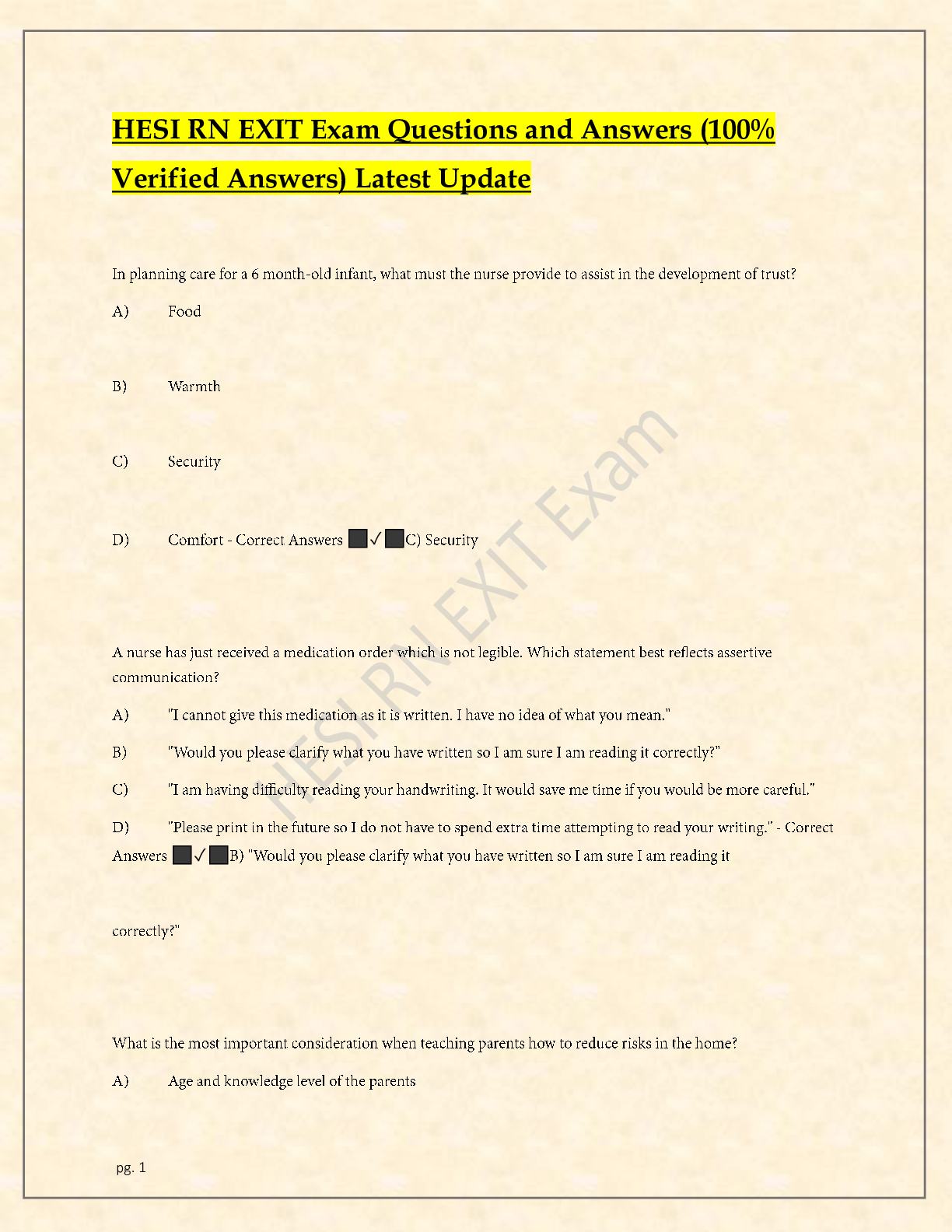
