*NURSING > SHADOW HEALTH > NURS MISC Heart Failure Unfolding Reasoning JoAnn Smith, 72 years old (All)
NURS MISC Heart Failure Unfolding Reasoning JoAnn Smith, 72 years old
Document Content and Description Below
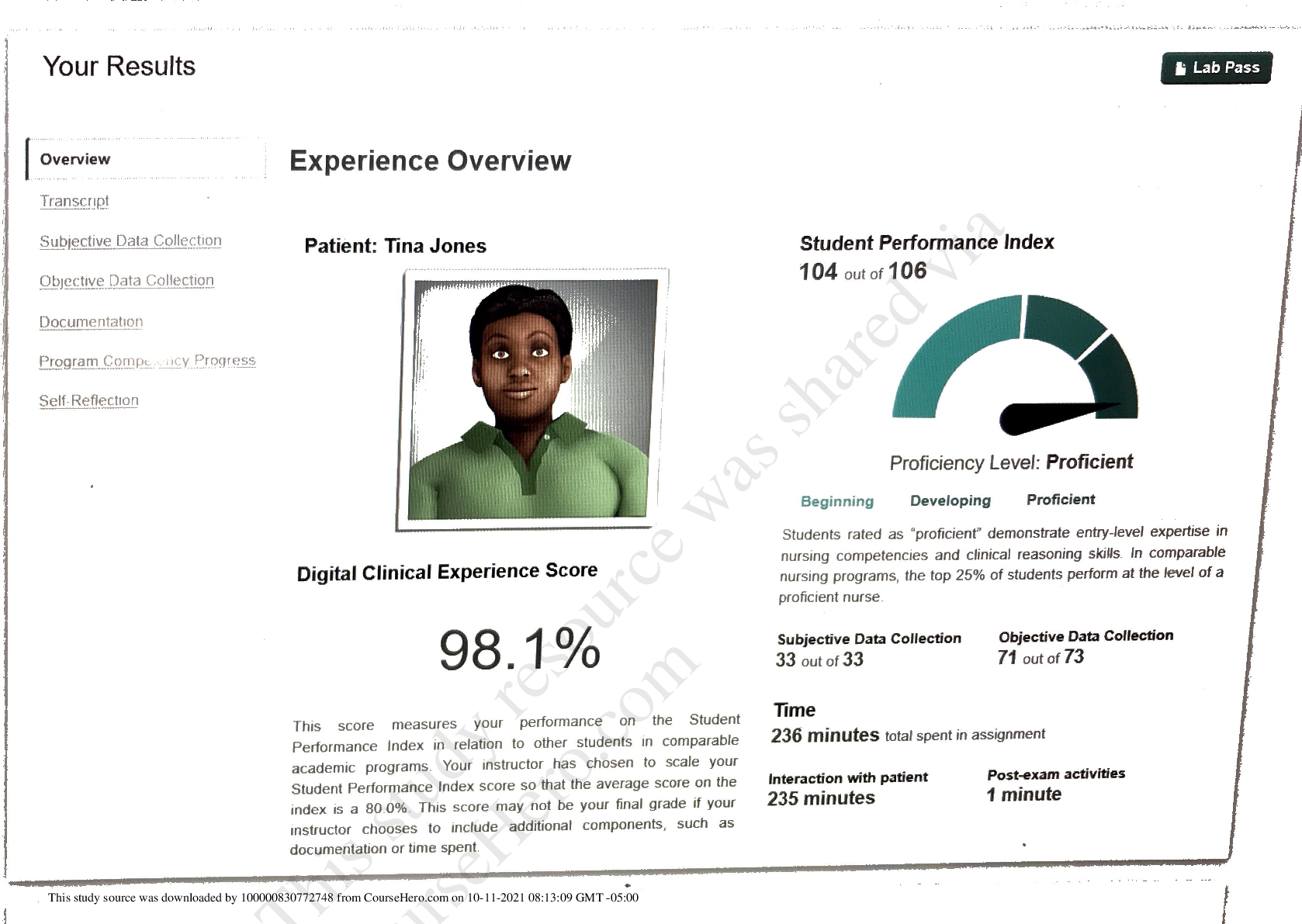
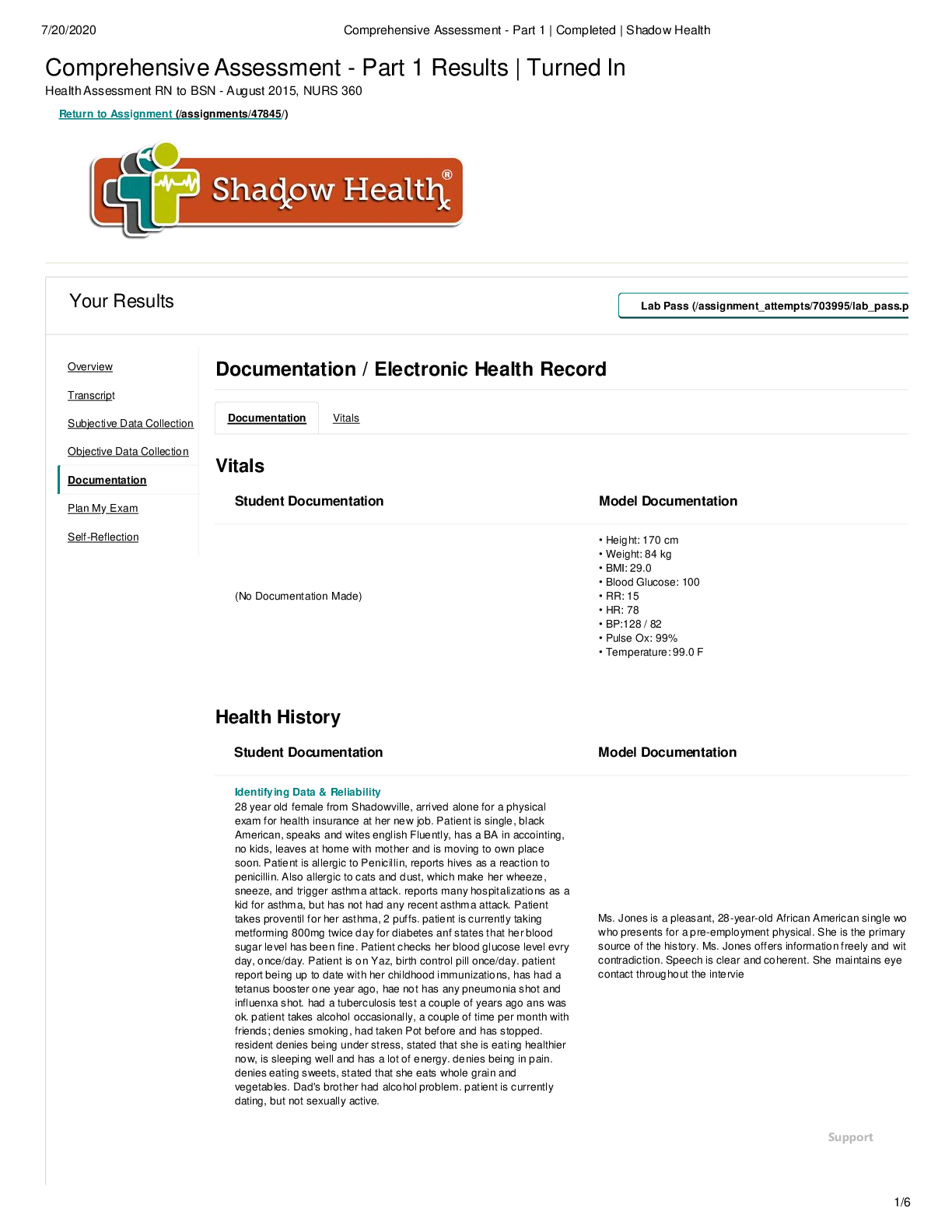
NURS MISC Heart Failure Unfolding Reasoning JoAnn Smith, 72 years old Heart Failure JoAnn Smith, 72 years old Primary Concept Perfusion Interrelated Concepts (In order of emphasis) 1. Gas Exchan... ge 2. Fluid and Electrolyte Balance 3. Clinical Judgment 4. Patient Education 5. Communication 6. Collaboration UNFOLDING Reasoning Case Study: STUDENT History of Present Problem: Heart FailureJoAnn Smith is a 72-year-old woman who has a history of myocardial infarction (MI) four years ago and systolic heart failure secondary to ischemic cardiomyopathy with a current ejection fraction (EF) of only 15%. She presents to the emergency department (ED) for shortness of breath (SOB) the past three days. Her shortness of breath has progressed from SOB with activity to becoming SOB at rest. The last two nights she had to sleep in her recliner chair to rest comfortably upright. She is able to speak only in partial sentences and then has to take a breath when talking to the nurse. She has noted increased swelling in her lower legs and has gained six pounds in the last three days. She is being transferred from the ED to the cardiac step-down where you are the nurse assigned to care for her. Personal/Social History: JoAnn is a retired math teacher who is unable to maintain the level of activity she has been accustomed to because of the progression of her heart failure the past two years. She has struggled with depression the past two years and has been more withdrawn since her husband of 52 years died unexpectedly three months ago from a myocardial infarction. What data from the histories is RELEVANT and has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: MI four years ago, increase shortness of breath at rest; can only speak in partial sentences, ischemic cardiomyopathy with EF of 15% last two nights slept in recliner increased swelling in lower legs gained 6 pounds in last 3 days MI is significant because it decreases heart function due to death of myocardial muscle EF of 15% shows that the heart is having a hard time pumping blood out to rest of the body therefore starving it of oxygenated blood. Weight gain and increased swelling signifies she is fluid overloaded and it can be reason why she is having a hard time talking, breathing, being active and why she has to sleep in a recliner the past 2 nights RELEVANT Data from Social History: Clinical Significance: Retired math teacher, recent widow, history of depression, decreasing activity level Depression might affect her enthusiasm to recover, to stick to a therapy regimen What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect) PMH: Home Meds: Pharm. Classification: Expected Outcome: Diabetes mellitus type II Hypertension Atrial fibrillation Hyperlipidemia Chronic renal insufficiency (baseline creatinine 2.0) Cerebral vascular accident (CVA) with no residual deficits Heart failure (systolic) secondary to ischemic cardiomyopathy MI with stent x2 to LAD 4 years ago 1. ASA 81 mg PO daily 2. Carvedilol 3.25 mg PO daily 3. Lisinopril 5 mg PO daily 4. Ezetimide 10 mg PO daily 5. Hydralazine 25 mg PO 4x daily 6. Torsemide 20 mg PO bid 7. KCL 20 meq PO daily 8. Warfarin 5 mg PO daily 9. Glyburide 5 mg PO daily