NR 602 Week 3 iHuman SOAP SOAP Note Template
Document Content and Description Below
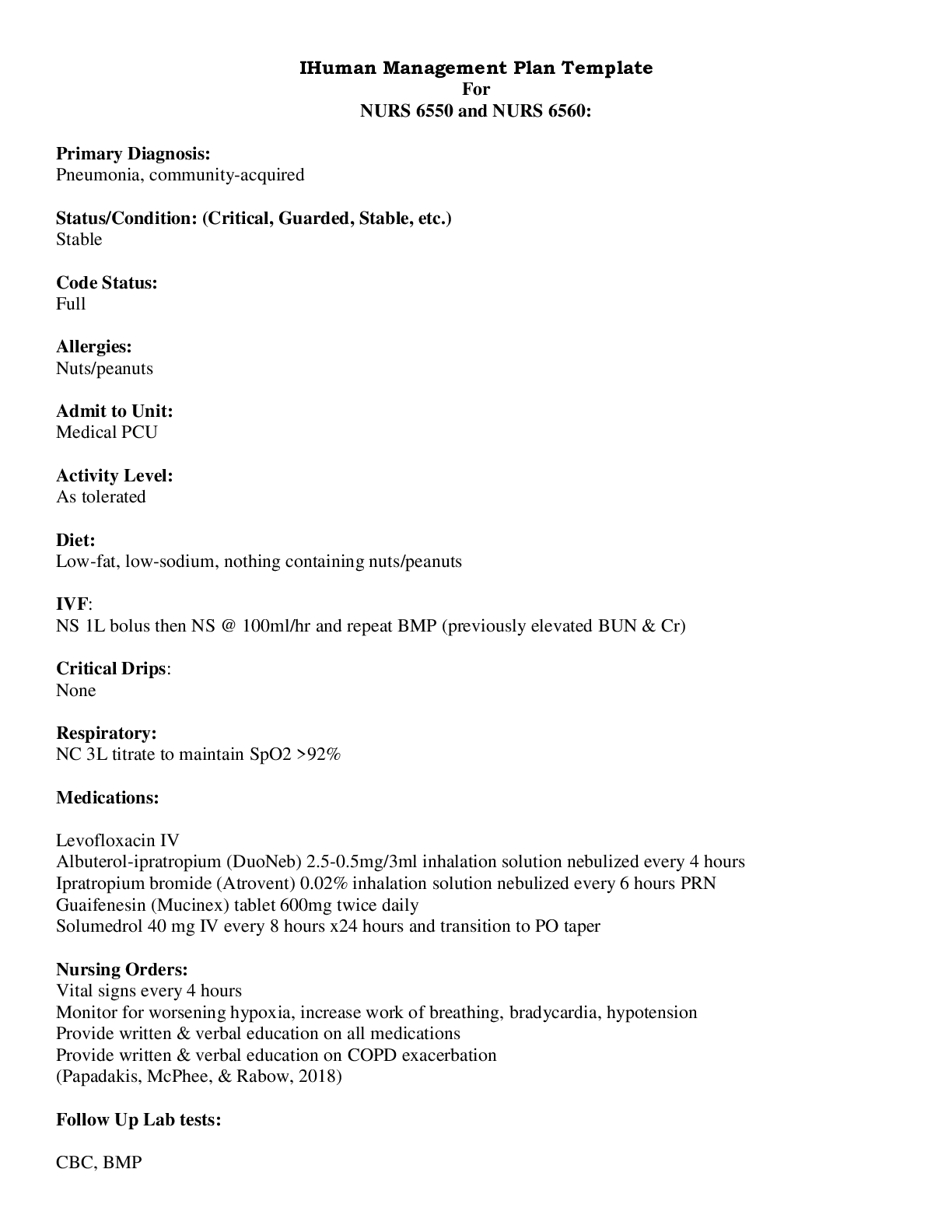
NR 602 Week 3 iHuman SOAP SOAP Note Template NR 602 Week 3 iHuman SOAP SOAPNoteTemplate Initials: J Age: 65 YO Gender: F Height Weight BP HR RR Temp SPO2 Pain Rating Allergies (and reaction) ... 5’5” 126 Clic kor tap here to ente r text. Clic k or tap her eto ent er text. Cli c k or tap her e to ent er text. Click or tap here to enter text. Click or tap hereto enter text. Medication: KNA Food: Click or tap here to enter text. Environment: Click or tap here to enter text. History of Present Illness (HPI) Chief Complaint (CC) Trouble sleeping and increase in fatigue CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset A few months ago, intermittent. Now several times a week Location Click or tap here to enter text. Duration Several months and several times a week Characteristics Gittery and nervous and losing weight. Difficulty falling asleep and awakening early. Difficulty getting back to sleep. Light sleeping and hearing everything.Can fall back asleep but it takes awhile. Aggravating Factors Denies Relieving Factors denies Treatment Has tried a glass of milk. Retired and denies pressure or anxiety. Gets up to do housework and goes back to bed later. Unsure of how frequently she’s wakingup and hasn’t kept track of what times she awakens. Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Dosage Frequency Length Used of Time Reason for Use S: Subjective Information the patient or patient representative told youHomeopathic) Multivitamin daily Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Calcium daily Click or tap here to Click or tap here to enter Click or tap here Click or tap here to enter text.enter text. text. to enter text. Metamucil daily Click or tap here toenter text. Click or tap here to entertext. Click or tap hereto enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here toenter text. Click or tap here to entertext. Click or tap hereto enter text. Click or tap here to enter text. Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Denies current or past medical problems. Occasional headaches. Occasional GERD. Chronic constipation. Hospitalized during the birth of her twochildren. Childhood illnesses: mumps, measles, rubella Immunizations: tetanus within the last 10 years, varicella Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Mother of two children. Normal American Diet Exercises – plays tennis on weekends. Colonscopy at age 58 normal. Yearly mammograms all negative with dense breast tissue. Non-smoker (smoked occasionally in college). Drinks alcohol socially (1-2x per month; goes out with girlfriends). Denies recreational drug use. Married, monogamous, no history of STDS or herpes. Retired high school science teacher. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent.Father: deceased at 90 from pneumonia, history of asthma and osteoarthritis Mother: died in hit and run car accident at age 71. Maternal grandmother: deceased and died of a stroke, history of being “nervous” and was told it was her thyroidMaternal grandfather: died in war, no medical problems Paternal grandmother: died of breast cancer Paternal grandfather: died of prostate cancerNo siblingsReview of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional