NCLEX RN STUDY GUIDE 1.
Document Content and Description Below
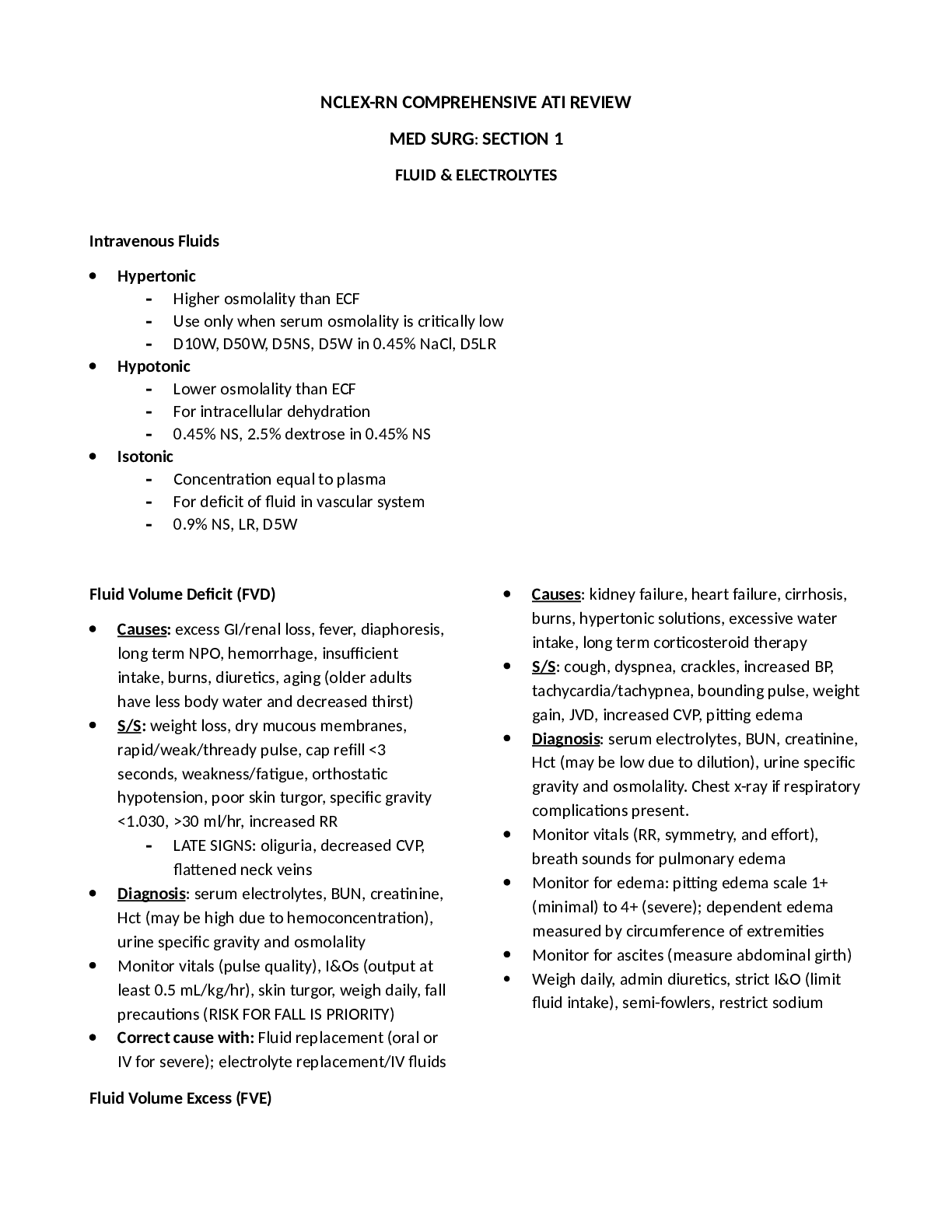
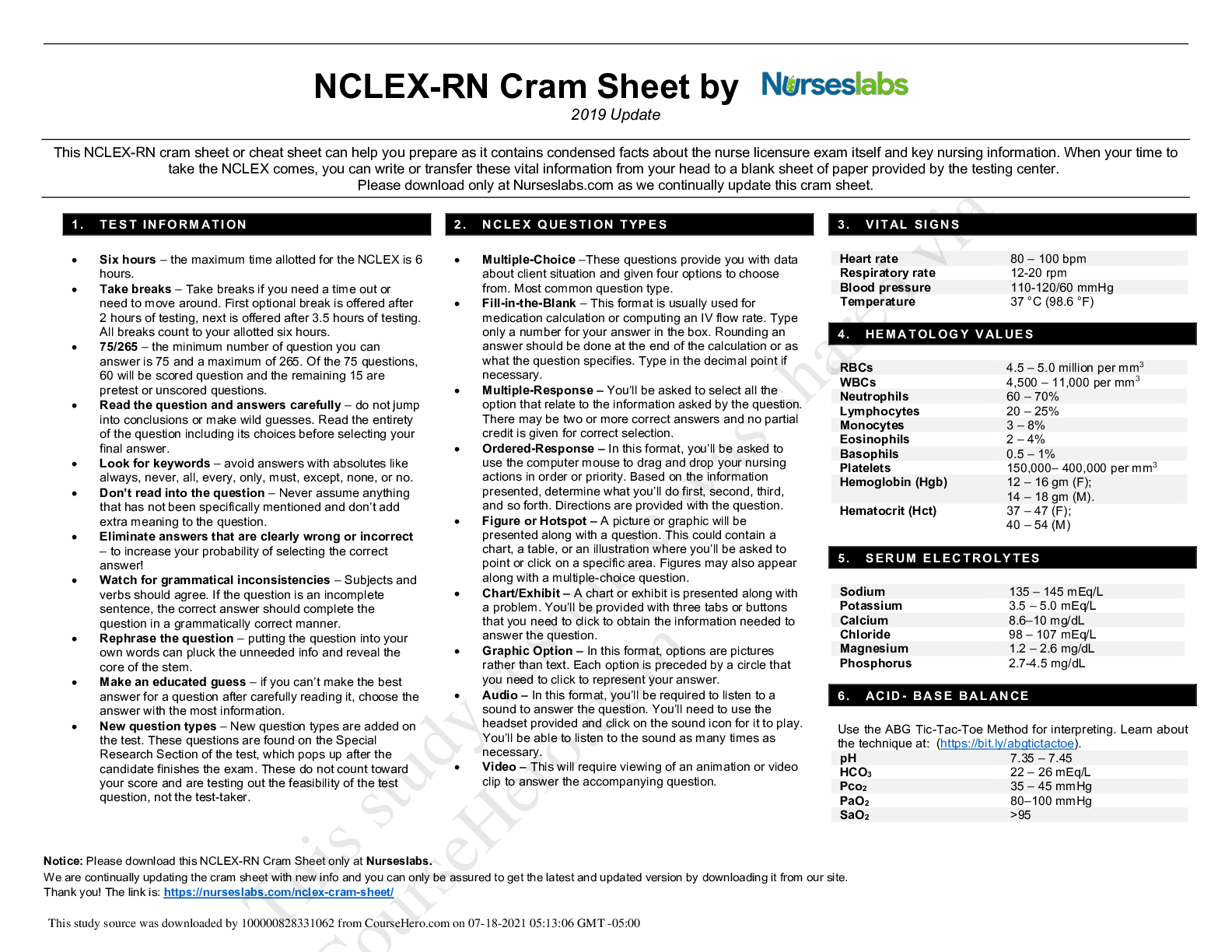
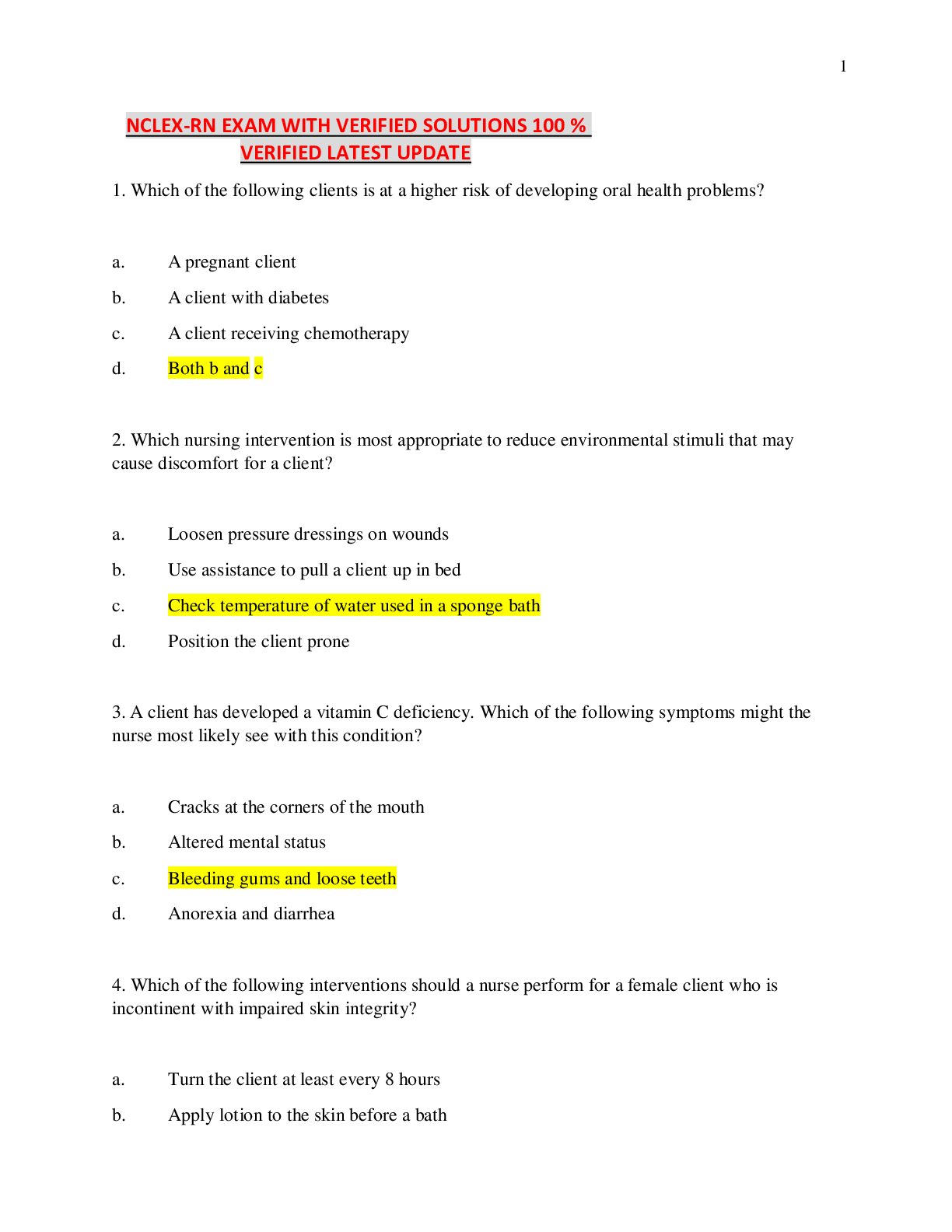
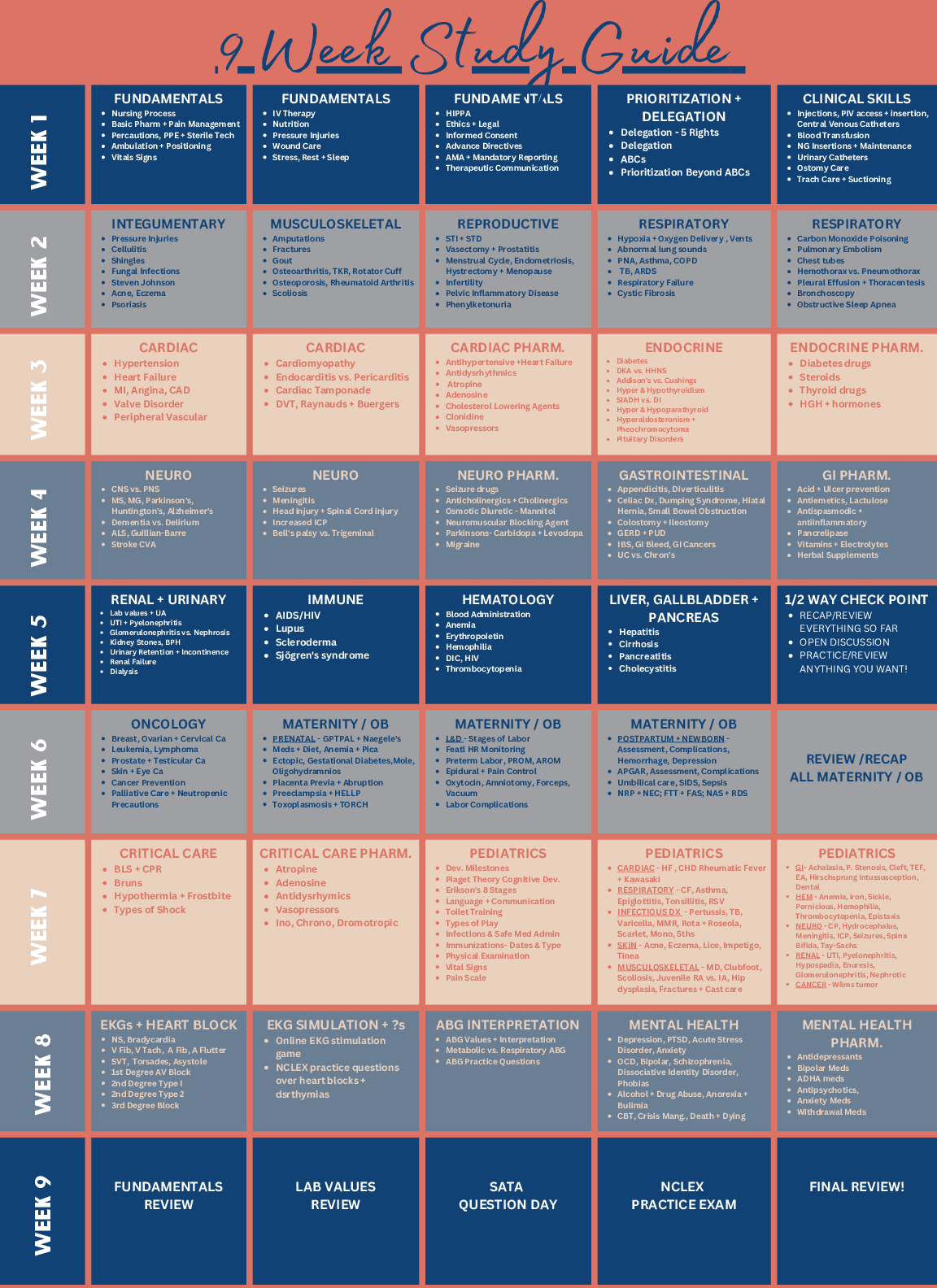
NCLEX RN STUDY GUIDE DO NOT DELEGATE WHAT YOU CAN EAT! Evaluate Assess Teach Don’t delegate Unstable patients Initial Assessment, Teaching, IV drips, Evaluations only RN AIRBORNE ... TRANSMISSION-BASED PRECAUTIONS: MTV Measles TB Varicella-Chicken Pox/Herpes Zoster-Shingles Private Room: Negative pressure with 6-12 air exchanges/hr Mask: N95 for TB DROPLET TRANSMISSION-BASED PRECAUTIONS: Think of SPIDERMAN! Sepsis Scarlet fever Streptococcal Pharyngitis (Streptococcus group A/ Strep Throat): Can Lead to Glomerulonephritis & Rheumatic Parvovirus B19 Fever. Pneumonia Pertussis Influenza/ Haemophilus influenza type B Diphtheria (Pharyngeal): Serious bacterial infection. Epiglottitis: Medial Emergency! No Throat Inspection. Rubella/ German measles Mumps Meningitis/ Neisseria Meningitidis Mycoplasma/ Meningeal Pneumonia An - Adenovirus Private Room or Cohort Surgical mask PRN for Procedures Mask 3ft Distance CONTACT PRECAUTION TRANSMISSION-BASED PRECAUTIONS: MRS.WEE Multidrug resistant organism/ MRSA/ VRE Respiratory infection Skin infections Wound infection Enteric infection - Clostridium Difficile Eye infection – Conjunctivitis *MRSA - Contact precaution ONLY. Use Chlorhexidine Wipe! *VRSA - Contact & Airborne precaution (Private room, door closed, negative pressure) *SARS (Severe Acute Resp Syndrome) Airborne & Contact (just like Varicella) SKIN INFECTIONS- VCHIPS- CONTACT Varicella Zoster Cutaneous Diphtheria (Bacteria Infection in the Wound) Herpes Simplex Impetigo (Bacterial Skin Infection) Pediculosis (Lice) Scabies (Itchy Skin condition. Burrowing Trail of the Scabies Mite) Middle East Respiratory Syndrome (MERS): Viral respiratory illness caused by Coronavirus (MERS-CoV). S/S: Fever, Cough, SOB, and Death. The Incubation Period is 5-6 days but can range from 2-14 days. CDC: Standard (Gloves), Contact (Gown), Eye Protection (Goggles), Airborne Precautions (N95) Negative room: Negative disease (TB, Disseminated Herpes Zoster) Positive room: Protect the Patient (HIV, Cancer) Addison’s= hyponatremia, hypotension, decreased blood vol, hypoglycemia, hyperKalemia, HyperCalcemia. Cushing’s= HyperNatremia, HyperTension, Incr. Blood Vol, HyperGlycemia, hypokalemia, hypocalcemia. Managing Stress in a patient with Adrenal Insufficiency (Addison’s) is paramount, because if the Adrenal glands are stressed further it could result in Addisonian Crisis. Addison’s: Remember BP is the most Important assessment parameter, as it causes Severe Hypotension. Addison’s: (need to "add" hormone): Hypoglycemia, Dark pigmentation, Decr. Resistance to Stress, fractures, Alopecia, Weight Loss, GI distress. Vitiligo. Mood swings (Normal) Need to Report S/S of Infection/ Fever (Addisonian Crisis) Tx: Mineral Corticoids. Addisonian Crisis: Hypoglycemia, Confusion, n/v, Abd Pain, Extreme Weakness, Dehydration, Decr. BP. Cushings: (have extra "Cushion" of Hormones): Hyperglycemia, prone to Infection, Muscle Wasting, Weakness, Edema, HTN, Hirsutism, Moonfaced/Buffalo Hump Cause: Excessive production of Corticotropin (Hyperplasia of the Adrenal Cortex) & Cortisol-secreting Adrenal Tumor. Prednisone Toxicity: Cushing’s syndrome- Buffalo Hump, Moon face, Hyperglycemia, Hypertension. Acetaminophen: 10-20. Max 4000mg per day. Acetaminophen Poisoning: Possible Liver Failure for about 4 days. Close observation required. Tx: (Antidote) n-AcetylCysteine/Mucomyst AcetylSalicyclic Acid (ASA): Metabolic Acidosis. S/S: Tinnitus, Coffee Ground Emesis (Old Blood), Black tarry stools (Melena), Bruising, Tachycardia, Hypotension, GI Ulcers. Tx: Activated Charcoal, then IV Na+ Carbonate. Acromegaly: Coarse Facial feature. Assess Cardiac Problems (eg. S3, S4). Acute Respiratory Distress Syndrome (ARDS): The 1st Sign is Incr. Respirations. Later comes Dyspnea, Retractions, Air Hunger, Cyanosis. Cardinal sign is Hypoxemia (Low O2 level in tissues). Refractory Hypoxemia is the hallmark of ARDS, a progressive form of acute respiratory failure that has a high Mortality rate. It can develop following a Pulmonary Insult (eg, aspiration, pneumonia, toxic inhalation) or nonpulmonary insult (eg, sepsis, multiple blood transfusions, trauma) to the Lung. The Inability to improve Oxygenation With Incr. in O2 concentration. The insult triggers a Massive Inflammatory response that causes the lung tissue to release inflammatory mediators (leukotrienes, proteases) that cause damage to the alveolar-capillary (A-C) membrane. As a result of the damage, the A-C membrane becomes more permeable, and intravascular fluid then leaks into the alveolar space, resulting in a Noncardiogenic Pulmonary Edema. The lungs become Stiff and Noncompliant, which makes Ventilation and Oxygenation less than optimal and results in increased work of breathing, tachypnea and alkalosis, atelectasis, and refractory hypoxemia. ARDS (fluids in alveoli), DIC (Disseminated Intravascular Coagulation) are always Secondary to something else (another disease process). – Impaired Gas Exchange. PreOxygenated with 100% O2, and Suction should be applied for no more than 10 seconds to prevent hypoxia. The nurse must wait 1-2 minutes between passes to ventilate to prevent hypoxia. Deep reBreathing should be encouraged. The Suction catheter should be No more than half the width of the artificial airway and inserted without suction. Don Sterile gloves if it is