Antiplatelets Beta blocker ACE inhibitor Cholesterol medication Vasodilator Diuretic Electrolyte replacement Anticoagulant Antidiabetic Decrease chance of clot formation Decrease blood pressure Decrease blood pressure, helps with heart failure, decrease chance of death from heart attack Decrease cholesterol Decrease blood pressure Decrease swelling, decrease fluid overload Increase serum potassium Thins the blood, decrease chance of clot forming Treat type 2 diabetes, helps control blood sugar levelsWhat medications treat which conditions? One disease process often influences the development of other illnesses. Based on your knowledge of pathophysiology, (if applicable), which disease likely developed FIRST that created a “domino effect” in her life? Circle what PMH problem likely started FIRST Diabetes Type 2 Underline what PMH problem(s) FOLLOWED as domino(s) DMT2>hyperlipidemia>hypertension>afib>CVA>MI>CKI>HF Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 98.6 F/37.0 C (oral) Provoking/Palliative: P: 92 (irregular) Quality: Denies Pain R: 26 (regular) Region/Radiation: BP: 162/54 MAP: 90 Severity: O2 sat: 90% (6 liters n/c) Timing: What VS data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: P:92 bpm, irregular R: 26, regular O2 sat: 90%, 6L n/c BP: 162/54 c MAP:90 Pulse is irregular due to atrial fibrillation, increases oxygen demand needs therefore breaths faster and need greater amount of O2 supplied by external oxygen device (nasal canula), Heart has to pump faster to get oxygenated blood out to systemic circulation MAP of 90 suggests that heart has low cardiac output therefore needs higher pressure to get blood to vital organs Current Assessment: GENERAL APPEARANCE: Appears anxious, restless RESP: Breath sounds have coarse crackles scattered throughout both lung fields ant/post, labored respiratory effort, patient sitting upright CARDIAC: Rhythm: atrial fibrillation, pale, cool to the touch, pulses palpable throughout, 3+ pitting edema lower extremities from knees down bilaterally, S3 gallop, irregular, no jugular venous distention (JVD) noted NEURO: Alert and oriented to person, place, time, and situation (x4) GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants GU: Voiding without difficulty, urine clear/yellow SKIN: Skin integrity intact, skin turgor elastic, no tenting present What assessment data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: Gen: appears anxious, restless Resp: coarse crackles through out both lung fields, labored respiratory effort though pt is sitting upright Cardiac: A.Fib, 3+pitting edema LE,s3 gallop, irregular General appearance suggests she is in some distress Lung sounds suggest trouble breathing, fluid overload A.Fib is a dysrhythmia that can impede proper perfusion of blood to body decrease it’s ability to pump oxygenated blood Pitting edema is another sign that pt is fluid overloaded S3 gallop murmur suggest possible mitral stenosisCardiac Telemetry Strip: Interpretation: Irregular, atrial fibrillation Clinical Significance: This cardiac dysrhythmia increases chance of stroke occuring Radiology Reports: Chest x-ray What diagnostic results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Results: Clinical Significance: Bilateral diffuse pulmonary infiltrates consistent with pulmonary edema Excess fluid in lungs, fluid overloaded causes pt to exert more energy to breathe 12 Lead EKG Interpretation: Irregular rhythm, some st segment elevation in leads V3, aVR, II, V2, and V4 