If patient denies all symptoms for this system,check here: ☐ Skin If patient denies all symptoms for this system, check here: ☐ HEENT If patient denies all symptoms for this system, check here: ☐ ☒Fatigue Click or tap hereto enter text. ☐ Weakness Click or taphere to enter text. ☐ Fever/Chills Click or taphere to enter text. ☐ Weight Gain denies ☒Weight Loss Click or taphere to enter text. ☒Trouble Sleeping Click ortap here to enter text. ☐ Night Sweats denies ☐ Other: Click or tap here to enter text. ☐ Itching Click or taphere to enter text. ☐ Rashes Click or taphere to enter text. ☒Nail Changes Clickor tap here to enter text. ☐ Skin Color ChangesClick or tap here to enter text. ☒Other: Hair thinning ☐ Diplopia Click or taphere to enter text. ☐ Eye Pain Click or taphere to enter text. ☐ Eye redness Click ortap here to enter text. ☐ Vision changes Click ortap here to enter text. ☐ Photophobia Click ortap here to enter text. ☐ Eye discharge Click ortap here to enter text. ☐ Earache Click or tap hereto enter text. ☐ Tinnitus Click or tap hereto enter text. ☐ Epistaxis Click or taphere to enter text. ☐ Vertigo Click or tap hereto enter text. ☐ Hearing Changes Clickor tap here to enter text. ☐ Hoarseness Click or tap hereto enter text. ☐ Oral Ulcers Click or tap hereto enter text. ☐ Sore Throat Click or tap hereto enter text. ☐ Congestion Click or tap hereto enter text. ☐ Rhinorrhea Click or tap hereto enter text. ☐ Other: Click or tap here to enter text.Respiratory If patient denies all symptoms for thissystem, check here: ☐ Neuro If patient denies all symptomsfor this system, check here: ☐ Cardiac and Peripheral Vascular If patient denies all symptoms for this system, check here: ☐ ☐ Cough Click or tap here to enter text. ☐ Syncope or Lightheadedness Click or tap ☐ Chest pain Click or tap here to entertext. ☒Palpitations over the pastfew years☐ Hemoptysis Click or tap here to enter text. ☐ Dyspnea Click or tap here to entertext. ☐ Wheezing Click or tap here to entertext. ☐ Pain on Inspiration Click or tap hereto enter text. ☐ Sputum Production ☐ Other: Click or tap here to entertext. here to enter text. ☒Headache Click or tap hereto enter text. ☐ Numbness Click or tap hereto enter text. ☐ Tingling Click or tap here toenter text. ☐ Sensation Changes ☐ Speech Deficits Click or taphere to enter text. ☐ Other: Click or tap here toenter text. ☒SOB breathing harder and heartbeats faster with ☒Exercise Intolerance exhausted withweekly tennis ☐ Orthopnea Click or tap here to entertext. ☐ Edema Click or tap here to enter text. ☐ Murmurs Click or tap here to entertext. ☒Faintness struggles withheat ☐ Claudications Click or taphere to enter text. ☐ PND Click or tap here toenter text. ☐ Other: Click or tap here toenter text. MSK If patient denies all symptoms forthis system, check here: ☒ GI If patient denies all symptoms for thissystem, check here: ☒ GU If patient denies all symptoms for this system, check here: ☒ PSYCH If patient denies all symptoms for this system, check here: ☐ ☐ Pain Click or tap here to entertext. ☐ Stiffness Click or tap here toenter text. ☐ Crepitus Click or tap here to entertext. ☐ Swelling Click or tap here to entertext. ☐ Limited ROM ☐ Redness Click or tap here toenter text. ☐ Misalignment Click or tap here toenter text. ☐ Other: Click or tap here to entertext. ☐ Nausea/Vomiting Click or tap here toenter text. ☐ Dysphasia Click or tap here to entertext. ☐ Diarrhea Click or tap here to entertext. ☐ Appetite Change Click or tap here toenter text. ☐ Heartburn Click or tap here to entertext. ☐ Blood in Stool Click or tap here toenter text. ☐ Abdominal Pain Click or tap here toenter text. ☐ Excessive Flatus Click or tap here toenter text. ☐ Urgency Click or tap here toenter text. ☐ Dysuria Click or tap here toenter text. ☐ Burning Click or tap here toenter text. ☐ Hematuria Click or tap hereto enter text. ☐ Polyuria Click or tap here toenter text. ☐ Nocturia Click or tap here toenter text. ☐ Incontinence Click or taphere to enter text. ☐ Other: Click or tap here toenter text. ☐ Stress Click or tap here toenter text. ☐ Anxiety Click or tap here toenter text. ☐ Depression Click or tap hereto enter text. ☐ Suicidal/Homicidal IdeationClick or tap here to enter text. ☐ Memory Deficits Click or taphere to enter text. ☐ Mood Changes Click or taphere to enter text. ☐ Trouble Concentrating Clickor tap here to enter text. ☐ Other: Click or tap heretoenter text.☐ Food Intolerance Click or tap here toenter text. ☐ Rectal Bleeding Click or tap here toenter text. ☐ Other: GYN If patient denies all symptoms for thissystem, check here: ☒ Hematology/Lymphatics If patient denies all symptoms for this system, check here: ☒ Endocrine If patient denies all symptoms for this system, check here: ☐ ☐ Rash Click or tap here to enter text. ☐ Discharge Click or tap here to enter text. ☐ Itching Click or tap here to enter text. ☐ Irregular Menses Click or tap here toenter text. ☐ Dysmenorrhea Click or tap here to entertext. ☐ Foul Odor Click or tap here to enter text. ☐ Amenorrhea Click or tap here to entertext. ☐ LMP: Click or tap here to enter text. ☐ Contraception Click or tap here to entertext. ☐ Other:Click or tap here to enter text. ☐ Anemia Click or tap here to enter text. ☐ Easy bruising/bleeding Click or tap here toenter text. ☐ Past Transfusions Click or tap here to entertext. ☐ Enlarged/Tender lymph node(s) Click or taphere to enter text. ☐ Blood or lymph disorder Click or tap here toenter text. ☐ Other Click or tap here to enter text. ☐ Abnormal growth Click or tap here to entertext. ☐ Increased appetite Click or tap here to entertext. ☐ Increased thirst denies ☐ Thyroid disorder Click or tap here to enter text. ☐ Heat/cold intolerance heat intolerant ☐ Excessive sweating Click or tap here to entertext. ☐ Diabetes Click or tap here to enter text. ☐ Other Click or tap here to enter text.O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and percussion. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. Pertinent positive are the “abnormal” findings and pertinent “negative” are the expected normal findings. Separate the assessment findings accordingly and be detailed.Body System Positive Findings Negative Findings General Pleasant 65-year-old female appropriately dressed and appropriateresponses to questions Click or tap here to enter text. Skin HEENT Warm and dry. Palms moist. No obvious skin lesions seen. Normalskin turgor. Hair is dry but typical for age. Normal thickness and distribution pattern for patient gender. Eyebrows: sparse; missing lateral aspect. No swelling of extremities or deformities. No cyanosis, clubbing or edema. Eyes: no erythema or