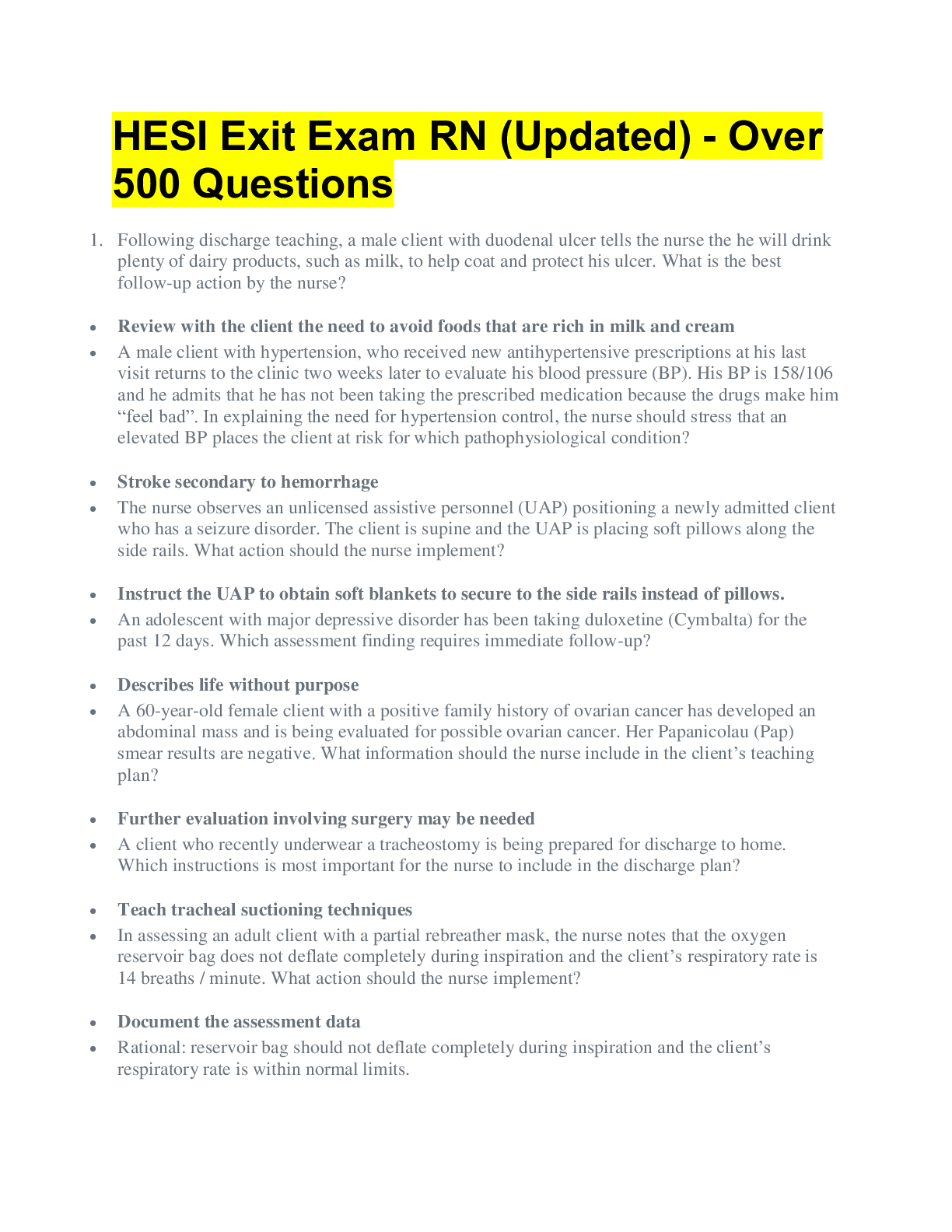