Clinical Significance: Irregular rhythm is consistent with diagnosis of atrial fibrillationST segment elevation in v3 and v4 suggest anterior MI ST segment elevation in V2 suggest septal MI MI occurred on LADLab Results: Complete Blood Count (CBC): Current: High/Low/WNL? Prior: WBC (4.5-11.0 mm 3) 4.8 WNL 5.8 Hgb (12-16 g/dL) 12.9 WNL 13.2 Platelets (150-450x 103/µl) 228 WNL 202 Neutrophil % (42-72) 68 WNL 65 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: WBC Platelets Hgb Decrease, no infection Can show sign of bleeding How well O2 is binding to hemoglobin = how well blood is oxygenated Stable Stable Stable Basic Metabolic Panel (BMP): Current: High/Low/WNL? Prior: Sodium (135-145 mEq/L) 133 low 138 Potassium (3.5-5.0 mEq/L) 4.9 wnl 4.2 Glucose (70-110 mg/dL) 105 wnl 118 Creatinine (0.6-1.2 mg/dL) 2.9 high 2.2 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Na: 133 mEq/L Creatine: 2.9 mg/dL Slight hyponatremia Kidney function slightly worse than her baseline Worsening worsening Misc. Chemistries: Current: High/Low/WNL? Prior: Magnesium (1.6-2.0 mEq/L) 1.9 wnl 1.8 PT/INR (0.9-1.1 nmol/L) 2.5 high 2.4 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: PT/INR Tells how long it take for her blood to clot; in therapeutic range for her medications StableWhat lab results are RELEVANT and must be recognized as clinically significant by the nurse? Cardiac Labs: Current: High/Low/WNL? Prior: Troponin (<0.05 ng/mL) 0.10 high 0.12 BNP (B-natriuretic Peptide) (<100 ng/L) 1855 high 155 RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Troponin: 0.10 ng/mL BNP:1855 Increase troponin correlates to injured heart, possible MI Sign of heart failure; inability for heart to pump, higher BNP = worst heart failure Improving Worsening Lab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Creatinine Value: 2.9 Critical value: >2 Measure kidney function Monitor intake and oputput, give diuretics, monitor creatinine for signs of improvement Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: BNP Value: 1855 Critical value: 100 The higher the number the more severe of heart failure the patient is exhibiting BNP is a measurement of how well the heart can pump blood Give ACE inhibitors, monitor BNP for signs of improvement or worsening heart failure Clinical Reasoning Begins… 1. What is the primary problem that your patient is most likely presenting with? The primary problem that my patient is most likely presenting with is congestive heart failure. 2. What is the underlying cause/pathophysiology of this primary problem? The underlying cause of this primary problem is her ejection fraction of 15% due to cardiomyopathy caused by an myocardial infarction and atrial fibrillation.Collaborative Care: Medical Management Care Provider Orders: Rationale: Expected Outcome: Titrate oxygen to keep O2 sat >92% Furosemide 40 mg IV push Nitroglycerin IV drip: titrate to keep SBP <130 Strict I&O Fluid restriction of 2000 mL PO daily Low sodium diet Help oxygenate blood so that her vital organs are sufficiently perfused Help diuresis her, lose water weight Decrease chest pain, decrease blood pressure since nitroglycerin is a vasodilator; it will open up arteries making it easier for the heart to pump blood out to vital oragans Closely monitor what she eats/drinks and voids to prevent further weight gain and or swelling By restricting her to 2000 ml of fluid she will hopefully not gain more water weight, her kidneys will not have to work to hard to eliminate waste