not have a closed suction system. Suction should be set at Medium Pressure (100-120 mm Hg for adults, 50-75 mm Hg for children) as Excess pressure will traumatize the mucosa and can cause hypoxia. Clients usually Cough as the catheter enters the trachea, and this helps loosen secretions. The catheter should be advanced until resistance is felt and then, to prevent mucosal damage, Retracted 1 cm before applying suction. You will ask every New Admission if he has an Advance Directive, and if not you will explain it, and he will have the option to sign or not. Alcohol: a Toxin that causes CNS Depression. Alcohol withdrawal generally starts within 8 hours after the last drink and peaks at 24-72 hours. Acute alcohol intoxication: Confusion, Coordination Impairment, Drowsiness, Slurred Speech, Mood Swings, and Uninhibited actions. Hypoglycemia. Chronic Alcohol Abuse/Alcoholism: Benzodiapepine (lorazepam, diazepam, chlordiazepoxide) – to Treat Gross Tremors, Seizures, Delirium symptom. Chlordiazepoxide: For Alcohol withdrawal. Don’t take with Alcohol (terrible N/V can occur) Thiamine (B1): to treat Wernicke Encephalopathy, a Serious complication that manifests as altered mental status, oculomotor dysfunction, and ataxia. Also can lead to death or neurologic morbidity (Korsakoff Psychosis). Give before or with IV Glucose. Alzheimer’s Disease: Chronic, progressive, degenerative cognitive disorder that accounts for more than 60% of All Dementias. Memantine: Cognition Enhancing medication. It can treat Dementia associated with Alzheimer's disease. Improve symptoms cognition, Daily function, Behavioral problems. Donepezil: Cognition Enhancing medication. Amyotrophic Lateral Sclerosis (ALS): a condition in which there is a Progressive, Degeneration of Motor Neurons in both the Upper & Lower Motor Neuron systems. Upper Motor Neuron issue: Hyper Reflexes Lower Motor Neuron issure: Absent Reflexes S/S: Limb weakness, Dysarthria (difficulty speaking), and Dysphagia. Iron: IM: should be given Z-track so they don't leak into SQ tissues IV: Iron Dextran (Imferon). Can cause hypersensitivity reaction (anaphylaxis), test dose needs to be given First. PO: give with Vitamin C or on an Empty stomach or Btw Meals. Place it on the back of the Month (Stain teeth). Expect Black/Green Tarry Stools. Take iron elixir with juice or water.... Never with milk (Vit D). Iron Poisoning: GI Bleed. Antidote: Deferoxamine Iron Deficiency Anemia: Microcytic anemia. S/S: Fatigue, Pallor, Fissures at the corner of the mouth, Spooning of the fingernail, Reduced exercise tolerance Thalassemia Major (Cooley’s Anemia): Microcytic anemia. S/S: Maxillary Hyperplasia, Frontal Bossing. Caused by: Defects in both Beta-chains of the Hgb molecule. Pernicious Anemia: Macrocytic anemia, Lack of required Intrinsic factor (B12 Deficiency) S/S: Pallor, Tachycardia, Sore Red Tongue (Beefy tongue), Enlarged Liver that can lead to R-sided HF. Take Vit. B12 for life. Shilling Test: Test for Pernicious Anemia. How well one absorbs Vit B12 Folate (Folic Acid) Deficiency: Macrocytic anemia. Risk: Alcoholism or Diet Low in Vegetables. S/S: Stomatitis, Ulcerations on the tongue. Dysphagia, Flatulence, watery Diarrhea Aplastic Anemia: Normocytic Anemia. Decline in blood cell production r/t to Bone Marrow Depression. Can cause an Extremely Low Hgb of 7 g/dL Severe Anemia: (Female hgb 11.7 ~ 15.5) Tachycardia. SOB (Dyspnea). Pallor. (Male hgb 13.2 ~ 17.3) Anorexic: Absence of Menstruation leads to Osteoporosis. Bulimia: Chipmunk Face. Antibiotic: Obtain Cultures before starting IV antibiotics. IV push should go over at least 2 Minutes. Always check for Allergies before Administering (especially PCN). Make sure Culture & Sensitivity has been done before First dose. Give Prophylactic Antibiotic therapy before any Invasive Procedure. Aminoglycocide ( _Mycin e.g. Vancomycin; except Erythromycin): Cause Nephrotoxicity and Ototoxicity. Adverse Effects are Bean Shaped - Nephrotoxic to Kidneys & Ototoxic to Ears Macrolide (Azithromycin, Erythromycin, Clarithromycin): can cause Prolonged QT interval. My lead to Torsade de Pointes (Life-threatening Arrhythmias). Antacids will Limit the Absorption of the antibiotics. Concurrent use of other prolong QT interval (Amiodarone, Sotalol, Haloperidol, Ziprasidone, Azole, Antifungals) will Incr. the risk. Risk of Hepatotoxicity: when taken in High doses. Report Elevated AST and ALT. Sulfamethoxazole/Trimethoprim: (Tx for UTI, PJP). Don’t take if Allergic to Sulfa drugs. Drink plenty of fluids. S/S: Diarrhea Penicillin Allergy: No Cephalexin, Cephalosporin. Amphotericin B: (antifungal) causes Hypokalemia. Premeditate Before giving. Pts will most likely get a Fever. Mebendazole: (antiparasite) Take it with High Fat diet (increases absorption). Anticholinergic Effects: Assessment Blocks the action of Acetylcholine (Neurotransmitter), blocks involuntary muscle movement. Many antihistamine (diphenhydramine) have anticholinergic effect. Dry mouth (Xerostomia)- can't spit Urinary retention- can't pee Constipated- can't poop Blurred vision- can't see Decreased Acetylcholine is related to Senile Dementia. Glucagon increases the effects of Oral Anticoagulants (Rivaroxaban). Appendicitis: Pain is in RL quadrant with Rebound Tenderness. Continuous. Guarding. Anorexia. N/V. McBurney’s Point – pain in RLQ indicative of appendicitis. Position on Right side with legs flexed After Appendectomy. Risk for Peritonitis. Peritonitis: Mucus in Ileal Conduit is expected. Blumberg’s Sign: Presence of rebound tenderness in the