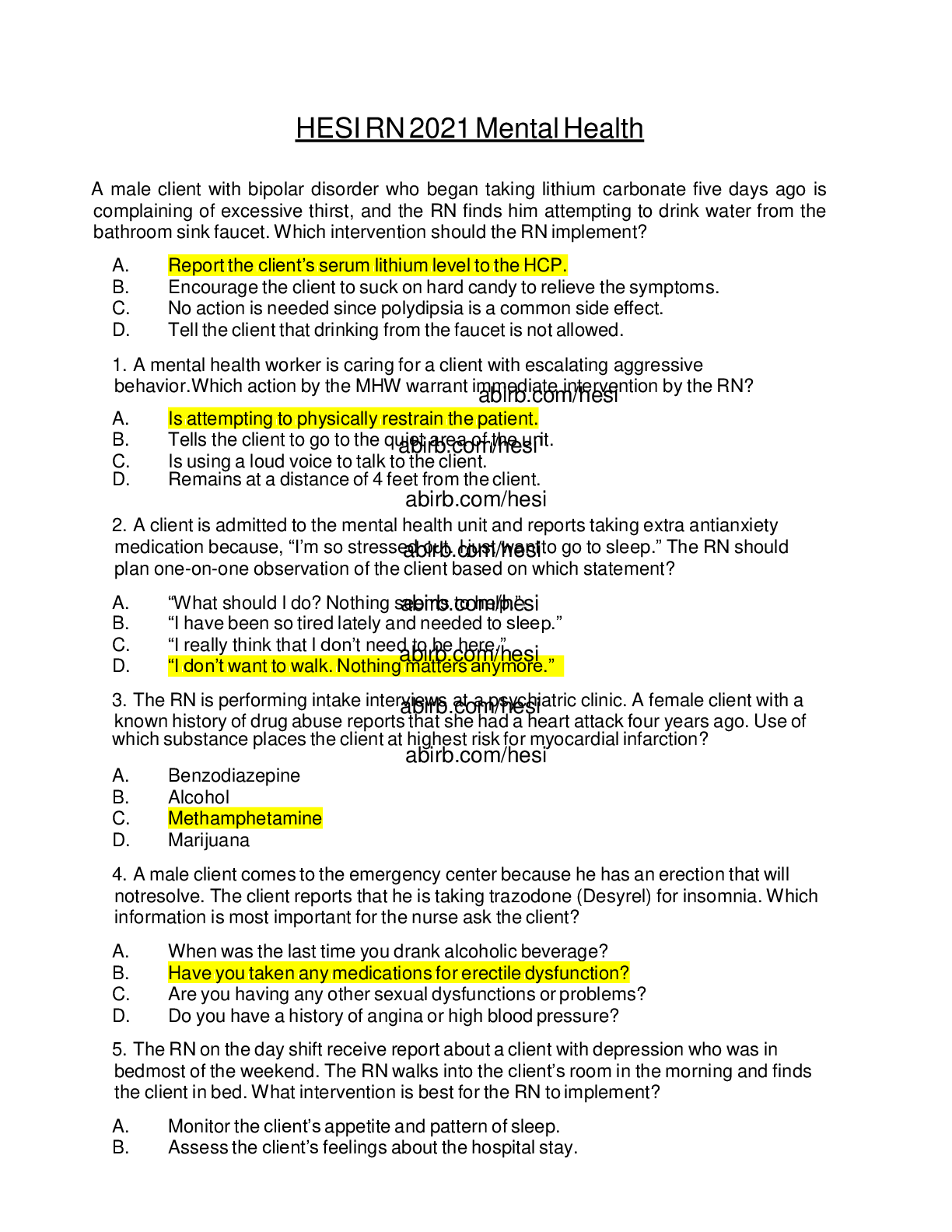
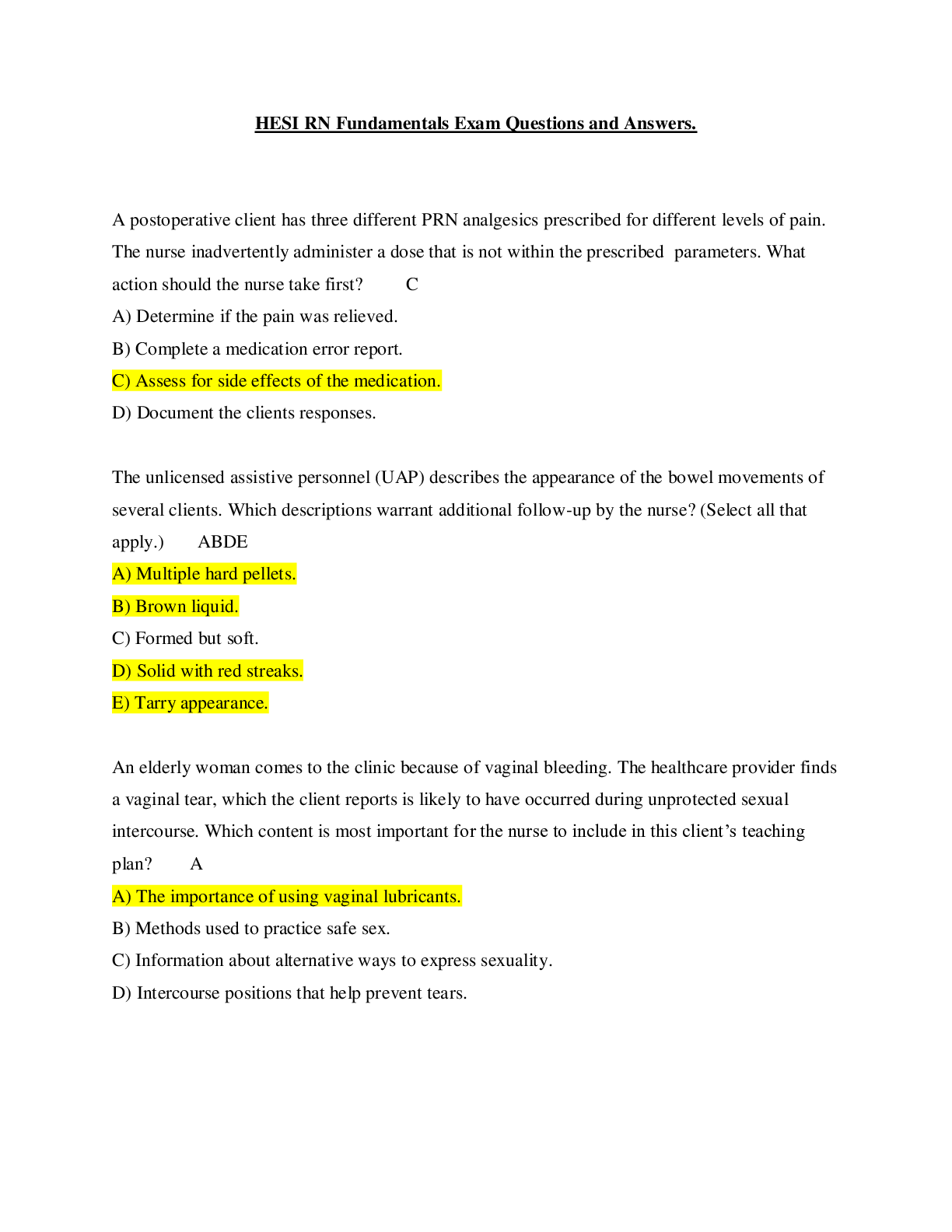