products By restricting sodium/consuming a low sodium diet she will not be at risk for fluid overload since water follows sodium. It is also healthy for the heart. Maintain an O2 saturation > 92% Her weight will decrease, swelling will go down, help kidney function Decrease blood pressure Decrease weight, decrease swelling Decrease weight, better kidney function, decrease edema Decrease edema, decrease blood pressure, decrease fluid overload PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: Strict I&O Titrate oxygen to keep O2 sat >95% Furosemide (Lasix) 40 mg IV push bid Nitroglycerin IV drip: titrate to keep SBP <130 Fluid restriction of 2000 mL PO daily Low sodium diet Titrate oxygen to keep O2 sat >95%, nitroglycerin IV drip, Furosemide 40 mg IV push, Strict I&O, fluid restriction =2000 ml and low sodium diet I would titrate to keep O2 saturation >95% first because O2 sat tells me how well she is perfusing oxygenate blood. An O2 saturation below 90% suggest that she may not be getting enough oxygenated blood to vital organs like the brain. She would then have to work harder breathing and her heart will have to pump harder. At the same time that I am titrating O2; I will titrate nitroglycerin to hopes that I can lower her blood pressure so that the heart doesn’t have to work as hard. Nitroglycerin accomplishes this by acting as a vasodilator; opening up the arteries to allow a smoother flow of blood from the heart to the rest of the body. Once blood pressure is under control then I would concentrate her fluid overload by giving her Lasix, this also has the added benefit of helping the heart and lungs since if she doesn’t way as much those organs will not have to work as hard. Strict I&O, fluid restriction and low sodium diet also helps attain this goal. 1 kg = 1000 ml Collaborative Care: Nursing 3. What nursing priority(ies) will guide your plan of care? (if more than one-list in order of PRIORITY) Priorities are maintain O2 sat >95%, decrease blood pressure, decrease fluid overload 4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome: Monitor oxygen saturation Monitor blood pressure Daily weights Strict intake and output Monitor VS, especially BP, HR, RR Ted stockings or SCDs if under bed rest O2 sat tells me how well her blood is oxygenating BP let’s me know how hard her heart is working to pump blood out Strict I&O, SCDs/TED stocking help with decreasing edema O2 sat will remain >95% Blood pressure will decrease to 130 mm Hg systolic Edema will go Ambulate if activity is tolerable Walking helps keep strength, gives her something to do, prevents bed sores, improves circulation down, energy level will increase, will not gain more weight5. What body system(s) will you most thoroughly assess based on the primary/priority concern? I will thoroughly assess her cardiac function, respiratory function, and neurologic functions. 6. What is the worst possible/most likely complication to anticipate? Most likely/worst complication to anticipate would be we over correct her too much and she becomes hypovolemic. 7. What nursing assessments will identify this complication EARLY if it develops? BP gets too low, respirations become shallow and less than 10 per minute, she show signs of change of level of consciousness. 