abdomen. Aortic Dissection: Risk Factor: HTN S/S: (Ascending)- Chest Pain, Radiate to the Back (Descending)- Abrupt in Onset, “Worst Ever” “Tearing”, Ripping Pain, Moving Back Pain, Epigastric Pain Abdominal Aortic Aneurysm (AAA): Definitive Diagnosis- CT scan. Hypoactive BS for few days after the Surgery. Computed Tomography (CT) Scan: Assess Allergies Osteoarthritis: a Degenerative Disease, causing pain With Activity. Inflammation occurs, but the joint does Not usually become swollen or red. It commonly affects the Larger, weight-bearing joints and affects both genders equally. Rheumatoid Arthritis: causes Pain and Inflammation After periods of rest. It affects the Small joints (like fingers) and is more common in women. Pain is usually the Highest Priority. Heat for Chronic (Rheumatoid Arthritis): Warm Shower/Bath in the Morning. Swimming is the Best. Order of Assessment: Inspection, Palpation, Percussion and Auscultation. Except… Abdomen Assessment: Inspect, Auscultate, Percuss then Palpate (Last, bc it may induce pain) Assessment with Kids: Least invasive to Most invasive. An example of when you would Implement Before going through a bunch of Assessments is when someone is experiencing Anaphylaxis. Get the Ordered Epinephrine in them STAT, especially if they clearly States the S/S (Difficulty Breathing, Increasing Anxiety, etc.) Anaphylaxis is a Medical Emergency. Epinephrine Injection is the Only option for treating anaphylaxis. Asthma: Wheezing on Expiration. Coughing Without other s/s is suggestive of asthma. If they stop Wheezing; it could mean it is Worsening. Hyperrsonance: Percussed over Hyperinflated (air) Lung (Asthma, Emphysema). Asthma and Arthritis: Swimming Best Avoid ASA, NSAID (ibuprofen), and Beta Blockers. Asthma has Intercostal Retractions (be Concerned) Exacerbation: Acute, Distress. Wheezing, Dyspnea, Sternal Retraction, Anxiety. Status Asthmaticus: Acute, Prolonged, and Severe Asthmatic Attack that is unresponsive to usual treatment. Hospitalization is usually required. When using a Bronchodilator inhaler in conjunction with a Glucocorticoid inhaler, administer the Bronchodilator First. Theophylline (Bronchodilator): Therapeutic Drug level: 10-20 Tx: of Asthma or COPD Increases the Risk of Digoxin Toxicity, Decreases the effects of Lithium and Phenytoin. Causes GI upset, give with food. Cromoglicic Acid (helps reduce Inflammation): an inhaler used to treat Allergy Induced Asthma. Not for acute asthma attack. Before Pulmonary Function Tests (PFT's): Hold the Bronchodilators. Stop Smoking for 4 hr prior. Incentive Spirometry: 1) Sit upright 2) Exhale 3) Insert mouthpiece 4) Inhale for 3 sec., then Hold for 10 sec. For Prevention of Atelectasis. Atropine: used to Decrease Secretions Atropine Blocks Acetylcholine (remember it reduces secretions). Atropine Overdose: Hot as a Hare (Temp), Mad as a Hatter (LOC), Red as a Beet (Flushed face) and Dry as a Bone (Thirsty) ADHD: Inattention, Hyperactivity, Impulsivity. Methylphenidate/ Ritalin: Assess for Heart related side effects report immediately. May need a Drug Holiday- it Stunts Growth. Dextroamphetamine: may alter Insulin needs, Avoid taking with MAOI's, take in Morning (Insomnia possible side effect) Atomoxetine: Norepinephrine-Specific Reuptake Inhibitor, and can be used for Depression. Autonomic Dysreflexia/Hyperreflexia: Neuro T6 or above. Life-threatening emergency. Uncompensated SNS stimulation (Inhibited Sympathetic Response) Tigger by: Bladder distention and Bowel impaction S/S: pounding/severe HA, profuse Sweating (Diaphoresis), Nasal Congestion, Bradycardia (30~40), Flushing, Piloerection (goose bumps), Nausea, Seizure, Uncontrolled HTN. Can occur weeks to years after the injury. Tx: Place client in sitting position (Elevate Hob) first before any other implementation. High Fowler’s (90o): assist w/ventilation & prevention of HtN Stroke! Loosen constrictive clothing (Decr. skin stimulation) SBP> 300mmHg. Administer antihypertensive meds (may cause stroke, MI, seizure) Most spinal cord injuries are at the Cervical or Lumbar regions. Spinal Shock occurs Immediately after Spinal Injury Halo: remember Safety First; have a Screwdriver nearby. Myelogram: NPO 4-6hr, allergy hx, Phenothiazine, CNS depressants, and Stimulants withheld 48hr prior, table will be moved to various positions during test. Post: Neuro q2-4, Water Soluble HOB Up. Oil Soluble HOB Down (Lie Flat Supine, to prevent HA, and Leaking of CSF) oral analgesics for HA, encourage PO fluids, assess for Distended Bladder, Inspect Site. Benign Prostatic Hyperplasia (BPH): Enlarged Prostate. Reduced size & force of urine. Tamsulosin, Terazosin, Prazosin (Antitensive med): Alpha1 Antagonist: Cause Orthostatic Hypotension & Dizziness. Take it at Bedtime to avoid Syncope and Dizziness or Lightheadedness. Water Intoxication will be Evidenced by Drowsiness and Altered Mental Status in a patient with TURP Syndrome, or as an Adverse Reaction to Desmopressin (for Diabetes Insipidus). Benzodiazepine: Alprazolam/ Xanax Clonazepam/ Klonopin Diazepam/ Distat/ Valium: Status Epilepticus & to treat Anxiety. Lorazepam/ Ativan Midazolam/ Versed: Surgery Zolpidem/ Ambien During Continuous Bladder Irrigation (CBI): Catheter is Taped to Thigh so Leg should be kept Straight. No other positioning restrictions. Maintain Urine that’s Pale Pink-Tinged. Red would indicate Active Bleeding. Bladder Cancer: Painless Hematuria A patient with a Low Hemoglobin and/or Hematocrit should be evaluated for Signs of Bleeding, such as Dark Stools. Blood Transfusion: Sign of Allergies