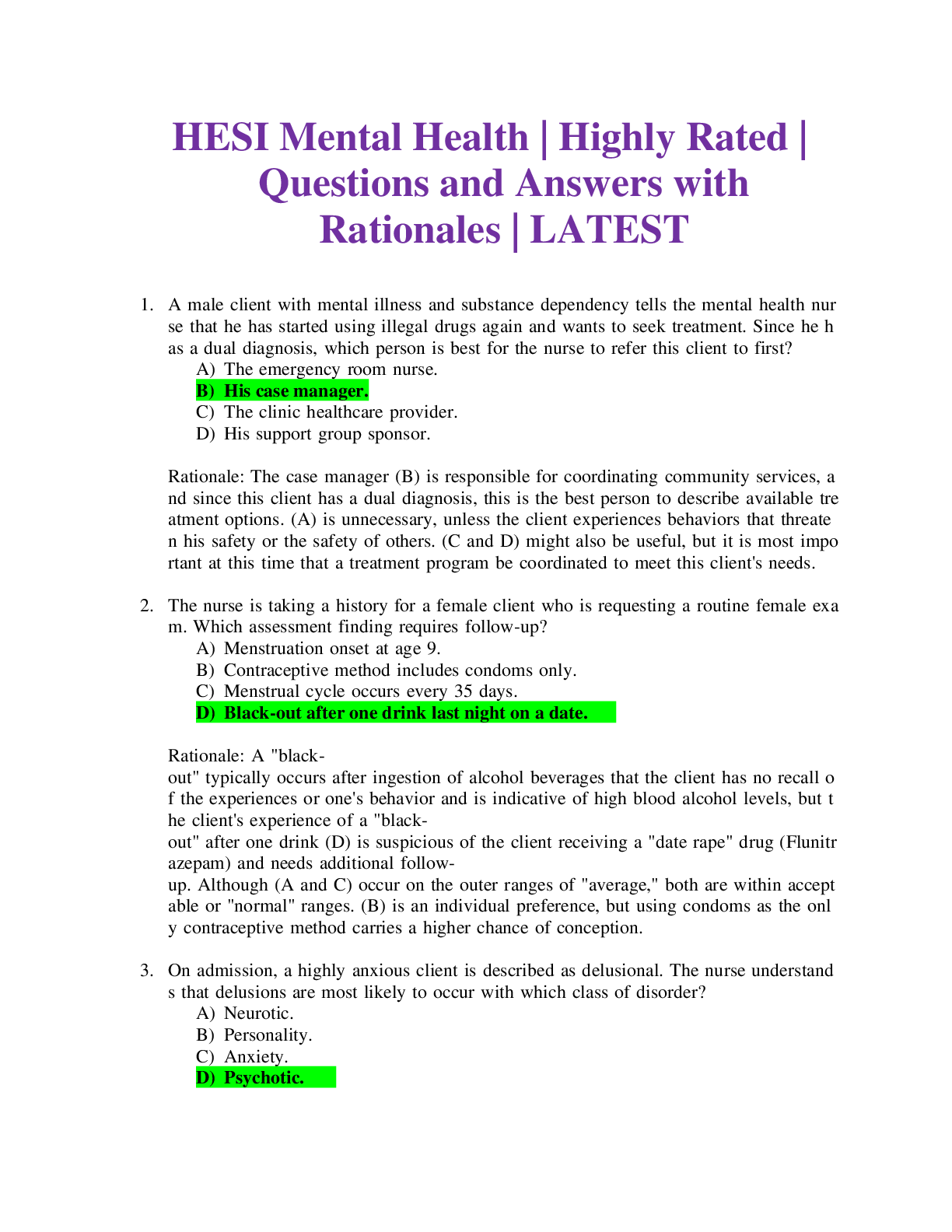