swelling; positive for lid retraction and mild lidlag; no proptosis. Conjunctivae: pink, no discharge. Sclerae: anicteric. Orbital area: no edema, redness, tenderness or lesions noted. Lateral outside third of eyebrow is missing bilaterally. Neck has no visible scars, deformities or other lesions and trachea is midline. Thyroid is soft, 45gm in size. Isthmus ropey, easily palpable, slight bilateral asymmetry R>L, no nodules palpated. Thyroid moves with swallowing and no nodules are felt. Click or tap here to enter text. Click or tap here to enter text. Respiratory Neuro Chest is symmetrical and the anterior-posterior diameter is normal.The excursion with respiration is symmetrical and there are no abnormal retractions or use of accessory muscles. No distention, scars, masses or rashes. No fasiculations. Slightly coarse tremor in extended hand. Hyperreflexia of biceps and brachioradialis tendons. Click or tap here to enter text. Click or tap here to enter text. Cardiovascular PMI is in the 5th intercostal space at the mid-clavicular line. RRR. Click or tap here to enter text. Musculoskeletal Normal muscle bulk and tone. Click or tap here to enter text.Gastrointestinal Abdomen is flat and symmetric with no scars, deformities, striae orlesions. Hyperactive bowel sounds. Click or tap here to enter text.2. Click or tap h A: Assessment Medical Diagnoses. Provide 3 differential diagnoses (DDx) which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support eachdiagnosis. Diagnosis ICD-10 Code Pertinent Findings Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Problem List 1. Click or tap here to enter text. 6. Click or tap here to enter text. 11. Click or tap here to enter text. ere to enter text. 7. Click or tap here to enter text. 12. Click or tap here to enter text. 3. Click or tap here to enter text. 8. Click or tap here to enter text. 13. Click or tap here to enter text. 4. Click or tap here to enter text. 9. Click or tap here to enter text. 14. Click or tap here to enter text. 5. Click or tap here to enter text. 10. Click or tap here to enter text. 15. Click or tap here to enter text.Click or tap here to enter text. Click or tap here to enter text.P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention. Diagnostics: List tests you will order this visit Test Rationale/Citatio n Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text.Click or tap here to enter text. Click or tap here to enter text. Medications: List medications/treatments including OTC drugs you will order and “continue meds” if pertinent. Dru g Dosag e Length of Treatment Rationale/CitationClick or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Referral/Consults: Click or tap here to enter text. Rationale/Citation Click or tap here to enter text. Education: Click or tap here to enter text. Rationale/Citation Click or tap here to enter text. Follow Up: Indicate when patient should return to clinic and provide detailed symptomatology indicating if the patient should return sooner than scheduled or seek attention elsewhere. Click or tap here to enter text. Rationale/Citation Click or tap here to enter text. . [Show More]
Last updated: 1 year ago
Preview 1 out of 17 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 07, 2022
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Nov 07, 2022
Downloads
0
Views
65