Health Care > DISCUSSION POST > HSM-542 Week 2 Discussion 1: Delineation of Clinical Privileges and Discussion 2: Ethics Committee (All)
HSM-542 Week 2 Discussion 1: Delineation of Clinical Privileges and Discussion 2: Ethics Committee (GRADED)
Document Content and Description Below
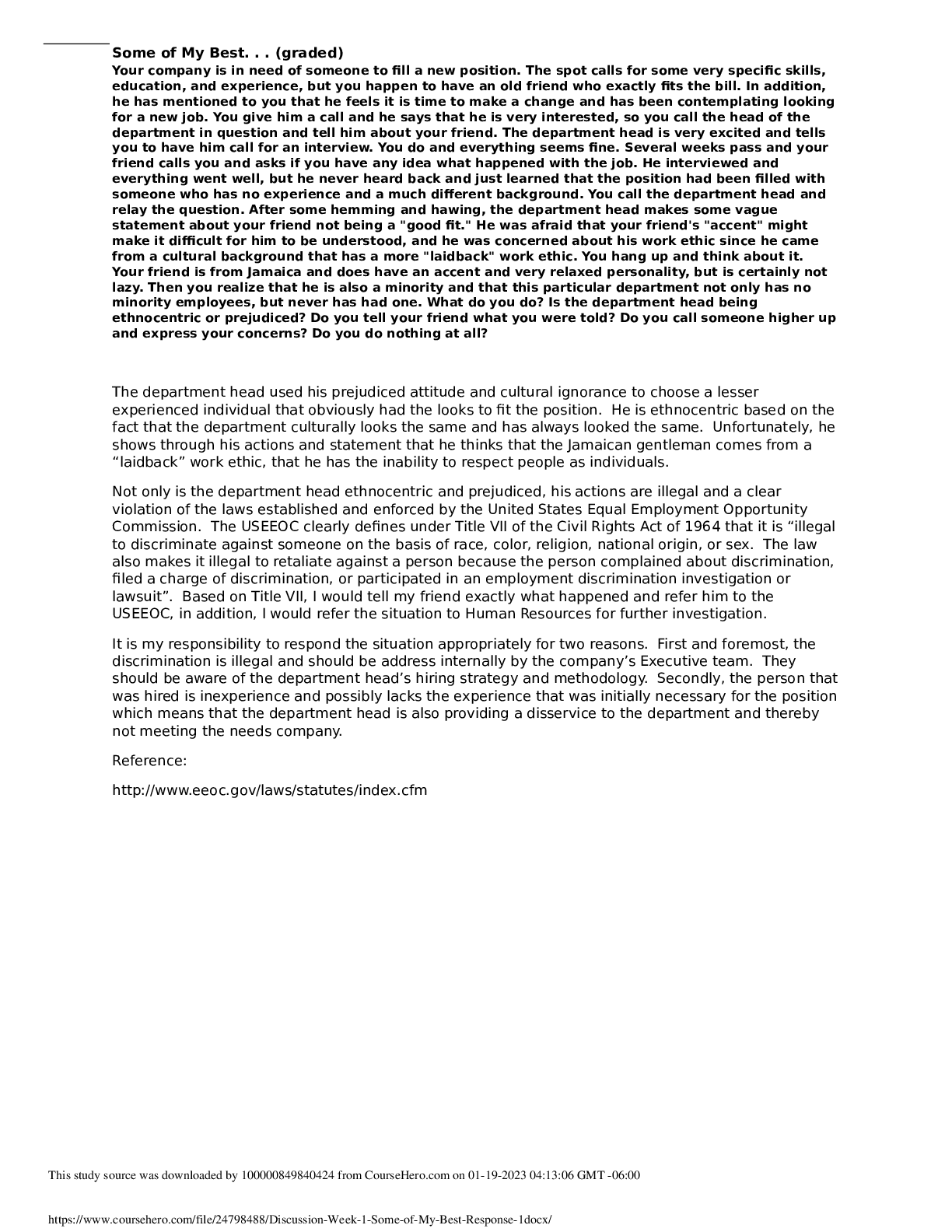
HSM-542 Week 2 Discussion 1: Delineation of Clinical Privileges According to this week’s lesson, the credentialing and privileging of physicians or medical staff is the responsibility ... of the board of directors. First step is the credentialing process, which reviews the verification of license, education, training, and experience (Showalter, 2017) of the candidate. “Medical staff credentialing is one of the most important tasks boards undertake to ensure quality of care in their organizations” (Boardroom Basics, n.d.). In order to determine that a physician applicant is qualified and competent, the hospital medical staff needs to go through the physician’s qualifications to make sure they match up with the requirements set forth by the hospital. This includes: • Education • Residency and fellowship experiences • Privileges at other healthcare organizations • Verification of professional liability insurance • History of any malpractice claims • Quality of care data collected at other healthcare organizations • Professional references • Other information as defined by the healthcare organization Once a practitioner is credentialed and all this information has been confirmed, the physician’s skills need to be evaluated to ensure that the candidate is proficient and can competently meet the needs of the facility. This will take place as part of the privileging process. This process reviews a physician's capability to deliver specific services and medical procedures (Showalter, 2017). Regular reappointment of the medical staff is important for patient safety because it ensures that they stay up to date and relevant on the latest knowledge and techniques. The re-credentialing process is important because it: • Helps to increase patient safety • Provides for a better quality of care • Reduces the risk of lawsuits that results from medical errors Sources: Boardroom Basics. (n.d.). Medical Staff Credentialing. Retrieved from https://www.mnhospitals.org/Portals/0/Documents/Trustees/briefs-resources/credential.pd Showalter, J. S. (2017). The Law of Healthcare Administration, Eighth Edition. [VitalSource Bookshelf]. Retrieved from https://online.vitalsource.com/#/books/9781567938777/cfi/277!/4/[email protected]:40. Ethics committees grew “out of legal controversies regarding the refusal of life-sustaining treatment” (Annas & Grodin, 2016) and have been evolving ever since. The purpose of most ethics committees today are to help when situations arise where families, patients and the medical staff involved either don’t agree on a prescribed treatment (where that treatment is deemed necessary for the well-being of the patient by the medical staff and the patient and/or family refuses), or there is a desire that an ongoing medical treatment be terminated by the patient or family. An instance of this can be in the case where a proposed treatment plan goes against someone’s religious beliefs (i.e. blood transfusion, etc.) or another example can be when a family refuses to go along with a patient’s DNAR request. In these instances, the ethics committee becomes involved. There are four (4) main things that these committees try to do. • Make sure that patients and their families are educated about what a treatment is, does and the result the treatment is trying to achieve, in the event the treatment is being refused or terminated • Assist with the development and implementation of policies, such as end-of-life care and drafting of DNAR (do not attempt resuscitation) policies and the review of complicated cases that reflect systemic problems and requiring policy changes • Assist with brain death determinations • Review of ongoing cases, which requires a consultation mechanism or subcommittee meeting rather than the convening of an entire committee (Annas & Grodin, 2016) Source: Annas, G., & Grodin, M. (2016). Hospital Ethics Committees, Consultants, and Courts. AMA Journal of Ethics, 18(5), 554-559. doi:10.1001/journalofethics.2016.18.5.sect1-1605. [Show More]
Last updated: 1 year ago
Preview 1 out of 2 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 06, 2022
Number of pages
2
Written in
Additional information
This document has been written for:
Uploaded
Oct 06, 2022
Downloads
0
Views
73


.png)