in order: 1. Flank pain 2. Frequent swallowing 3. Rashes 4. Fever 5. Chills Botox (Botulin Toxin): Used with Strabismus (Patch the Good eye, so the Weaker eye can get stronger). To relax Vocal Cords in Spasmodic Dysphonia. Bowel Sounds: Normal: High-Pitched, Gurgling sounds. Cardiovascular Bruits: (Swishing, Humming, Buzzing): usually indicate Arterial narrowing (Obstruction) or dilation (Aneurysm). After Surgery, BS are Absent first 24-48 hrs. Return to the Small intestine in 24hr; Large intestine may delayed 3~5 days. Borborygmi Sounds: are Loud, Gurgling sounds suggesting increased Peristalsis (Gastroenteritis, Diarrhea). Obstructed Ileostomy (Bowel Obstruction): S/S: N/V, Abd Distention, Decr. Stool. Ileostomy: Liquid Stool (Bypass the Colon). Low Fiber Diet: White rice, Pasta, Refined grains. Avoid High Fiber (Popcorn, Coconut, Brown Rice, Multigrain bread), Stringy Veg (Celery, Broccoli, Asparagus), Seeds or Pits (Strawberry, Raspberries, Olives), Edible Peels (Apple, Cucumber, Dried fruit). Colon: Fluid & Electrolyte Absorption, Vit K Production. Don’t Fall for ‘reestablishing a normal bowel pattern’ as a priority with Small Bowel Obstruction. Because the patient Can’t take in oral fluids ‘Maintaining Fluid Balance’ comes First. Small Bowel Follow-Through (SBFT): Sequential X-ray images to visualize the Structure and Function. Barium is Ingested, and X-ray images are taken every 15-60 minutes to visualize the barium as it passes through the small intestine. Using this technique, Decreased Motility (eg, Ileus), increased motility (eg, Malabsorption Syndromes), Fistulas, or Obstructions are identified. Fast 8 hours Prior to the examination. The test usually takes 60-120 minutes, but if obstruction or decreased motility is present, it can take longer. Drink plenty of Fluids After the examination to facilitate barium Removal. Chalky stools may be present 24-72 hours after the examination. If brown stools do Not return after 72 hours or abdominal pain or fullness is present, contact the HCP. Burns: Rule of Nines Head and Neck= 9% Each upper ext= 9% Each lower ext= 18% Front trunk= 18% Back trunk= 18% Genitalia= 1% Assess for Smoke Inhalation/ Burns: 1st Degree - Red and Painful 2nd Degree - Blisters 3rd Degree - No Pain because of Blocked and Burned nerves. Tx: High-Flow O2 (100%) to displace CO & Cyanide from hgb. (1st 24 hour): Lactated Ringer’s: 4mL/kg HyperCalcemia: muscle weakness, lack of coordination, abd pain, confusion, absent tendon reflexes, sedative effect on CNS HypoCalcemia: CATS – Convulsions, Arrhythmias, Tetany, Spasms and Stridor. Trousseau’s & Chvostek’s. Ca2+ absorption is impaired when taken in excess of 500 mg per dose. Taken within an hour of meals as food incr. Ca2+ absorption. Constipation is a frequent side effect of Ca2+ supplements. For Chronic Kidney Disease take Ca2+ supplements before meals, to reduce Phosphorus levels Non-dairy sources of Ca2+: Rhubarb, Sardines, Collard Greens. Carbon Monxide (CO): More readily binds to Hemoglobin than O2. Pulse Oximeter: Can’t Differentiate between O2 & CO. CO Poisoning: S/S: HA, Dizziness, Fatigue, Nausea, Dyspnea. Tx: 100% O2. Serum CarboxyHemoglobin Test to Confirm Diagnosis. Normal Value: < 5% Non Smoker. < 10% Smoker. Carbon Dioxide (CO2) Narcosis: High K+ (Expected- Hydrogen floods the cell forcing K+ out). Causes Increased Intracranial Pressure. Cataract: S/S: Painless Vision Loss, Cloudy, Blurry vision, Opacity of the lens. Worst at Night. Tx: Lens Removal Surgery After Cataract Surgery: Sleep on Unaffected side with a Night Shield for 1~4 weeks. Celiac Disease: Barley, Rye, Oats, Wheat. Cephalhematoma (Caput Succinidanium): Resolves on its own in a few days. This is the type of Edema that Crosses the Suture lines. Cerebral Palsy: Poor muscle control due to birth injuries and/or Decrease Oxygen to brain tissues. Head Injury: Elevate HOB 30o to Decr. Intracranial Pressure. No Nasotracheal Suctioning with Head Injury or Skull Fracture. Basilar Skull Fracture: Otorrhea (discharge from the external ear) Orbital Fracture: Battles Sign and Raccoons Eyes Cushing Ulcer: Gastric ulcer associated with IICP. (r/t Brain Injury) Mannitol: Head injury Medication (Osmotic Diuretic): Decr. Cerebral Edema, Decr. ICP, Incr. Urine Output Crystallizes at Room Temp so Always use Filter needle. TIA (Transient Ischemic Attack): Mini Stroke with No Dead Brain Tissue. Short period of cerebral Ischemic. S/S: Brief period of Loss of Vision, Hemiparesis and Slurred Speech. CVA (CerebroVascular Accident): with Dead Brain Tissue. Permanent Deficits. Horner Syndrome. R-CVA: Left-sided hemiplegia, Impulsive, Lack Judgment L-CVA: R-sided hemiplegia, Impairment in Speech and Language. Broca’s area (Frontal): Expressive Aphasia. Wernicke’s area (Parietal/Temporal): Receptive Aphasia. TPA- Aminocaproic Acid Stroke is Not considered Stabilized until approximate 48hr pass without changes. Cerebral Angiogram: Prep: well Hydrated, lie Flat, site Shaved, pulses Marked Post: keep Flat 12-14hr, check Site & Pulses, force Fluids. Subarachnoid Hemorrhage: Emergent, Serious presentation often described as the "Worst Headache of My Life." The onset is usually Abrupt due to rupture of the vessel; High Mortality from recurrent bleeding. Chemotherapy: S/S: Oral mucosa, n/v (GI), Decr. Blood cell count (Bone Marrow) Neutropenic Precautions: No Yogurt (has Live Cultures), No Milk, No Fresh fruit or veggies. Radiation Therapy: Risk for Leukopenia. Infection kills cancer patients. Cisplatin: May cause Kidney injury. Vincristine: For Leukemia (Risk