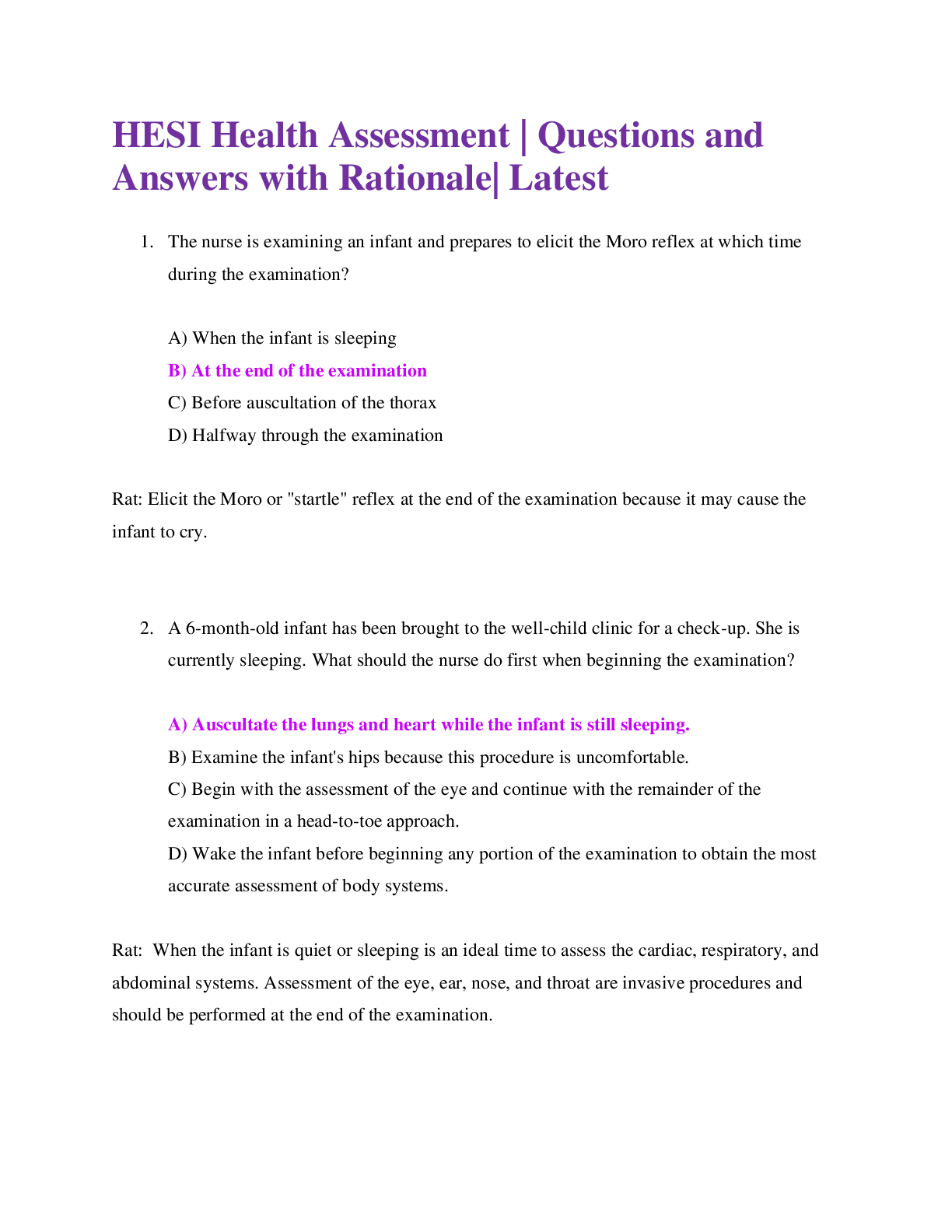