8. What nursing interventions will you initiate if this complication develops? Stop infusing nitroglycerin first and foremost, increase oxygen if needed. Call HCP to see if I can give a med to increase blood pressure/decrease HR. 9. What psychosocial needs will this patient and/or family likely have that will need to be addressed? See if she wants to talk to a Chaplin or other spiritual leader about the unexpected loss of her husband. See if she interested in talking to a psychiatrist about her depression 10. How can the nurse address these psychosocial needs? Get referral for social worker for group therapy, try to contact a chaplin for her to talk to. Just being there and talking to her like a human being and not just a patient. Medication Dosage Calculation: Medication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: Medication/Dose: Furosemide 40 mg IV push loop diuretic that prevent the absorption of sodium IV Push: Volume every 15 sec? 4mg/minute Monitor for signs of hyponatremia Monitor for intake and output Monitor heart rate and blood pressure Daily weights Evaluation: Evaluate the response of your patient to nursing and medical interventions during your shift. All orders have been implemented that are listed under medical management. Four Hours Later… Current VS: Most Recent: Current PQRST: T: 98.4 F/36.9 C (oral) T: 98.6 F/37 C (oral) Provoking/Palliative: P: 88 (irregular) P: 82 (irregular) Quality: Denies pain R: 24 (regular) R: 26 (regular) Region/Radiation: BP: 112/50 MAP: 71 BP: 162/54 MAP: 90 Severity:O2 sat: 91% (12 liters high flow n/c) O2 sat: 90% (6 liters n/c) Timing:Current Assessment: GENERAL APPEARANCE: Not as anxious, but appears restless at times RESP: Coarse crackles scattered throughout both lung fields, labored respiratory effort CARDIAC: Rhythm: atrial fibrillation, pale, cool to the touch, pulses palpable throughout, 3+ pitting edema in lower extremities NEURO: Alert and oriented to person, place, time, and situation (x4) GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all 4 quadrants GU: 30 mL of urine out in the last 4 hours after furosemide IV given, 50 mL residual urine in bladder with bladder scan SKIN: Skin integrity intact 1. What clinical data is RELEVANT that must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: P= 88 bpm, irregular R= 24 breathes/min, regular BP= 112/50; MAP= 71 O2= 91%; 12 high flow n/c Still has A.Fib, breathing has slowed down; blood pressure has decreased therefore heart is not having to pump so hard to get blood out and to organs. O2 saturation still less than 95%; needs twice as much O2 as before and high flow nasal canula. Still might be struggling to get oxygenated blood to other organs RELEVANT Assessment Data: Clinical Significance: Resp: coarse crackles, labored respiratory effort GU: 30 ml of urine in 4 hours even with furosemide IV given Cardiac: no S3 sound, atrial fibrillation persist Pulmonary edema may have worsen, furosemide has not been as effective as thought; renal failure may be more chronic than once thought, should recheck creatinine and BUN. No S3 sound suggests mitral valve functioning more properly. Has not converted out of a. fib, still at risk for clots/stroke developing. 2. Has the status improved or not as expected to this point? Her blood pressure has improved; she still requires a bunch of supplemental oxygen to, coarse crackles can still be heard upon auscultating her lungs. She only managed to produce 30 ml of urine in 4 hours even after receiving 40 ml of furosemide. Has not converted out of atrial fibrillation. 3. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? I would say yes. I would contact HCP to see if her dose of furosemide can be increased. See she needs an echocardiogram to see if her ejection fraction improved; check and see if there are clots forming due to a. fib. 4. Based on your current evaluation, what are your nursing priorities and plan of care? Now that her blood pressure has significantly improved I would divert most of my care with improving her breathing and oxygenation saturation. I would still monitor her blood pressure. See if there is a way to increase her urine output, watch for signs of PE and assess for increase swelling.Your knowledge and application of the pathophysiology of heart failure and renal failure have allowed you to make a series of needed assessments and judgments that have facilitated the treatment and care of your patient. You recognize that an SBAR is needed to update the primary care provider with your concerns. SBAR: Nurse-to-Primary Care Provider Situation: Name/age: JoAnn Smith, 72 BRIEF summary of primary problem: exacerbation of CHF due possible PE and chronic renal failure Day of admission/post-op #:1 Background: Primary problem/diagnosis: Congestive heart failure related to cardiomyopathy AEB increase shortness of breath, ejection fraction of 15%, and atrial fibrillation RELEVANT past medical history: MI 4 years ago, type 2 diabetes, hypertension, atrial fibrillation, hyperlipidemia, Assessment: Most recent vital signs: P: 88 (irregular), R: 24 (regular), BP: 112/50 (MAP= 71), T: 98.4 °F, O2 sat: 91% (12 L high flow n/c), no pain RELEVANT body system nursing assessment data: Resp: coarse crackles, labored respiratory effort GU: 30 ml of urine in 4 hours even with furosemide IV given Cardiac: no S3 sound, atrial fibrillation persist RELEVANT lab values: Creatinine: 2.9 mg/dL, BNP: 1855 ng/L, Troponin:0.10 ng/mL, Na:133 mEq/L, Mg: 1.9 mEq/L INTERPRETATION of current clinical status (stable/unstable/worsening): worsening Recommendation: Suggestions to advance plan of care: transfer to ICU, check K+ stat, check ABG, check creatinine, new 12 ECGNew Orders from Primary Care Provider: Stat potassium, creatinine, arterial blood gases Transfer to ICU RESULTS: Current High/Low/WNL? Most Recent Potassium (3.5-5.0 mEq/L) 5.9 high 5.5 Creatinine (0.6-1.2 mg/dL) 3.5 high 2.7 RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: K+: 5.9 mEq/L Creatinine: 3.5 mg/dL Hyperkalemia, can cause cardiac dysrhythmias Increase sign of renal failure, kidney function is getting worst Worsening Worsening Arterial Blood Gas: Current: pH (7.35–7.45) 7.46 pCO2 (35–45) 30 pO2 (80–-100) 72 HCO3 (18–26) 22 O2 sat (>92%) 91% RELEVANT Lab(s): Clinical Significance: pH: 7.46 pCO2: 30 HCO3: 22 Respiratory alkalosis most likely due to hyperventilation ABG Interpretation: Respiratory alkalosis, compensatedIt is now the end of your shift. Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the nurse who will be caring for this patient in ICU: SBAR: Nurse-to-Nurse Situation: Name/age: JoANN Smith, 72 BRIEF summary of primary problem: exacerbation of CHF due possible PE and chronic renal failure Day of admission/post-op #: 1 Background: Primary problem/diagnosis: Congestive heart failure RELEVANT past medical history: MI past 4 years, increase SOB, ejection fraction 15%, hypertension, hyperlipidemia, type 2 diabetes, A. Fib Assessment: Most recent vital signs: P: 88 bpm (irregular), R: 24 breathes/min (regular), T: 98.4°F, BP:112/50 (MAP:71), O2 sat:91% on 12 L high flow n/c RELEVANT body system nursing assessment data: Resp: coarse crackles, labored breathing, Cardiac: A.Fib, GU: 30 mL of urine produced in 4 hours even after receiving 40 mg IV push RELEVANT lab values: Creatinine: 3.5 mg/dL, BNP: 1855 ng/L, Troponin:0.10 ng/mL, Na: 133 mEq/L, Mg: 1.9 mEq/L, K+: 5.9 mEq/L, pH: 7.46, PaCO2: 30, HCO3: 22, INR/PT: 2.5 . TREND of any abnormal clinical data (stable/increasing/decreasing): creatinine is worsening, K+ is worsening, troponin is stable, PT/INR is stable, BNP is worsening INTERPRETATION of current clinical status (stable/unstable/worsening): unstable, worsening Recommendation: Suggestions to advance plan of care: transfer to ICU, monitor ABGs q4 hours, blood pressure q15 minutes, monitor K+, creatinine and BNP q4 hoursEducation Priorities/Discharge Planning 1. What will be the most important discharge/education priorities you will reinforce with the patient’s medical condition to prevent future readmission with the same problem? The most important discharge/education I will reinforce how to use supplemental oxygen properly and the signs and symptoms pulmonary edema. I would advise her wear TED stockings, watch her weight, try and be active as much as possible so that she doesn’t develop any pressure ulcers from being bed rest. Take her blood pressure frequently through out the day. The importance of taking her medication especially the furosemide and warfarin. The furosemide is important because it will help prevent her from retaining fluid and swelling up. The warfarin is important because it will prevent clots forming and decrease the possibility of having a stroke as result. 2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient?I would ask her to demonstrate taking her blood pressure, have her tell me what the s/sx of respiratory alkalosis are, s/sx of hyperkalemia. I would have her demonstrate using the supplemental oxygen system and demonstrate how to turn, cough, deep breath Caring and the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? She probably still struggling to breathe but not as much as she did when she first got admitted 2. What can you do to engage yourself with this patient’s experience, and show that she matters to you as a I would demonstrate how to use TCDB method, don’t rush out of the room as soon as I am done taking blood pressure or whatever nursing intervention I came in to do. Just letting her know that I am there for her if she needs anything or just wants talk. Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? I learned that a person can function with a low ejection fraction for a while before it becomes too debilitating. I learned that the domino effect is not something to take lightly and it is our job as RNs to educate a patient as well as possible so that they can understand how a disease may effect them in the future. How it canprogress into something that is not treatable. I also learned that I person can lose all desire to live after the passing of a loved one. 2. How can I use what has been learned from this scenario to improve patient care in the future? I would try and contact the HCP sooner to get an ABG and maybe a BMP.Lastly, create a Shift Summary Nursing Note. The below are recommended subject areas: Reason for hospitalization: Abnormal and pertinent normal on nursing assessment: Nursing Interventions for shift: Patient Education: Discharge plan: [Show More]
Last updated: 1 year ago
Preview 1 out of 19 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
19
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
160










 Transcript.png)