for Epistaxis bc of Low Platelets) Given IV only. Methotrexate: For RA & Psoriasis. Hepatotoxic Teratogenic. Immunosuppressant. Folate antimetabolite. (Risk for infection, No Live Vaccine). Infliximab, Adalimumab, Ehanercept (Tumor Necrosis Factor Inhibitors): For RA, Crohn disease, Psoriasis. Risk for infection, No Live Vaccine. Test for TB every year while on the medication. Cyclophosphamide: Complication: Hemorrhagic Cystitis (bladder inflammation/bloody urine). Tx: Drink plenty of fluids or IV hydration. Mesna: Detoxifying agent. Prophylactic agent in reducing the incidence of cyclophosphamide/ ifosfamide-induced Hemorrhagic Cystitis. Asparaginase: Test For Hypersensitivity Before the administration. Common sites for Metastasis: Liver, Brain, Lung, Bone, and Lymph. Lymphedema: Complication from Cancer. When the Lymph System is Blocked or Damaged. Fluid builds up in soft body tissues and causes Swelling Colorectal Cancer: Shouldn't have Cantaloupe before Fecal Occult Blood Test (FOBT), because Cantaloupe is high in vit C and vit C causes a False Positive for Occult Blood. FOBT: Detect blood. 1. Apple Stool first then dry. 2. Then Solution. Tamoxifen: For Breast cancer. Report changes in Visual Acuity, the Adverse effect could be Irreversible. Risk for Endometrial Cancer (Heavy Period) & Thromboembolic Event. Hemovac: used after Mastectomy. Empty when Full or q8hr, remove plug, empty contents, place on flat surface, cleanse opening and plug with Alcohol sponge, compress evacuator completely to remove air, release plug, check system for operation. Don’t place Immunosuppressed pt With Any pt with an Infectious disease or Open wound. Basal Cell Carcinomas: Translucent, Raised, and Smooth. Rarely Metastasize or cause death. Most Common. Squamous Cell Carcinomas: characterized by Local Invasion. Fast Growing and Infrequent Metastasis. They are Red Nodules with Crust or Ulceration. Malignant Melanomas: Appears Black or Brown with Irregular Borders. Often Metastasize. Most Deathly form of Skin Cancer. Least Common. Chest Tube Drainage System: Placed in the Pleural space. If chest tube is dislodged, immediate action should be to apply a Sterile Occlusive Dressing (eg, petroleum jelly dressing) taped on 3 sides. This permits air to escape on exhalation and inhibits air intake on inspiration. Notify the HCP and arrange for the reinsertion of another chest tube. Suction Control Chamber: Set at -20 cm H2O to maintain Negative pressure in the system. Bubbling will occur when suction is applied. Water Seal Chamber of the chest tube drainage system is filled with Sterile water and acts as a One-Way Valve preventing air from entering the client's chest cavity. Tidaling: The water level in the water seal chamber Rises and Falls with Inspiration and Expiration. (Maintaining appropriate Negative pressure/ indicating Proper function of the chest tube drainage system) Air Leak Gauge: (part of the Water Seal Chamber) allows for assessment of air leaks. Continuous Bubbling: indicates an Air Leak in the system. Drainage Collection Chamber: which Fluid from the client's Pleural Cavity will collect; the nurse will assess the color and amount and record the output. Sucking Stab Wound: Immediately dress the wound and tape it on Three sides which allows air to Escape. Do not use an occlusive dressing, which could convert the wound from Open pneumo to Closed one. Tension Pneumothorax: develops when air enters the pleural space but Cannot escape. Increased intrapleural pressure and excessive accumulation of air can apply pressure to the heart and great vessels and drastically decrease cardiac output. An occlusive dressing taped on 4 sides would prevent the air in the pleural space from escaping on exhalation and would increase the risk for a tension pneumothorax. Tension pneumothorax trachea shifts to Opposite side. Tracheal Deviation: Reduce Cardiac Output & Hypotension. After that get your Chest Tube Tray, Labs, IV. Removal: Take a breath and hold it or Bare down by attempting to Exhale through the mouth and nose with your lips held Closed. Cholecystitis: Limit Fatty foods. Fat stimulates the release of Bile form the Gallbladder. N/V, Restlessness, Diaphoresis. Referred to the R Scapula & Epigastric tenderness. Murphy’s Sign: Pain w/ palpation of Gallbladder (RUQ) area. Cholera: Infection of the small intestine by some strains of bacterium Vibrio Cholerae. Acute Diarrheal Disease; Rice Watery Stool. Chronic Obstructive Pulmonary Disease (COPD): the Baroreceptors that detect the CO2 level are destroyed. Therefore, O2 level must be Low bc High O2 Conc. blows the patient’s Stimulus for Breathing. 2L Nasal Cannula or less (Hypoxic Not Hypercapnic drive), PaO2 of ~60 Chronic CO2 retainer: SaO2 90% (Normal) CO2 causes Vasoconstriction. Venti Mask for Distress COPD pt. Tiotropium, Ipratropium, Benztropine. Bronchitis: Rhonchi: Continuous, Low-pitched Wheezes usually heard on Expiration that sound like moaning or snoring. The sound originates from air moving through large airways (Bronchi) filled with Mucus Secretions Tx: Medication, Mobilization of secretions. Emphysema: Barrel-Chest. The Stimulus to breathe is Low PO2, Not Increased PCO2 like the rest of us, so don’t slam them with Oxygen. Encourage Pursed-Lip Breathing which Promotes CO2 Elimination. Encourage up to 3000mL/day Fluids, High-Fowlers and Leaning Forward. Cognitive behavioral therapy (CBT): requires that the client learn about the disorder and engage in self-observation and monitoring, relaxation techniques, desensitization activities, and changing negative thoughts. 