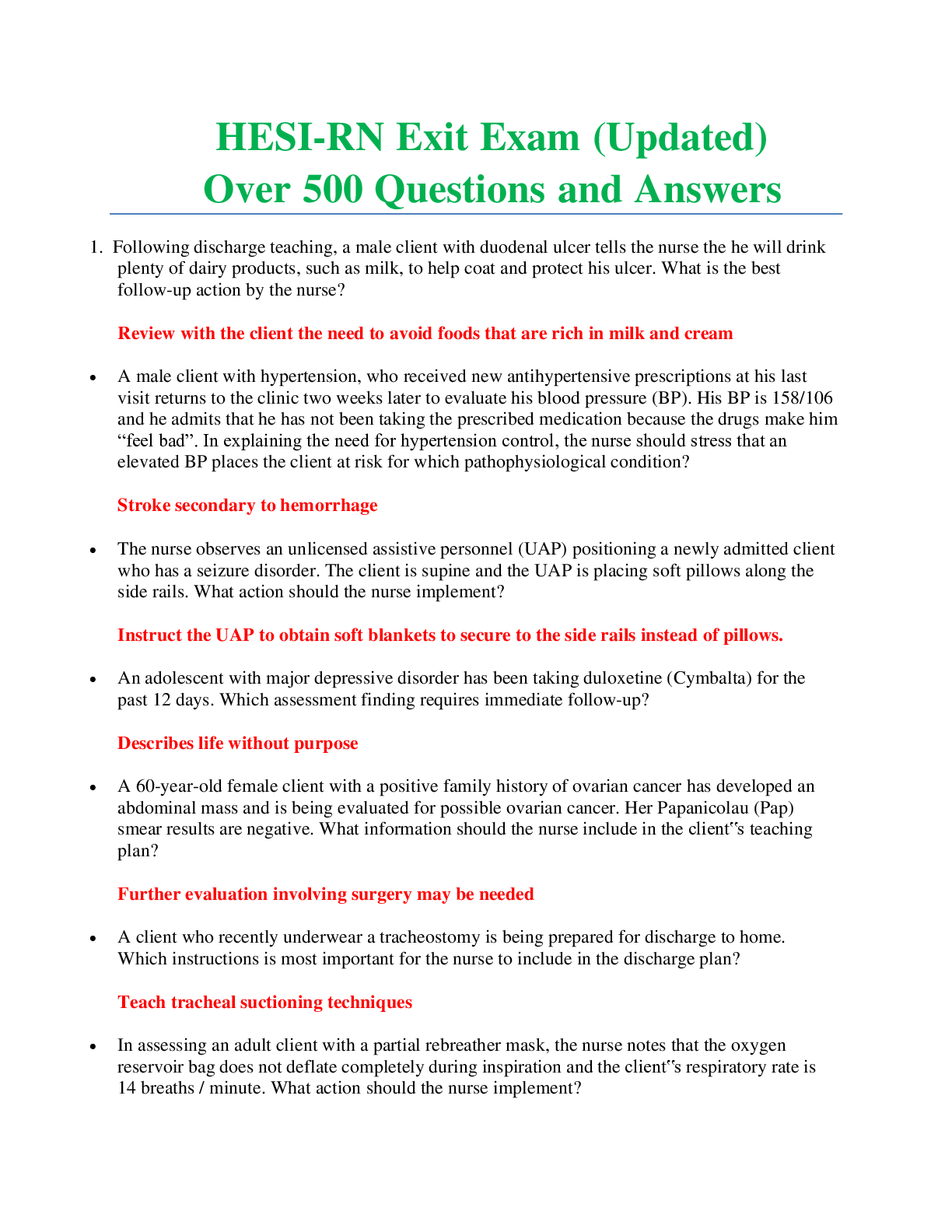
.png)