5 basic components: Education about the client's specific disorder Self-observation and monitoring - the client learns how to monitor anxiety, identify triggers, assess the severity Physical control strategies – deep breathing and muscle relaxation exercises Cognitive restructuring – learning new ways to reframe thinking patterns, challenging negative thoughts Behavioral strategies – focusing on situations that cause anxiety and practicing new coping behaviors, desensitization to anxiety-provoking situations or events Cranial Nerves: Sensory=S Motor=M Both=B Oh (Olfactory I) Some Oh (Optic II) Say Oh (Oculomotor III) Marry To (Trochlear IV) Money Touch (Trigeminal V) But And (Abducens VI) My Feel (Facial VII) Brother -Bell’s Palsy A (Auditory VIII) Says Girls (Glossopharyngeal IX) Big -Swallowing & Gag reflex Vagina (Vagus X) Bras - Swallowing & Gag reflex And (Accessory XI) Matter Hymen (Hypoglassal XII) More Assessing Extraocular Eye Movements: Check Cranial Nerves 3, 4, and 6. Cystic Fibrosis: Salty Skin. Fatty Stools. Diet: Low Fat, High Sodium, Fat Soluble Vitamins ADEK. Pancreatic Enzymes are taken with each meal. Respiratory Problems are the Chief concern: Treat with Aerosol Bronchodilators, Mucolytic. Cystitis: Burning on Urination. Frequency, Urgency, Suprapubic Discomfort, Hematuria. CytoMegaloVirus: Ganciclovir: For CMV Retinitis. Pt will need regular Eye exams, report Dizziness, Confusion, or Seizures Immediately. DecortiCate: (Flexor) Toward the 'Cord'. Cortex involvement. Problem with Cervical Spinal Tract or Cerebral Hemisphere. DecerEbrate: (Extensor) The Other way (Out). Cerebellar, Brain Stem involvement. Problem w/in Midbrain or Pons. Weight is the Best indicator of Dehydration. 1kg = 1L Diagnose of Delirium: Acute Mental Changes, Inattention with disorganized thinking, Altered Level of Consciousness, Hallucination. Dengue Fever: Hemorrhagic. Petechiae or (+) Herman’s sign. MonoAmine Oxidase Inhibitors (MAOI): Antidepressant. Isocarboxazid Phenelzine Selegiline Tranylcypromine Avoid Tyramine containing foods Don’t take it with SSRI; at least 14 days in between. Administered in the morning, as sleep dysfunction is common. Increased risk for Suicidal Ideation, particularly children, adolescents, and young adults. The risk of suicidal thoughts can be more prevalent when Starting the medication or with dose Increases. Feelings of hopelessness or despair must be evaluated to assess if suicidal ideation or thoughts of self-harm are present. Safety over Nutrition with a severely depressed client. Depression often manifests itself in Somatic (Relating to the Body) ways, such as Psychomotor retardation, GI complaints, and Pain. Amitriptyline: Tricyclic Antidepressant. Somatic Symptom Disorder (SSD): Mental disorder which manifests as physical symptoms but cannot explained fully by a general medical condition. Selective Serotonin Reuptake Inhibitors (SSRIs): Sertraline Fluoxetine Citalopram Paroxetine Take about 3 weeks to Work. Sertraline: Agitation, Sleep disturb, and Dry mouth St John's Wort: used to treat Depression and Anxiety. Mimics the action of SSRI by Increasing available Serotonin in the brain. Taken in combination with an SSRI, may cause an Excess of Serotonin, resulting in Serotonin Syndrome. Serotonin Syndrome: characterized by Mental Status Changes (anxiety, agitation, disorientation) Autonomic Dysregulation (hyperthermia, diaphoresis, tachycardia/hypertension) Neuromuscular Hyperactivity (tremor, muscle rigidity, clonus, hyperreflexia) Mydriasis (dilation of pupil) Caused by: taking More Than One or an Overdose of Antidepressant med that incr. Serotonin levels. Diabetes Mellitus (DM): Polyuria, Polydipsia, Polyphagia. Metformin: Can’t be Given w/Contrast for CT Scan (Kidney Injury). Hold for 48hr. HbA1c - test to assess how well blood sugars have been controlled over the past 90-120 days. 4- 6 corresponds to a blood sugar of 70-110; 7 is ideal for a diabetic and corresponds to a blood sugar of 130. Diabetic ketoacidosis (DKA): when body is breaking down fat instead of sugar for energy. Fats leave Ketones (acids) that cause pH to decrease. DKA is rare in diabetes mellitus type II because there is enough insulin to prevent breakdown of fats. Serum acetone and serum ketones Rise in DKA. As you treat the Acidosis and Dehydration expect the potassium to Drop rapidly, so be ready, with K+ Replacement. While treating DKA, bringing the Glucose Down too far and too fast can result in Increased ICP due to water being pulled into the CSF. Wherever there is Sugar (Glucose) Water Follows. S/S: Kussmauls breathing (Deep Rapid RR), N/V, Abd Pain (Acidic Ketones). Can lead to Death. Fluids are the most important intervention with HHNS as well as DKA, so get Fluids going first. With HHNS there is No Ketosis, and No Acidosis. Potassium is Low in HHNS (due to Diuresis). Second Voided Urine most accurate when testing for Ketones and Glucose. Oral Hypoglycemic: Typical Adverse reaction: Rash, Photosensitivity Extra Insulin may be needed for a patient taking Prednisone (Steroids cause Increased Glucose). Diabetes Insipidus (decreased ADH): Thirst, Dehydration, Weakness, Excessive Urine Output (Diluted Urine) Administer Pitressin SIADH (increased ADH): Change in LOC, Decr. deep tendon reflexes, Tachycardia, n/v, HA, No Urine Output (Conc. Urine). HypoNa+, HypoCa2+. Administer Declomycin, Diuretics Hemodialysis (HD): Solutes (e.g. Urea) are removed from the blood. Complication: Dialysis Disequilibrium Syndrome (DDS) Allen’s Test: occlude both Ulnar and Radial artery until hand blanches then release ulnar. If the hand pinks up, ulnar artery is good and you can carry on with ABG/radial stick as planned. (To check for sufficient blood flow) ABG: must be put on Ice and Whisked to the lab. When drawing an ABG, you need to put the blood in a Heparinized tube, make sure there are no bubbles, put on ice immediately after drawing, with a label indicating if the pt was on room air or how many liters of O2. Peritoneal Dialysis (Cath Tenckhoff): Normal to have Abdominal Crap, Blood tinged outflow and Leaking around site if it was placed in the last 1-2 wks. When Outflow is Inadequate: Turn pt from Side to Side before checking for kinks in tubing. Monitor for Resp. Distress (e.g. Crackles) Cloudy outflow (Infection) Dialysis Disequilibrium Syndrome (DDS): Life-Threatening! Solutes (e.g. Urea) are removed more quickly from the blood than from the brain cells and Cerebrospinal fluid, creating a Concentration gradient that can lead to Excess Fluid in the brain cells and Increased Intracranial Pressure (IICP). Characteristic Neurologic manifestations include n/v, ha, restlessness, change in mentation, seizure, and Pupillary changes. Can be prevented by Slow/Stop the Rate of dialysis. Can progress to Coma and Death. Tx: Decrease Cerebral Edema and manage symptoms. HCP should be contacted Immediately. Diaphragm must stay in place 6 hours After intercourse. They are also fitted so must be refitted if you Lose or Gain a significant amount of Weight. Acid Ash Diet: Bread, Cheese, Corn, Cranberries, Meat, Poultry, Plums, Prunes, Pastry. Alk Ash Diet: Milk, Rhubarb, Salmon, Vegetables. Diphtheria: Pseudomembrane formation. Serious bacterial infection that can cause Organ Damage and Breathing problems. Disseminated Herpes Zoster: Airborne Precaution Localized Herpes Zoster: Contact Precaution A nurse with a Localized herpes zoster can care for patients as long as the Patients are Not Immunosuppressed and the lesions must be Covered. Diverticulitis: Inflammation of the Diverticulum in the Colon. Often in the Sigmoid Colon. Pain is around LL quadrant. Low Residue (Low Fiber), No Seeds, Nuts, Peas. Complication: Peritonitis (LUQ Pain). Down Syndrome: Protruding Tongue. Floppy muscle tone. To Prevent Dumping Syndrome (Post-Operative ulcer/stomach surgeries): eat in Low-Fowler’s during meals, lie Down after meals for 20-30 minutes (Decrease Peristalsis), Restrict Fluids during meals (wait 1hr), Low CHO and Fiber diet, Incr. Fat and Protein, Small frequent meals, Eat slowly. S/S: Dizziness, Hypotension, Syncope, Generalized Sweating, Tachycardia, Palpitation, n/v, Diarrhea, Abd pain. Gastrojejunostomy (Roux-En-Y Surgery): Risk for Dumping Syndrome. Iron Deficiency Anemia. Cobalamin Deficiency. DVT (Homan’s Sign): who need Enoxaparin, should not be Delegate. Does Not Need to be on bed rest, unless they have Severe Edema or Leg Pain. Edema: is in the Interstitial Space Not in the Cardiovascular Space. Electrocardiogram (EKG): Atrial Fibrillation: Cardioversion: Anterior-Posterior Paddle Placement- One paddle is places just to the Right of the sternum at the Fourth Intracostal space and the Other paddle is placed between the scapulae on the Back. The Shock runs Diagonally through the chest. Cardiac Output Decreases with Dysrhythmias. Dopamine increases BP. Med of choice for Vtach is Lidocaine/ Amiodarone (antiarrhythmic). Med of choice for SVT is Adenosine. Med of choice for Bipolar is Lithium. Med of choice for Asystole (no heart beat) is Atropine/ Epi Med of choice for Paroxysmal Atrial Tachycardia is Adenosine. Amiodarone is effective in both Ventricular and Atrial complications & Vfib/Vtach. V. Bigeminy. Flecainide (an antiarrhythmic): Limit Fluids and Na+ intake, because Na+ increases Water Retention which could lead to Heart Failure. PT/PTT are Elevated when patient is on Warfarin. No ASA & NSAID. Warfarin- Vitamin K Enoxaparin: LMWH. Monitor CBC to asses for Thrombocytopenia. Electroencephalogram (EEG): Before: Hold meds for 24-48 hrs prior, No Stimulants for 24hr Before, No caffeine or cigarettes for 24 hrs Prior, Can eat, pt Must Stay Awake night. During: Pt may be asked to Hyperventilate (3-4min) and watch a Bright flashing light. After: Assess pt for Seizures (Increased Risk) After Endoscopy Check Gag Reflex. Administration of Enema: position pt in Left side-lying (Sim's) with Knee Flexed. Fleet Enema: To Stimulate defecation & Relieve Constipation. Neomycin Enema: Administer before Bowel Surgery to decr. bacteria in the Colon. Epiglottitis: No Throat Inspection. Severe Inflammatory Obstruction. Drooling, Dysphonia (hoarse voice), Dysphagia (difficulty swallowing). Tripod Position. Inspiratory Stridor (Airway Distress). Caused by: Hib w/O Vaccine. Tx: Endotracheal Intubation w/ Tracheostomy Kit Standby. Dealing with Fire in Inpatient Setting (RACE): Rescue Activate the fire Alarm, Code Red Confine/ Close the Doors/Windows Extinguish the Fire. No Water. Using the Extingusher (PASS) Pull the Pin Aim the Nozzle Squeeze the Handle Sweep back and forth over the fire. Fractured Hip: S/S: External Rotation, Shortening, Adduction. Fat Embolism: Blood tinged sputum (r/t Inflammation), Incr. ESR, Respiratory Alkalosis (Not Acidosis r/t Tachypnea), Resp. Distress, Altered Mental Status, Hypocalcemia, Incr. serum Lipids, "Snow Storm" Effect on CXR. Petechiae (Treated w/ Heparin) in the chest, axillae, soft palate. Heparin Prevents Platelet Aggregation. No ASA & NSAID. Monitor PTT. Antidote: Protamine sulfate Reduce the Risk: Minimizing the move of a fractured long bone &early stabilization of the injury w/ surgery. Tx? Greenstick Fractures: usually seen in Kids bone breaks on one side and bends on the other Compartment Syndrome: an Emergency situation. Paresthesia and Incr. Pain are classic symptoms. Neuromuscular Damage is Irreversible 4-6 hours After onset. Cast: Petal the rough edges of a plaster cast with tape to avoid skin irritation. Itching under cast area- cool air via blow dryer, ice pack for 10- 15 minutes. Never use anything to scratch area Place Wheelchair Parallel to the bed on the side of Weakness. “Step Up” when picturing a person going Up Stairs with crutches. The Good leg goes Up first, followed by the crutches and the bad leg. The opposite happens going Down. The Crutches go first, followed by the good leg. COAL (Cane Walking) Cane Opposite Affected Leg 4 Point Gait: Move the Right crutch forward. Move the Left foot forward. Move the Left crutch forward. Move the Right foot forward. GastroEnteritis (Stomach Flu): Trimethobenzaminde: Tx for Nausea associated with Gastroenteritis (Stomach Flu) and PostOp n/v GastroEsophageal Reflux Disease (GERD): Barrett’s Esophagus (Erosion of the Lower portion of the Esophageal Mucosa) Patients should lay on their Left side with the HOB elevated 30 degrees. Weight Loss. Small Frequent Meals Nonfat milk Reduces reflux by Incr. Lower Esophageal Sphincter Pressure. No Carbonated drink (Incr. Pressure). Peptic Ulcers (Coffee-Brown Emesis) caused by H. Pylori (duodenal ulcer) are treated with Metronidazole (can cause dark-urine [Expected]), Clarithromycin, and Omeprazole. This Treatment Kills bacteria and Stops production of stomach acid, but does Not heal ulcer. Cause: NSAID (Celecoxib, Naproxen) Gastric Ulcer Pain: occurs 30 minutes to 90 minutes after eating, not at night, and doesn't go away with food. Pantoprazole/ Protonix (PPI): given Prophylactically to Prevent Stress Ulcers. Omeprazole (PPI): Take it Before breakfast (72 hour duration) Combined with Warfarin (Take it at Evening), Can Incr. INR. Metoclopramide/ Reglan (Antiemetic): prescribed for the GERD. Decr. Post-up Nausea by Promoting Gastric Emptying. Common Side Effects: Sedation, Fatigue, Restlessness, HA, Sleeplessness, Dry mouth, Constipation, Diarrhea Extrapyramidal adverse effects, including tardive dyskinesia (TD), especially in older adults w/ long-term use. TD Symptoms: Call HCP if develops. Protruding and twisting of the tongue Lip smacking Puffing of cheeks Chewing movements Frowning or blinking of eyes Twisting fingers Twisted or rotated neck (torticollis) Cimetidine (H2 antagonist): Antacid and Antihistamine. Take with Food. Caution with Elders. Interacts with a lot of things. Aluminum Hydroxide/ Amphojel: Antacid and Phosphate Binders. Tx of GERD and Kidney Stones. Risk for Constipation. Long term use leads to Weaker Bones (Decr. Phosphates, Incr. Ca2+ (from the Bones). Sevelamer HCl (Phosphate Binder): Take with food. Sucralfate (Antacid): Risk for Constipation. Tx of Duodenal Ulcers. Coats the ulcer/Mucosal Barrier (take one hour Before meals to Coat the stomach). Create Viscous Substance Forms a Protective Barrier. Misoprostol: Prevent Stomach Ulcers caused by NSAIDs. Give Antacid to a Mechanically Ventilated patient w/ NG tube if the pH of the Aspirate is < 5.0, Checked at least every 12 hrs. Glasgow Coma Scale Eye opening (Maximum = 4) 4 - Spontaneous (open with blinking at baseline) 3 - To speech 2 - To pain only 1 - None (C - Not assessable [eg, trauma, edema]) Verbal response (Maximum = 5) 5 - Oriented 4 - Confused (converses but confused, disoriented) 3 - Inappropriate (inappropriate words) 2 - Incomprehensible (sounds, no words) 1 - None (T - Not assessable [intubated]) Motor response (Maximum = 6) 6 - Obeys commands for movement 5 - Localizes to pain 4 - Withdraws from pain 3 - Flexion in response to pain (decorticate posturing) 2 - Extension in response to pain (decerebrate posturing) 1 - None Use best response for each category (range, 3-15). Coma: Does not open eyes, does not follow commands, and does not utter understandable words; GCS 3-8. Head injury classification: Mild, GCS 13-15; moderate, GCS 9-12; severe, GSC ≤8. Below 8 you are in Coma. Intubated for Airway Protection. Dysphagia: Difficulty Swallowing (Risk for Aspiration) Dysarthria: Weakness of the Muscles for Speech (mumble, lisp) Aphasia: Impaired Communication (Words don’t make Sense) Apraxia: Loss of ability to perform a movement (clipping, whistling) Glaucoma: Intraocular Pressure is greater than the normal (22 mm Hg) Painful, Vision Loss, Tunnel/gun barrel/halo Vision (Peripheral Vision Loss) Pilocarpine/Miotics: to Constrict the pupils. Acetazolamide: Don’t take if allergic to Sulfa drug. Can cause HypoK+. Also can treat High altitude sickness. Timolol Maleate/Timoptic (Beta-adrenergic blocker): Eye drops. No Atropine. Primary Open-Angel Glaucoma: “Tunnel” Vision. Slow. Painless. Primary Angel-Closure Glaucoma: Medical Emergency! Apply eye drop to conjunctival sac and after wards apply pressure to nasolacrimal duct / inner canthus OU- both eyes OS- Left eye OD- Right eye (dominant Right eye- just a tip to remember) Gonorrhea is a Reportable Disease. Goodpasture’s Syndrome: Rare, Autoimmune Disease that affect’s Kidneys & Lungs. ……………………………continued……………… [Show More]
Last updated: 1 year ago
Preview 1 out of 89 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 08, 2021
Number of pages
89
Written in
Additional information
This document has been written for:
Uploaded
Jan 08, 2021
Downloads
0
Views
101